Immunodeficiencies and autoimmune diseases Martin Lika Immunodeficiencies Humoral



- Slides: 47
Immunodeficiencies and autoimmune diseases Martin Liška
Immunodeficiencies • Humoral – innate immunity - complement, MBL acquired immunity – immunoglobulins (B lymphocytes) • Cell mediated immunity – innate immunity – phagocytes - acquired immunity – T lymphocytes • Primary – congenital, genetically defined, symptoms predominantly at early age • Secondary – the onset of symptoms at any age chronic diseases effect of irradiation immunosuppression surgical intervention, injuries stress
Immunodeficiencies – critical life periods in respect to symptoms onset • Newborn age - severe primary disorders of cell mediated immunity • 6 mth. – 2 yrs. – severe humoral immunodeficiencies cong. /transient • 3 - 5 yrs. – transient and selective humoral immunodeficiencies, secondary immunodeficiencies • 15 – 20 yrs. – hormonal instability, thymus involution, life-style changes, some typical infections first symptoms of CVID • Middleage – often excessive workload, stress first symptoms of autoimmune disorders (also immunodeficiency) • Advanced and old age – rather symptoms of severe secondary immunodeficiencies, repercussion of functional disorders
Immunodeficiencies – major clinical features • Antibodies - microbial infections (capsulated bacteria) respiratory - pneumonia, sinusitis, otitis GIT – diarrhea • Complement system – microbial infections (pyogenic), sepsis edema (HAE) – C 1 -INH deficiency • T cells - bacterial, fungal, viral infections GIT – diarrhoea respiratory – pneumonia, sinusitis • Phagocytes - abscesses, recurrent purulent skin infections granulomatous inflammation
I. Primary immunodeficiencies – defects of phagocytosis 1/ Quantitative – decreased numbers of granulocytes Congenital chronic agranulocytosis Cyclic agranulocytosis (neutropenia)
I. Primary immunodeficiencies – defects of phagocytosis 2/ Qualitative – phagocytes functional disorders, various enzyme deficits, inability of phagocytes to degrade the ingested material Chronic Granulomatous Disease (CGD) • Approximately in 60% X-linked, some forms AR • Enzymatic inability to generate toxic oxygen metabolites (H 2 O 2) during oxygen consumption) - defect in neutrophilic cytochrome b (part of complex containing NADPH oxidase) • Inability to kill catalase producing bacteria such as Staph. aureus, Pseud. aeruginosa • Clinical features: granulomas of skin, organs • Treatment: long-term ATB prophylaxis, in severe cases BMT
II. Primary immunodeficiencies – complement system disorders Hereditary angioedema (HAE) • Absence or functional defect of C 1 -inhibitor • Recurrent swellings of skin or mucosa (oropharynx, gut) triggered by intercurrent infect, trauma or surgery • Uncontroled activation of kinin system • Laryngeal edemas could be life-threatening, immediate treatment is necessary • Treatment: preventive – androgens, EACA, C 1 -inhibitor concentrate rescue - administration of C 1 -inh. concentrate (or recombinantly prepared) - administration of bradykinin receptor antagonist (icatibant)

III. Primary immunodeficiencies – antibody deficiencies X-linked hypogamaglobulinemia (XLA, Bruton’s agammaglobulinemia) • Most common X-linked form • Block of maturation of pre-B cells into B cells (Bruton’s tyrosine kinase defect) • Undetectable or very low serum levels of Ig, absence of B cells • Symptoms: pneumonias, pyogenic otitis, increased occurrence of pulmonary fibrosis • Treatment: life-long Ig replacement CVID – Common Variable Immuno. Deficiency • Heterogenous group of B cell functional defects • Low levels of Ig. G and Ig. A, B cell counts normal • Symptoms: onset mostly between 3 rd and 4 th decade recurrent respiratory tract infections (pneumonia, sinusitis) • Treatment: life-long Ig replacement
III. Primary immunodeficiencies – antibody deficiencies Selective Ig. A deficiency • Disorder of B cell function: absence of Ig. A, levels of the other Ig normal • Recurrent mild/moderate infections or asymptomatic • Risk of reaction to live attenuated vaccines or generation of anti-Ig. A antibodies after blood transfusion Selective Ig. G subclasses deficiency, specific Ig. G deficiency • B cell functional disorder • Onset of symptoms in childhood, mostly respiratory tract infections caused by encapsulated bacteria (H. influenzae, Pneumococci) Transitory hypogammaglobulinemia of infancy • Milder and transitory decrease of Ig. G and Ig. A
IV. Primary immunodeficiencies – combined T and B cell disorders di. George syndrome • Disorder of development of 3 rd and 4 th branchial pouch → congenital heart disease + absence of thymus + absence of parathyroid glands • Complete or parcial • Symptoms: symptoms of cong. heart dis. – prominent immunodeficency – variable (mild functional → absence of T cells) hypocalcemic spasms – possible mental deficit • Treatment: symptomatic, in complete form BMT
IV. Primary immunodeficiencies – combined T and B cell disorders SCID – Severe Combined Immuno. Deficiency X-linked recessive or AR disease, combined disorder of humoral and cell mediated immunity • Severe disorder (patients often die during until 2 nd year of age), onset of symptoms soon after birth (severe diarrhoea, pneumonia, meningitis, BCGitis) • Immunological features: typically lymphopenia, absence of T cells, hypogammaglobulinemia • Forms: X-linked form – the most common, T-B+NK-, defect of common gamma chain shared by receptors of various important cytokines → absence of T cells AR form – T-B-, enzymatic defect (ADA, PNP) → accumulation of metabolites toxic for DNA synthesis → lymphopenia Ommen sy. - defect of recombinases → defect of VDJ recombination → proliferation of one or more clones of autoreactive T cells • Treatment: BMT is of critical significance, in ADA deficiency gene therapy ATB, IVIG •
V. Primary immunodeficiencies immunodeficiency with immune dysregulation X-linked lymphoproliferative syndrome (XLP) • Abnormal immune response to EBV infection which leads to uncontroled lymphoproliferation • Disorder of gene localized on X chromosome - mutation of gene coding protein associated with signal activating molecule of lymphocytes SLAM (SAP) or inhibitor of apoptosis (XIAP) • Development of uncontroled lymphoproliferation and NK cell disorder • EBV infection with fulminant or fatal course leading to liver failure → surviving patients are at risk of B cell lymphoma development, hypogammaglobulinemia similar to CVID or aplastic anemia • Without BMT performed before EBV infection development, XLP is fatal sooner or later
VI. Primary immunodeficiencies –well-defined syndromes with immunodeficiency Hyper. Ig. E syndrome (HIES, Job’s syndrome) • Eczema + combined immunodeficiency manifesting by recurrent abscesses (cold abscesses) + recurrent sinopulmonary infections • More common AD form caused by mutation of STAT 3 gene (Signal Transducer and Activator of Transcription 3), less common AR form caused by mutation of DOCK 8 gene (Dedicator Of Cyto. Kinesis 8) Symptoms: onset frequently in infancy recurrent staphylococcal abscesses of skin, lungs, joints or internal organs recurrent sinopulmonary infections, pneumatocele severe atopic eczema in AD form: skeletal disorders (facial asymmetry, prominent forehead, broad nasal bridge, spontaneous bone fractures, osteopenia), delayed dental erruption
VI. Primary immunodeficiencies –well-defined syndromes with immunodeficiency Hyper. Ig. E syndrome (HIES, Job’s syndrome) Symptoms: in AR form, recurrent viral infections (herpetic), increased frequency of autoimmune or allergic diseases, skeletal disorders often absent Dg: clinical features enormously increased level of serum Ig. E (˃ 2000 IU/ml) genetic tests Th: prophylaxis with anti-staphylococcal ATB dermatological therapy of eczema surgical treatment of abscesses
VI. Primary immunodeficiencies –well-defined syndromes with immunodeficiency Wiskott-Aldrich syndrome (WAS) • X-linked recessive disease • Decreased number of small platelets (microthrombocytopenia), eczema and immunodeficiency • Mutation of WASp gene → decreased production of WASp protein (exprimed on hematopoietic cells, provides dynamic changes of cytoskeleton which are necessary for function of immune cells) Symptoms: combined immunodeficiency: decreased Ig levels (↓Ig. M; ↑Ig. A and Ig. E) + defects of T cell function → recurrent otitis and sinusitis, autoimmune diseases thrombocytopenia → increased bleeding

VI. Primary immunodeficiencies –well-defined syndromes with immunodeficiency Wiskott-Aldrich syndrome (WAS) Dg: clinical symptoms proof of decreased expression of WASp on leukocytes genetic tests Th: symptomatic treatment in case of matched donor BMT studies of gene therapy
Immunoglobulin replacement therapy • Immunoglobulin concentrates are made from human plasma pooled from thousands of donors • Donors are tested for infectious diseases (HIV, hepatitis), inactivating procedures to minimize the risk of transmitting infection • Ig concentrates contain only Ig. G, content of Ig. A is minimal • Preparates for i. v. (Gammagard, Octagam) or s. c. administration (Subcuvia, Gammanorm)
Indications for Ig replacement therapy • Primary antibody deficiencies (IVIG) – life-long in XLA or CVID, transitory in combined immunodeficiencies (SCID) • Ig. G subclasses or specific Ig deficiency is sometimes also indication • Secondary antibody deficiencies – typically multiple myeloma, chronic lymphocytic leukaemia, biological treatment (rituximab)
Dosage of Ig concentrates • Agammaglobulinemia – i. v. imunoglobulins 400 -600 mg/kg/month • Regular administration in day-care centres every 3 or 4 weeks • Last years, „home therapy“ is frequently used - administration of subcutaneous Ig by infusion pump (cca every 5 to 7 days, more comfortable for patient, less adverse effects)
Secondary immunodeficiencies • Acute and chronic viral infections – infectious mononucleosis, influenza • Metabolic disorders – diabetes mellitus, uremia • Autoimmune diseases – autoantibodies against immunocompetent cells (neutrophils, lymphocytes); autoimmune phenomena also after administration of certain drugs (e. g. oxacilin, quinidine) • Chronic GIT diseases • Malignant diseases (leukemia) • Hypersplenism/asplenia • Burn, postoperative status, injuries • Severe nutritional disorders • Chronic infections • Ionizing radiation • Drug induced immunodeficiencies (chemotherapy) • Immunosupressive therapy • Chronic stress • Chronic exposure to harmful chemical substances
Acquired Immuno. Deficiency Syndrome (A. I. D. S. ) • Caused by retrovirus HIV 1 or HIV 2 • Virus has a tropism for cells bearing CD 4 surface marker (Th CD 4+ lymphocytes); also infects macrophages and CNS cells • Viral genome transcribes into human DNA and infected cell provides viral replication • Transmission: sexual contact contact with blood or blood products mother-to-child – prenatally, delivery, breast feeding • Phases: acute (flu-like symptoms) asymptomatic – months to years, viral replication, loss of Th cells symptomatic – infections, autoimmune disorders, malignancies, allergy final – systemic breakdown, opportune infections (Pneumocystis jirovecii, Cryptococcus neoformans, Toxoplasma gondii, Candida albicans, CMV etc. ) - Kaposi’s sarcoma
Acquired Immuno. Deficiency Syndrome (A. I. D. S. ) Diagnosis: - Serology - specific antibodies, 4 to 12 weeks after primoinfection Measurement of antigen p 24 – before seroconversion Viral RNA measurement – before seroconversion, PCR testing Th cells counts Therapy: - HAART (Highly Active Antiretroviral Therapy) – combination of nucleoside (Zidovudine) and non-nucleoside (Nevirapin) reverse transcriptase inhibitors and protease inhibitors (Lopinavir)

Acquired Immuno. Deficiency Syndrome (A. I. D. S. ) Therapy: - Prophylaxis with antibiotics and antimycotics - TBC prevention (isoniazid) - Ig replacement
AUTOIMMUNE DISEASES
Autoimmune disease • Results from a failure of self-tolerance • Immunological tolerance is specific unresponsiveness to an antigen • All individuals are tolerant of their own (self) antigens
AUTOIMMUNE PATOLOGICAL RESPONSEETIOLOGY • the diseases are chronic and usually irreversible • incidence: 5%-7% of population, higher frequencies in women, increases with age • factors contribute to autoimmunity: - internal (HLA association, polymorphism of cytokine genes, defect in genes regulating apoptosis, polymorphism in genes for TCR a H immunoglobulin chains, association with immunodeficiency, hormonal factors) - external (infection, stress by activation of neuroendocrine axis and hormonal dysbalance, drug and ionization through modification of autoantigens)
CLINICAL CATEGORIES • systemic - affect many organs and tissue • organoleptic - affect predominantly one organ accompanied by affection of other organs (inflammatory bowel diseases, celiac disease, AI hepatitis, pulmonary fibrosis) • organ specific - affect one organ or group of organs connected with development or function
SYSTEMIC AUTOIMMUNE DISEASES • • Systemic lupus erythematosus Rheumathoid arthritis Sjögren‘s syndrome Dermatopolymyositis Systemic sclerosis Mixed connective tissue disease Vasculitis
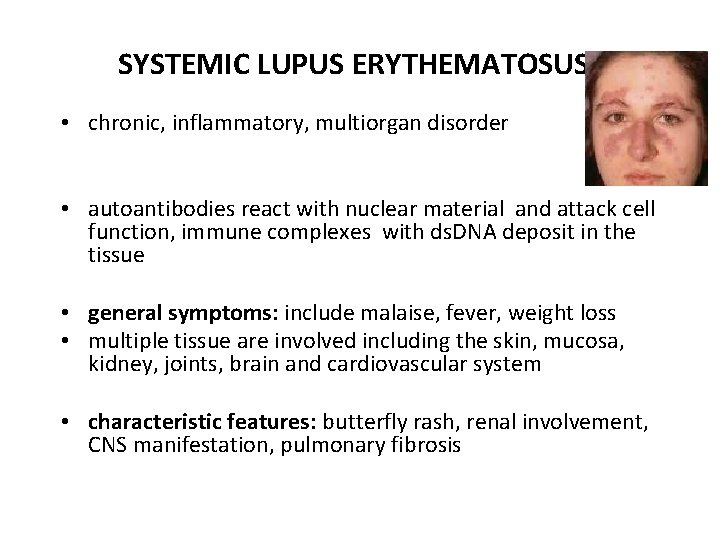
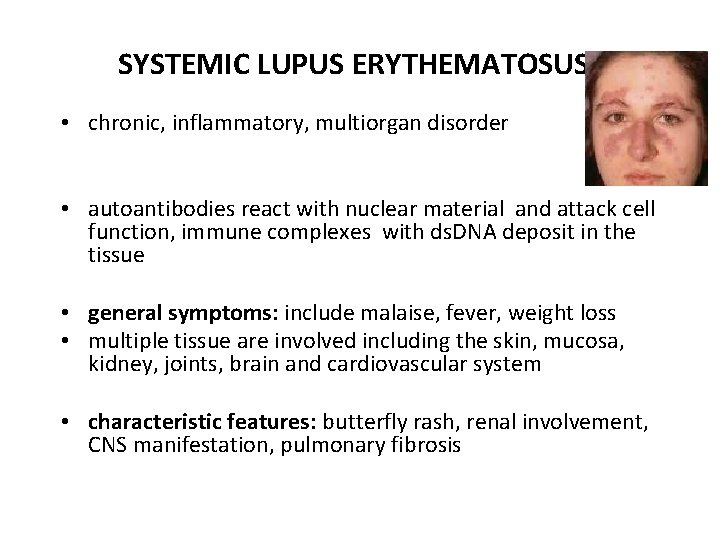
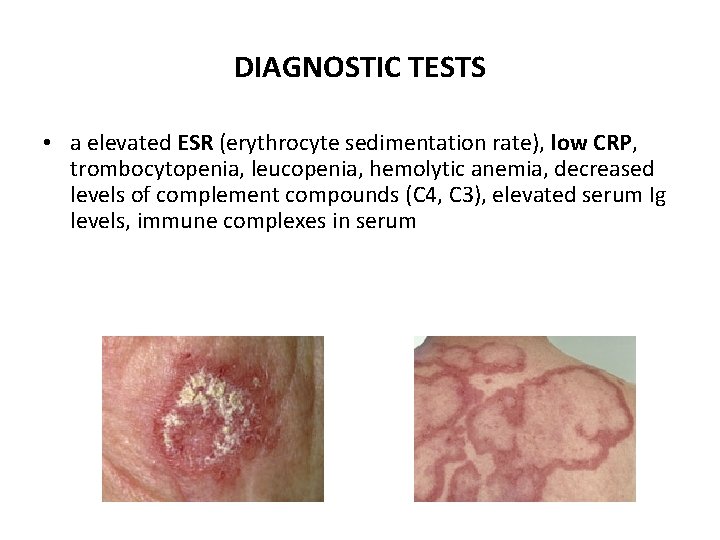
SYSTEMIC LUPUS ERYTHEMATOSUS • chronic, inflammatory, multiorgan disorder • autoantibodies react with nuclear material and attack cell function, immune complexes with ds. DNA deposit in the tissue • general symptoms: include malaise, fever, weight loss • multiple tissue are involved including the skin, mucosa, kidney, joints, brain and cardiovascular system • characteristic features: butterfly rash, renal involvement, CNS manifestation, pulmonary fibrosis
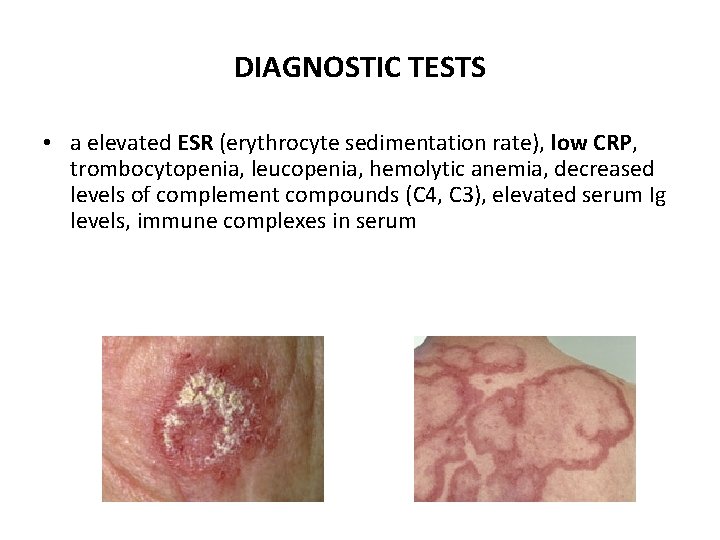
DIAGNOSTIC TESTS • a elevated ESR (erythrocyte sedimentation rate), low CRP, trombocytopenia, leucopenia, hemolytic anemia, decreased levels of complement compounds (C 4, C 3), elevated serum Ig levels, immune complexes in serum
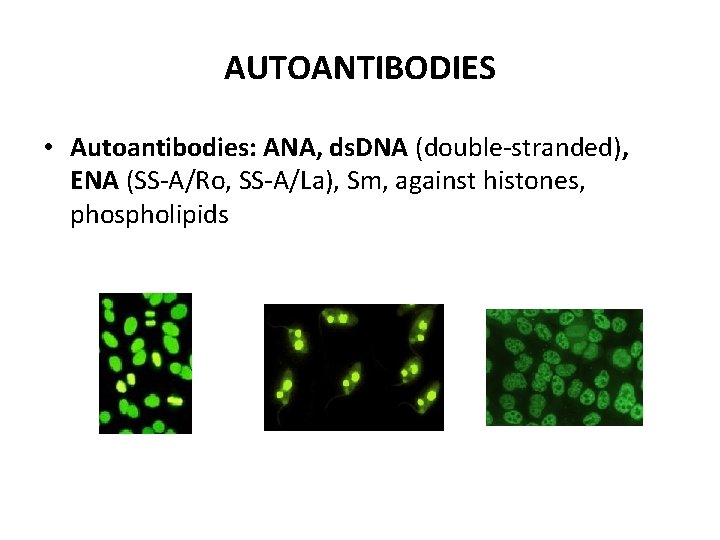
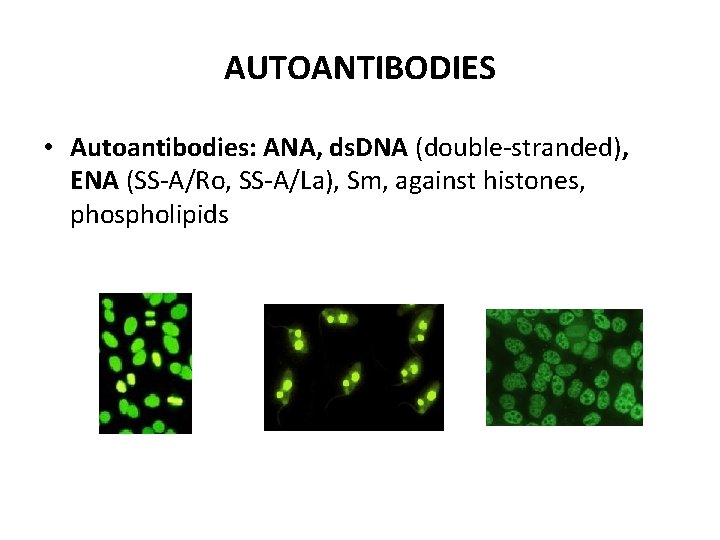
AUTOANTIBODIES • Autoantibodies: ANA, ds. DNA (double-stranded), ENA (SS-A/Ro, SS-A/La), Sm, against histones, phospholipids
RHEUMATOID ARTHRITIS • chronic, inflammatory disease with systemic involvement • characterized by an inflammatory joint lesion in the synovial membrane, destruction of the cartilage and bone, results in the joint deformation • clinical features: arthritis, fever, fatigue, weakness, weight loss • systemic features: vasculitis, pericarditis, uveitis, nodules under skin, intersticial pulmonary fibrosis • diagnostic tests: elevated C- reactive protein and ESR, elevated serum gammaglobulin levels - autoantibodies against Ig. G = rheumatoid factor (RF), a-CCP (cyclic citrulline peptid), ANA - X-rays of hands and legs- show a periarticular porosis, marginal erosion
SJÖGREN‘S SYNDROME • • chronic inflammatory disease affecting exocrine glands the primary targets are the lacrimal and salivary gland duct epithelium general features: malaise, weakness, fever primary syndrome - features: dry eyes and dry mouth, swollen salivary glands, dryness of the nose, larynx, bronchi and vaginal mucosa, involvement kidney, central and periferal nervous system, arthritis • secondary syndrome – is associated with others AI diseases (SLE, RA, sclerodermia, polymyositis, primary biliary cirhosis, AI thyroiditis) • autoantibodies against ENA (SS-A, SS-B), ANA, RF • The Schirmer test - measures the production of tears
Vasculitis • characterized by inflammatory destruction of vessels leading to thrombosis and aneurysms • proliferation of the intimal part of blood-vessel wall and fibrinoid necrosis • affect mostly lung, kidneys, skin • diagnostic tests: elevated ESR, CRP, leucocytosis, biopsy of affected organ (necrosis, granulomas), angiography
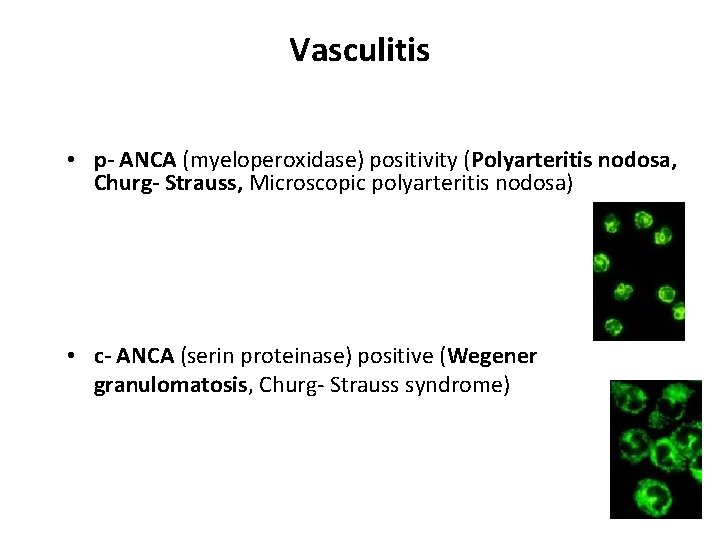
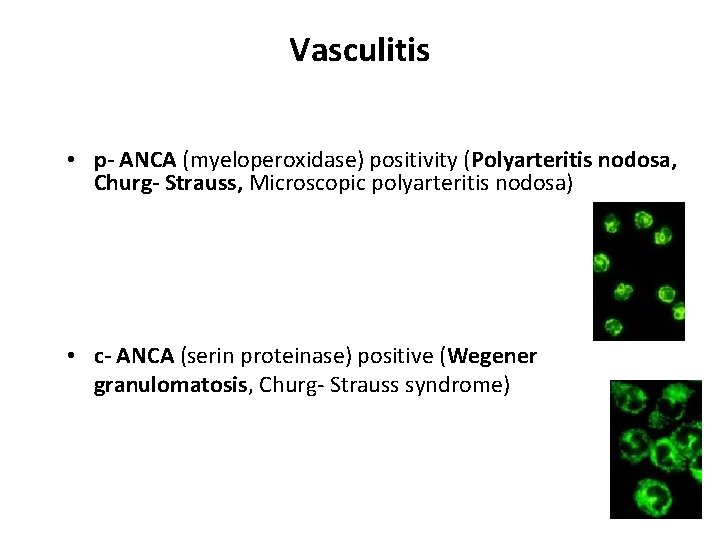
Vasculitis • p- ANCA (myeloperoxidase) positivity (Polyarteritis nodosa, Churg- Strauss, Microscopic polyarteritis nodosa) • c- ANCA (serin proteinase) positive (Wegener granulomatosis, Churg- Strauss syndrome)
Vasculitis - classification • Large vessel vasculitis (Takayasu arteritis, Giant cell (temporal) arteritis) • Medium vessel vasculitis (Polyarteritis nodosa, Wegener's granulomatosis, Kawasaki disease) • Small vessel vasculitis (Churg-Strauss arteritis, Microscopic polyarteritis, Henoch-Schönlein purpura) • Symptoms: fatigue, weakness, fever, arthralgias, abdominal pain, hypertension, renal insufficiency, and neurologic dysfunction
ORGANOLEPTIC AUTOIMMUNE DISEASES • • • Ulcerative colitis Crohn‘s disease Autoimmune hepatitis Primary biliary cirhosis Pulmonary fibrosis
Ulcerative colitis • chronic inflammation of the large intestine mucosa and submucosa • features: diarrhea, bloody and mucus stools • extraintestinal features (arthritis, uveitis) • Autoantibodies: p. ANCA, a- large intestine
Crohn‘s disease • the granulomatous inflammation of whole intestinal wall with ulceration and scarring that can result in abscess and fistula formation • the inflammation of Crohn's disease the most commonly affects the terminal ileum, presents with diarrhea and is accompanied by extraintestinal features - iridocyclitis, uveitis, artritis, spondylitis • antibodies against Saccharomyces cerevisiae (ASCA), a- pancreas
ORGAN SPECIFIC AUTOIMMUNE DISEASES AUTOIMMUNE ENDOCRINOPATHIES • • • Hashimoto‘s thyroiditis Graves-Basedow disease Diabetes mellitus I. type Addison‘s disease Autoimmune polyglandular syndrome
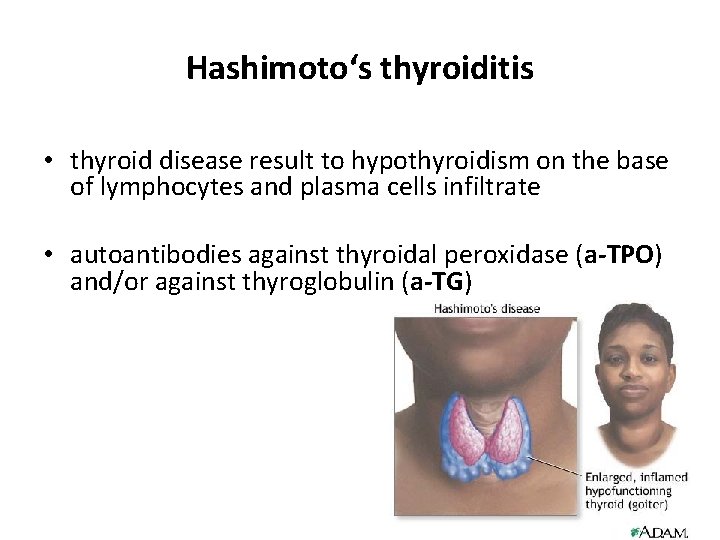
Hashimoto‘s thyroiditis • thyroid disease result to hypothyroidism on the base of lymphocytes and plasma cells infiltrate • autoantibodies against thyroidal peroxidase (a-TPO) and/or against thyroglobulin (a-TG)
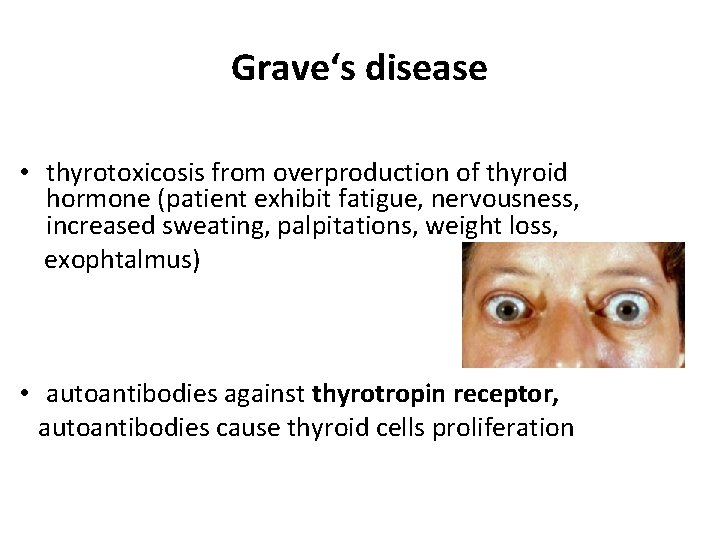
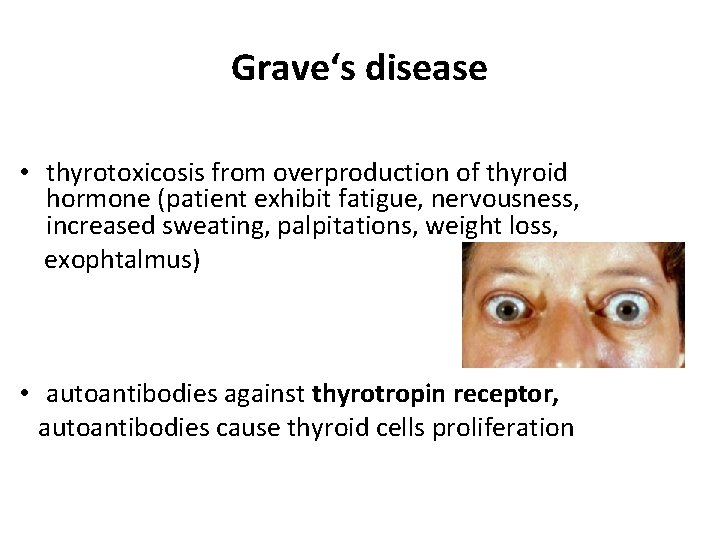
Grave‘s disease • thyrotoxicosis from overproduction of thyroid hormone (patient exhibit fatigue, nervousness, increased sweating, palpitations, weight loss, exophtalmus) • autoantibodies against thyrotropin receptor, autoantibodies cause thyroid cells proliferation
Diabetes mellitus (insulin- dependent) • characterized by an inability to process sugars in the diet, due to a decrease in or total absence of insulin production • results from immunologic destruction of the insuline- producing β-cells of the islets of Langerhans in the pancreas • autoantibodies against GAD (glutamic acid decarboxylase = primary antigen), autoantibodies anti- islet cell, anti- insulin • islets are infiltrated with B and T cells
ORGAN SPECIFIC AUTOIMMUNE DISEASES AUTOIMMUNE NEUROPATHIES • Guillain-Barré syndrome (acute idiopathic polyneuritis) • Myasthenia gravis • Multiple sclerosis
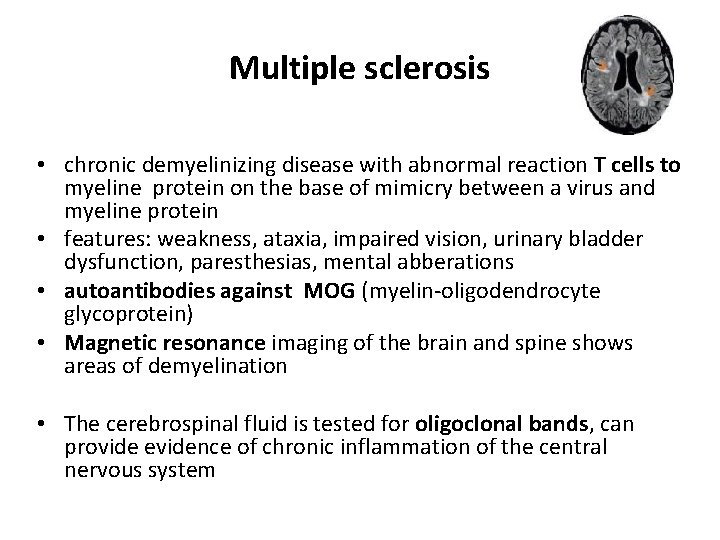
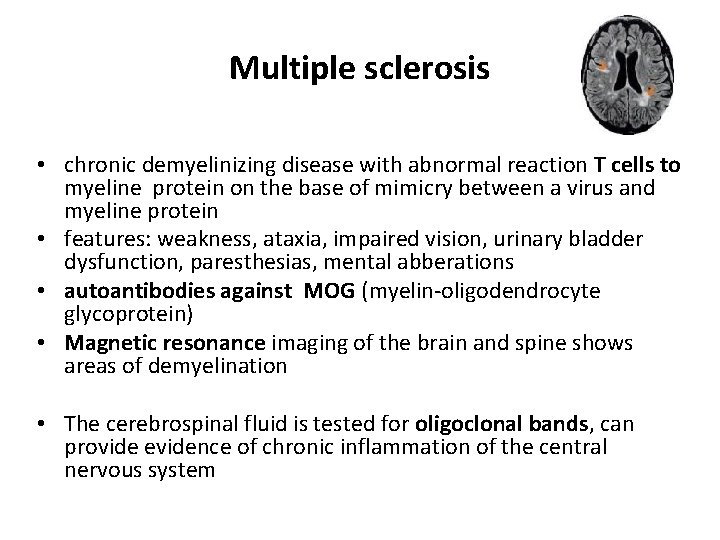
Multiple sclerosis • chronic demyelinizing disease with abnormal reaction T cells to myeline protein on the base of mimicry between a virus and myeline protein • features: weakness, ataxia, impaired vision, urinary bladder dysfunction, paresthesias, mental abberations • autoantibodies against MOG (myelin-oligodendrocyte glycoprotein) • Magnetic resonance imaging of the brain and spine shows areas of demyelination • The cerebrospinal fluid is tested for oligoclonal bands, can provide evidence of chronic inflammation of the central nervous system
ORGAN SPECIFIC AUTOIMMUNE DISEASES AUTOIMMUNE CYTOPENIA • AI hemolytic disease- autoantibodies against membrane erythrocyte antigens • AI trombocytopenia - autoantibodies against trombocyte antigens (GPIIb/IIIa) • AI neutropenia - autoantibodies against membrane neutrofil antigens
Treatment of autoimmune diseases Systemic AI – non-specific immunosuppression: glucocorticoids cytostatics: • alkylating agents cyclophosphamide • purine analogs - azathioprine, mycophenolate, • antimetabolites - metotrexate • antibiotics - cyclosporin A, tacrolimus • monoclonal antibodies Organ specific AI non-specific immunosuppression Endocrinopathies Substitution of lacking product of endocrinal gland destroyed by AI process -insulin, thyroid gland hormones
 Cupping therapy for thyroid
Cupping therapy for thyroid Endocrine system pearson
Endocrine system pearson Humoral and cell mediated immunity difference
Humoral and cell mediated immunity difference Penyebab pew pada ckd
Penyebab pew pada ckd Crohn's disease test
Crohn's disease test Rheumatic heart disease
Rheumatic heart disease Humoral stimulus
Humoral stimulus Humoral stimulus
Humoral stimulus Effector mechanism of humoral immunity
Effector mechanism of humoral immunity Celular
Celular Actihol
Actihol Respuesta adaptativa humoral
Respuesta adaptativa humoral Humoral patoloji paradigması
Humoral patoloji paradigması Limfoblast
Limfoblast Respuesta humoral
Respuesta humoral Abbas
Abbas Xhosa cattle-killing movement map
Xhosa cattle-killing movement map Moralna karakterizacija
Moralna karakterizacija Kiklop likovi
Kiklop likovi Baločanski
Baločanski Opseg kvadrata i pravokutnika 4 razred
Opseg kvadrata i pravokutnika 4 razred Opseg lika
Opseg lika Taktika darba laiks
Taktika darba laiks Povratak filipa latinovicza
Povratak filipa latinovicza Lika i gorski kotar
Lika i gorski kotar Lik ruznog paceta
Lik ruznog paceta Dnevnik pauline p. lektira
Dnevnik pauline p. lektira Lika syndrome
Lika syndrome Alegorijska pripovijetka
Alegorijska pripovijetka Načelo lika in podlage
Načelo lika in podlage Judita miro gavran pdf
Judita miro gavran pdf Arber lika
Arber lika Ivica kičmanović opis lika
Ivica kičmanović opis lika Simetrija naloge
Simetrija naloge Jednostavni epski oblici
Jednostavni epski oblici Dijalektalna lirika
Dijalektalna lirika Lika syndrome
Lika syndrome Lifestyle modern
Lifestyle modern Venn diagram of communicable and noncommunicable diseases
Venn diagram of communicable and noncommunicable diseases Section 19-3 diseases caused by bacteria and viruses
Section 19-3 diseases caused by bacteria and viruses Chapter 8 skin disorders and diseases review questions
Chapter 8 skin disorders and diseases review questions Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Chapter 22 genetics and genetically linked diseases
Chapter 22 genetics and genetically linked diseases Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Onychomycosis milady
Onychomycosis milady