Imaging pattern of respiratory disease Liu Lin Xiang


























- Slides: 122
Imaging pattern of respiratory disease Liu Lin Xiang 刘林祥 Radiology school 6222136, lxliu@tsmc. edu. cn 2022/1/4
Imaging pattern ¶ Obstructive change of bronchiel ¶emphysema W Atelectasis · Pleural abnormalities Ø Pleural effusion Ø pneumothorax Ø Pleural thickening 2022/1/4 Lung disease ØConsolidation ØFibrosis ØCalcification ØNodule and mass ØCavity and ØInterstitial changes

Chronic diffuse obstructive emphysema 2022/1/4
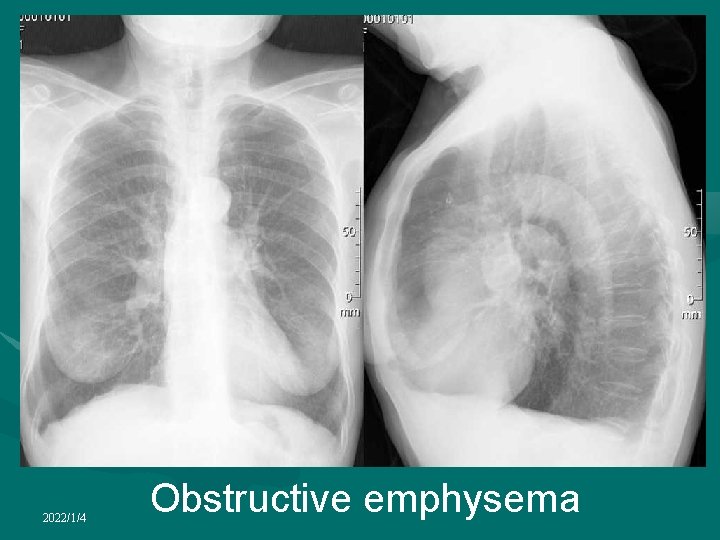
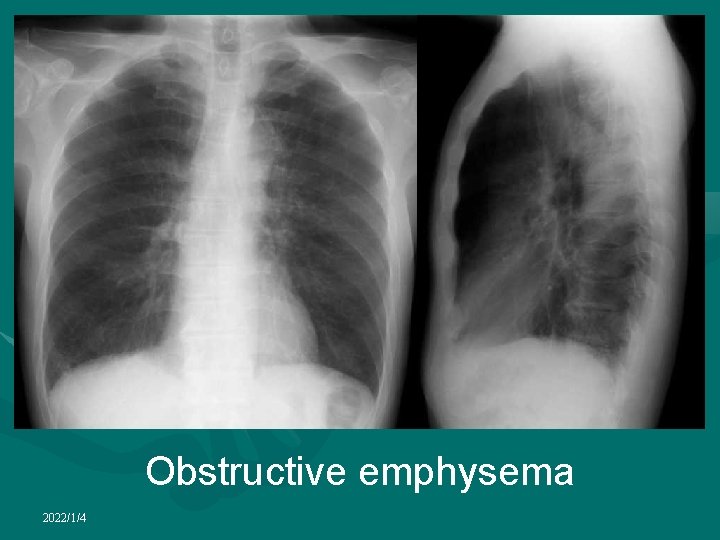
Chronic diffuse obstructive emphysema 1. Increased translucency of both lungs 2. Lung marking scattered, thined 3. normal domed diagphragms are flattened 4. Retrosternal space is increased on the lateral film 5. Heart tends to be elongated, narrow and central in position 2022/1/4
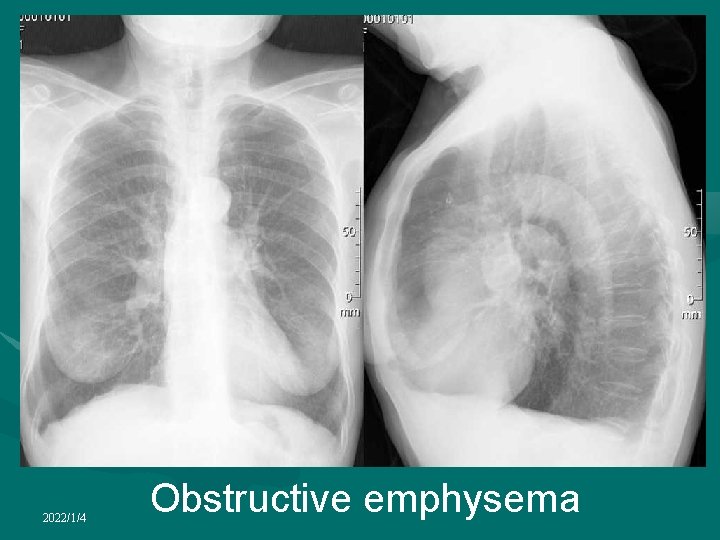
2022/1/4 Obstructive emphysema

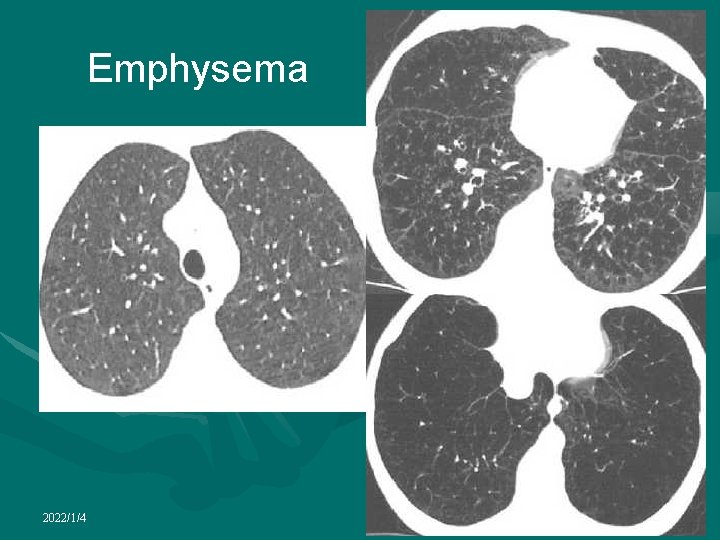
CT findings of emphysema • Centrilobular emphysema • Panlobular emphysema • Paraseptal emphysema 2022/1/4
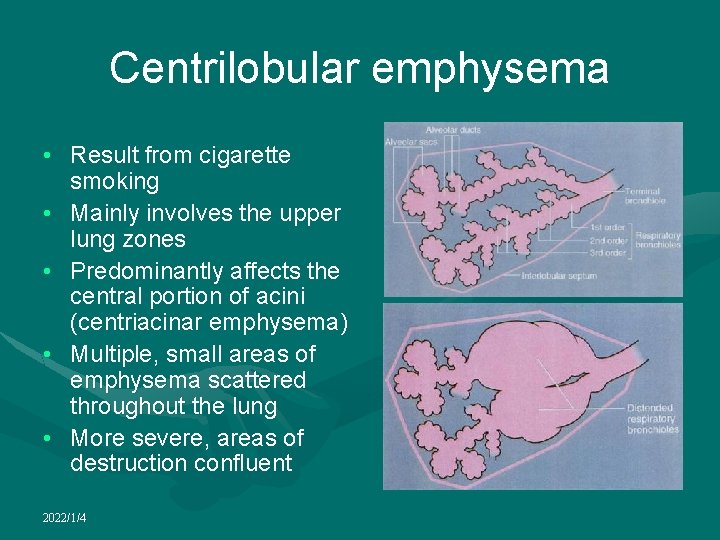
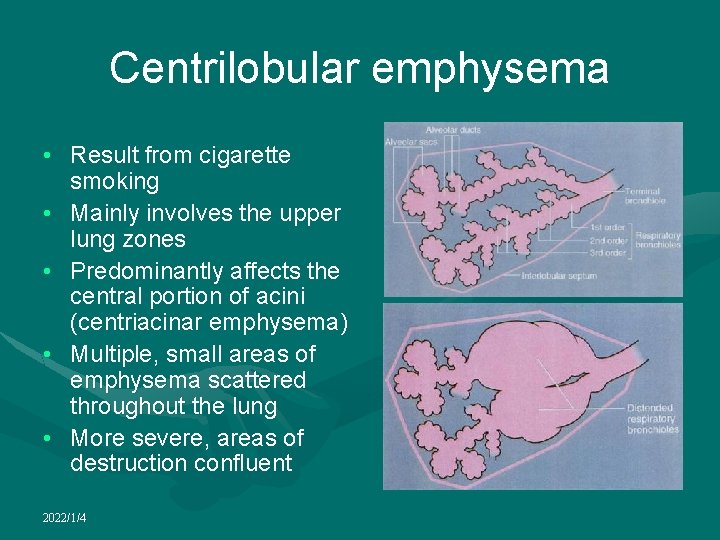
Centrilobular emphysema • Result from cigarette smoking • Mainly involves the upper lung zones • Predominantly affects the central portion of acini (centriacinar emphysema) • Multiple, small areas of emphysema scattered throughout the lung • More severe, areas of destruction confluent 2022/1/4
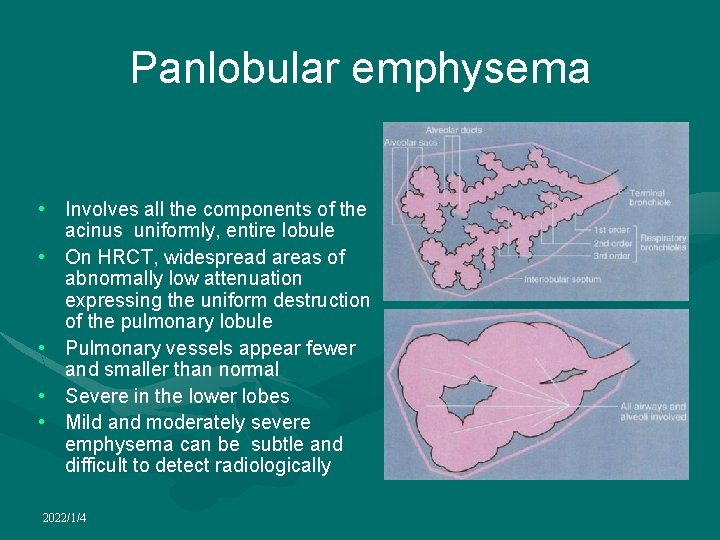
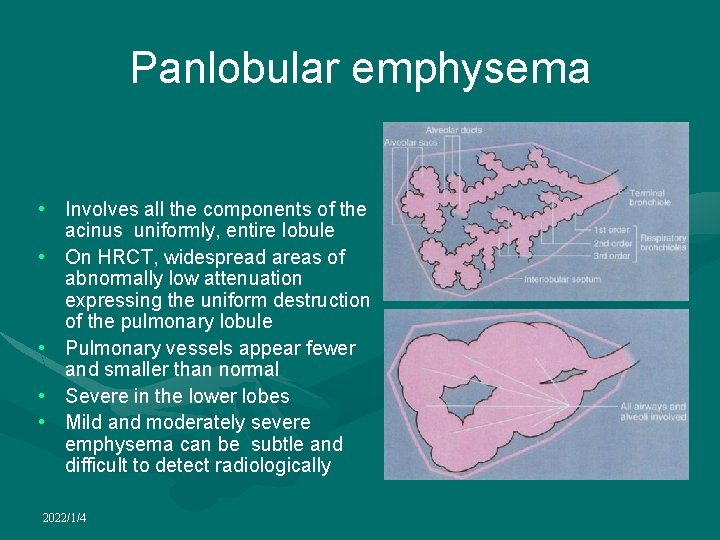
Panlobular emphysema • Involves all the components of the acinus uniformly, entire lobule • On HRCT, widespread areas of abnormally low attenuation expressing the uniform destruction of the pulmonary lobule • Pulmonary vessels appear fewer and smaller than normal • Severe in the lower lobes • Mild and moderately severe emphysema can be subtle and difficult to detect radiologically 2022/1/4
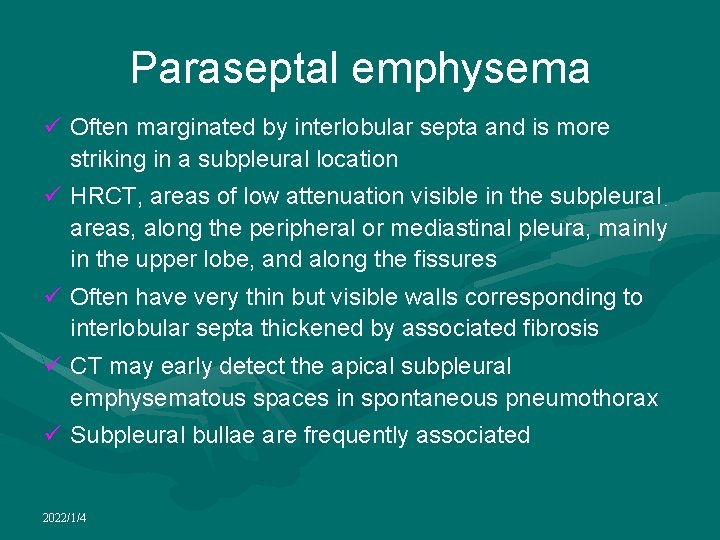
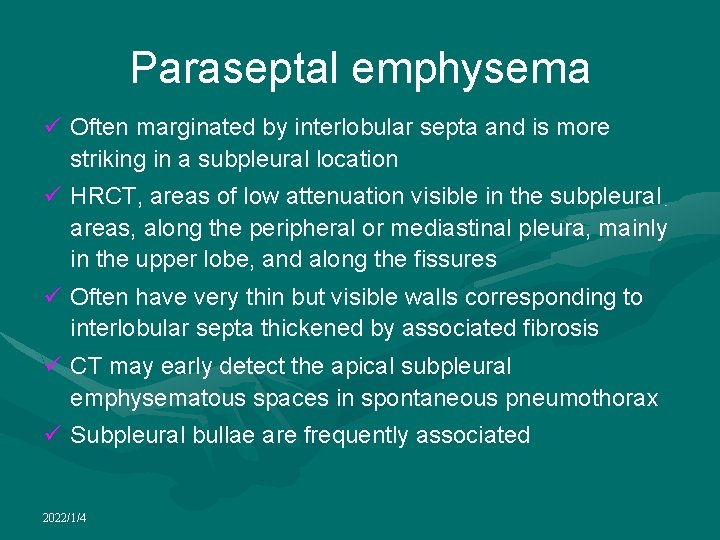
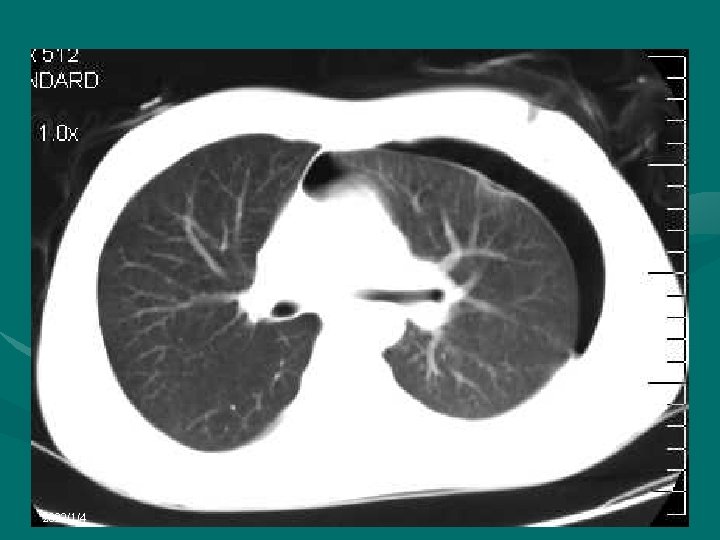
Paraseptal emphysema ü Often marginated by interlobular septa and is more striking in a subpleural location ü HRCT, areas of low attenuation visible in the subpleural areas, along the peripheral or mediastinal pleura, mainly in the upper lobe, and along the fissures ü Often have very thin but visible walls corresponding to interlobular septa thickened by associated fibrosis ü CT may early detect the apical subpleural emphysematous spaces in spontaneous pneumothorax ü Subpleural bullae are frequently associated 2022/1/4
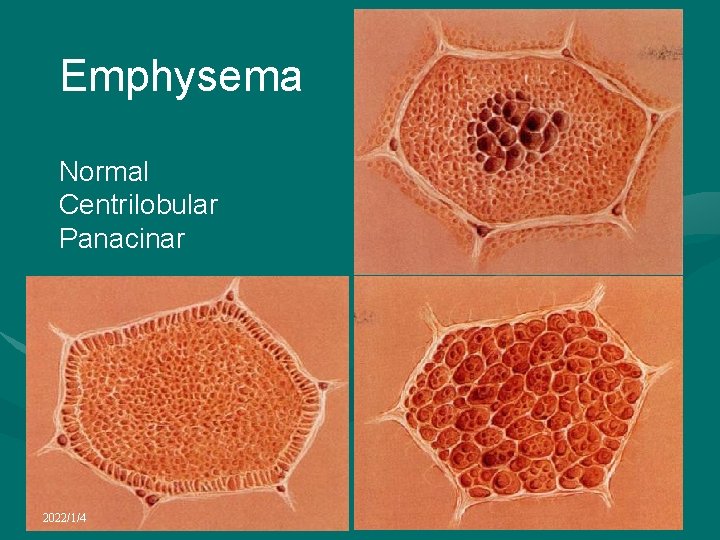
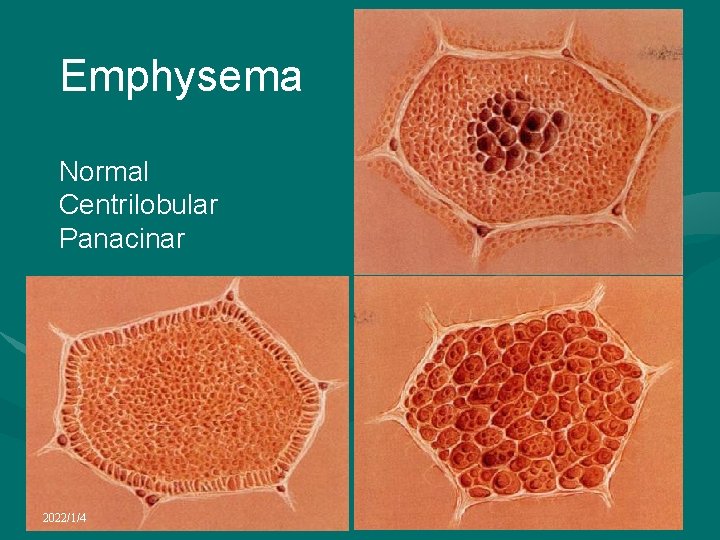
Emphysema Normal Centrilobular Panacinar 2022/1/4
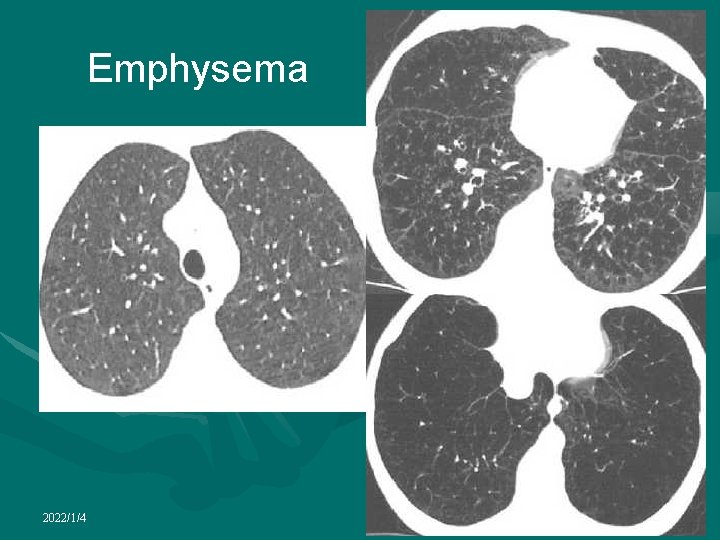
Emphysema 2022/1/4
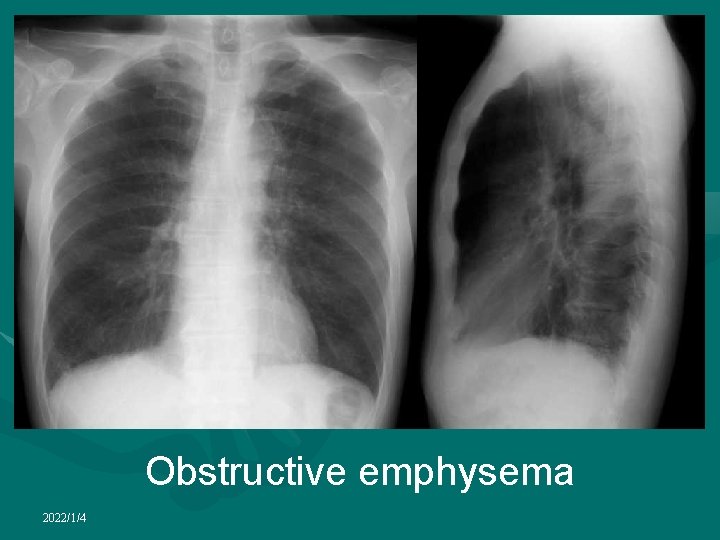
Obstructive emphysema 2022/1/4

Obstructive emphysema 2022/1/4
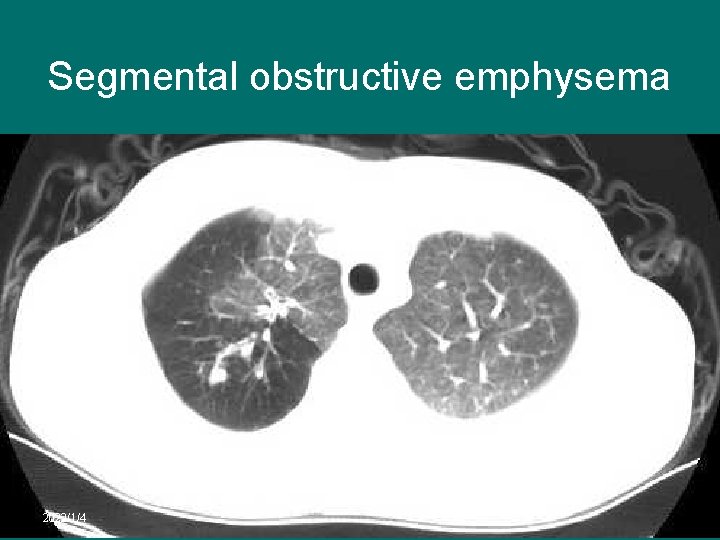
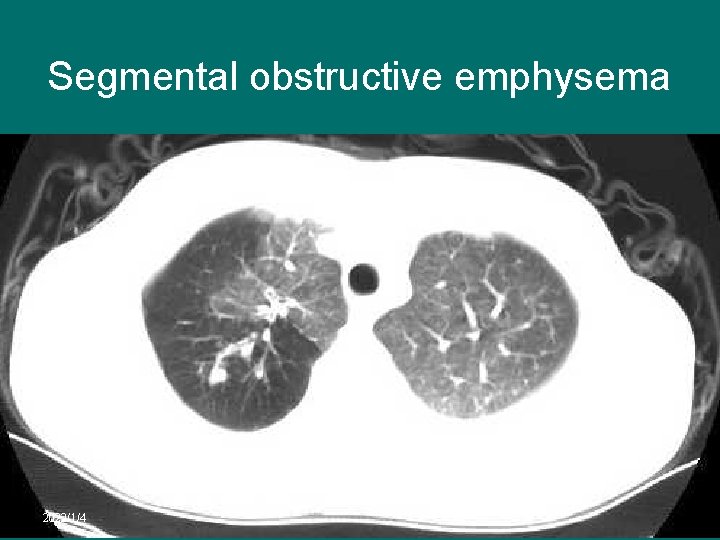
Segmental obstructive emphysema 2022/1/4
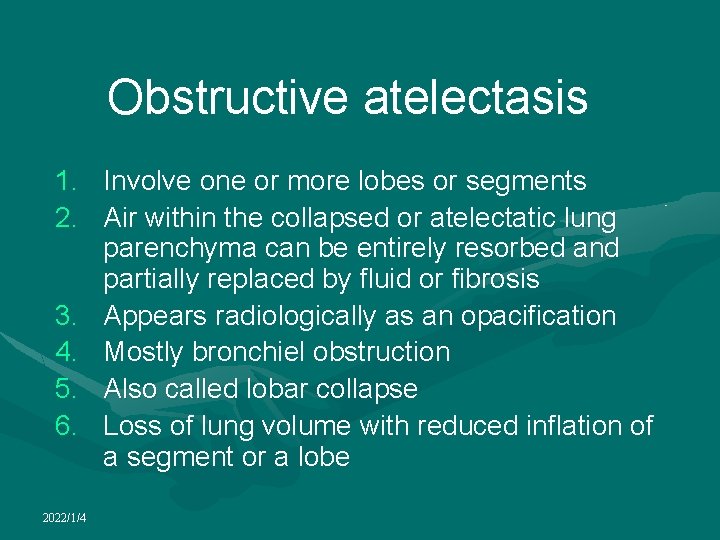
Obstructive atelectasis 1. Involve one or more lobes or segments 2. Air within the collapsed or atelectatic lung parenchyma can be entirely resorbed and partially replaced by fluid or fibrosis 3. Appears radiologically as an opacification 4. Mostly bronchiel obstruction 5. Also called lobar collapse 6. Loss of lung volume with reduced inflation of a segment or a lobe 2022/1/4
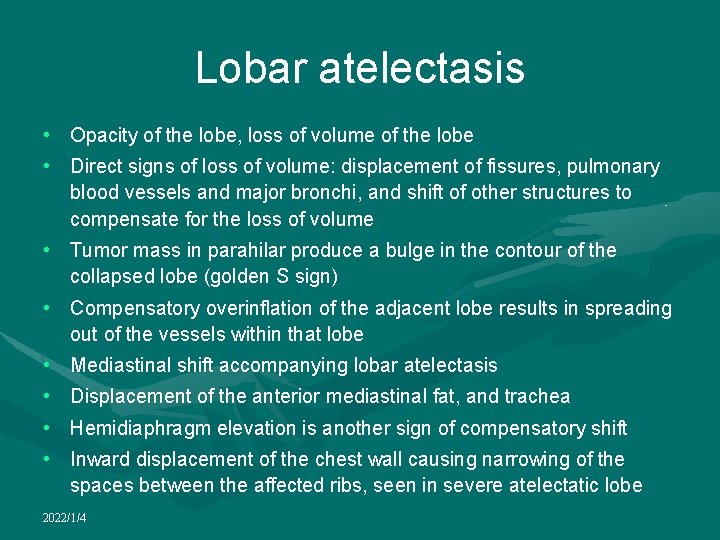
Lobar atelectasis • Opacity of the lobe, loss of volume of the lobe • Direct signs of loss of volume: displacement of fissures, pulmonary blood vessels and major bronchi, and shift of other structures to compensate for the loss of volume • Tumor mass in parahilar produce a bulge in the contour of the collapsed lobe (golden S sign) • Compensatory overinflation of the adjacent lobe results in spreading out of the vessels within that lobe • Mediastinal shift accompanying lobar atelectasis • Displacement of the anterior mediastinal fat, and trachea • Hemidiaphragm elevation is another sign of compensatory shift • Inward displacement of the chest wall causing narrowing of the spaces between the affected ribs, seen in severe atelectatic lobe 2022/1/4
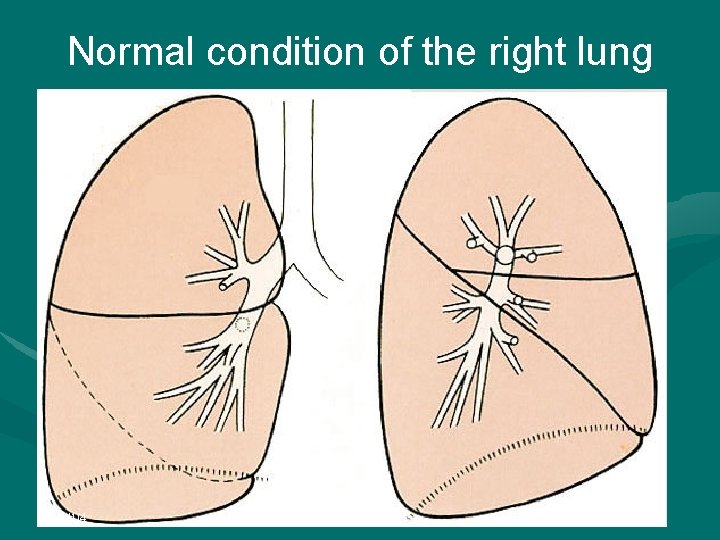
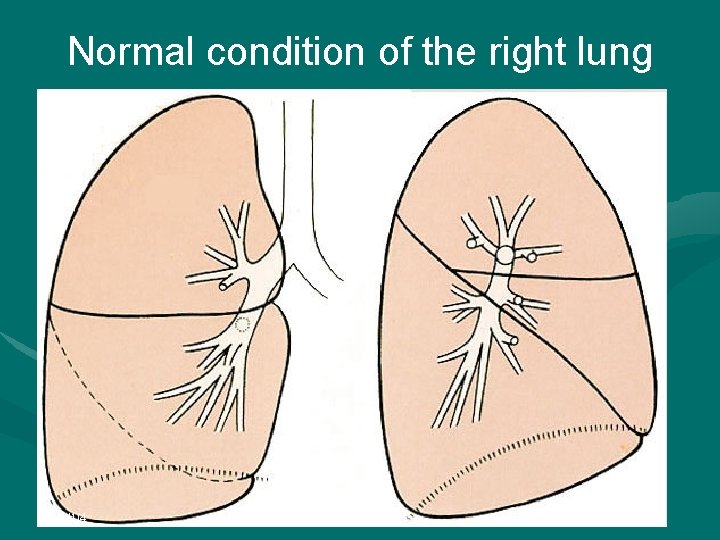
Normal condition of the right lung 2022/1/4
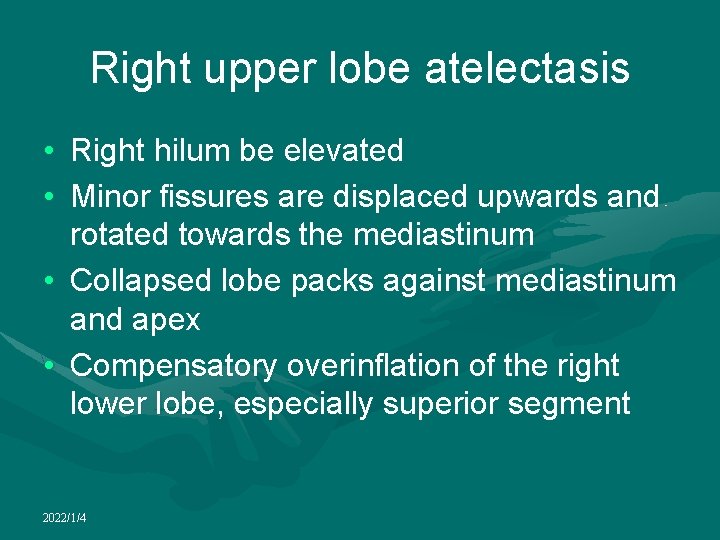
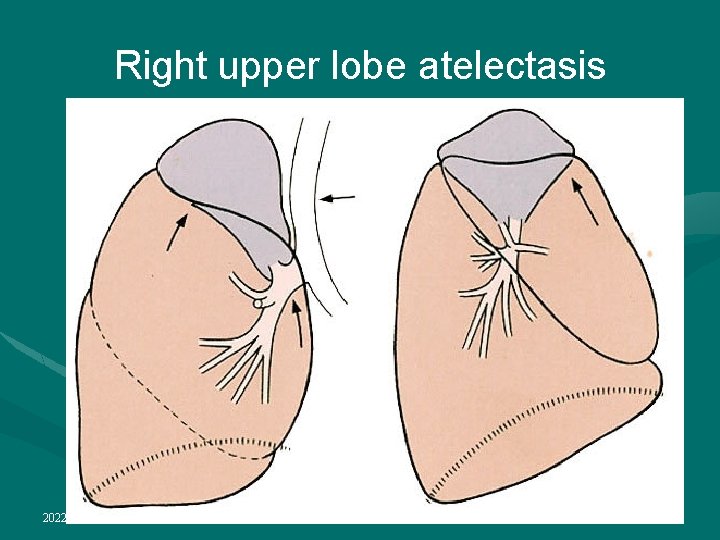
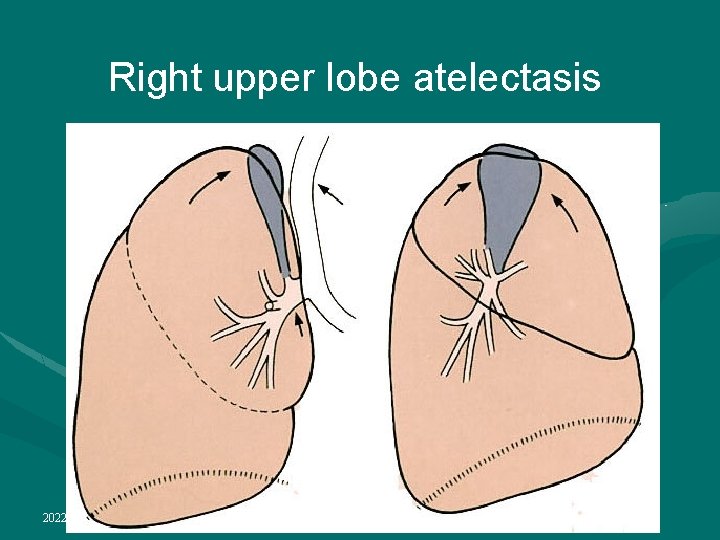
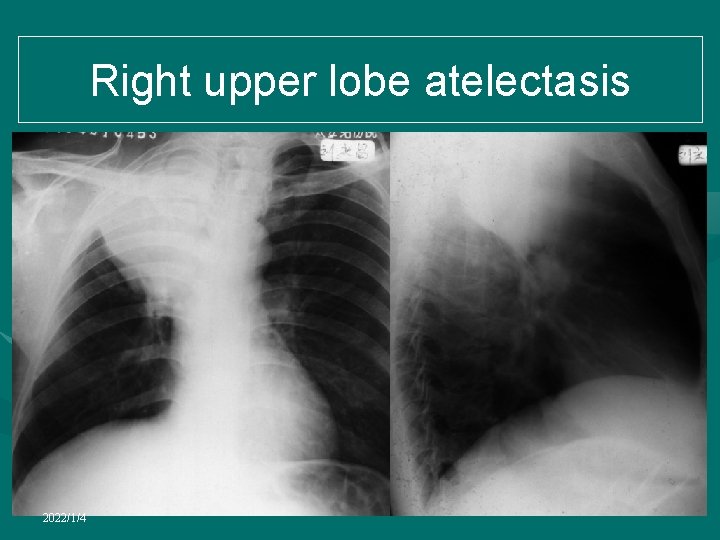
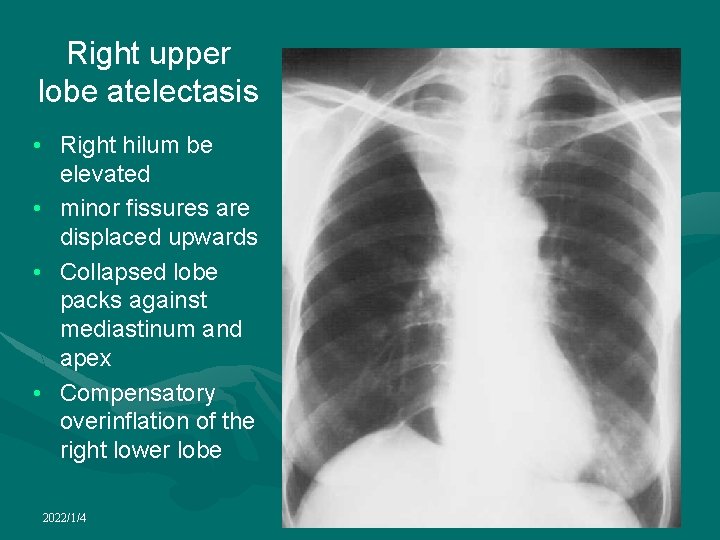
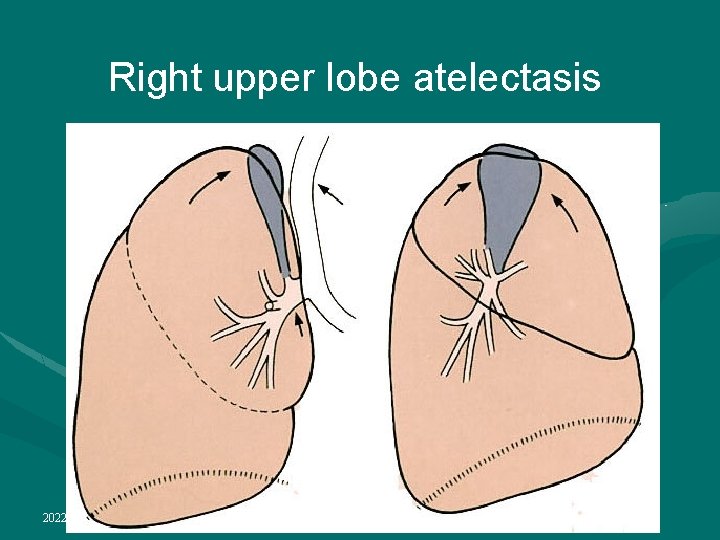
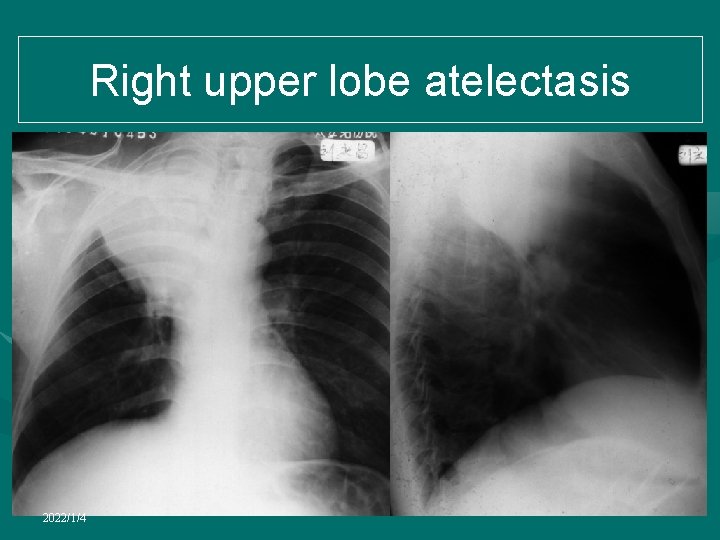
Right upper lobe atelectasis • Right hilum be elevated • Minor fissures are displaced upwards and rotated towards the mediastinum • Collapsed lobe packs against mediastinum and apex • Compensatory overinflation of the right lower lobe, especially superior segment 2022/1/4
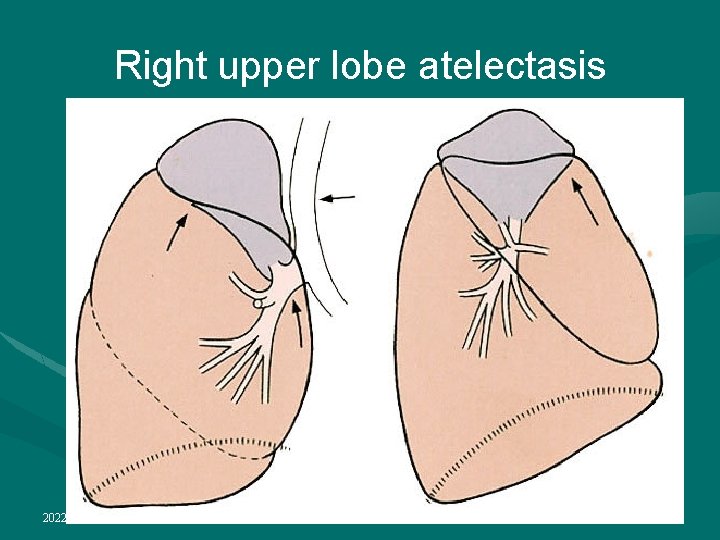
Right upper lobe atelectasis 2022/1/4
Right upper lobe atelectasis 2022/1/4
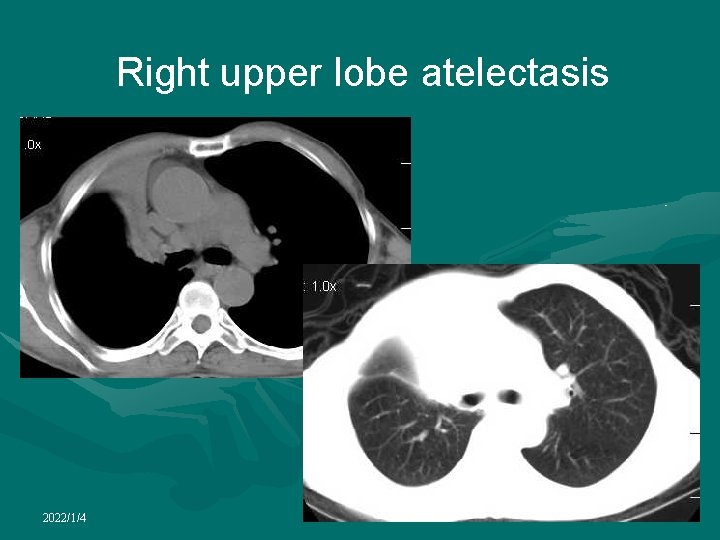
Right upper lobe atelectasis 2022/1/4
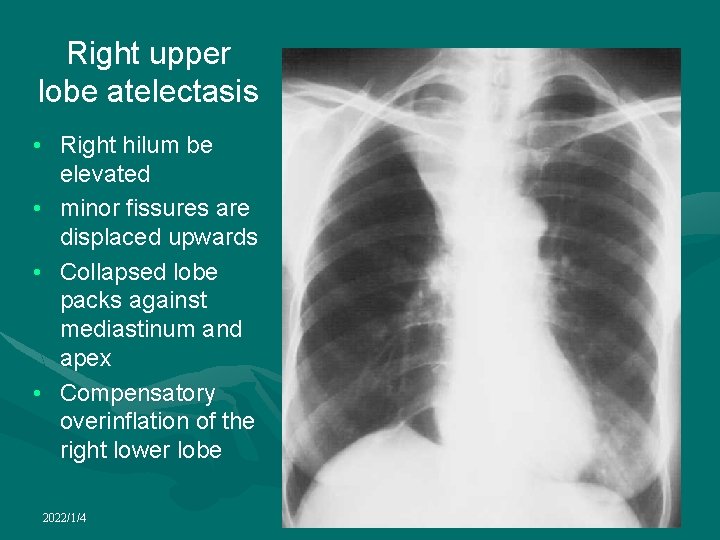
Right upper lobe atelectasis • Right hilum be elevated • minor fissures are displaced upwards • Collapsed lobe packs against mediastinum and apex • Compensatory overinflation of the right lower lobe 2022/1/4
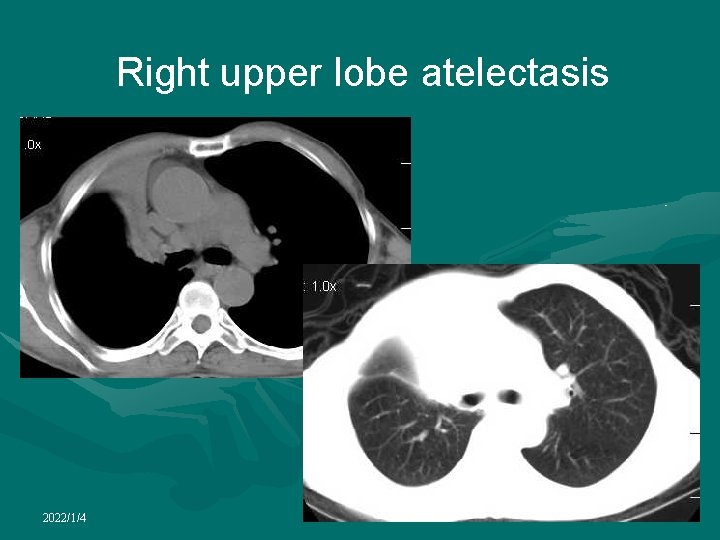
Right upper lobe atelectasis 2022/1/4
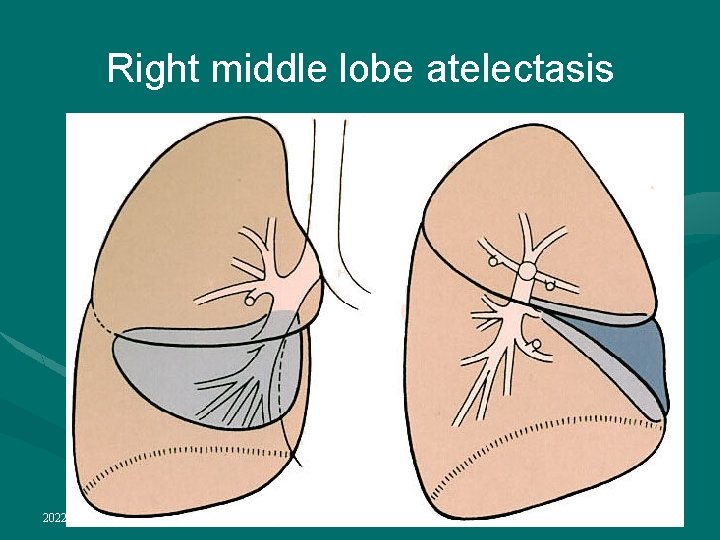
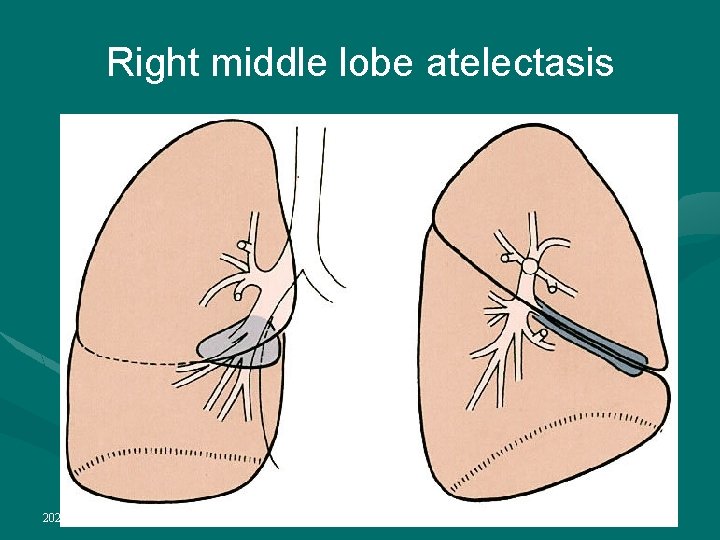
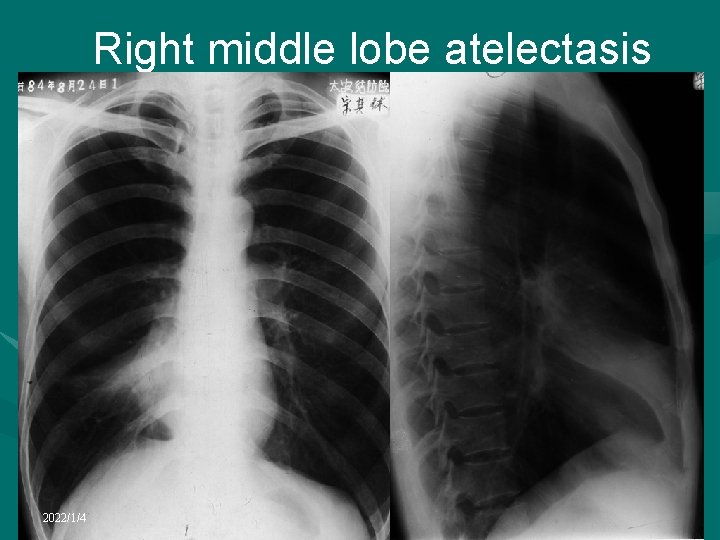
Right middle lobe atelectasis • The collapsed lobe is easily and reliably recognized on the lateral chest radiograph • The major and minor fissures move towards one another and the collapsed lobe resembles a curved, elongated wedge • The right hilum is not displaced • The right hemidiaphragm and mediastinum are in a normal position 2022/1/4
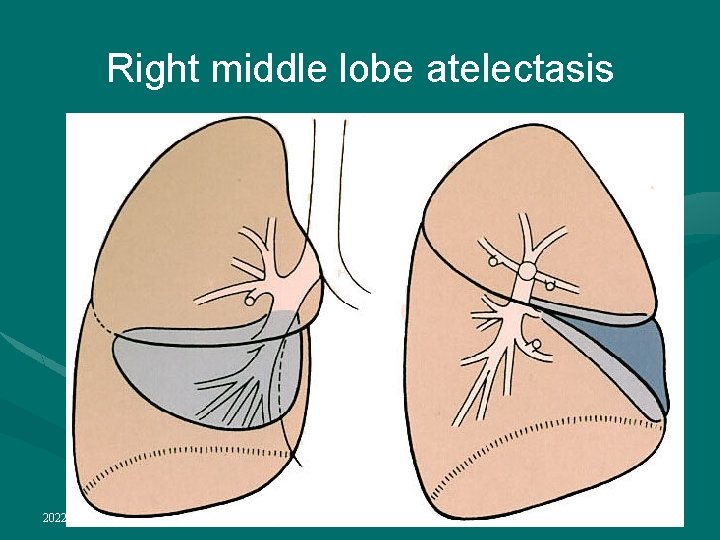
Right middle lobe atelectasis 2022/1/4
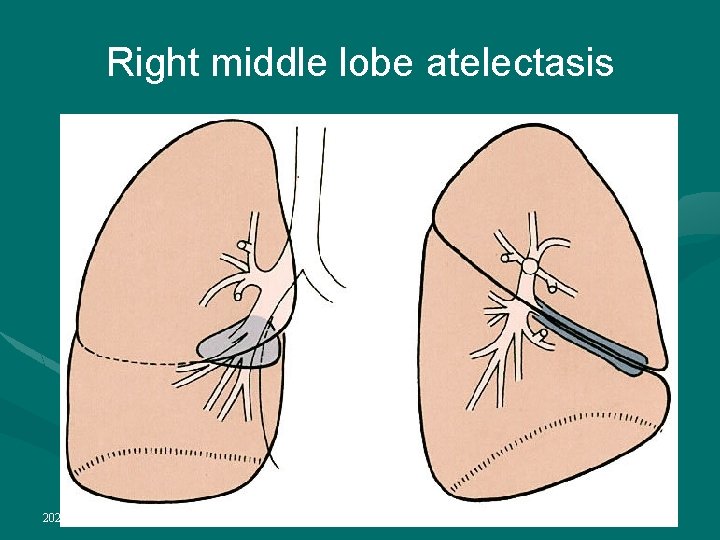
Right middle lobe atelectasis 2022/1/4
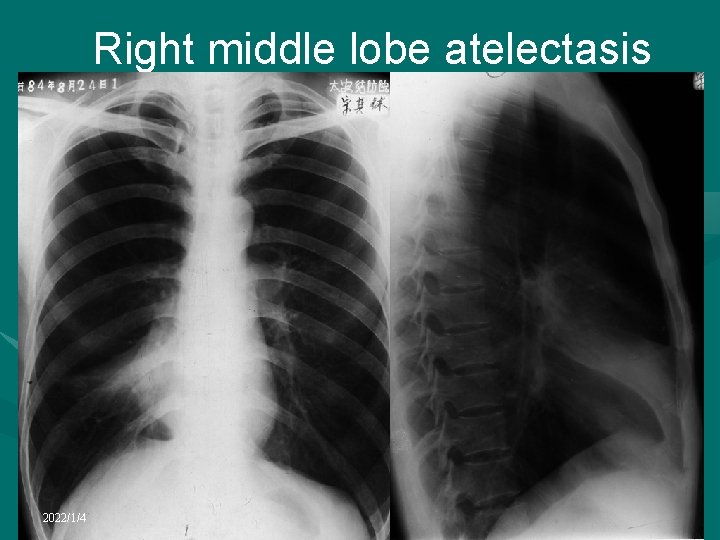
Right middle lobe atelectasis 2022/1/4
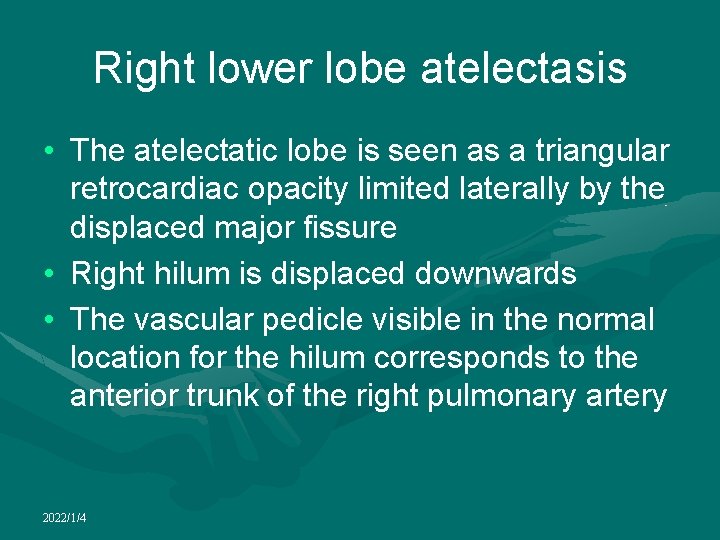
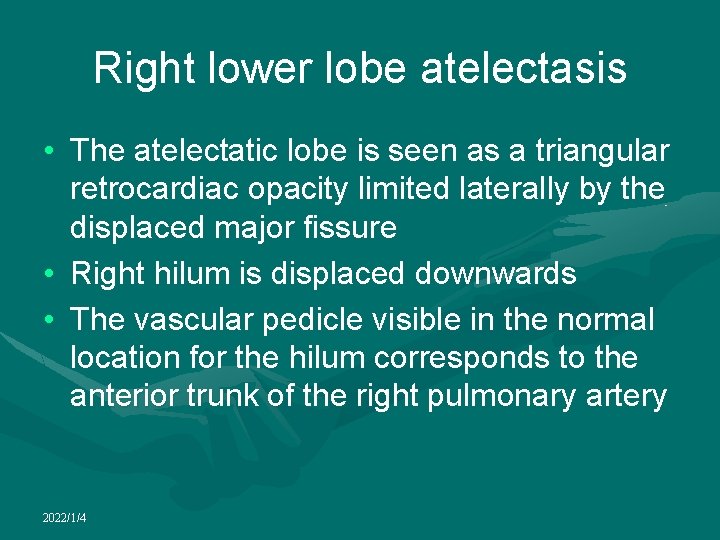
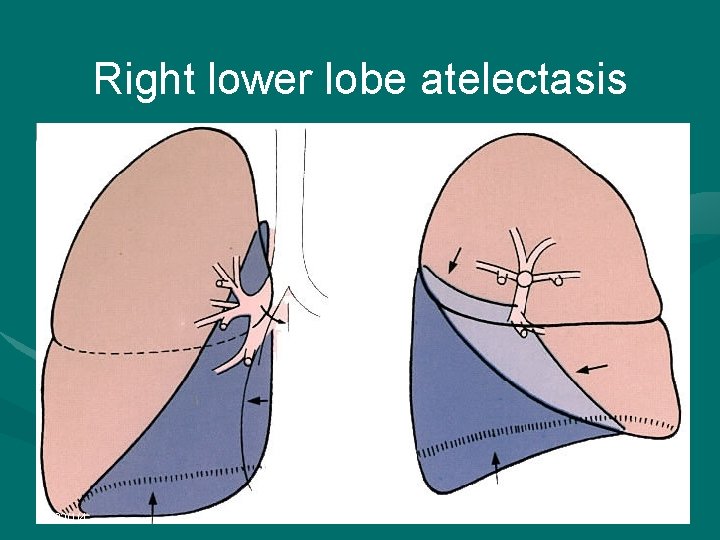
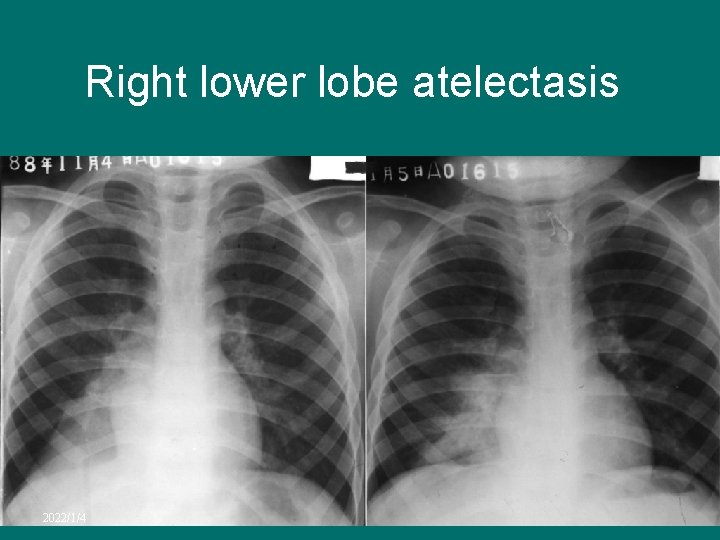
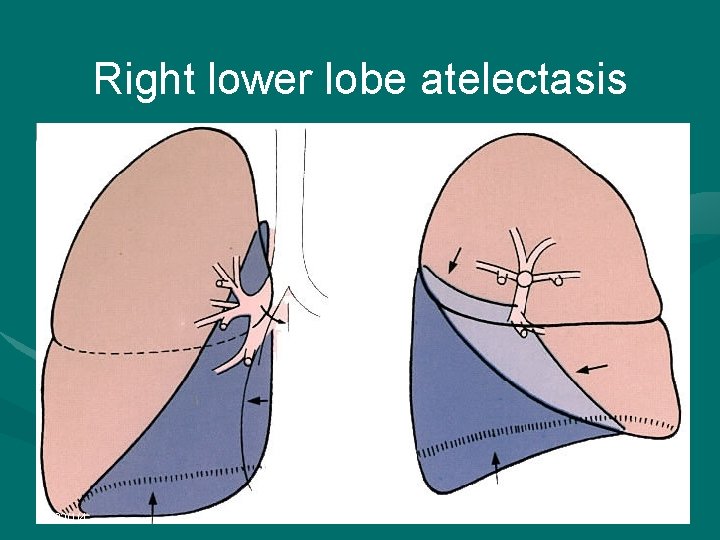
Right lower lobe atelectasis • The atelectatic lobe is seen as a triangular retrocardiac opacity limited laterally by the displaced major fissure • Right hilum is displaced downwards • The vascular pedicle visible in the normal location for the hilum corresponds to the anterior trunk of the right pulmonary artery 2022/1/4
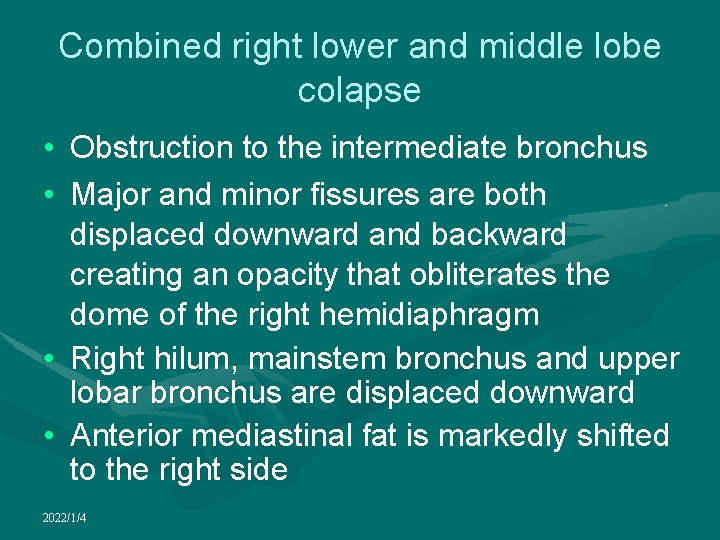
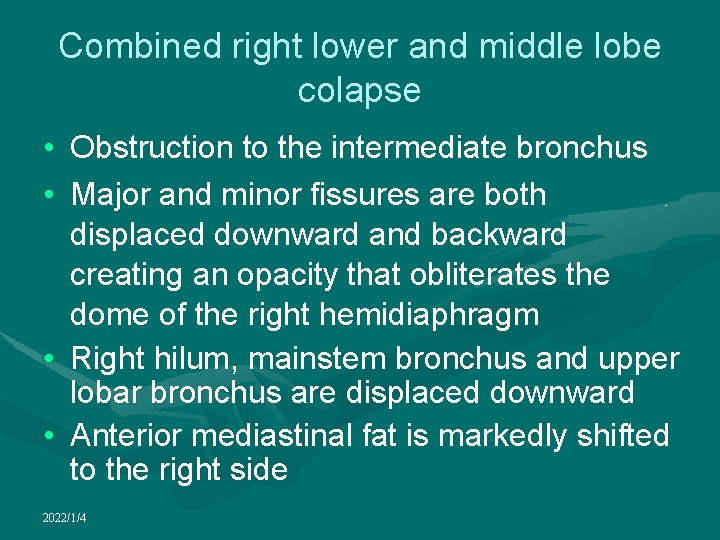
Combined right lower and middle lobe colapse • Obstruction to the intermediate bronchus • Major and minor fissures are both displaced downward and backward creating an opacity that obliterates the dome of the right hemidiaphragm • Right hilum, mainstem bronchus and upper lobar bronchus are displaced downward • Anterior mediastinal fat is markedly shifted to the right side 2022/1/4
Right lower lobe atelectasis 2022/1/4
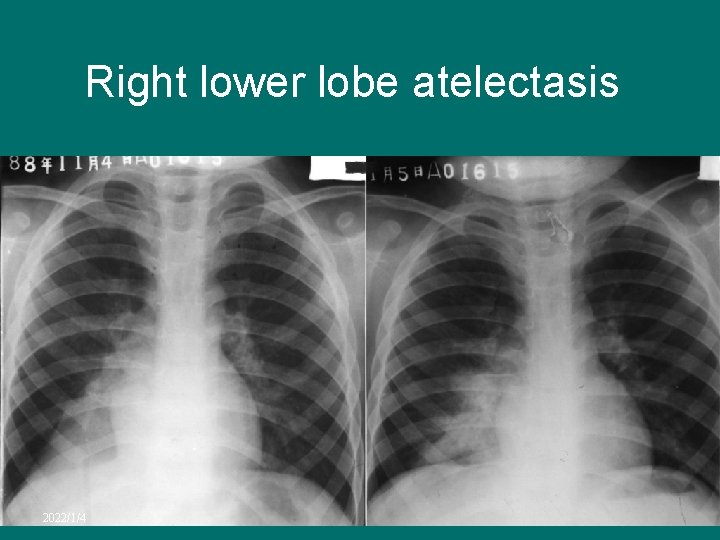
Right lower lobe atelectasis 2022/1/4

Right lower lobe atelectasis 2022/1/4

Right lower lobe atelectasis 2022/1/4
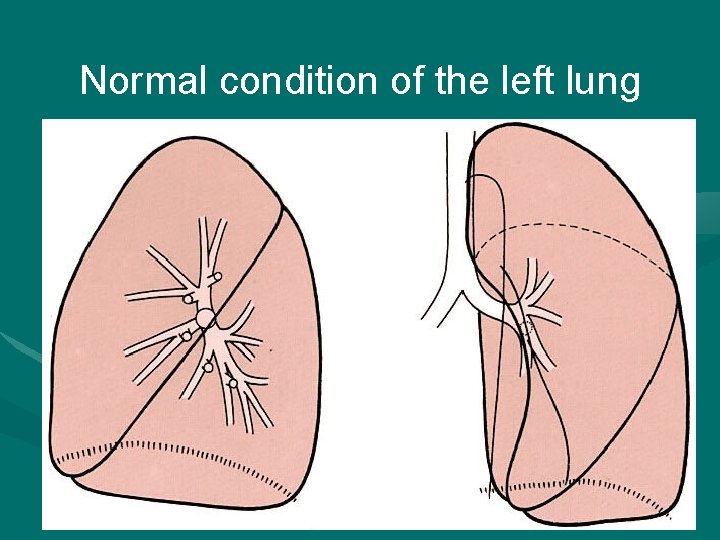
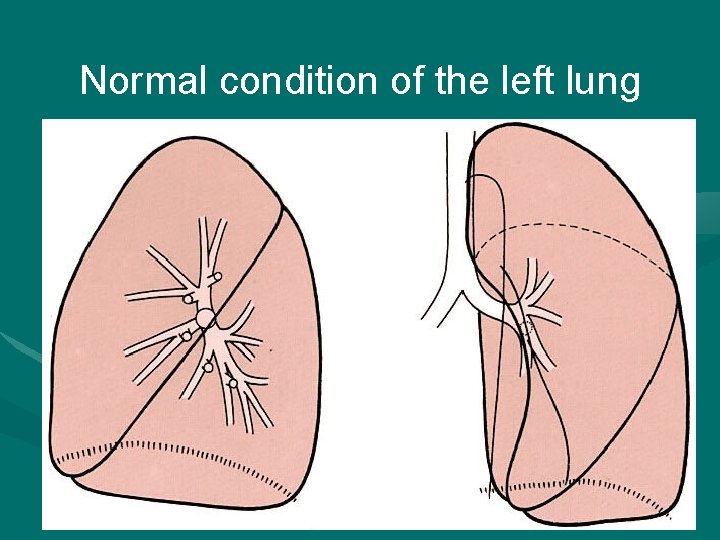
Normal condition of the left lung 2022/1/4
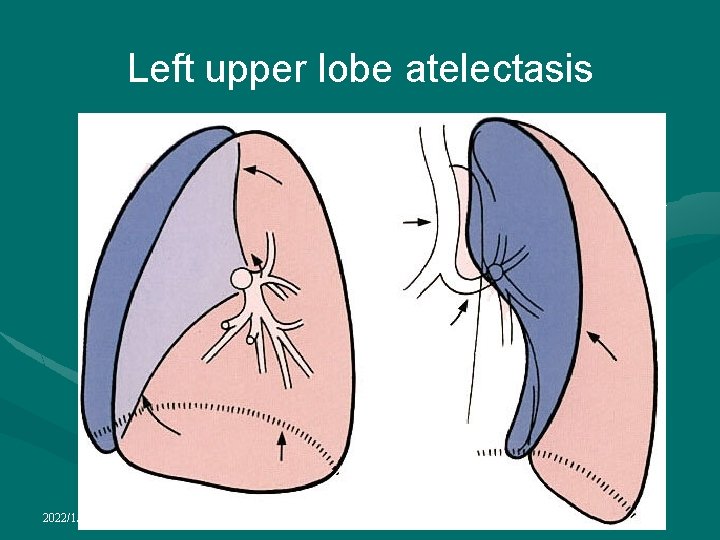
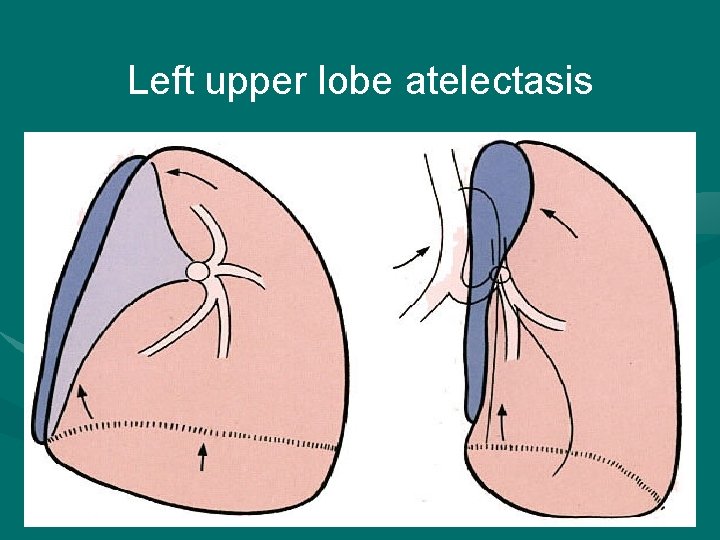
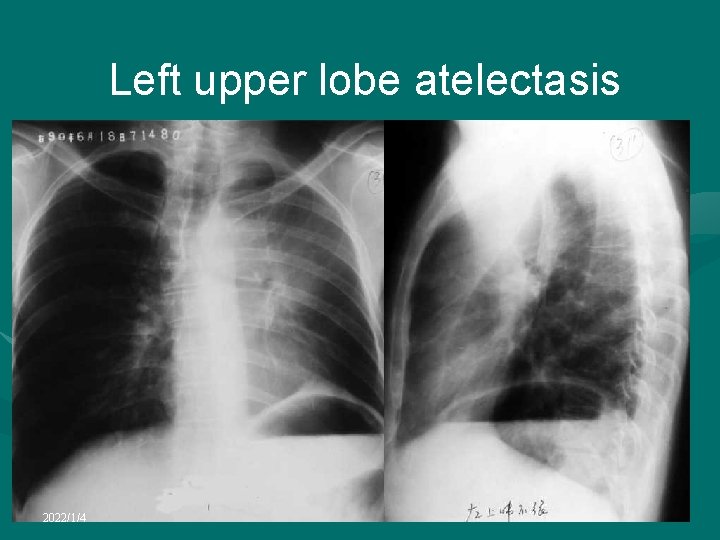
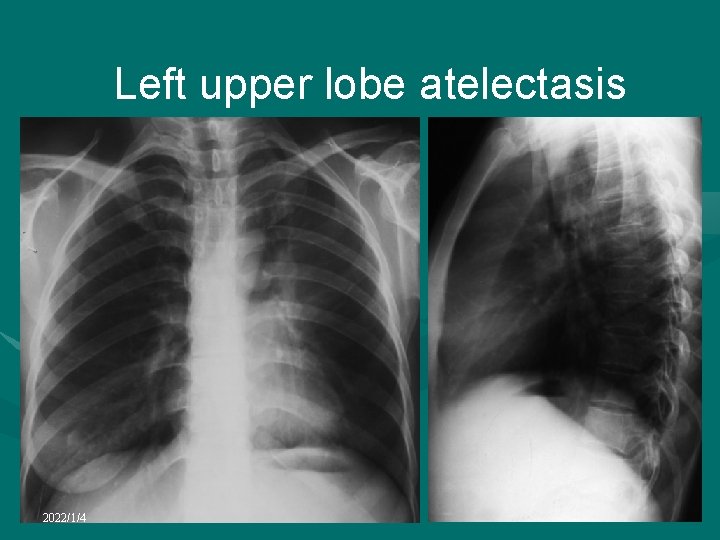
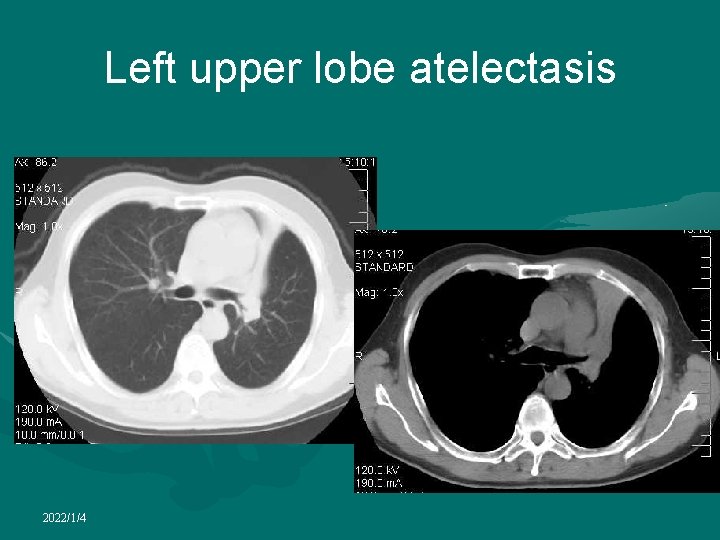
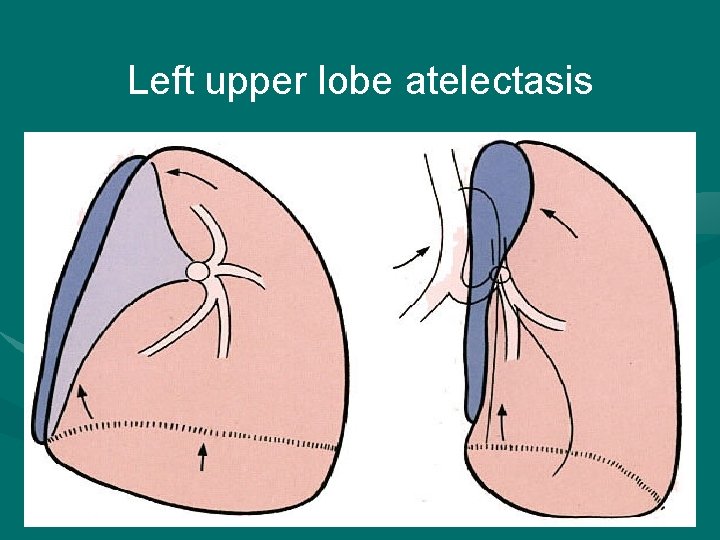
Left upper lobe atelectasis • Hilum is displaced upwards and the major fissure forwards • Lobe retains much of its original contact with the anterior chest wall • Displacement of the anterior mediastinum fat and displacement of the trachea towards the left are commonly present • Left hemidiaphragm is moderately elevated 2022/1/4
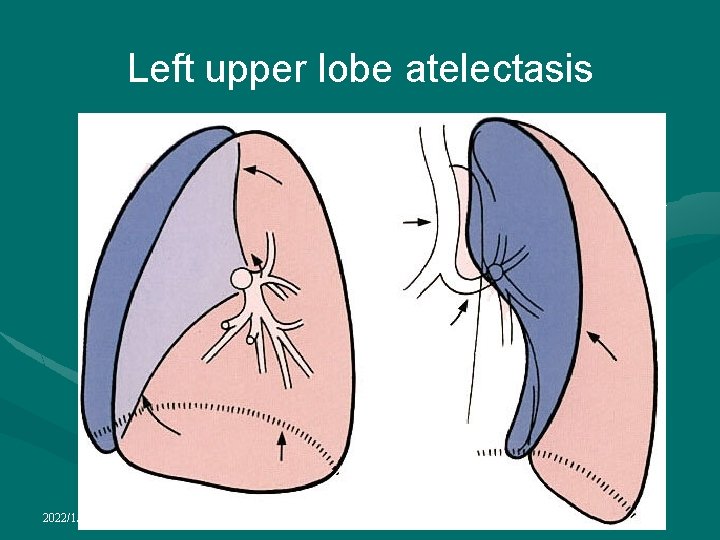
Left upper lobe atelectasis 2022/1/4
Left upper lobe atelectasis 2022/1/4
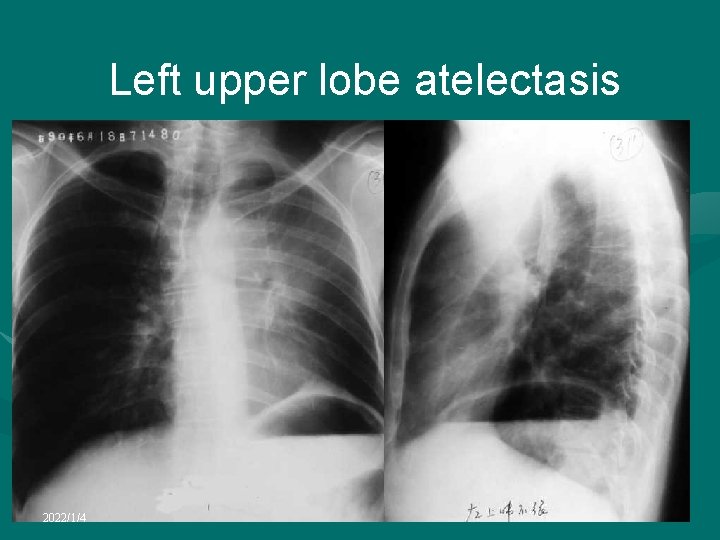
Left upper lobe atelectasis 2022/1/4
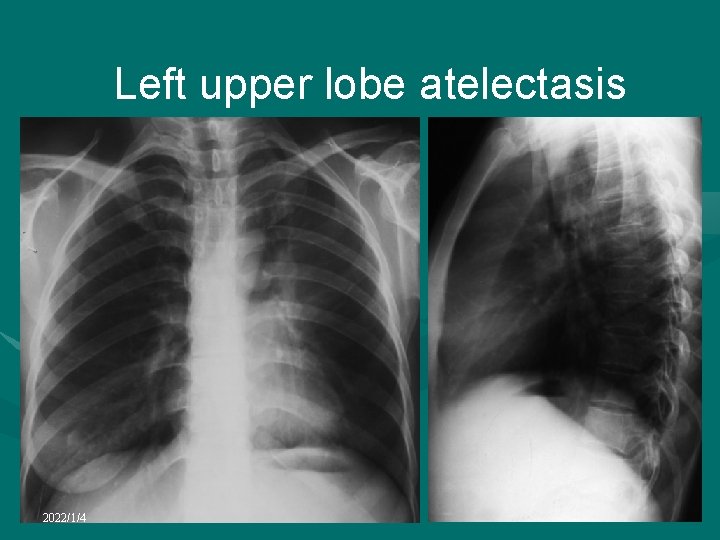
Left upper lobe atelectasis 2022/1/4
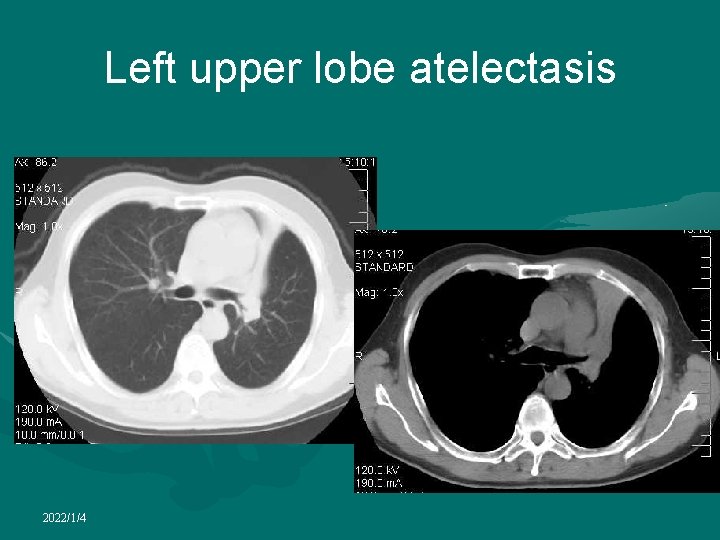
Left upper lobe atelectasis 2022/1/4
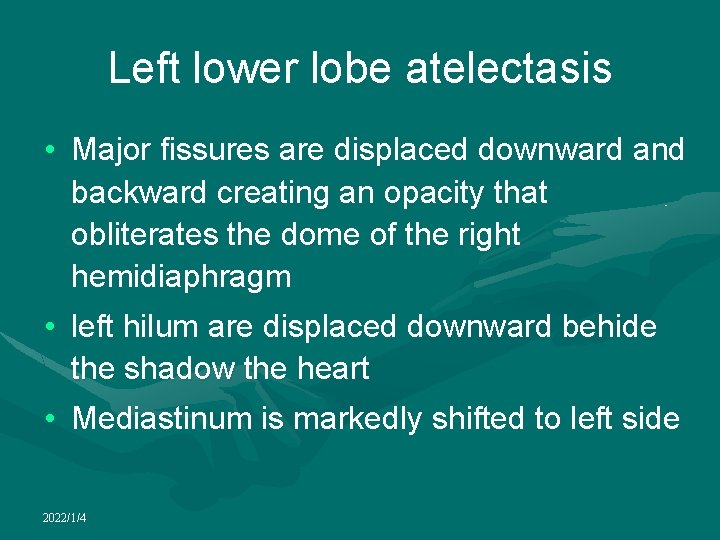
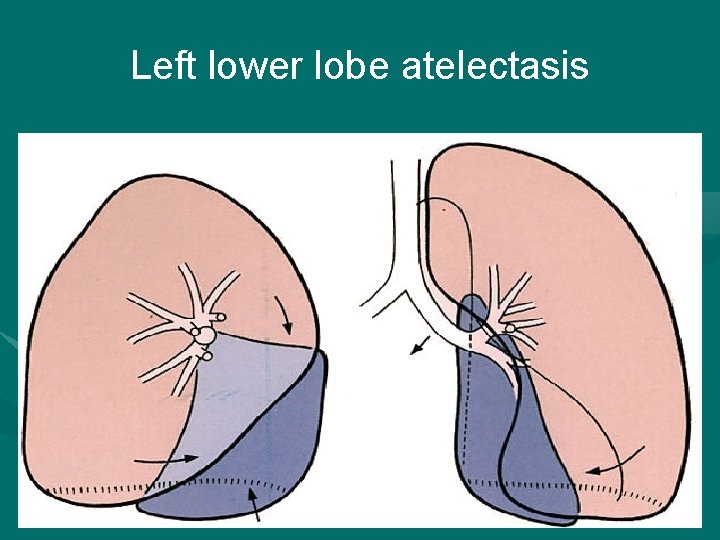
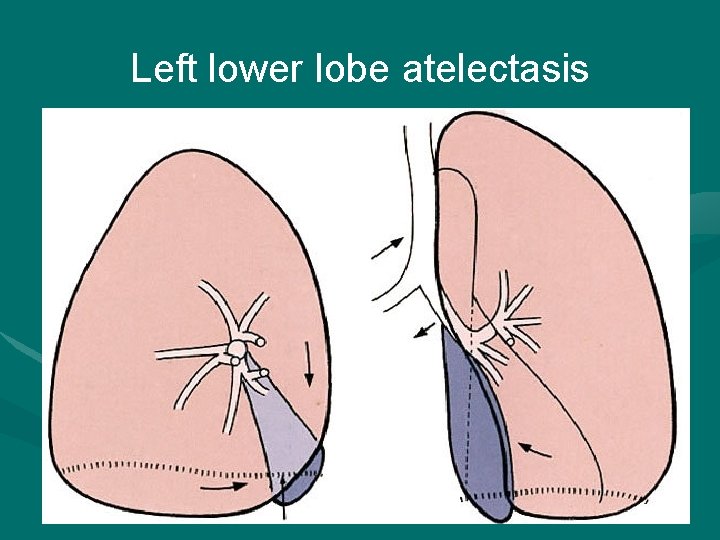
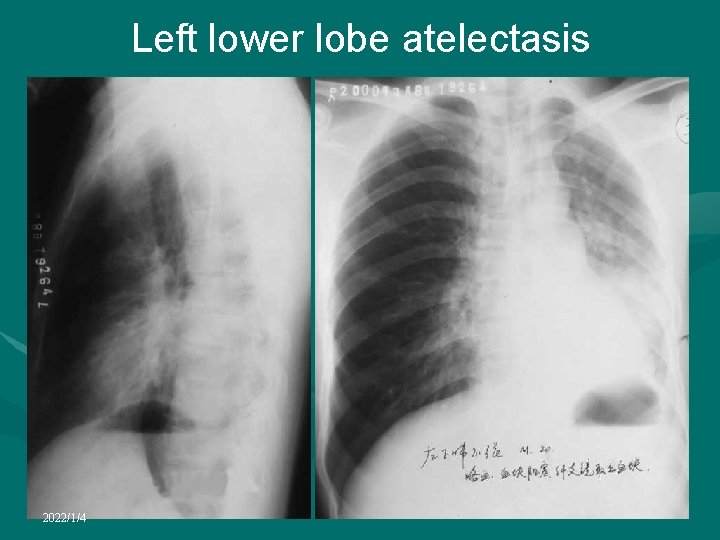
Left lower lobe atelectasis • Major fissures are displaced downward and backward creating an opacity that obliterates the dome of the right hemidiaphragm • left hilum are displaced downward behide the shadow the heart • Mediastinum is markedly shifted to left side 2022/1/4
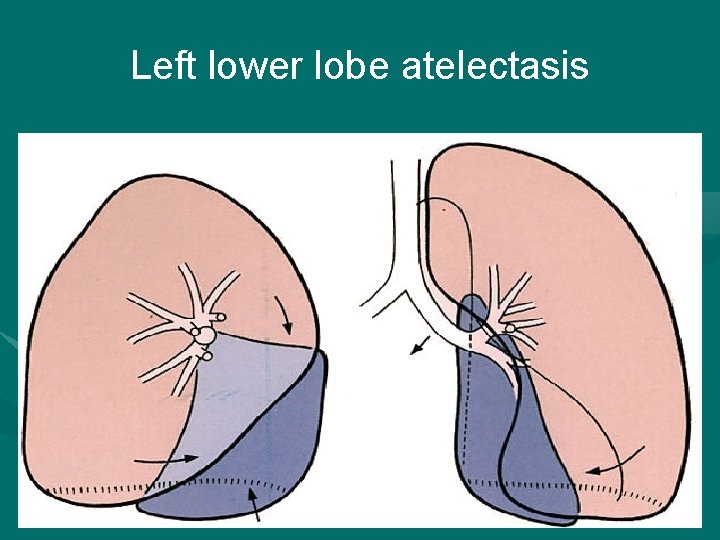
Left lower lobe atelectasis 2022/1/4
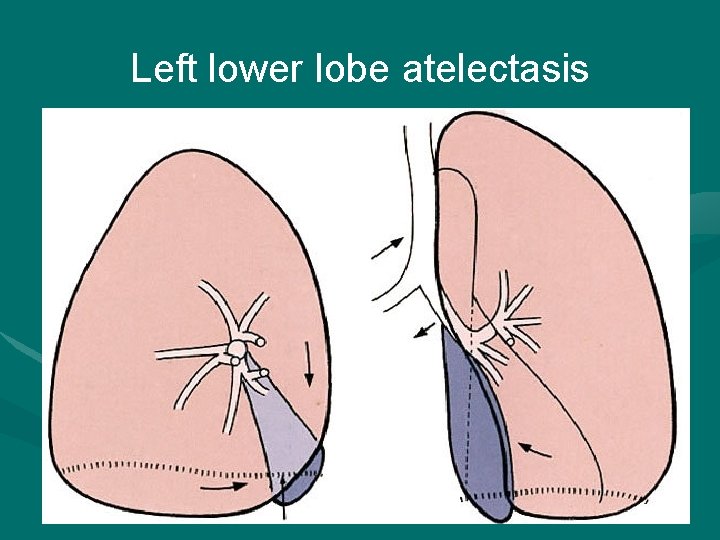
Left lower lobe atelectasis 2022/1/4
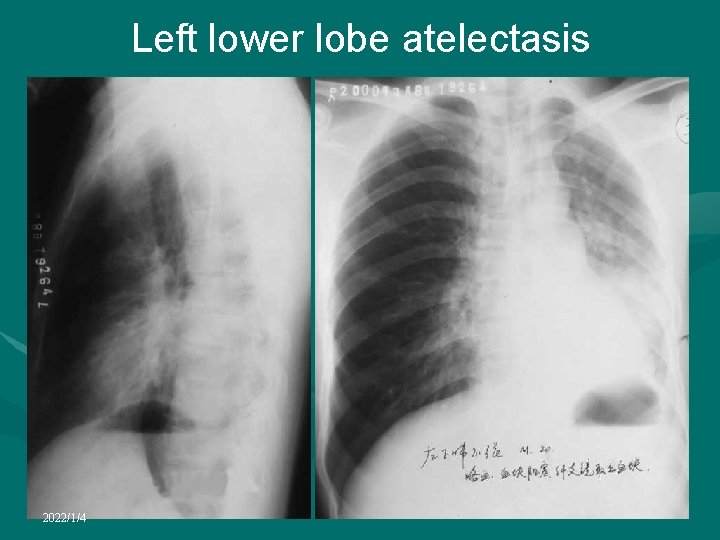
Left lower lobe atelectasis 2022/1/4

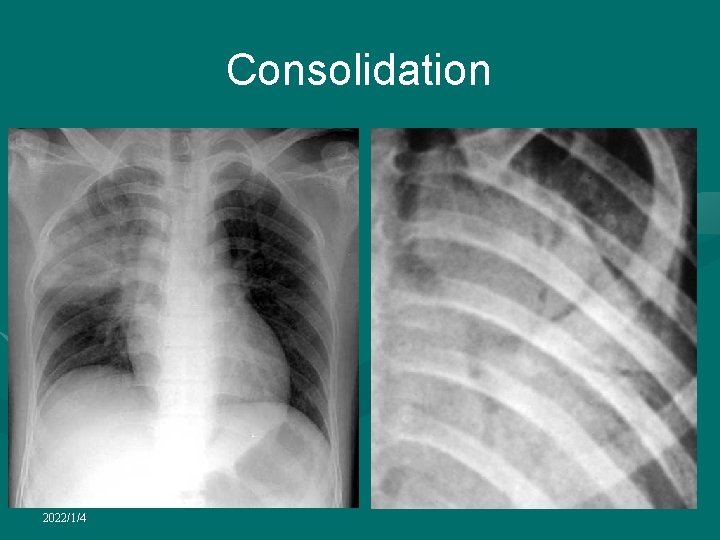
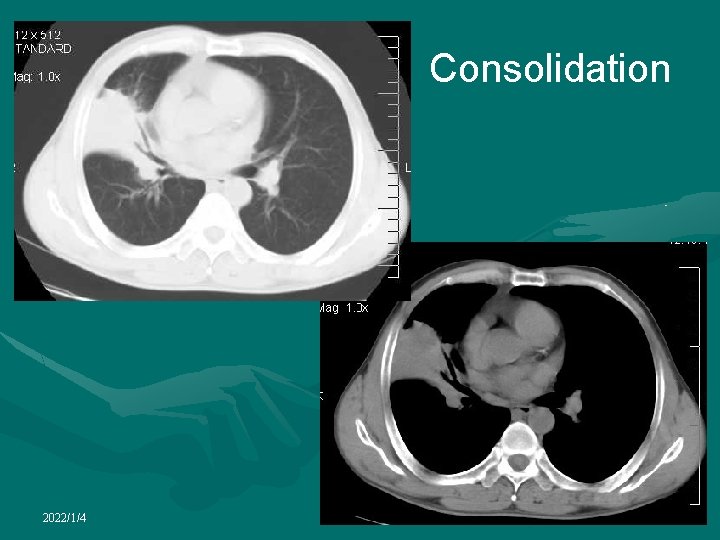
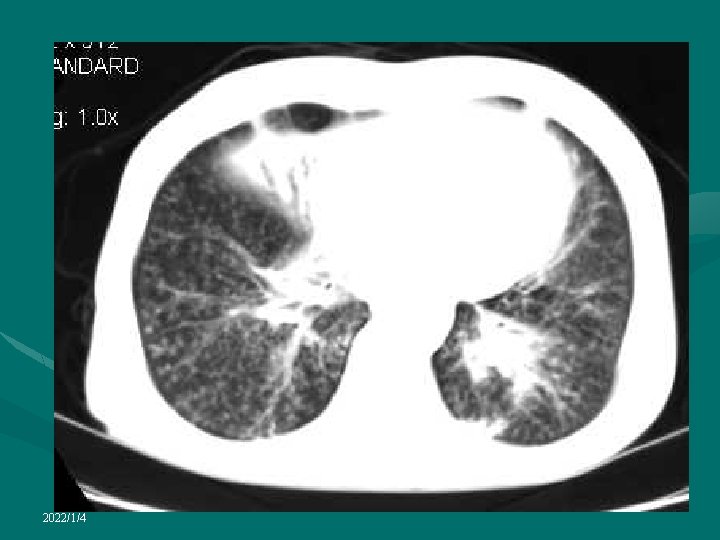
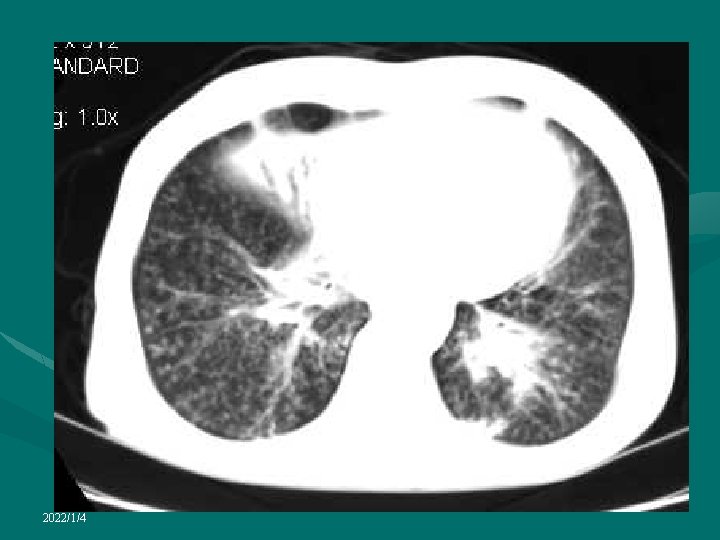
Consolidation • Replacement of alveolar air by fluid, cells, tissue, or other material • Homogeneous increase in lung attenuation with obscuration of underlying pulmonary vessels • Air bronchogram may be seen 2022/1/4

Exudate 2022/1/4
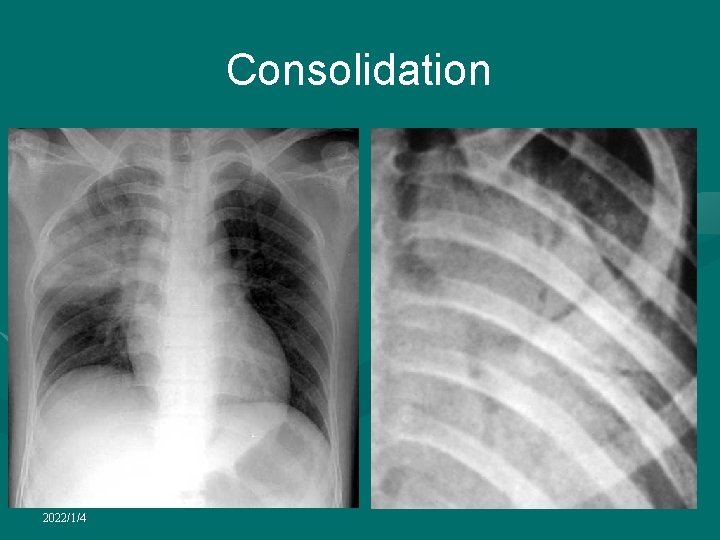
Consolidation 2022/1/4
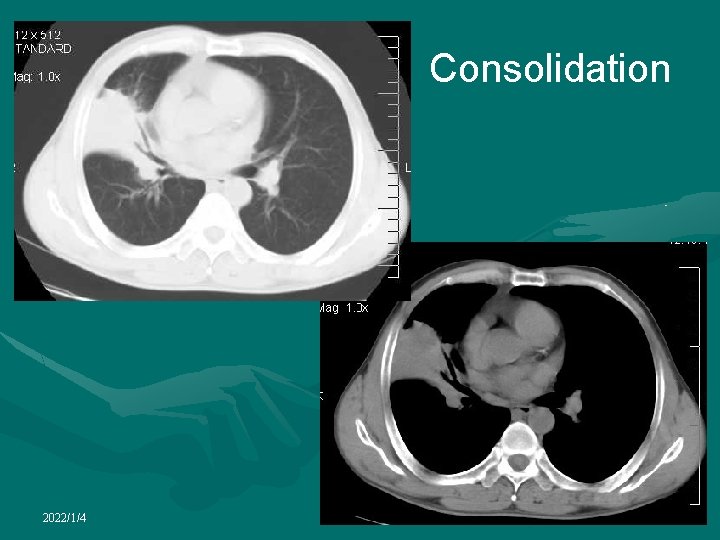
Consolidation 2022/1/4

Proliferation 2022/1/4
2022/1/4
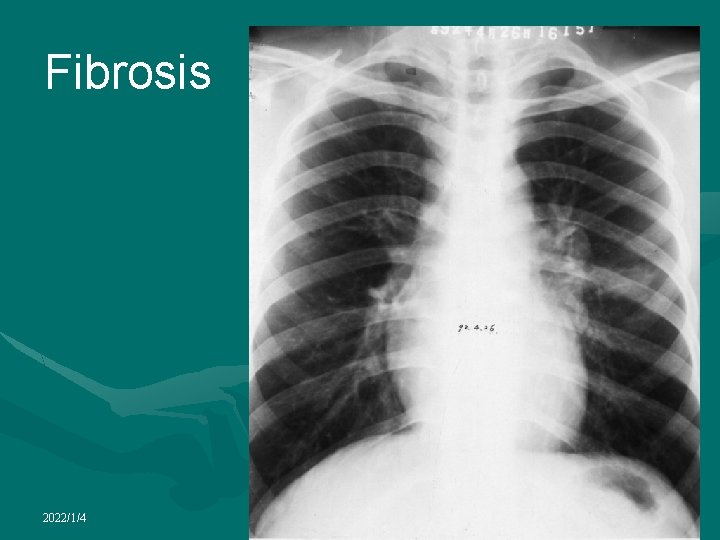
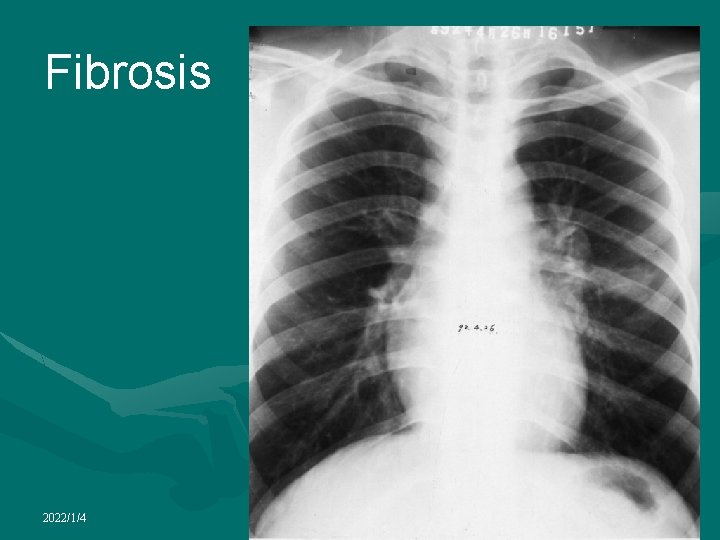
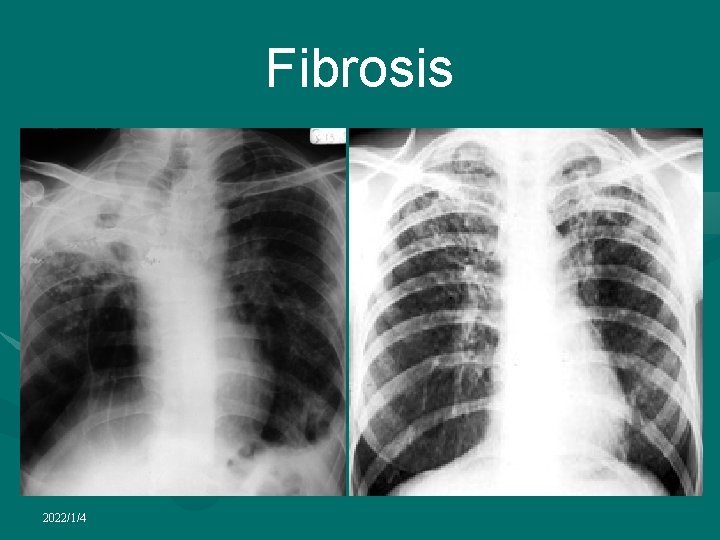
Fibrosis 2022/1/4
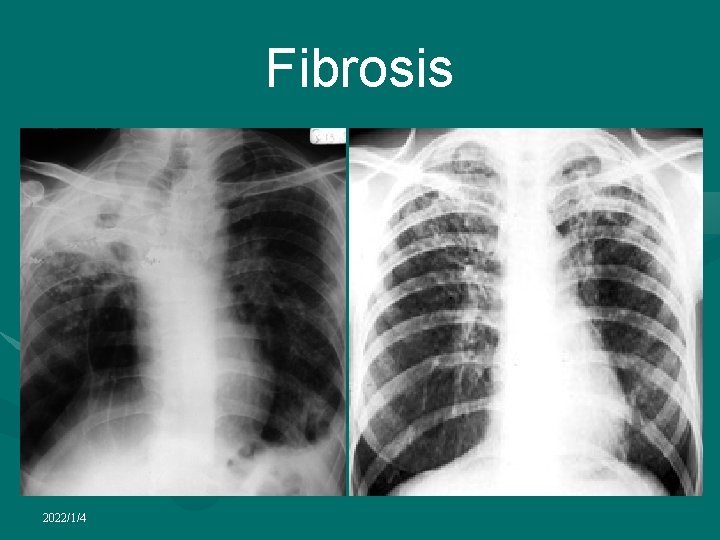
Fibrosis 2022/1/4
Calcification • Pattern of calcification in a solitary pulmonary nodule can help differentiate benign from malignant nodules • Four benign patterns of calcification: central, diffuse solid, laminated, and "popcornlike. " • The first three patterns are typically seen with prior infections, particularly histoplasmosis or tuberculosis. • Popcornlike calcification is characteristic of chondroid calcification in a hamartoma. When present, are reliable indicators of a benign cause • Unfortunately, 38%– 63% of benign nodules are not calcified, and the reported prevalence of calcification in hamartomas at CT varies from 5% to 50% 2022/1/4
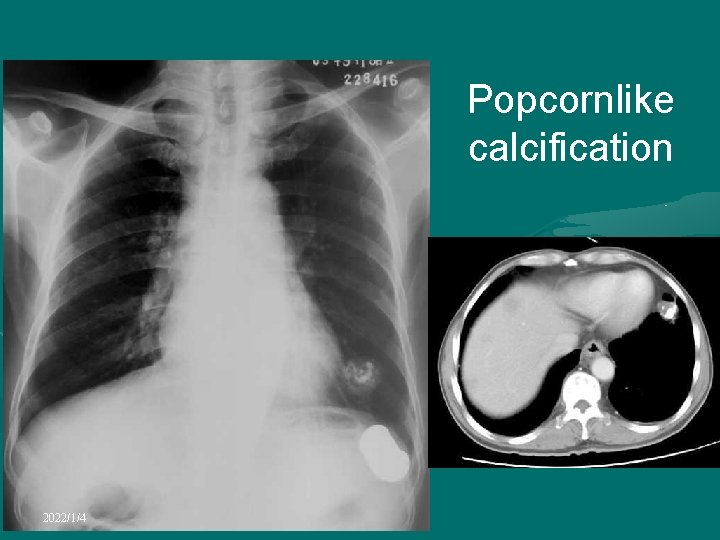
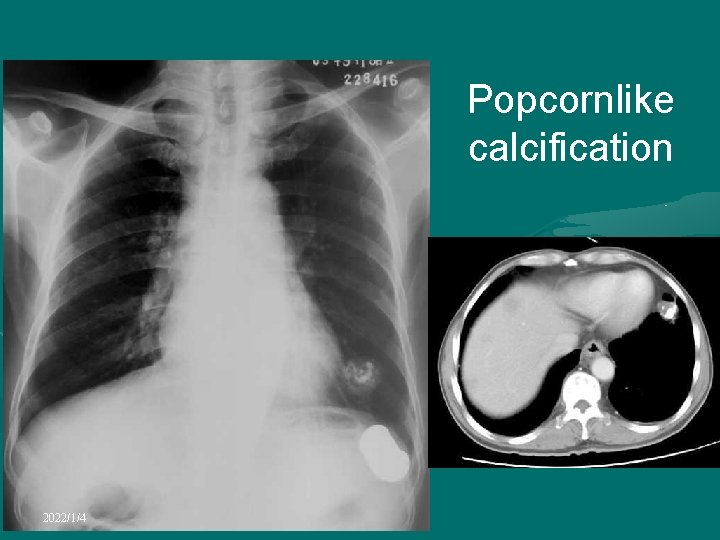
Popcornlike calcification 2022/1/4
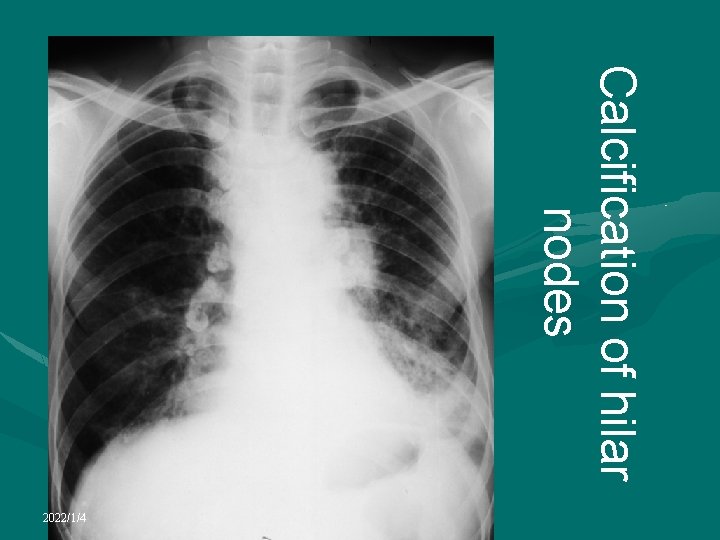
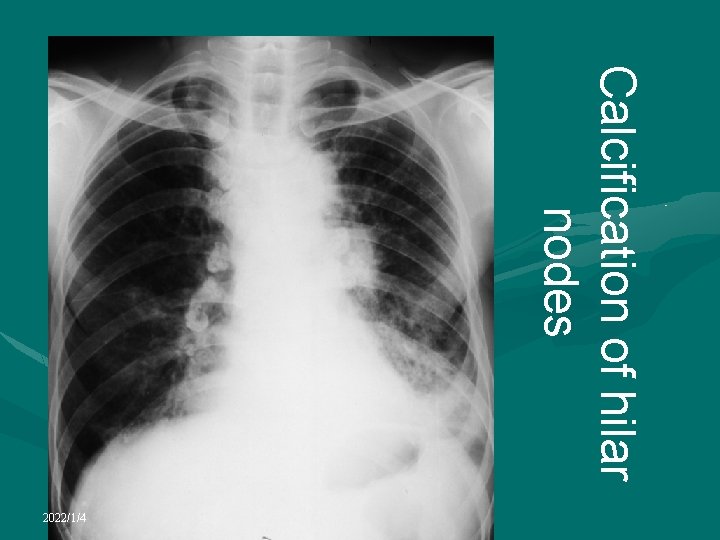
Calcification of hilar nodes 2022/1/4
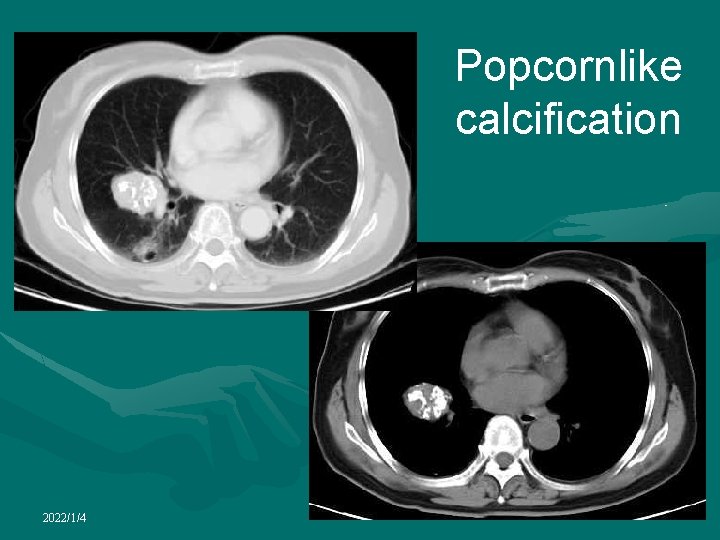
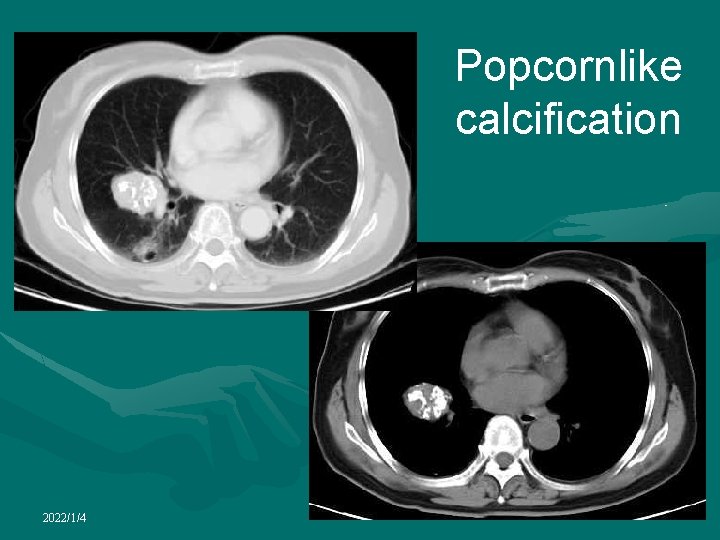
Popcornlike calcification 2022/1/4
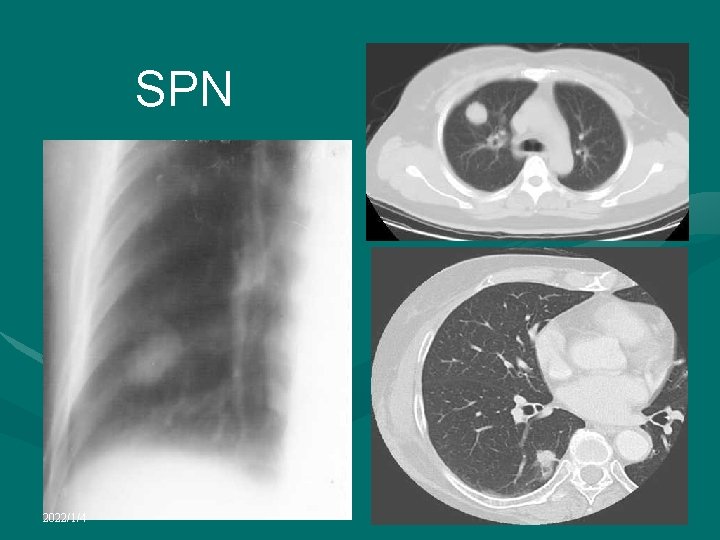
Solitary pulmonary nodule • A well-circumscribed round or oval-shaped lesion measuring less than 3 cm in diameter • Common finding on routine screening chest radiograph in adults • vast majority of such incidentally detected lesions are benign • Most common radiological manifestation in patients with asymptomatic lung cancer • Almost always benign in patients under 30. • but should be followed for at least 2 years. • At the age of 40 and beyond, the likelihood of malignancy is increased • Most prove resectable, early diagnosis remains essential 2022/1/4
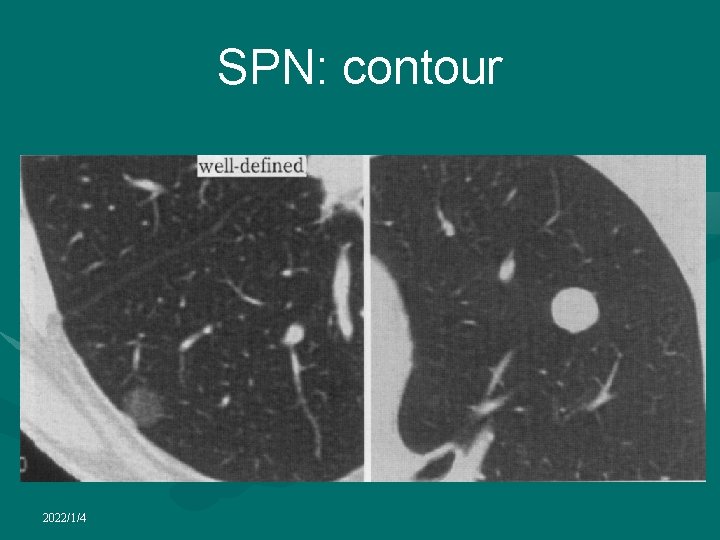
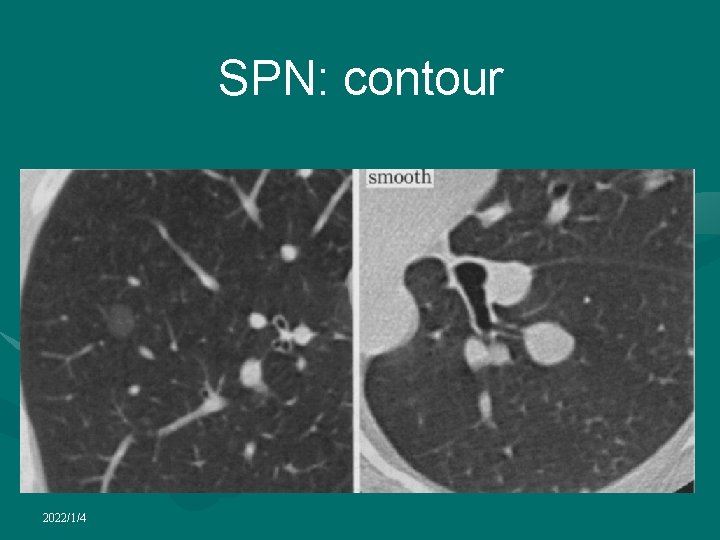
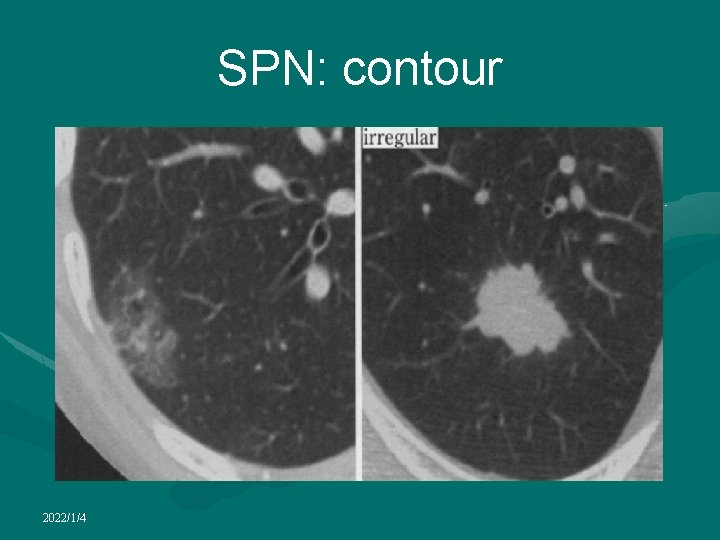
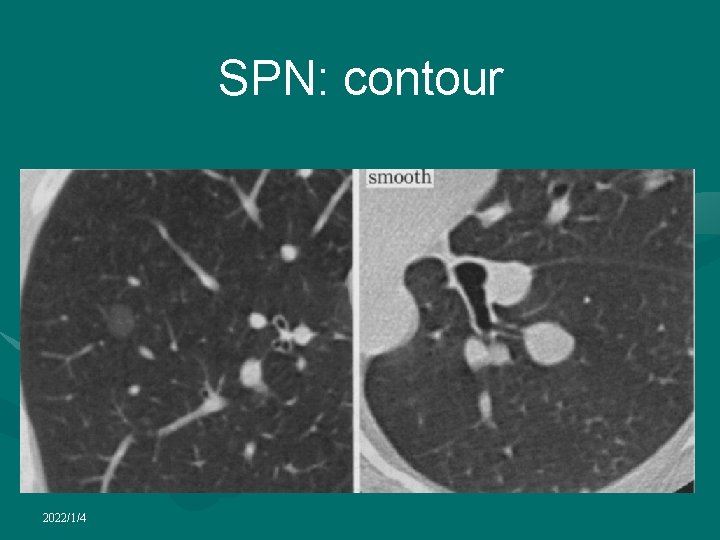
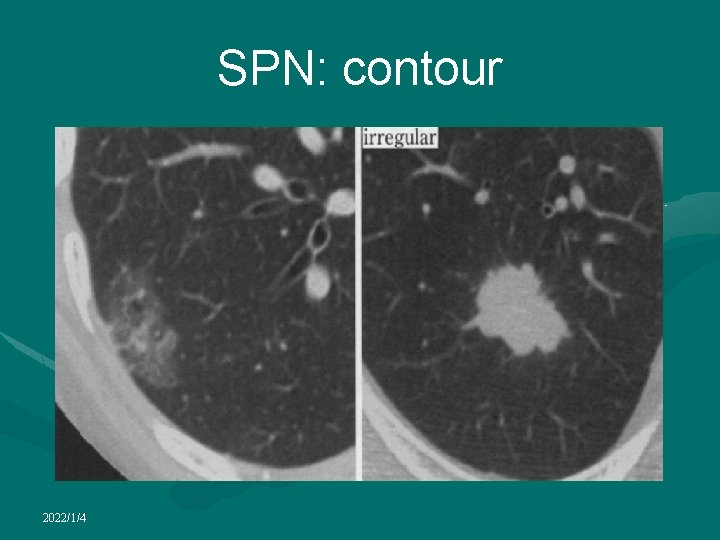
Solitary pulmonary nodule • CT is almost always obtained in the diagnostic work-up of SPN • Radiological factors most often considered useful in determining nature of a SPN: • lesion size • Nodule margins and contours can be classified as smooth, lobulated, irregular, or spiculated • growth rate • presence of calcification 2022/1/4

Solitary pulmonary nodule • Likelihood of malignancy in an indeterminate SPN detected by chest radiography is a direct function of the size of the lesion • Large majority of nodules > 2 cm are malignant while only about 50% of nodules < 2 cm are malignant • Pulmonary malignant nodules often appear ill-defined and/or irregular in shape • A spiculated appearance on HRCT strongly suggests malignancy • Benign nodules are often well-defined, round and smooth in contour • However, solitary pulmonary metastases may have the same appearance 2022/1/4
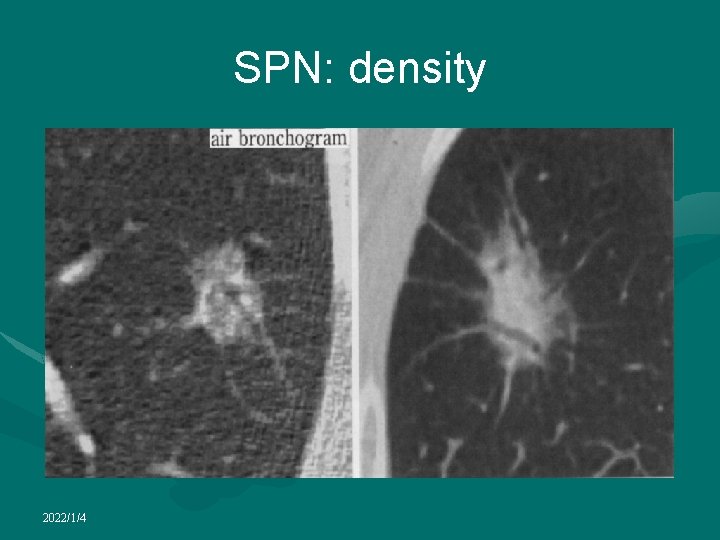
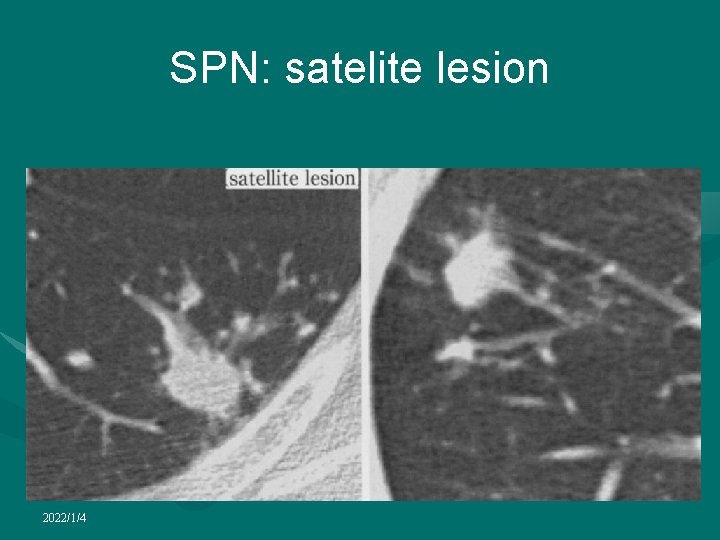
Solitary pulmonary nodule • Air bronchograms within a nodule are more common in malignancies than in benign nodules and more suggestive of adenocarcinomas or bronchioalveolar cell carcinomatosis • Cavitation is also more common in malignant nodules than benign nodules • But focal benign pulmonary lesions such lung abscess can also cavitate • Satellite nodules in association with an SPN suggest granulomatous disease • Skip metastases around a bronchogenic carcinoma cannot be ruled out 2022/1/4
Solitary pulmonary nodule • Presence of calcification within a SPN is generally a reliable sign of benignancy • Benign types of calcification include diffuse, those with a central nidus, laminated or popcorn • While stippled or eccentric calcification may be present in as many as 10% of malignant lung neoplasms • CT is more sensitive than radiography in the detection of calcification • Measuring CT number can allow the detection of calcifications invisible on CT scans in some patients with benign nodules (CT nodule densitometry) • Pixels denser than 200 HU usually indicate the presence of calcifications 2022/1/4

Solitary pulmonary nodule • By detecting the presence of fat, CT may be helpful in diagnosing pulmonary hamartoma, or other benign lesions such as lipoid pneumonia • Certain lesions in the lung may display the nonspecific features of an SPN on chest radiography, while CT may identify specific diagnostic features 2022/1/4
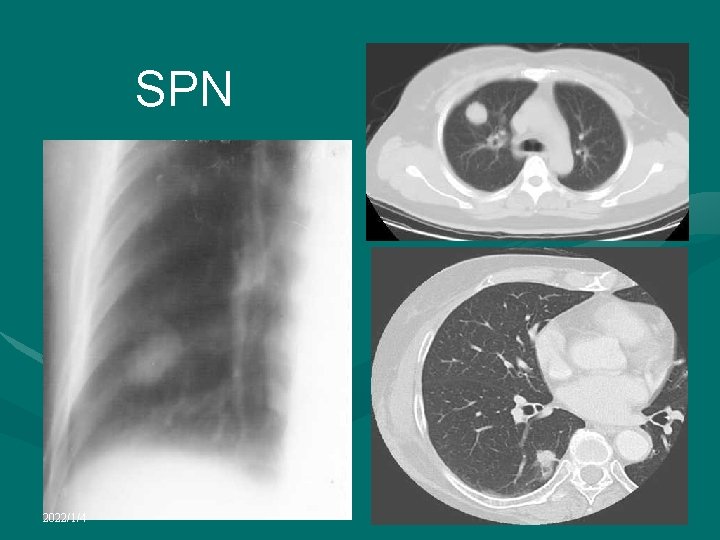
SPN 2022/1/4
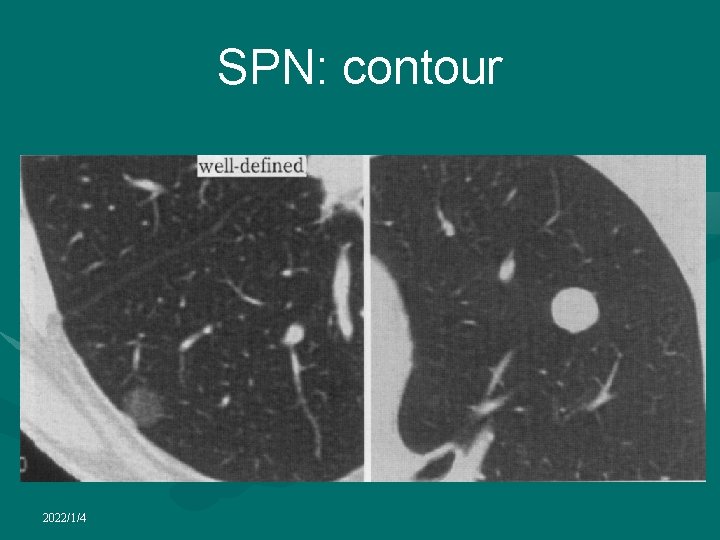
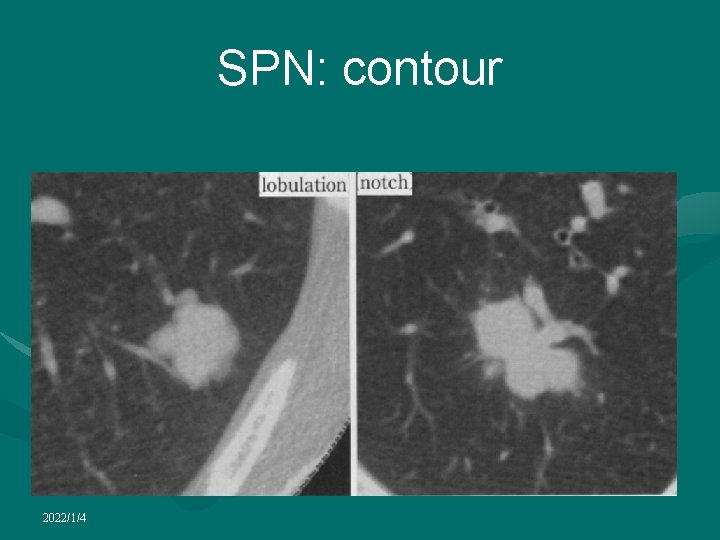
SPN: contour 2022/1/4

SPN: contour 2022/1/4
SPN: contour 2022/1/4
SPN: contour 2022/1/4

SPN: contour 2022/1/4
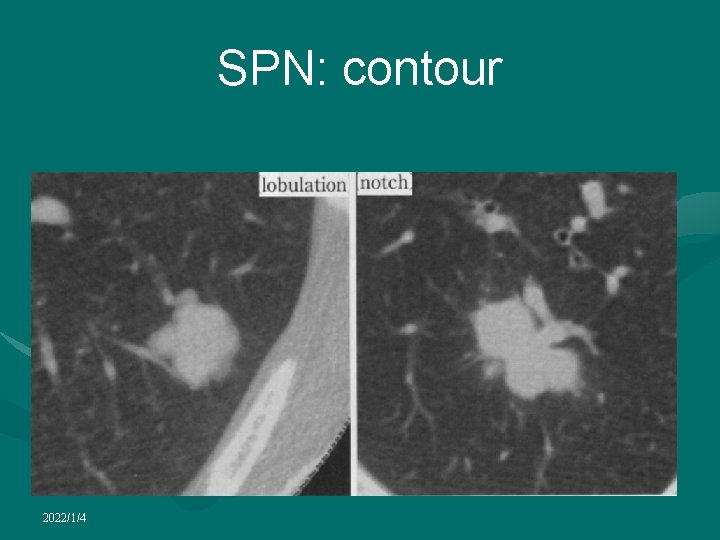
SPN: contour 2022/1/4
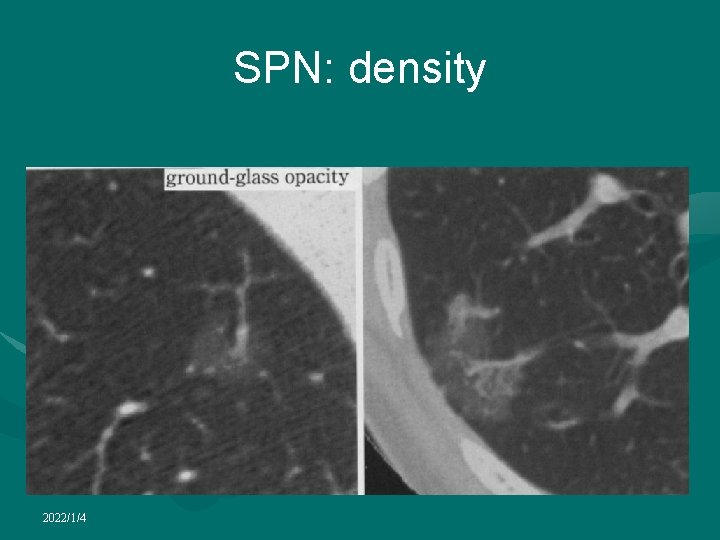
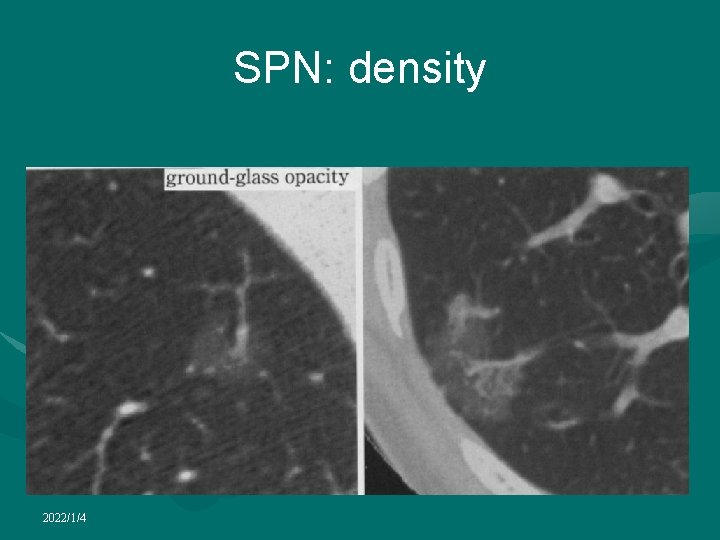
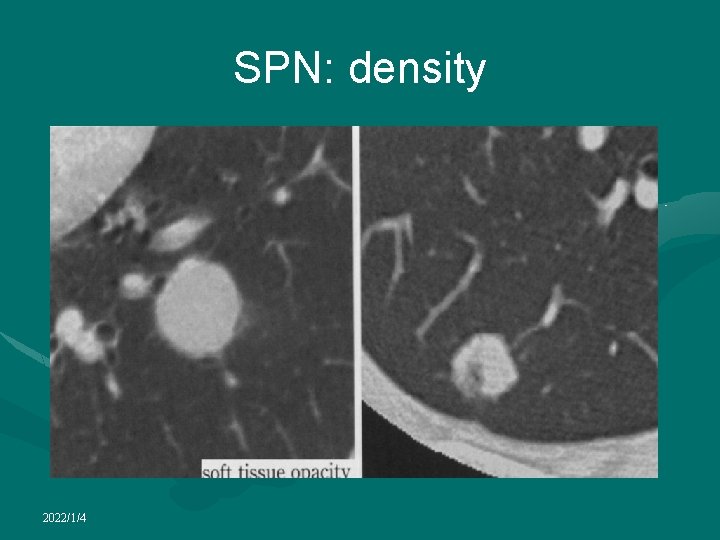
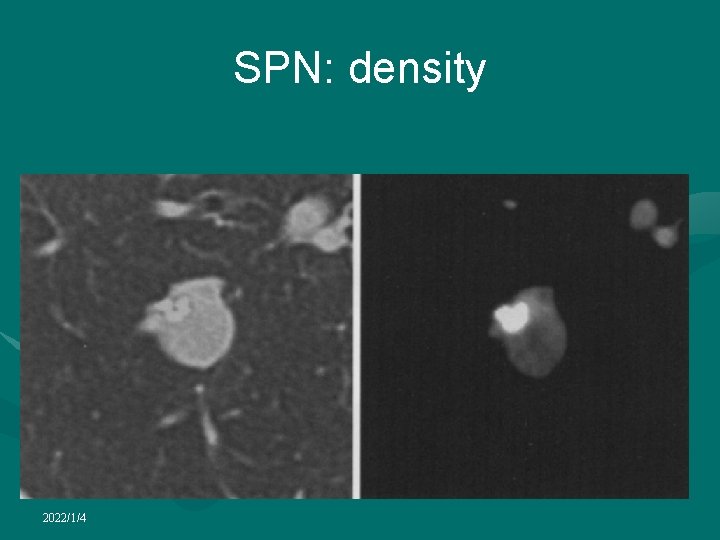
SPN: density 2022/1/4
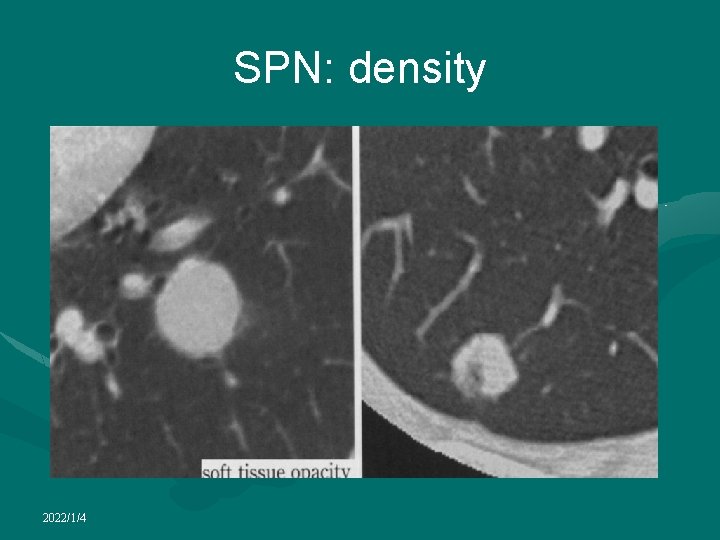
SPN: density 2022/1/4

SPN: density 2022/1/4

SPN: density 2022/1/4
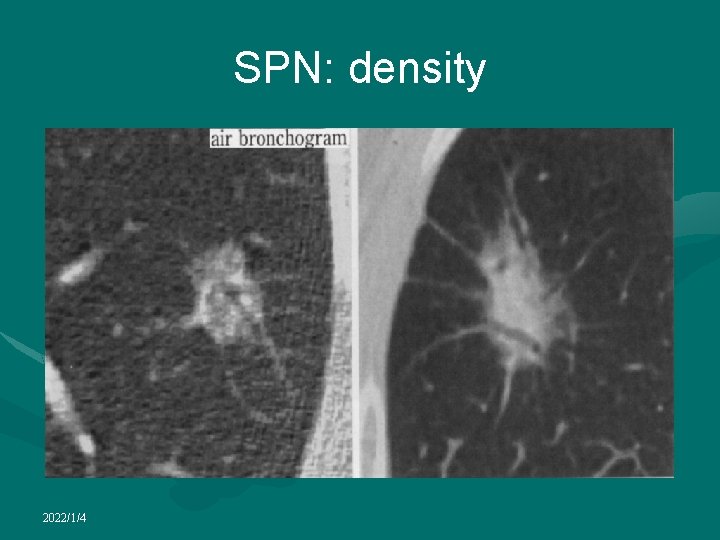
SPN: density 2022/1/4

SPN: density 2022/1/4
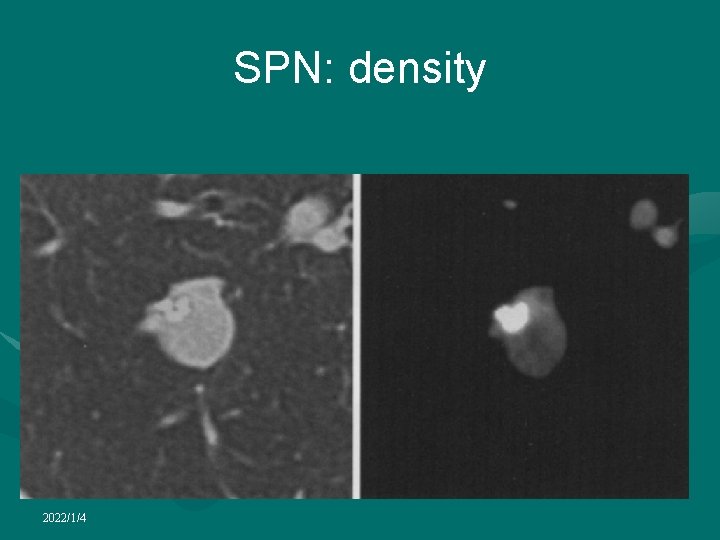
SPN: density 2022/1/4
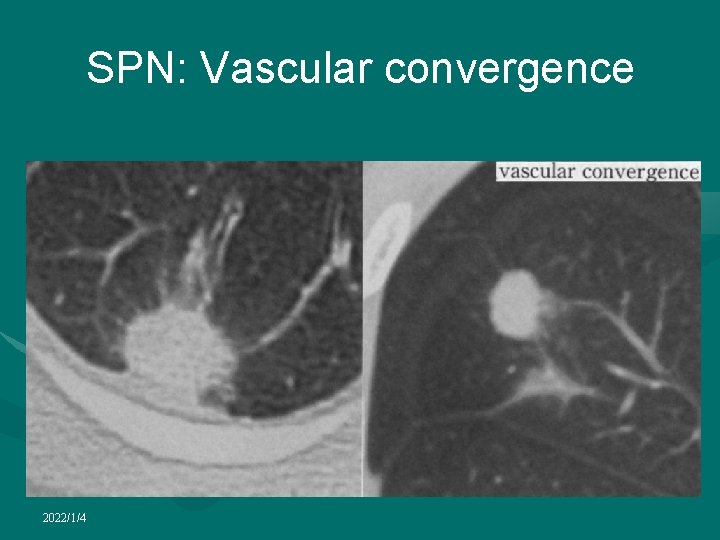
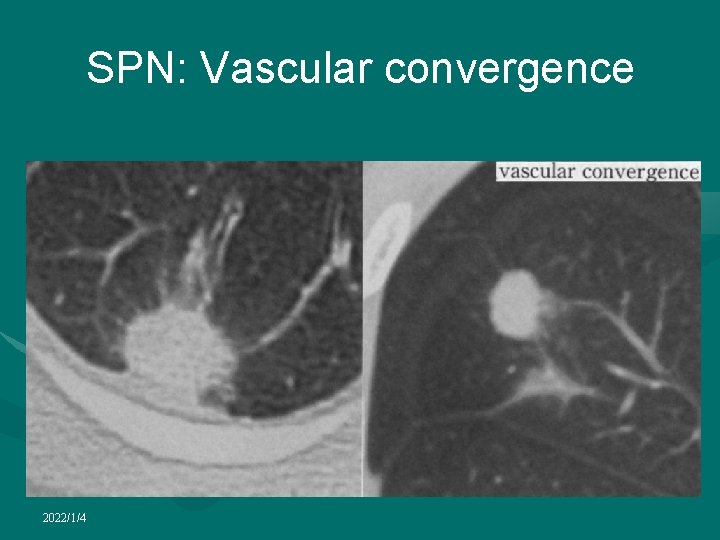
SPN: Vascular convergence 2022/1/4
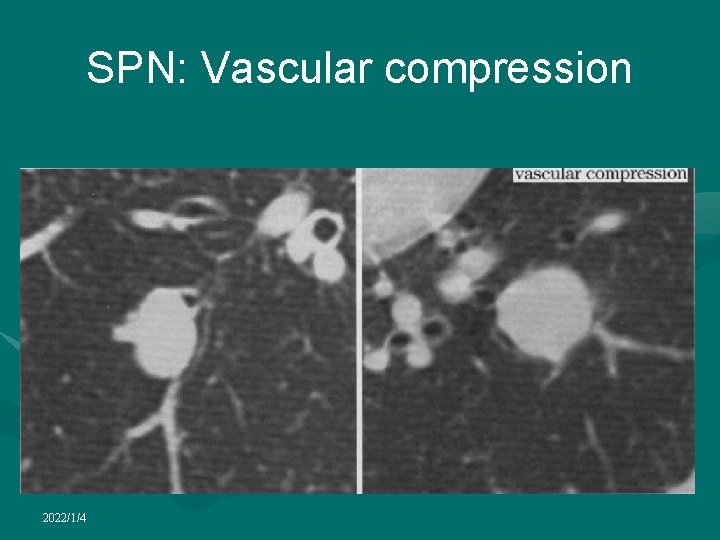
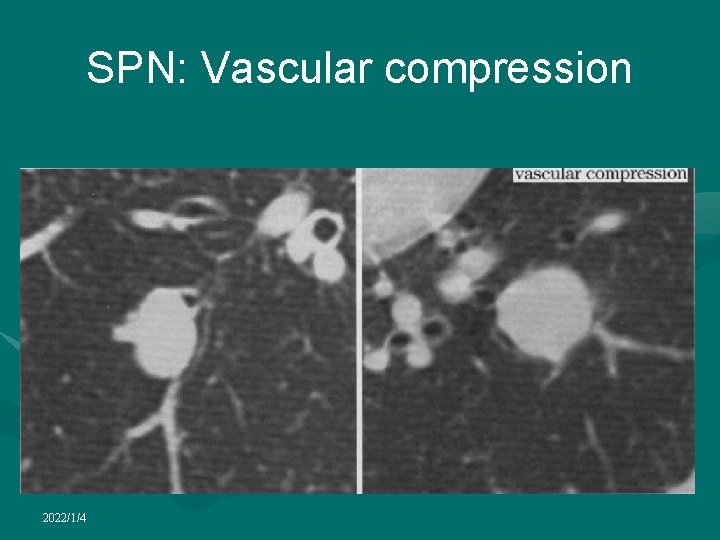
SPN: Vascular compression 2022/1/4
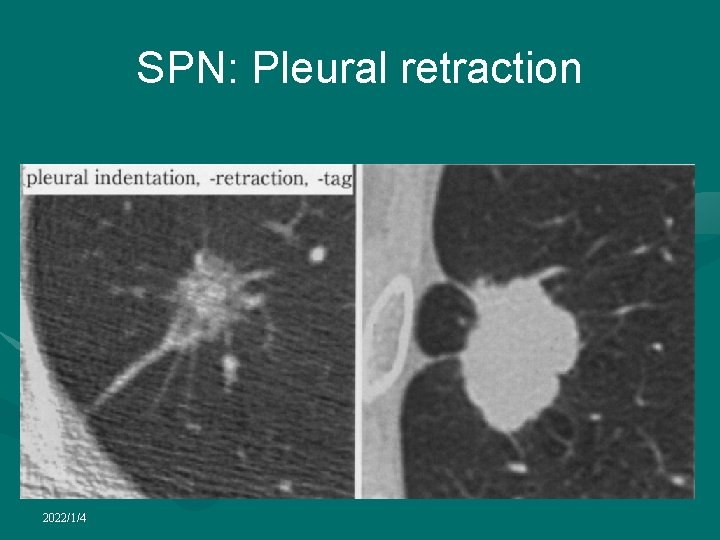
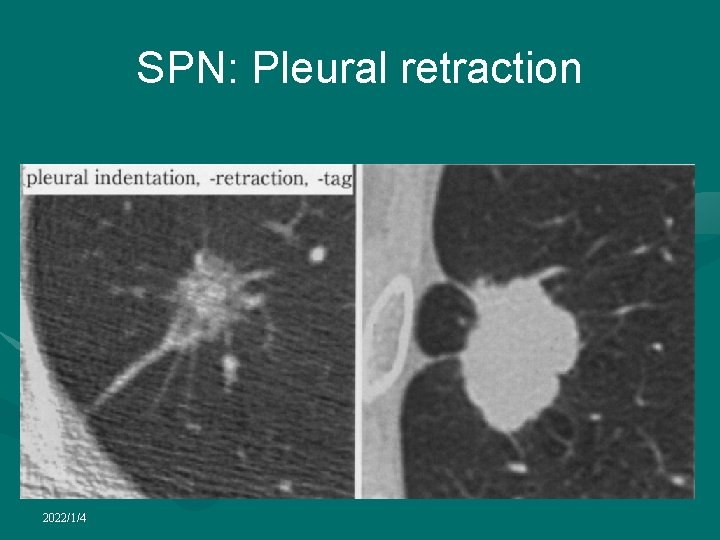
SPN: Pleural retraction 2022/1/4
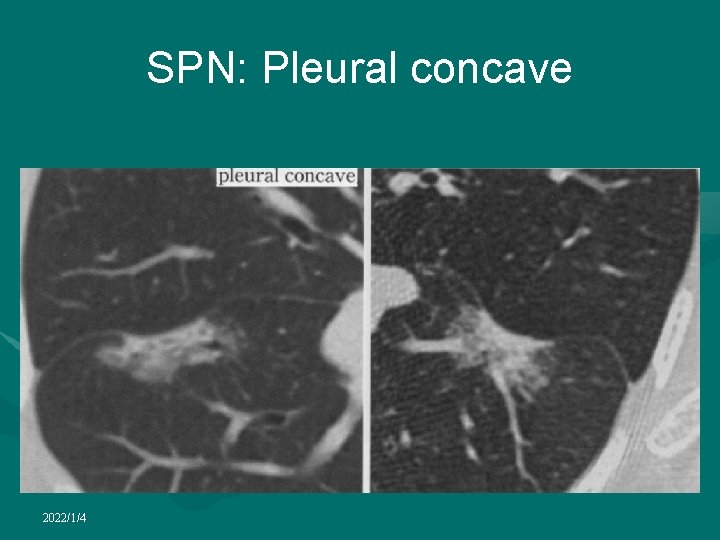
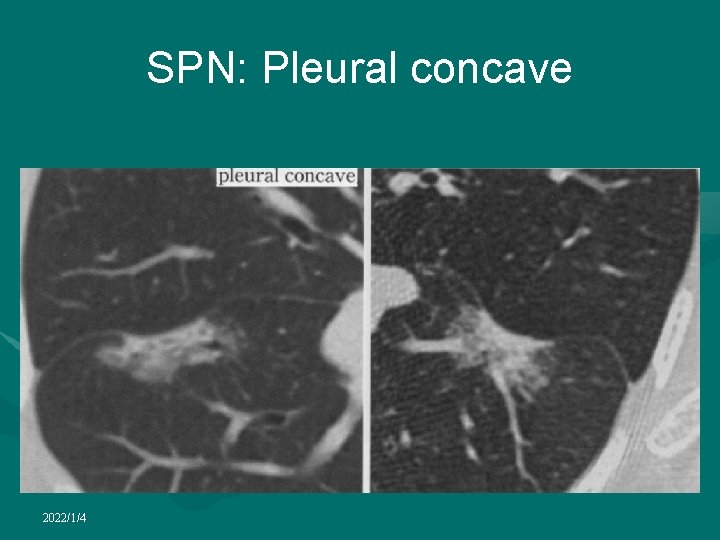
SPN: Pleural concave 2022/1/4
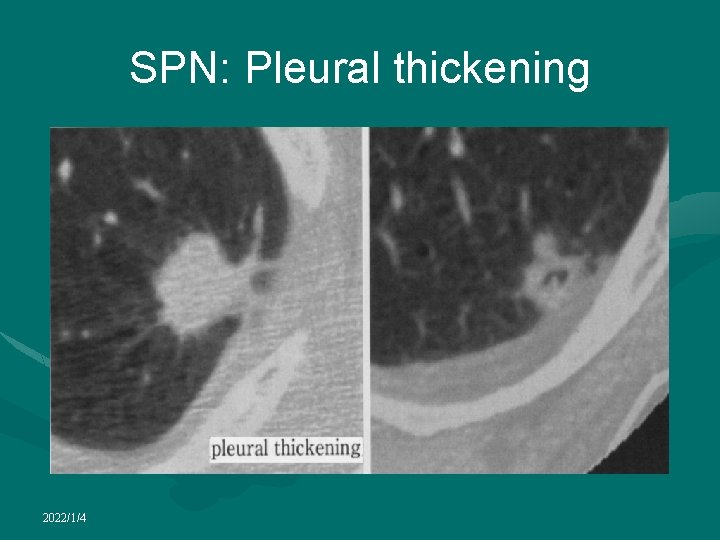
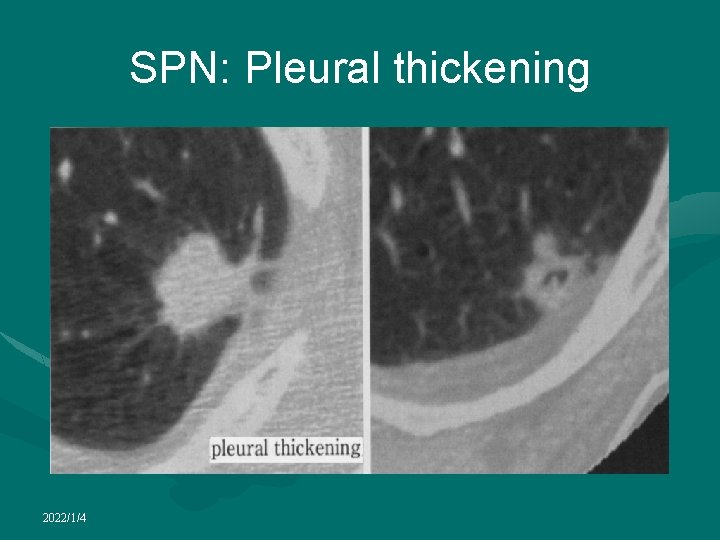
SPN: Pleural thickening 2022/1/4
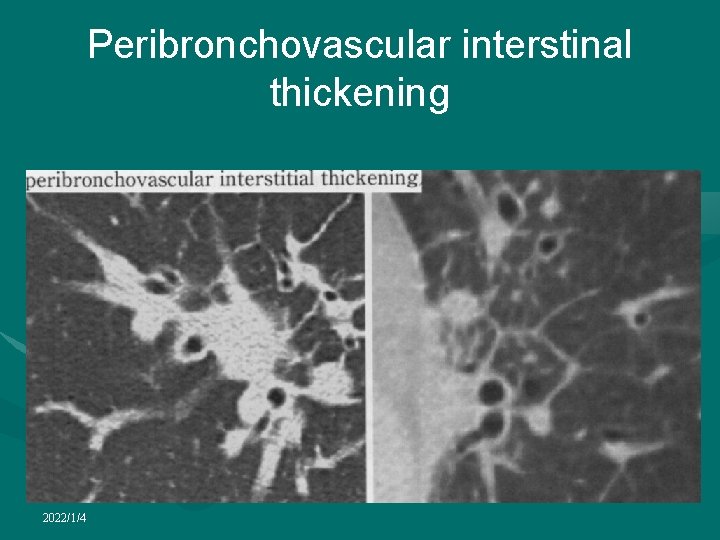
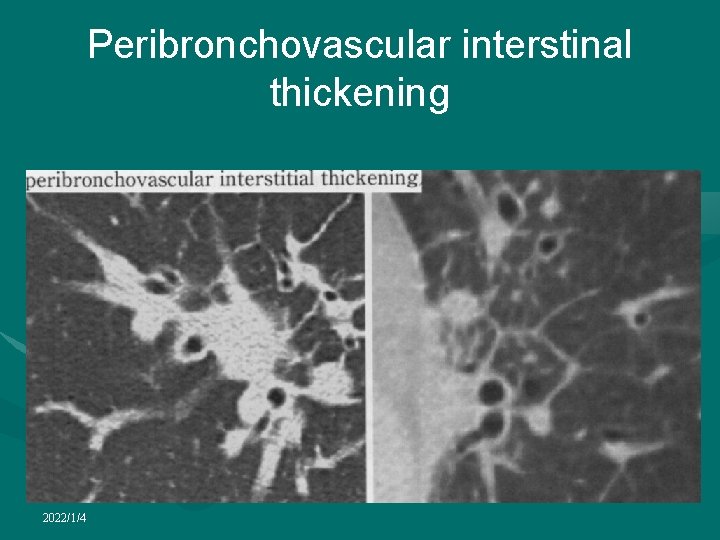
Peribronchovascular interstinal thickening 2022/1/4
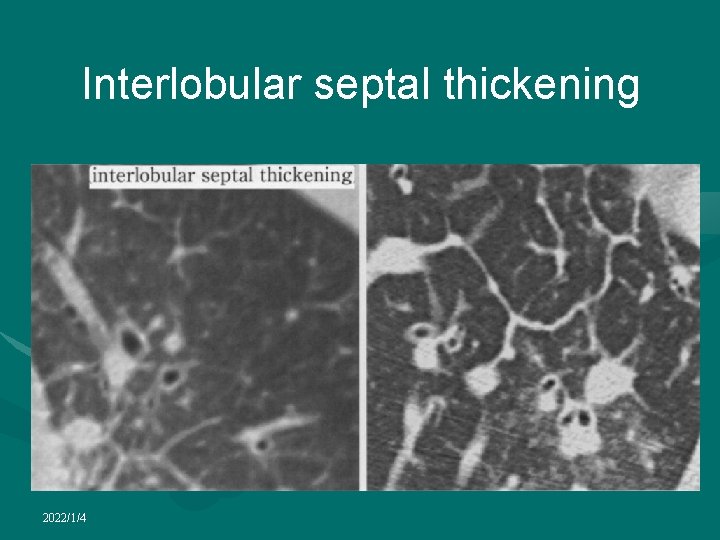
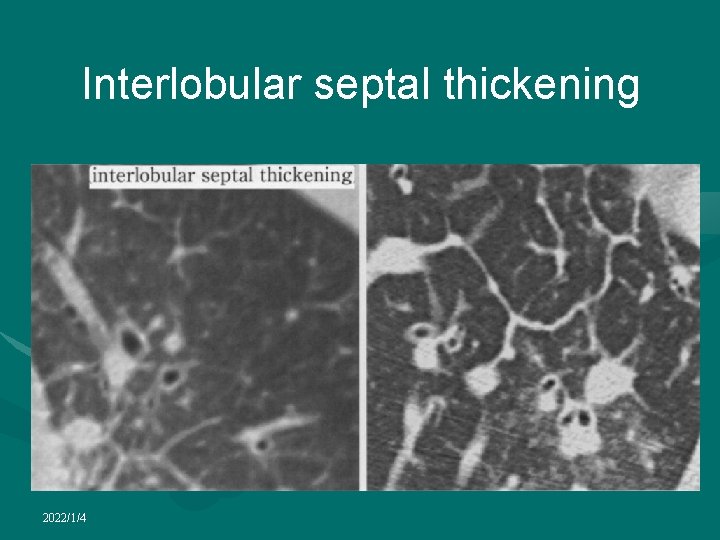
Interlobular septal thickening 2022/1/4
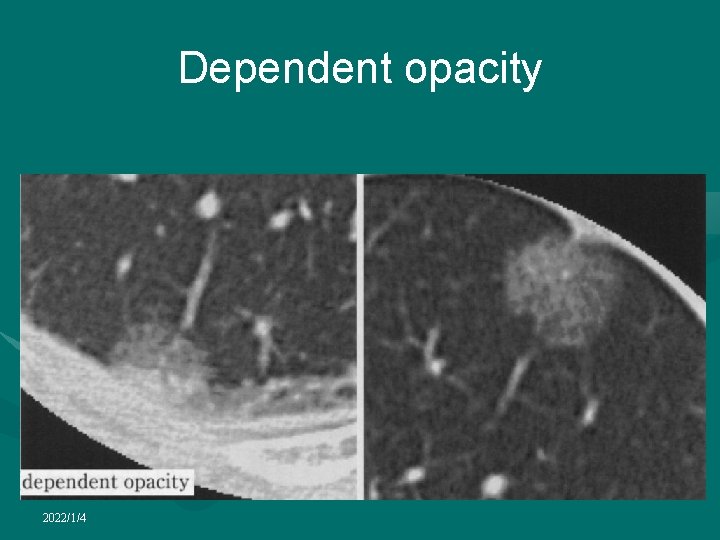
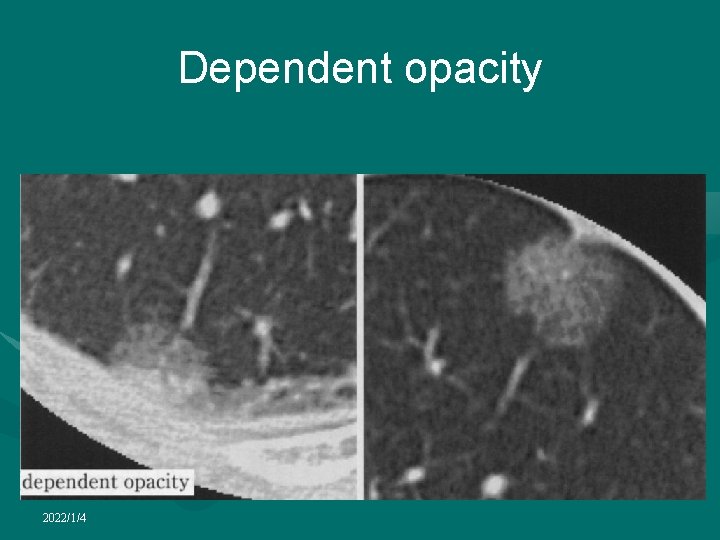
Dependent opacity 2022/1/4
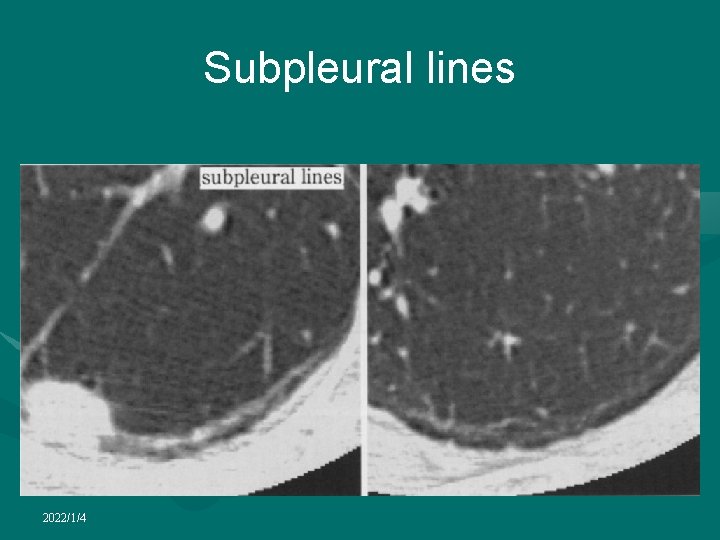
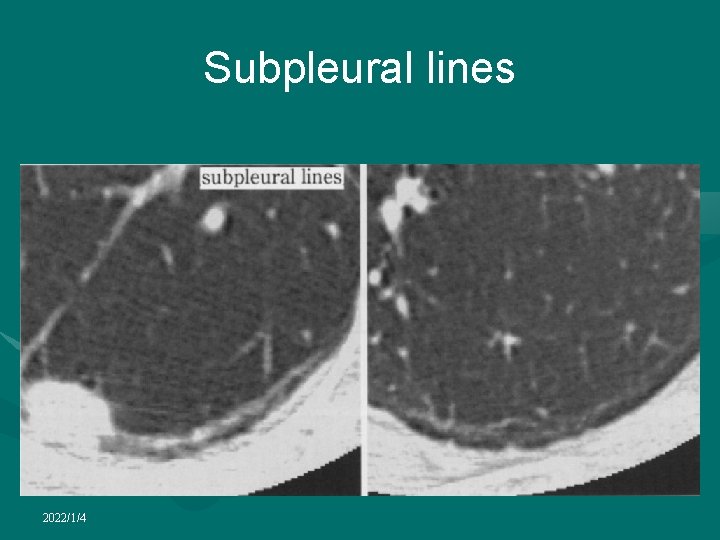
Subpleural lines 2022/1/4
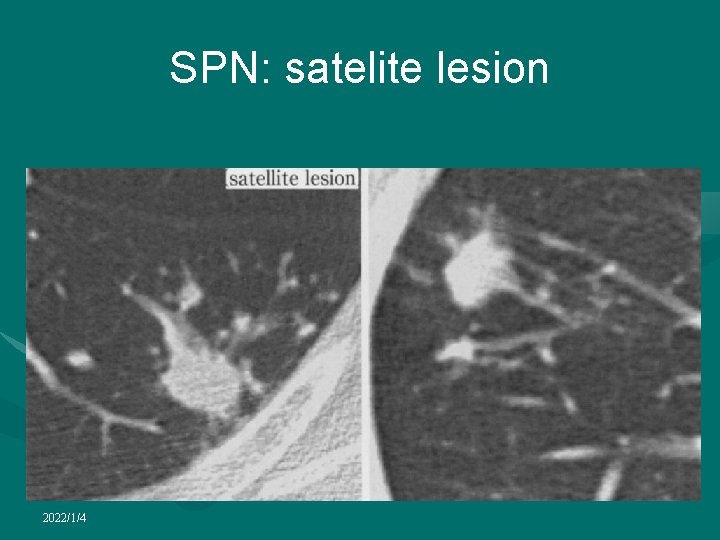
SPN: satelite lesion 2022/1/4

SPN 2022/1/4
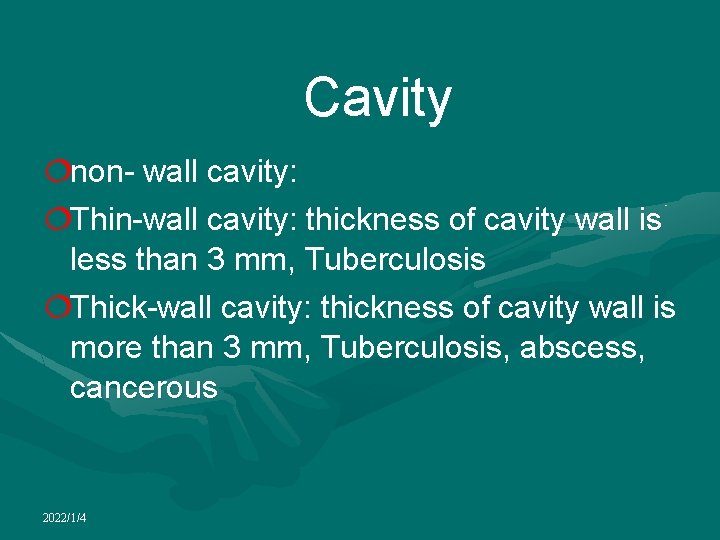
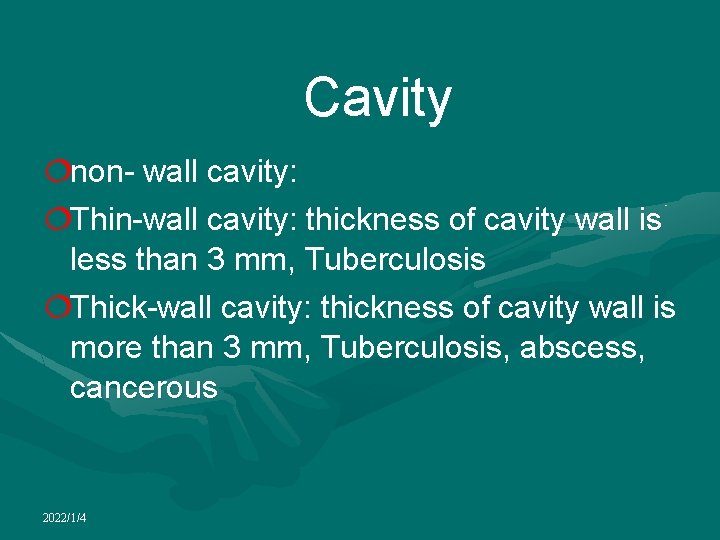
Cavity ¦non- wall cavity: ¦Thin-wall cavity: thickness of cavity wall is less than 3 mm, Tuberculosis ¦Thick-wall cavity: thickness of cavity wall is more than 3 mm, Tuberculosis, abscess, cancerous 2022/1/4
Cavitation • Occurs in both benign and malignant nodules • Benign cavitary nodules generally have smooth, thin walls, whereas malignant nodules typically have thick, irregular walls • Most nodules with a wall thickness greater than 16 mm are malignant, whereas those with a wall thickness less than 4 mm are usually benign 2022/1/4

Non-wall cavity 2022/1/4

Tuberculous cavity 2022/1/4

Thin-walled cavity 2022/1/4

Tuberculous cavity 2022/1/4

Abscese cavity 2022/1/4
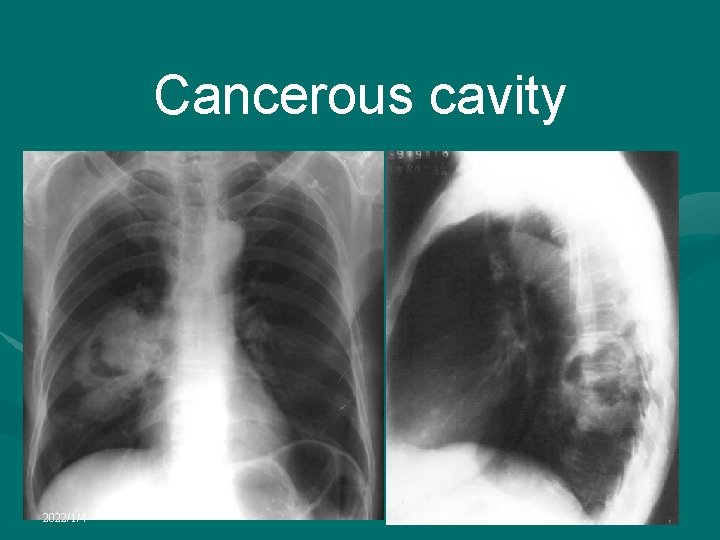
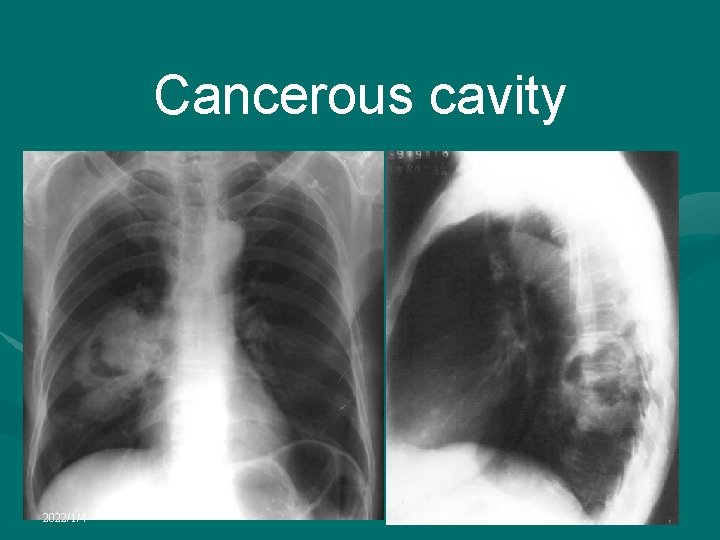
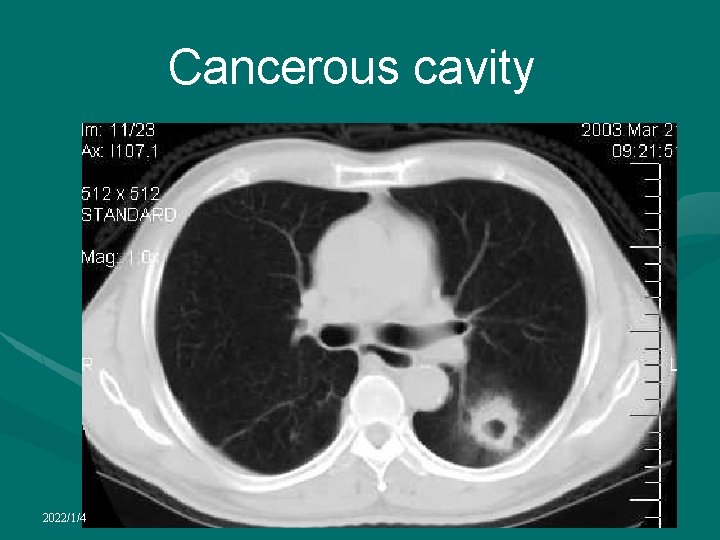
Cancerous cavity 2022/1/4
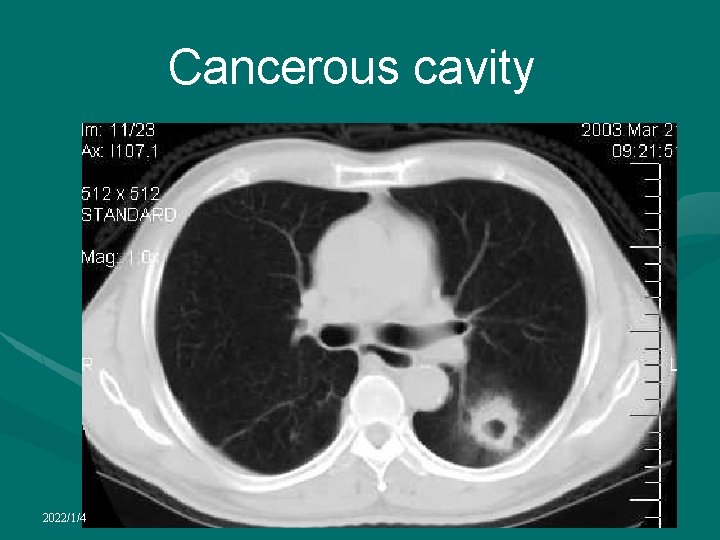
Cancerous cavity 2022/1/4
Bullae • • Emphysematous spaces larger than 1 cm • presence of emphysema associated with large bullae is referred to as bullous emphysema • • Patients with isolated bullae are usually without signs or symptoms • On the chest radiograph, large bullae are seen as avascular transradiant areas usually separated from the remaining lung parenchyma by a thin curvilinear wall of a very variable extent • • cause marked relaxation collapse of the adjacent lung • CT is the best available technique for assessing the number, size and location of bullae, which is essential in cases considered for bullectomy • avascular, low attenuation areas that are larger than 1 cm and that can have a thin but perceptible wall Generally seen in centrilobular emphysema and/or paraseptal emphysema Occasionally large bullae produce dyspnoea that may necessitate bullectomy even extend across into the opposite hemithorax, particularly by way of the anterior junctional area 2022/1/4
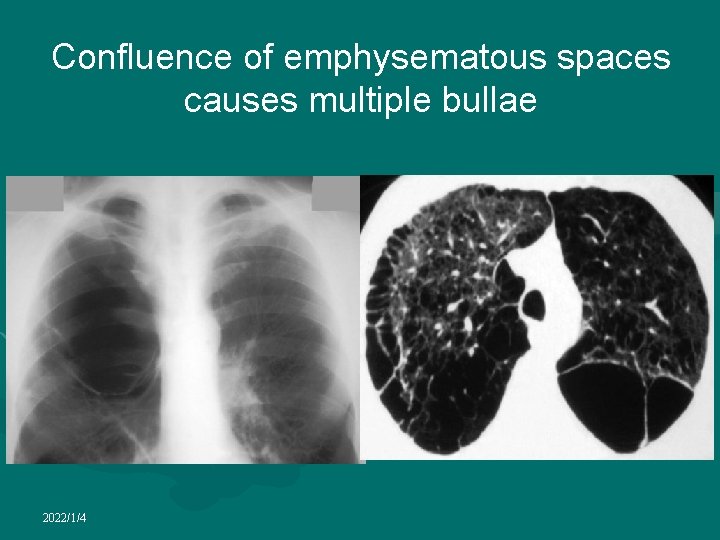
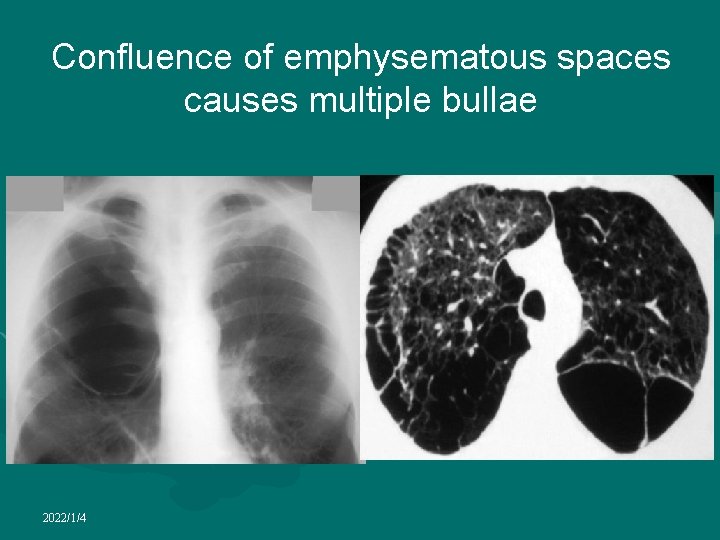
Confluence of emphysematous spaces causes multiple bullae 2022/1/4

Bullae 2022/1/4
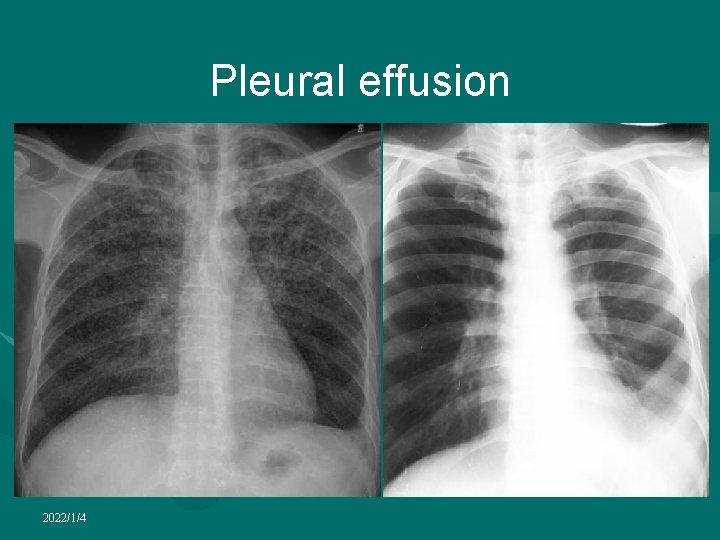
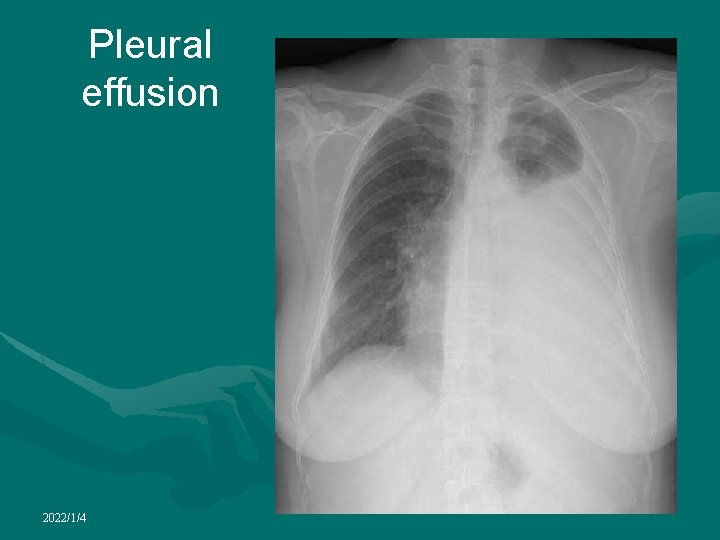
Pleural effusion • Develops when the rate of formation of pleural fluid exceeds its absorption • Formed principally by the parietal pleura and absorbed by the lymphatics • There is normally less than 5 ml of fluid within the pleural space • Several mechanisms contribute to the formation of a pleural effusion • Raised pulmonary venous pressure with resultant increased microvascular hydrostatic pressure • Increased microvascular permeability as in inflammatory lung disease • Reduced pleural space pressure (for example, in lobar collapse), which results in leakage of intravascular fluid into the pleural space • Decreased plasma oncotic pressure as in hypoproteinaemia • Impaired lymphatic drainage • Transdiaphragmatic passage of peritoneal fluid • May be a transudate or an exudate and these can be distinguished by biochemical analysis of the fluid content 2022/1/4
Pleural effusion • Radiological signs of a pleural effusion depend on the amount and distribution and whether fluid is freely mobile or loculated • Free fluid tends to collect in dependent areas, initially in the subpulmonary region beneath the lower lobes • As the volume increases, it spills into the posterior and then lateral costophrenic angles • Blunting of the lateral costophrenic angle on an erect frontal chest radiograph occurs when 25~525 ml is present. However, as little as 10 ml can be detected with a lateral decubitus view • With an increasing volume of pleural fluid the hemidiaphragm outline is obscured and there is homogeneous opacification of the lower hemithorax associated with a meniscus shape of the fluid at its upper, lateral margin 2022/1/4

Pleural effusion • In supine, pleural fluid collects posteriorly, producing reduced transradiancy of the ipsilateral hemithorax but vascular markings are preserved, enabling differentiation from consolidation • Supine chest radiographs are relatively insensitive for pleural fluid detection • • • Larger volumes of fluid may produce a peripheral opacity between the lung and chest wall, particularly towards the apex of the lung and there may be thickening of the minor fissures and widening of the paraspinal soft tissues A massive effusion causes dense opacification of the hemithorax with displacement of the mediastinum to the contralateral side and flattening or inversion of the ipsilateral hemidiaphragm Collapse of the underlying lung such as occurs with an endobronchial malignancy or extensive pleural thickening should be considered if the mediastinum remains central 2022/1/4
Pleural effusion • The differential diagnosis of a completely opaque hemithorax includes a massive pleural effusion, lung collapse or consolidation, massive tumor, pneumonectomy or lung agenesis • Unusual radiographic appearances may be produced if fluid lies within the pleural fissures, is loculated or is subpulmonary • Fluid may collect adjacent to the mediastinum, especially on the left, producing a triangular retrocardiac opacity, simulating left lower lobe collapse which is differentiated from true collapse by the normally positioned lower lobe bronchus • Right-sided pleural effusions may displace the azygoesophageal line to the left producing a retrocardiac opacity • Fluid in the azygoesophageal recess may simulate subcarinal lymphadenopathy 2022/1/4
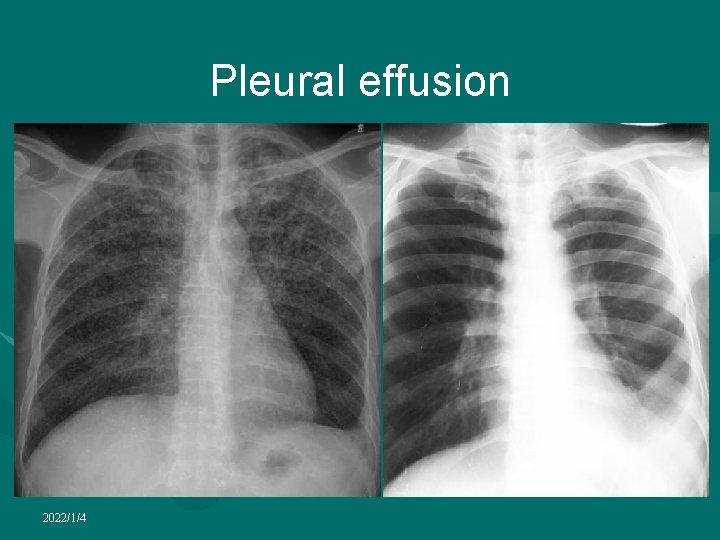
Pleural effusion 2022/1/4
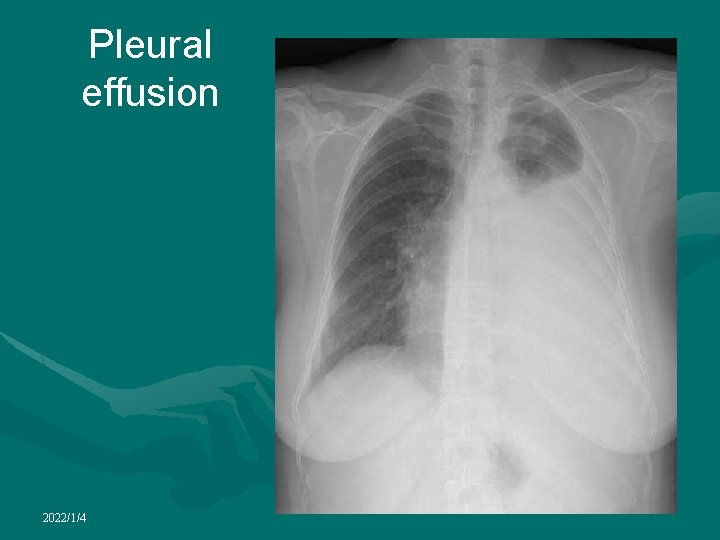
Pleural effusion 2022/1/4
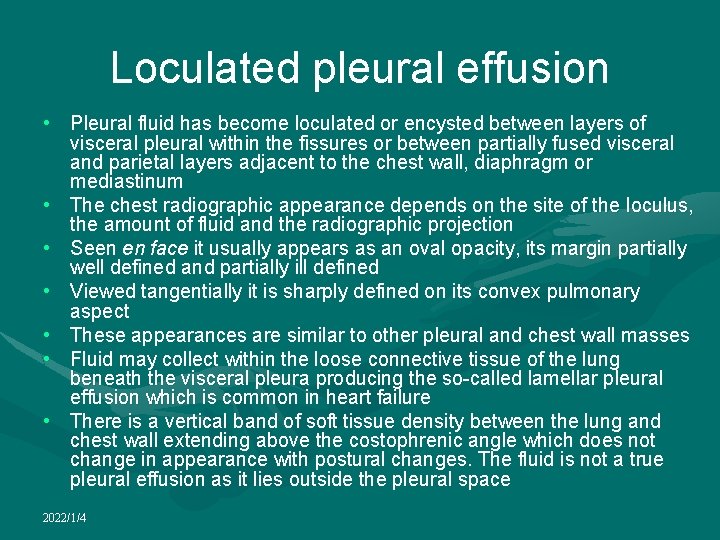
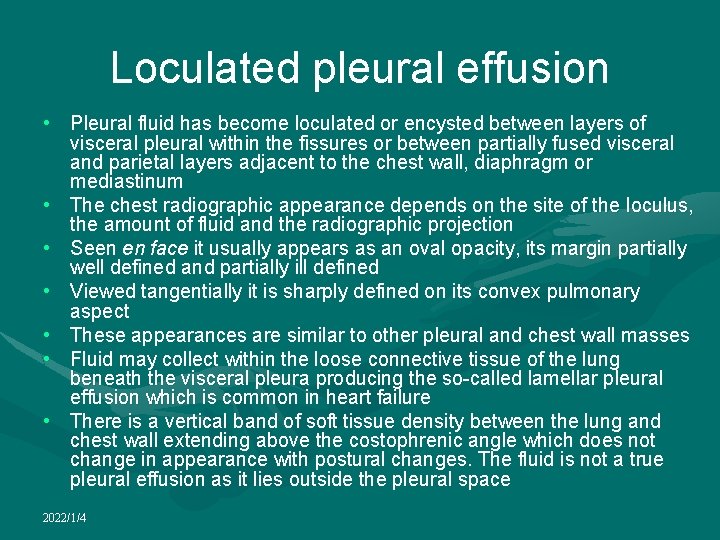
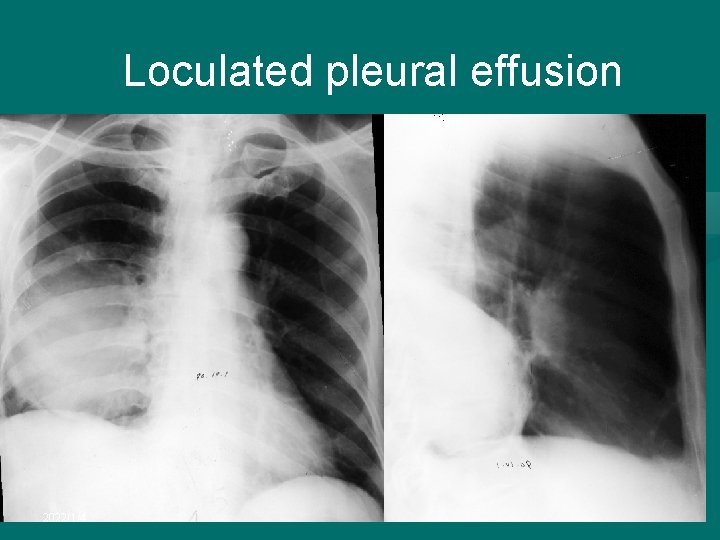
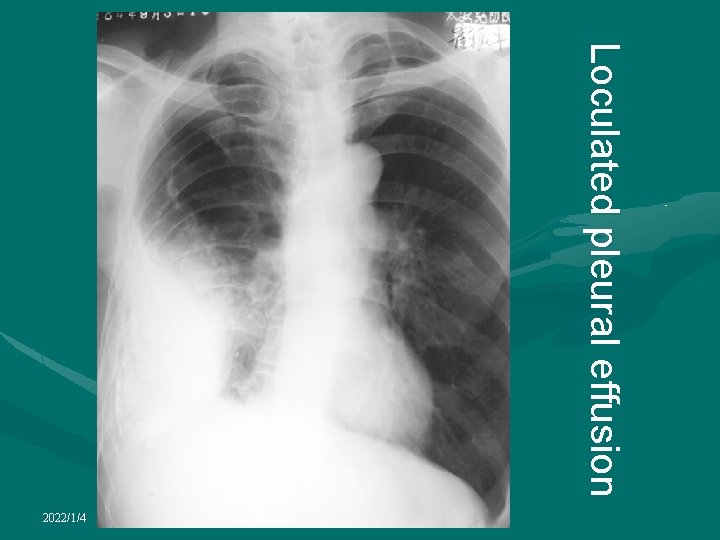
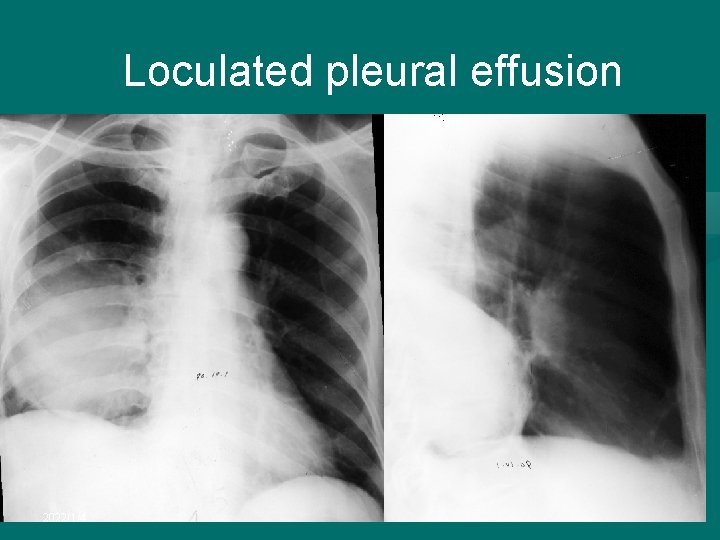
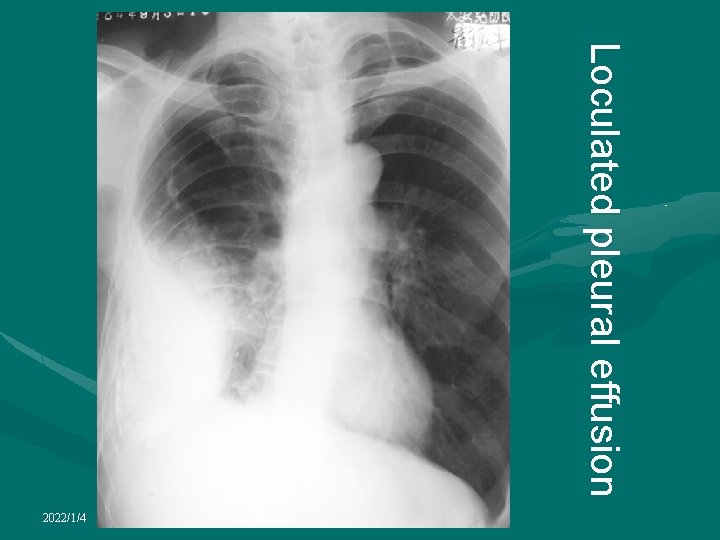
Loculated pleural effusion • Pleural fluid has become loculated or encysted between layers of visceral pleural within the fissures or between partially fused visceral and parietal layers adjacent to the chest wall, diaphragm or mediastinum • The chest radiographic appearance depends on the site of the loculus, the amount of fluid and the radiographic projection • Seen en face it usually appears as an oval opacity, its margin partially well defined and partially ill defined • Viewed tangentially it is sharply defined on its convex pulmonary aspect • These appearances are similar to other pleural and chest wall masses • Fluid may collect within the loose connective tissue of the lung beneath the visceral pleura producing the so-called lamellar pleural effusion which is common in heart failure • There is a vertical band of soft tissue density between the lung and chest wall extending above the costophrenic angle which does not change in appearance with postural changes. The fluid is not a true pleural effusion as it lies outside the pleural space 2022/1/4
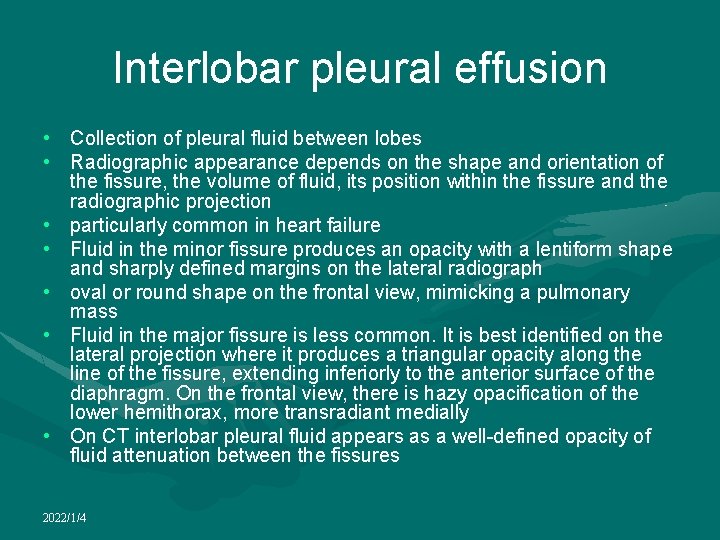
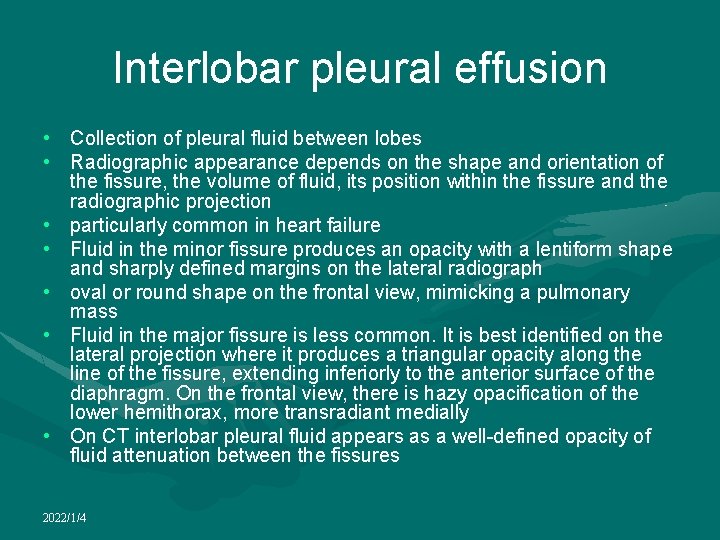
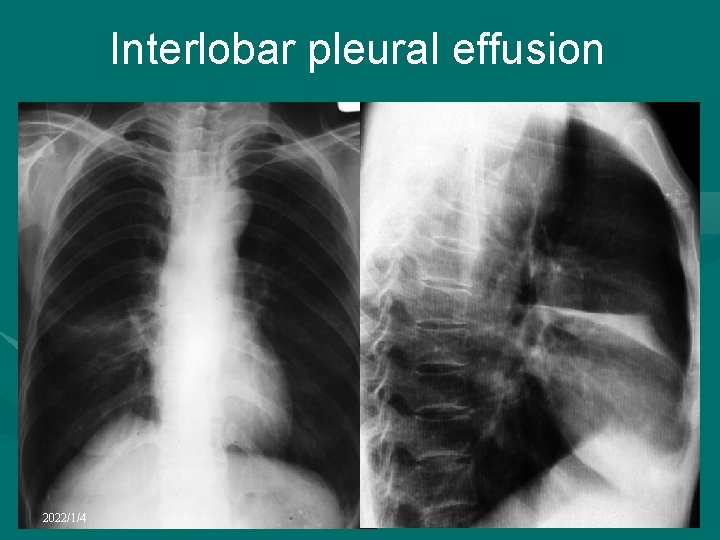
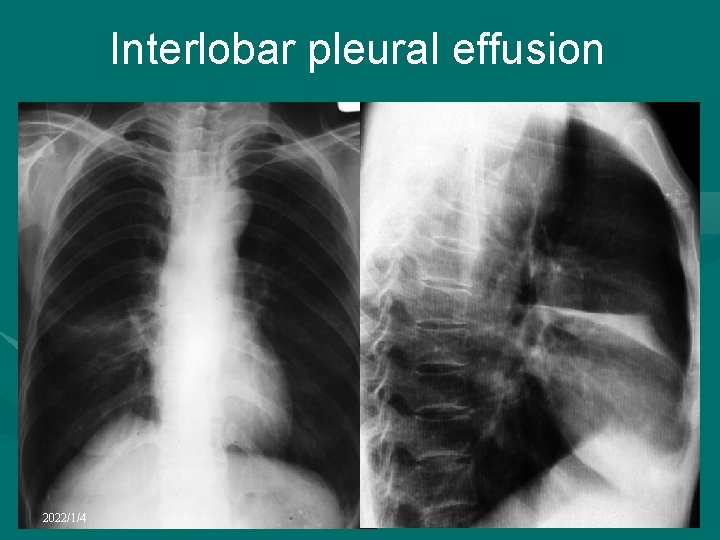
Interlobar pleural effusion • Collection of pleural fluid between lobes • Radiographic appearance depends on the shape and orientation of the fissure, the volume of fluid, its position within the fissure and the radiographic projection • particularly common in heart failure • Fluid in the minor fissure produces an opacity with a lentiform shape and sharply defined margins on the lateral radiograph • oval or round shape on the frontal view, mimicking a pulmonary mass • Fluid in the major fissure is less common. It is best identified on the lateral projection where it produces a triangular opacity along the line of the fissure, extending inferiorly to the anterior surface of the diaphragm. On the frontal view, there is hazy opacification of the lower hemithorax, more transradiant medially • On CT interlobar pleural fluid appears as a well-defined opacity of fluid attenuation between the fissures 2022/1/4
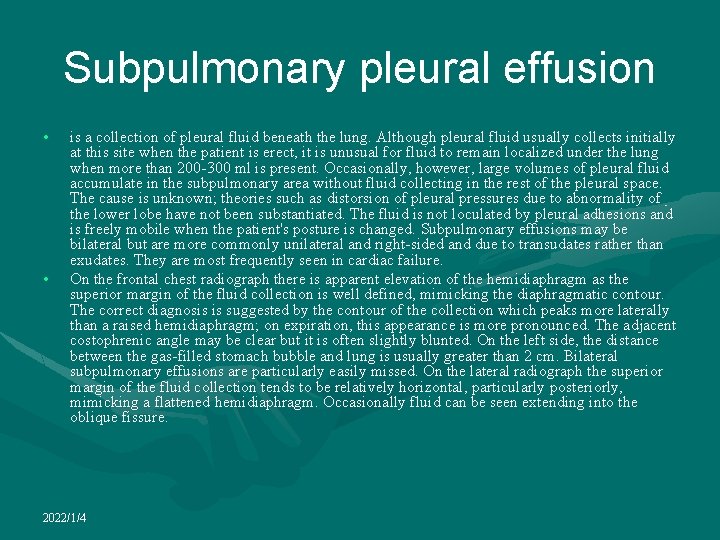
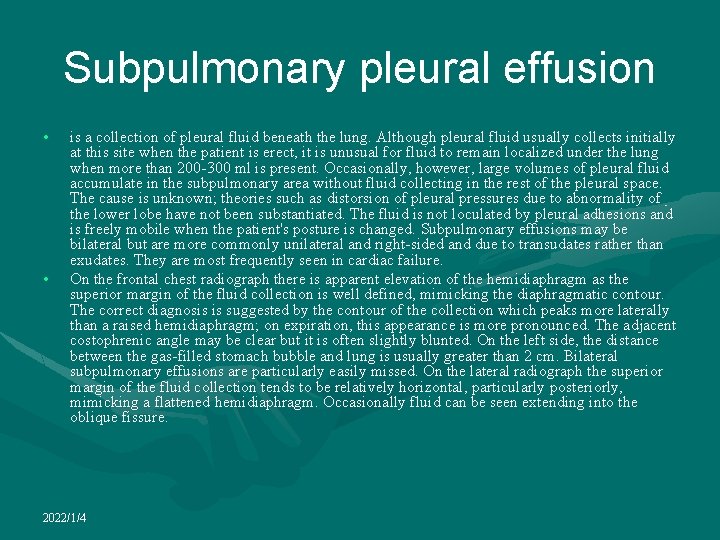
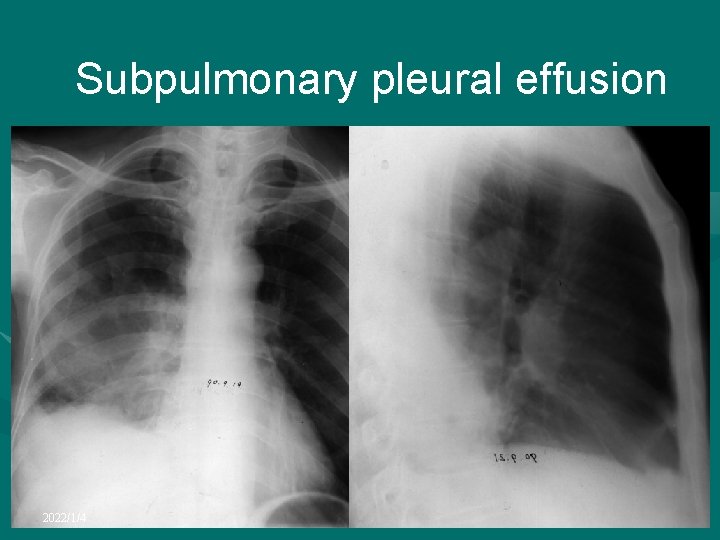
Subpulmonary pleural effusion • • is a collection of pleural fluid beneath the lung. Although pleural fluid usually collects initially at this site when the patient is erect, it is unusual for fluid to remain localized under the lung when more than 200 -300 ml is present. Occasionally, however, large volumes of pleural fluid accumulate in the subpulmonary area without fluid collecting in the rest of the pleural space. The cause is unknown; theories such as distorsion of pleural pressures due to abnormality of the lower lobe have not been substantiated. The fluid is not loculated by pleural adhesions and is freely mobile when the patient's posture is changed. Subpulmonary effusions may be bilateral but are more commonly unilateral and right-sided and due to transudates rather than exudates. They are most frequently seen in cardiac failure. On the frontal chest radiograph there is apparent elevation of the hemidiaphragm as the superior margin of the fluid collection is well defined, mimicking the diaphragmatic contour. The correct diagnosis is suggested by the contour of the collection which peaks more laterally than a raised hemidiaphragm; on expiration, this appearance is more pronounced. The adjacent costophrenic angle may be clear but it is often slightly blunted. On the left side, the distance between the gas-filled stomach bubble and lung is usually greater than 2 cm. Bilateral subpulmonary effusions are particularly easily missed. On the lateral radiograph the superior margin of the fluid collection tends to be relatively horizontal, particularly posteriorly, mimicking a flattened hemidiaphragm. Occasionally fluid can be seen extending into the oblique fissure. 2022/1/4
Loculated pleural effusion 2022/1/4
Loculated pleural effusion 2022/1/4
Interlobar pleural effusion 2022/1/4

Interlobar pleural effusion 2022/1/4
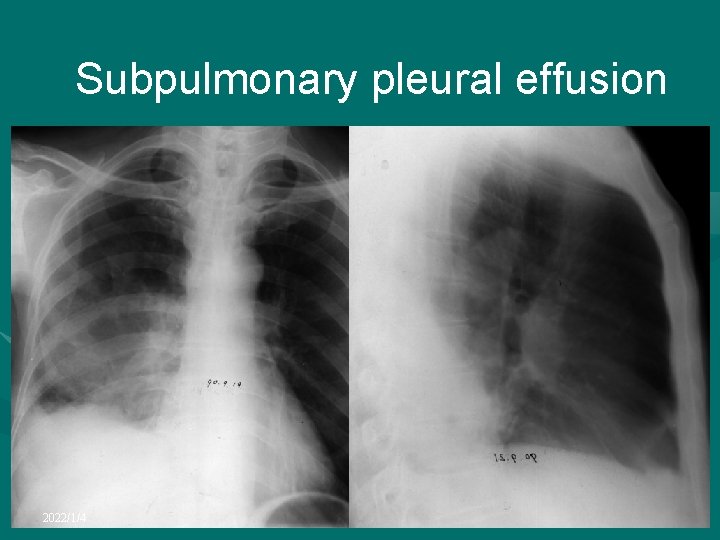
Subpulmonary pleural effusion 2022/1/4
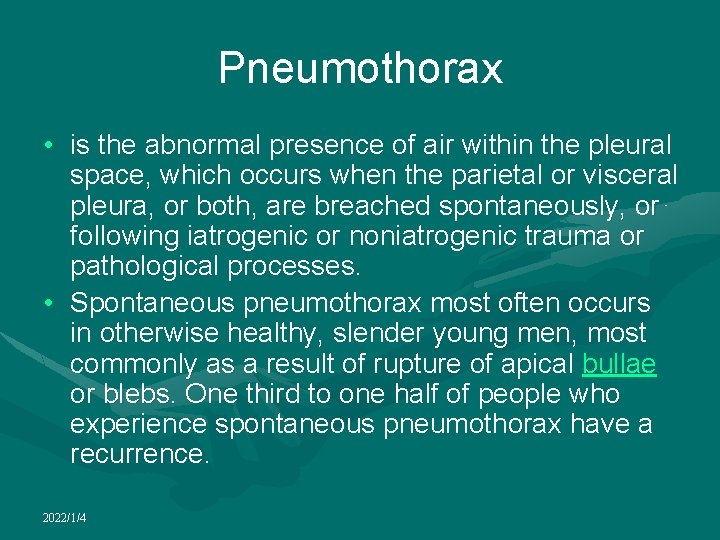
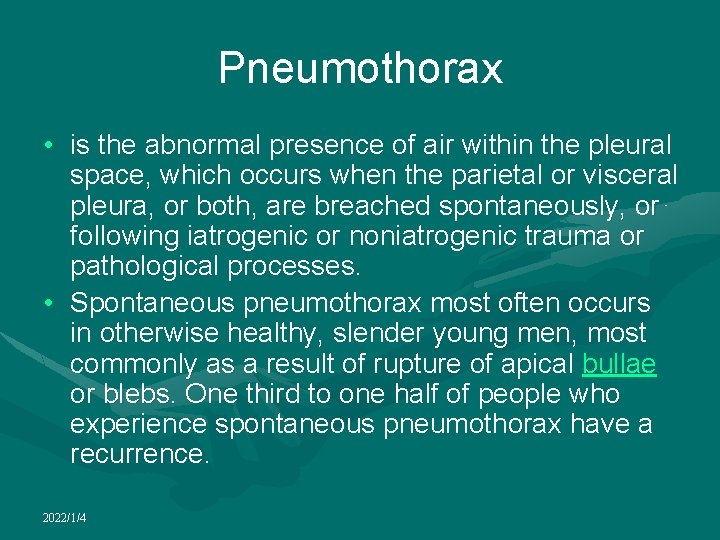
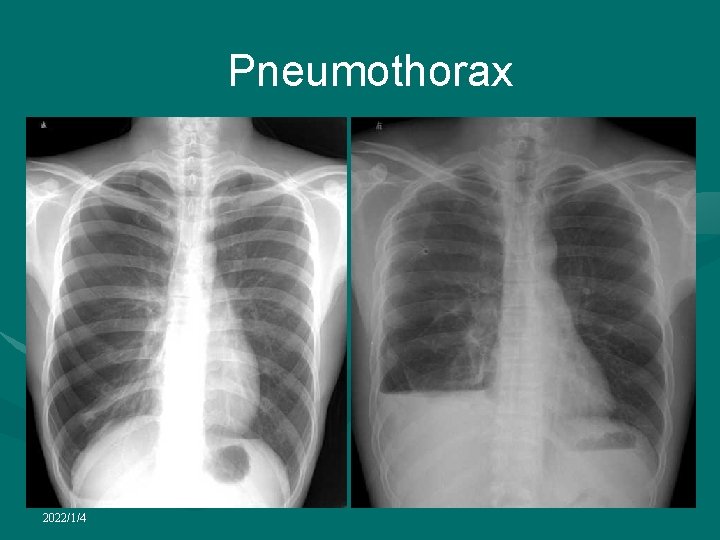
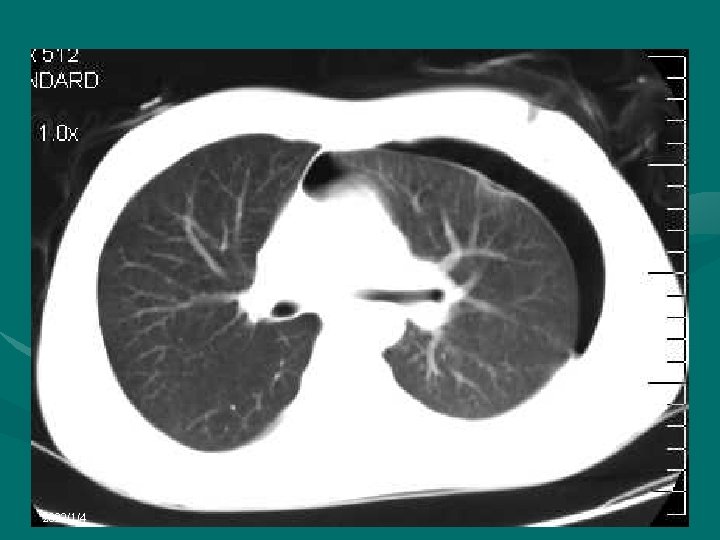
Pneumothorax • is the abnormal presence of air within the pleural space, which occurs when the parietal or visceral pleura, or both, are breached spontaneously, or following iatrogenic or noniatrogenic trauma or pathological processes. • Spontaneous pneumothorax most often occurs in otherwise healthy, slender young men, most commonly as a result of rupture of apical bullae or blebs. One third to one half of people who experience spontaneous pneumothorax have a recurrence. 2022/1/4
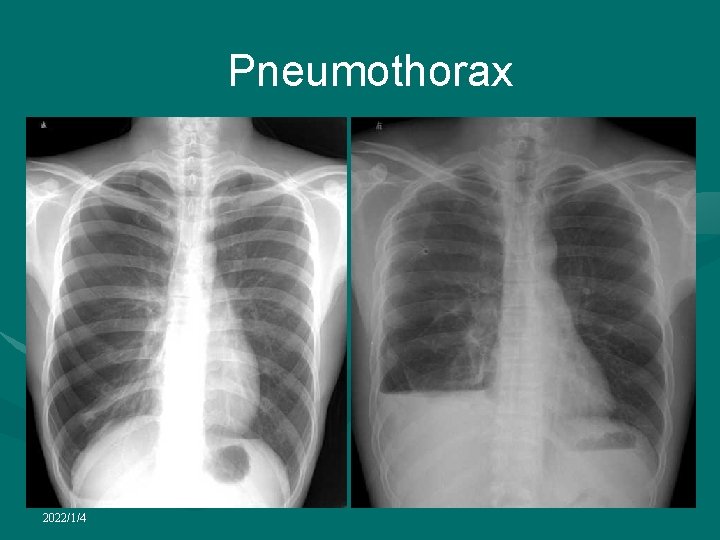
Pneumothorax 2022/1/4
2022/1/4
Pleural thickening • May follow organization of a variety of inflammatory processes involving the pleura • Include infective pleural effusions, empyema, hemothorax, occupational exposure to asbestos or talc, rheumatoid lung disease, radiation therapy and drugs • May also occur as a result of infiltration of the pleura by various malignant tumors, especially mesothelioma and metastatic adenocarcinoma • May be uni- or bilateral, diffuse or localized and may be calcified 2022/1/4
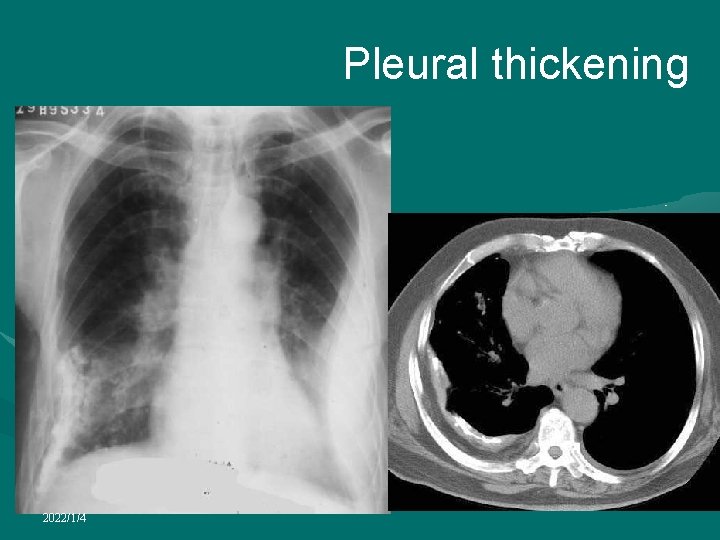
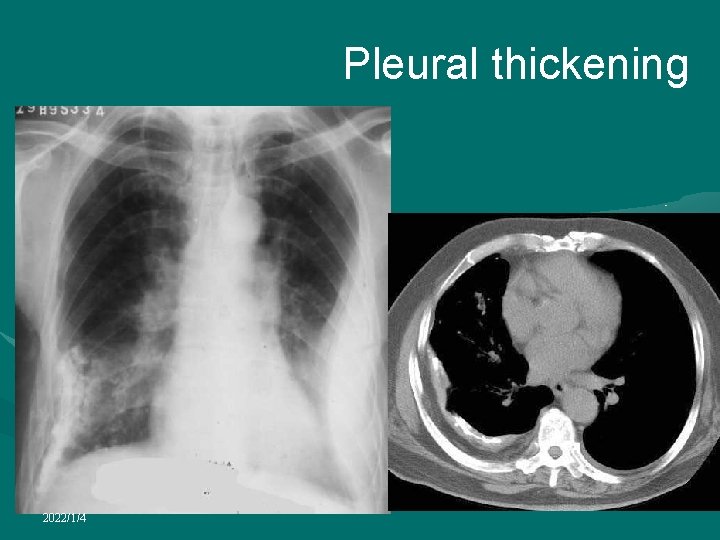
Pleural thickening • On the chest radiograph the changes predominantly affect the dependent areas with blunting of the costophrenic angle • Extensive pleural thickening produces volume loss and a veil-like reduction in transradiancy of the hemithorax • There is a soft tissue density medial to and paralleling the chest wall with a well-defined inner margin • There may be extension into the fissures which appear thickened 2022/1/4
Pleural thickening • CT is much more sensitive in detecting pleural thickening which is seen as a layer of soft tissue density between the chest wall and lungs • Thickening of as little as 12 mm can be detected with HRCT • best assessed immediately internal to the ribs where there is normally no detectable soft tissue • Between the ribs the normal pleura and innermost intercostal muscle produce a thin line which should not be mistaken for pleural thickening • In the paravertebral region, any thickening of the pleural line is abnormal • In many diseases causing pleural thickening the layer of extrapleural fat between parietal pleura and chest wall is increased, allowing a subtle degree of thickening to be detected, especially with HRCT 2022/1/4

Pleural thickening • The distribution and shape of pleural thickening as determined by CT are useful for differentiating between benign and malignant causes of pleural thickening • The most useful signs in predicting the presence of malignancy are circumferential thickening, nodularity, thickening of greater than 1 cm and involvement of the mediastinal pleura • Localized pleural thickening often occurs at the lung apices with increasing age, forming an apical cap • This may be uni- or bilateral and is usually of homogeneous, soft tissue density, usually less than 5 mm thick, with a well-defined inferior margin 2022/1/4
Pleural thickening 2022/1/4

Pleural thickening 2022/1/4
 E e e poem
E e e poem Xiang yu liu bang
Xiang yu liu bang Liu xiang
Liu xiang Liu xiang weightlifter
Liu xiang weightlifter Xiang yang liu
Xiang yang liu Liu xiang
Liu xiang Frc control system
Frc control system Alex liu cecilia liu
Alex liu cecilia liu Líu líu lo lo ta ca hát say sưa
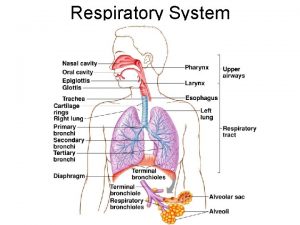
Líu líu lo lo ta ca hát say sưa Respiratory zone of the respiratory system
Respiratory zone of the respiratory system Disease respiratory
Disease respiratory Bharathi viswanathan
Bharathi viswanathan Chengxiang zhai
Chengxiang zhai Xiang cheng mit
Xiang cheng mit Morrp
Morrp Cheng xiang zhai
Cheng xiang zhai Cheng xiang zhai
Cheng xiang zhai Cheng xiang zhai
Cheng xiang zhai Yongqing xiang
Yongqing xiang Xiang su
Xiang su Perfume xia xiang
Perfume xia xiang Cheng xiang zhai
Cheng xiang zhai Music producer job description
Music producer job description Vex xiang
Vex xiang Vex xiang
Vex xiang Cheng xiang zhai
Cheng xiang zhai Pu tao you
Pu tao you Max pattern and closed pattern
Max pattern and closed pattern Spiral pattern with 2 deltals and many forms of pattern.
Spiral pattern with 2 deltals and many forms of pattern. Nfrequent
Nfrequent Pattern and pattern classes in image processing
Pattern and pattern classes in image processing Support implementation
Support implementation Fhir imaging study
Fhir imaging study Spie medical imaging
Spie medical imaging Seaview ocean imaging
Seaview ocean imaging Is sentara a nonprofit organization
Is sentara a nonprofit organization Live cell imaging ppt
Live cell imaging ppt Sira imaging
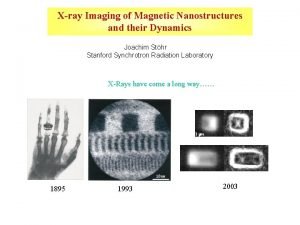
Sira imaging X ray imaging
X ray imaging Wittgenstein picture theory
Wittgenstein picture theory Sami haims
Sami haims Biomedical imaging
Biomedical imaging Chapter 42 extraoral imaging
Chapter 42 extraoral imaging Velocity map imaging
Velocity map imaging Medical terminology in radiology
Medical terminology in radiology Digital imaging terminology
Digital imaging terminology Spectral imaging
Spectral imaging Velocity map imaging
Velocity map imaging Echo planar imaging
Echo planar imaging Translate
Translate Hardware independent imaging
Hardware independent imaging Medical imaging software
Medical imaging software Veterinary imaging associates
Veterinary imaging associates Gabriela barreto lemos
Gabriela barreto lemos Nsi2000
Nsi2000 Chester f. carlson
Chester f. carlson Pulse inversion harmonic imaging
Pulse inversion harmonic imaging Global imaging systems inc
Global imaging systems inc Basic principles of the bitewing technique include the
Basic principles of the bitewing technique include the Prestage enrollment
Prestage enrollment Imaging near redwood city
Imaging near redwood city Optical imaging
Optical imaging Velocity map imaging
Velocity map imaging Prompt gamma imaging
Prompt gamma imaging Salt for concave mirrors
Salt for concave mirrors Digital ultrasonic diagnostic imaging system
Digital ultrasonic diagnostic imaging system Ultrasound imaging
Ultrasound imaging Nuance document imaging
Nuance document imaging Digital color imaging
Digital color imaging Corlumina
Corlumina Ppmc diagnostic imaging
Ppmc diagnostic imaging Coulomb explosion
Coulomb explosion Body quadrants and organs
Body quadrants and organs Windows imaging component
Windows imaging component Imaging biomedico
Imaging biomedico Magnetic resonance imaging nait
Magnetic resonance imaging nait Chapter 39 digital imaging film and radiographs
Chapter 39 digital imaging film and radiographs Digital imagery definition
Digital imagery definition Medical imaging workstations
Medical imaging workstations Do reptiles show up on thermal imaging
Do reptiles show up on thermal imaging Ohiohealth berger hospital mammography circleville
Ohiohealth berger hospital mammography circleville Whole slide imaging
Whole slide imaging Cytopeia
Cytopeia Ishan imaging centre
Ishan imaging centre Tissue doppler imaging
Tissue doppler imaging Ucsf nikon imaging center
Ucsf nikon imaging center Echo planar imaging
Echo planar imaging Is2000 the advanced imaging solution
Is2000 the advanced imaging solution Fundamentals of digital imaging
Fundamentals of digital imaging Picture perfect imaging
Picture perfect imaging Imaging lifecycle services
Imaging lifecycle services Velocity map imaging
Velocity map imaging Focused imaging learning
Focused imaging learning Brain imaging
Brain imaging Diagnostic imaging
Diagnostic imaging Blackett laboratory
Blackett laboratory Birads staging
Birads staging Brain stem on mri
Brain stem on mri Mental imagery
Mental imagery Princeton imaging and analysis center
Princeton imaging and analysis center Infinite imaging
Infinite imaging Broad based protrusion
Broad based protrusion Amy nau
Amy nau Digital imaging artist
Digital imaging artist Affordable hyperspectral imaging
Affordable hyperspectral imaging Kodak 9000 3d price
Kodak 9000 3d price Brong-kog-rah-fee
Brong-kog-rah-fee Uwe diagnostic imaging
Uwe diagnostic imaging Pet imaging
Pet imaging Abbe imaging experiment
Abbe imaging experiment Amanda dermer
Amanda dermer Microsanj
Microsanj Fourier transform
Fourier transform Chapter 39 digital imaging film and radiographs
Chapter 39 digital imaging film and radiographs Nuclear imaging techniques
Nuclear imaging techniques Giuseppe bonifazi
Giuseppe bonifazi Astronomy science olympiad 2020
Astronomy science olympiad 2020 Direct imaging subsystem
Direct imaging subsystem Advantages of paralleling technique
Advantages of paralleling technique Describe in detail
Describe in detail Windows image acquisition service
Windows image acquisition service Mobile imaging solutions
Mobile imaging solutions Velocity map imaging
Velocity map imaging