Immunology 1 Lectures 1 4 5 9 Ayesha
- Slides: 26
Immunology 1 Lectures 1, 4, 5, 9 Ayesha Ali
Lecture 1 1. Explain the importance of immunology for human health. 2. Summarise the two basic strategies used by the immune system to recognise danger and initiate a response. 3. Innate versus adaptive immunity: differentiate between innate and adaptive immune responses, comparing the timescales in which they occur. 4. Clonal selection: summarise the concept of clonal selection, and its role in immune responses.
LO 1. Explain the importance of immunology for human health • Protection: -Distinguishes ‘self’ from ‘non self’ -Identifies danger signals • Homeostasis: involved in repair Immunopathology – balance between eliminating pathogen and not harming the host If things go wrong: § SCID § Cancer § Autoimmune disease e. g. MS, Coeliac § Allergy
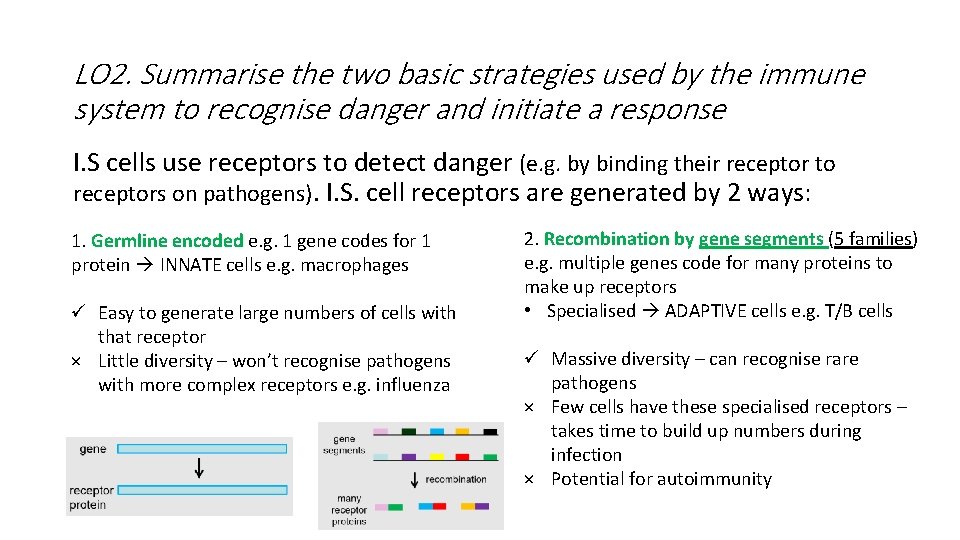
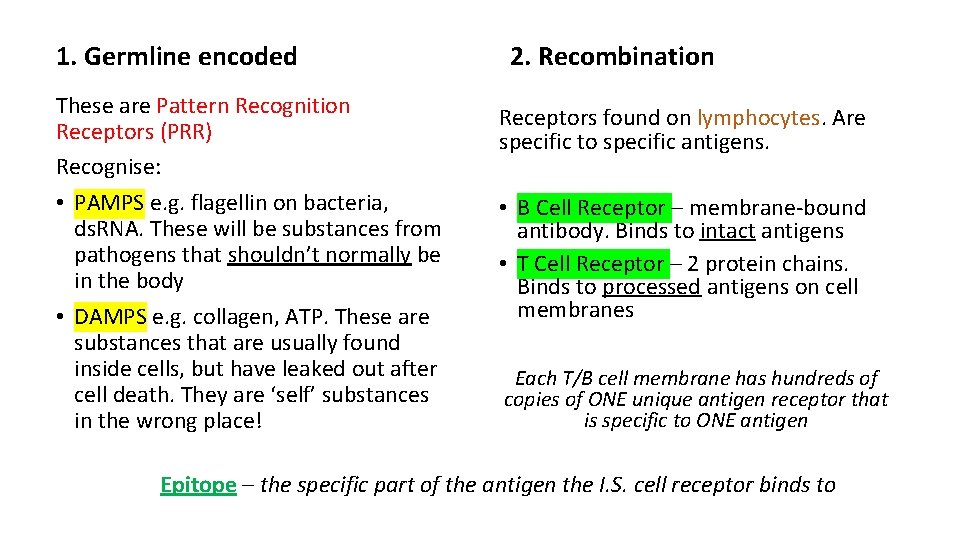
LO 2. Summarise the two basic strategies used by the immune system to recognise danger and initiate a response I. S cells use receptors to detect danger (e. g. by binding their receptor to receptors on pathogens). I. S. cell receptors are generated by 2 ways: 1. Germline encoded e. g. 1 gene codes for 1 protein INNATE cells e. g. macrophages ü Easy to generate large numbers of cells with that receptor × Little diversity – won’t recognise pathogens with more complex receptors e. g. influenza 2. Recombination by gene segments (5 families) e. g. multiple genes code for many proteins to make up receptors • Specialised ADAPTIVE cells e. g. T/B cells ü Massive diversity – can recognise rare pathogens × Few cells have these specialised receptors – takes time to build up numbers during infection × Potential for autoimmunity
1. Germline encoded These are Pattern Recognition Receptors (PRR) Recognise: • PAMPS e. g. flagellin on bacteria, ds. RNA. These will be substances from pathogens that shouldn’t normally be in the body • DAMPS e. g. collagen, ATP. These are substances that are usually found inside cells, but have leaked out after cell death. They are ‘self’ substances in the wrong place! 2. Recombination Receptors found on lymphocytes. Are specific to specific antigens. • B Cell Receptor – membrane-bound antibody. Binds to intact antigens • T Cell Receptor – 2 protein chains. Binds to processed antigens on cell membranes Each T/B cell membrane has hundreds of copies of ONE unique antigen receptor that is specific to ONE antigen Epitope – the specific part of the antigen the I. S. cell receptor binds to
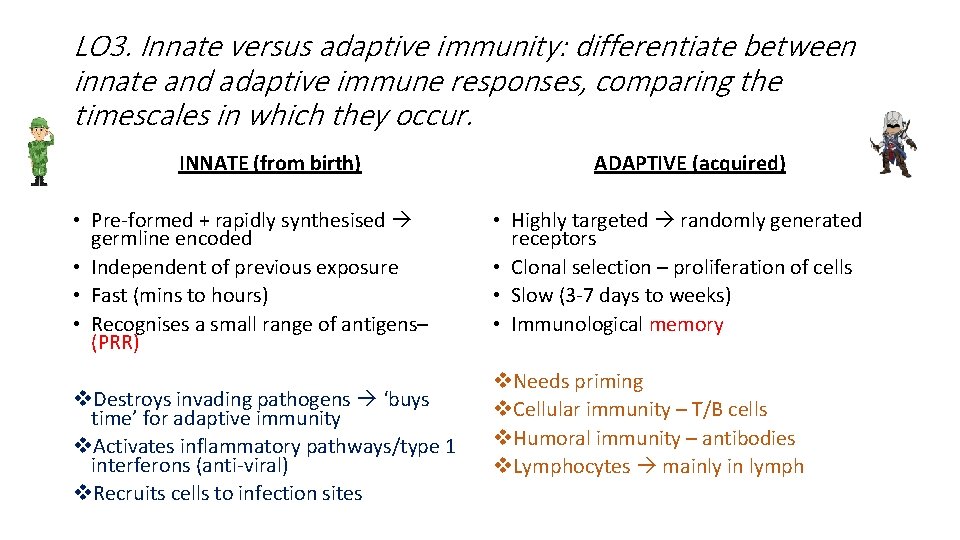
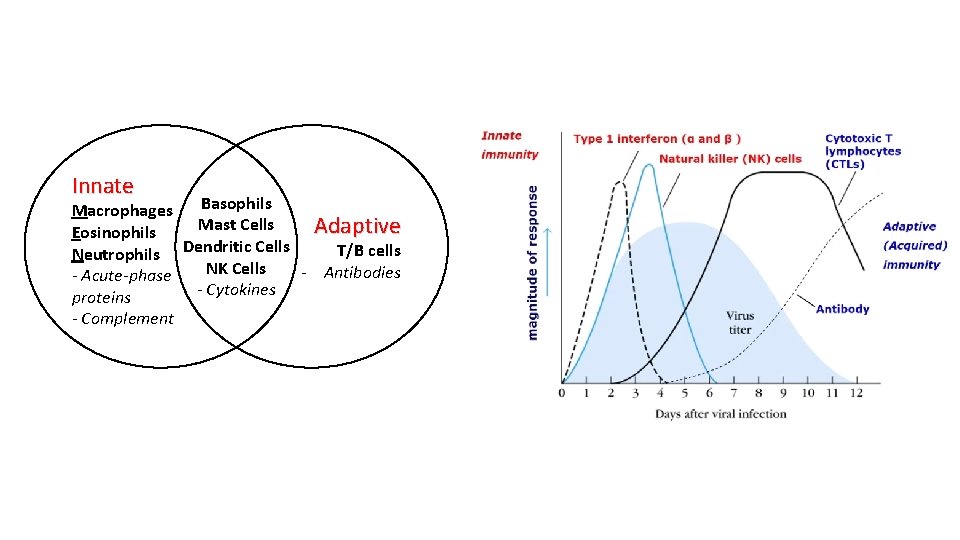
LO 3. Innate versus adaptive immunity: differentiate between innate and adaptive immune responses, comparing the timescales in which they occur. INNATE (from birth) • Pre-formed + rapidly synthesised germline encoded • Independent of previous exposure • Fast (mins to hours) • Recognises a small range of antigens– (PRR) v. Destroys invading pathogens ‘buys time’ for adaptive immunity v. Activates inflammatory pathways/type 1 interferons (anti-viral) v. Recruits cells to infection sites ADAPTIVE (acquired) • Highly targeted randomly generated receptors • Clonal selection – proliferation of cells • Slow (3 -7 days to weeks) • Immunological memory v. Needs priming v. Cellular immunity – T/B cells v. Humoral immunity – antibodies v. Lymphocytes mainly in lymph
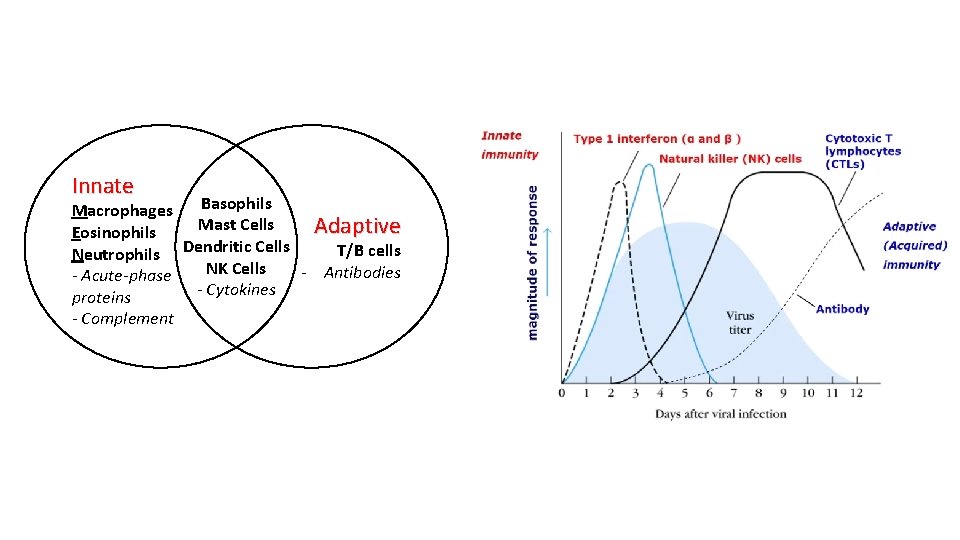
Innate Basophils Macrophages Mast Cells Adaptive Eosinophils T/B cells Neutrophils Dendritic Cells NK Cells - Antibodies - Acute-phase - Cytokines proteins - Complement
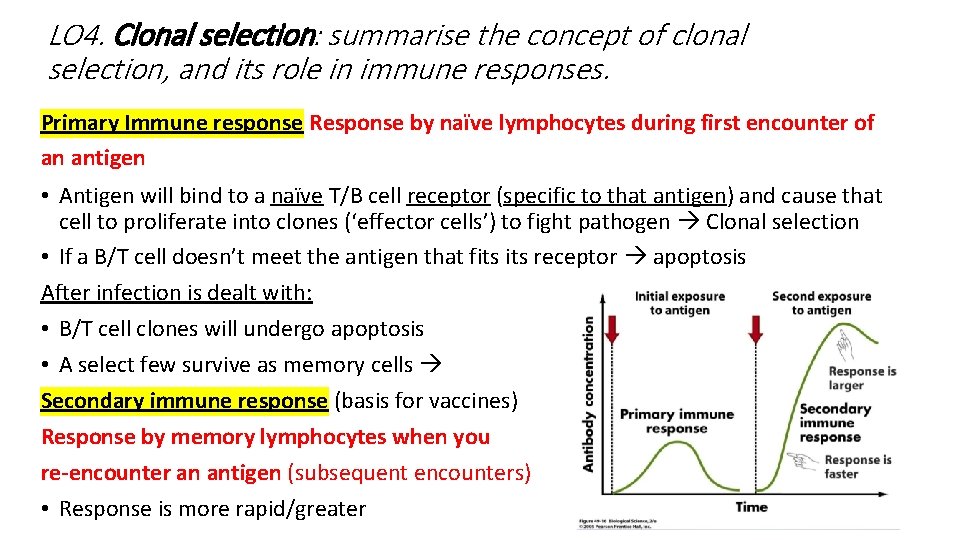
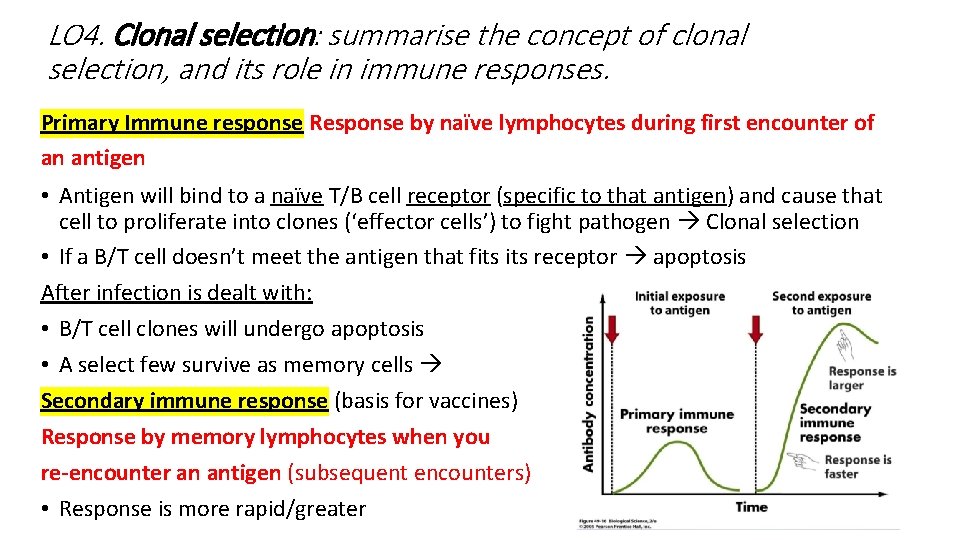
LO 4. Clonal selection: summarise the concept of clonal selection, and its role in immune responses. Primary Immune response Response by naïve lymphocytes during first encounter of an antigen • Antigen will bind to a naïve T/B cell receptor (specific to that antigen) and cause that cell to proliferate into clones (‘effector cells’) to fight pathogen Clonal selection • If a B/T cell doesn’t meet the antigen that fits receptor apoptosis After infection is dealt with: • B/T cell clones will undergo apoptosis • A select few survive as memory cells Secondary immune response (basis for vaccines) Response by memory lymphocytes when you re-encounter an antigen (subsequent encounters) • Response is more rapid/greater
Lecture 4 1. Immunoglobulin molecular structure: explain with the aid of a simple diagram the outline structure and function of the immunoglobulin molecule, identifying the antigen-binding site (Fab) and Fc portions of the molecule. 2. Antigen binding: explain how antibodies bind to antigen, and the consequences of such antigen binding.
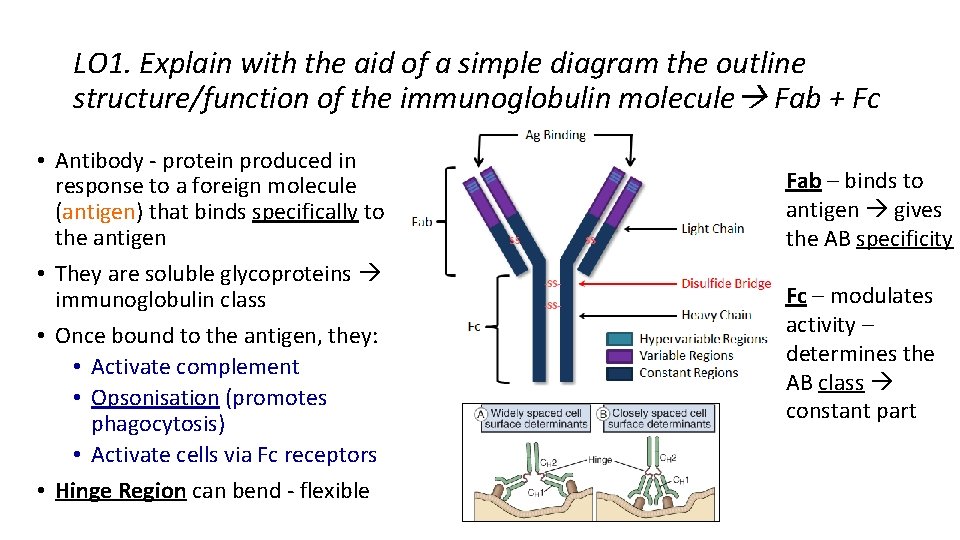
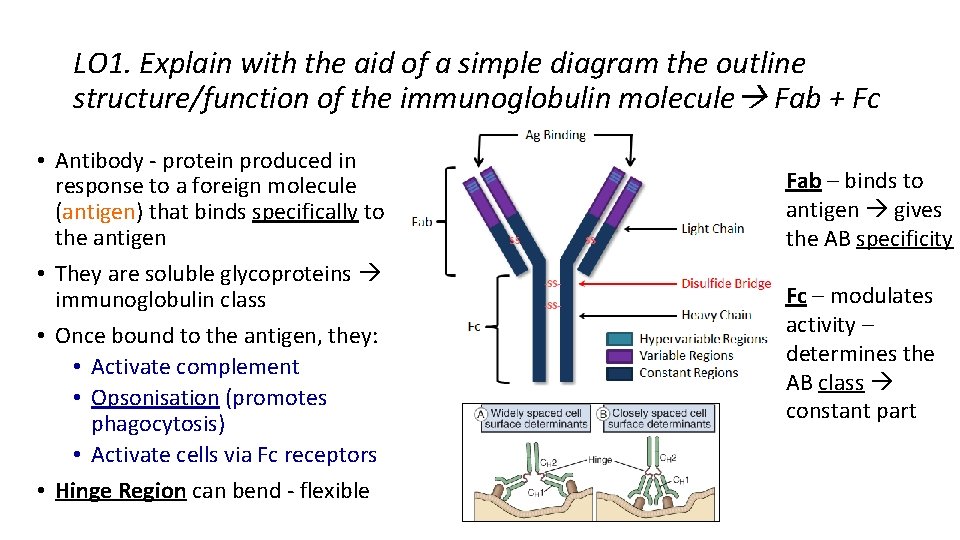
LO 1. Explain with the aid of a simple diagram the outline structure/function of the immunoglobulin molecule Fab + Fc • Antibody - protein produced in response to a foreign molecule (antigen) that binds specifically to the antigen • They are soluble glycoproteins immunoglobulin class • Once bound to the antigen, they: • Activate complement • Opsonisation (promotes phagocytosis) • Activate cells via Fc receptors • Hinge Region can bend - flexible Fab – binds to antigen gives the AB specificity Fc – modulates activity – determines the AB class constant part
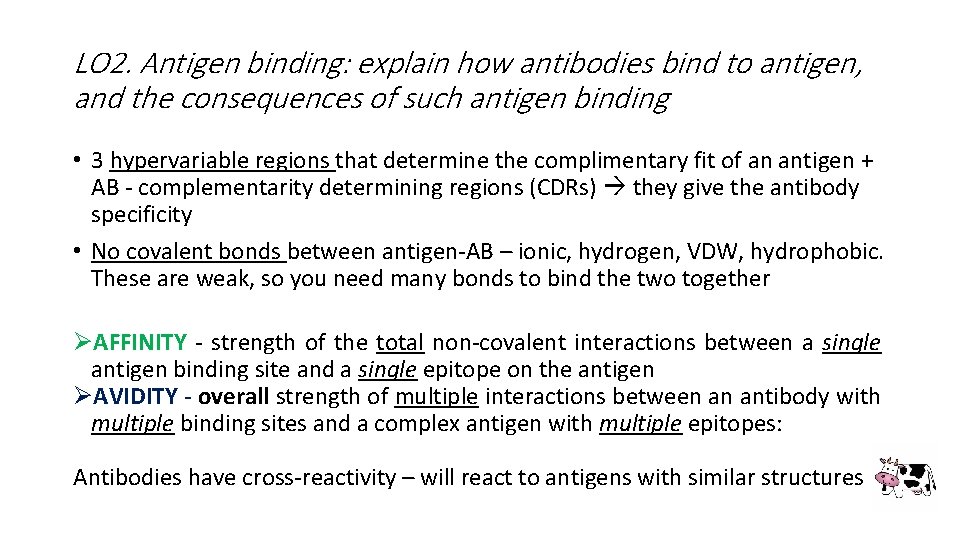
LO 2. Antigen binding: explain how antibodies bind to antigen, and the consequences of such antigen binding • 3 hypervariable regions that determine the complimentary fit of an antigen + AB - complementarity determining regions (CDRs) they give the antibody specificity • No covalent bonds between antigen-AB – ionic, hydrogen, VDW, hydrophobic. These are weak, so you need many bonds to bind the two together ØAFFINITY - strength of the total non-covalent interactions between a single antigen binding site and a single epitope on the antigen ØAVIDITY - overall strength of multiple interactions between an antibody with multiple binding sites and a complex antigen with multiple epitopes: Antibodies have cross-reactivity – will react to antigens with similar structures
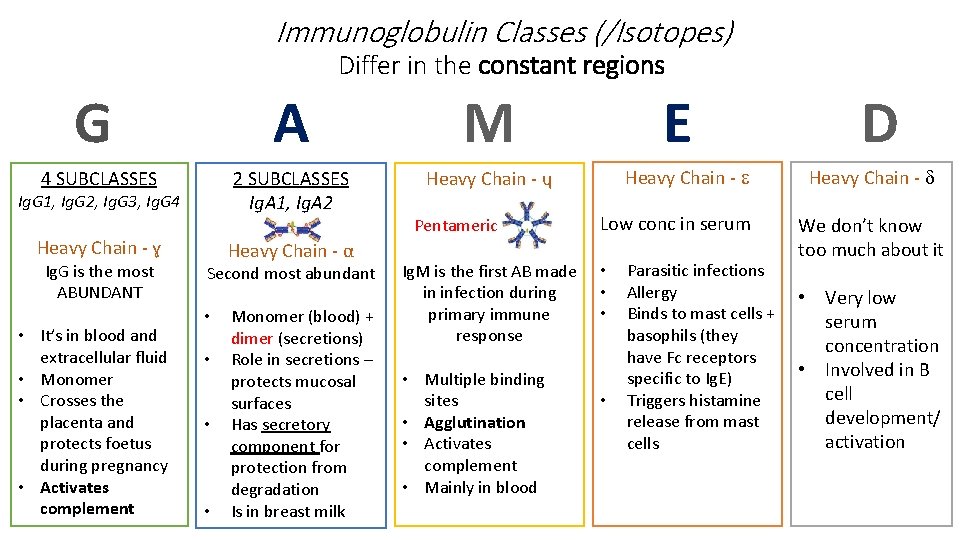
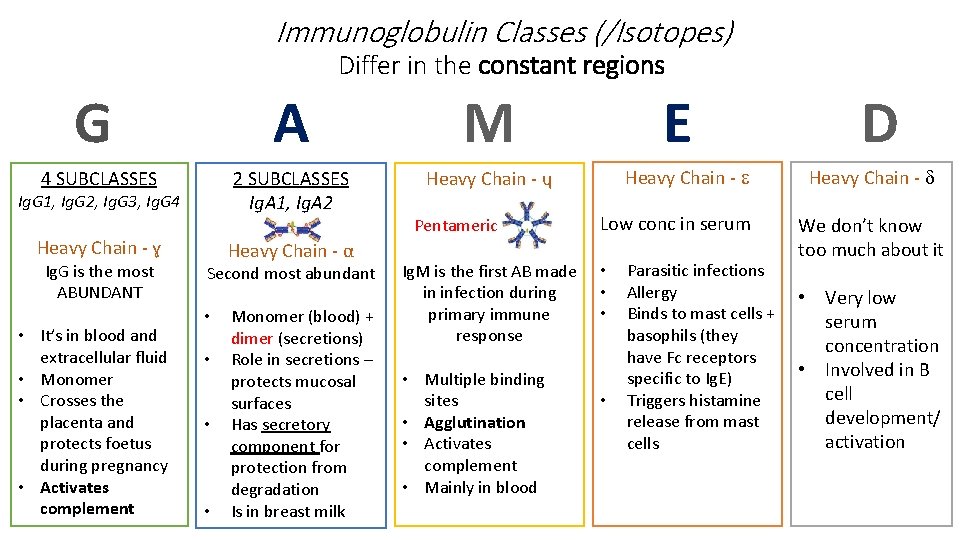
Immunoglobulin Classes (/Isotopes) Differ in the constant regions G A M 4 SUBCLASSES 2 SUBCLASSES Ig. A 1, Ig. A 2 Heavy Chain - ɥ Ig. G 1, Ig. G 2, Ig. G 3, Ig. G 4 Heavy Chain - ɣ Ig. G is the most ABUNDANT • It’s in blood and extracellular fluid • Monomer • Crosses the placenta and protects foetus during pregnancy • Activates complement Heavy Chain - α Second most abundant • • Monomer (blood) + dimer (secretions) Role in secretions – protects mucosal surfaces Has secretory component for protection from degradation Is in breast milk Pentameric Ig. M is the first AB made in infection during primary immune response • Multiple binding sites • Agglutination • Activates complement • Mainly in blood E Heavy Chain - Low conc in serum • • Parasitic infections Allergy Binds to mast cells + basophils (they have Fc receptors specific to Ig. E) Triggers histamine release from mast cells D Heavy Chain - We don’t know too much about it • Very low serum concentration • Involved in B cell development/ activation
Role of the AB DEFENCE • Neutralisation – AB binding to the pathogen/toxin and neutralising it • Agglutination – clumping together (Ig. M) • Opsonisation – coating pathogen with AB to aid phagocytes (Fc receptors) • Complement activation (via classical pathway) – Ig. G and Ig. M • Give new-borns passive immunity (rely on AB gained from mother) MEDICINE • Levels can help diagnose diseases • Passive immunity • Monoclonal antibodies for cancer therapy
Lecture 5 1. B lymphocyte origin: explain the origin and maturation of B lymphocytes, including the principle of immunoglobulin gene rearrangement. 2. B lymphocyte activation: explain the process of activation of B lymphocytes to divide and differentiate into antibody-secreting and memory cells, and the differences in antibody production in primary and secondary immune responses.
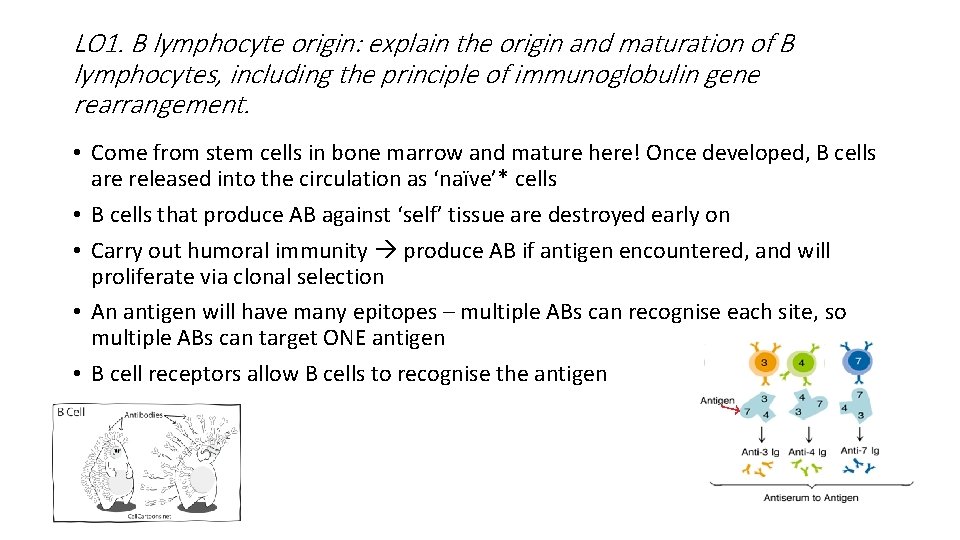
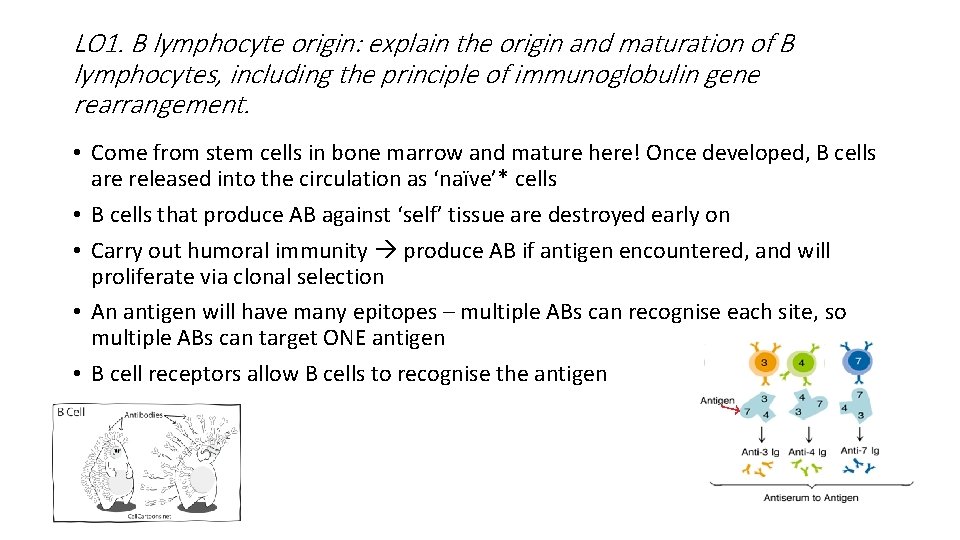
LO 1. B lymphocyte origin: explain the origin and maturation of B lymphocytes, including the principle of immunoglobulin gene rearrangement. • Come from stem cells in bone marrow and mature here! Once developed, B cells are released into the circulation as ‘naïve’* cells • B cells that produce AB against ‘self’ tissue are destroyed early on • Carry out humoral immunity produce AB if antigen encountered, and will proliferate via clonal selection • An antigen will have many epitopes – multiple ABs can recognise each site, so multiple ABs can target ONE antigen • B cell receptors allow B cells to recognise the antigen
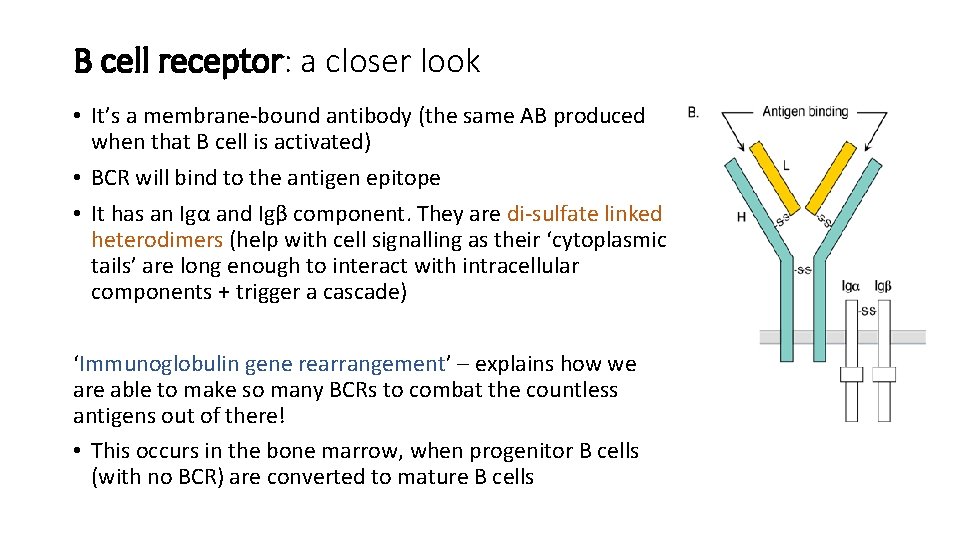
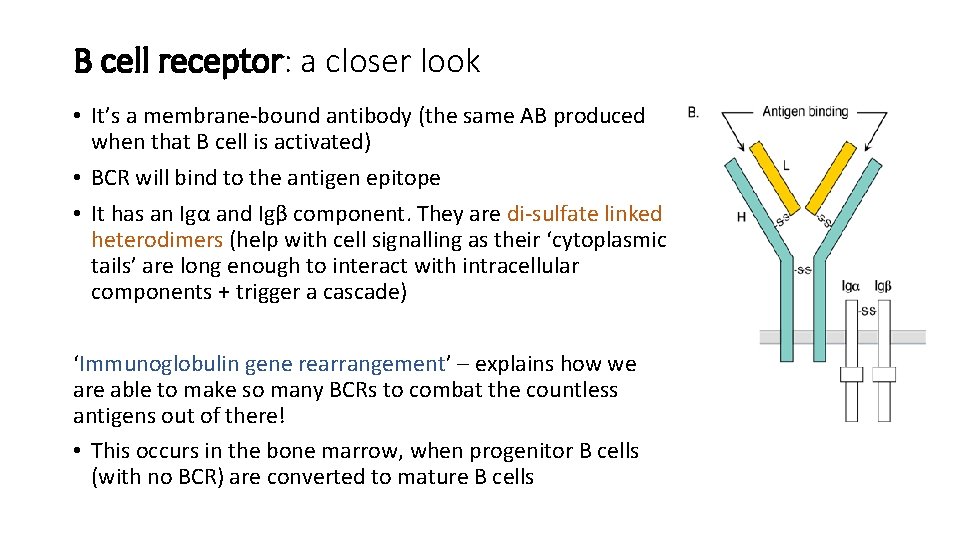
B cell receptor: a closer look • It’s a membrane-bound antibody (the same AB produced when that B cell is activated) • BCR will bind to the antigen epitope • It has an Igα and Igβ component. They are di-sulfate linked heterodimers (help with cell signalling as their ‘cytoplasmic tails’ are long enough to interact with intracellular components + trigger a cascade) ‘Immunoglobulin gene rearrangement’ – explains how we are able to make so many BCRs to combat the countless antigens out of there! • This occurs in the bone marrow, when progenitor B cells (with no BCR) are converted to mature B cells
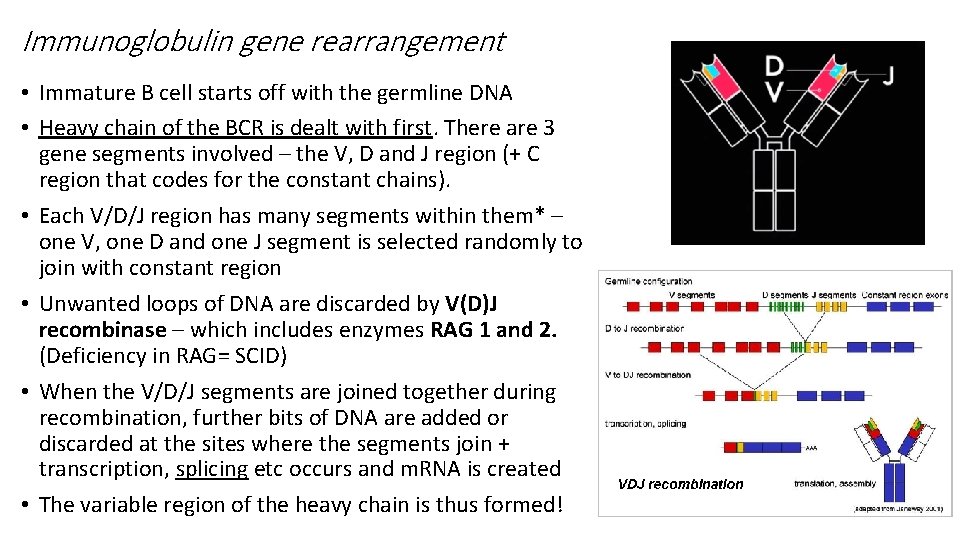
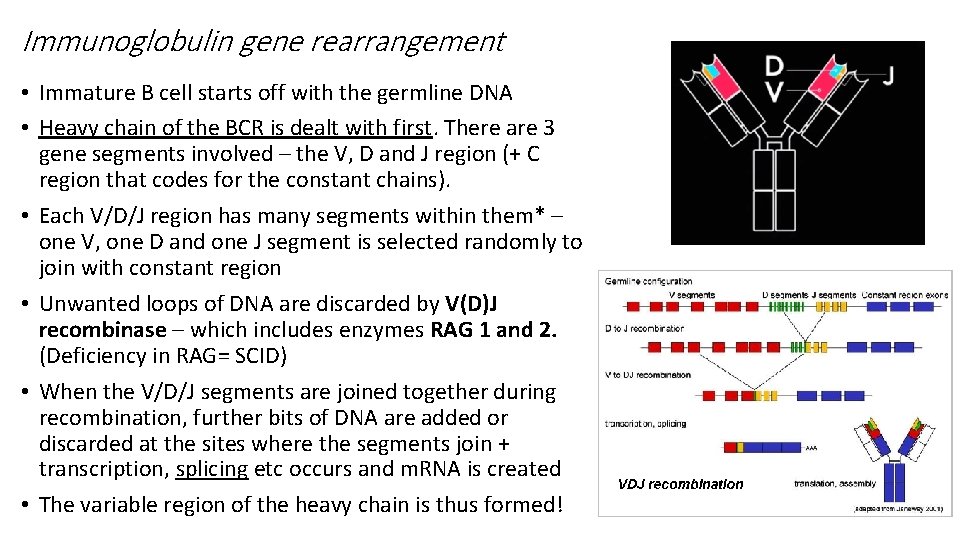
Immunoglobulin gene rearrangement • Immature B cell starts off with the germline DNA • Heavy chain of the BCR is dealt with first. There are 3 gene segments involved – the V, D and J region (+ C region that codes for the constant chains). • Each V/D/J region has many segments within them* – one V, one D and one J segment is selected randomly to join with constant region • Unwanted loops of DNA are discarded by V(D)J recombinase – which includes enzymes RAG 1 and 2. (Deficiency in RAG= SCID) • When the V/D/J segments are joined together during recombination, further bits of DNA are added or discarded at the sites where the segments join + transcription, splicing etc occurs and m. RNA is created • The variable region of the heavy chain is thus formed!
Light chain coding works in the similar way with key differences: - There is no D segment, only V and J - The light chain can be kappa or lambda – giving more variety § Three chromosomes are involved in coding for Ig chains. One for kappa chains, one for lambda chains and one for all the heavy chains § Once an immature B cell has its BCR, if this is capable of attacking body cells, it is removed § The mature B cell is then released to the circulation and goes into lymph nodes etc q (NOTE) Sometimes Ig. D is co-expressed with Ig. M on a B cell – not much is known about Ig. D, but we know this process happens due to alternative RNA splicing
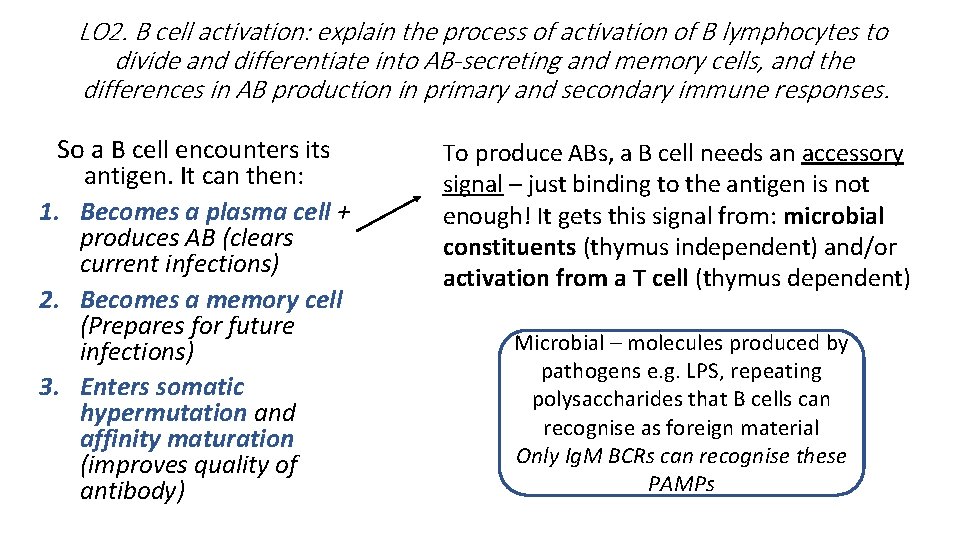
LO 2. B cell activation: explain the process of activation of B lymphocytes to divide and differentiate into AB-secreting and memory cells, and the differences in AB production in primary and secondary immune responses. So a B cell encounters its antigen. It can then: 1. Becomes a plasma cell + produces AB (clears current infections) 2. Becomes a memory cell (Prepares for future infections) 3. Enters somatic hypermutation and affinity maturation (improves quality of antibody) To produce ABs, a B cell needs an accessory signal – just binding to the antigen is not enough! It gets this signal from: microbial constituents (thymus independent) and/or activation from a T cell (thymus dependent) Microbial – molecules produced by pathogens e. g. LPS, repeating polysaccharides that B cells can recognise as foreign material Only Ig. M BCRs can recognise these PAMPs
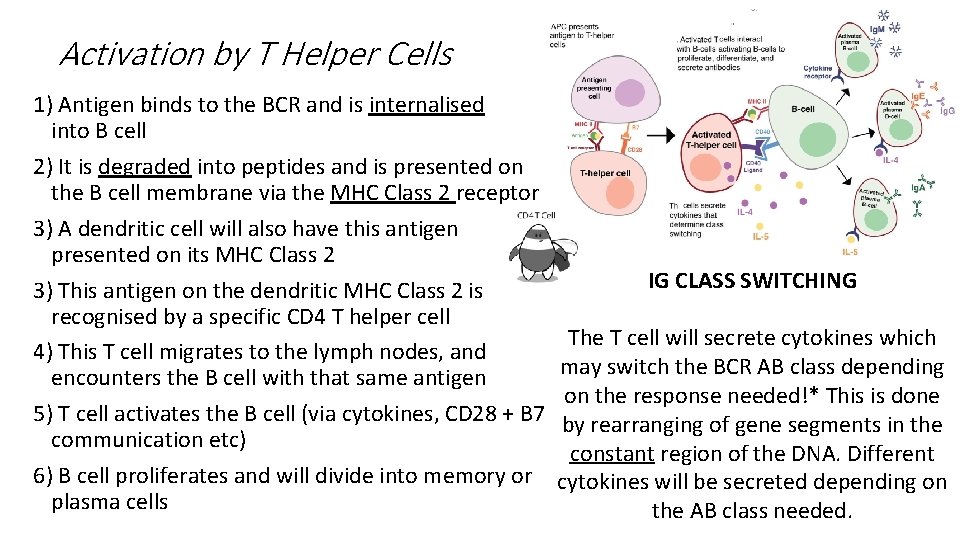
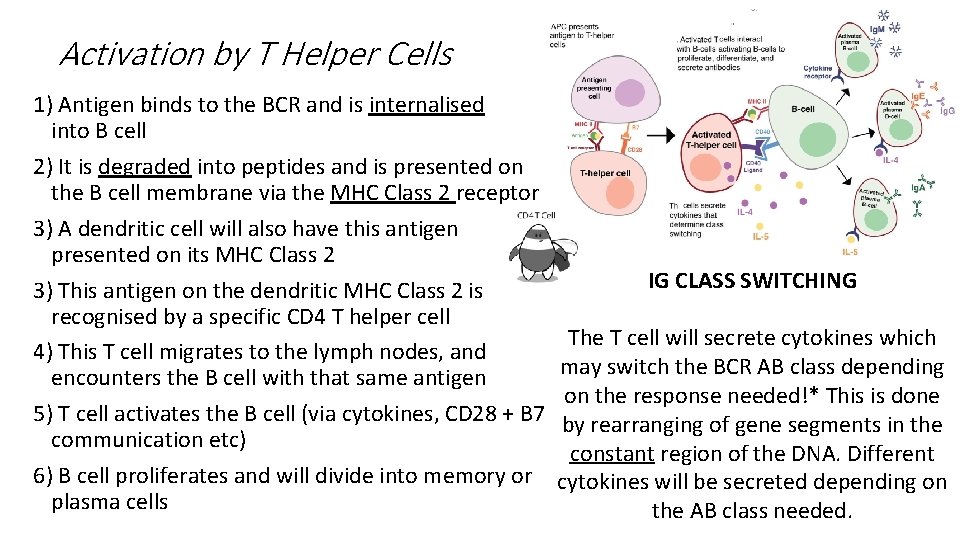
Activation by T Helper Cells 1) Antigen binds to the BCR and is internalised into B cell 2) It is degraded into peptides and is presented on the B cell membrane via the MHC Class 2 receptor 3) A dendritic cell will also have this antigen presented on its MHC Class 2 3) This antigen on the dendritic MHC Class 2 is recognised by a specific CD 4 T helper cell 4) This T cell migrates to the lymph nodes, and encounters the B cell with that same antigen 5) T cell activates the B cell (via cytokines, CD 28 + B 7 communication etc) 6) B cell proliferates and will divide into memory or plasma cells IG CLASS SWITCHING The T cell will secrete cytokines which may switch the BCR AB class depending on the response needed!* This is done by rearranging of gene segments in the constant region of the DNA. Different cytokines will be secreted depending on the AB class needed.
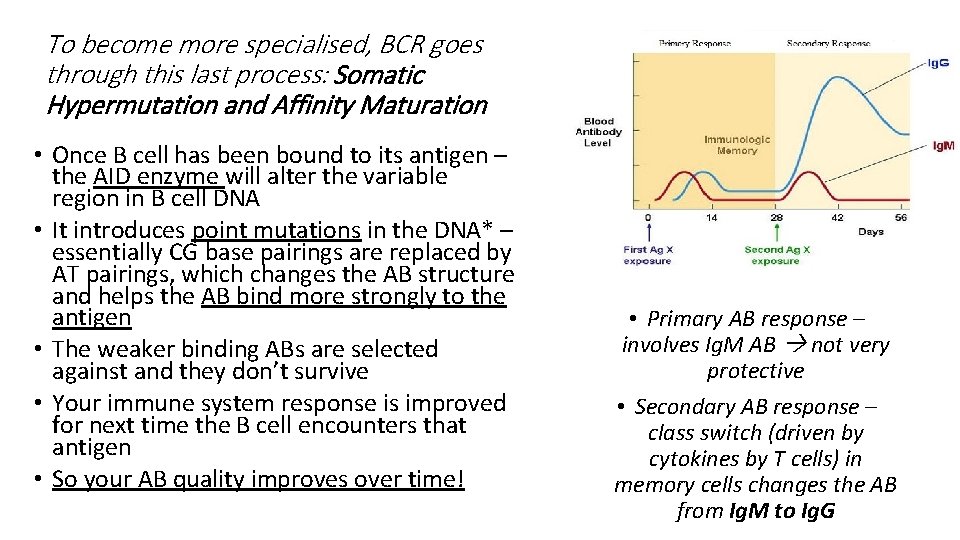
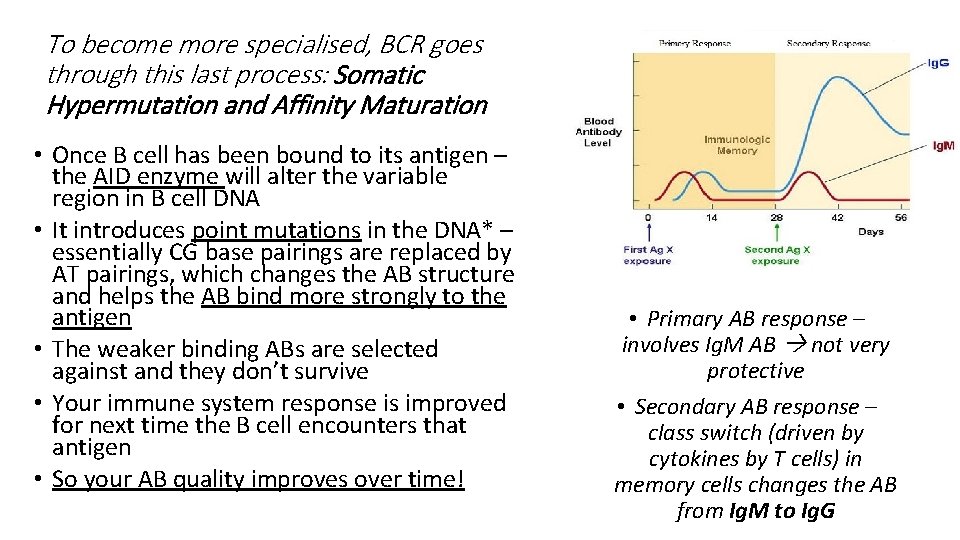
To become more specialised, BCR goes through this last process: Somatic Hypermutation and Affinity Maturation • Once B cell has been bound to its antigen – the AID enzyme will alter the variable region in B cell DNA • It introduces point mutations in the DNA* – essentially CG base pairings are replaced by AT pairings, which changes the AB structure and helps the AB bind more strongly to the antigen • The weaker binding ABs are selected against and they don’t survive • Your immune system response is improved for next time the B cell encounters that antigen • So your AB quality improves over time! • Primary AB response – involves Ig. M AB not very protective • Secondary AB response – class switch (driven by cytokines by T cells) in memory cells changes the AB from Ig. M to Ig. G
Lecture 9 ‘Aims’ List the main components of the immune system. Summarise the sequence and timing of events during infection. Summarise and give examples of the roles taken by: (i) physical, chemical and mechanical barriers (ii) antigen presenting cells (iii) immune regulatory mechanisms. Define, explain and compare: (i) innate versus adaptive/acquired immunity (ii) humoral versus cellular immunity (iii) defences against viruses and bacteria (iv) defence at mucosa versus the skin
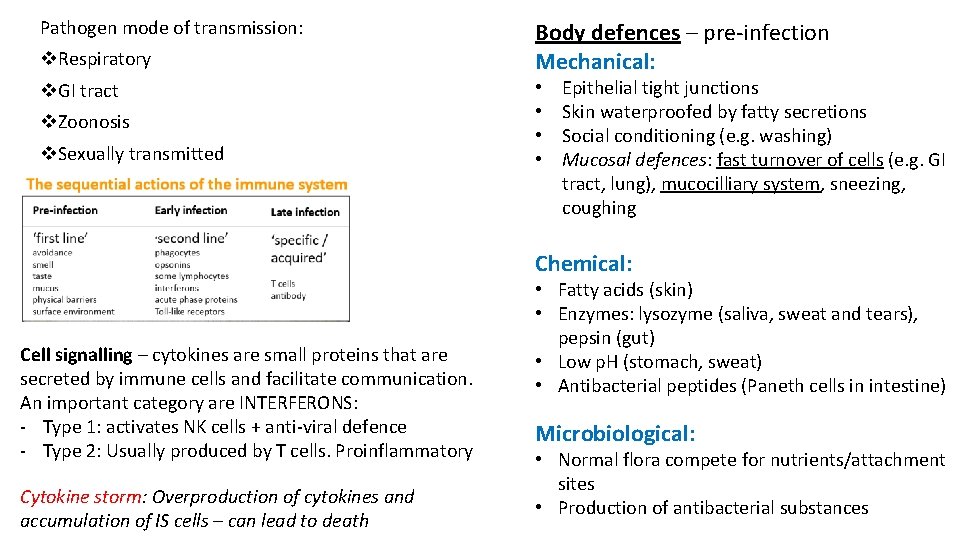
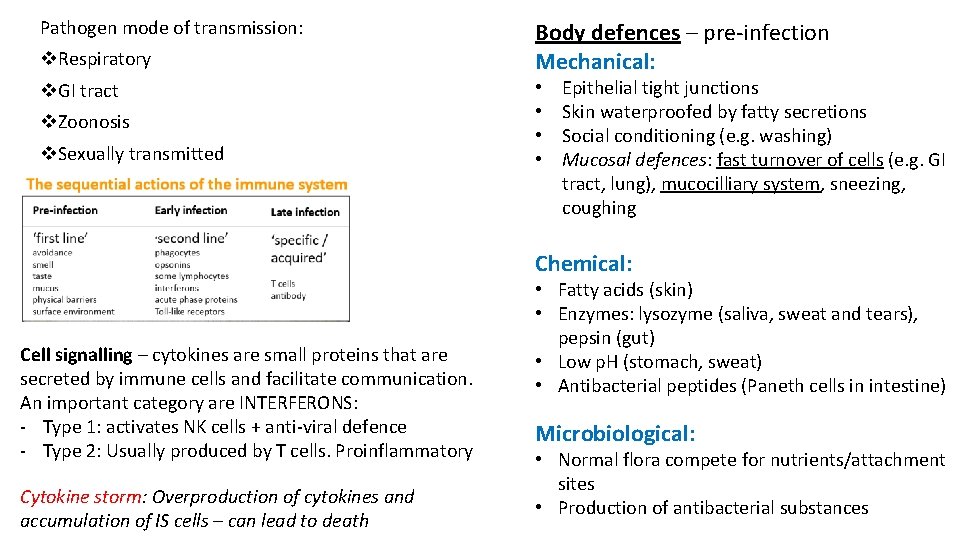
Pathogen mode of transmission: v. Respiratory v. GI tract v. Zoonosis v. Sexually transmitted Body defences – pre-infection Mechanical: • • Epithelial tight junctions Skin waterproofed by fatty secretions Social conditioning (e. g. washing) Mucosal defences: fast turnover of cells (e. g. GI tract, lung), mucocilliary system, sneezing, coughing Chemical: Cell signalling – cytokines are small proteins that are secreted by immune cells and facilitate communication. An important category are INTERFERONS: - Type 1: activates NK cells + anti-viral defence - Type 2: Usually produced by T cells. Proinflammatory Cytokine storm: Overproduction of cytokines and accumulation of IS cells – can lead to death • Fatty acids (skin) • Enzymes: lysozyme (saliva, sweat and tears), pepsin (gut) • Low p. H (stomach, sweat) • Antibacterial peptides (Paneth cells in intestine) Microbiological: • Normal flora compete for nutrients/attachment sites • Production of antibacterial substances
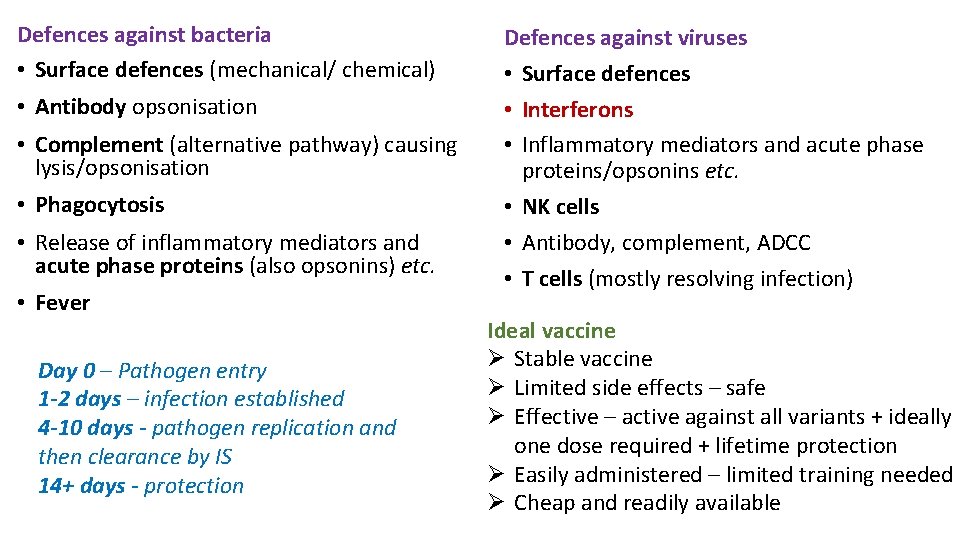
Defences against bacteria • Surface defences (mechanical/ chemical) • Antibody opsonisation • Complement (alternative pathway) causing lysis/opsonisation • Phagocytosis • Release of inflammatory mediators and acute phase proteins (also opsonins) etc. • Fever Day 0 – Pathogen entry 1 -2 days – infection established 4 -10 days - pathogen replication and then clearance by IS 14+ days - protection Defences against viruses • Surface defences • Interferons • Inflammatory mediators and acute phase proteins/opsonins etc. • NK cells • Antibody, complement, ADCC • T cells (mostly resolving infection) Ideal vaccine Ø Stable vaccine Ø Limited side effects – safe Ø Effective – active against all variants + ideally one dose required + lifetime protection Ø Easily administered – limited training needed Ø Cheap and readily available
Practice Questions* answers in the notes 1. What are the differences in the pathogen specificity between the innate and acquired (adaptive) immune response? [4 marks] 2012 2. Name the innate cell and humoral response to i) bacterial infection or ii) viral infection (4 marks) 2012 3. Name 3 leukocytes present in NORMAL blood 2013 4. 4 characteristics of an ideal vaccine (2 marks) 2018 5. What region of the antibody determines class? (1 mark) 2018 6. Sketch a simple diagram of an Ig molecule and label the antigen binding site and the Fc part. (4 marks) 2017 7. Which 2 Immunoglobulins are multimeric? State what they are and what they are responsible for? (2 marks) 2017 8. 2 differences between the primary immune response and the secondary immune response (2 marks) 2017
Thank you! Please leave feedback: bit. ly/muslimmedics Feel free to email me if you have any questions (Immunology related or otherwise): aa 16017@ic. ac. uk i. Cal - bit. ly/MMi. Cal https: //www. union. ic. ac. uk/medic/muslim/education/year-1/