Imageguided intensitymodulated radiotherapy for postoperative highrisk oral cavity

![n Zeidan et al [1] n Even under every other day using IGRT n n Zeidan et al [1] n Even under every other day using IGRT n](https://slidetodoc.com/presentation_image_h2/31fb7c1c1d019ca8b8c433bb3ef24338/image-43.jpg)
![Surgery + postoperative IMRT ± concurrent chemotherapy – Marginal misses Modality UC Davis [9] Surgery + postoperative IMRT ± concurrent chemotherapy – Marginal misses Modality UC Davis [9]](https://slidetodoc.com/presentation_image_h2/31fb7c1c1d019ca8b8c433bb3ef24338/image-47.jpg)



- Slides: 63
Image-guided intensity-modulated radiotherapy for post-operative high-risk oral cavity cancer patients – a single institution's experience Far Eastern Memorial Hospital, Division of Radiation Oncology Department of Radiology Chen-Hsi Hsieh M. D. , Ph. D. 1
Conflict of interest: None 2

Warnakulasuriya S, Oral Oncol 2009; 45: 309 3
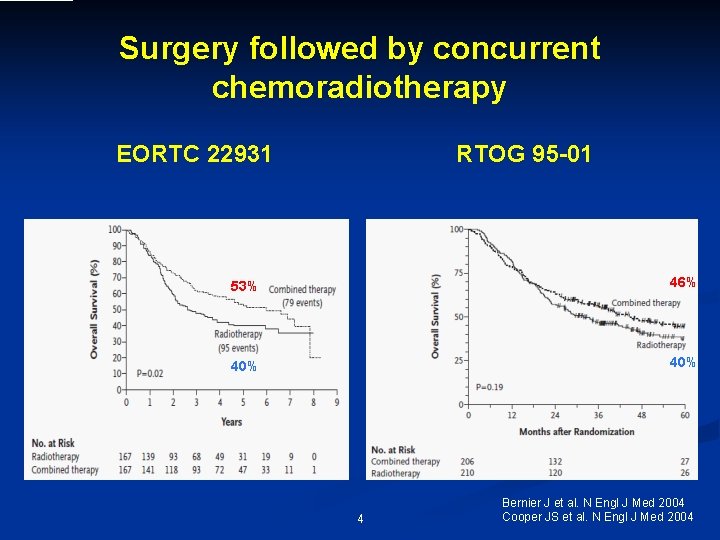
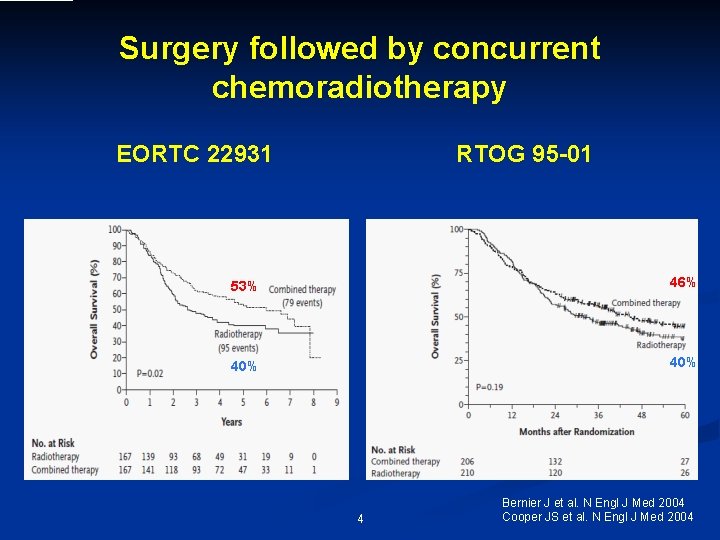
Surgery followed by concurrent chemoradiotherapy EORTC 22931 RTOG 95 -01 53% 46% 40% 4 Bernier J et al. N Engl J Med 2004 Cooper JS et al. N Engl J Med 2004
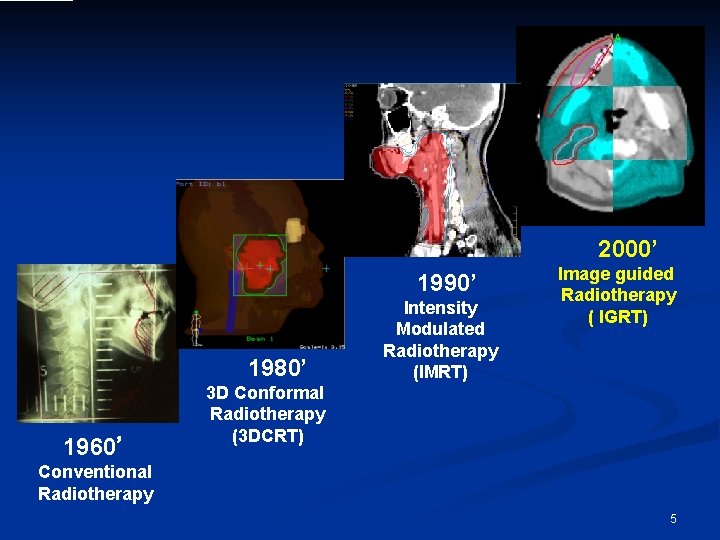
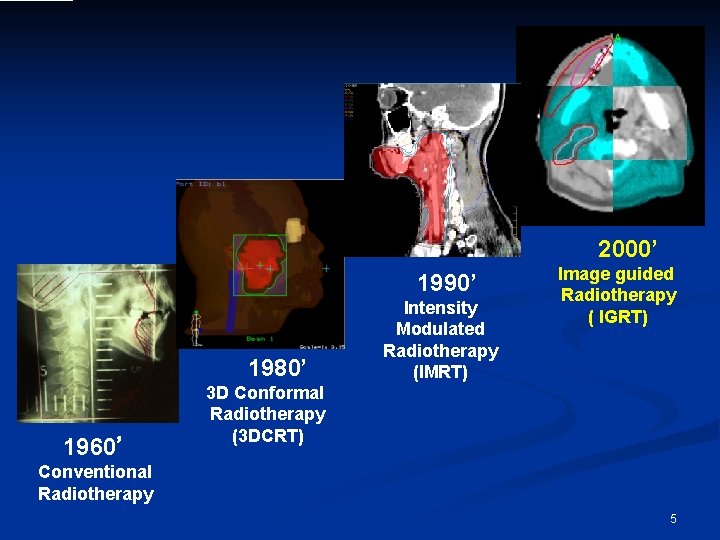
2000’ 1990’ 1980’ 1960’ Intensity Modulated Radiotherapy (IMRT) Image guided Radiotherapy ( IGRT) 3 D Conformal Radiotherapy (3 DCRT) Conventional Radiotherapy 5
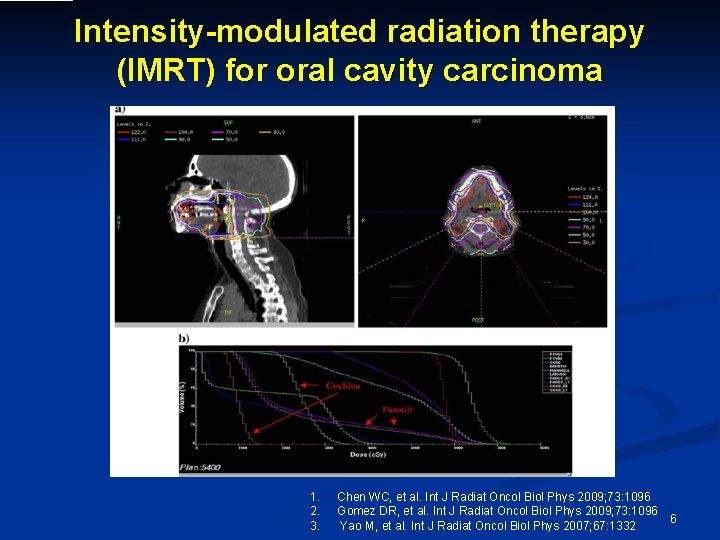
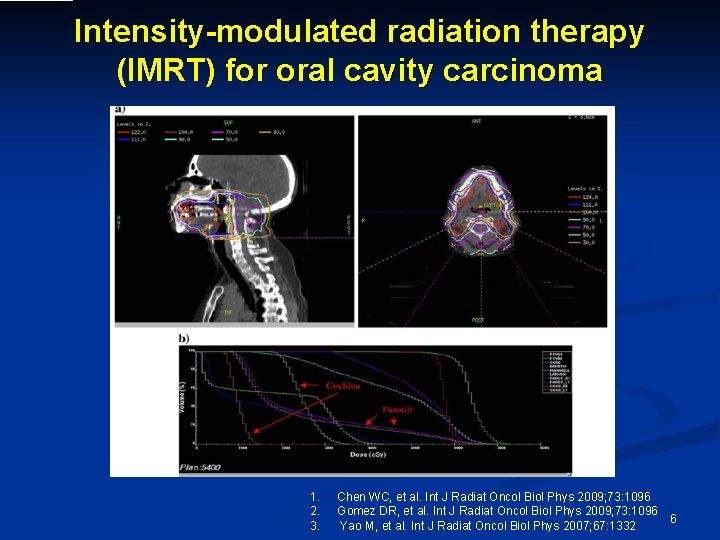
Intensity-modulated radiation therapy (IMRT) for oral cavity carcinoma 1. 2. 3. Chen WC, et al. Int J Radiat Oncol Biol Phys 2009; 73: 1096 Gomez DR, et al. Int J Radiat Oncol Biol Phys 2009; 73: 1096 Yao M, et al. Int J Radiat Oncol Biol Phys 2007; 67: 1332 6
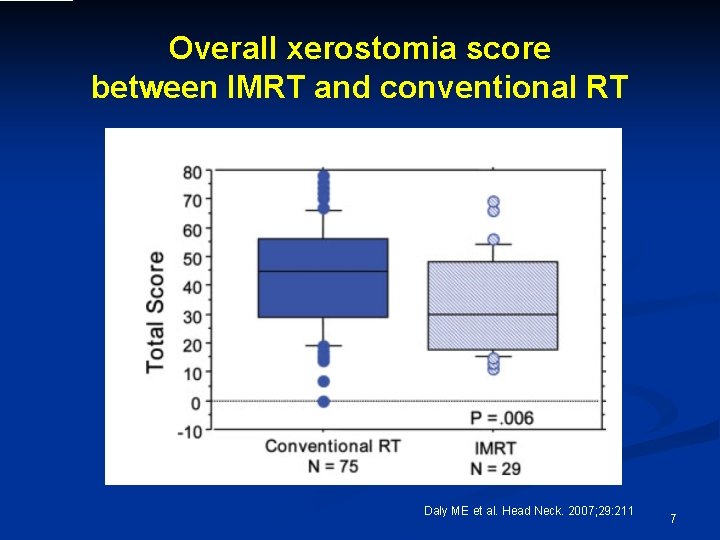
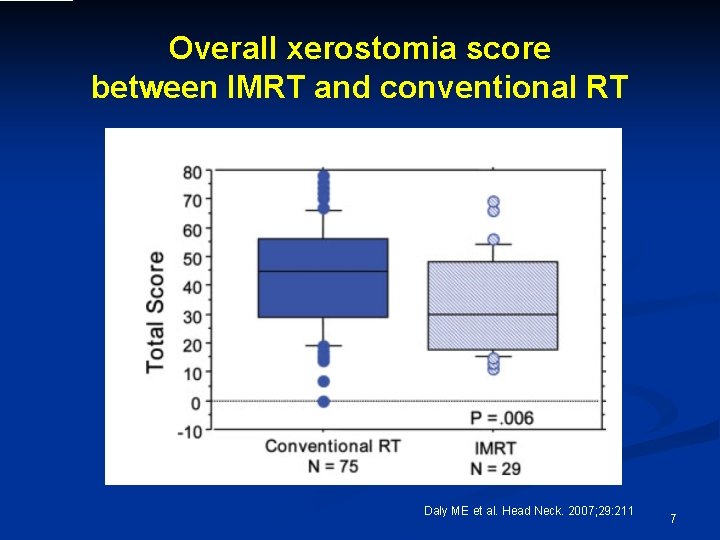
Overall xerostomia score between IMRT and conventional RT Daly ME et al. Head Neck. 2007; 29: 211 7
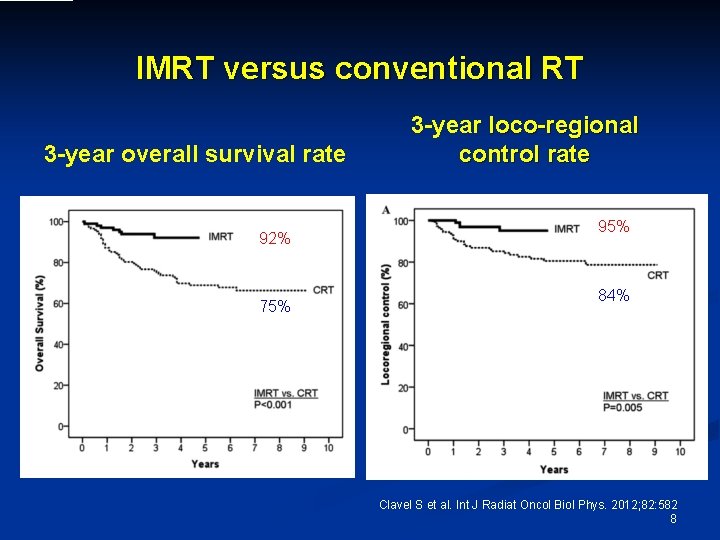
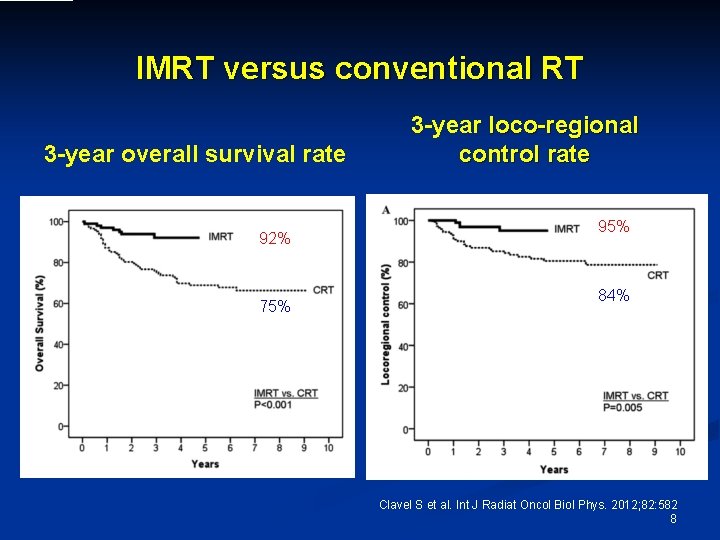
IMRT versus conventional RT 3 -year overall survival rate 92% 75% 3 -year loco-regional control rate 95% 84% Clavel S et al. Int J Radiat Oncol Biol Phys. 2012; 82: 582 8
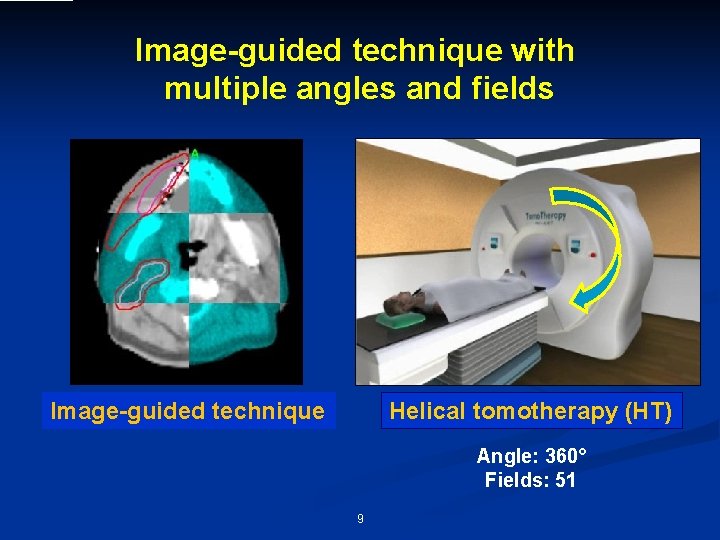
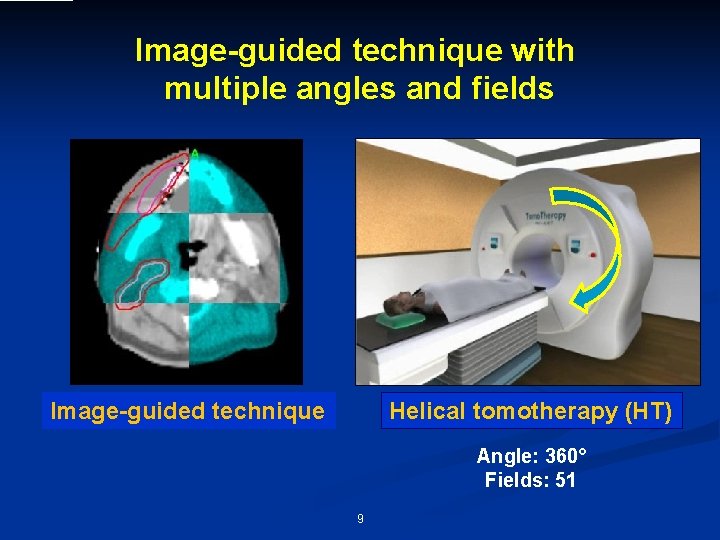
Image-guided technique with multiple angles and fields Image-guided technique Helical tomotherapy (HT) Angle: 360° Fields: 51 9
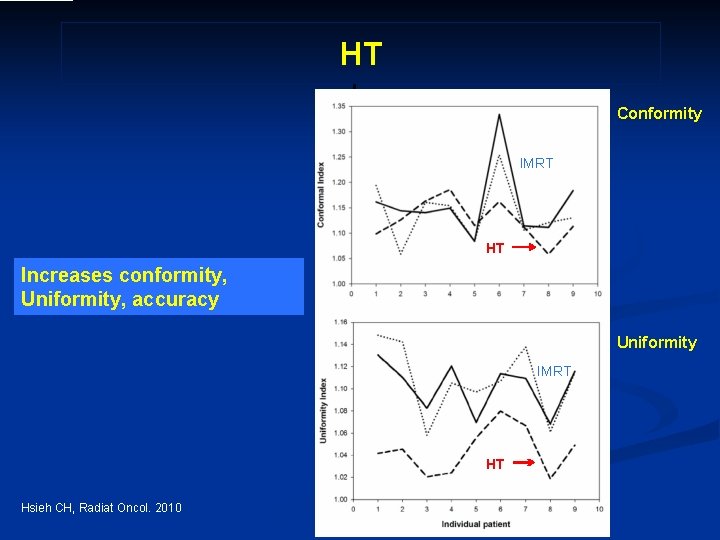
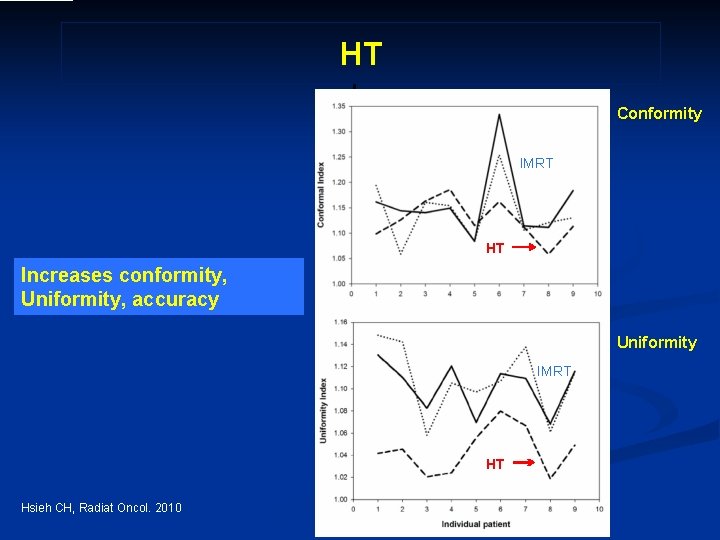
HT Conformity IMRT HT Increases conformity, Uniformity, accuracy Uniformity IMRT HT Hsieh CH, Radiat Oncol. 2010 10
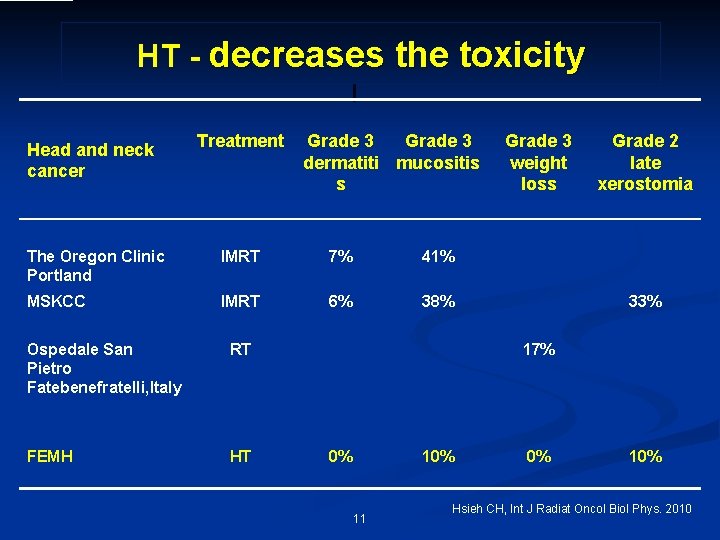
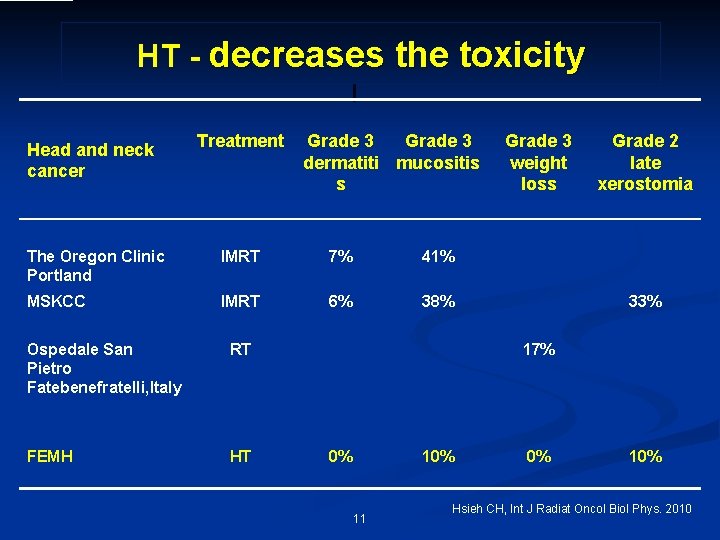
HT - decreases the toxicity Head and neck cancer Treatment Grade 3 dermatiti mucositis s The Oregon Clinic Portland IMRT 7% 41% MSKCC IMRT 6% 38% Ospedale San Pietro Fatebenefratelli, Italy RT FEMH HT Grade 3 weight loss Grade 2 late xerostomia 33% 17% 0% 11 0% 10% Hsieh CH, Int J Radiat Oncol Biol Phys. 2010
Can IGRT in crease IGRT thehasoavpoeternall s r vival and failure tiality tou a v than I local co nt. Mr. Ro. Tldoroeaisd tmeargtinhala n IMRT like IM RT is better than 2 DRT? 12
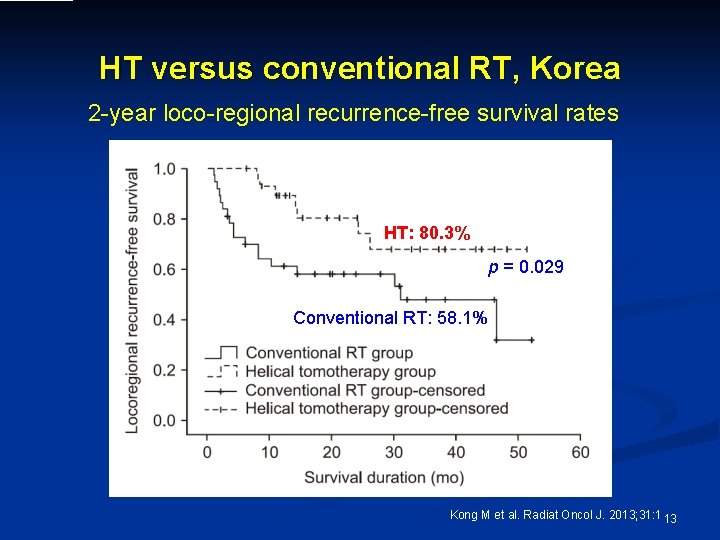
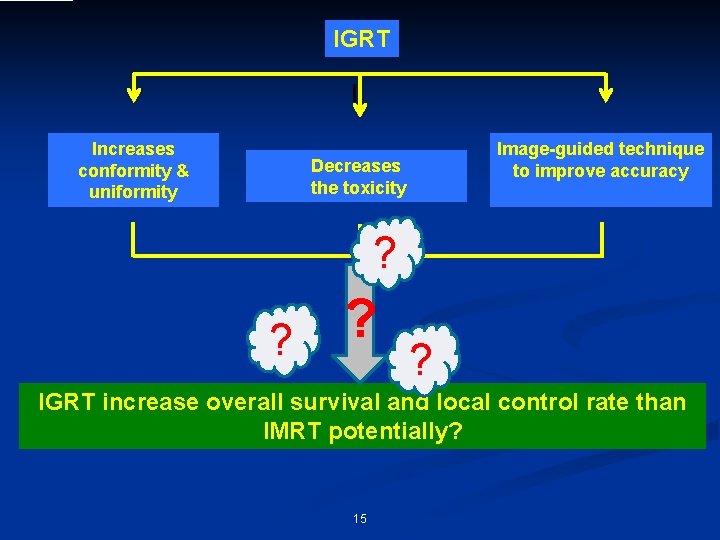
HT versus conventional RT, Korea 2 -year loco-regional recurrence-free survival rates HT: 80. 3% p = 0. 029 Conventional RT: 58. 1% Kong M et al. Radiat Oncol J. 2013; 31: 1 13
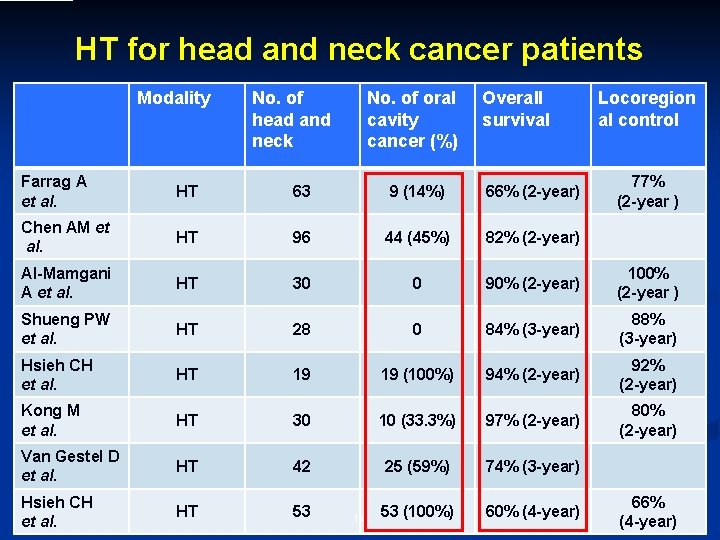
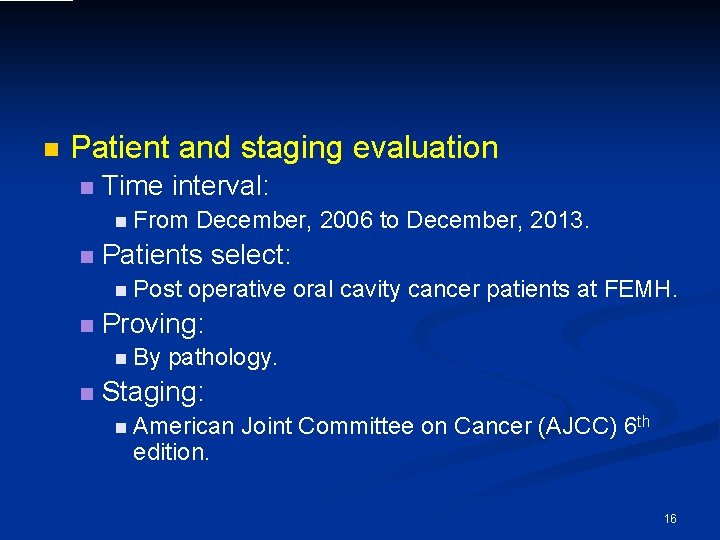
HT for head and neck cancer patients Modality No. of head and neck No. of oral cavity cancer (%) Overall survival Locoregion al control Farrag A et al. HT 63 9 (14%) 66% (2 -year) Chen AM et al. HT 96 44 (45%) 82% (2 -year) Al-Mamgani A et al. HT 30 0 90% (2 -year) 100% (2 -year ) Shueng PW et al. HT 28 0 84% (3 -year) 88% (3 -year) Hsieh CH et al. HT 19 19 (100%) 94% (2 -year) 92% (2 -year) Kong M et al. HT 30 10 (33. 3%) 97% (2 -year) 80% (2 -year) Van Gestel D et al. HT 42 25 (59%) 74% (3 -year) Hsieh CH et al. HT 53 53 (100%) 60% (4 -year) 14 77% (2 -year ) 66% (4 -year)
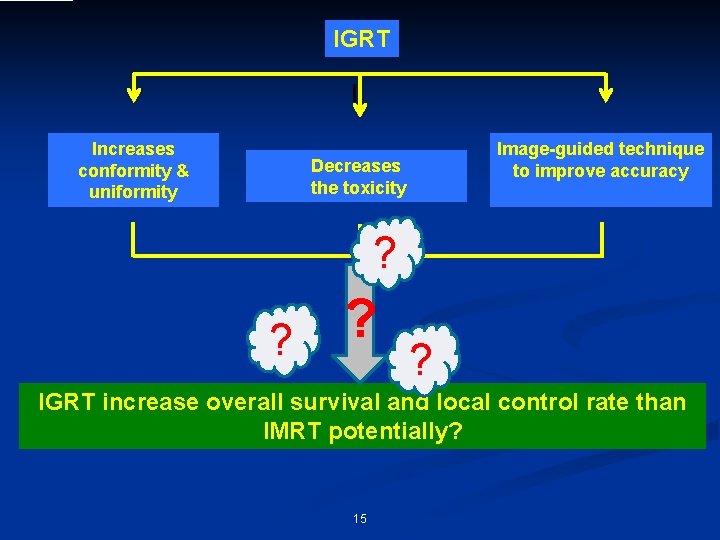
IGRT Increases conformity & uniformity Decreases the toxicity Image-guided technique to improve accuracy ? ? ? ? IGRT increase overall survival and local control rate than IMRT potentially? 15
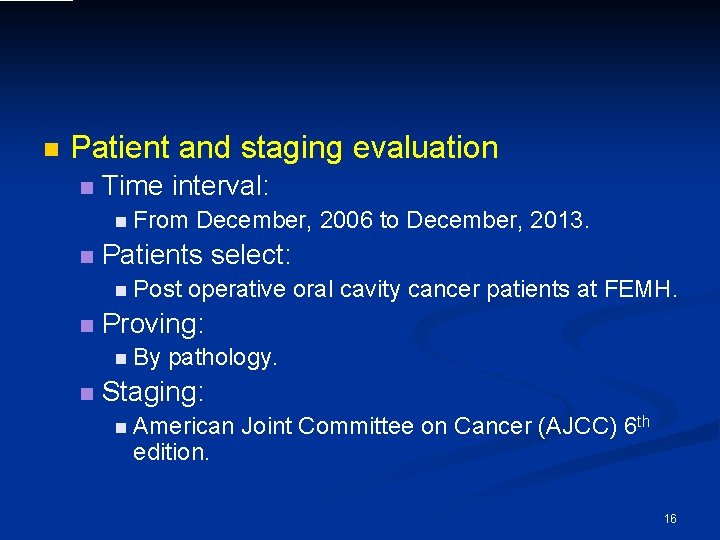
n Patient and staging evaluation n Time interval: n From n Patients select: n Post n operative oral cavity cancer patients at FEMH. Proving: n By n December, 2006 to December, 2013. pathology. Staging: n American edition. Joint Committee on Cancer (AJCC) 6 th 16
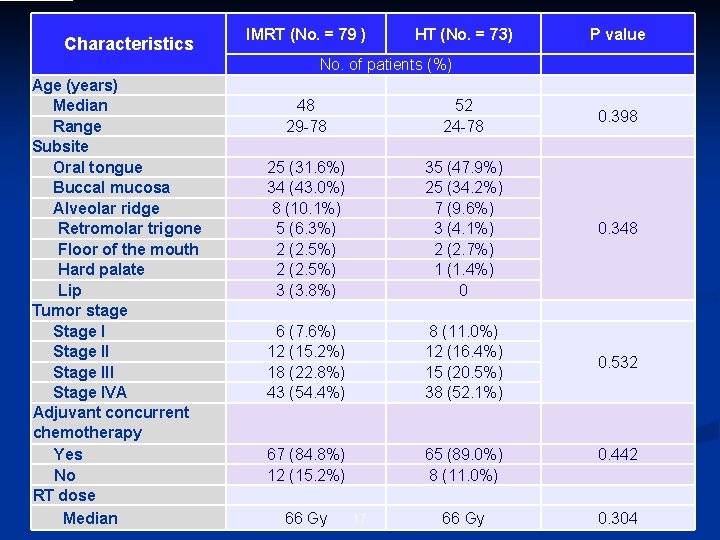
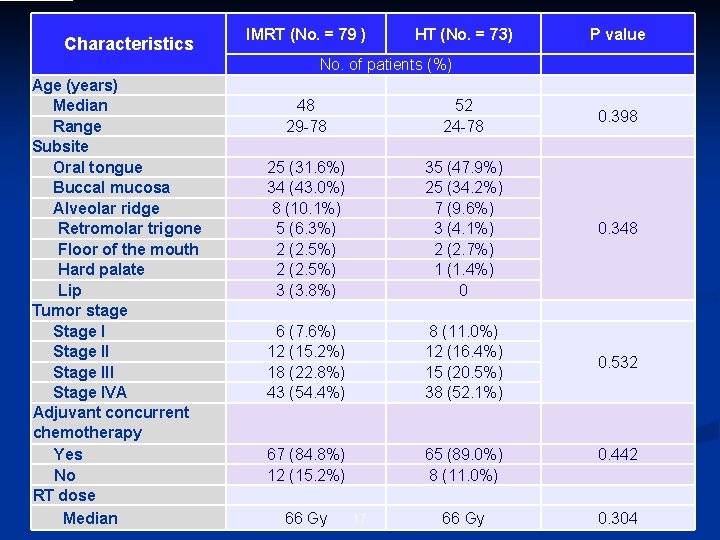
Characteristics IMRT (No. = 79 ) HT (No. = 73) P value No. of patients (%) Age (years) Median Range Subsite Oral tongue Buccal mucosa Alveolar ridge Retromolar trigone Floor of the mouth Hard palate Lip Tumor stage Stage III Stage IVA Adjuvant concurrent chemotherapy Yes No RT dose Median 48 29 -78 52 24 -78 0. 398 25 (31. 6%) 34 (43. 0%) 8 (10. 1%) 5 (6. 3%) 2 (2. 5%) 3 (3. 8%) 35 (47. 9%) 25 (34. 2%) 7 (9. 6%) 3 (4. 1%) 2 (2. 7%) 1 (1. 4%) 0 0. 348 6 (7. 6%) 12 (15. 2%) 18 (22. 8%) 43 (54. 4%) 8 (11. 0%) 12 (16. 4%) 15 (20. 5%) 38 (52. 1%) 0. 532 67 (84. 8%) 12 (15. 2%) 65 (89. 0%) 8 (11. 0%) 0. 442 66 Gy 0. 304 66 Gy 17
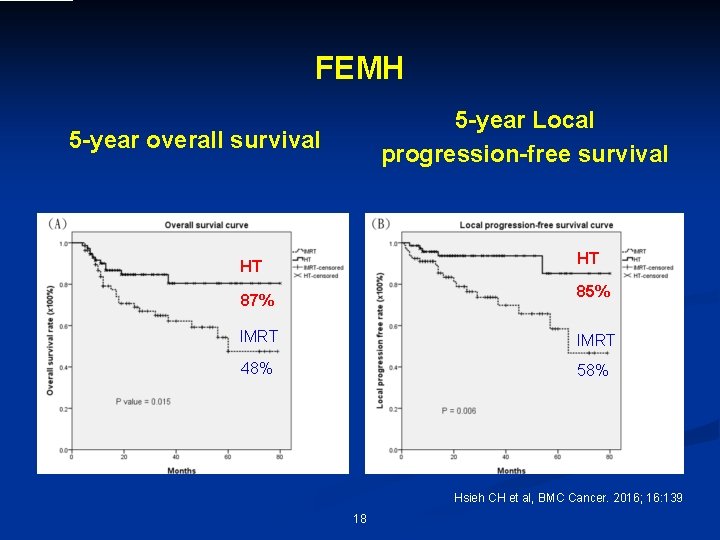
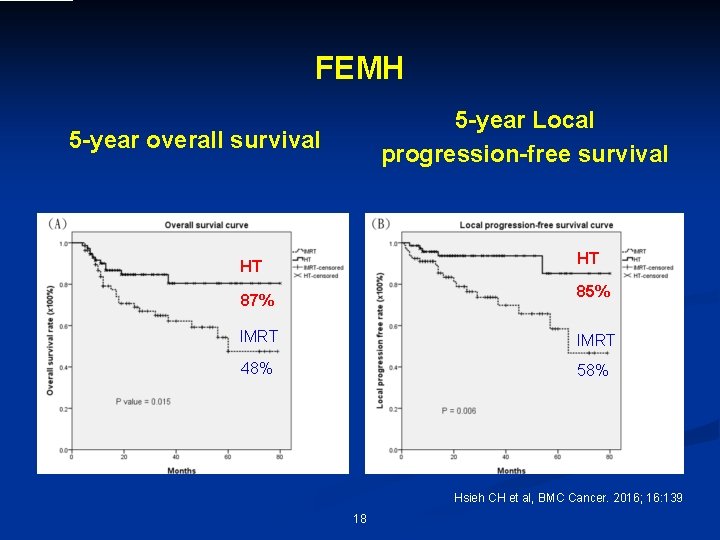
FEMH 5 -year Local progression-free survival 5 -year overall survival HT HT 85% 87% IMRT 48% 58% Hsieh CH et al, BMC Cancer. 2016; 16: 139 18
IGR T ha Are tsha ep se d a o failu tentialit ta comparteitb halne y to avo IMR w. T idthid p marr evio gina us o published es l series? 19
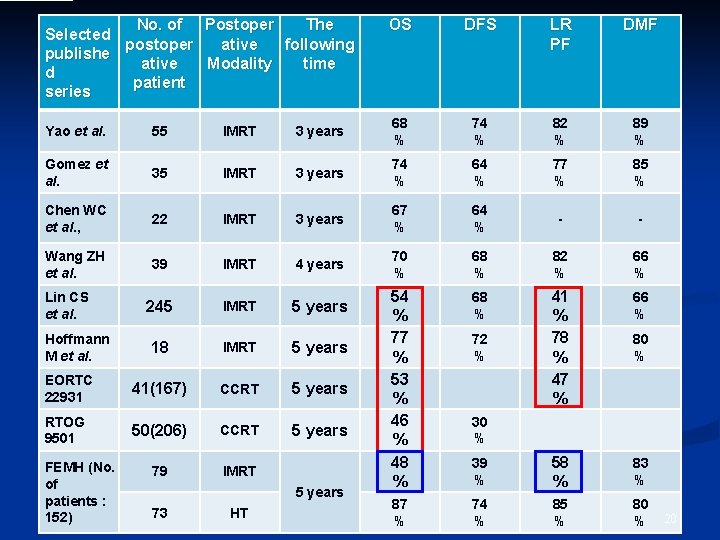
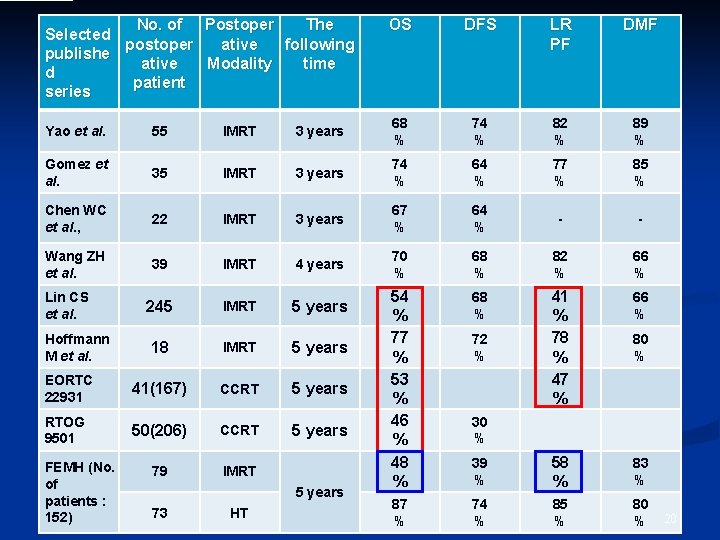
No. of Postoper The Selected postoper ative following publishe ative Modality time d patient series OS DFS LR PF DMF Yao et al. 55 IMRT 3 years 68 % 74 % 82 % 89 % Gomez et al. 35 IMRT 3 years 74 % 64 % 77 % 85 % Chen WC et al. , 22 IMRT 3 years 67 % 64 % - - Wang ZH et al. 39 IMRT 4 years 70 % 68 % 82 % 66 % 245 IMRT 5 years 68 % IMRT 5 years EORTC 22931 41(167) CCRT 5 years 41 % 78 % 47 % 66 % 18 RTOG 9501 50(206) CCRT 5 years 79 IMRT 54 % 77 % 53 % 46 % 48 % 39 % 58 % 83 % 87 % 74 % 85 % 80 % Lin CS et al. Hoffmann M et al. FEMH (No. of patients : 152) 5 years 73 HT 72 % 80 % 30 % 20
Yes! IMRT’s data is com patible with other reports! IGRT ha s a poten tiality to avoid ma failure th rginal a n HT provides b. IMe. Rtt. Tedroersesu lts IMRT: It could be believ ed probably……. than 21
Why does HT provide better outcom es than IMRT? IGRT h as a po tentialit y to avo failure id marg than IM inal RT doe s 22
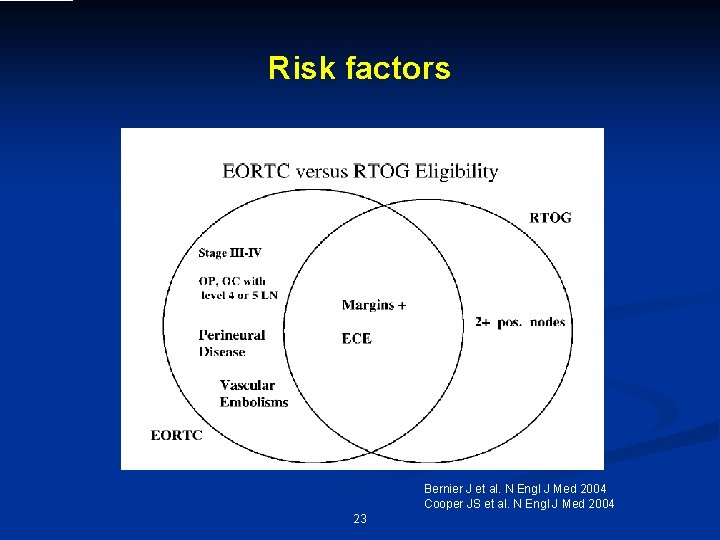
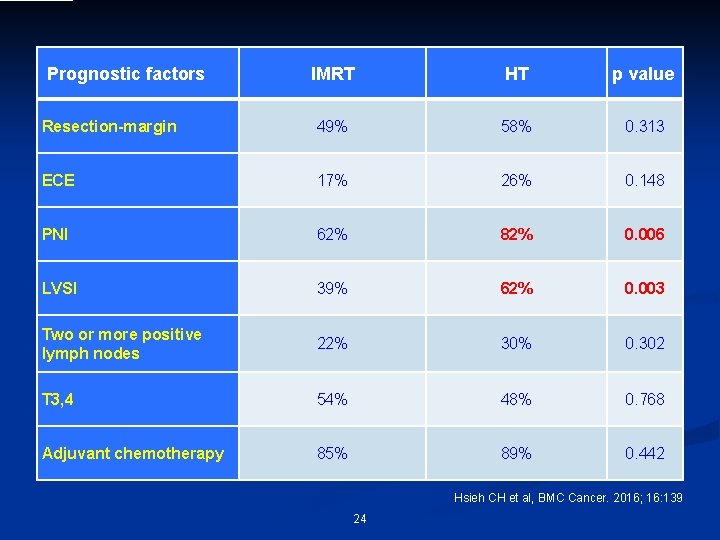
Risk factors Bernier J et al. N Engl J Med 2004 Cooper JS et al. N Engl J Med 2004 23
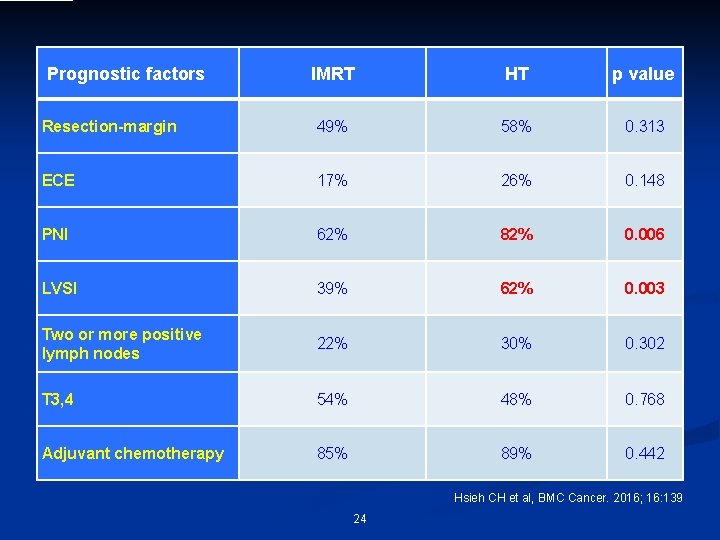
Prognostic factors IMRT HT p value Resection-margin 49% 58% 0. 313 ECE 17% 26% 0. 148 PNI 62% 82% 0. 006 LVSI 39% 62% 0. 003 Two or more positive lymph nodes 22% 30% 0. 302 T 3, 4 54% 48% 0. 768 Adjuvant chemotherapy 85% 89% 0. 442 Hsieh CH et al, BMC Cancer. 2016; 16: 139 24
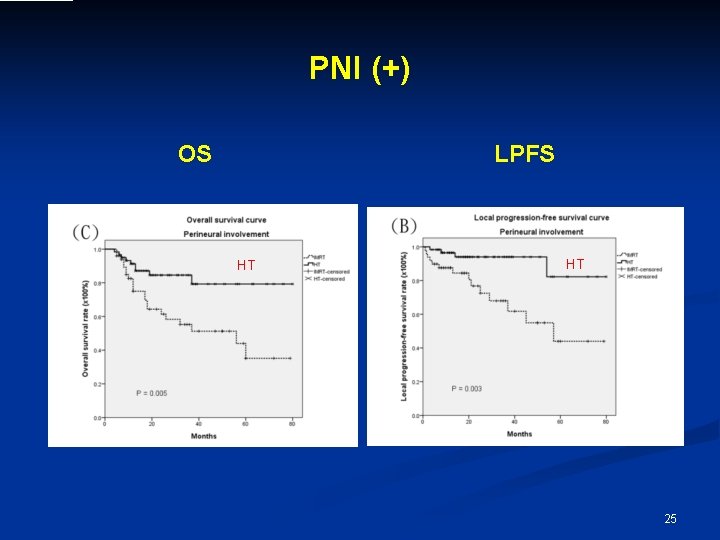
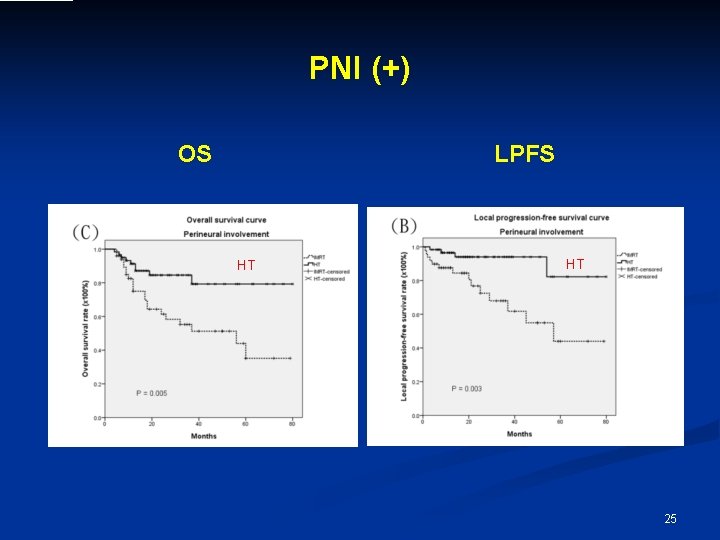
PNI (+) OS LPFS HT HT 25
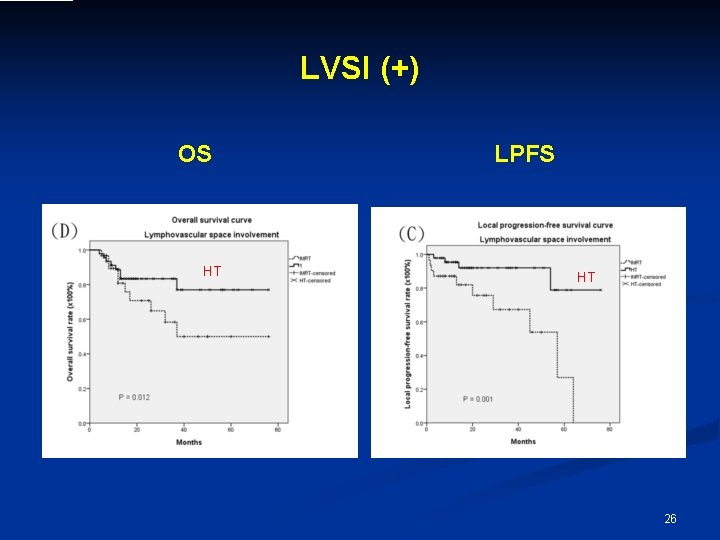
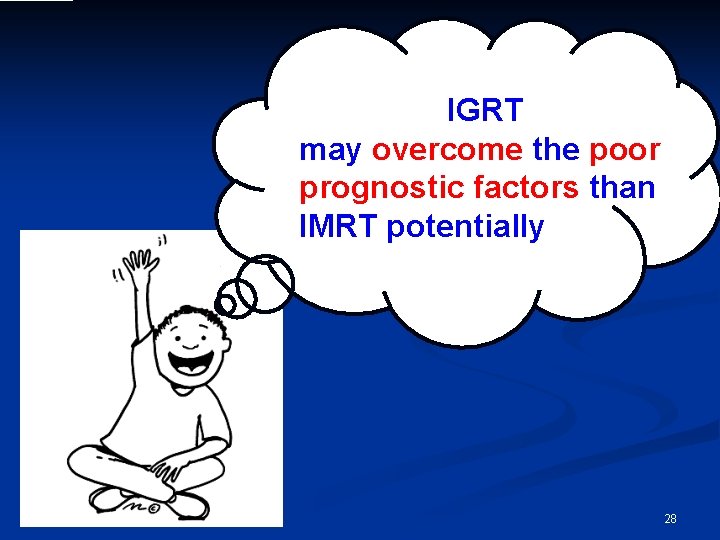
LVSI (+) OS HT LPFS HT 26
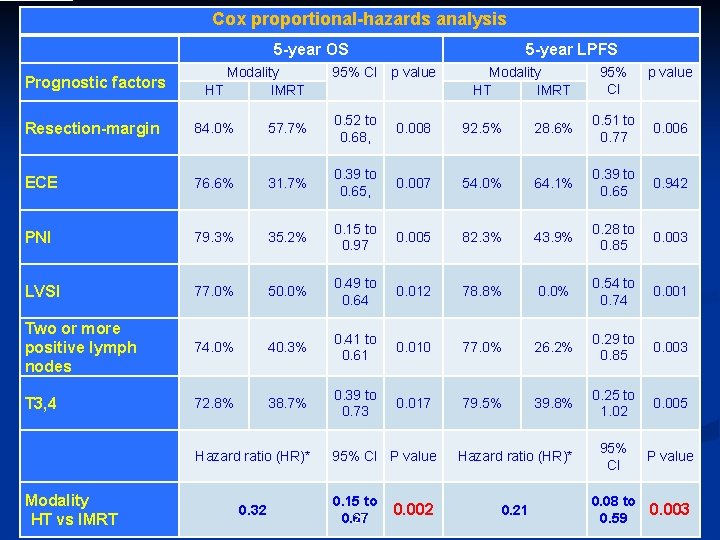
Cox proportional-hazards analysis 5 -year OS Prognostic factors Modality HT IMRT 5 -year LPFS 95% CI p value Modality HT IMRT 95% CI p value Resection-margin 84. 0% 57. 7% 0. 52 to 0. 68, 0. 008 92. 5% 28. 6% 0. 51 to 0. 77 0. 006 ECE 76. 6% 31. 7% 0. 39 to 0. 65, 0. 007 54. 0% 64. 1% 0. 39 to 0. 65 0. 942 PNI 79. 3% 35. 2% 0. 15 to 0. 97 0. 005 82. 3% 43. 9% 0. 28 to 0. 85 0. 003 LVSI 77. 0% 50. 0% 0. 49 to 0. 64 0. 012 78. 8% 0. 0% 0. 54 to 0. 74 0. 001 Two or more positive lymph nodes 74. 0% 40. 3% 0. 41 to 0. 61 0. 010 77. 0% 26. 2% 0. 29 to 0. 85 0. 003 T 3, 4 72. 8% 38. 7% 0. 39 to 0. 73 0. 017 79. 5% 39. 8% 0. 25 to 1. 02 0. 005 Hazard ratio (HR)* 95% CI P value 0. 21 0. 08 to 0. 59 0. 003 Hazard ratio (HR)* Modality HT vs IMRT 0. 32 95% CI P value 0. 15 to 0. 67 27 0. 002
IGRT has a potentia lity to the may marginovercome avoid poor al failure t han IMRT does prognostic factors than IMRT potentially 28
Whyas a. HT can overcom e potent i a lity to a the pfariluoregthn void m ano t ic artgo IMs inarl s RT doefac s than IMRT? IGRT h 29
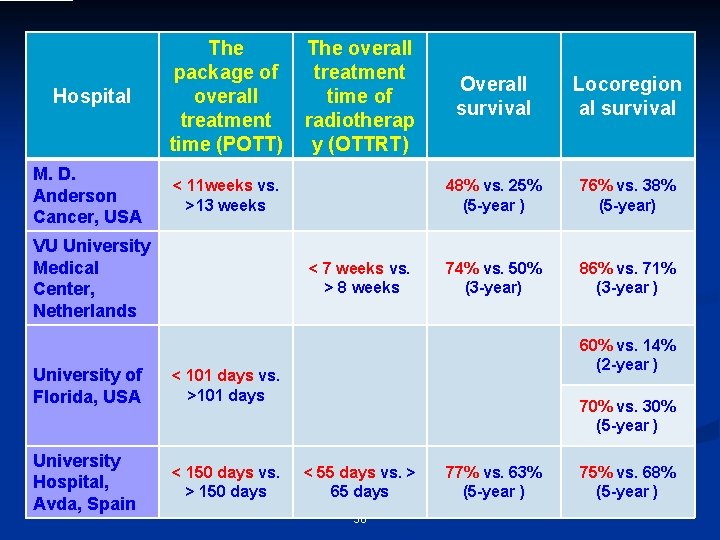
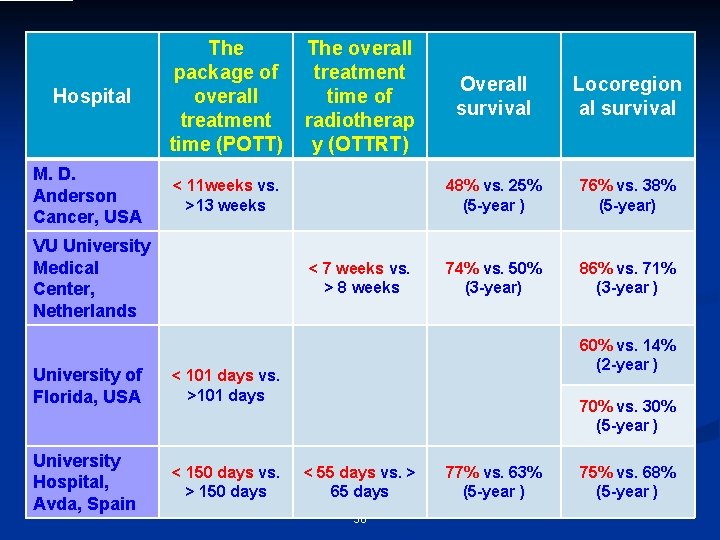
Hospital M. D. Anderson Cancer, USA The package of overall treatment time (POTT) The overall treatment time of radiotherap y (OTTRT) < 11 weeks vs. >13 weeks VU University Medical Center, Netherlands < 7 weeks vs. > 8 weeks University of Florida, USA < 101 days vs. >101 days University Hospital, Avda, Spain < 150 days vs. > 150 days Overall survival Locoregion al survival 48% vs. 25% (5 -year ) 76% vs. 38% (5 -year) 74% vs. 50% (3 -year) 86% vs. 71% (3 -year ) 60% vs. 14% (2 -year ) 70% vs. 30% (5 -year ) < 55 days vs. > 65 days 30 77% vs. 63% (5 -year ) 75% vs. 68% (5 -year )
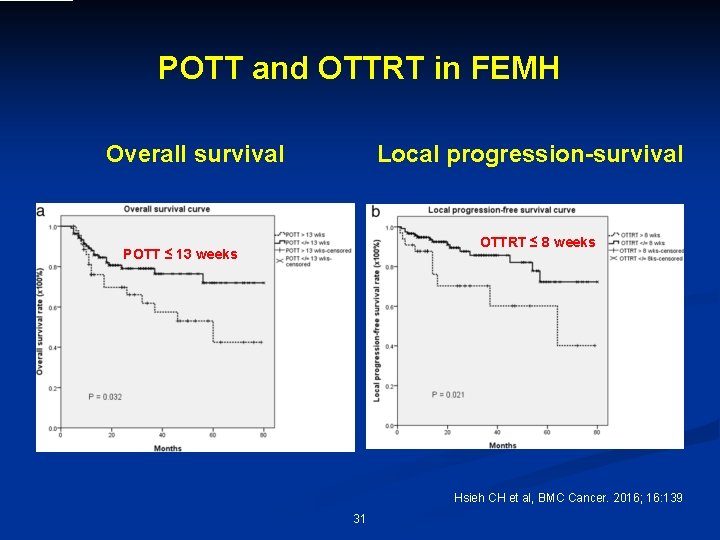
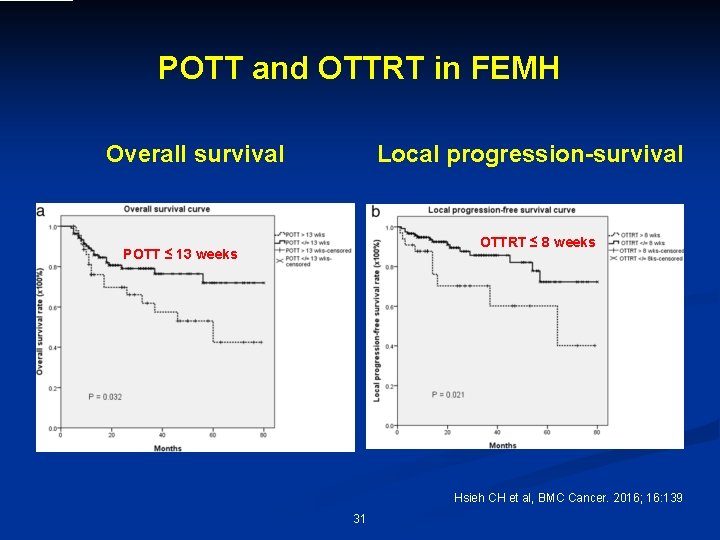
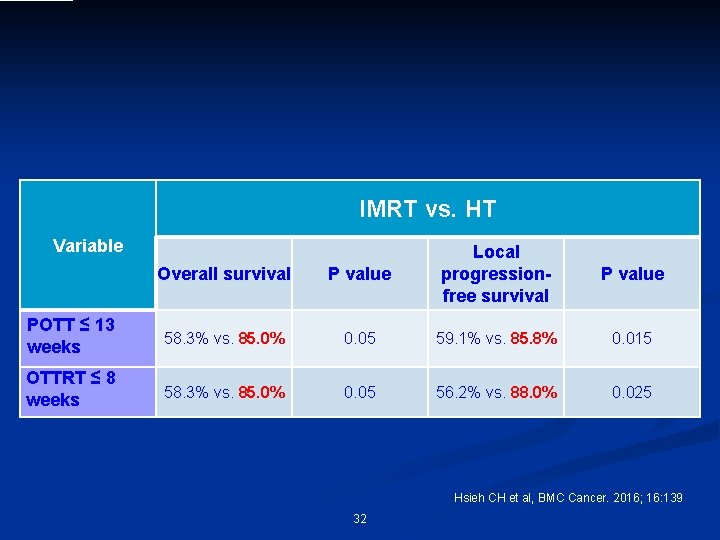
POTT and OTTRT in FEMH Overall survival Local progression-survival OTTRT ≤ 8 weeks POTT ≤ 13 weeks Hsieh CH et al, BMC Cancer. 2016; 16: 139 31
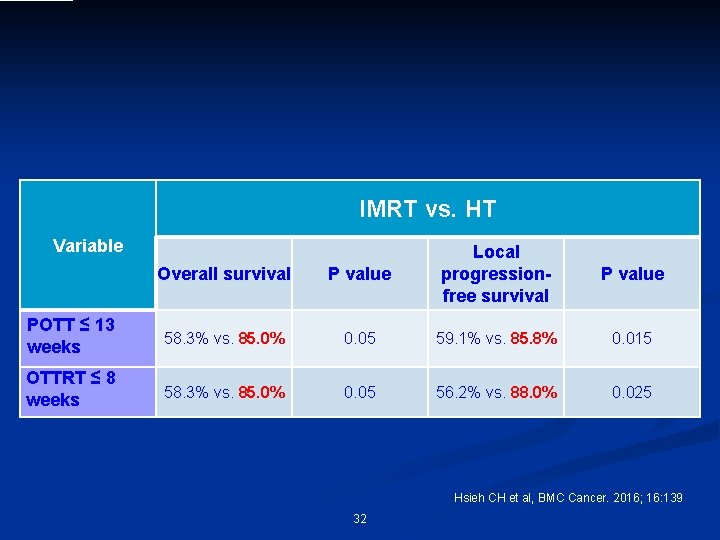
IMRT vs. HT Variable Overall survival P value Local progressionfree survival POTT ≤ 13 weeks 58. 3% vs. 85. 0% 0. 05 59. 1% vs. 85. 8% 0. 015 OTTRT ≤ 8 weeks 58. 3% vs. 85. 0% 0. 05 56. 2% vs. 88. 0% 0. 025 P value Hsieh CH et al, BMC Cancer. 2016; 16: 139 32
Why HT has be tter outcome than I MRT under the simil ar POTT or OTTRT? IGRT ha margi s a potenti nal fai a lure th lity to avoid an IM RT do es 33
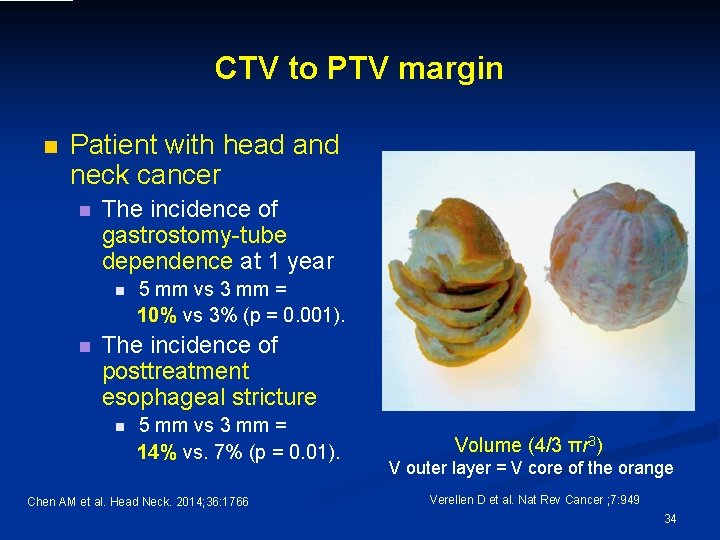
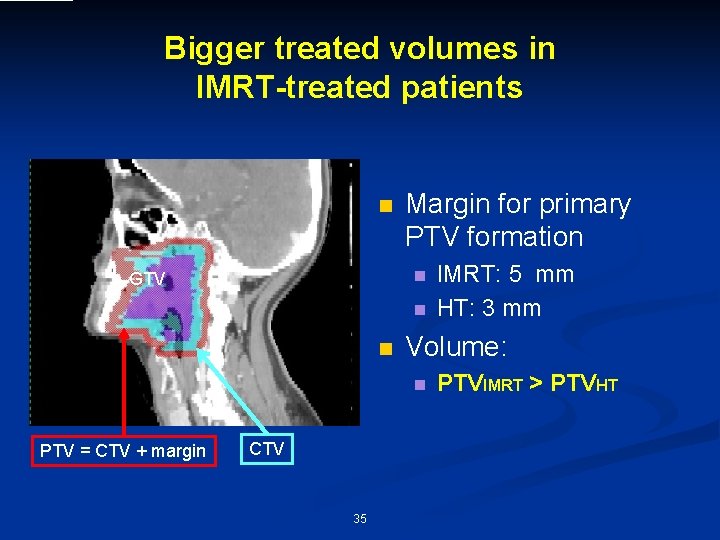
CTV to PTV margin n Patient with head and neck cancer n The incidence of gastrostomy-tube dependence at 1 year n n 5 mm vs 3 mm = 10% vs 3% (p = 0. 001). The incidence of posttreatment esophageal stricture n 5 mm vs 3 mm = 14% vs. 7% (p = 0. 01). Chen AM et al. Head Neck. 2014; 36: 1766 Volume (4/3 πr 3) V outer layer = V core of the orange Verellen D et al. Nat Rev Cancer ; 7: 949 34
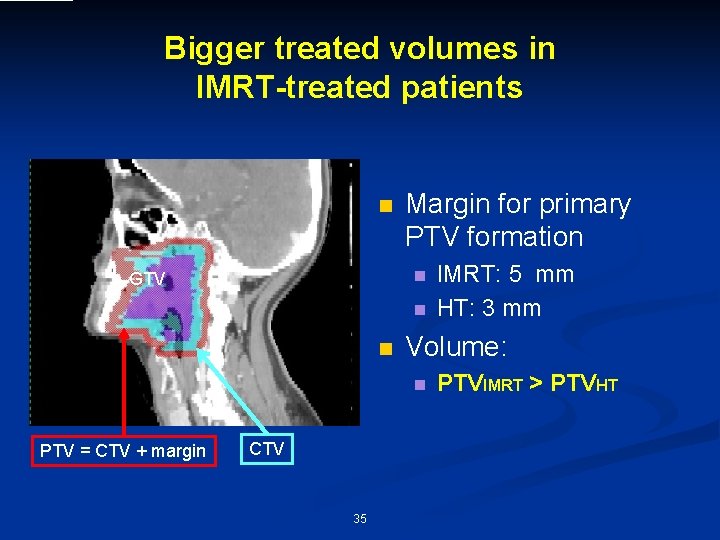
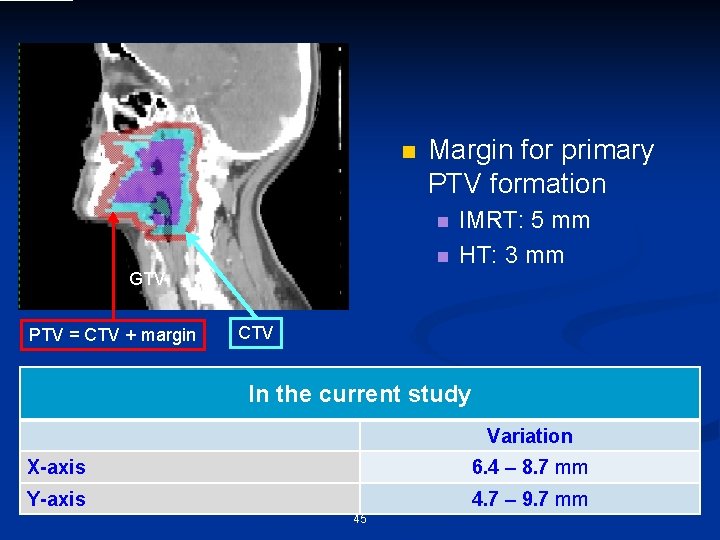
Bigger treated volumes in IMRT-treated patients n Margin for primary PTV formation n GTV n n Volume: n PTV = CTV + margin CTV 35 IMRT: 5 mm HT: 3 mm PTVIMRT > PTVHT
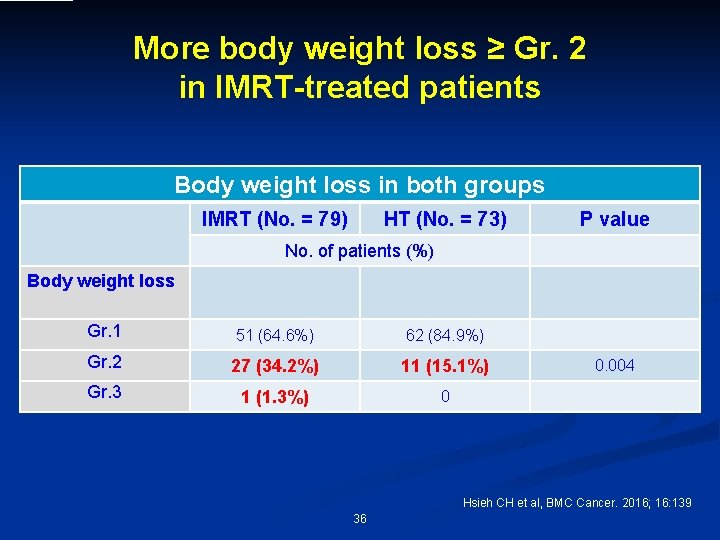
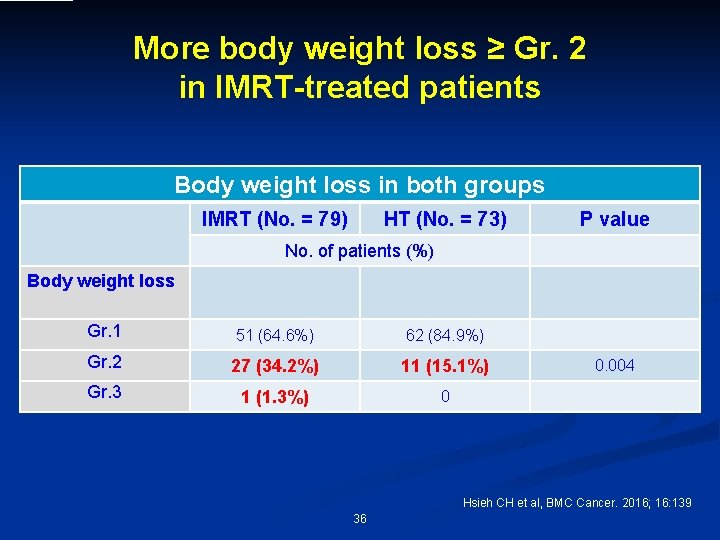
More body weight loss ≥ Gr. 2 in IMRT-treated patients Body weight loss in both groups IMRT (No. = 79) HT (No. = 73) P value No. of patients (%) Body weight loss Gr. 1 51 (64. 6%) 62 (84. 9%) Gr. 2 27 (34. 2%) 11 (15. 1%) Gr. 3 1 (1. 3%) 0 0. 004 Hsieh CH et al, BMC Cancer. 2016; 16: 139 36
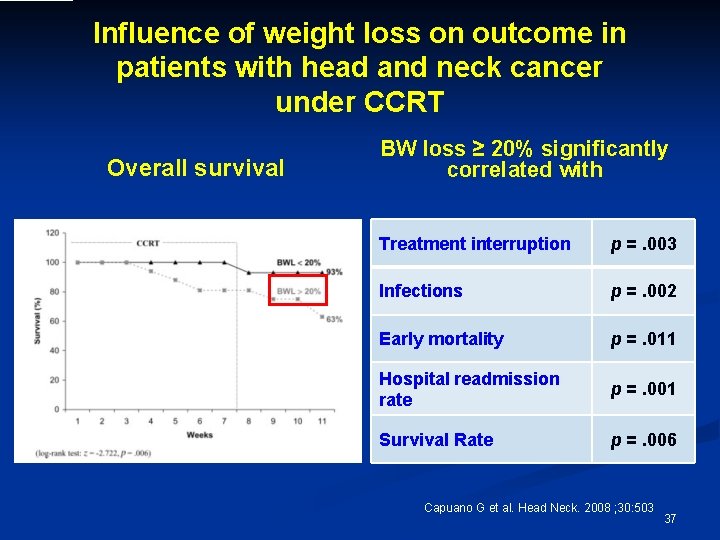
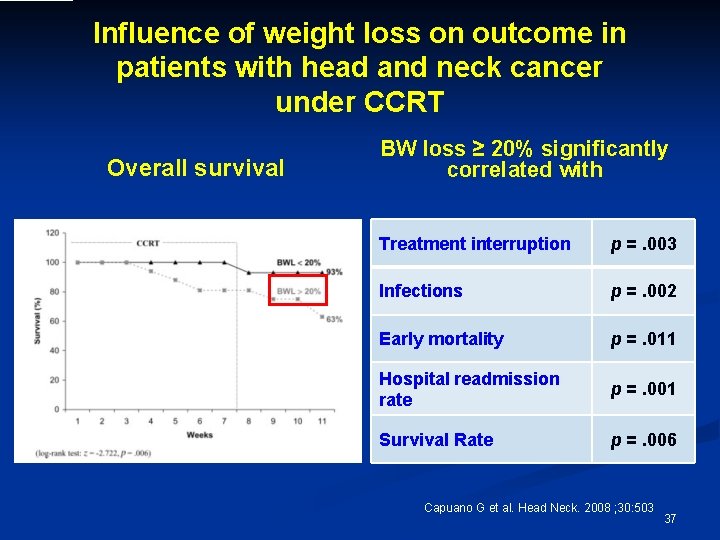
Influence of weight loss on outcome in patients with head and neck cancer under CCRT Overall survival BW loss ≥ 20% significantly correlated with Treatment interruption p =. 003 Infections p =. 002 Early mortality p =. 011 Hospital readmission rate p =. 001 Survival Rate p =. 006 Capuano G et al. Head Neck. 2008 ; 30: 503 37
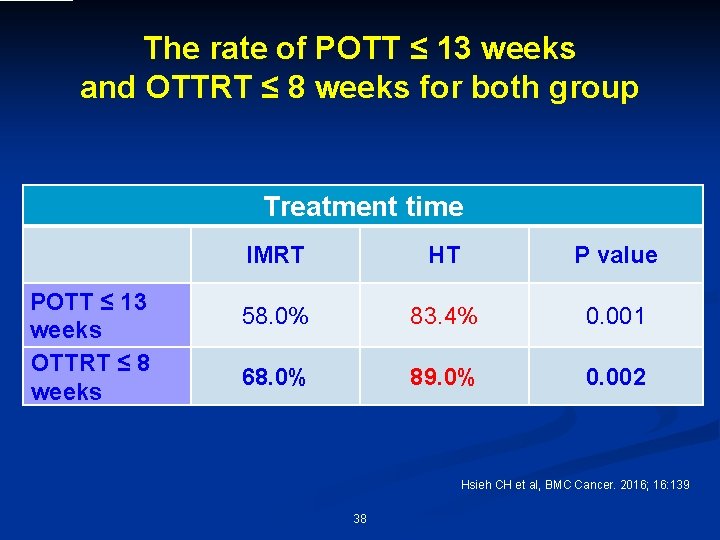
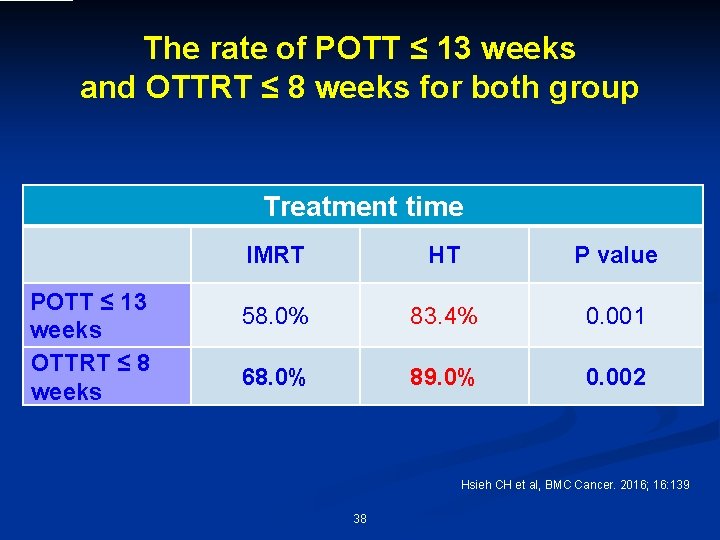
The rate of POTT ≤ 13 weeks and OTTRT ≤ 8 weeks for both group Treatment time POTT ≤ 13 weeks OTTRT ≤ 8 weeks IMRT HT P value 58. 0% 83. 4% 0. 001 68. 0% 89. 0% 0. 002 Hsieh CH et al, BMC Cancer. 2016; 16: 139 38
IGRT decreases the potential risk of IGRT ha s a pote loss body weight ntiality to avoid margina an IMRT l does failure th increases the chance to complete POTT ≤ 13 weeks and OTTRT ≤ 8 weeks 39
IGRT h Can image-guided a margin s a potentia lity to a al failu void any r e techniquethanprovide IMRT does benefits? 40
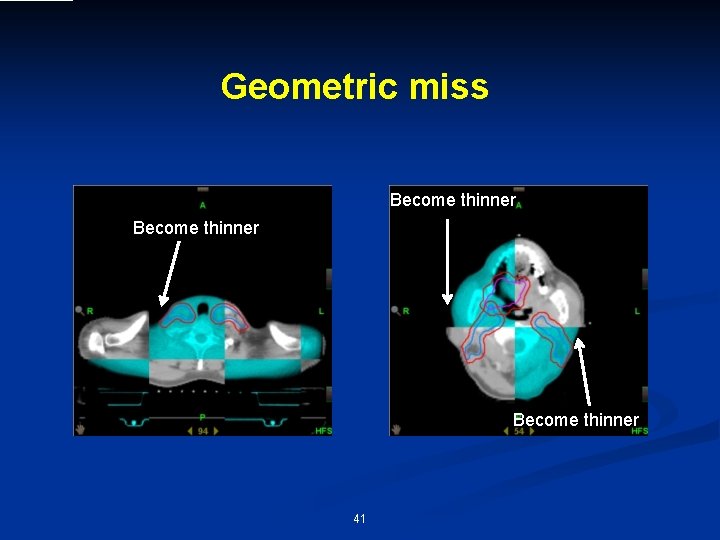
Geometric miss Become thinner 41
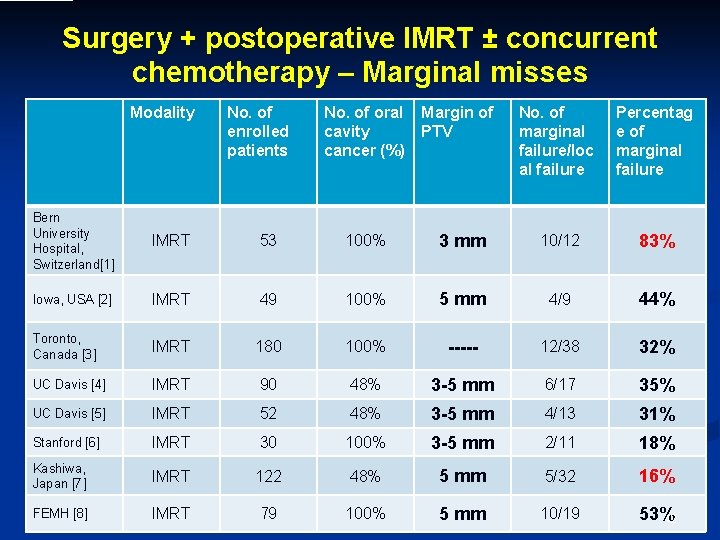
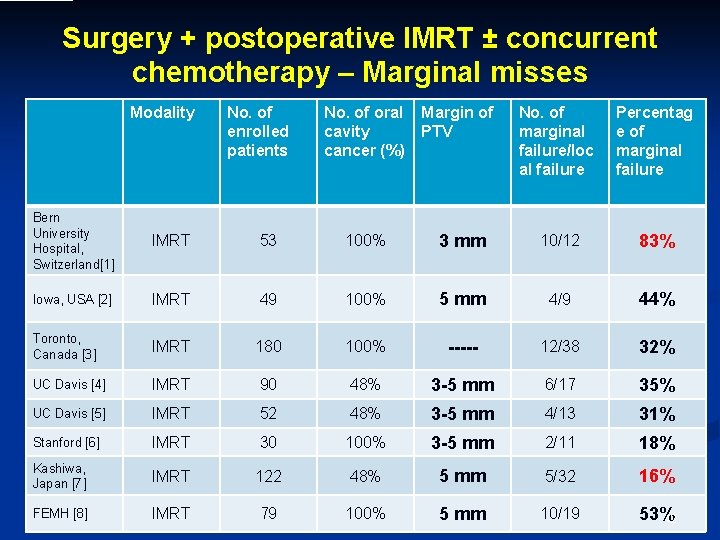
Surgery + postoperative IMRT ± concurrent chemotherapy – Marginal misses Modality No. of enrolled patients No. of oral cavity cancer (%) Margin of PTV No. of marginal failure/loc al failure Percentag e of marginal failure Bern University Hospital, Switzerland[1] IMRT 53 100% 3 mm 10/12 83% Iowa, USA [2] IMRT 49 100% 5 mm 4/9 44% Toronto, Canada [3] IMRT 180 100% ----- 12/38 32% UC Davis [4] IMRT 90 48% 3 -5 mm 6/17 35% UC Davis [5] IMRT 52 48% 3 -5 mm 4/13 31% Stanford [6] IMRT 30 100% 3 -5 mm 2/11 18% Kashiwa, Japan [7] IMRT 122 48% 5 mm 5/32 16% FEMH [8] IMRT 79 100% 5 mm 10/19 53% 42
![n Zeidan et al 1 n Even under every other day using IGRT n n Zeidan et al [1] n Even under every other day using IGRT n](https://slidetodoc.com/presentation_image_h2/31fb7c1c1d019ca8b8c433bb3ef24338/image-43.jpg)
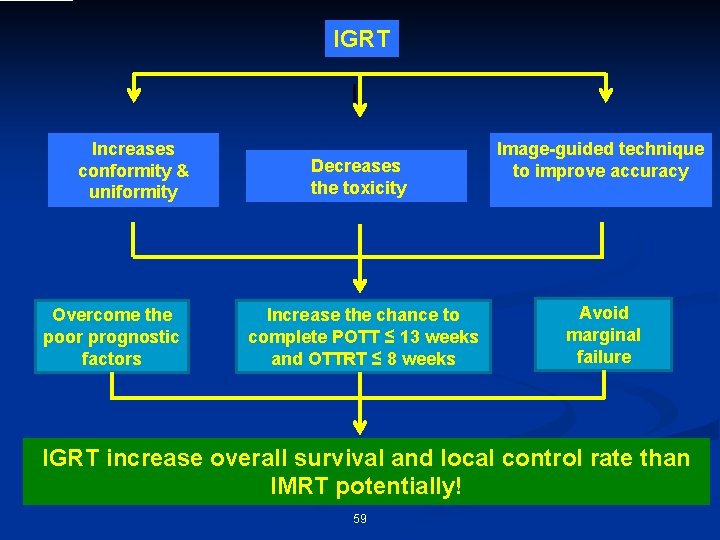
n Zeidan et al [1] n Even under every other day using IGRT n Residual errors >3 mm occurred 29% of treated head and neck cancer patients. n 5 -mm margins are mandated in the setting of less-than-daily IGRT. 1. Zeidan et al Int J Radiat Oncol Biol Phys 2007; 67: 670 43
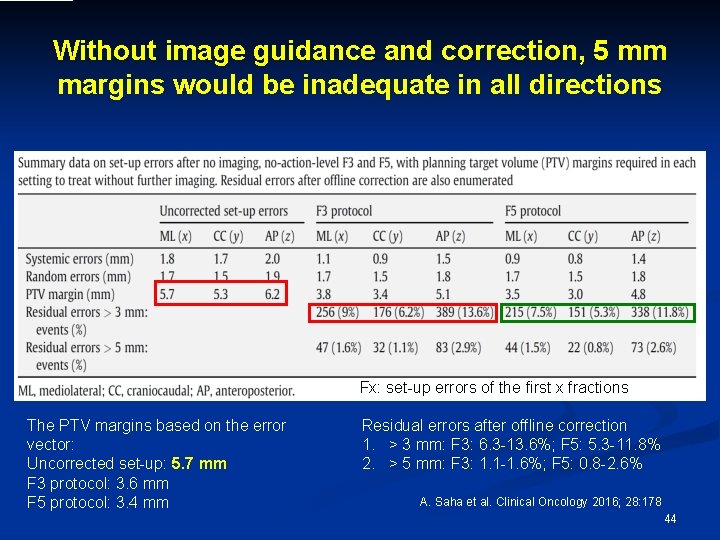
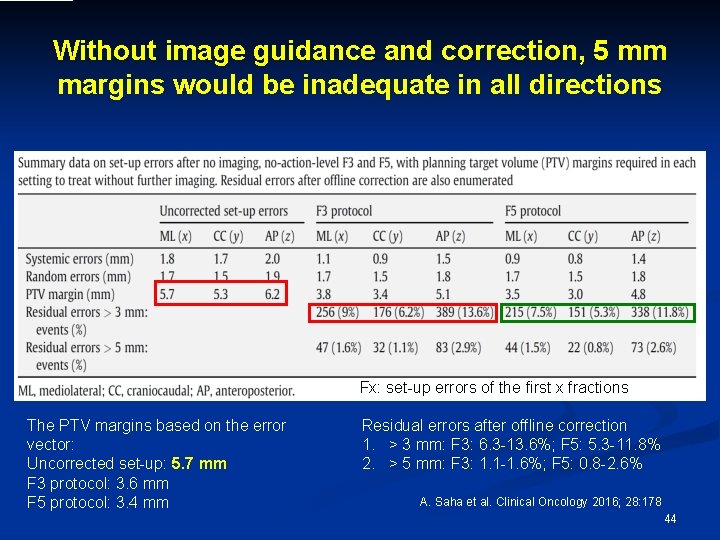
Without image guidance and correction, 5 mm margins would be inadequate in all directions Fx: set-up errors of the first x fractions The PTV margins based on the error vector: Uncorrected set-up: 5. 7 mm F 3 protocol: 3. 6 mm F 5 protocol: 3. 4 mm Residual errors after offline correction 1. > 3 mm: F 3: 6. 3 -13. 6%; F 5: 5. 3 -11. 8% 2. > 5 mm: F 3: 1. 1 -1. 6%; F 5: 0. 8 -2. 6% A. Saha et al. Clinical Oncology 2016; 28: 178 44
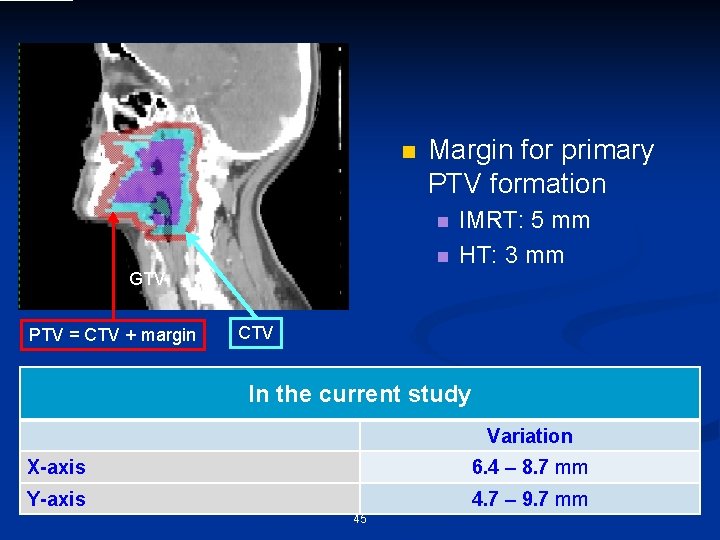
n Margin for primary PTV formation n n IMRT: 5 mm HT: 3 mm GTV PTV = CTV + margin CTV In the current study Variation X-axis 6. 4 – 8. 7 mm Y-axis 4. 7 – 9. 7 mm 45
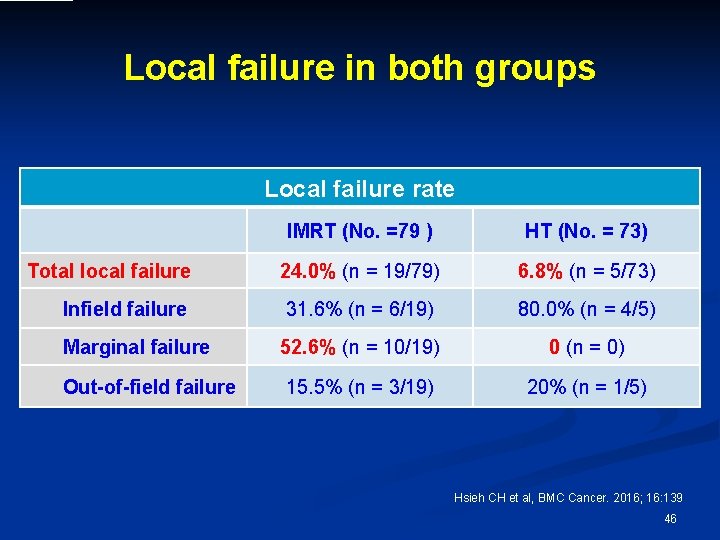
Local failure in both groups Local failure rate IMRT (No. =79 ) HT (No. = 73) Total local failure 24. 0% (n = 19/79) 6. 8% (n = 5/73) Infield failure 31. 6% (n = 6/19) 80. 0% (n = 4/5) Marginal failure 52. 6% (n = 10/19) 0 (n = 0) Out-of-field failure 15. 5% (n = 3/19) 20% (n = 1/5) Hsieh CH et al, BMC Cancer. 2016; 16: 139 46
![Surgery postoperative IMRT concurrent chemotherapy Marginal misses Modality UC Davis 9 Surgery + postoperative IMRT ± concurrent chemotherapy – Marginal misses Modality UC Davis [9]](https://slidetodoc.com/presentation_image_h2/31fb7c1c1d019ca8b8c433bb3ef24338/image-47.jpg)
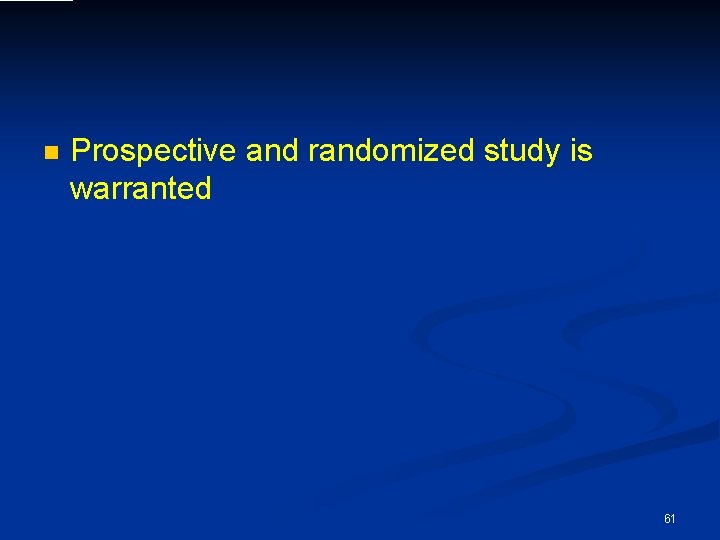
Surgery + postoperative IMRT ± concurrent chemotherapy – Marginal misses Modality UC Davis [9] FEMH[8] 1. 2. 3 4. No. of enrolled patients No. of oral cavity cancer (%) Margin of No. of PTV marginal failure/lo cal failure Percenta ge of marginal failure 103 31% 5 mm 5/76 7% 264 21% 3 mm 4/76 5% 73 100% 3 mm 0 0% IG-IMRT (HT) Geretschläger A et al. Radiat Oncol. 2012; 7: 175 Yao M et al. Int J Radiat Oncol Biol Phys. 2007; 67: 1332 Chan AK et al. Oral Oncol. 2013; 49: 255 Chen AM et al. Int J Radiat Oncol Biol Phys. 2011; 80: 1423 5. Chen AM et al. Head Neck. 2010; 32: 1452 6. Daly ME et al. Int J Radiat Oncol Biol Phys. 2011; 80: 1412 7. Ooishi M et al. Jpn J Clin Oncol. 2016; 46: 919 8. Hsieh CH et al, BMC Cancer. 2016; 16: 139 9. Chen AM et al. Head Neck. 2014; 36: 1766 47
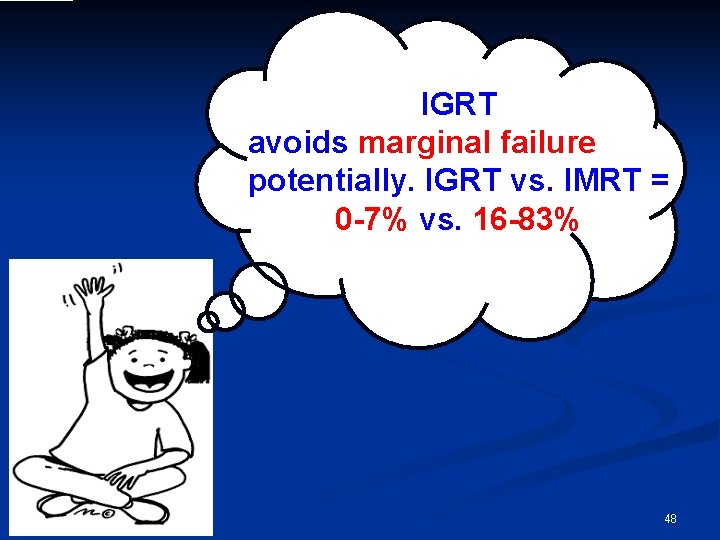
IGRT avoids marginal failure potentially. IGRT vs. IMRT = 0 -7% vs. 16 -83% IGR T mar has a p gina l fail otential ure than ity to av oi IMR T do d es 48
HIo. GRw. T haasbaout th potentialit e marginal f toxicitiaeilusre tohafn t. IMry. Rto. T advooid eatem s ent? 49
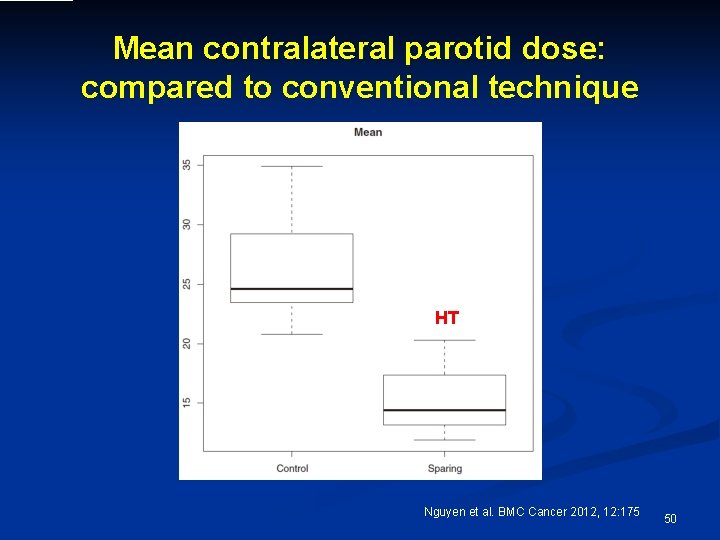
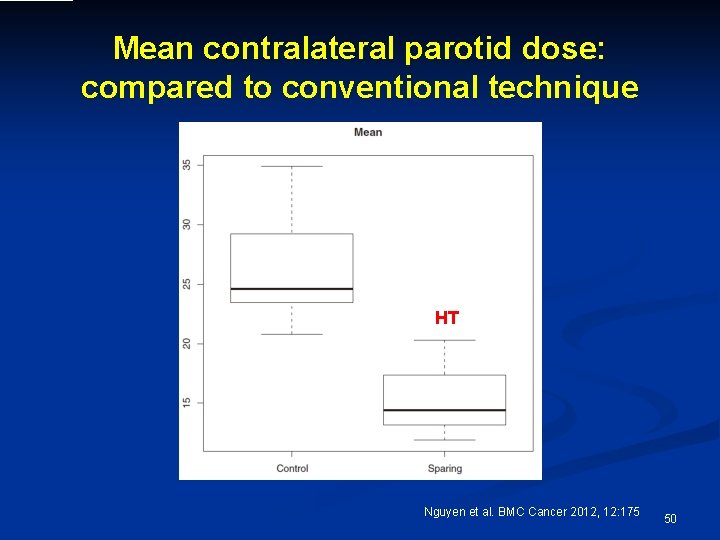
Mean contralateral parotid dose: compared to conventional technique HT Nguyen et al. BMC Cancer 2012, 12: 175 50
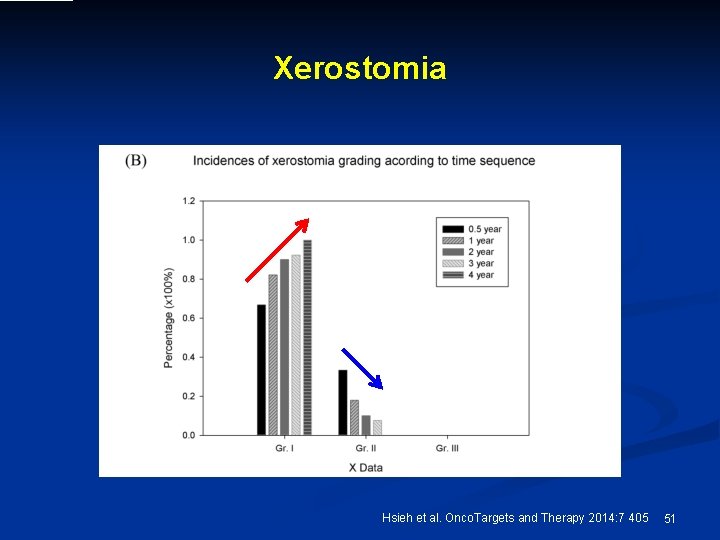
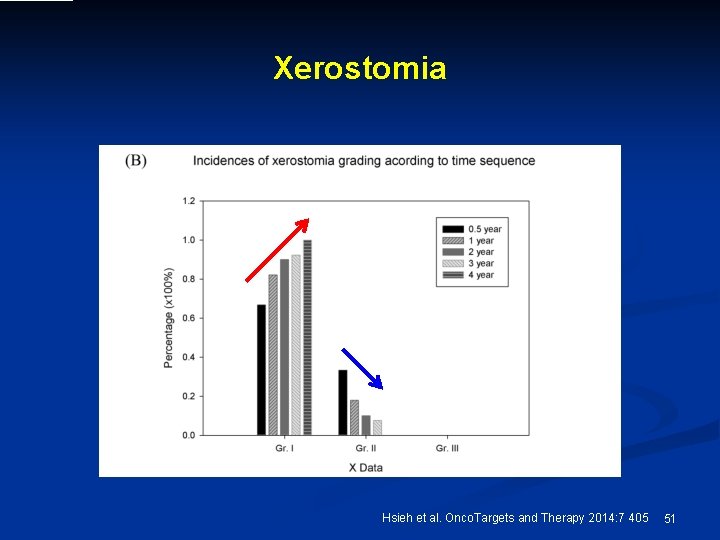
Xerostomia Hsieh et al. Onco. Targets and Therapy 2014: 7 405 51
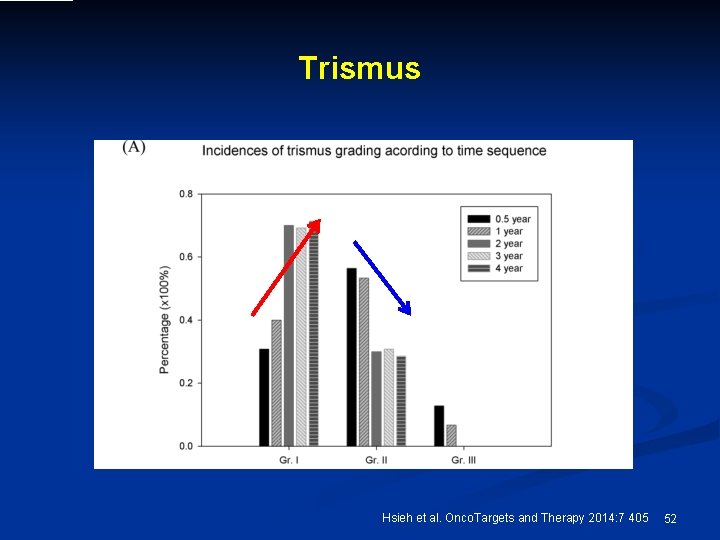
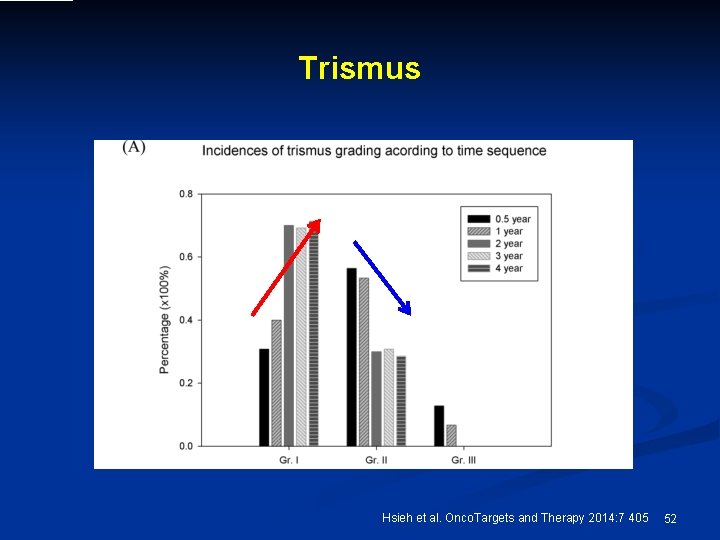
Trismus Hsieh et al. Onco. Targets and Therapy 2014: 7 405 52
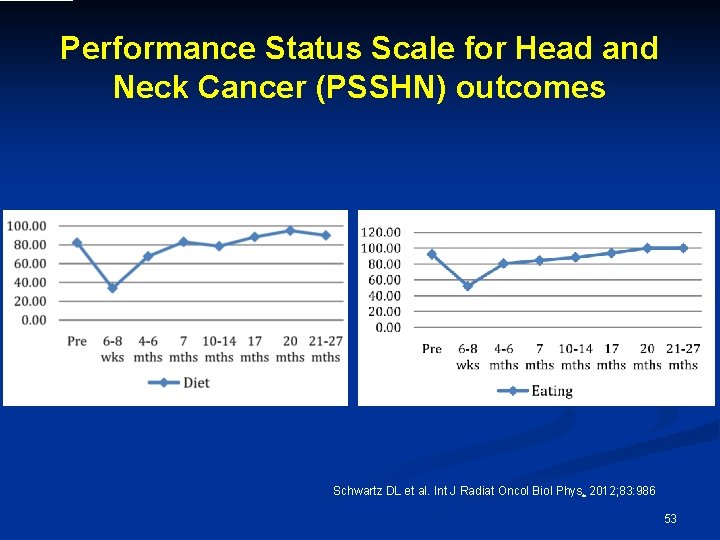
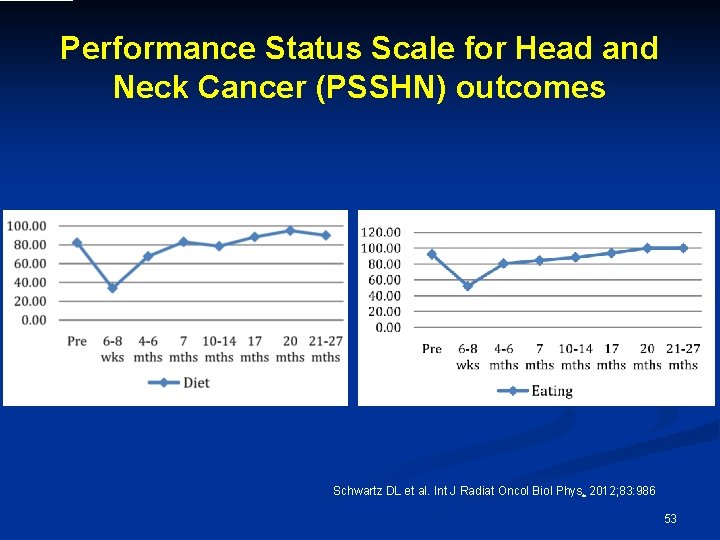
Performance Status Scale for Head and Neck Cancer (PSSHN) outcomes Schwartz DL et al. Int J Radiat Oncol Biol Phys. 2012; 83: 986 53
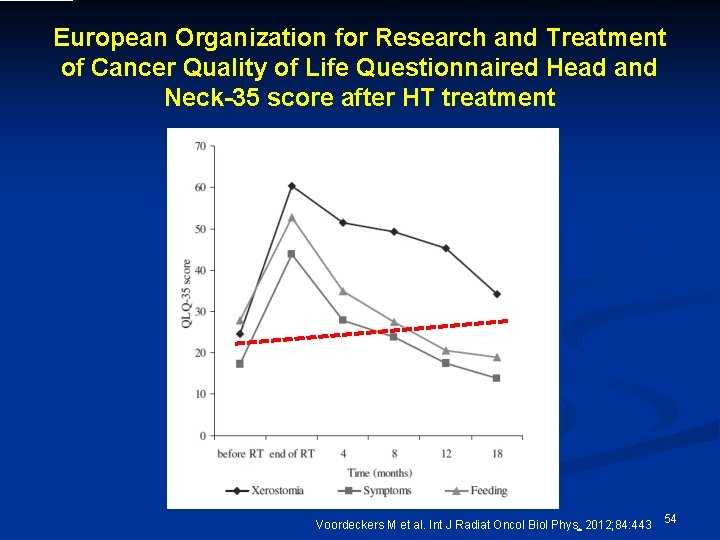
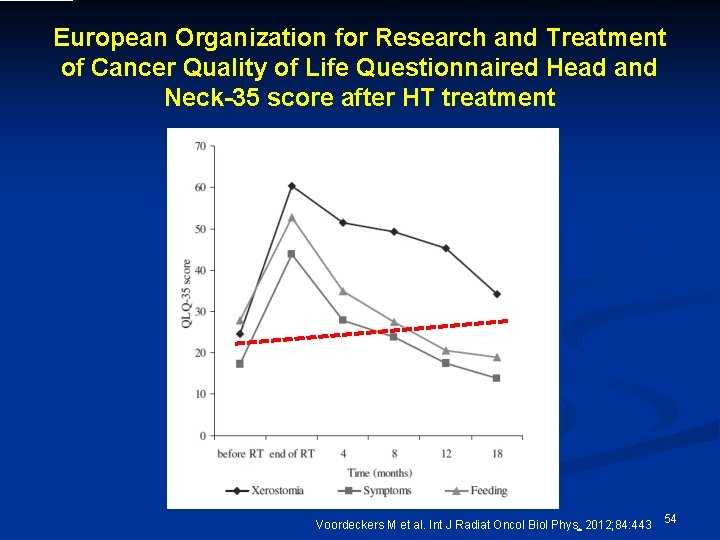
European Organization for Research and Treatment of Cancer Quality of Life Questionnaired Head and Neck-35 score after HT treatment Voordeckers M et al. Int J Radiat Oncol Biol Phys. 2012; 84: 443 54
IGRT potentiality to avoid ma failure ththe inverses rginof al life an IMRquality T does by time sequence IGRT has a 55
Limitations of the study 56
n n n This is a retrospective study. The choice of treatment modality was according to patients’ will. The quality of both IMRT and HT planning, Improved over time. 57
Conclusion 58
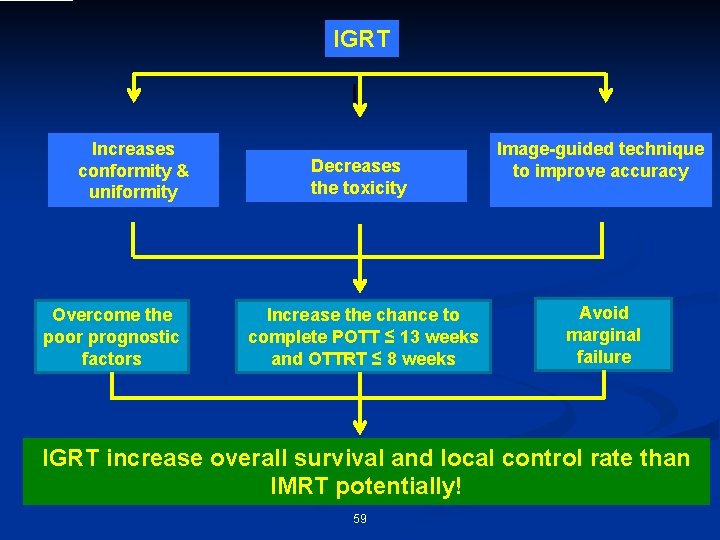
IGRT Increases conformity & uniformity Overcome the poor prognostic factors Decreases the toxicity Increase the chance to complete POTT ≤ 13 weeks and OTTRT ≤ 8 weeks Image-guided technique to improve accuracy Avoid marginal failure IGRT increase overall survival and local control rate than IMRT potentially! 59

e r u t u f e h In t 60
n Prospective and randomized study is warranted 61

Acknowledgment n Department of Dentistry and Oral Surgery, FEMH n n n n Ying-Shiung Kuo Chien-Fu Tseng Kwang-Yu Hu Bing-Yi Lin Department of Otolaryngology, FEMH n n Li-Jen Liao Wu-Chia Lo Division of Radiation Oncology, Department of Radiology, FEMH n n n Pei-Wei Shueng Le-Jung Wu Hui-Ju Tien Mei-Hui Lu Department of Medical Research, CMUH n Yu-Chuen Huang Division of Medical Oncology and Hematology, Department of Internal Medicine, FEMH n Yu-Chin Lin 62

Thank you for your attention ! 63