Immediate implant placement and restoration in the anterior
- Slides: 40
Immediate implant placement and restoration in the anterior maxilla: Tissue dimensional changes after 2‐ 5 year follow up Arora H, Khzam N, Roberts D, Bruce WL, Ivanovski S. Clinical Implant Dentistry and Related Research. 2017 Apr 1.
TOPIC FOR TODAYS DISCUSSION? • What are the tissue changes in immediate loading? ?
Terms to be talk • Immediate implant Loading • Osseointegration
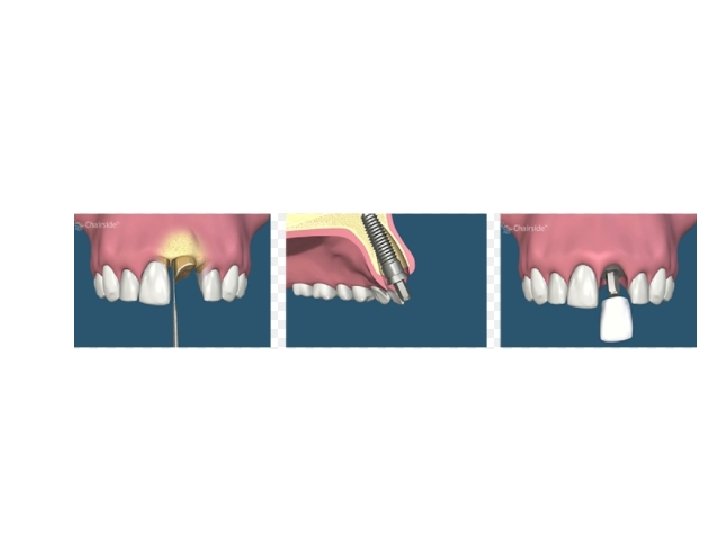
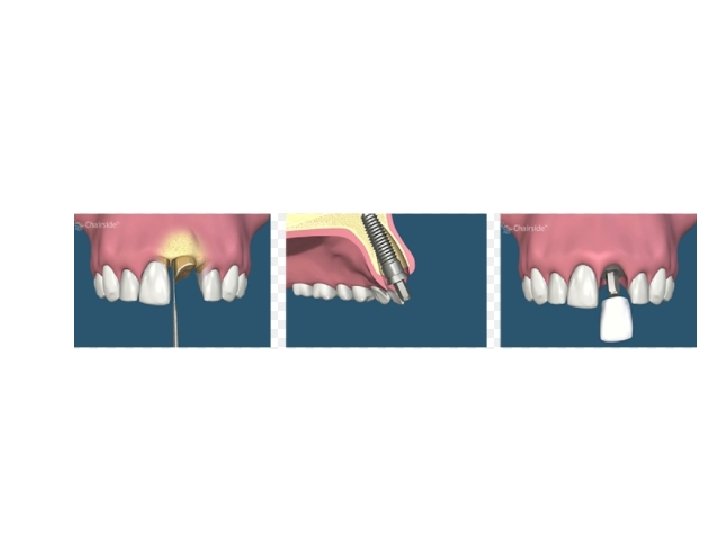
Immediate loading • immediate loading (provisionalization) of an implant at the time of placement has become a viable treatment option, particularly in the esthetic zone. When replacing one or two teeth in the anterior maxilla, provisionalization can be simplified by immediately loading the implant.
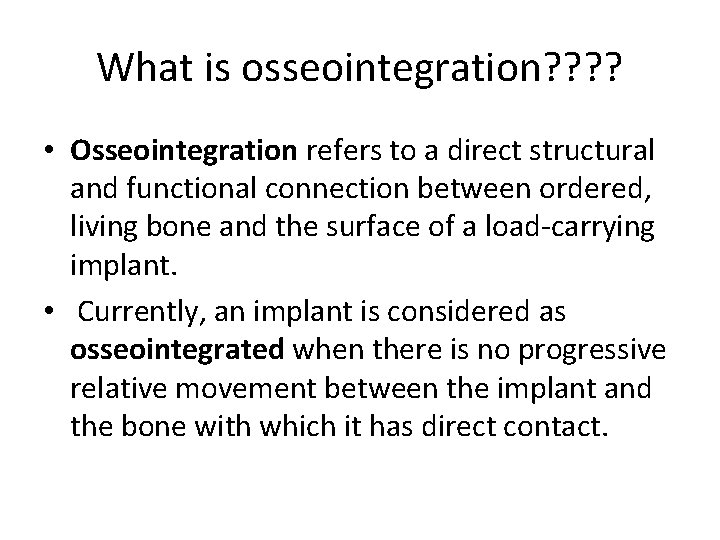
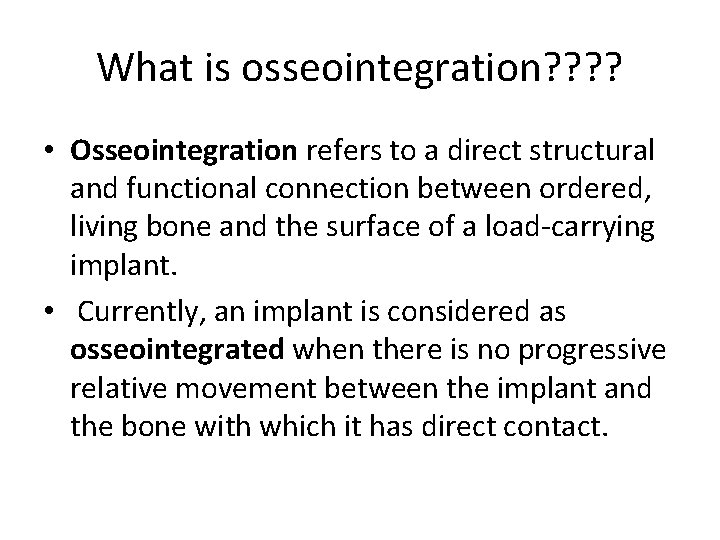
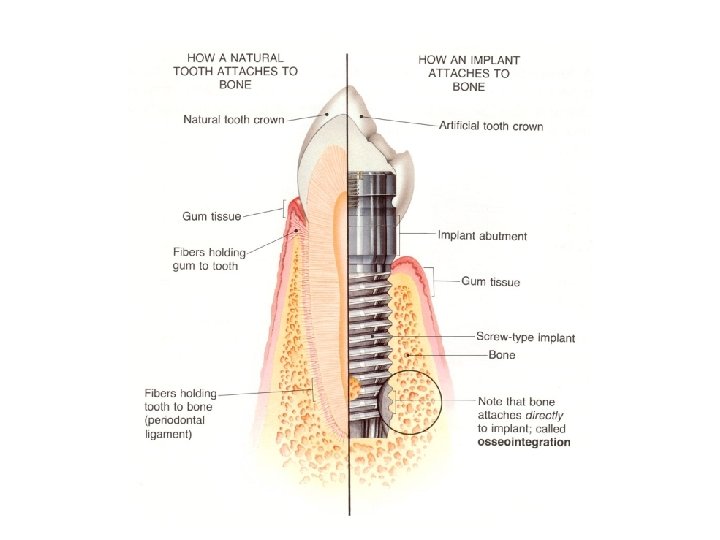
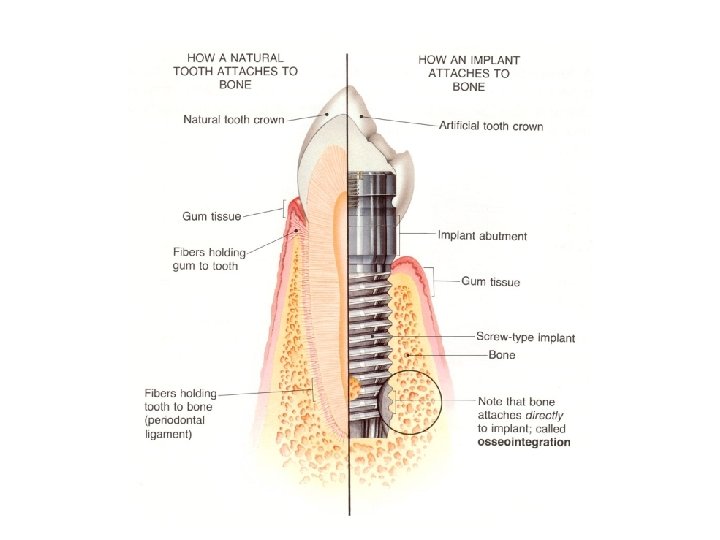
What is osseointegration? ? • Osseointegration refers to a direct structural and functional connection between ordered, living bone and the surface of a load‐carrying implant. • Currently, an implant is considered as osseointegrated when there is no progressive relative movement between the implant and the bone with which it has direct contact.
Immediate implant placement and restoration in the anterior maxilla: Tissue dimensional changes after 2‐ 5 year follow up Arora H, Khzam N, Roberts D, Bruce WL, Ivanovski S. Clinical Implant Dentistry and Related Research. 2017 Apr 1.
Background of the study • There was a lack of litrature were there regarding soft and hard tissue changes of Immediate implant placement and restoration in the anterior maxilla
Materials and methods • This study included 30 patients who were recruited and treated for immediate single tooth implants in the maxillary anterior region at a private practice in Brisbane, Australia.
Inclusion criteria: 1. Age at least 18 years 2. Presence of a single failing tooth in the anterior maxillary region (13‐ 23) 3. Presence of natural teeth adjacent to the tooth being replaced 4. Adequate bone height apical to the failing tooth to allow for placement of an implant and to achieve a primary stability of at least 30 Ncm
Exclusion criteria 1. Contraindications for routine implant therapy (untreated periodontitis, uncontrolled diabetes, medical conditions that contraindicate elective surgery) 2. Smoking >10 cigarettes per day 3. Presence of acute infection around the tooth being replaced 4. Presence of any soft tissue pathology at the gingival margin. 5. Any fenestration or dehiscence in the socket wall of the failing tooth
Surgical and prosthetic procedures • All surgical procedures were conducted by a single operator under local anaesthesia. • A prophylactic antibiotic dose of Amoxicillin, 500 mg three times daily, was started a day before surgery and continued for 1 week. • On the day of the surgery, the tooth scheduled to be replaced was removed as atraumatically as possible using periotomes and without flap elevation.
• Every attempt was made to engage the palatal and apical bone to achieve a high primary stability (30 Ncm) while placing the implant in a correct three‐dimensional position. • In all implant sites, the gap between the implant and the inner aspect of the buccal socket wall was filled with deproteinized bovine bone particles (Bio‐Oss, Geistlich Pharma AG, Wolhusen, Switzerland).
• Postoperative instructions included Chlorhexidine rinses twice daily, for a period of 2 weeks. • For pain control, Ibuprofen 400 mg was prescribed, to be used as needed.
• Implant placement was immediately followed by connection of a temporary abutment onto which a prefabricated screw‐retained temporary crown was placed. • The provisional restoration was adjusted to ensure that it was free of any contact in both centric and eccentric positons. • After a period of 3‐ 4 months, the provisional restoration was replaced by a permanent restoration.
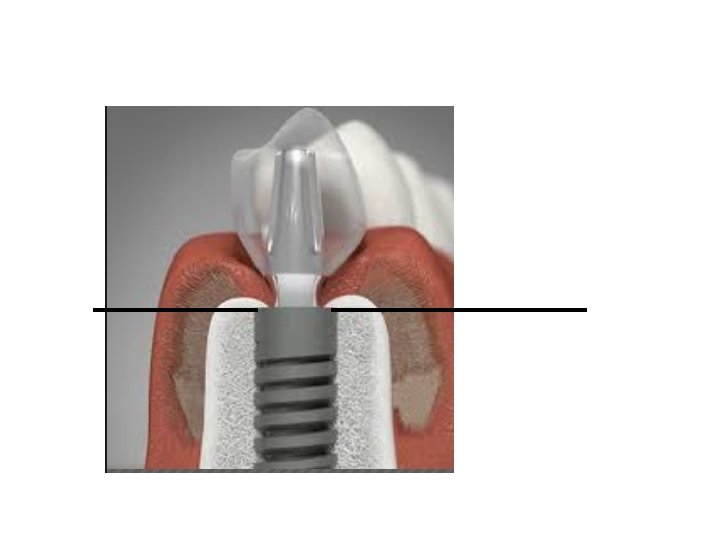
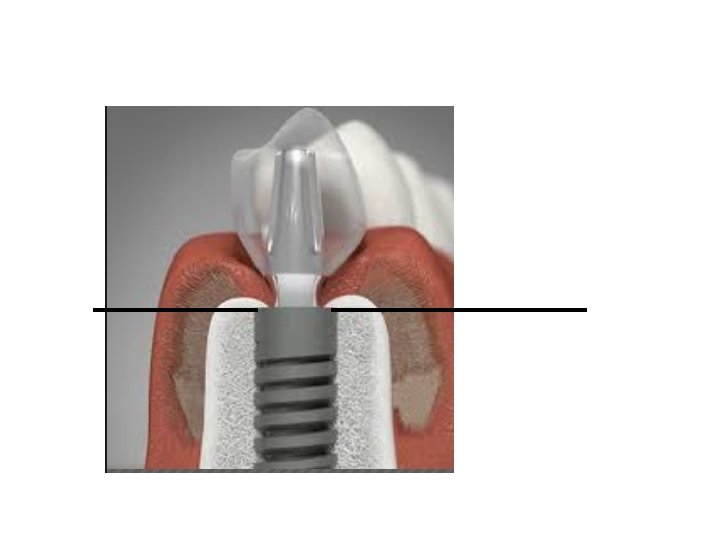
Hard tissue measurements • Periapical radiographs were taken with a paralleling technique after implant placement (baseline) and follow‐up appointments to measure the changes in the alveolar bone height surrounding the implant. • The implant shoulder was used as a reference level from which mesial and distal lines were drawn in an apical direction to the first point of contact between implant and bone
Soft tissue measurements • Intraoral photographs were taken before extraction and implant placement (baseline) and follow‐up visits to evaluate the soft tissue changes.
• Photographs were imported into software (Image J 1. 43 u, NIH, Bethesda, Maryland) for further measurements. • A line extending from the incisal edges of teeth adjacent to the implant was used as the reference point for measurements.
• From this line, perpendicular lines were drawn extending to the tip of the mesial papilla, distal papilla, and the mid‐buccal gingival margin. • The variations in the length of these lines over time were calculated to quantify the soft tissue changes
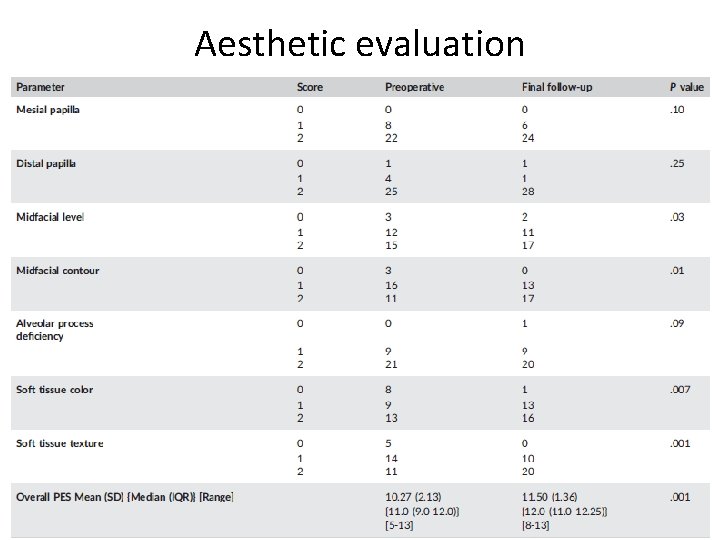
Aesthetic evaluation • PES is used to evaluate the peri‐implant soft tissue and includes seven variables: mesial papilla, distal papilla, soft tissue level, soft tissue contour, alveolar process deficiency, soft tissue color, and soft tissue texture. • Each parameter is assessed with a 0‐ 1‐ 2 score with 2 being the best and 0 being the worst score.
RESULTS • Bone levels around the implants showed an overall gain in bone height at the final follow up when compared to baseline. • Mesial bone levels showed a mean gain of 0. 18‐ 1. 38 mm while distal bone levels showed a mean gain of 0. 34‐ 1. 40 mm.
Soft tissue measurements • After a follow‐up period of 2‐ 5 years, the mesial and distal papillae showed a mean recession of 0. 05‐ 0. 64 mm and 0. 16‐ 0. 63 mm, respectively. • mid‐facial mucosal margin showed a mean recession of 0. 29‐ 0. 74 mm, with no value reaching statistical significance.
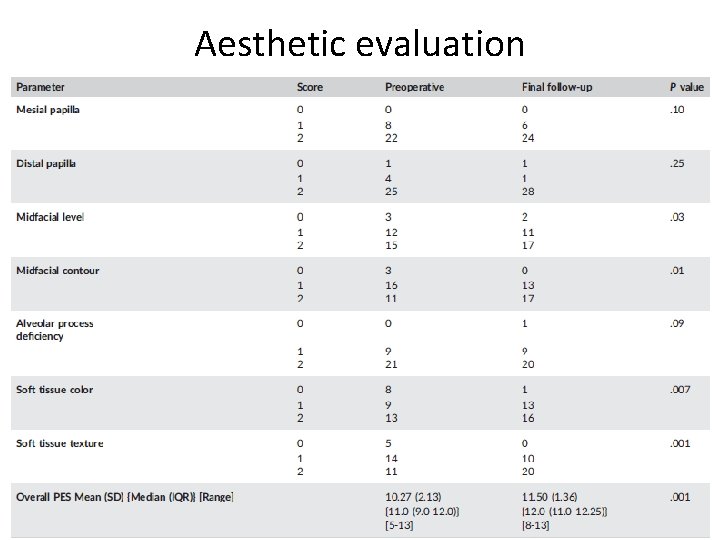
Aesthetic evaluation
DISCUSSION WHY THERE IS A BONE GAIN IN THIER STUDY? ? • The increase in bone levels could be attributed to the filling of bone in the extraction socket, and could further have been favored by the implant design. • The positive influence of grafting the peri‐implant gap and placing an immediate provisional restoration subsequent to flapless immediate implant placement on maintaining the ridge contour dimensions
• WHY THERE IS A SOFT TISSUE RECESSION? ? ? • interesting finding as sometimes gingival recession can be deliberately induced by the prosthodontist to create harmony with the soft tissue level on the contralateral tooth.
WHY THERE IS SIGNIFICANT IMPROVEMENT IN THE AESTHETIC INDEX? ? ? • The reasons for this observation are unclear and warrant further investigation. Interestingly, the mid‐facial gingival levels were maintained between the period of 1‐ 5 years in this study.
CONCLUSION • This prospective 2‐ 5 year follow‐up study showed that immediately placed and restored implants with a flapless technique in the maxillary anterior region yielded positive results in terms of osseointegration, hard, and soft tissue results, as well as aesthetic outcomes.
Correlation between pre‐operative buccal bone thickness and soft tissue changes around immediately placed and restored implants in the maxillary anterior region: A 2‐year prospective study Arora H, Ivanovski S. Clinical oral implants research. 2017 Oct 1; 28(10): 118894.
METHODS • Eighteen patients (3 males, 15 females) with an age range of 19– 57 years requiring the replacement of a single maxillary anterior tooth were included in this prospective study. • Buccal bone thickness was evaluated using pre‐ operative CBCT scans. Intra‐oral photographs were taken before implant placement (baseline) and at 1‐ and 2‐year follow‐up to assess soft tissue changes around the implants. • Aesthetic evaluation was carried out using the pink esthetic score (PES).
RESULTS • All implants remained osseointegrated during the follow‐up period of 2 years • mesial papilla, distal papilla, and mid‐facial gingiva showing a mean recession of 0. 06 from 0. 71 mm, 0. 25 from 0. 78 mm, and 0. 22 from 0. 83 mm, respectively. • Pink esthetic score values improved from a median value of 9 (IQR 8. 75– 10. 25) pre‐operatively to 11 (IQR 9. 75– 12) at the end of 2 years. • No significant correlation was found between buccal bone thickness (range 0. 45– 1. 24 mm) and soft tissue or aesthetic changes.
Immediate single‐tooth implants in the anterior maxilla: a 1‐year case cohort study on hard and soft tissue response. De Rouck T, Collys K, Cosyn J. Journal of Clinical Periodontology. 2008 Jul 1; 35(7): 649 -57.
MATERIALS AND METHODS • Patients with a missing maxillary tooth (15‐ 25) were randomly assigned to IL or DL. • The protocol included implant installation in healed sites, immediate loading, delayed loading, temporary screw‐retained restoration, and replacement with a permanent single implant crown. • Outcome measures were implant survival, marginal bone level, soft tissue changes, papillae index, pink, and white esthetic score (PES and WES), patient judged aesthetics, and oral health impact profile
RESULTS • Statistically significant lower papilla index scores were found in the IL group at temporary crown and definitive crown placement. An overall statistically significant improvement after 12 months for PES, WES and OHIP‐ 14 was found.
CONCLUSION • This prospective randomized study showed that single implants in the maxilla can present satisfactory results with respect to either immediate loading or delayed loading after 12 months.
Clinical and radiographic outcome following immediate loading and delayed loading of single‐tooth implants: Randomized clinical trial. Gjelvold B, Kisch J, Chrcanovic BR, Albrektsson T, Wennerberg A. Clinical Implant Dentistry and Related Research. 2017 Jun 1; 19(3): 549 -58.
MATERIALS AND METHODS • Thirty consecutive patients were treated for single‐tooth replacement in the aesthetic zone by means of immediate implant placement and provisionalization. • Clinical and radiographic evaluation was completed at 1, 3, 6 and 12 months to assess implant survival and complications, hard and soft tissue parameters and patient’s aesthetic satisfaction.
RESULTS • One implant had failed at 1 month of follow‐ up, resulting in an implant survival rate of 97%. • Radiographic examination yielded 0. 98 mm mesial, respectively, 0. 78 mm distal bone loss. • Midfacial soft tissue recession and mesial/distal papilla shrinkage were 0. 53, 0. 41 and 0. 31 mm, respectively. Patient’s aesthetic satisfaction was 93%.
CONCLUSION • maxillary anterior region yielded positive results in terms of osseointegration, hard, and soft tissue results, as well as aesthetic outcomes