IMMUNOLOGICAL TOLERANCE AND AUTOIMMUNITY Tolerance is specific immunologic

- Slides: 29
IMMUNOLOGICAL TOLERANCE AND AUTOIMMUNITY
• Tolerance – is specific immunologic unresponsiveness. • Unresponsiveness to self antigens is called auto-tolerance. • This is the natural tolerance that is essential for our survival. • Loss of self tolerance results in autoimmune diseases.
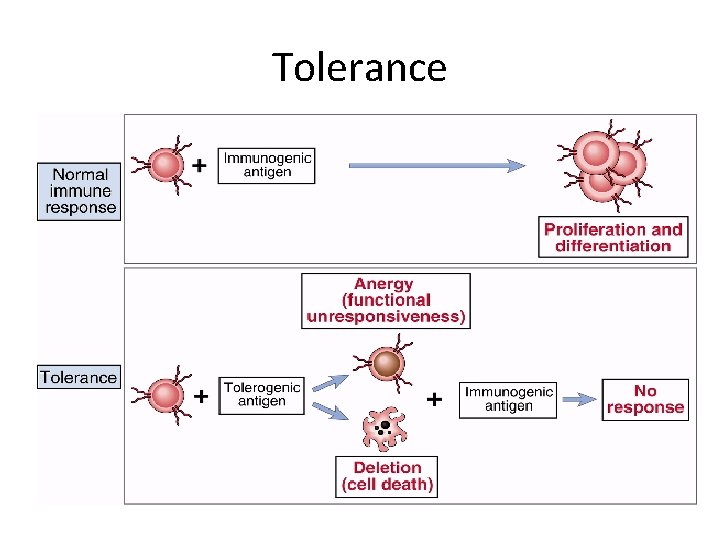
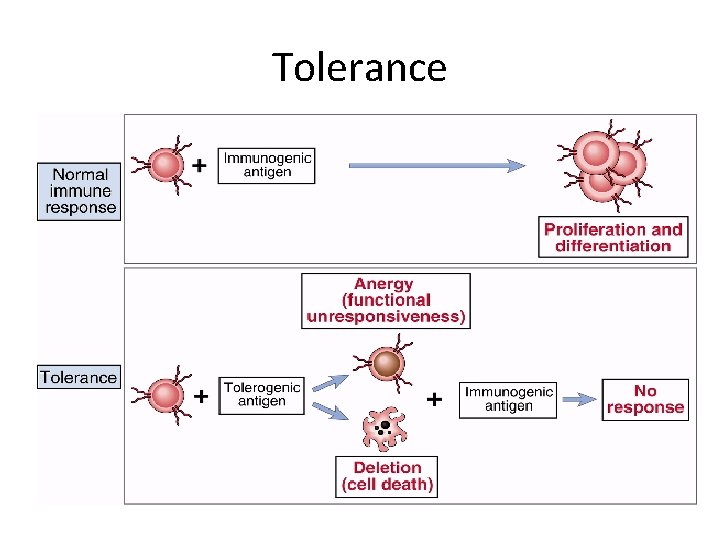
Tolerance
Mechanism of tolerance • Self tolerance is acquired prenatally. • Antigens present in an organism during the development of the immune system are accepted as self. • Antigens encountered later in life, after the development of the immune system are recognised as non-self or foreign and induce an immune response.
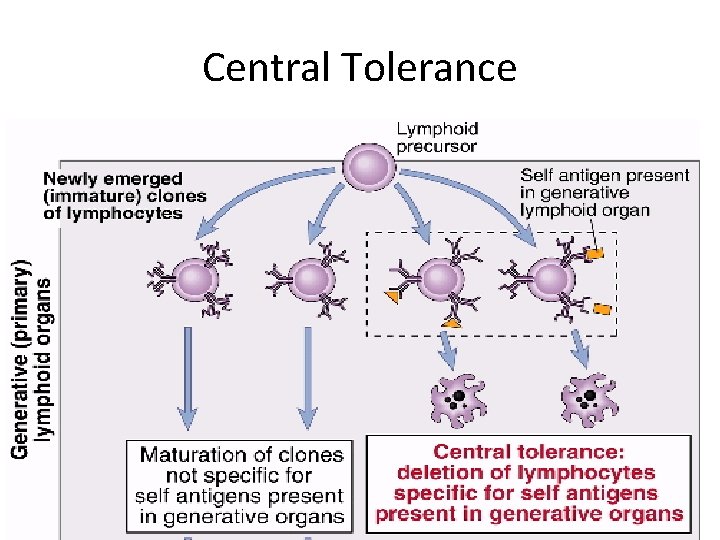
• Central Tolerance (Clonal deletion) – Deletion or killing of self reactive cells occurs by apoptosis (programmed cell death) during the embryonic life. This is also called ‘negative selection’. – Clonal deletion of self reactive T lymphocytes occurs in the thymus and clonal deletion of self reactive B cells occurs in the bone marrow. – Likewise, differentiating early B cells become tolerant when they encounter cell-associated or soluble self antigen.
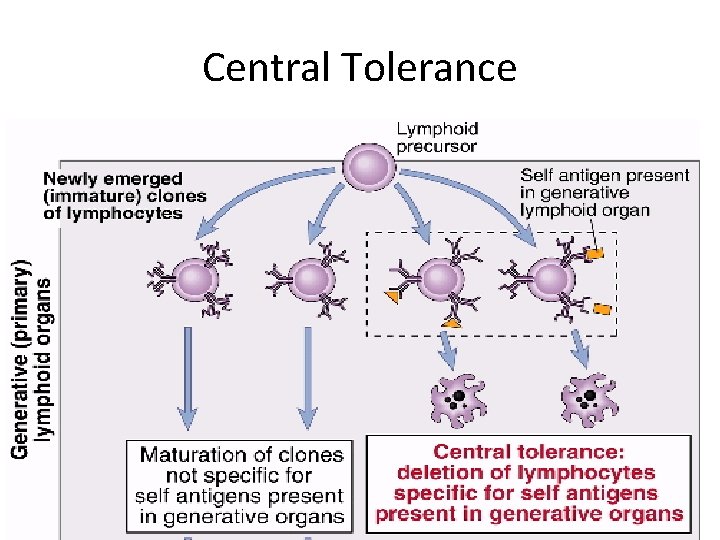
Central Tolerance
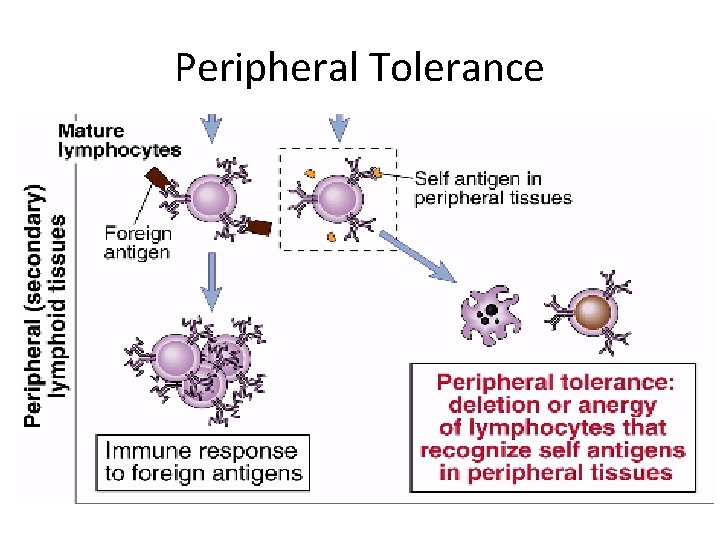
• Peripheral Tolerance (Clonal Anergy) – Mature immunocompetent cells recognise the antigen but do not respond to it. – Auto-reactive T cells, when exposed to antigenic peptides which do not possess costimulatory molecules (B 7 -1 or B 7 -2), become anergic to the antigen.
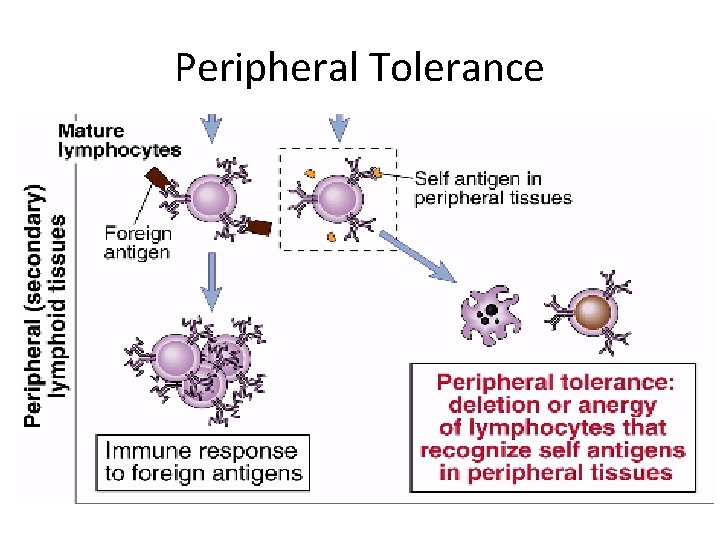
Peripheral Tolerance
Induction of tolerance • Antigen is administered in a specialized way (as a tolerogen) that will lead to induction of tolerance. • Induction of tolerance may be used as a therapeutic approach for preventing harmful immune responses. • Tolerance may be induced – • In the prevention of graft rejection. • In the treatment of autoimmune diseases. • In the treatment of allergic conditions.
Mechanism of Auto-immunity • Breakdown of self tolerance results in autoimmunity. When this occurs, auto-antibodies and self reactive T cells are produced, resulting in tissue damage. • Tolerance in B cells is less complete than in T cells, which explains why most autoimmune diseases are antibody mediated.
• Altered antigens (Neoantigens) • Tissue or cell antigens may undergo antigenic alteration as a result of combining with drugs or microbial components. • Such altered or neo-antigens are no longer recognized as self and may elicit an immune response.
Hidden (Sequestered antigens) • Certain self antigens are present within closed systems and are not accessible to the immune system. These are known as hidden or sequestered antigens. When these antigens are released into circulation, they may evoke an immune response. For example, • Lens protein enclosed within the lens capsule is a sequestered antigen. After cataract surgery or penetrating eye injury, lens protein may be released and the immune system may mount an immune response causing inflammation of the eye.
• Developing immune system will not encounter sperm antigen, as the sperms are produced later, during puberty. • Mumps virus may damage the testis and expose the sperm antigen resulting in inflammation of testis.
Cross Reacting Foreign Antigens • Streptococcal M Protein – Repeated streptococcal infections can damage the heart due to shared antigenic characteristics between Streptococcal M protein and the myosin of the heart muscle. • Nephritiogenic Strains of streptococci – Infection with Nephritiogenic strains of streptococci may lead to glomerulonephritis due to antigenic sharing with renal glomerulus.
Imbalance of Ts & Th cells • Loss of Ts cell control may explain the rising incidence of autoimmune diseases with advancing age. • Loss of Ts activity has been demonstrated in SLE. • Occasionally, increased Th cell activity may lead to the development of autoimmunity.
Factors responsible for autoimmune diseases • Genetic factors are believed to be important in determining the frequency and the nature of autoimmune diseases. • Autoimmune diseases often occur as familial diseases. • They appear to be associated with certain MHC genes. • Rheumatoid arthritis is associated with HLA DR 4, multiple sclerosis with HLA DR 2 and Ankylosing Spondylitis with HLA B 27.
• Hormonal factors • Hormones may play a role in the development of some of the autoimmune diseases. Approximately 90% of all autoimmune diseases occur in women. • Systemic lupus erythomatosus (SLE) is ten times more common in females than in males.
Autoimmune diseases • Autoimmune diseases are the diseases resulting from immune response against host’s own cells or tissues. Autoimmune diseases may be classified as – • Organ-specific – In these diseases the target is a single organ or tissue, such as thyroid causing thyroiditis. • Non-organ specific – In these diseases the target is spread over many different organs or tissues (E. g. Systemic lupus erythomatosus).
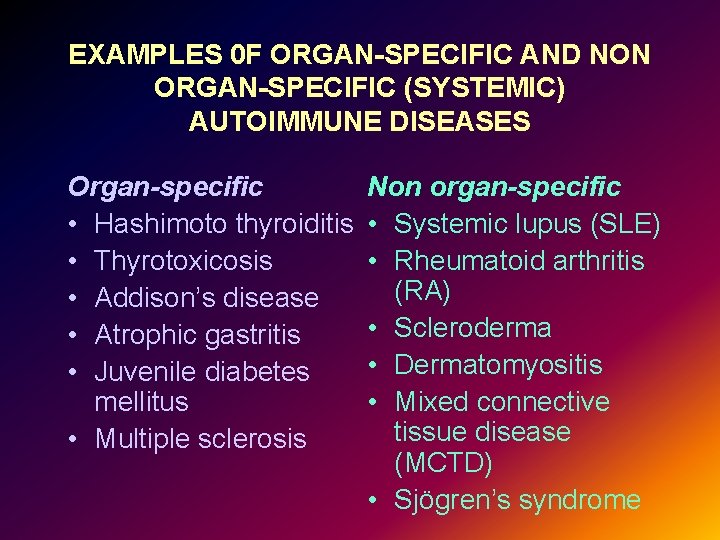
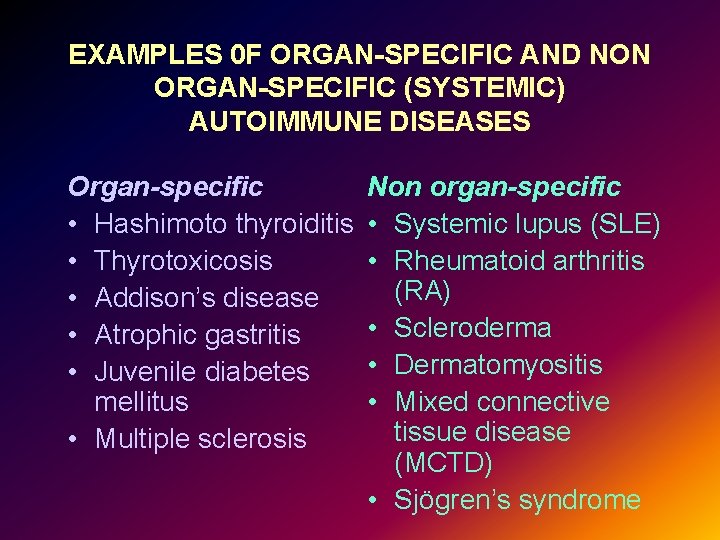
EXAMPLES 0 F ORGAN-SPECIFIC AND NON ORGAN-SPECIFIC (SYSTEMIC) AUTOIMMUNE DISEASES Organ-specific • Hashimoto thyroiditis • Thyrotoxicosis • Addison’s disease • Atrophic gastritis • Juvenile diabetes mellitus • Multiple sclerosis Non organ-specific • Systemic lupus (SLE) • Rheumatoid arthritis (RA) • Scleroderma • Dermatomyositis • Mixed connective tissue disease (MCTD) • Sjögren’s syndrome
• Hashimoto’s Thyroiditis – In this disease, antibodies are produced against Thyroglobulin, and these antibodies provoke an inflammatory process that leads to fibrosis of thyroid gland. • Multiple Sclerosis – In this disease, auto-reactive T lymphocytes and macrophages cause demyelination of the white matter of the brain. • Insulin dependent diabetes mellitus (IDDM) – In this disease, auto-reactive T lymphocytes destroy the beta cells of the islets of pancreas.

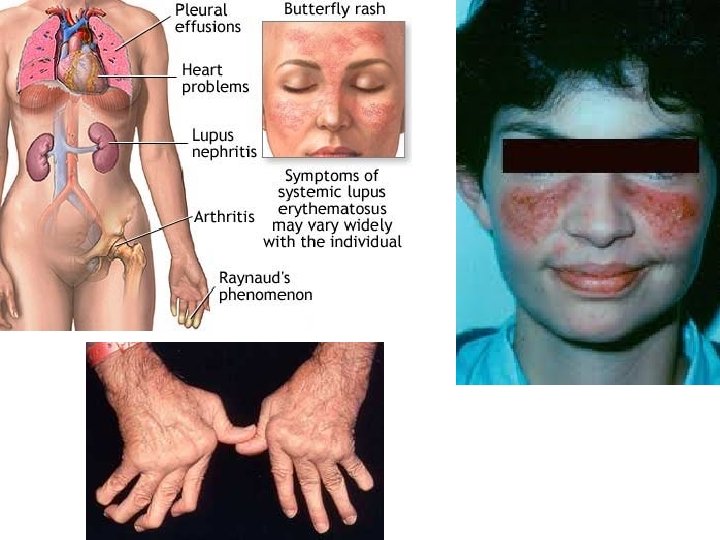
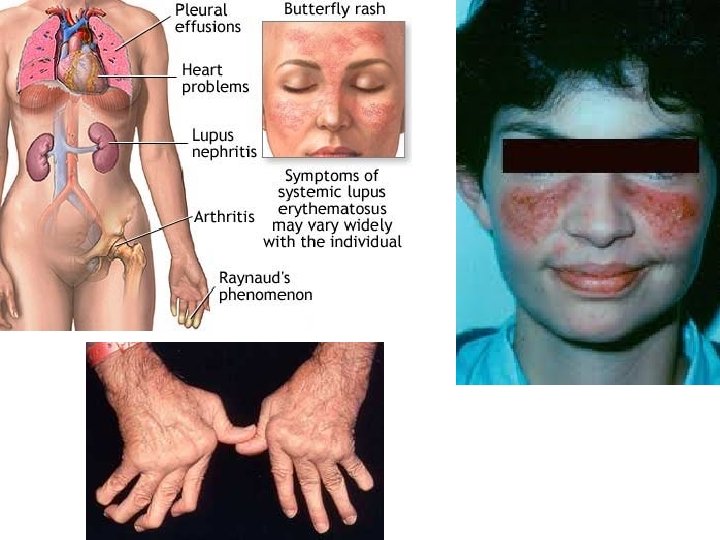
• Systemic Lupus Erythomatosus – It is a rare multi -system autoimmune disease that occurs in young women. • Tissue damage is caused by antinuclear antibodies (ANA), which can be detected in patient’s serum. • Skin, kidneys, joints and other serous membranes are most frequently affected. The disease is characterised by relapses and remissions.
• Rheumatoid arthritis – It is a chronic, systemic autoimmune disease in which joints are frequently affected. Rheumatoid factor, an antibody against the Fc fragment of human Ig. G can be demonstrated in patient’s serum and synovial fluid.
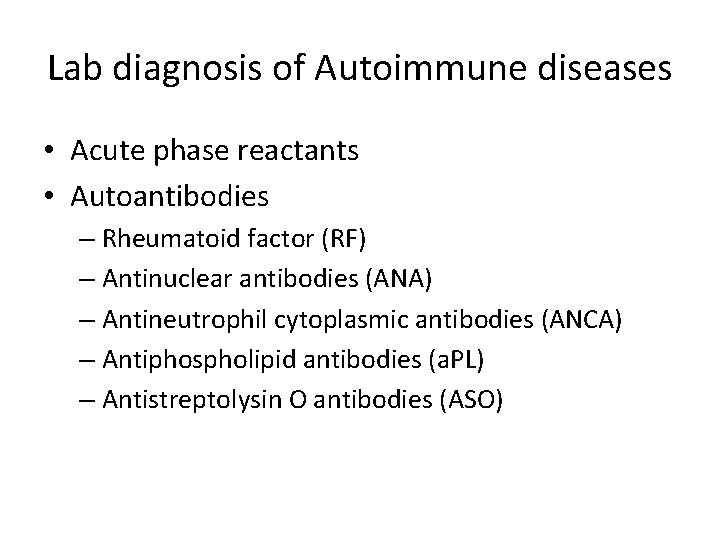
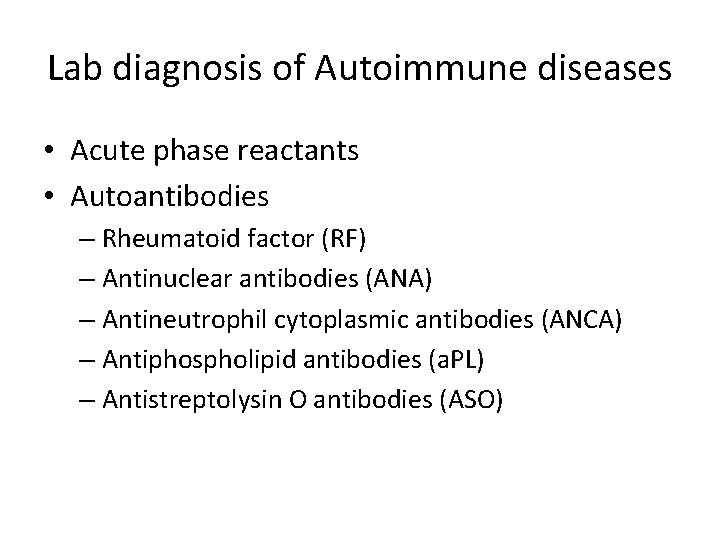
Lab diagnosis of Autoimmune diseases • Acute phase reactants • Autoantibodies – Rheumatoid factor (RF) – Antinuclear antibodies (ANA) – Antineutrophil cytoplasmic antibodies (ANCA) – Antiphospholipid antibodies (a. PL) – Antistreptolysin O antibodies (ASO)
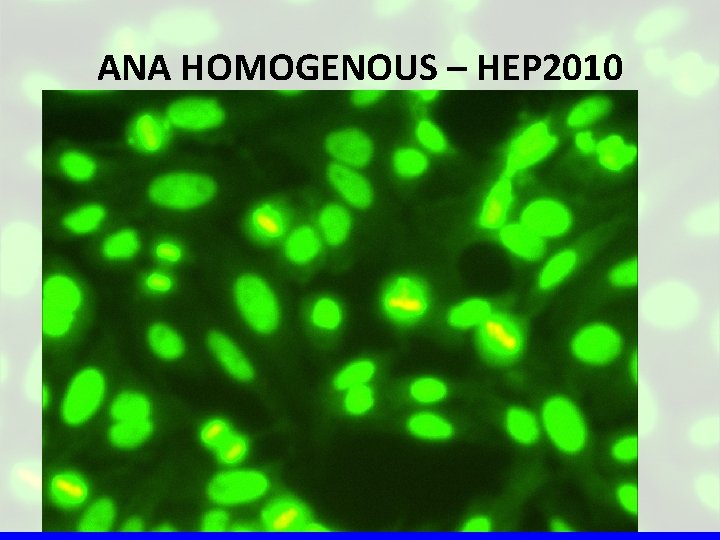
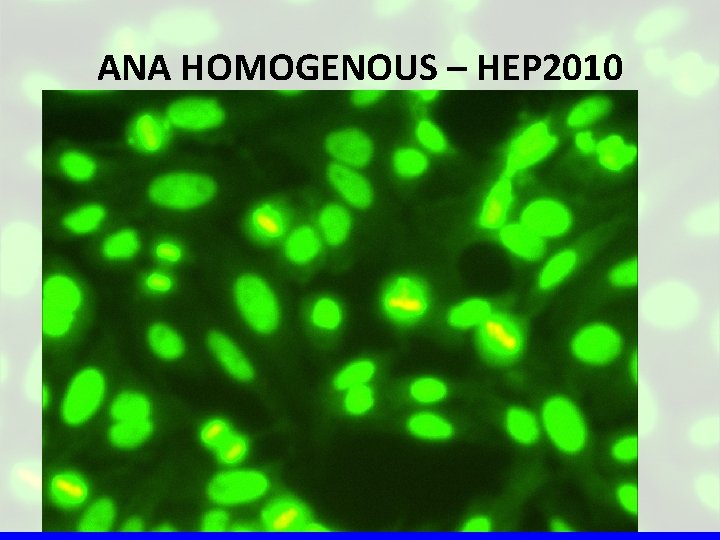
ANA HOMOGENOUS – HEP 2010
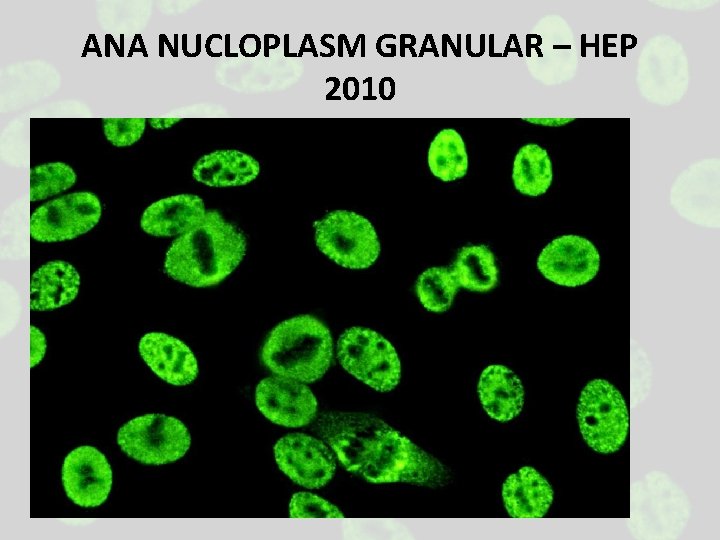
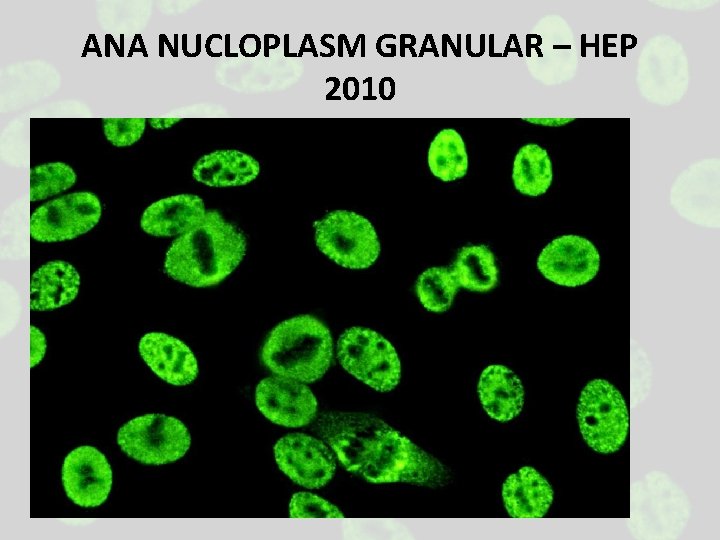
ANA NUCLOPLASM GRANULAR – HEP 2010
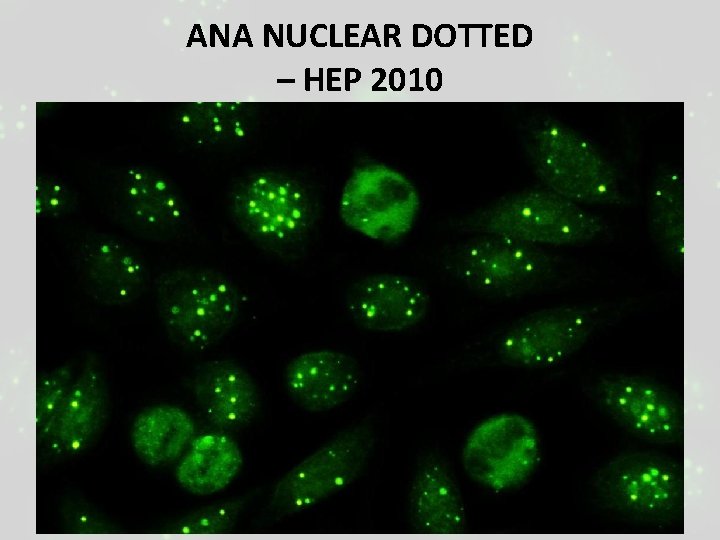
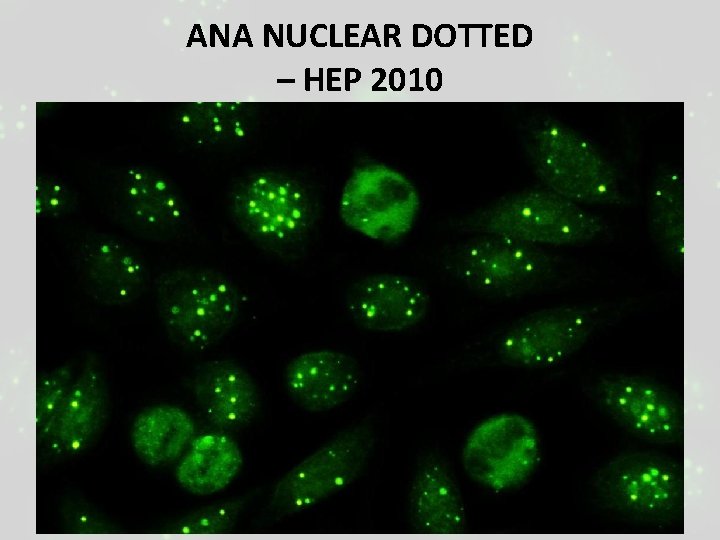
ANA NUCLEAR DOTTED – HEP 2010
Treatment of autoimmune diseases • Non-steroidal anti-inflammatory drugs – e. g. aspirin, indomethacin. • Steroidal anti-inflammatory drugs – corticosteroids. • Immunosuppressive cytotoxic drugs – azathioprine, cyclophosphamide. • Antibiotics – cyclosporine.
• Surgery – thymectomy for myasthenia gravis. • Plasmapheresis – to remove the offending immune complexes or antibodies. • Anti-TNF antibodies or soluble form of TNF receptor may neutralize TNF and are approved for the treatment of rheumatoid arthritis.