Imaging of Skull Base CSF leaks in the
Imaging of Skull Base CSF leaks in the Setting of Idiopathic Intracranial Hypertension: Pearls and Pitfalls ASNR 2016 ; e. Ed. E-140 Reddy MN, Baugnon KL, Aiken AH, Hudgins PA Dept. of Radiology and Imaging Sciences Division of Neuroradiology, Head & Neck
Disclosures § MN Reddy : None § KL Baugnon : None § AH Aiken : None § PA Hudgins : None
Purpose § Review pathophysiology of Idiopathic Intracranial Hypertension (IIH) & skull base cerebrospinal fluid (CSF) leaks § Discuss ideal imaging work up § Illustrate characteristic imaging findings § Focus on potential pitfalls § Describe what the treating physician needs to know
IIH § Headache Syndrome caused by ↑CSF pressure w/o underlying cause (such as a mass or hydrocephalus) § Prevalence: 8. 6 cases/100, 000 § Probable increasing incidence of IIH given rise in obesity § F: M = 4: 1 – 15: 1 Obese women of childbearing age § Strong correlation w/ obesity (> 70% IIH adults) § Diagnostic criteria: § International Classification of Headache Disorders : 2 nd Edition § Originally classified by Dandy in 1937 : 2002 version § PTCS Criteria Hoffmann, J & Goadsby PJ. "Update on intracranial hypertension and hypotension. " 2013. Current Opinion in Neurology 26 (3): 240 -247.
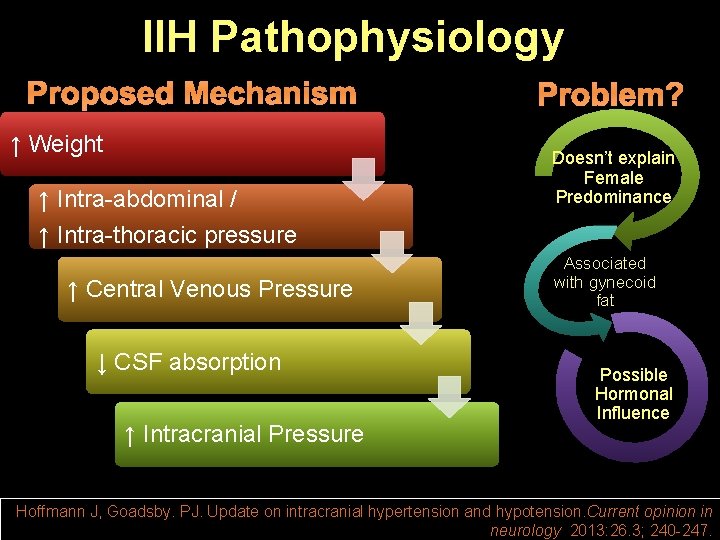
IIH Pathophysiology ↑ Weight ↑ Intra-abdominal / Doesn’t explain Female Predominance ↑ Intra-thoracic pressure ↑ Central Venous Pressure ↓ CSF absorption ↑ Intracranial Pressure Associated with gynecoid fat Possible Hormonal Influence Hoffmann J, Goadsby. PJ. Update on intracranial hypertension and hypotension. Current opinion in neurology 2013: 26. 3; 240 -247.
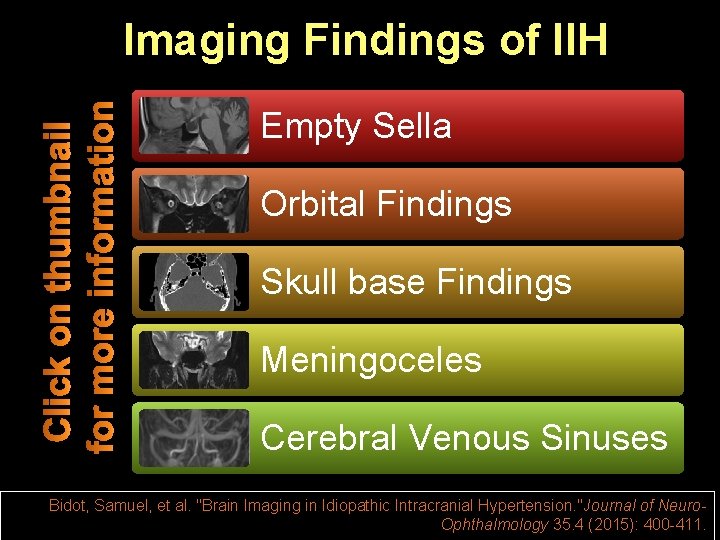
Imaging Findings of IIH Empty Sella Orbital Findings Skull base Findings Meningoceles Cerebral Venous Sinuses Bidot, Samuel, et al. "Brain Imaging in Idiopathic Intracranial Hypertension. "Journal of Neuro. Ophthalmology 35. 4 (2015): 400 -411.
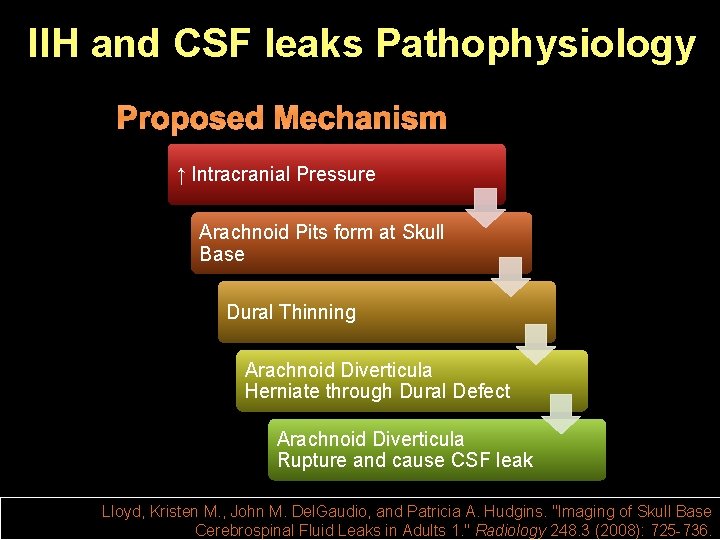
IIH and CSF leaks Pathophysiology ↑ Intracranial Pressure Arachnoid Pits form at Skull Base Dural Thinning Arachnoid Diverticula Herniate through Dural Defect Arachnoid Diverticula Rupture and cause CSF leak Lloyd, Kristen M. , John M. Del. Gaudio, and Patricia A. Hudgins. "Imaging of Skull Base Cerebrospinal Fluid Leaks in Adults 1. " Radiology 248. 3 (2008): 725 -736.
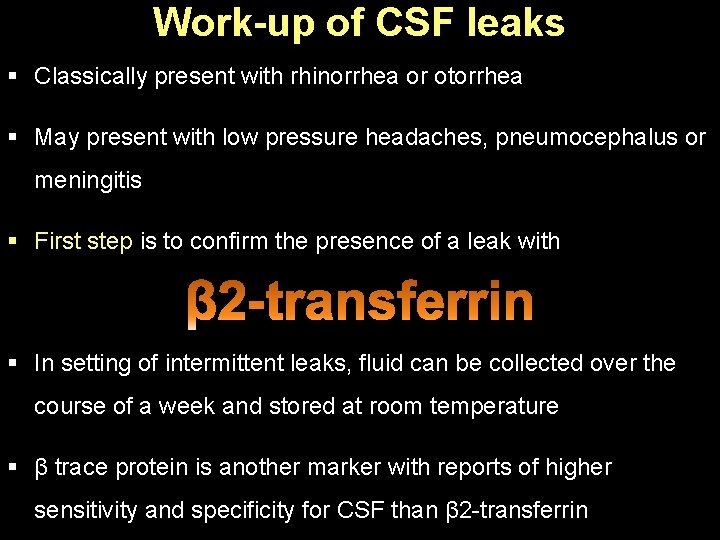
Work-up of CSF leaks § Classically present with rhinorrhea or otorrhea § May present with low pressure headaches, pneumocephalus or meningitis § First step is to confirm the presence of a leak with § In setting of intermittent leaks, fluid can be collected over the course of a week and stored at room temperature § β trace protein is another marker with reports of higher sensitivity and specificity for CSF than β 2 -transferrin
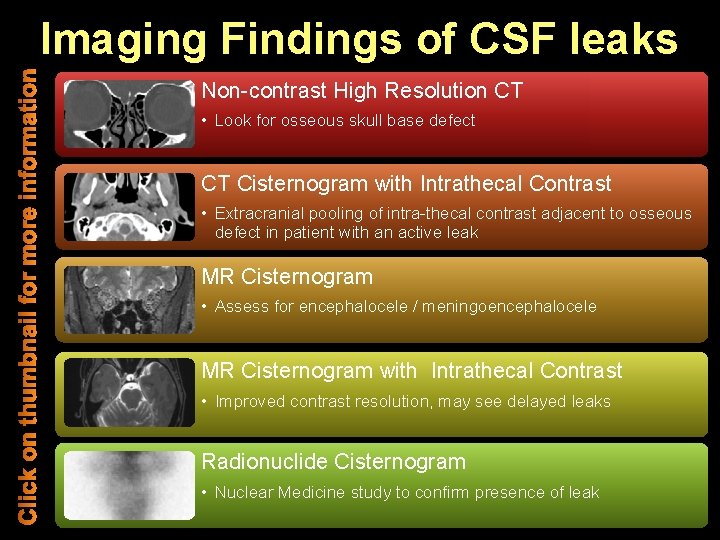
Imaging Findings of CSF leaks Non-contrast High Resolution CT • Look for osseous skull base defect CT Cisternogram with Intrathecal Contrast • Extracranial pooling of intra-thecal contrast adjacent to osseous defect in patient with an active leak MR Cisternogram • Assess for encephalocele / meningoencephalocele MR Cisternogram with Intrathecal Contrast • Improved contrast resolution, may see delayed leaks Radionuclide Cisternogram • Nuclear Medicine study to confirm presence of leak
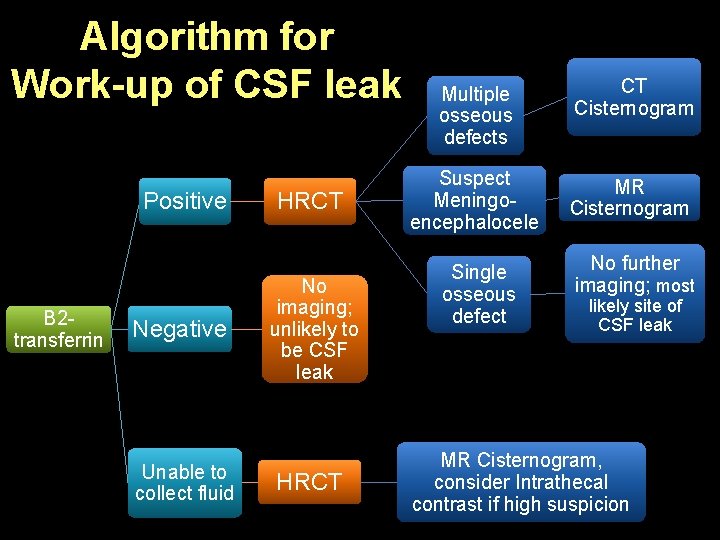
Algorithm for Work-up of CSF leak Positive B 2 transferrin Negative Unable to collect fluid HRCT No imaging; unlikely to be CSF leak HRCT Multiple osseous defects Suspect Meningoencephalocele Single osseous defect CT Cisternogram MR Cisternogram No further imaging; most likely site of CSF leak MR Cisternogram, consider Intrathecal contrast if high suspicion
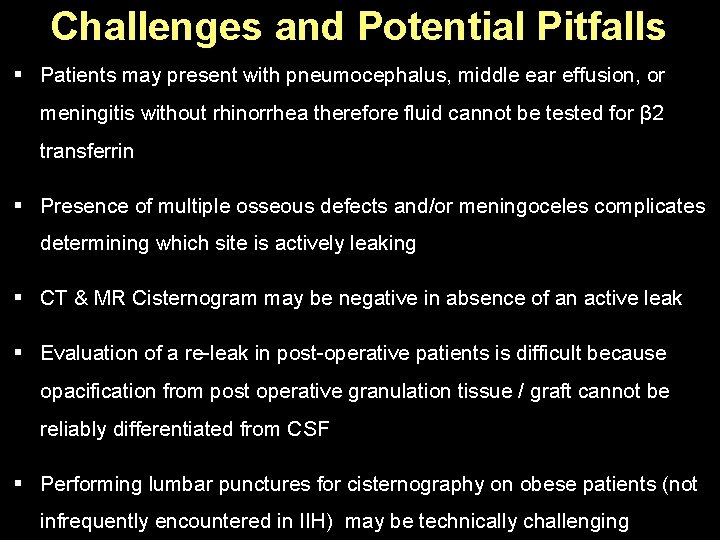
Challenges and Potential Pitfalls § Patients may present with pneumocephalus, middle ear effusion, or meningitis without rhinorrhea therefore fluid cannot be tested for β 2 transferrin § Presence of multiple osseous defects and/or meningoceles complicates determining which site is actively leaking § CT & MR Cisternogram may be negative in absence of an active leak § Evaluation of a re-leak in post-operative patients is difficult because opacification from post operative granulation tissue / graft cannot be reliably differentiated from CSF § Performing lumbar punctures for cisternography on obese patients (not infrequently encountered in IIH) may be technically challenging
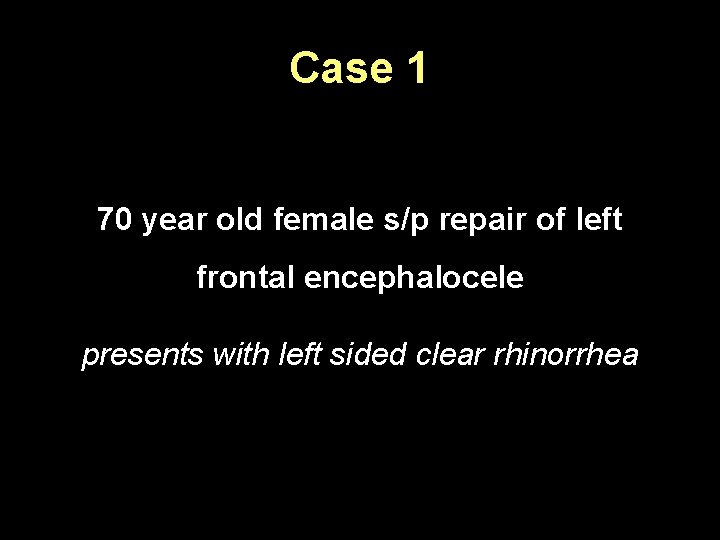
Case 1 70 year old female s/p repair of left frontal encephalocele presents with left sided clear rhinorrhea
Case 1 What would you do first? Test fluid for β 2 transferrin Positive What would you do next?
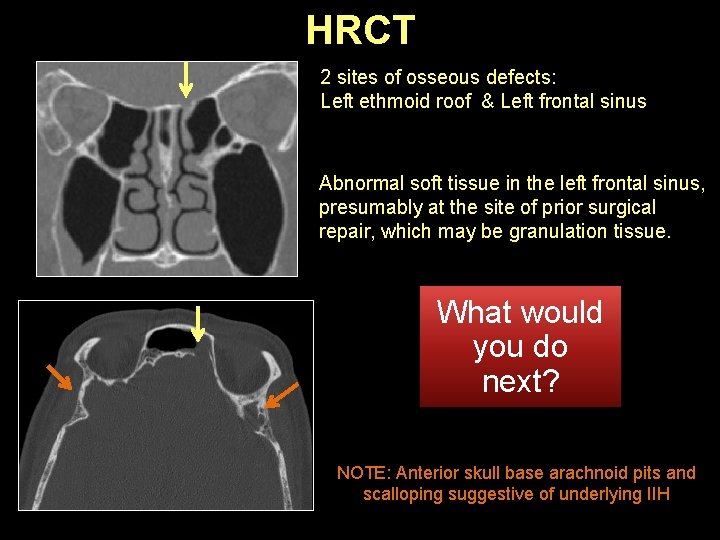
HRCT 2 sites of osseous defects: Left ethmoid roof & Left frontal sinus Abnormal soft tissue in the left frontal sinus, presumably at the site of prior surgical repair, which may be granulation tissue. What would you do next? NOTE: Anterior skull base arachnoid pits and scalloping suggestive of underlying IIH
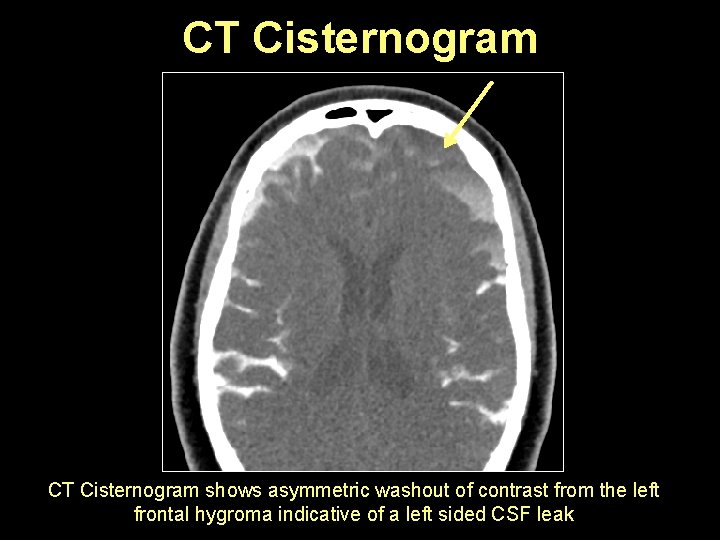
CT Cisternogram shows asymmetric washout of contrast from the left frontal hygroma indicative of a left sided CSF leak
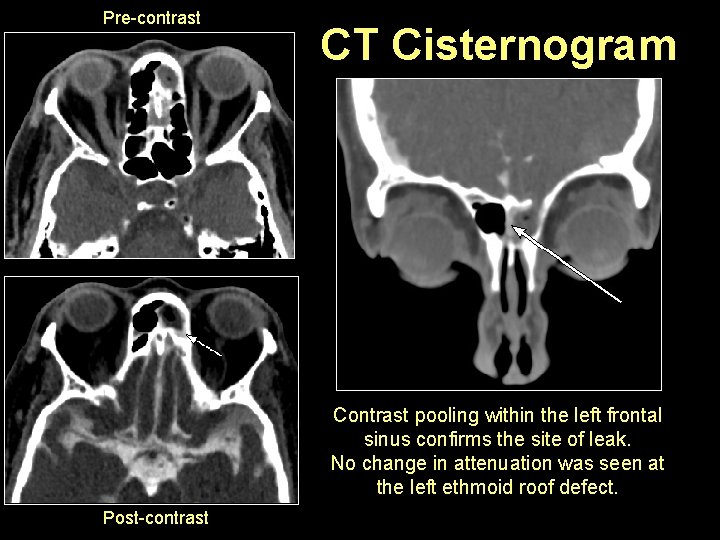
Pre-contrast CT Cisternogram Contrast pooling within the left frontal sinus confirms the site of leak. No change in attenuation was seen at the left ethmoid roof defect. Post-contrast
What the surgeon needs to know? § Patients with IIH may have multiple potential sites of leak on non-contrast HRCT due to predisposition to skull base defects § Not uncommon for patients to leak at a different location after one site is repaired § Must thoroughly assess the entire skull base, including tegmen, for possible sites of leak § Re-leak at the site of surgery is also possible and even more challenging to assess due to pre-existing granulation tissue § Important to compare pre and post contrast images side by side
Case 2 68 year old female presents with meningitis x 2 Intermittent rhinorrhea by history and bilateral middle ear effusions by exam
Case 2 What would you do first? Unable to collect fluid for β 2 -transferrin High suspicion for intermittent leak What would you do next?
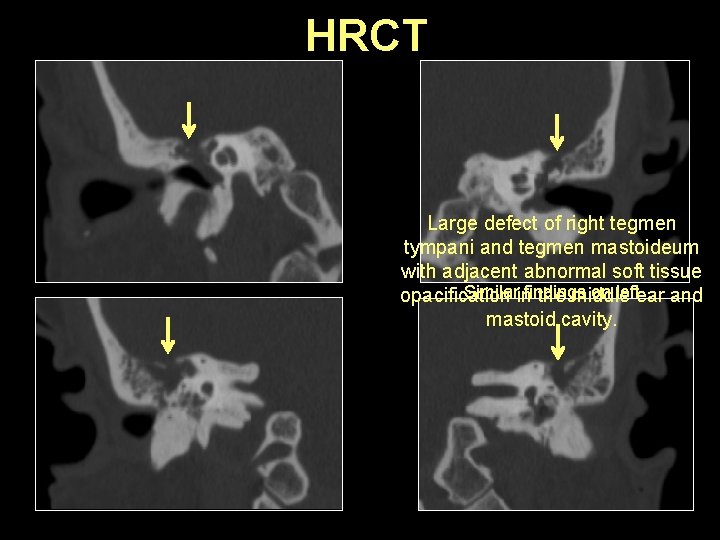
HRCT Large defect of right tegmen tympani and tegmen mastoideum with adjacent abnormal soft tissue Similar findings on left opacification in the middle ear and mastoid cavity.
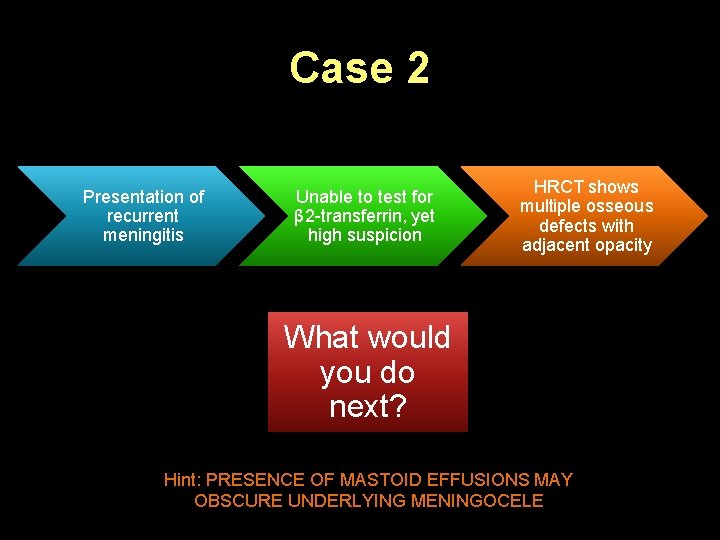
Case 2 Presentation of recurrent meningitis Unable to test for β 2 -transferrin, yet high suspicion HRCT shows multiple osseous defects with adjacent opacity What would you do next? Hint: PRESENCE OF MASTOID EFFUSIONS MAY OBSCURE UNDERLYING MENINGOCELE
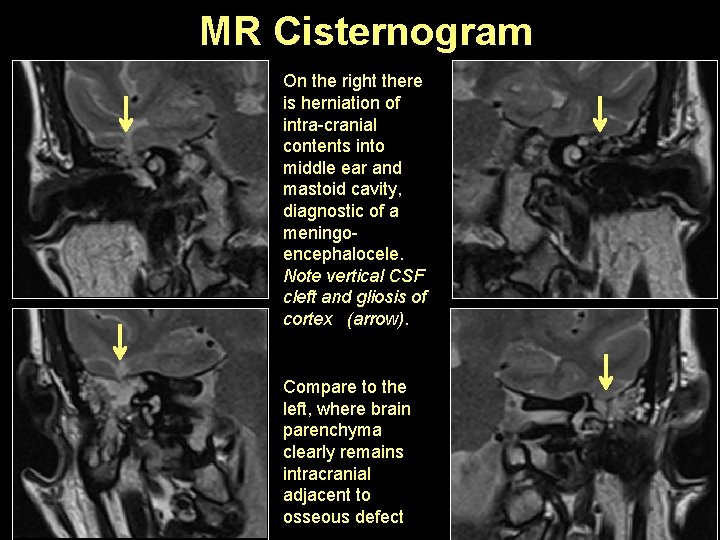
MR Cisternogram On the right there is herniation of intra-cranial contents into middle ear and mastoid cavity, diagnostic of a meningoencephalocele. Note vertical CSF cleft and gliosis of cortex (arrow). Compare to the left, where brain parenchyma clearly remains intracranial adjacent to osseous defect
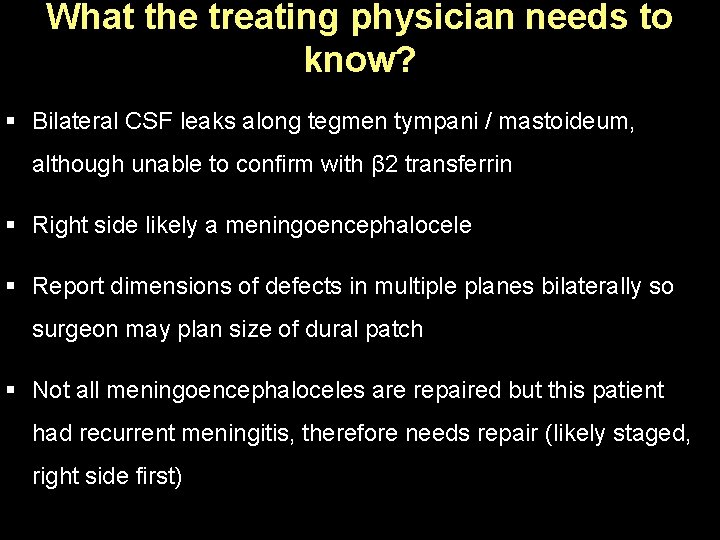
What the treating physician needs to know? § Bilateral CSF leaks along tegmen tympani / mastoideum, although unable to confirm with β 2 transferrin § Right side likely a meningoencephalocele § Report dimensions of defects in multiple planes bilaterally so surgeon may plan size of dural patch § Not all meningoencephaloceles are repaired but this patient had recurrent meningitis, therefore needs repair (likely staged, right side first)
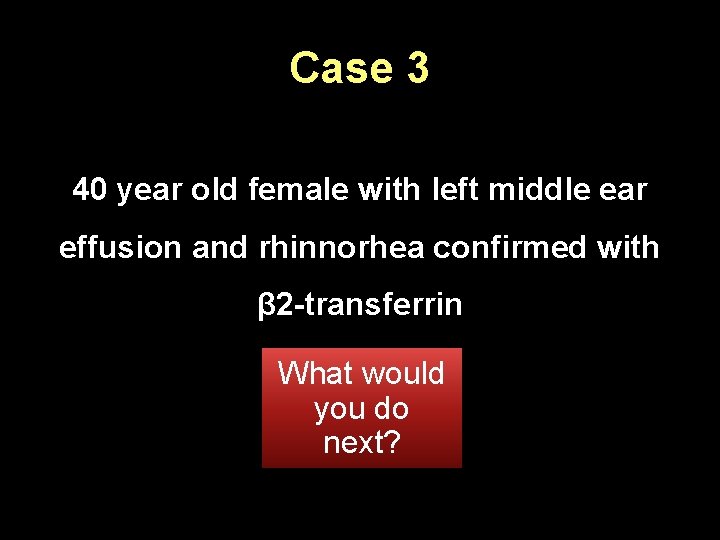
Case 3 40 year old female with left middle ear effusion and rhinnorhea confirmed with β 2 -transferrin What would you do next?
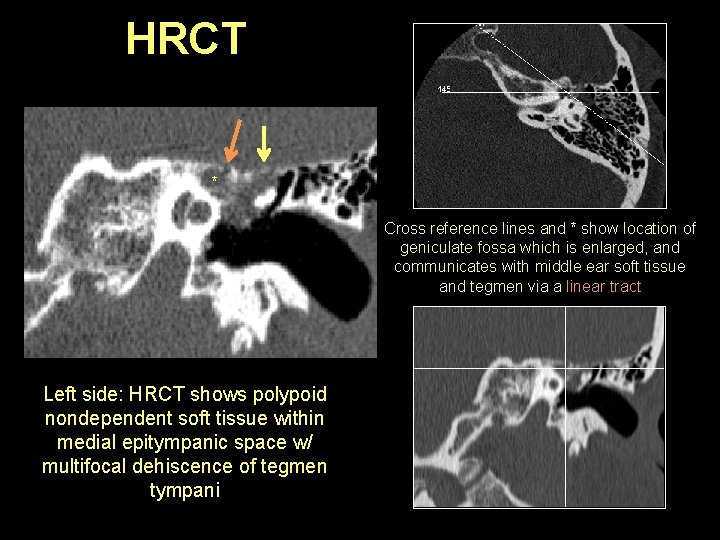
HRCT * Cross reference lines and * show location of geniculate fossa which is enlarged, and communicates with middle ear soft tissue and tegmen via a linear tract Left side: HRCT shows polypoid nondependent soft tissue within medial epitympanic space w/ multifocal dehiscence of tegmen tympani
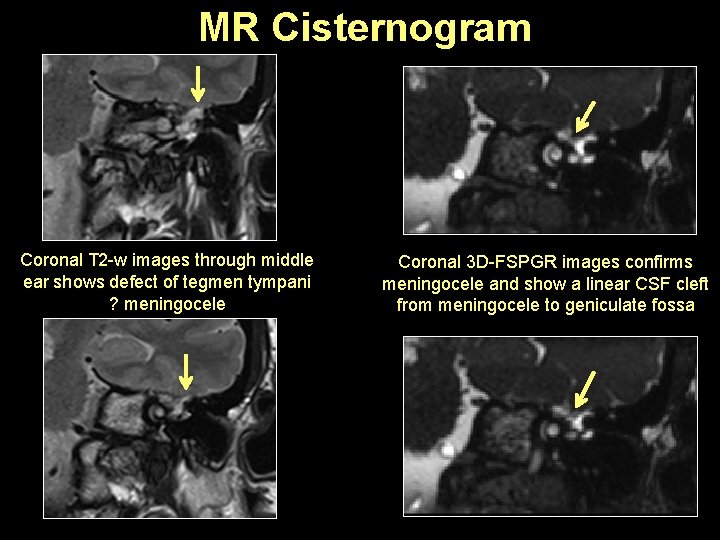
MR Cisternogram Coronal T 2 -w images through middle ear shows defect of tegmen tympani ? meningocele Coronal 3 D-FSPGR images confirms meningocele and show a linear CSF cleft from meningocele to geniculate fossa
What the surgeon needs to know? § Left middle ear cavity meningocele, small, with communication to geniculate fossa § In surgery, an active peri-geniculate CSF leak was found § Linear “clefts” or tracts of communication should be followed to determine complete extent of the meningocele § Thin section heavily T 2 w images (i. e. CISS, FIESTA, SPACE) helpful § Specify involvement of discrete structures such as facial nerve canal or semi-circular canals
Case 4 50 year old morbidly obese male with vision changes and clear rhinorrhea confirmed with β 2 -transferrin BMI 54 What would you do next?
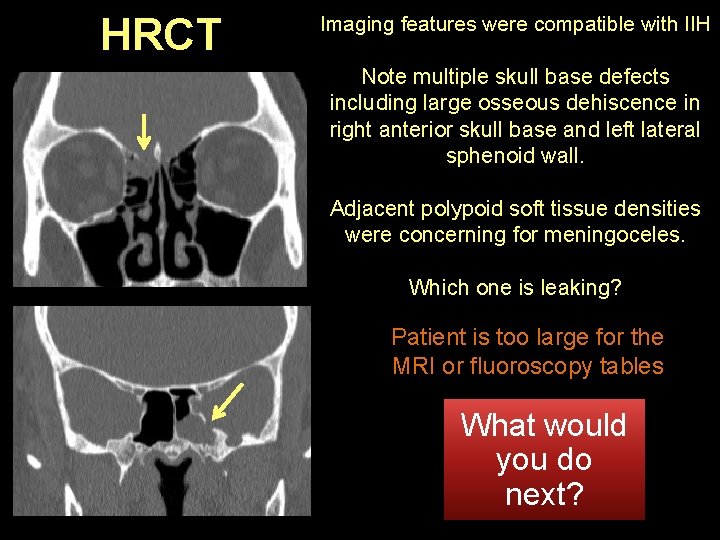
HRCT Imaging features were compatible with IIH Note multiple skull base defects including large osseous dehiscence in right anterior skull base and left lateral sphenoid wall. Adjacent polypoid soft tissue densities were concerning for meningoceles. Which one is leaking? Patient is too large for the MRI or fluoroscopy tables What would you do next?
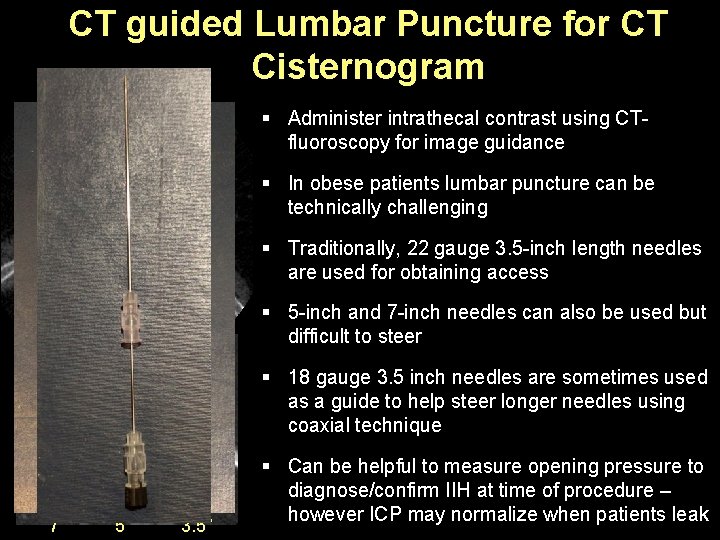
CT guided Lumbar Puncture for CT Cisternogram § Administer intrathecal contrast using CTfluoroscopy for image guidance § In obese patients lumbar puncture can be technically challenging § Traditionally, 22 gauge 3. 5 -inch length needles are used for obtaining access § 5 -inch and 7 -inch needles can also be used but difficult to steer § 18 gauge 3. 5 inch needles are sometimes used as a guide to help steer longer needles using coaxial technique 7” 5” 3. 5” § Can be helpful to measure opening pressure to diagnose/confirm IIH at time of procedure – however ICP may normalize when patients leak
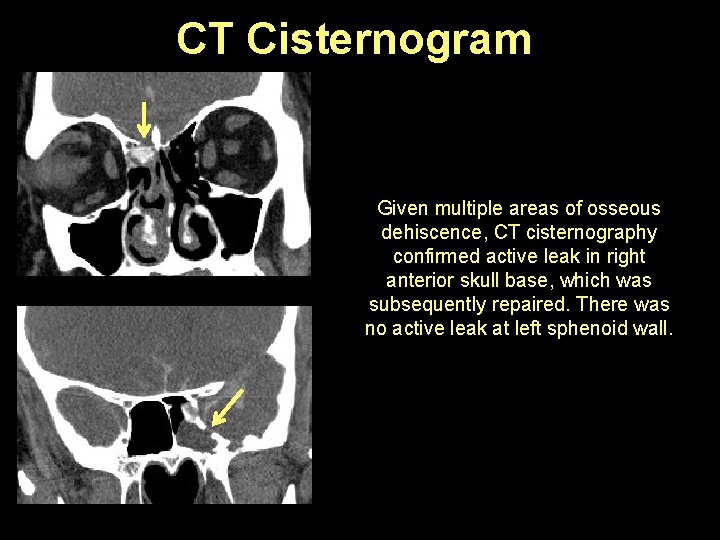
CT Cisternogram Given multiple areas of osseous dehiscence, CT cisternography confirmed active leak in right anterior skull base, which was subsequently repaired. There was no active leak at left sphenoid wall.
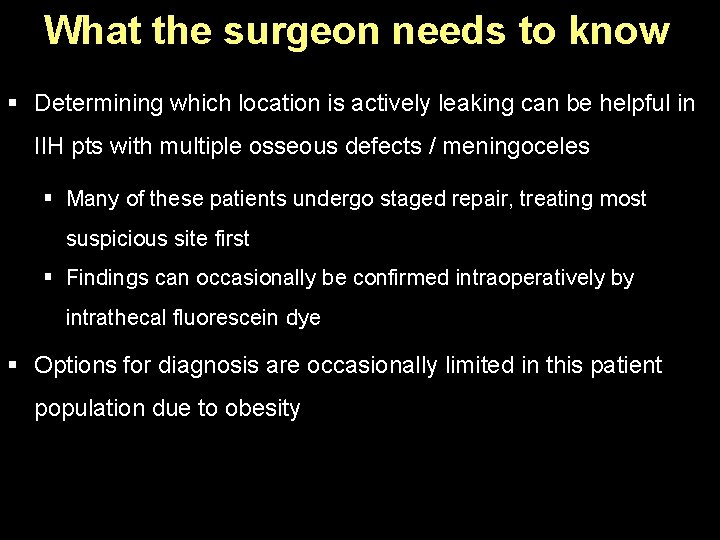
What the surgeon needs to know § Determining which location is actively leaking can be helpful in IIH pts with multiple osseous defects / meningoceles § Many of these patients undergo staged repair, treating most suspicious site first § Findings can occasionally be confirmed intraoperatively by intrathecal fluorescein dye § Options for diagnosis are occasionally limited in this patient population due to obesity
SUMMARY § IIH has characteristic radiologic features that can be seen on both CT and MRI imaging § Skull base CSF leaks without or with meningoceles are common complications of IIH but there are imaging pitfalls § Workup should start with β 2 transferrin testing and HRCT § CT / MR Cisternogram can be helpful when there are multiple potential sites of leak, suspected meningocele or intermittent leaks § Obesity can complicate imaging workup and diagnosis
SUMMARY § Surgeons need to know: § Presence of imaging features suggestive of IIH § Location and size of defects measured in multiple planes – scrutinize entire skull base including sinuses and mastoids § Anatomy of sinonasal cavity (i. e. nasal septal deviation, perforation, variants) for surgical planning / approach § Associated meningoencephalocele(s) § Site(s) which is (are) actively leaking § Entire course of meningocele tract (Heavily T 2 w images & CT)
- Slides: 34