Immunity Chapter 35 Three Lines of Defense Barriers
Immunity Chapter 35
Three Lines of Defense • Barriers at body surfaces • Nonspecific responses • Immune responses
Barriers at Body Surface • Intact skin and mucous membranes • Lysozyme • Normal bacterial flora • Flushing effect and low p. H of urine
Nonspecific Responses • Lymph nodes trap and kill pathogens • Natural killer cells attack a range of targets • Inflammation
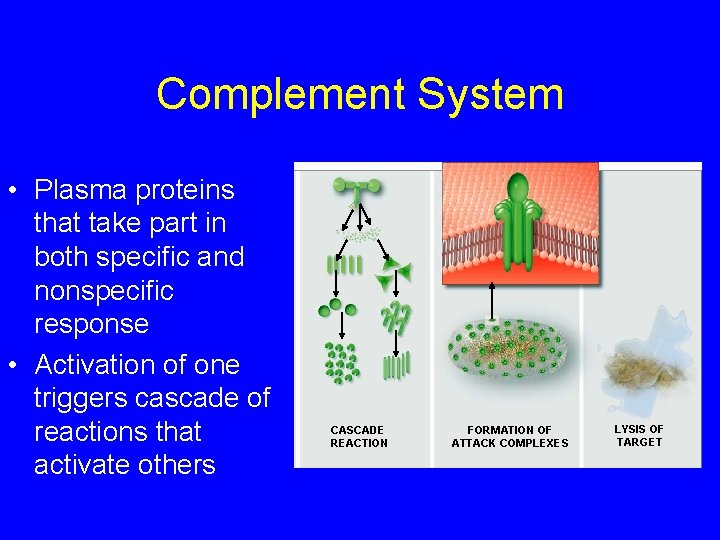
Complement System • Plasma proteins that take part in both specific and nonspecific response • Activation of one triggers cascade of reactions that activate others CASCADE REACTION FORMATION OF ATTACK COMPLEXES LYSIS OF TARGET
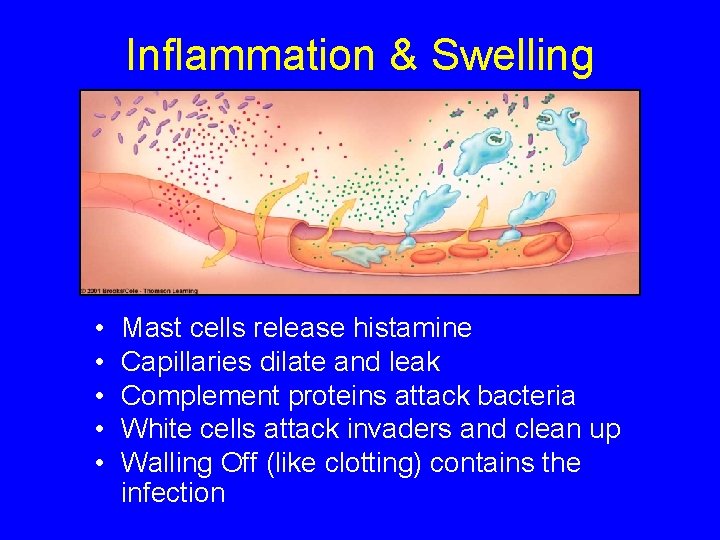
Inflammation & Swelling • • • Mast cells release histamine Capillaries dilate and leak Complement proteins attack bacteria White cells attack invaders and clean up Walling Off (like clotting) contains the infection
Immune Responses • Directed against specific invaders • Carried out by T cells, B cells, and macrophages • Communication signals such as interleukins play a vital role
Features of Immune System • Immunological specificity – B and T cells zero in on certain kinds of pathogens; response is pathogen specific • Immunological memory – Immune system recognizes and reacts swiftly to a pathogen it has “seen”
Memory and Effector Cells • When a B or T cell is stimulated to divide, it produces more than one cell type • Memory cells are set aside for future use; they are the basis for immune memory • Effector cells engage and destroy the current threat
Key Component of Immune Response • • • MHC markers Antigen-presenting cells Helper T cells Effector cytotoxic T cells Natural killer cells B cells make antibodies
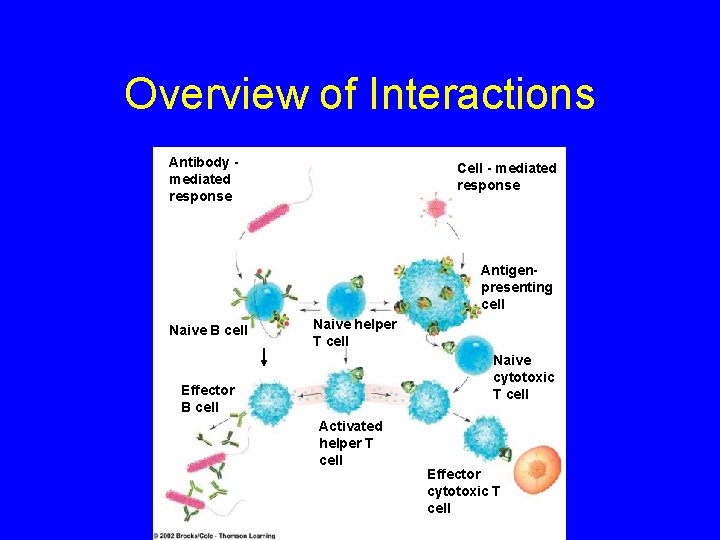
Overview of Interactions Antibody mediated response Cell - mediated response Antigenpresenting cell Naive B cell Naive helper T cell Naive cytotoxic T cell Effector B cell Activated helper T cell Effector cytotoxic T cell
B Cell Formation • Derived from stem cells in bone marrow • Acquire unique antigen-binding receptors in marrow • Receptors interact with just one antigen • Exposure to that antigen causes clonal selection – Division of cells specific for that antigen
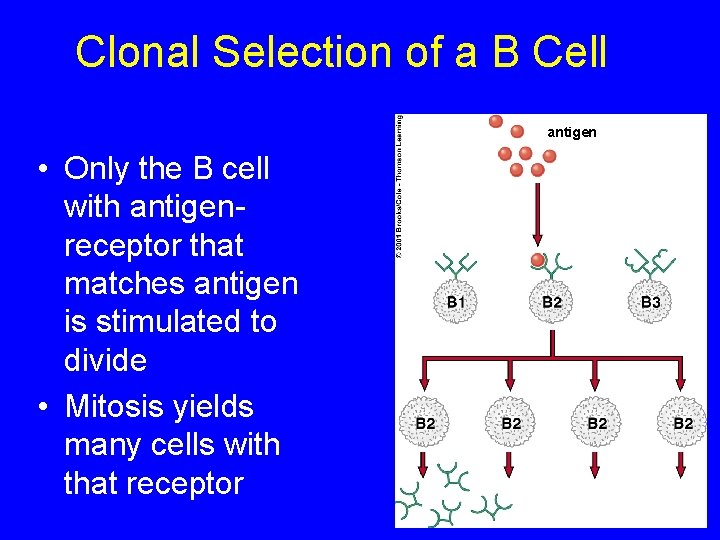
Clonal Selection of a B Cell antigen • Only the B cell with antigenreceptor that matches antigen is stimulated to divide • Mitosis yields many cells with that receptor
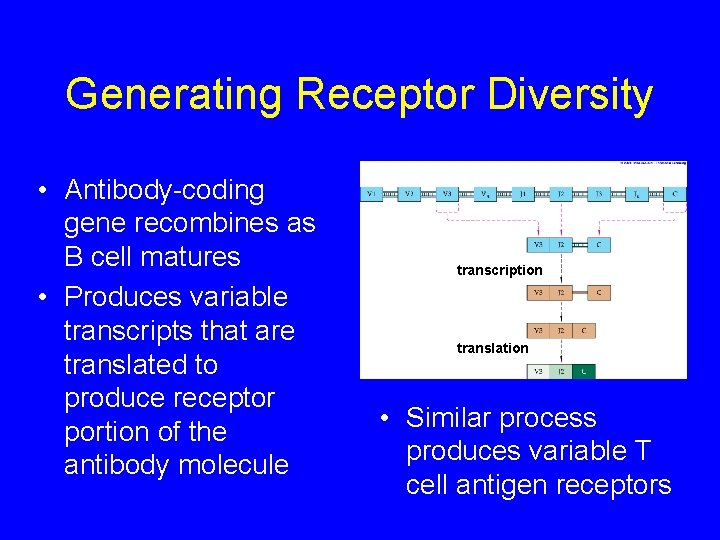
Generating Receptor Diversity • Antibody-coding gene recombines as B cell matures • Produces variable transcripts that are translated to produce receptor portion of the antibody molecule transcription translation • Similar process produces variable T cell antigen receptors
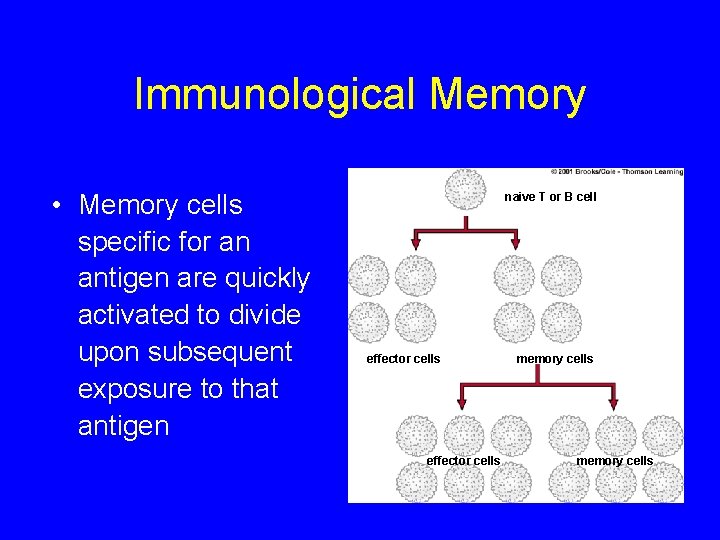
Immunological Memory • Memory cells specific for an antigen are quickly activated to divide upon subsequent exposure to that antigen naive T or B cell effector cells memory cells
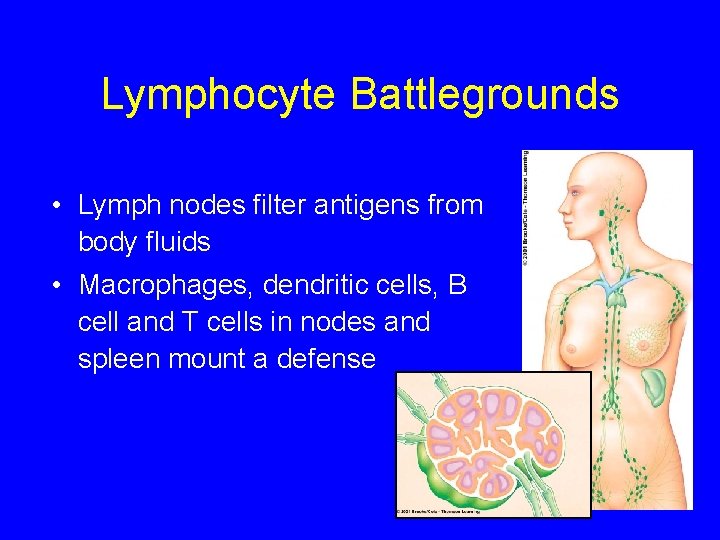
Lymphocyte Battlegrounds • Lymph nodes filter antigens from body fluids • Macrophages, dendritic cells, B cell and T cells in nodes and spleen mount a defense
Antibody-Mediated Response • Carried out by B cells • Targets are extracellular pathogens and toxins • Antibodies bind to target and mark it for destruction by phagocytes and complement
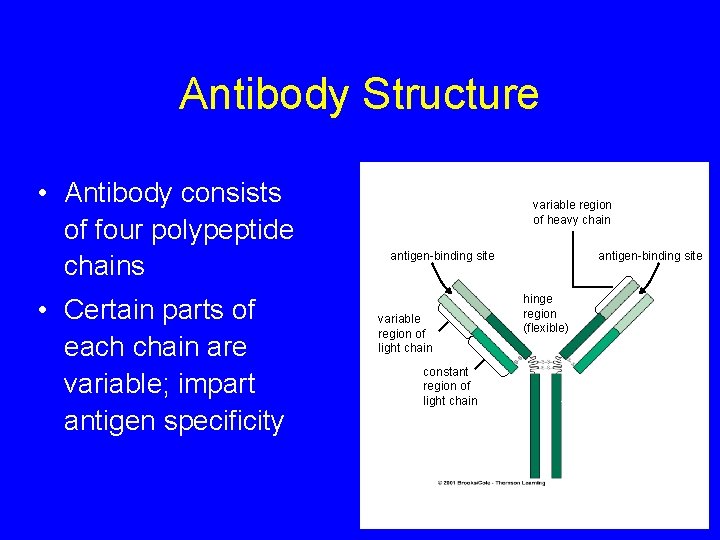
Antibody Structure • Antibody consists of four polypeptide chains • Certain parts of each chain are variable; impart antigen specificity variable region of heavy chain antigen-binding site variable region of light chain constant region of light chain antigen-binding site hinge region (flexible)
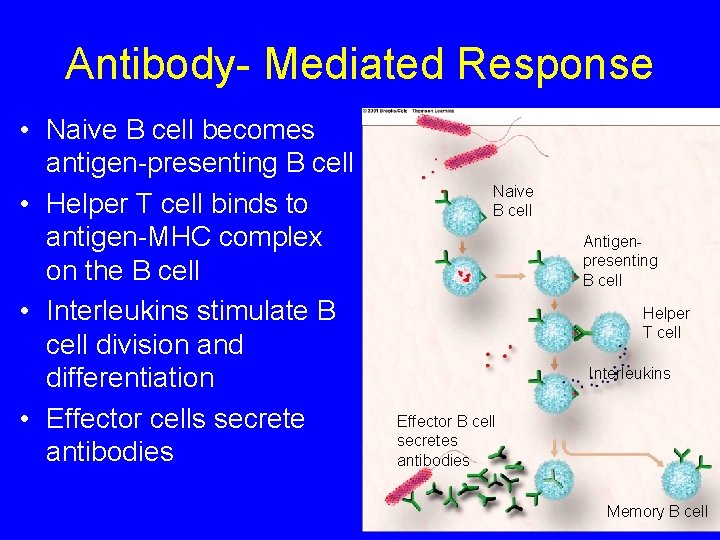
Antibody- Mediated Response • Naive B cell becomes antigen-presenting B cell • Helper T cell binds to antigen-MHC complex on the B cell • Interleukins stimulate B cell division and differentiation • Effector cells secrete antibodies Naive B cell Antigenpresenting B cell Helper T cell Interleukins Effector B cell secretes antibodies Memory B cell
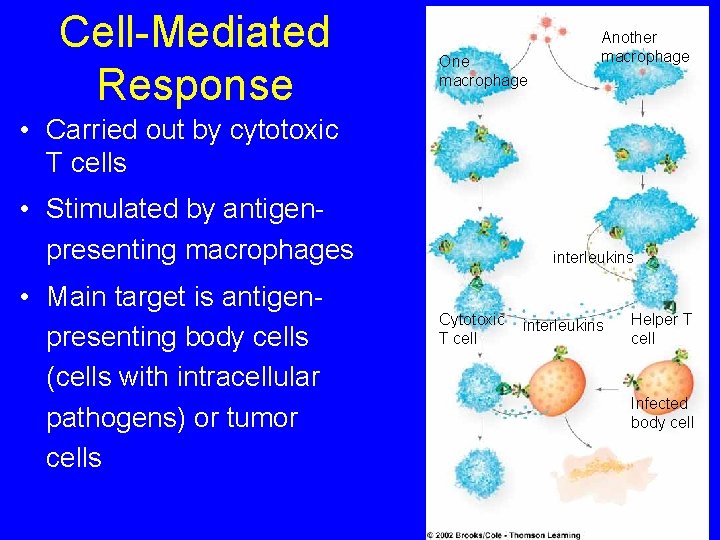
Cell-Mediated Response One macrophage Another macrophage • Carried out by cytotoxic T cells • Stimulated by antigenpresenting macrophages • Main target is antigenpresenting body cells (cells with intracellular pathogens) or tumor cells interleukins Cytotoxic T cell interleukins Helper T cell Infected body cell
Immunization • Process that promotes immunity • Active immunization – Antigen-containing material is injected – Confers long lasting immunity • Passive – Purified antibody is injected – Protection is short lived
Allergies • Immune reaction to a harmless substance like pollen (allergens) • Genetic predisposition • Ig. E responds to antigen by binding to mast cells and basophils • These cells secrete the substances, like histamine, that cause symptoms
Anaphylactic Shock • A life-threatening allergic reaction • Caused by the release of histamine by many mast cells and basophils • Airways constrict and blood pressure drops as capillary permeability soars
Autoimmune Disorders • Immune system makes antibodies against self antigens • Sometimes triggered by exposure to a virus
AIDS = Acquired Immune Deficiency Syndrome • Combination of disorders that follows infection with HIV • Opportunistic diseases like – Yeast (Candida) infections – Pneumocystis pneumonia – Karposi’s sarcoma
HIV Replication (1) • RNA retrovirus • A protein at virus surface binds to host cells with CD 4 receptors • These receptors occur on helper T cells • Once bound, RNA and viral enzymes enter the host cell
HIV Replication (2) • Viral RNA is reverse transcribed to DNA • HIV DNA is called provirus; it inserts into host DNA • The host cell makes copies of viral DNA and viral proteins that assemble to form new virus particles
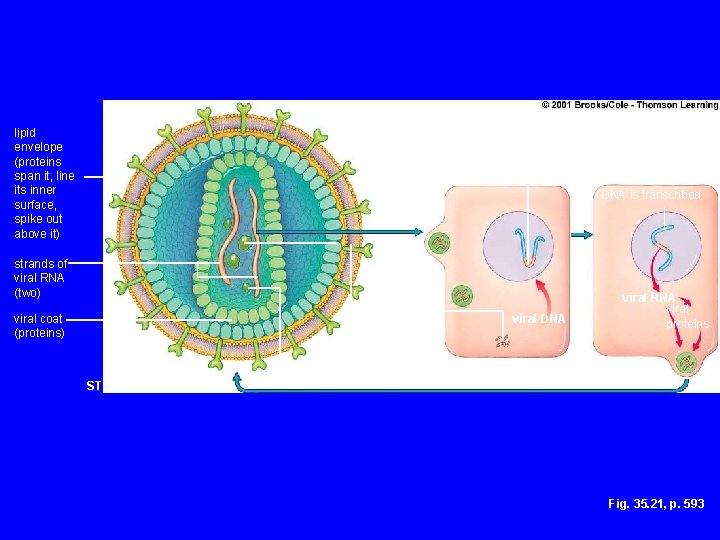
lipid envelope (proteins span it, line its inner surface, spike out above it) viral genes are integrated into the host DNA is transcribed viral RNA enters cell strands of viral RNA (two) a strand of viral RNA undergoes reverse transcription viral coat (proteins) intergrase reverse transcriptase viral DNA host cell viral RNA viral proteins budding STRUCTURE OF HIV Fig. 35. 21, p. 593
Effect of T Cell Decline • CD 4 helper T cells play a vital role in immune function • They are required for both cell-mediated antibody-mediated immunity • Infected individual becomes vulnerable to other infections, which eventually result in death
Transmission of HIV • HIV does not live long outside human body • Most often spread by exchange of bodily fluids with an infected person • In the U. S. , anal intercourse and needle sharing are main modes of transmission
Transmission of HIV • Less commonly transmitted by vaginal intercourse and oral sex • Can travel from mothers to offspring during pregnancy, birth, or breastfeeding • Not known to be transmitted by food, air, water, casual contact, or insect bites
Treatment • No cure • Once HIV genes are incorporated, no way to get them out • AZT, and other drugs slow the course of the disease and increase life span • Researchers continue to develop drugs and to work toward an AIDS vaccine
- Slides: 32