Imaging Interpretation for the Comprehensive Eye Care Professional

- Slides: 69
Imaging Interpretation for the Comprehensive Eye Care Professional Blair Lonsberry, MS, OD, MEd. , FAAO Diplomate, American Board of Optometry Clinic Director and Professor of Optometry Pacific University College of Optometry blonsberry@pacificu. edu
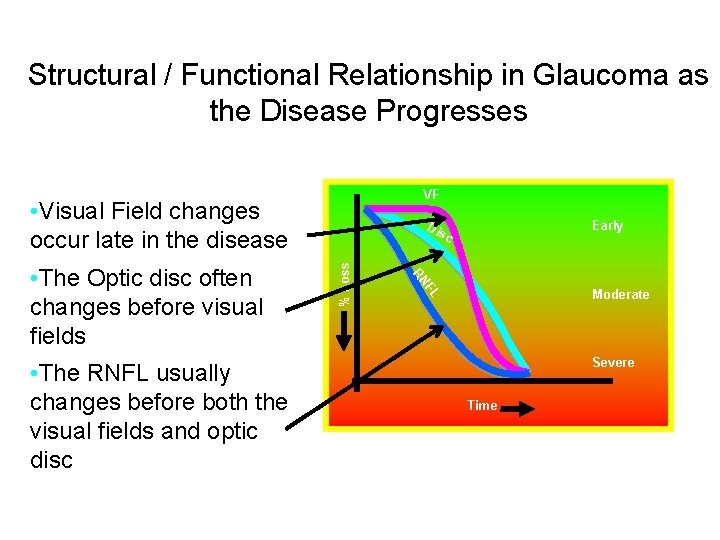
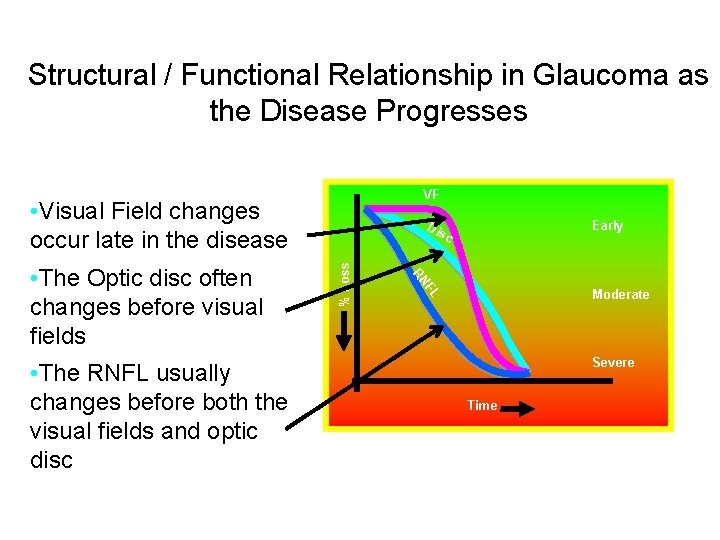
Structural / Functional Relationship in Glaucoma as the Disease Progresses VF • Visual Field changes occur late in the disease % Loss Moderate L • The RNFL usually changes before both the visual fields and optic disc Early c F RN • The Optic disc often changes before visual fields Dis Severe Time
Clinical Exam of the Optic Nerve Head Utility and Limitations • Disc exam at the first visit – normal or abnormal? – Disc exams are subjective, or at best semiquantitative – The wide variety of disc appearances requires long experience and expert judgment to separate normal from abnormal – Disc diameter must be taken into account • Disc exam to assess change – Unless stereoscopic photographs are taken and compared over time, the ability of a clinician to
OCT: The Basics 4
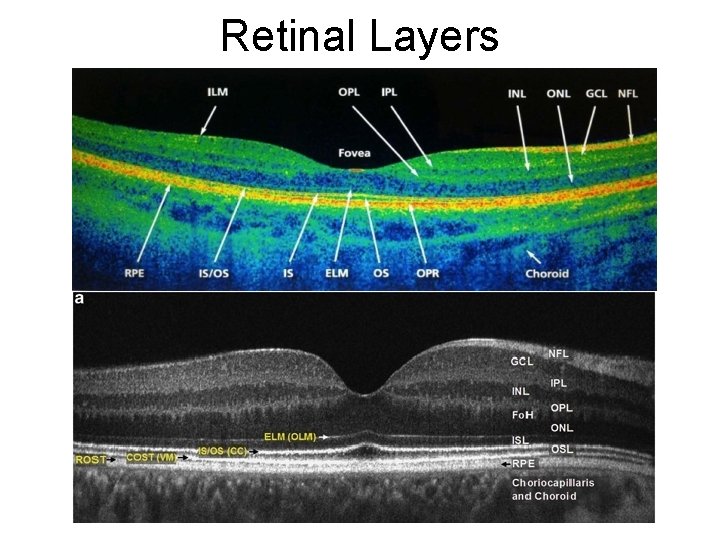
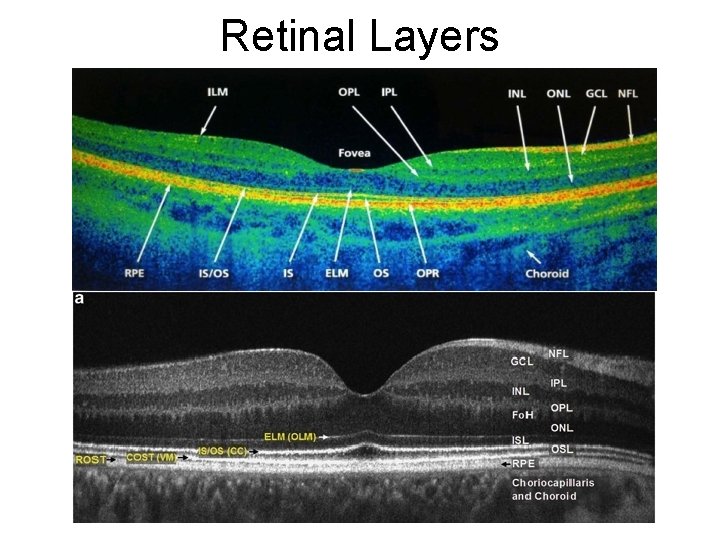
Retinal Layers
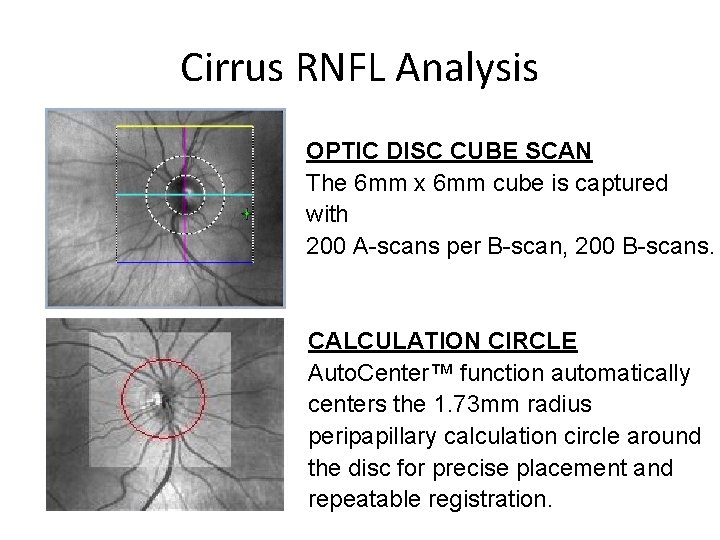
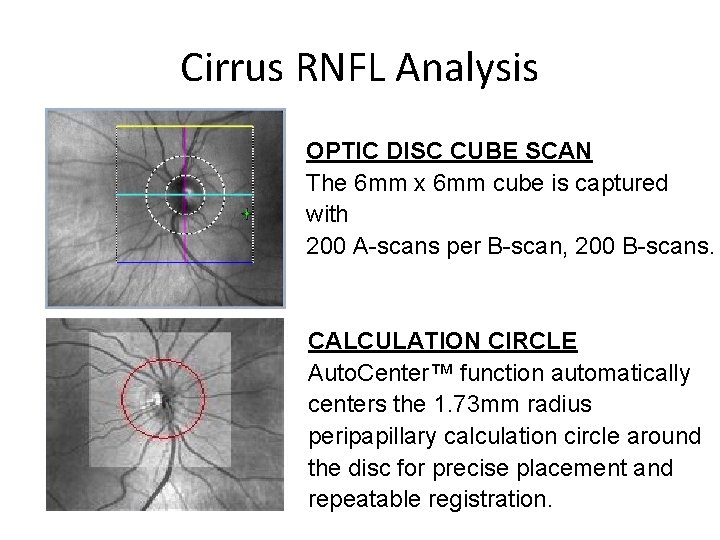
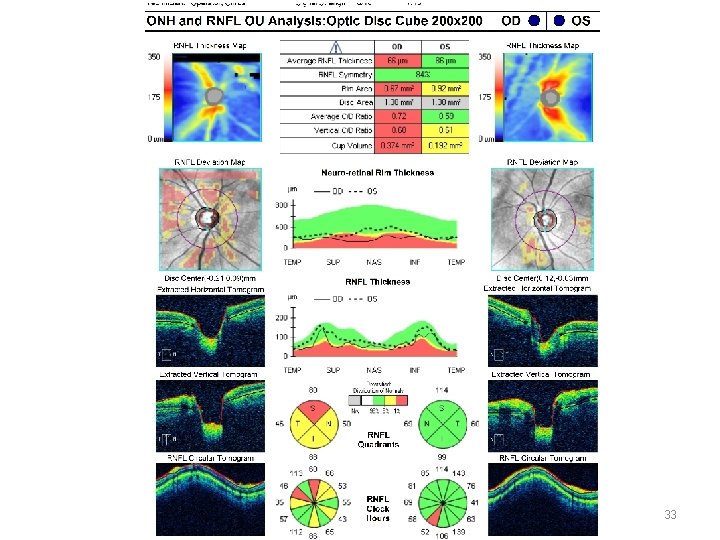
Cirrus RNFL Analysis OPTIC DISC CUBE SCAN The 6 mm x 6 mm cube is captured with 200 A-scans per B-scan, 200 B-scans. CALCULATION CIRCLE Auto. Center™ function automatically centers the 1. 73 mm radius peripapillary calculation circle around the disc for precise placement and repeatable registration.
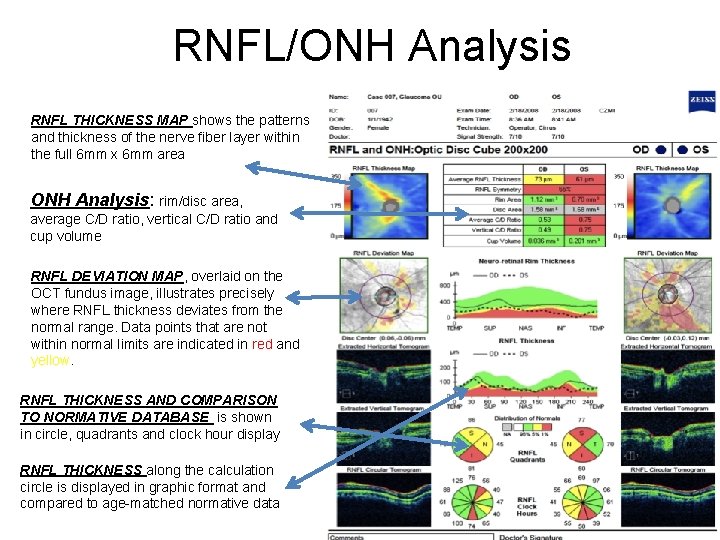
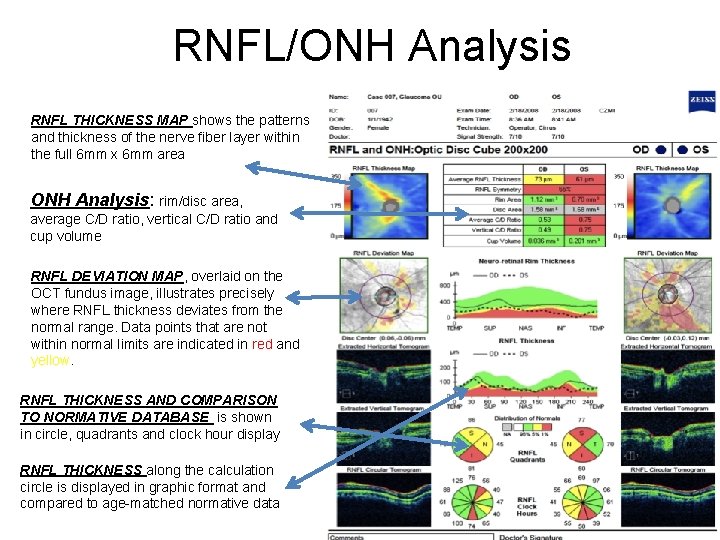
RNFL/ONH Analysis RNFL THICKNESS MAP shows the patterns and thickness of the nerve fiber layer within the full 6 mm x 6 mm area ONH Analysis: rim/disc area, average C/D ratio, vertical C/D ratio and cup volume RNFL DEVIATION MAP, overlaid on the OCT fundus image, illustrates precisely where RNFL thickness deviates from the normal range. Data points that are not within normal limits are indicated in red and yellow. RNFL THICKNESS AND COMPARISON TO NORMATIVE DATABASE is shown in circle, quadrants and clock hour display RNFL THICKNESS along the calculation circle is displayed in graphic format and compared to age-matched normative data
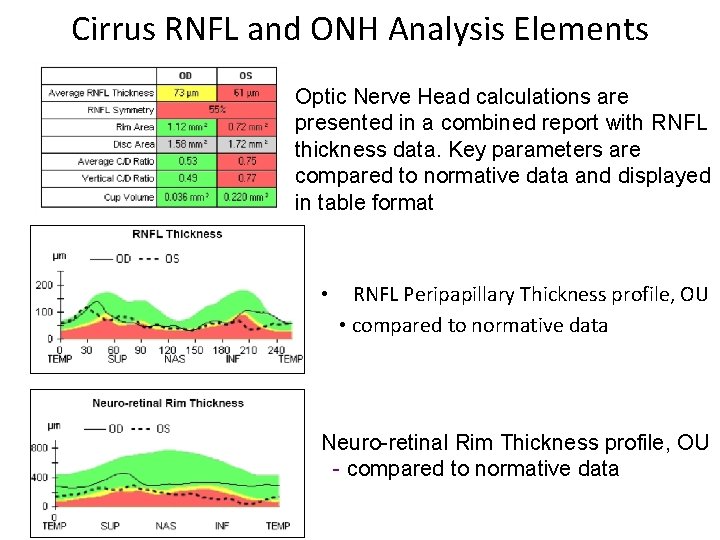
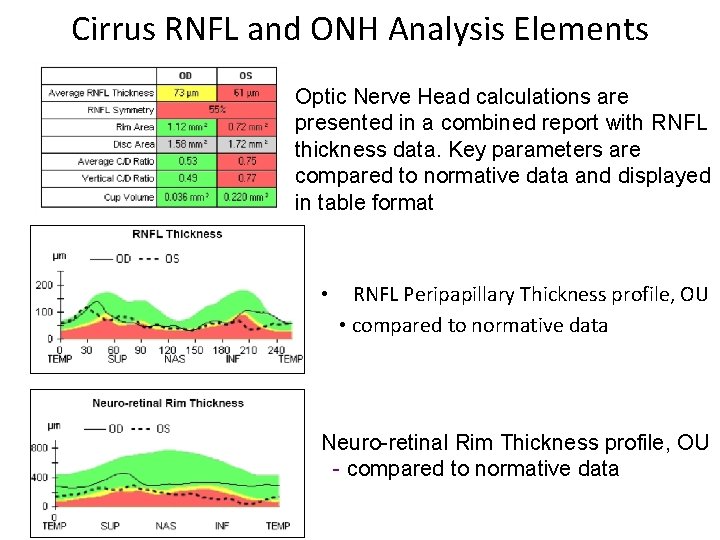
Cirrus RNFL and ONH Analysis Elements Optic Nerve Head calculations are presented in a combined report with RNFL thickness data. Key parameters are compared to normative data and displayed in table format • RNFL Peripapillary Thickness profile, OU • compared to normative data Neuro-retinal Rim Thickness profile, OU - compared to normative data
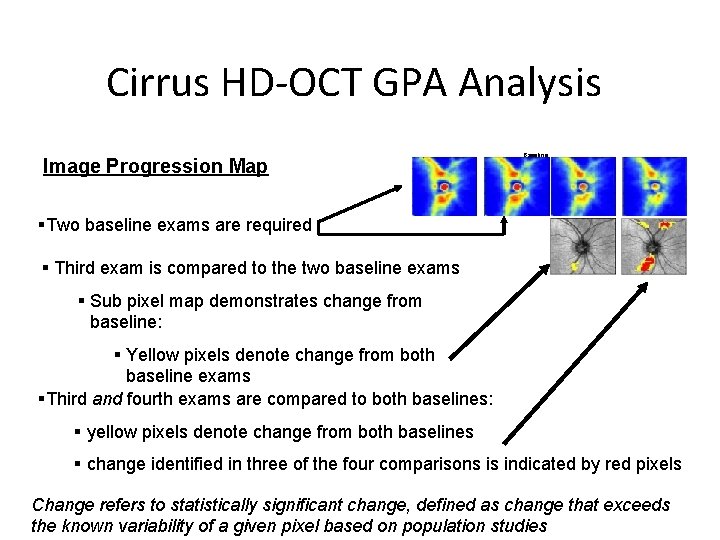
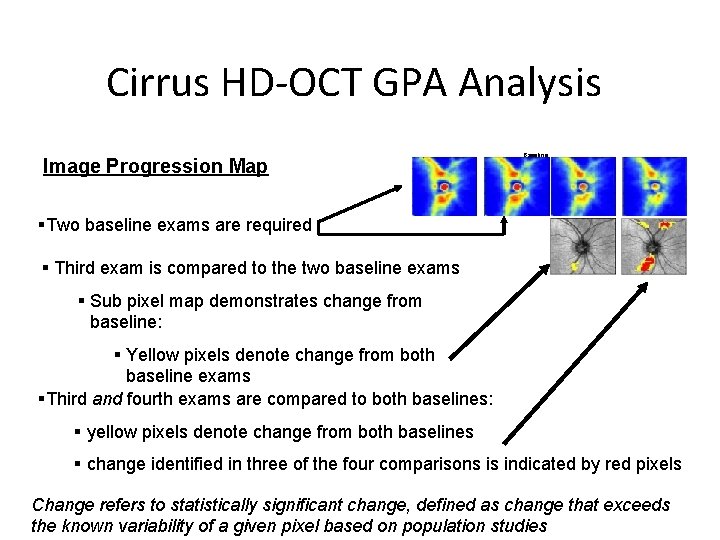
Cirrus HD-OCT GPA Analysis Image Progression Map Baseline §Two baseline exams are required § Third exam is compared to the two baseline exams § Sub pixel map demonstrates change from baseline: § Yellow pixels denote change from both baseline exams §Third and fourth exams are compared to both baselines: § yellow pixels denote change from both baselines § change identified in three of the four comparisons is indicated by red pixels Change refers to statistically significant change, defined as change that exceeds the known variability of a given pixel based on population studies
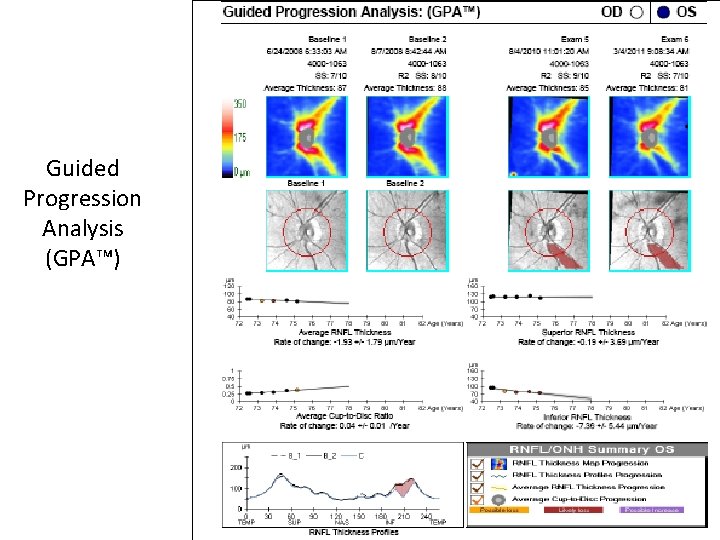
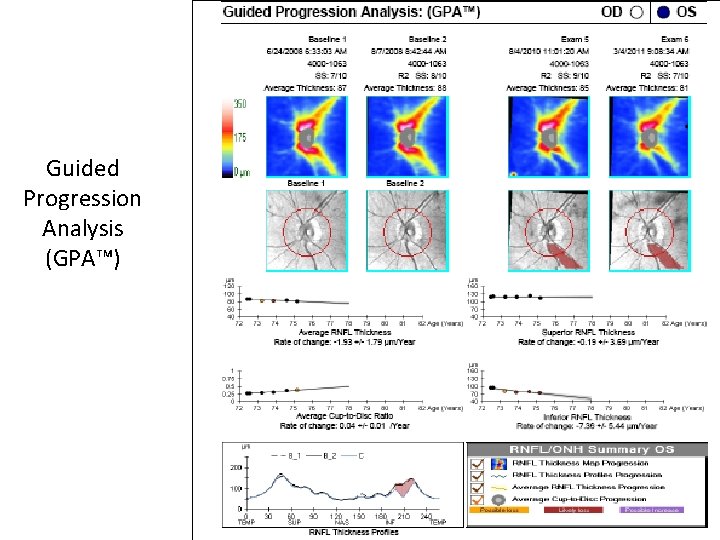
Page 2 Guided Progression Analysis (GPA™) 10
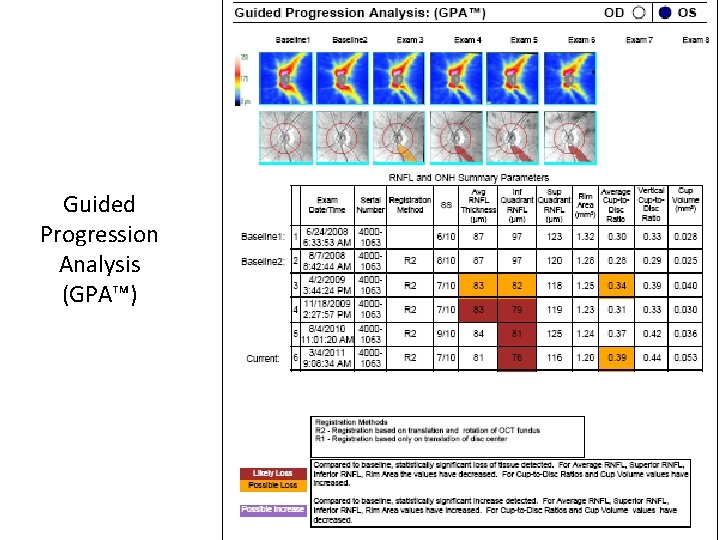
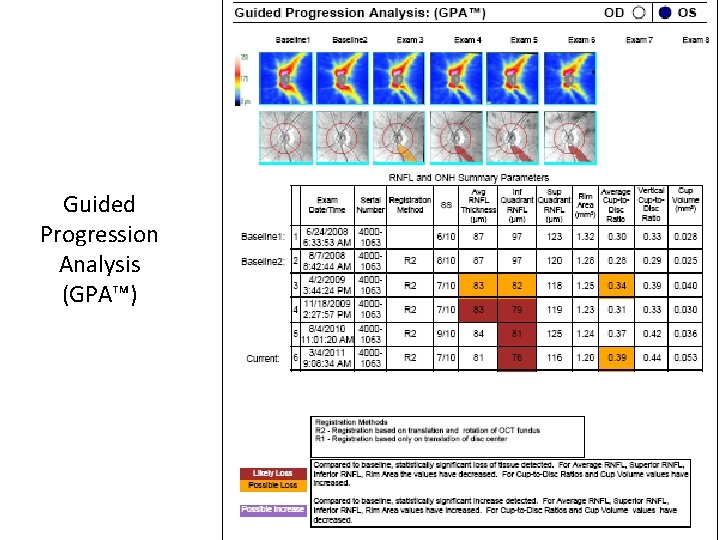
Guided Progression Analysis (GPA™) 11
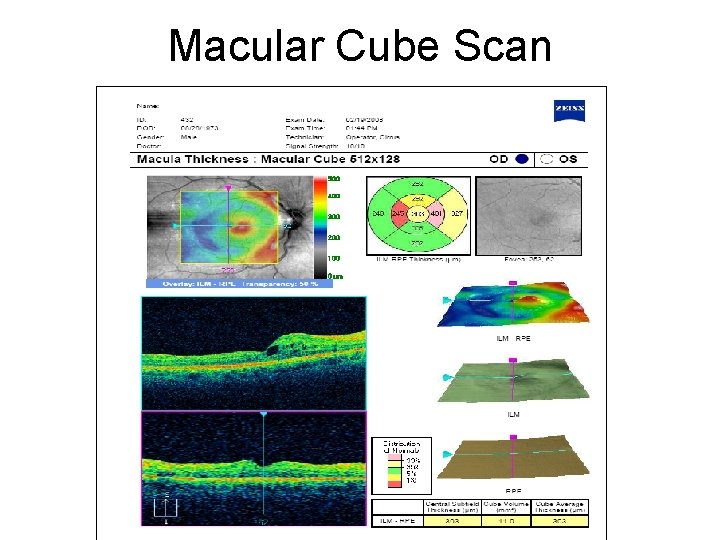
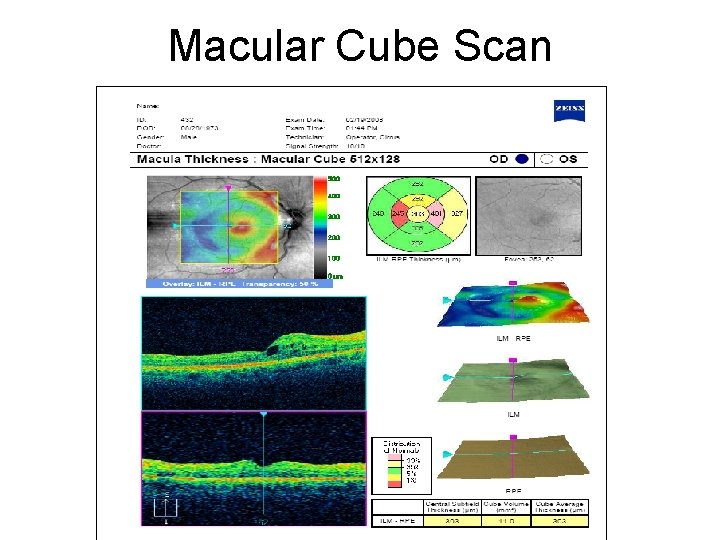
Macular Cube Scan
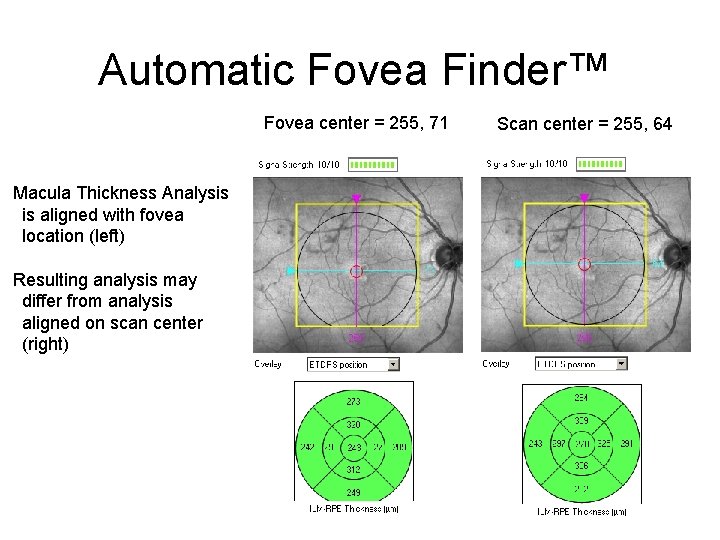
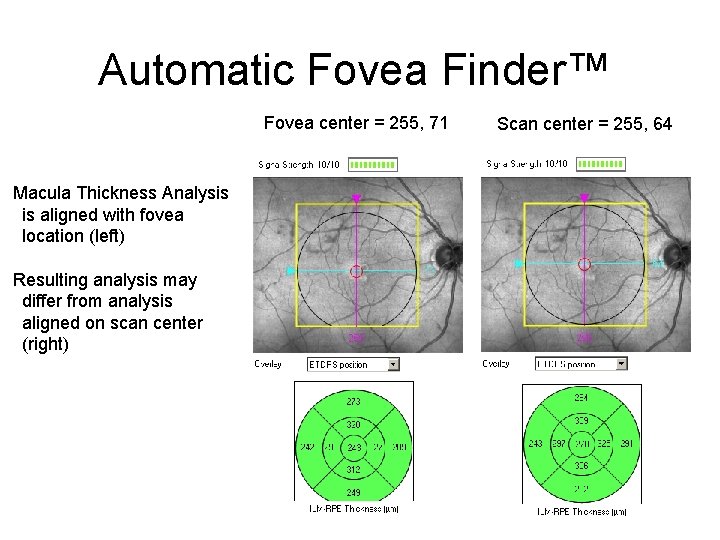
Automatic Fovea Finder™ Fovea center = 255, 71 Macula Thickness Analysis is aligned with fovea location (left) Resulting analysis may differ from analysis aligned on scan center (right) Scan center = 255, 64
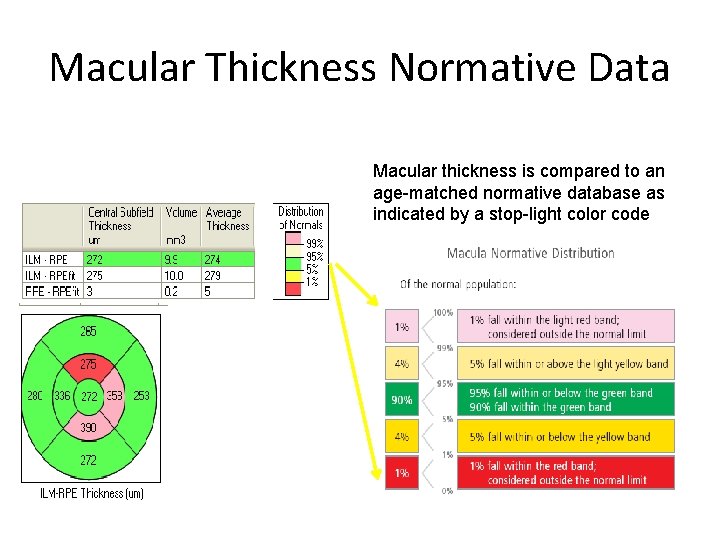
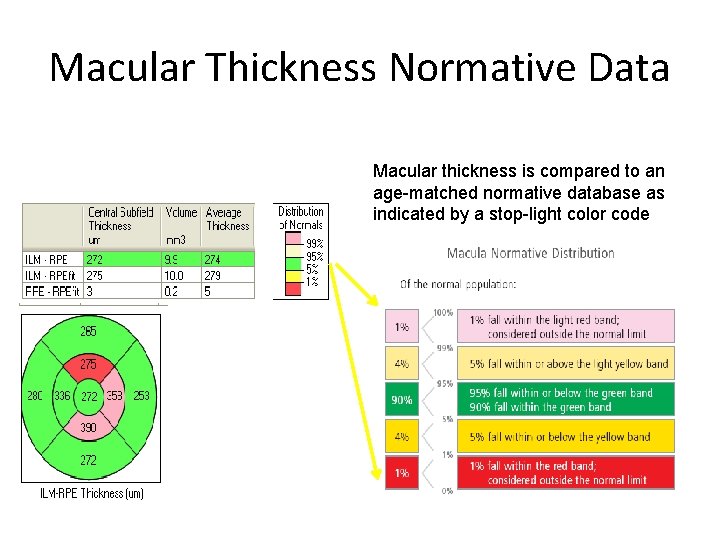
Macular Thickness Normative Data Macular thickness is compared to an age-matched normative database as indicated by a stop-light color code
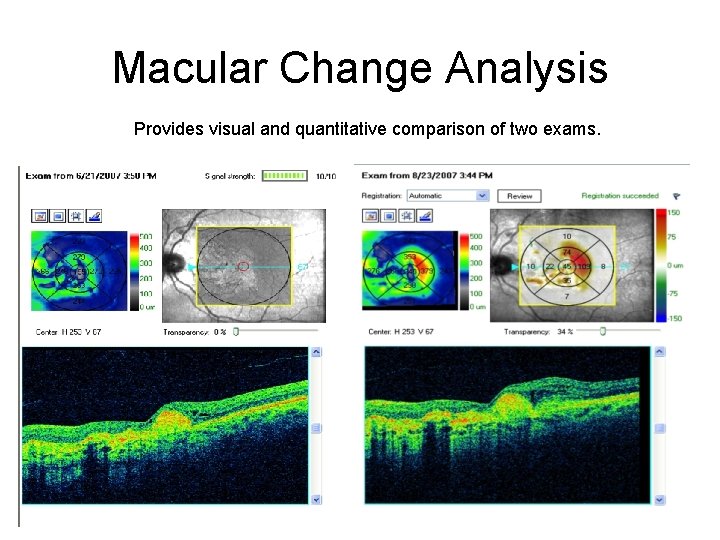
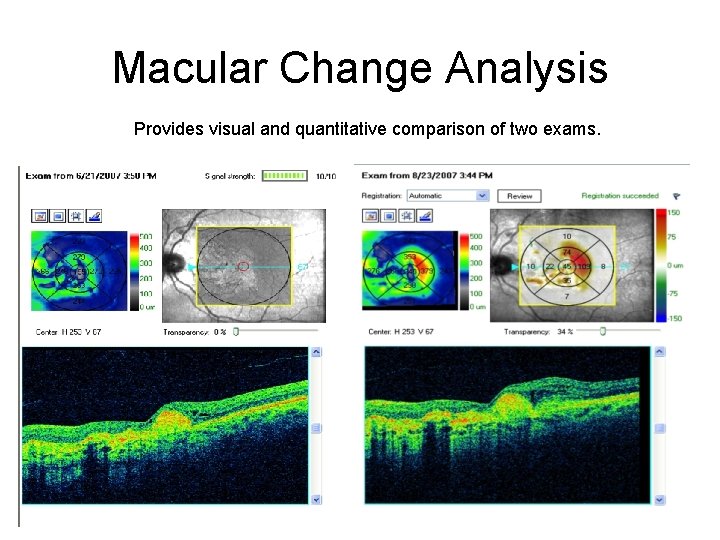
Macular Change Analysis Provides visual and quantitative comparison of two exams.
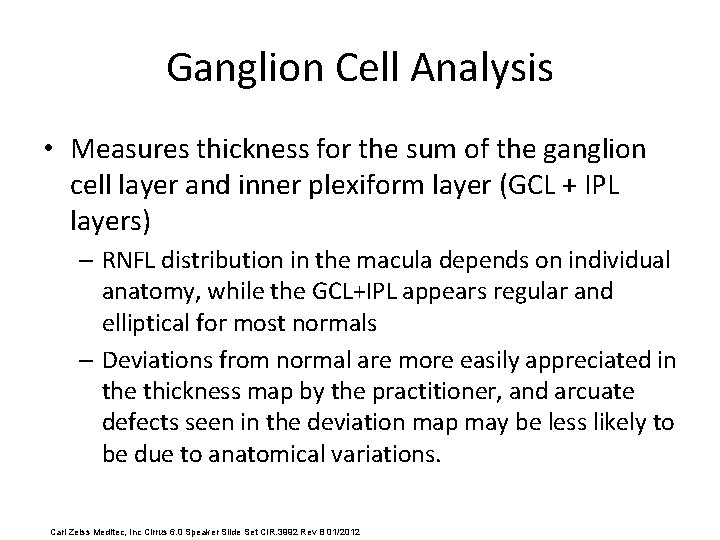
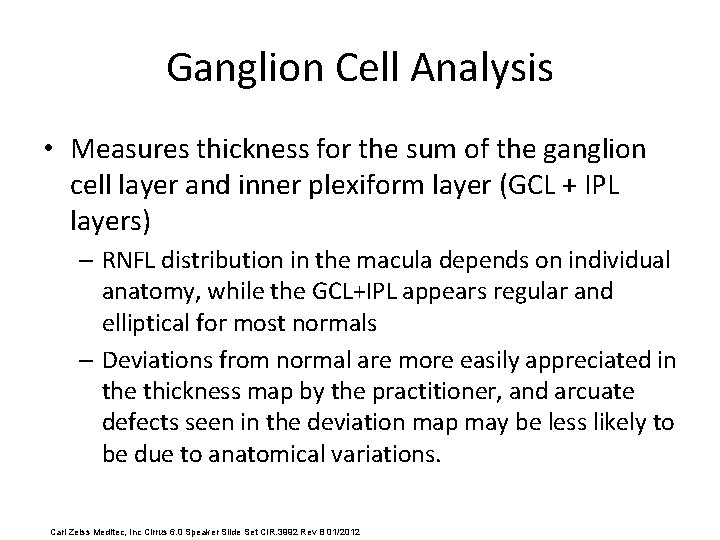
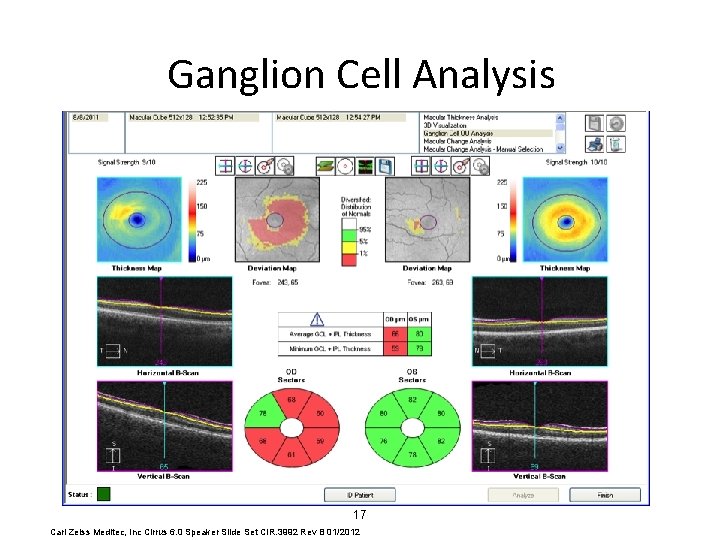
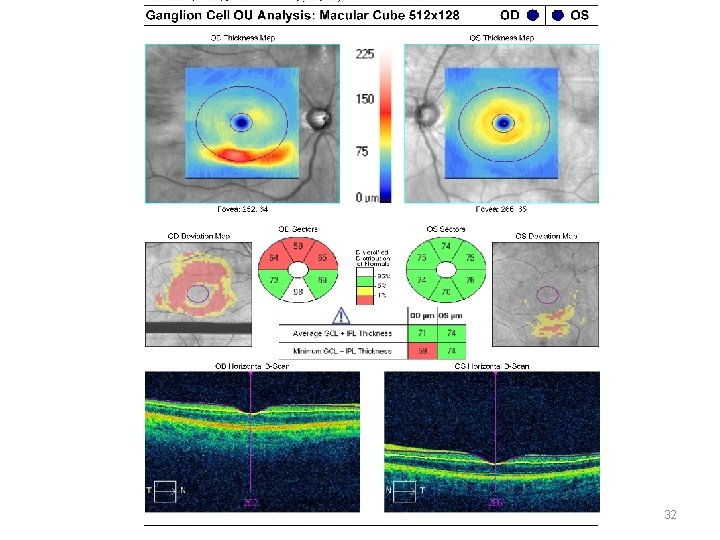
Ganglion Cell Analysis • Measures thickness for the sum of the ganglion cell layer and inner plexiform layer (GCL + IPL layers) – RNFL distribution in the macula depends on individual anatomy, while the GCL+IPL appears regular and elliptical for most normals – Deviations from normal are more easily appreciated in the thickness map by the practitioner, and arcuate defects seen in the deviation map may be less likely to be due to anatomical variations. Carl Zeiss Meditec, Inc Cirrus 6. 0 Speaker Slide Set CIR. 3992 Rev B 01/2012
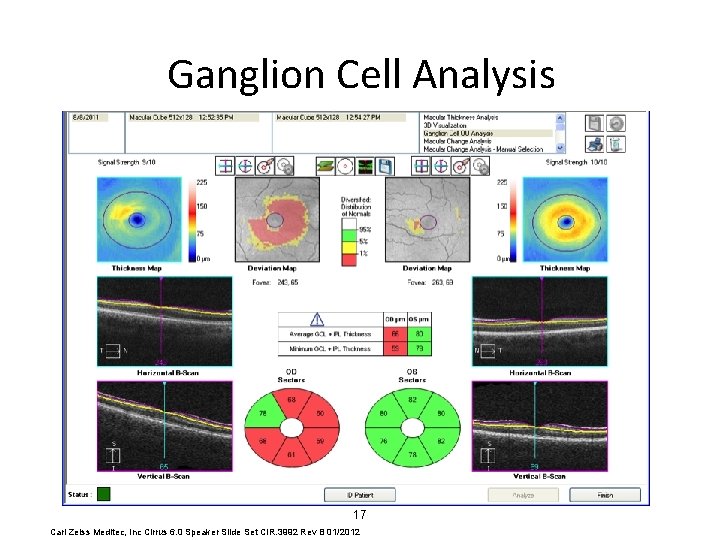
Ganglion Cell Analysis 17 Carl Zeiss Meditec, Inc Cirrus 6. 0 Speaker Slide Set CIR. 3992 Rev B 01/2012
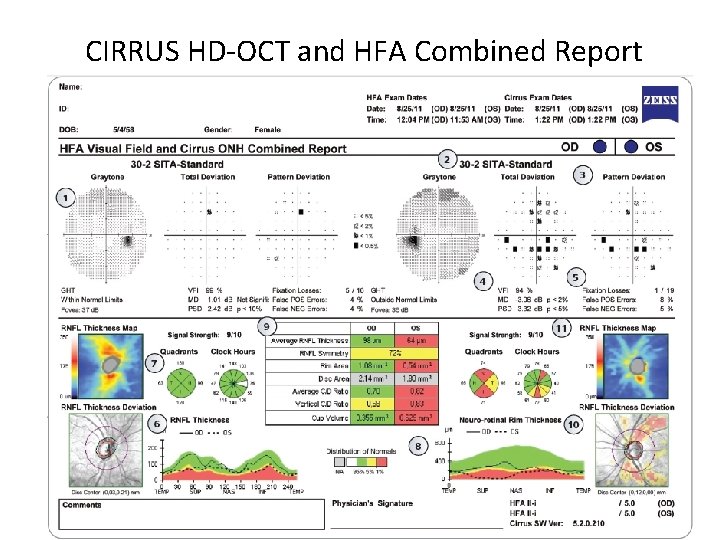
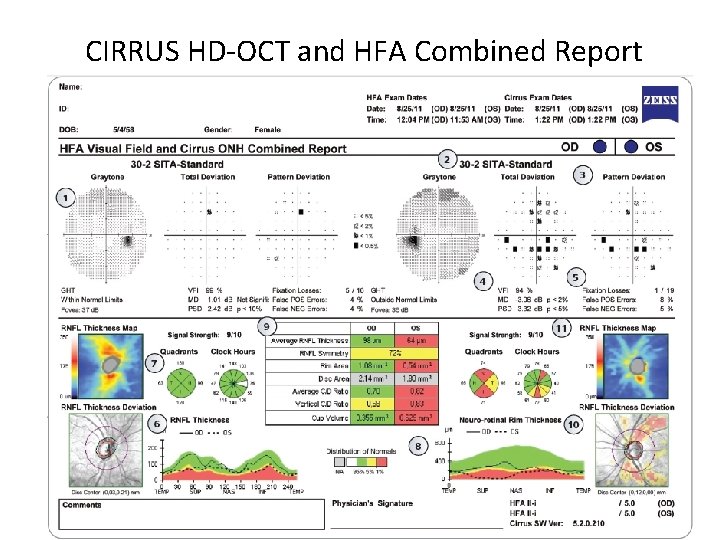
CIRRUS HD-OCT and HFA Combined Report
Case 1 19
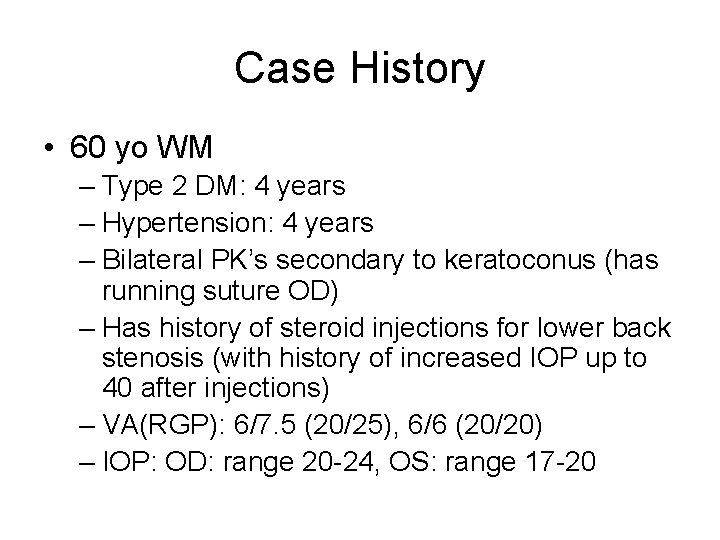
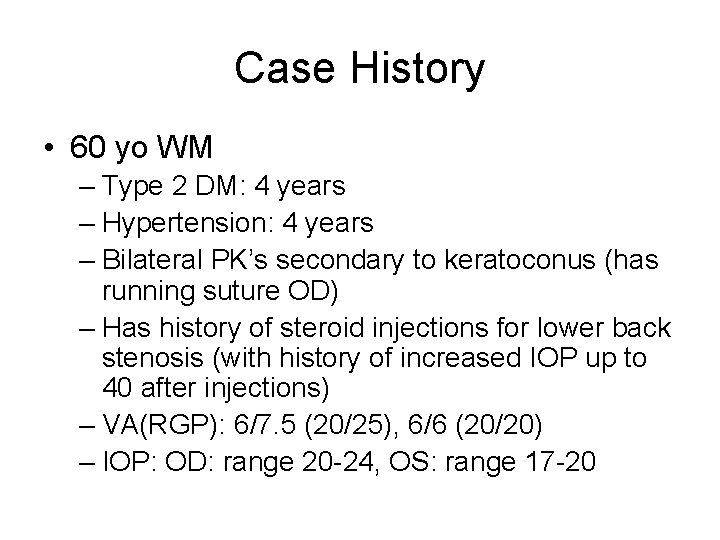
Case History • 60 yo WM – Type 2 DM: 4 years – Hypertension: 4 years – Bilateral PK’s secondary to keratoconus (has running suture OD) – Has history of steroid injections for lower back stenosis (with history of increased IOP up to 40 after injections) – VA(RGP): 6/7. 5 (20/25), 6/6 (20/20) – IOP: OD: range 20 -24, OS: range 17 -20
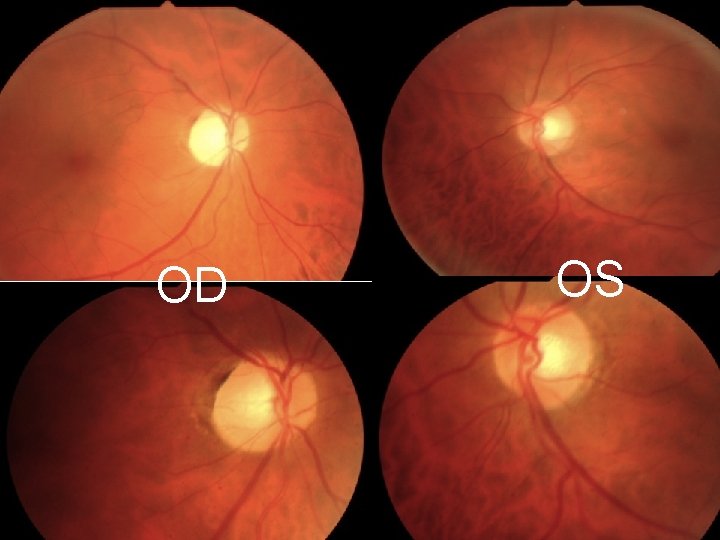
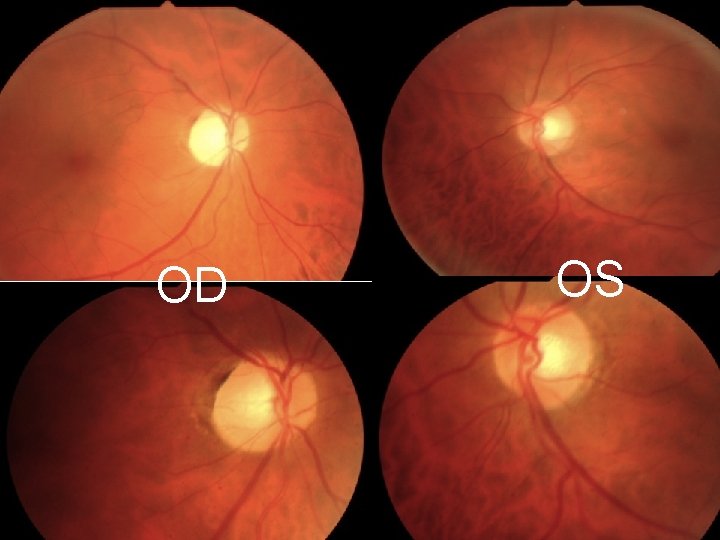
OD OS
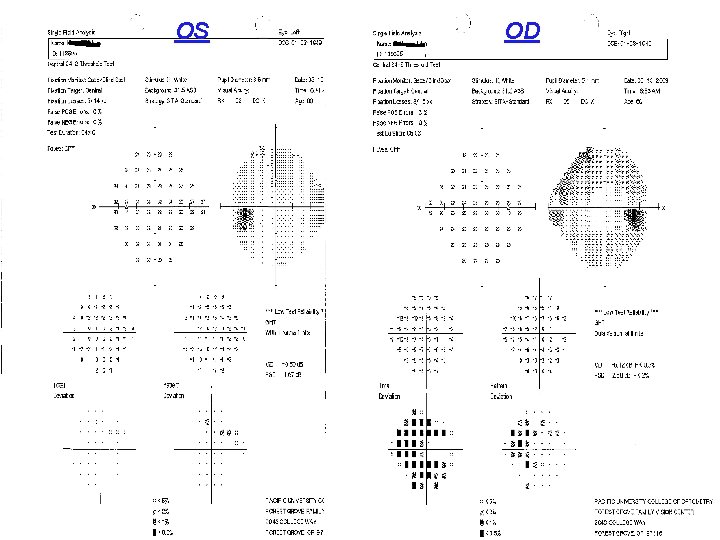
OS OD
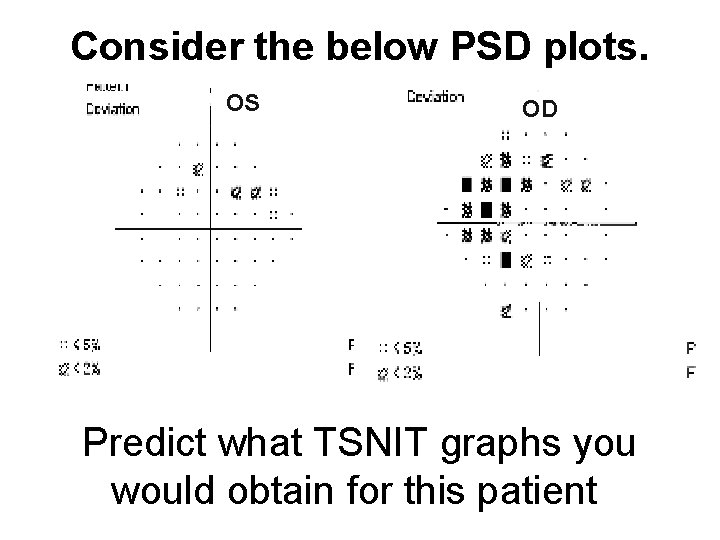
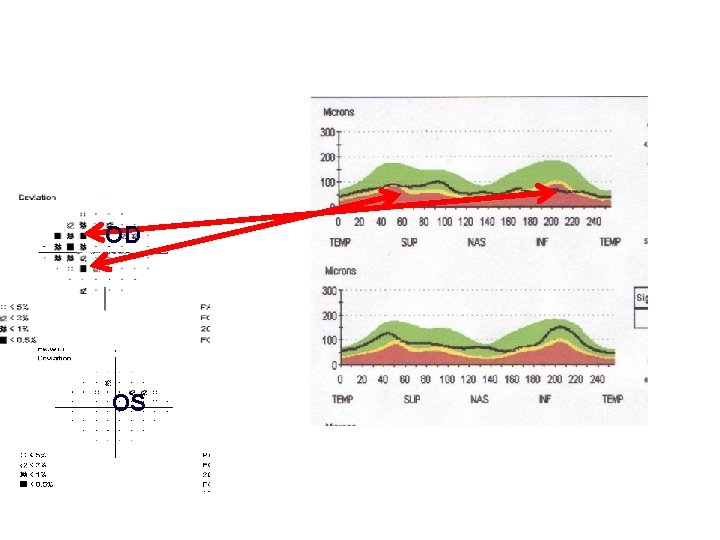
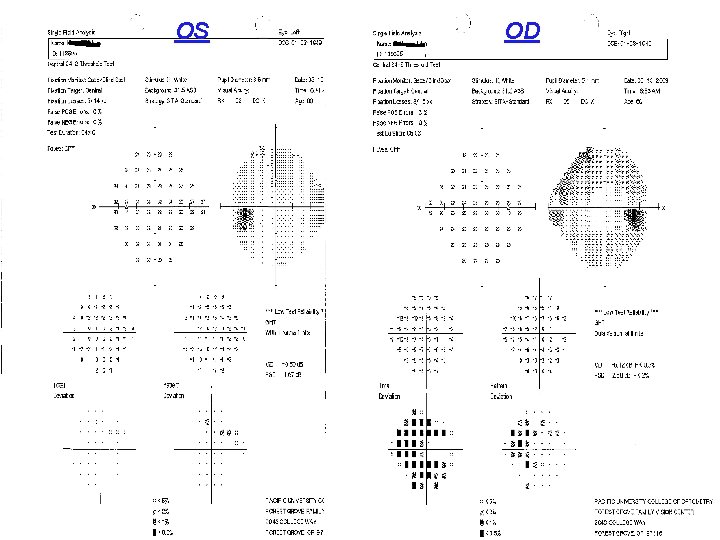
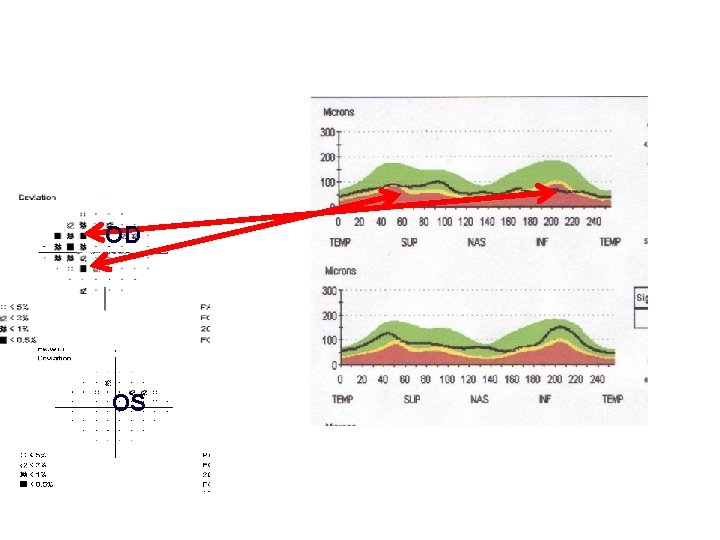
Consider the below PSD plots. OS OD Predict what TSNIT graphs you would obtain for this patient.
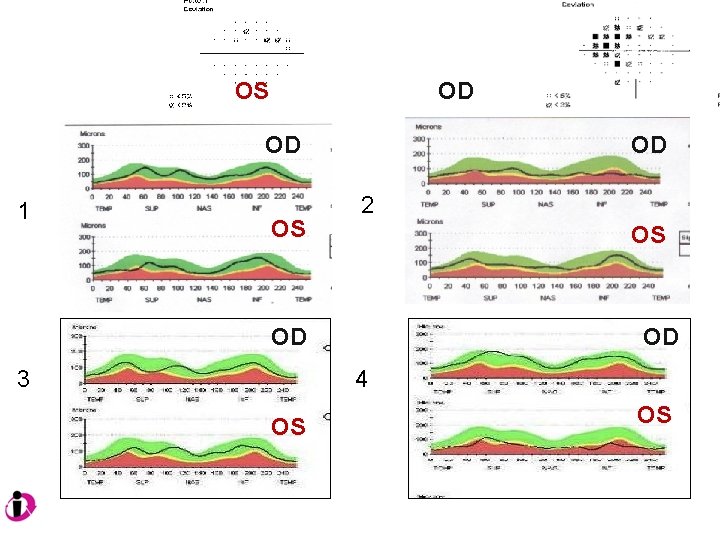
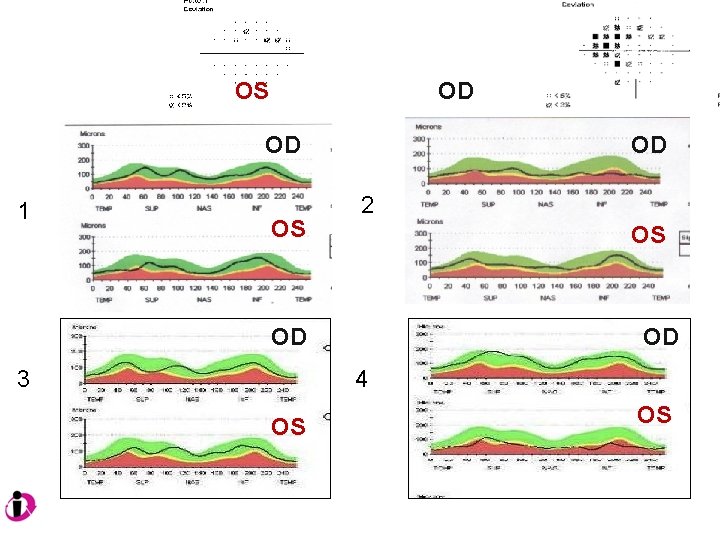
OS OD OD 1 OS OD 2 OS OD 3 OD 4 OS OS
OD OS
OS OD
Case 2
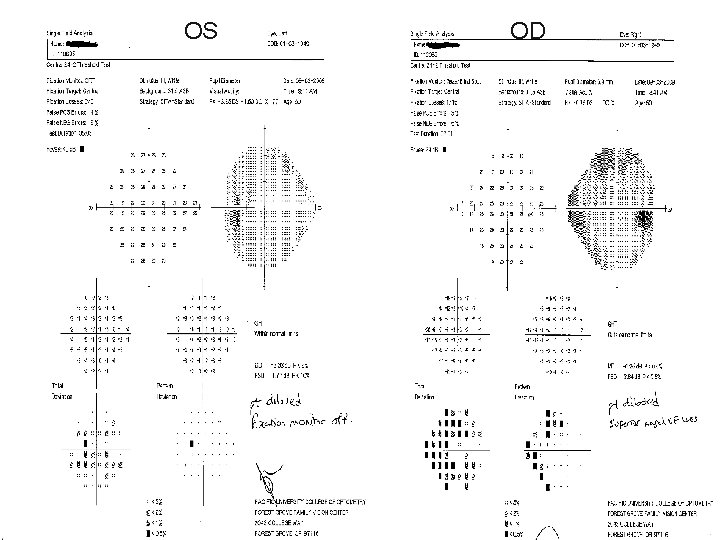
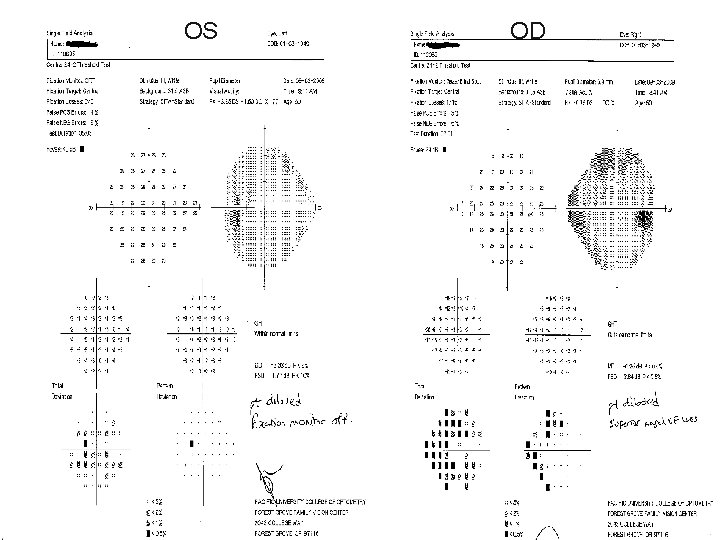
Entrance Skills • 60 YR WM – Complaint of blurry vision – Currently wearing sister’s contacts as he lost his glasses – PMHx: depression but not currently controlled – POHx: unremarkable – BCVa: 6/6 (20/20) OD, OS – All other entrance skills unremarkable 28
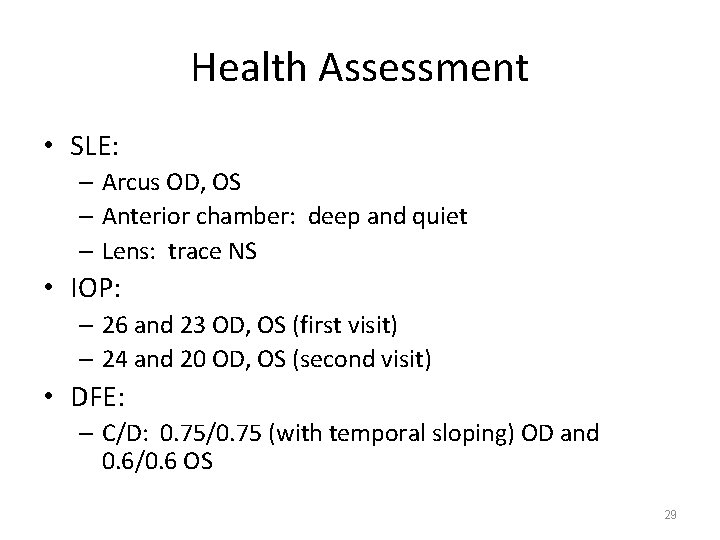
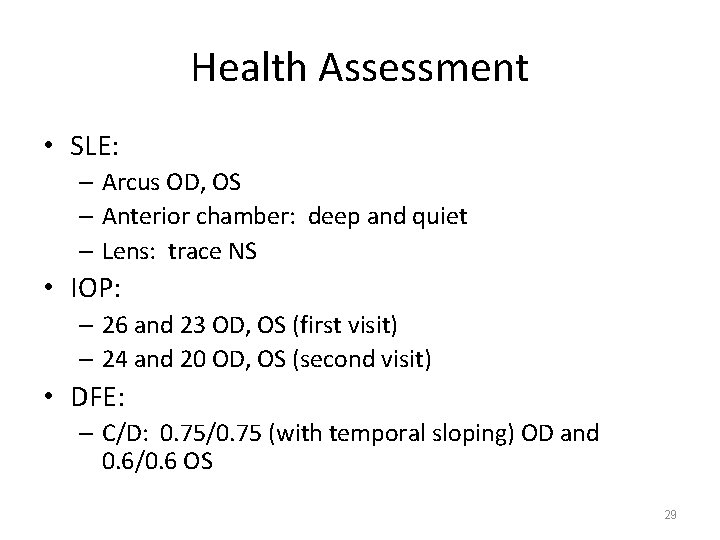
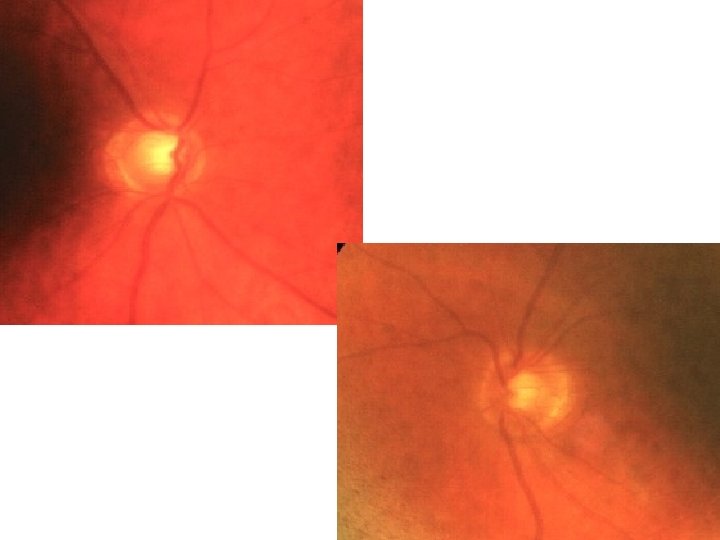
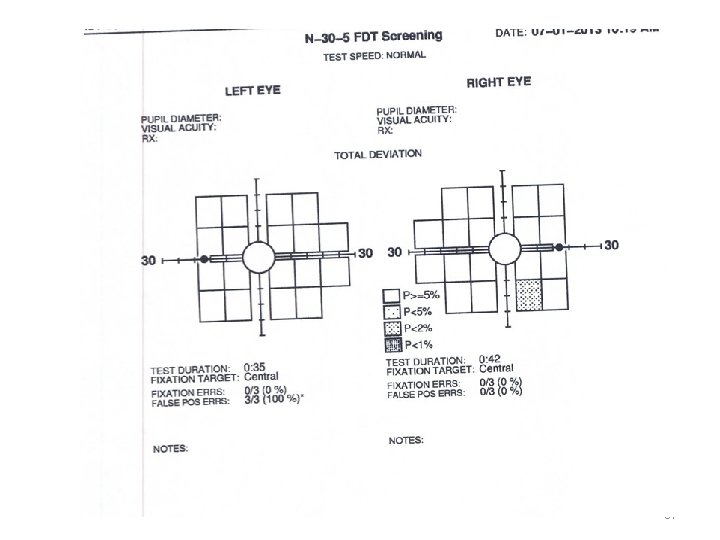
Health Assessment • SLE: – Arcus OD, OS – Anterior chamber: deep and quiet – Lens: trace NS • IOP: – 26 and 23 OD, OS (first visit) – 24 and 20 OD, OS (second visit) • DFE: – C/D: 0. 75/0. 75 (with temporal sloping) OD and 0. 6/0. 6 OS 29
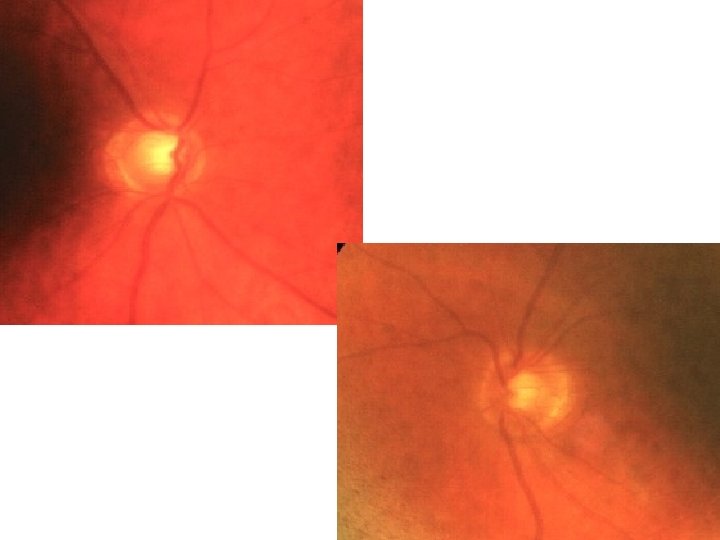
30
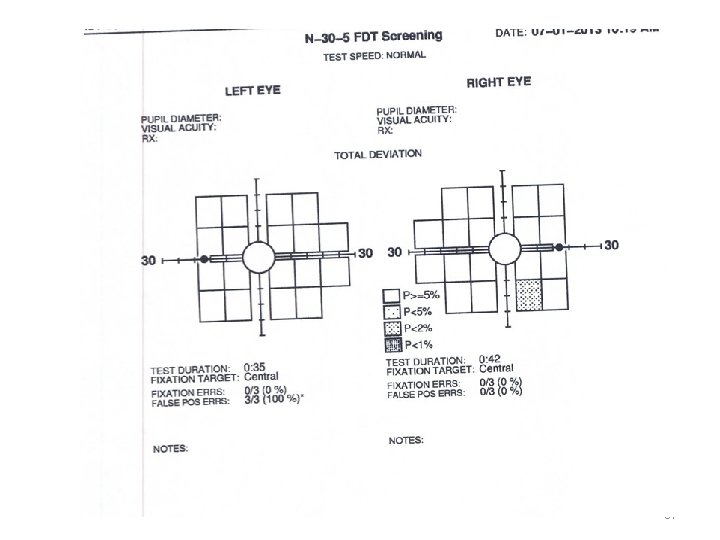
31
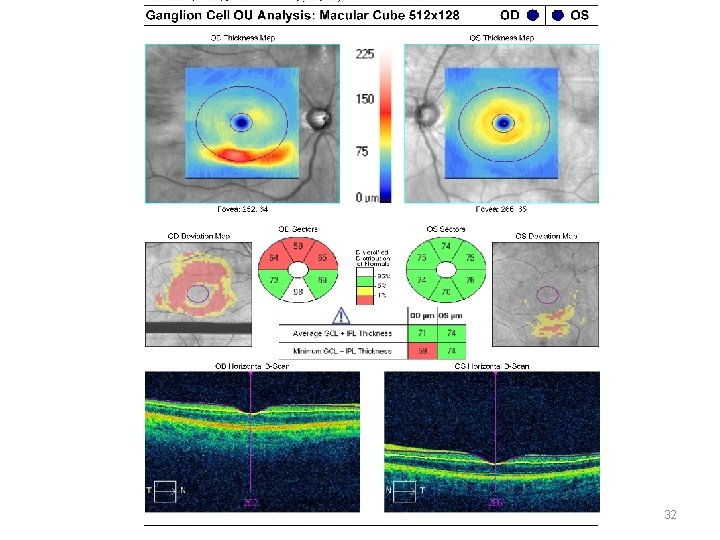
32
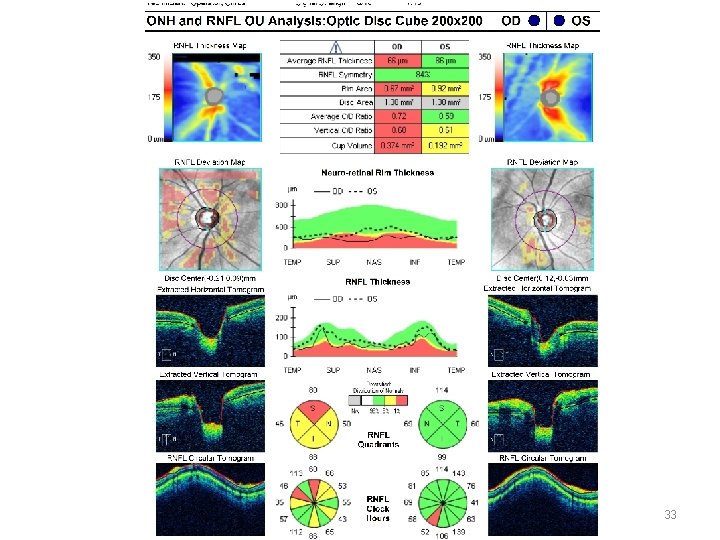
33
Case 3 34
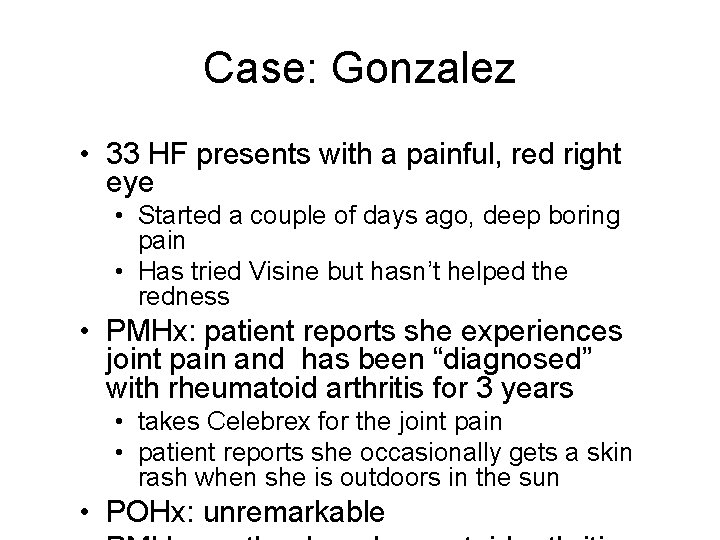
Case: Gonzalez • 33 HF presents with a painful, red right eye • Started a couple of days ago, deep boring pain • Has tried Visine but hasn’t helped the redness • PMHx: patient reports she experiences joint pain and has been “diagnosed” with rheumatoid arthritis for 3 years • takes Celebrex for the joint pain • patient reports she occasionally gets a skin rash when she is outdoors in the sun • POHx: unremarkable
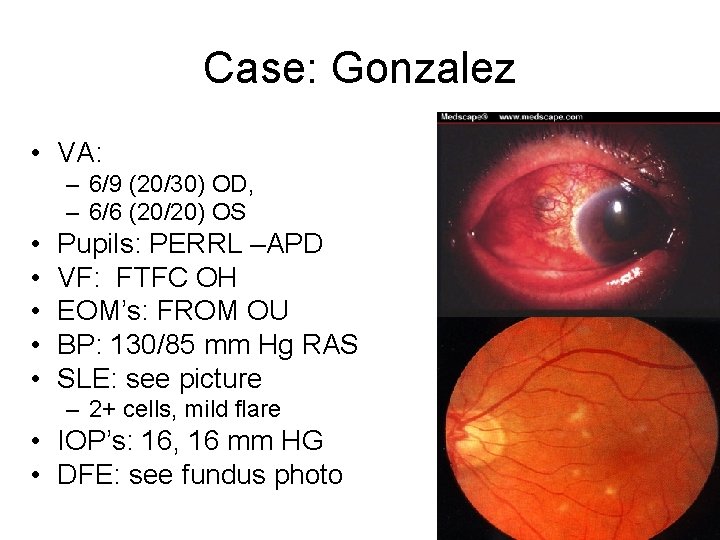
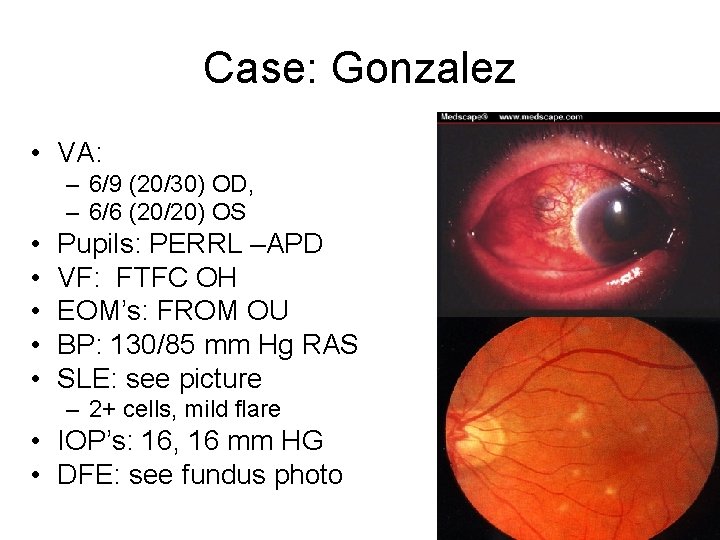
Case: Gonzalez • VA: – 6/9 (20/30) OD, – 6/6 (20/20) OS • • • Pupils: PERRL –APD VF: FTFC OH EOM’s: FROM OU BP: 130/85 mm Hg RAS SLE: see picture – 2+ cells, mild flare • IOP’s: 16, 16 mm HG • DFE: see fundus photo
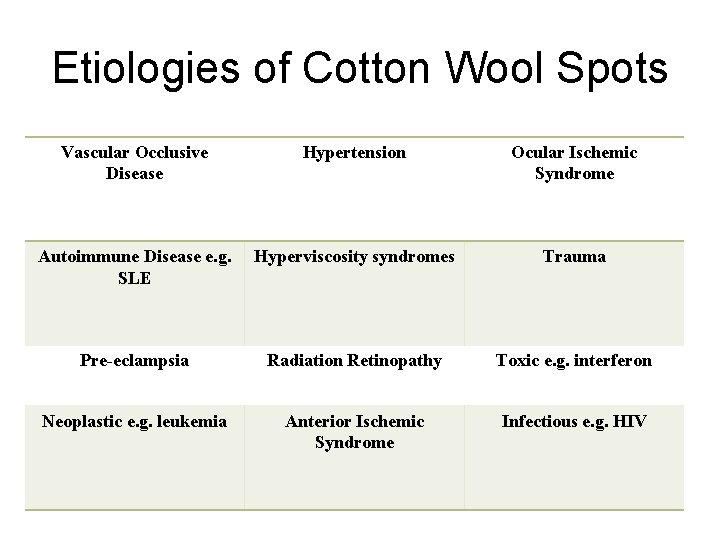
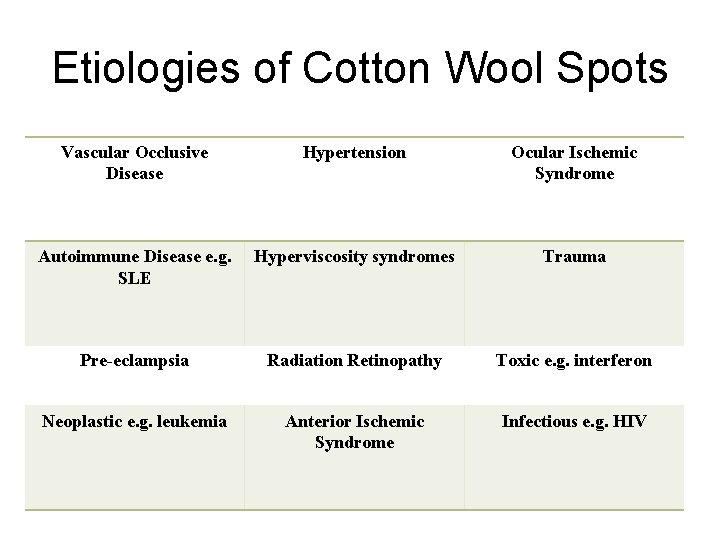
Etiologies of Cotton Wool Spots Vascular Occlusive Disease Hypertension Ocular Ischemic Syndrome Autoimmune Disease e. g. SLE Hyperviscosity syndromes Trauma Pre-eclampsia Radiation Retinopathy Toxic e. g. interferon Neoplastic e. g. leukemia Anterior Ischemic Syndrome Infectious e. g. HIV
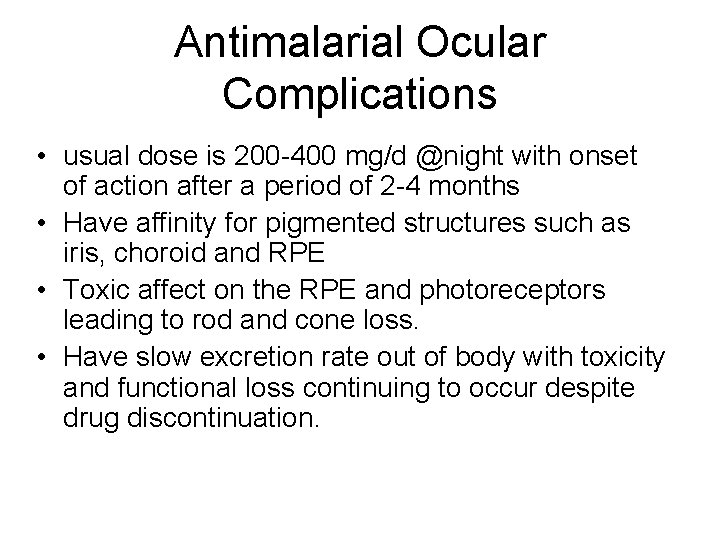
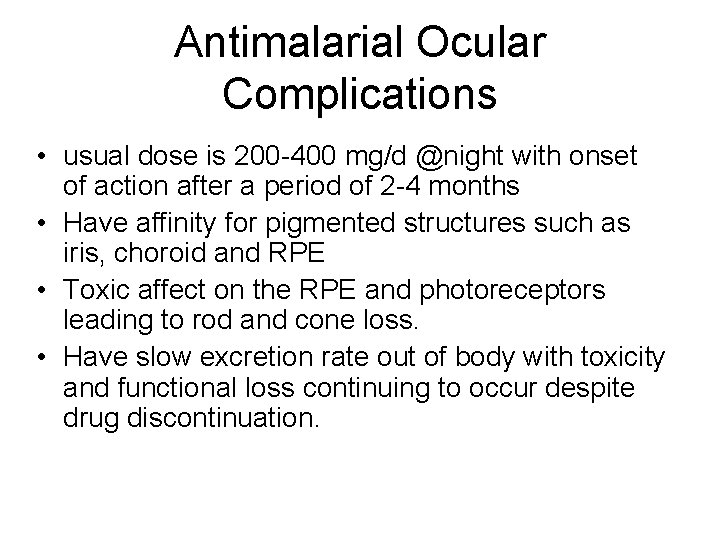
Antimalarial Ocular Complications • usual dose is 200 -400 mg/d @night with onset of action after a period of 2 -4 months • Have affinity for pigmented structures such as iris, choroid and RPE • Toxic affect on the RPE and photoreceptors leading to rod and cone loss. • Have slow excretion rate out of body with toxicity and functional loss continuing to occur despite drug discontinuation.
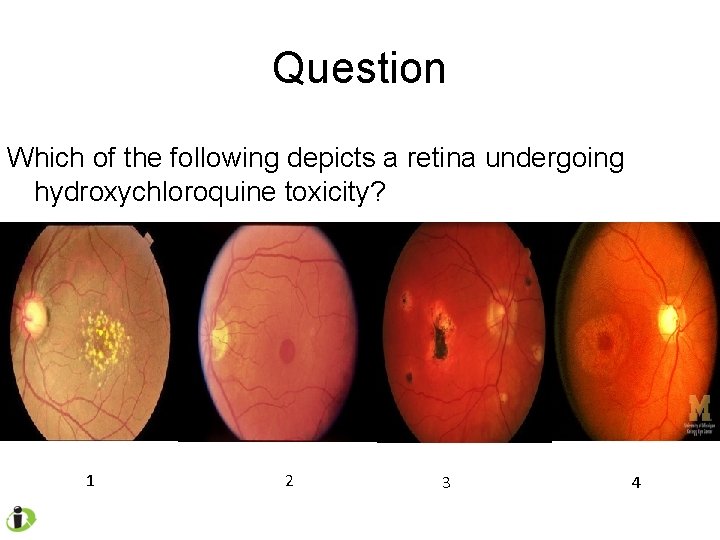
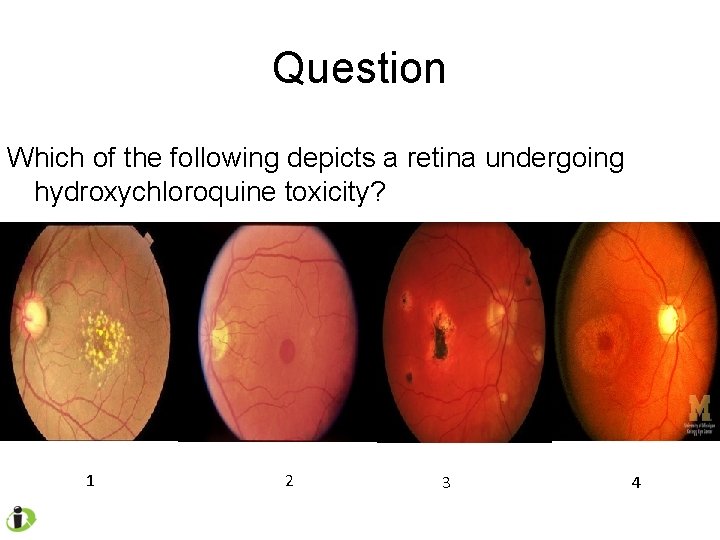
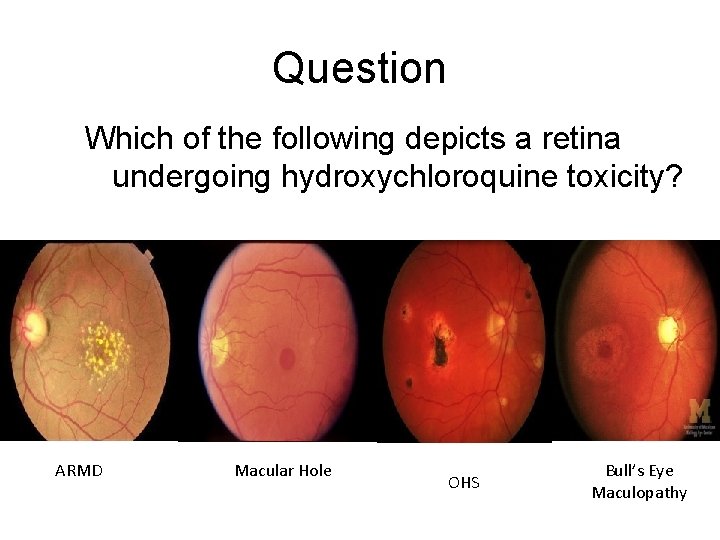
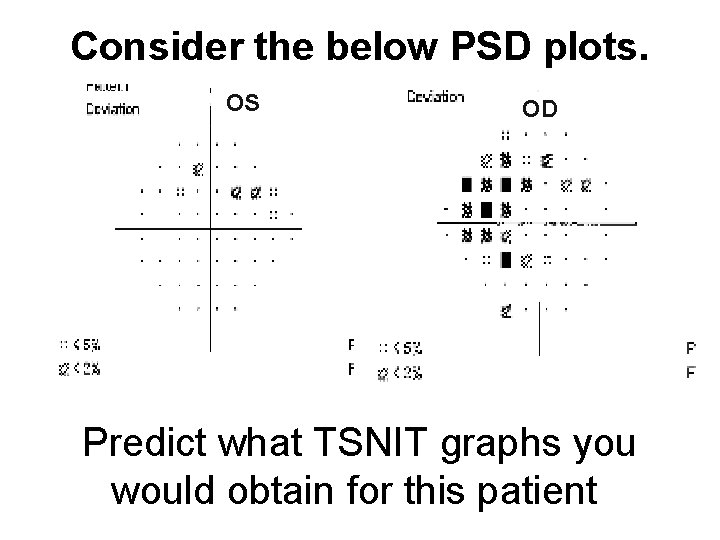
Question Which of the following depicts a retina undergoing hydroxychloroquine toxicity? 1 2 3 4
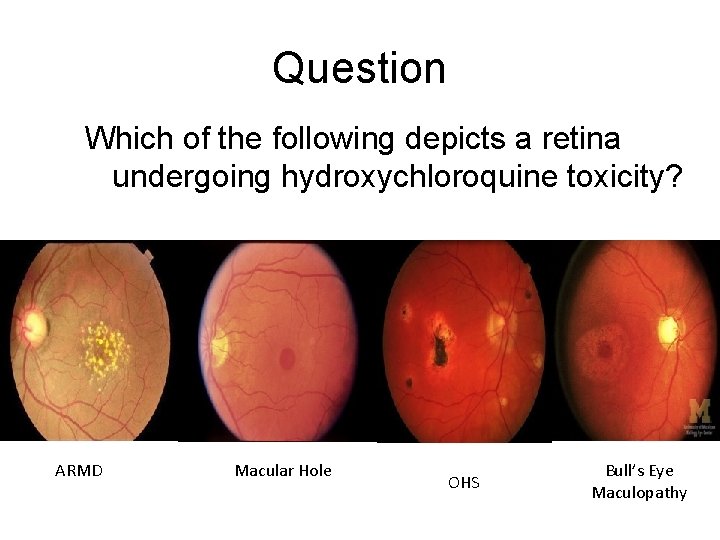
Question Which of the following depicts a retina undergoing hydroxychloroquine toxicity? ARMD Macular Hole OHS Bull’s Eye Maculopathy
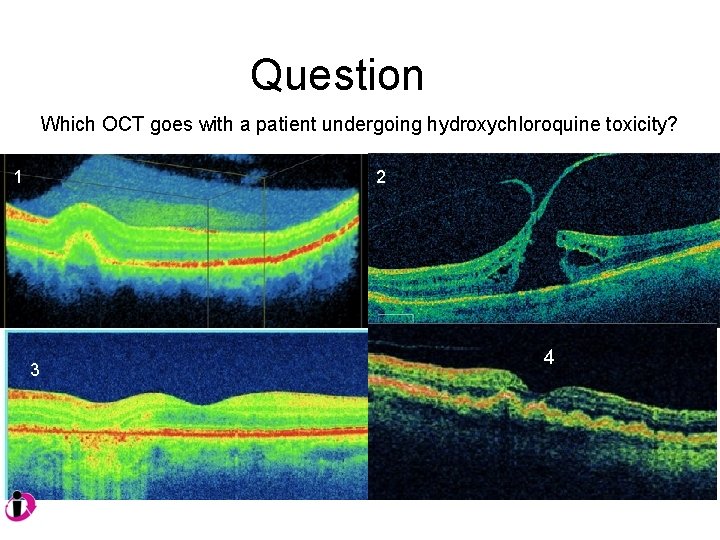
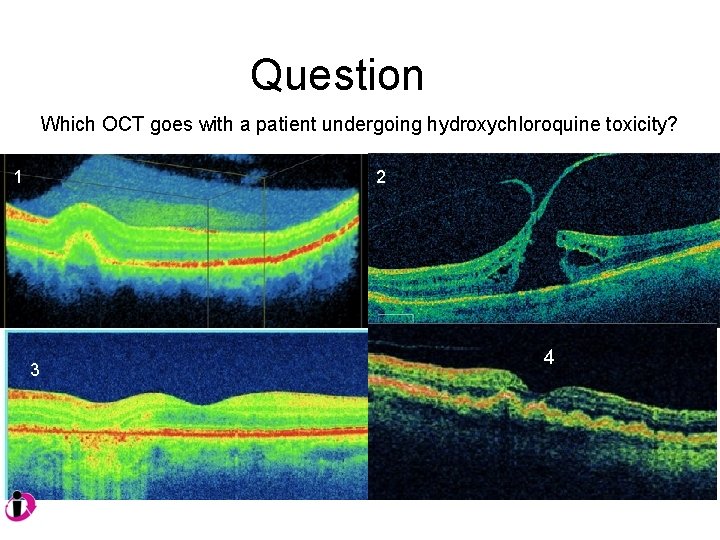
Question Which OCT goes with a patient undergoing hydroxychloroquine toxicity? 1 2 3 4
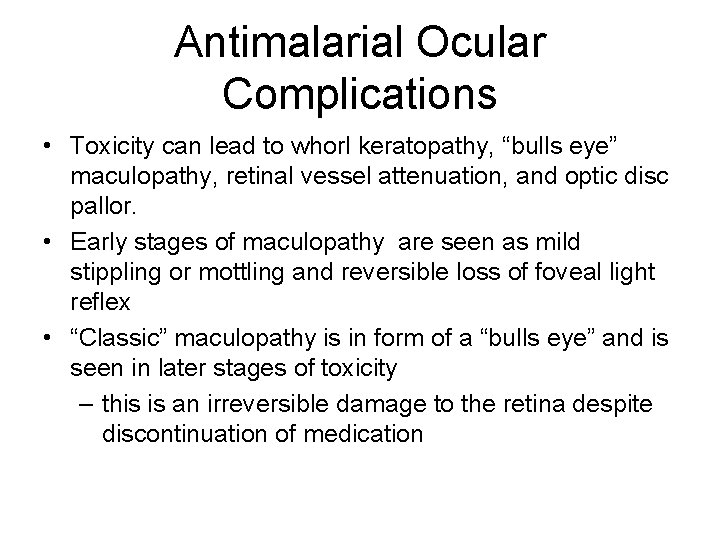
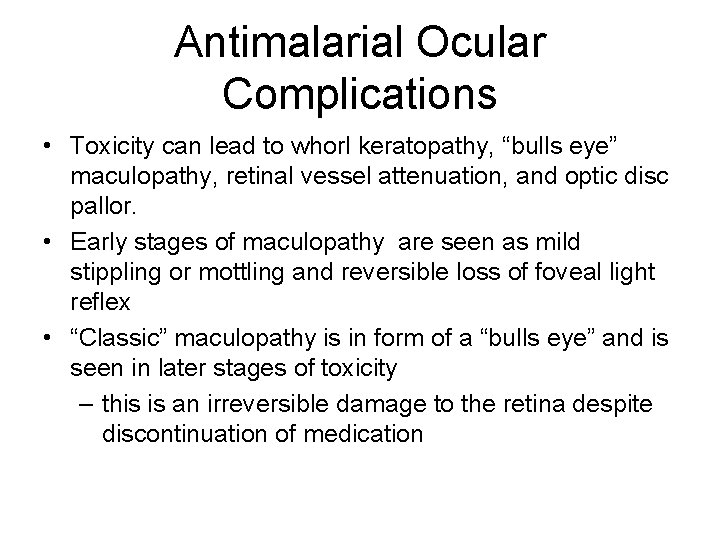
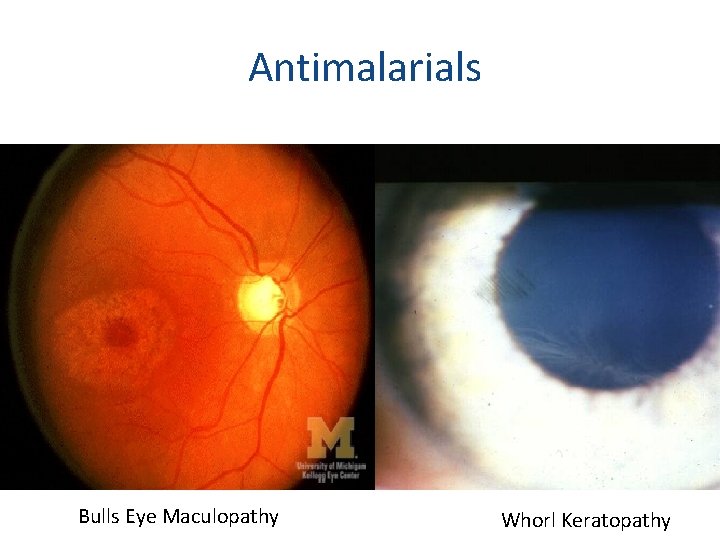
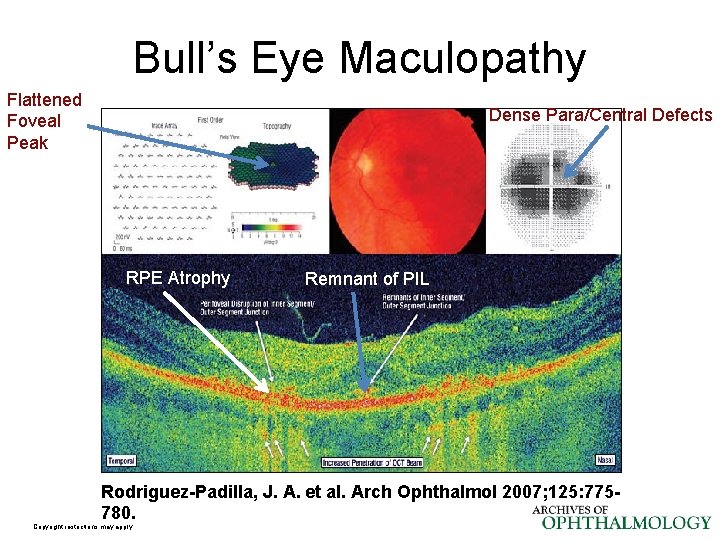
Antimalarial Ocular Complications • Toxicity can lead to whorl keratopathy, “bulls eye” maculopathy, retinal vessel attenuation, and optic disc pallor. • Early stages of maculopathy are seen as mild stippling or mottling and reversible loss of foveal light reflex • “Classic” maculopathy is in form of a “bulls eye” and is seen in later stages of toxicity – this is an irreversible damage to the retina despite discontinuation of medication
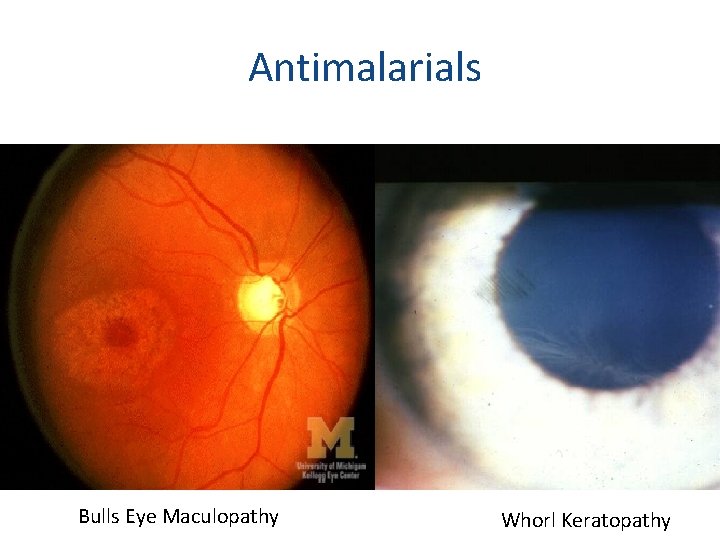
Antimalarials 29 Bulls Eye Maculopathy Whorl Keratopathy
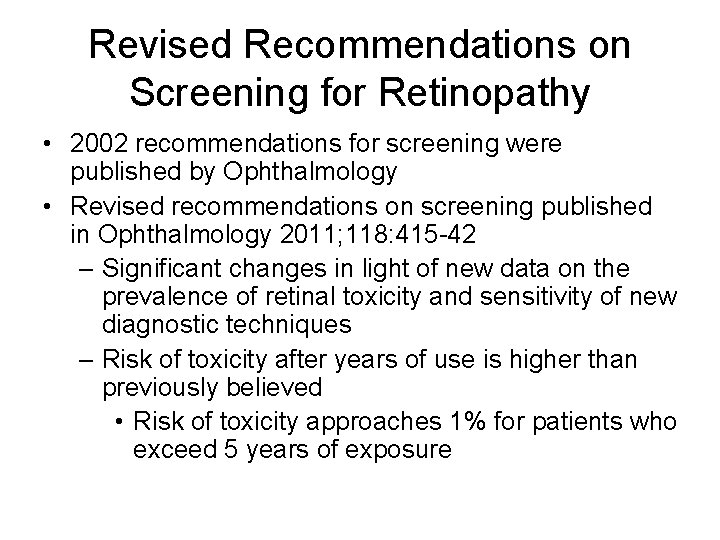
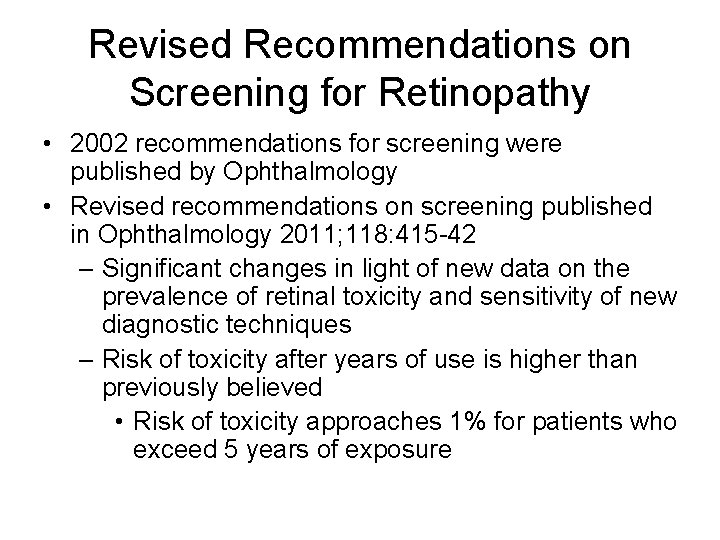
Revised Recommendations on Screening for Retinopathy • 2002 recommendations for screening were published by Ophthalmology • Revised recommendations on screening published in Ophthalmology 2011; 118: 415 -42 – Significant changes in light of new data on the prevalence of retinal toxicity and sensitivity of new diagnostic techniques – Risk of toxicity after years of use is higher than previously believed • Risk of toxicity approaches 1% for patients who exceed 5 years of exposure
Revised Recommendations on Screening for Retinopathy • Amsler grid testing removed as an acceptable screening technique – NOT equivalent to threshold VF testing • Strongly advised that 10 -2 VF screening be supplemented with sensitive objective tests such as: – Multifocal ERG – Spectral domain OCT – Fundus autofluorescence
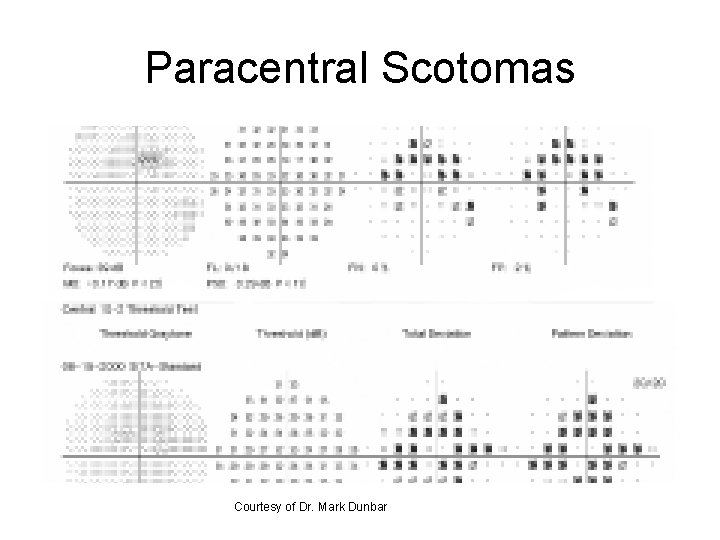
Revised Recommendations on Screening for Retinopathy • Parafoveal loss of visual sensitivity may appear before changes are seen on fundus evaluation • Many instances where retinopathy was unrecognized for years as field changes were dismissed as “non-specific” until the damage was severe • 10 -2 VF should always be repeated promptly when central or parafoveal changes are observed to determine if they are repeatable • Advanced toxicity shows well-developed paracentral scotoma
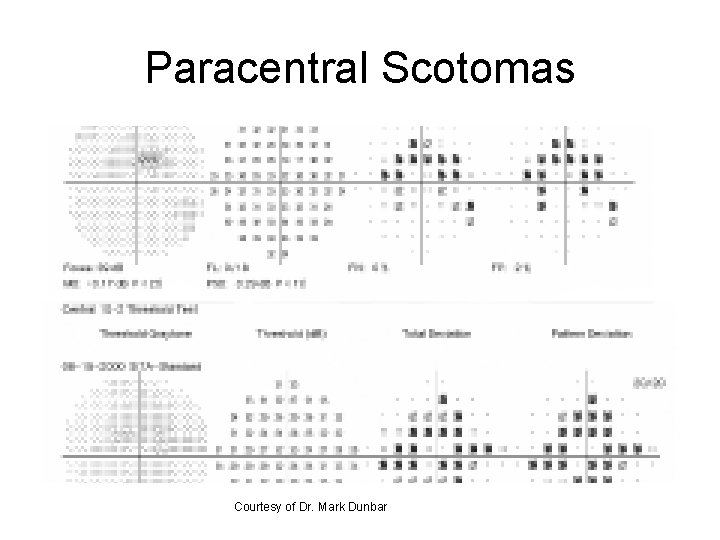
Paracentral Scotomas Courtesy of Dr. Mark Dunbar
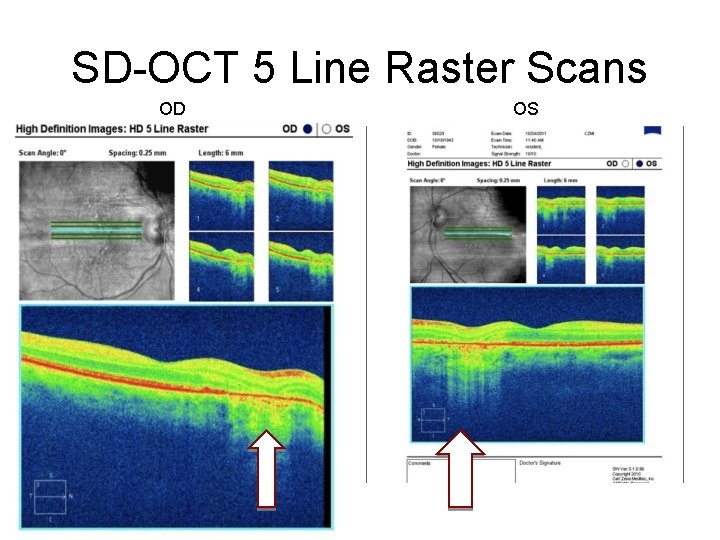
Revised Recommendations on Screening for Retinopathy • SD-OCT can show localized thinning of the parafoveal retinal layers confirming toxicity – not appreciable with time-domain OCT – changes maybe visible prior to VF defects • Fundus autofluorescence may reveal subtle RPE defects with reduced auto. FL or show areas of early photoreceptor damage • MF-ERG can objectively document localized paracentral ERG depression in early retinopathy
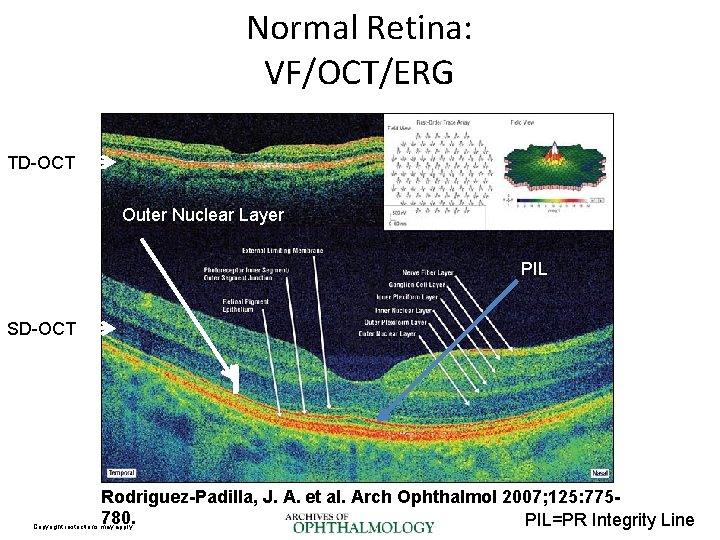
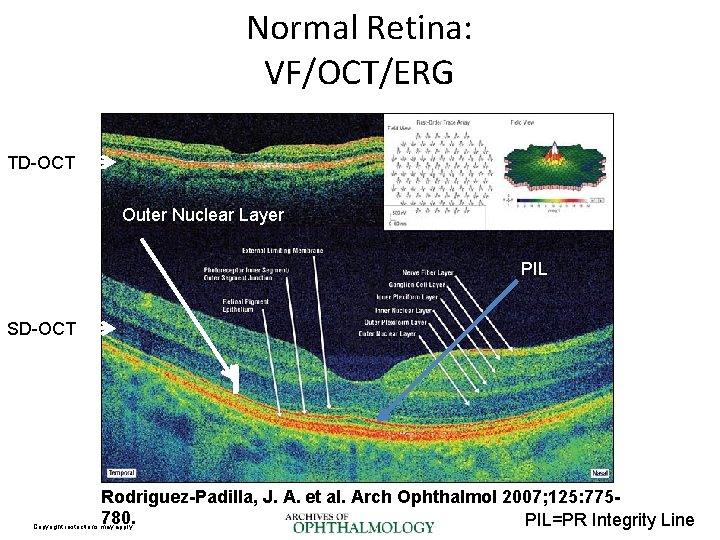
Normal Retina: VF/OCT/ERG TD-OCT Outer Nuclear Layer PIL SD-OCT Rodriguez-Padilla, J. A. et al. Arch Ophthalmol 2007; 125: 775780. PIL=PR Integrity Line Copyright restrictions may apply.
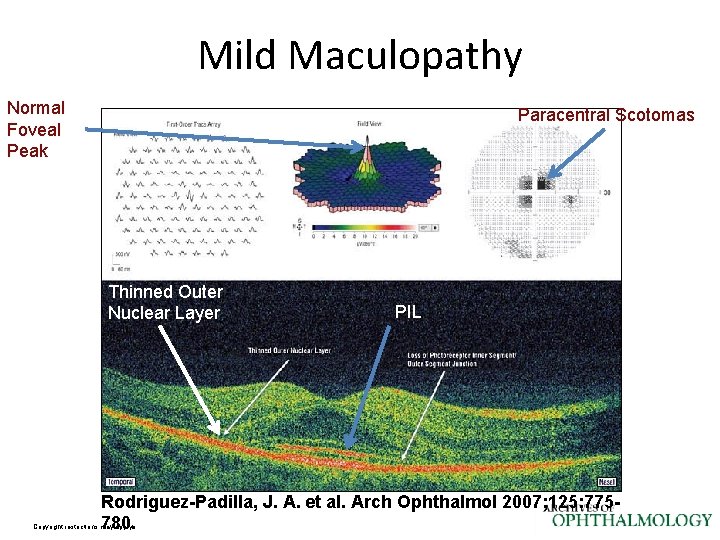
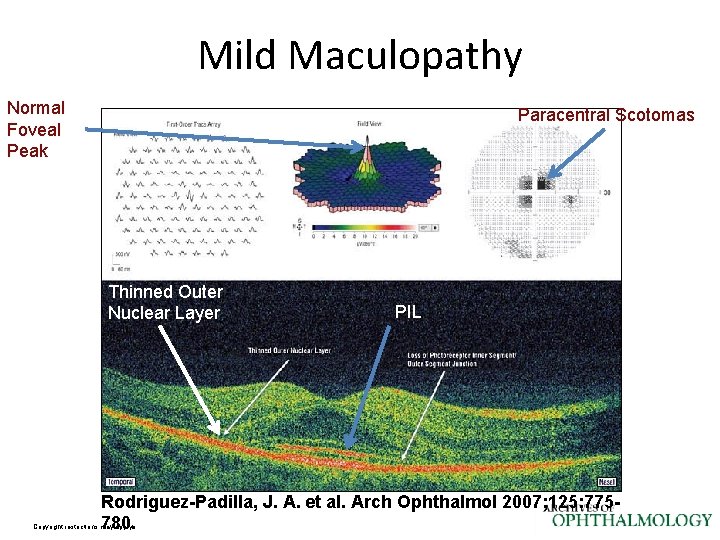
Mild Maculopathy Normal Foveal Peak Paracentral Scotomas Thinned Outer Nuclear Layer PIL Rodriguez-Padilla, J. A. et al. Arch Ophthalmol 2007; 125: 775780. Copyright restrictions may apply.
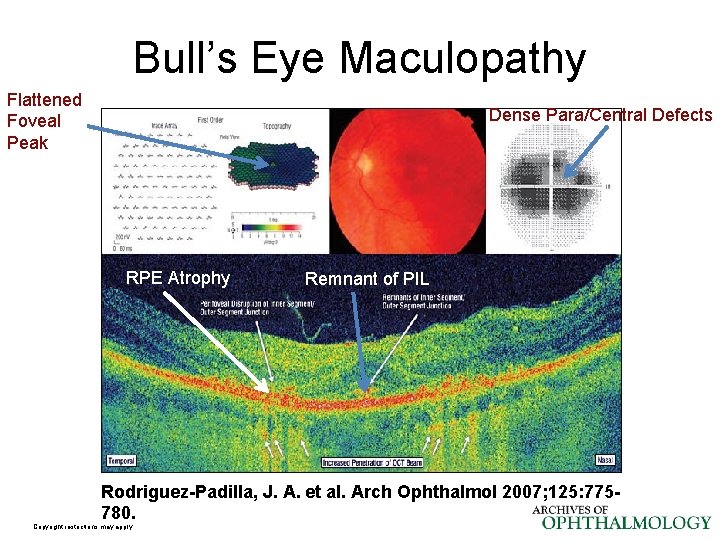
Bull’s Eye Maculopathy Flattened Foveal Peak Dense Para/Central Defects RPE Atrophy Remnant of PIL Rodriguez-Padilla, J. A. et al. Arch Ophthalmol 2007; 125: 775780. Copyright restrictions may apply.
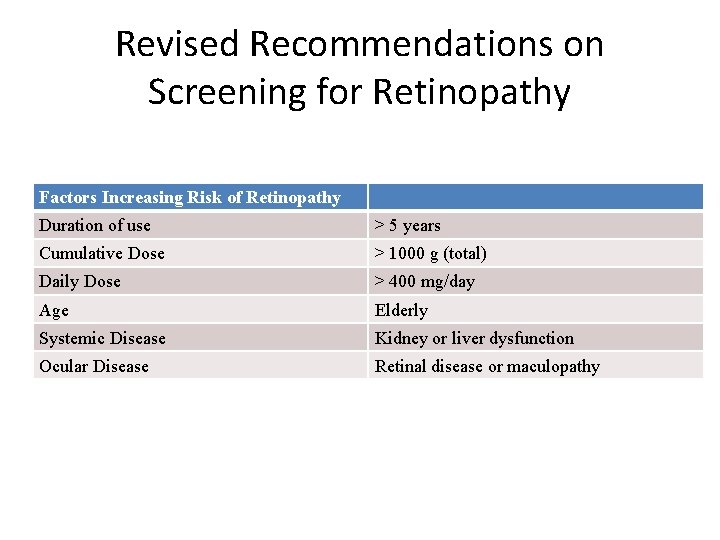
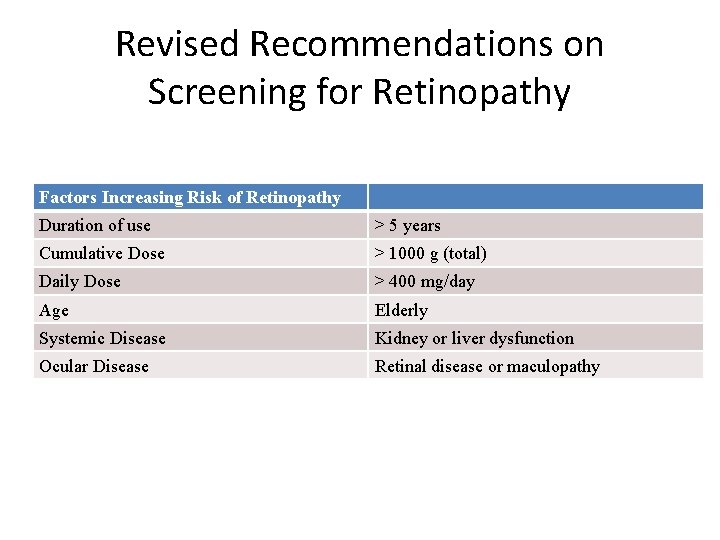
Revised Recommendations on Screening for Retinopathy Factors Increasing Risk of Retinopathy Duration of use > 5 years Cumulative Dose > 1000 g (total) Daily Dose > 400 mg/day Age Elderly Systemic Disease Kidney or liver dysfunction Ocular Disease Retinal disease or maculopathy
Revised Recommendations on Screening for Retinopathy • Older literature focused on daily dose/kg whereas newer literature emphasizes cumulative dose as the most critical factor – Initial baseline then screening for toxicity should be initiated no later than 5 years after starting the medication
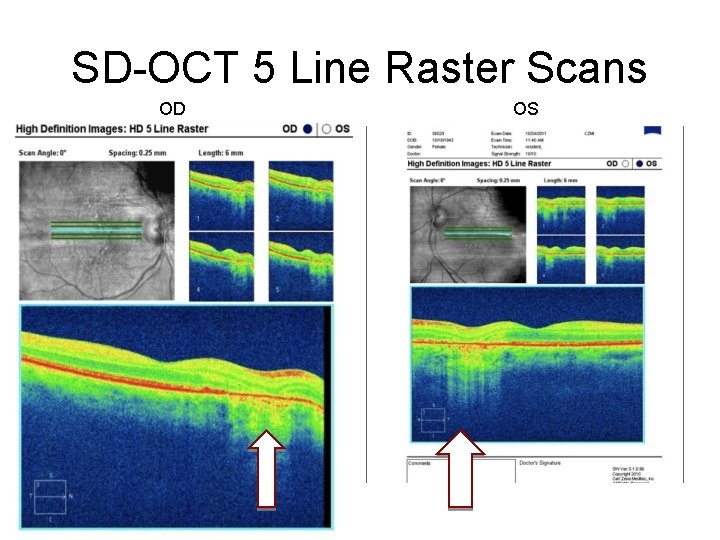
SD-OCT 5 Line Raster Scans OD OS
Case 4
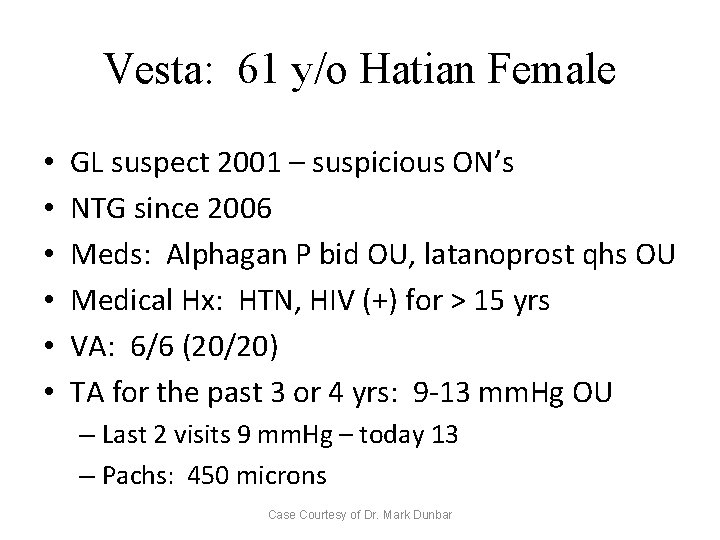
Vesta: 61 y/o Hatian Female • • • GL suspect 2001 – suspicious ON’s NTG since 2006 Meds: Alphagan P bid OU, latanoprost qhs OU Medical Hx: HTN, HIV (+) for > 15 yrs VA: 6/6 (20/20) TA for the past 3 or 4 yrs: 9 -13 mm. Hg OU – Last 2 visits 9 mm. Hg – today 13 – Pachs: 450 microns Case Courtesy of Dr. Mark Dunbar
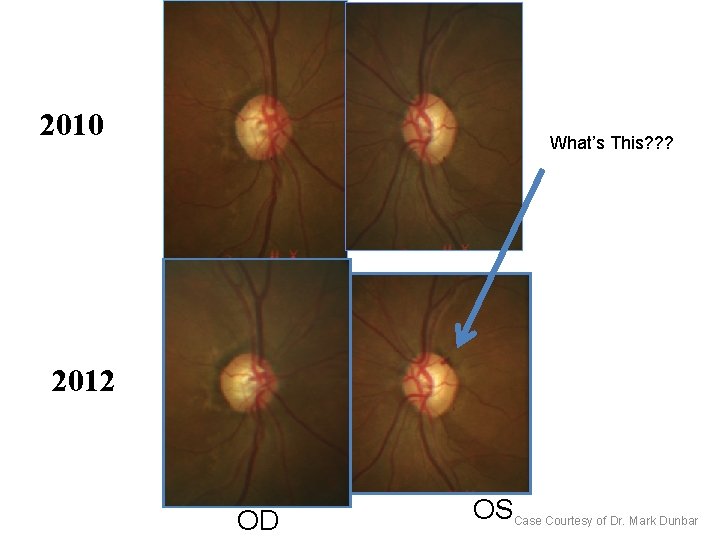
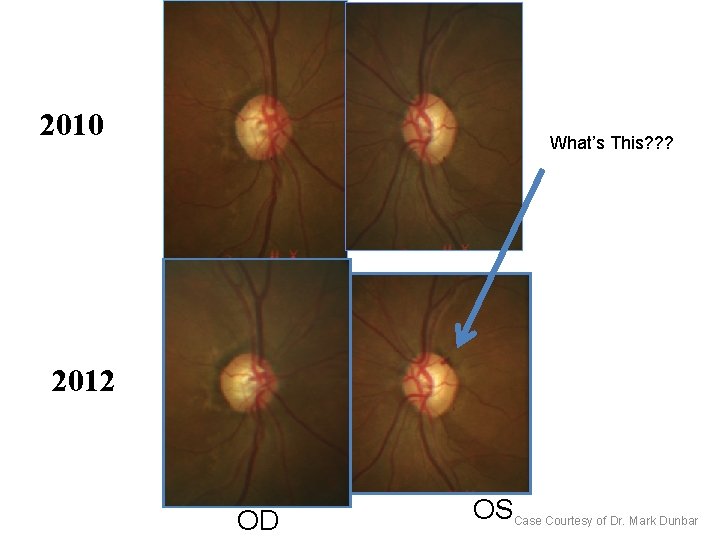
2010 What’s This? ? ? 2012 OD OSCase Courtesy of Dr. Mark Dunbar
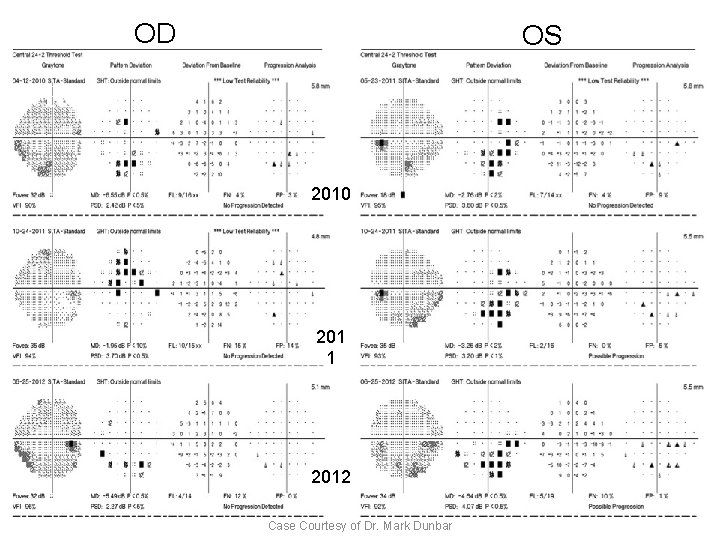
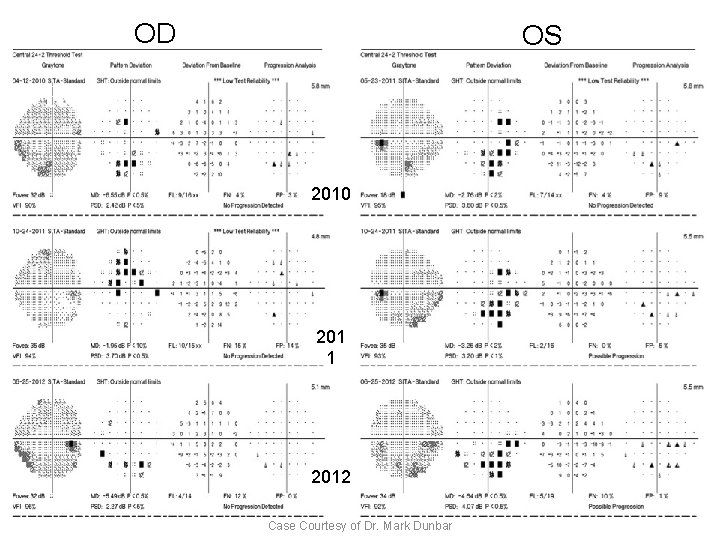
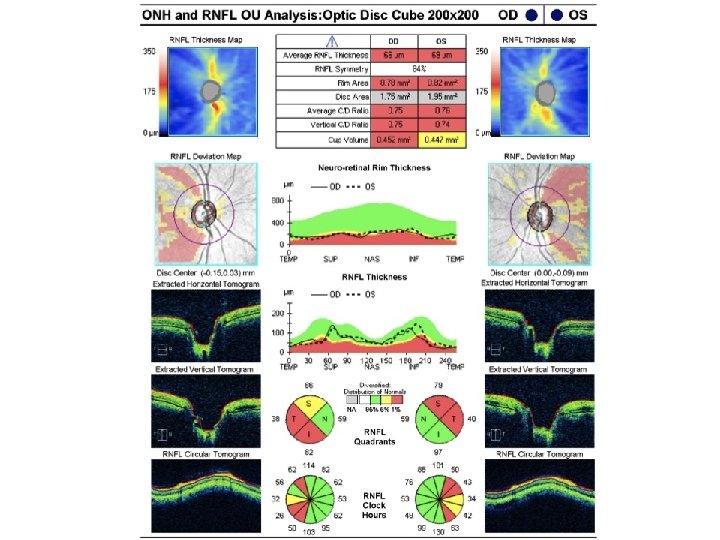
OD OS RE 2010 201 1 2012 Case Courtesy of Dr. Mark Dunbar
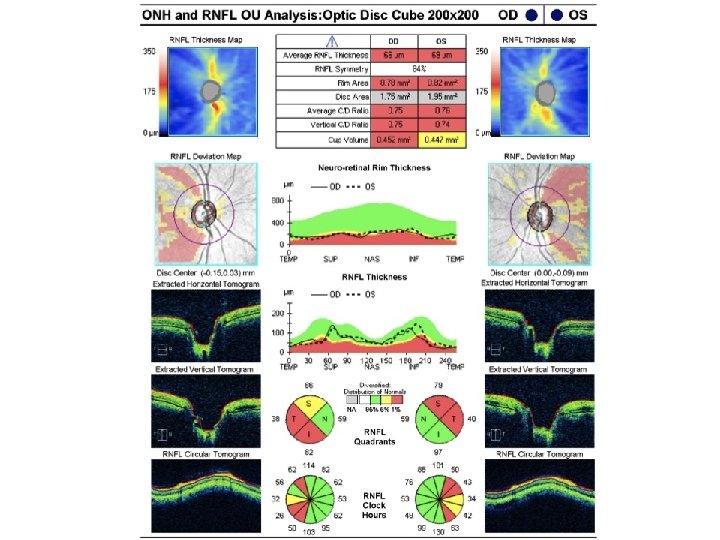
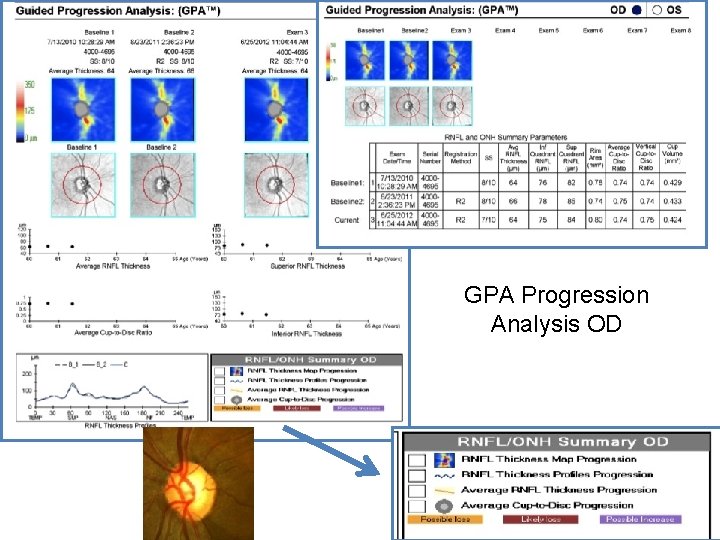
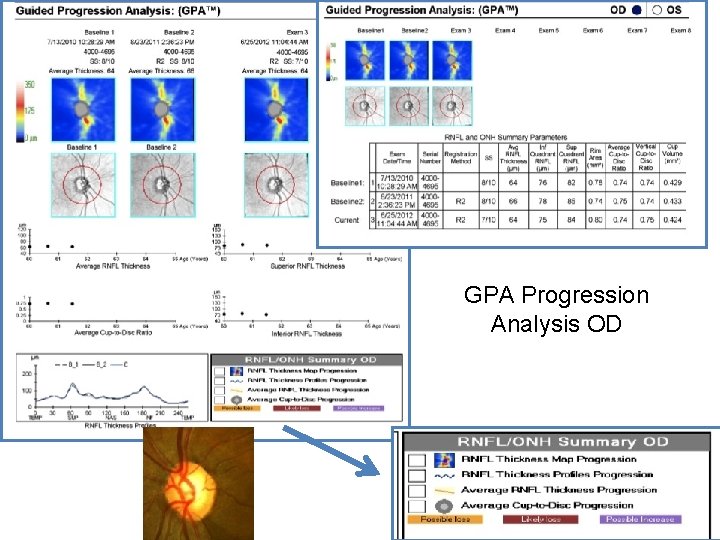
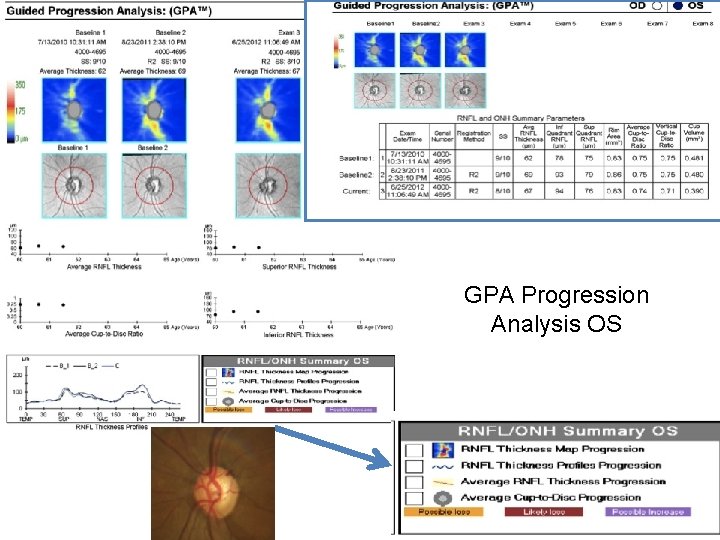
GPA Progression Analysis OD
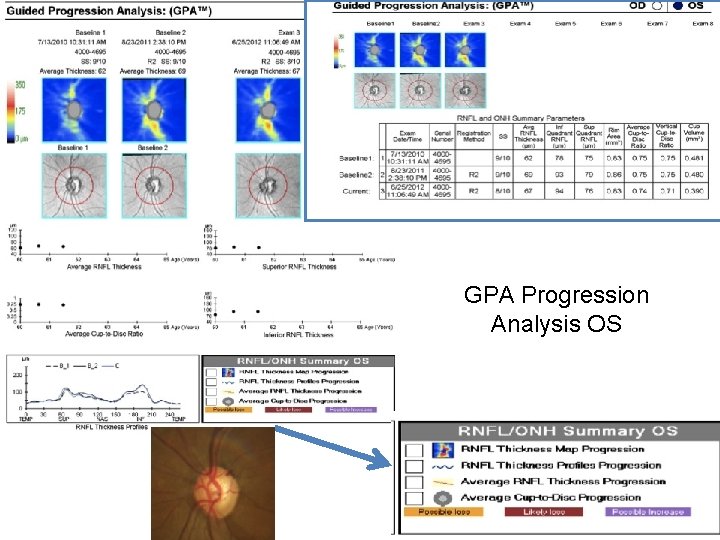
GPA Progression Analysis OS
Vesta: 61 y/o Hatian Female • NTG OU with thin corneas • OS: – Optic Nerve and HVF show trend towards progression…. • OCT shows no change Case Courtesy Dr. Mark Dunbar
Vesta: 61 y/o Hatian Female • How do you manage this patient? – Currently on latanoprost and alphagan OU • This is what was done…. – Stopped Alphagan P – Switch to Combigan bid OU – Continue with latanoprost qhs OU – RTC 1 mo Case Courtesy of Dr. Mark Dunbar
OCT Retinal Images
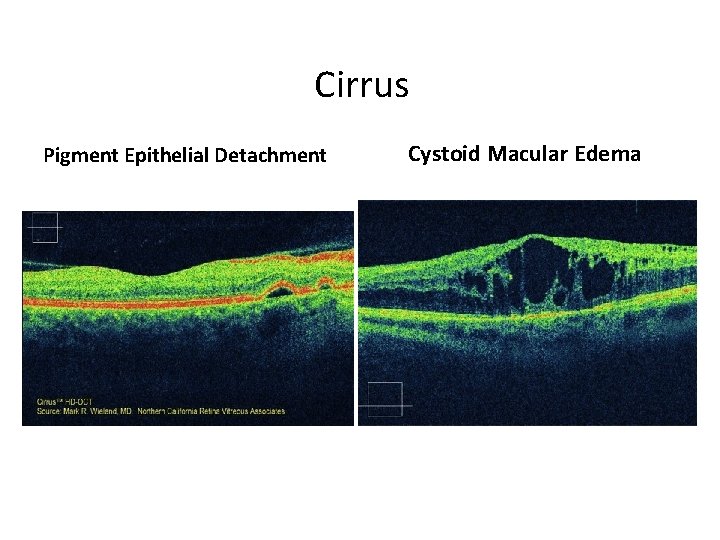
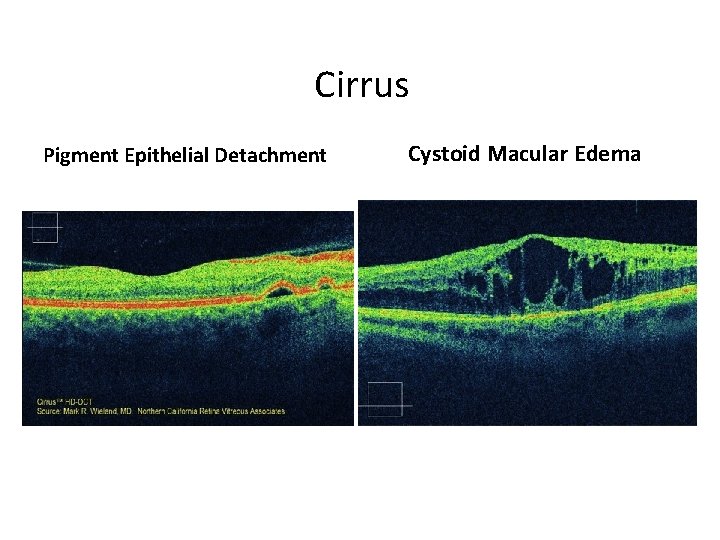
Cirrus Pigment Epithelial Detachment Cystoid Macular Edema
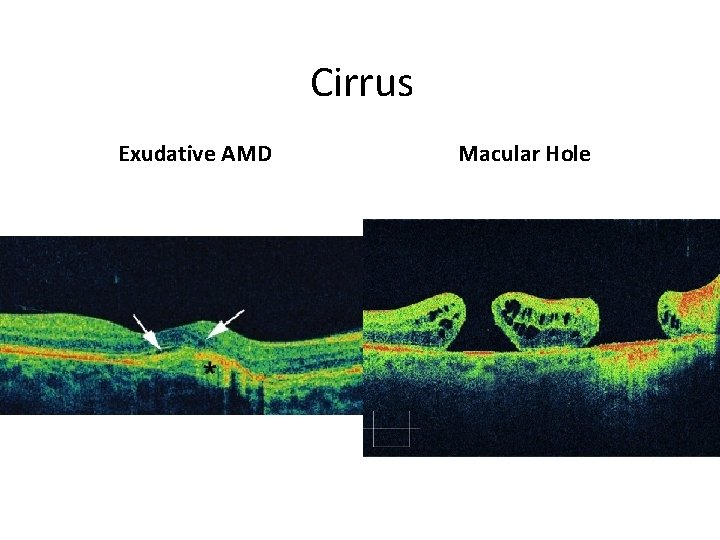
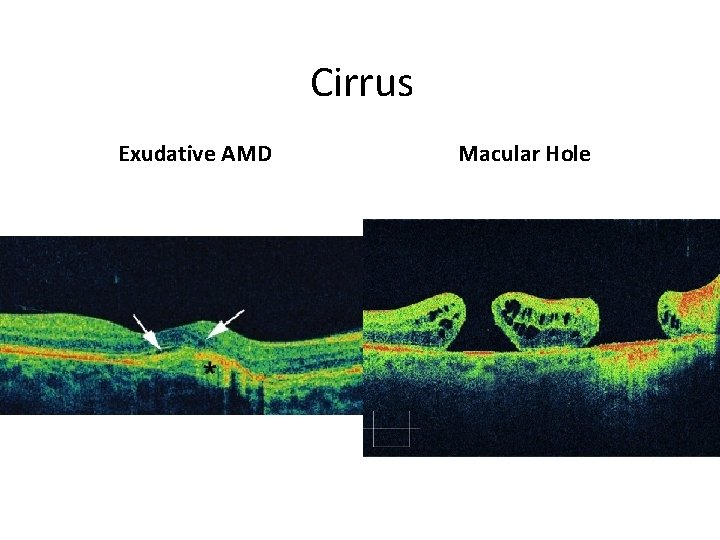
Cirrus Exudative AMD Macular Hole
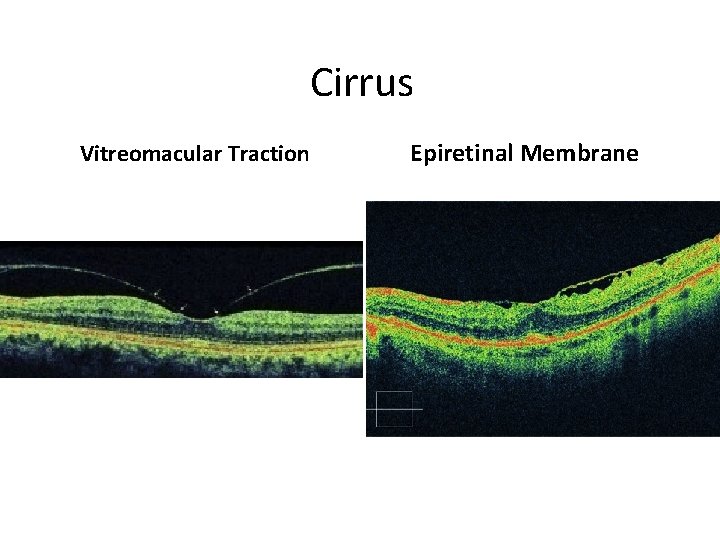
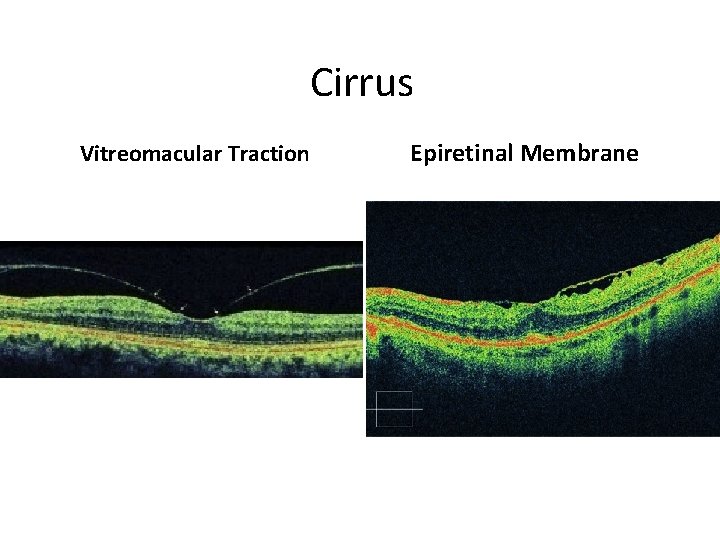
Cirrus Vitreomacular Traction Epiretinal Membrane
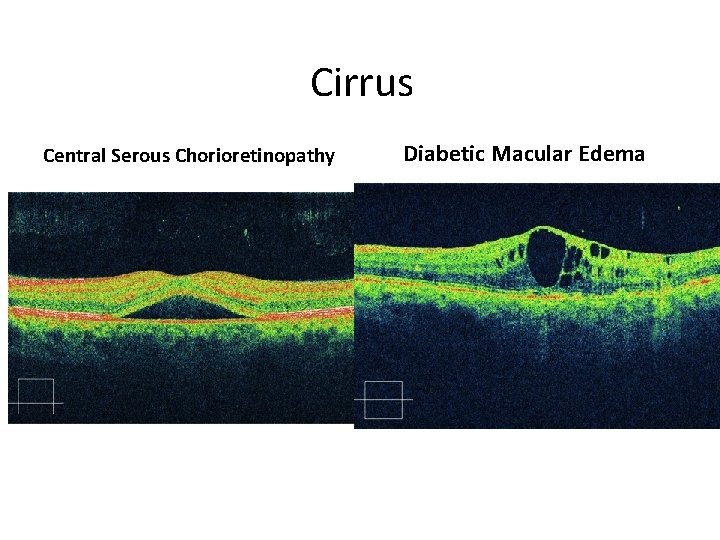
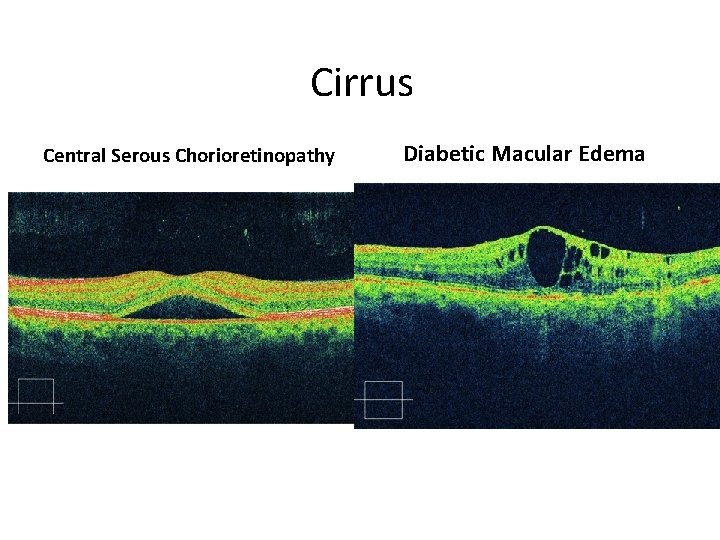
Cirrus Central Serous Chorioretinopathy Diabetic Macular Edema

Thank You! 69