ILLINOIS DEPARTMENT OF HUMAN SERVICES DIVISION OF ALCOHOLISM






- Slides: 60
ILLINOIS DEPARTMENT OF HUMAN SERVICES DIVISION OF ALCOHOLISM AND SUBSTANCE ABUSE Drug Overdose Prevention Program Training Module Dr. Seth Eisenberg, MD Rosie Gianforte, LCSW
TOPICS § Overview of the Heroin/Opiate Problem § Illinois Public Act 099 -0480 (HB 0001) § IDHS/DASA Drug Overdose Prevention Program (DOPP) and how to enroll § Identifying Opioid Overdoses § How to Respond to an Overdose § Use of Naloxone § After Naloxone – Outreach Efforts/Treatment Referrals
OBJECTI VES § Explain the risk factors for opioid abuse and overdose and discuss strategies for preventing overdose § Gain an understanding of the opiate overdose problem & how opioids work § Identify people who meet the criteria for the provision of naloxone, and explain how to respond to opioid overdose § Compare the different types of Naloxone: § Intra-nasal § Intra-muscular
OBJECTIVES (CONT. ) § Explain how a person will respond to naloxone rescue therapy § § and discuss managing adverse events following the use of naloxone rescue therapy Discuss indications, contraindications, safety, any drug interactions, and adverse effects of naloxone rescue therapy Explore Medication Assisted Treatment MAT Options (PA 99 -0553) Effective January 1, 2017, all substance use treatment programs licensed by IDHS/DASA must provide educational information to clients identified as having or seeking treatment for opioid use disorder, including the use of a medication for the use of opioid use disorder, recognition of and response to opioid overdose, and the use and administration of naloxone Recommend support programs and resources for clients and care -givers for follow-up care for opioid use disorder.
Why focus on the heroin/opioid epidemic?
OPIOIDS § Opioids are a class of drugs in both legal (prescription medications such as oxycodone, hydrocodone, morphine, fentanyl) and illegal(heroin) forms. § Opioids are natural or synthetic substances that act on the brains opiate receptors. § Opioids dull pain and relieve anxiety. § People may misuse opioids because they are in pain (physical and emotional) and opioids produce a feeling of euphoria.
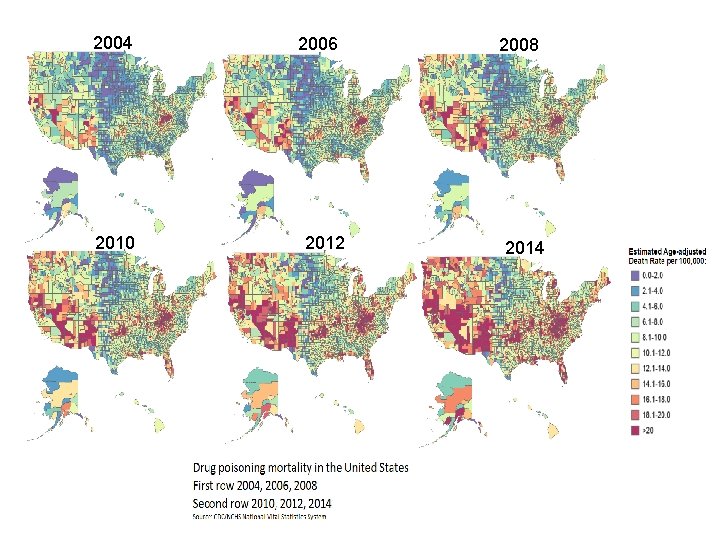
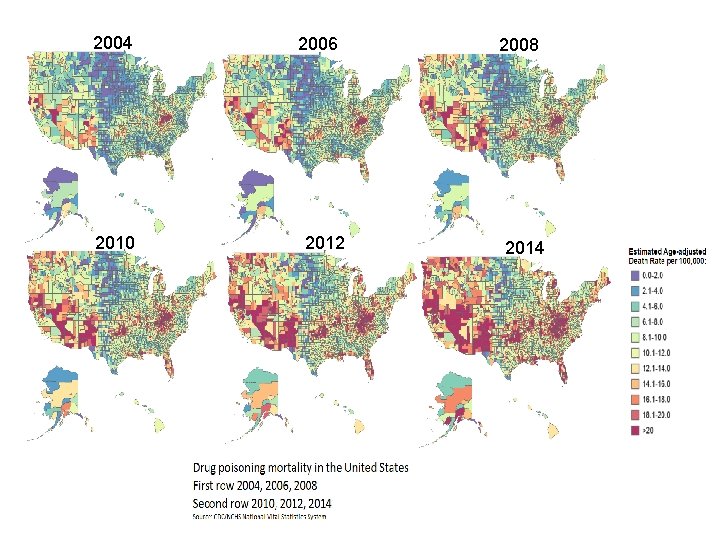
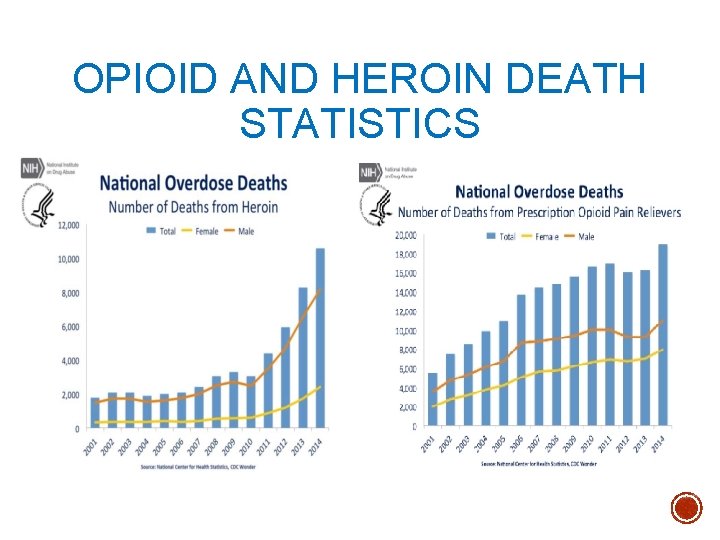
2004 2010 2006 2012 2008 2014
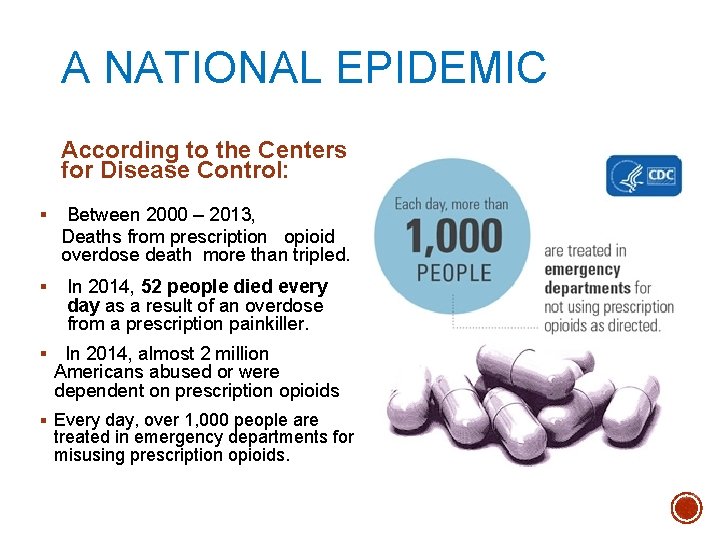
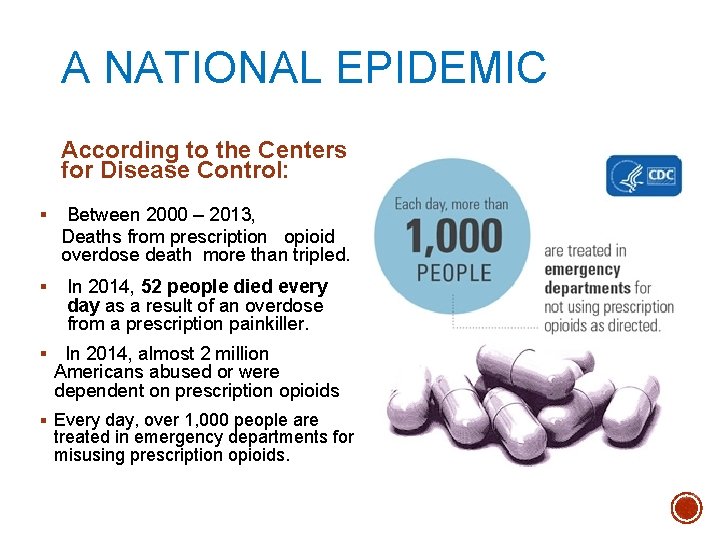
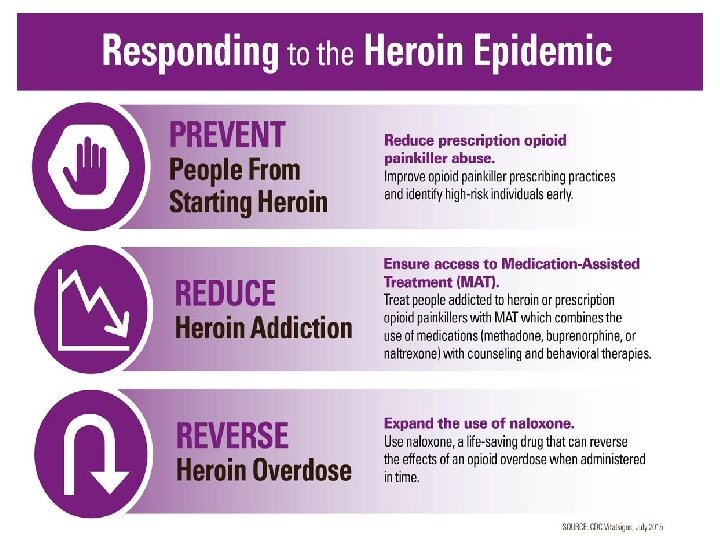
A NATIONAL EPIDEMIC According to the Centers for Disease Control: § Between 2000 – 2013, Deaths from prescription opioid overdose death more than tripled. § In 2014, 52 people died every day as a result of an overdose from a prescription painkiller. § In 2014, almost 2 million Americans abused or were dependent on prescription opioids § Every day, over 1, 000 people are treated in emergency departments for misusing prescription opioids.
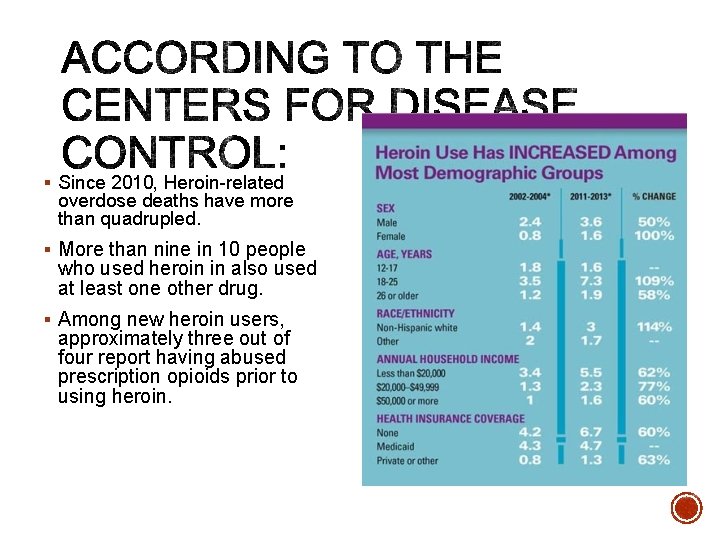
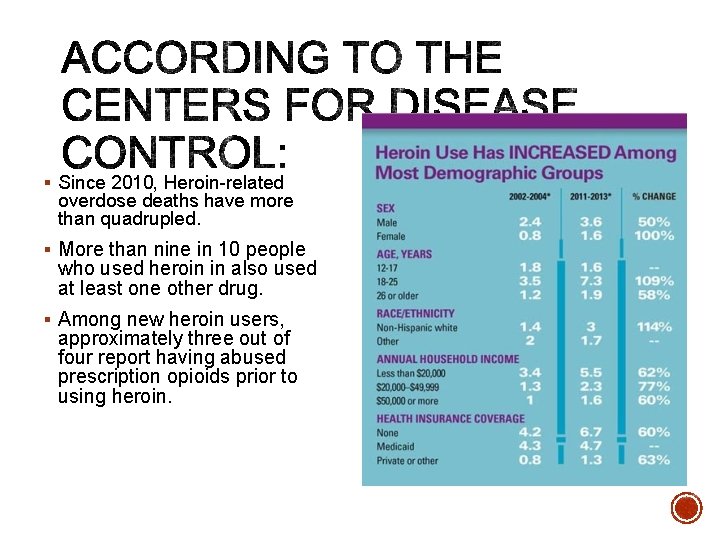
§ Since 2010, Heroin-related overdose deaths have more than quadrupled. § More than nine in 10 people who used heroin in also used at least one other drug. § Among new heroin users, approximately three out of four report having abused prescription opioids prior to using heroin.

FENTANYL § Fentanyl is a synthetic opioid pain reliever that is much more powerful than any other opioids. § It is prescribed for severe pain, such as advanced cancer pain. It has been illegally made and distributed through illegal drug markets, and is often mixed with heroin and other drugs, sometimes without the buyer’s knowledge. § Fentanyl overdoses are more lethal than heroin or prescription opioids alone. § Overdose deaths involving synthetic opioids, which includes fentanyl, increased by 80% from 2013 to 2014.
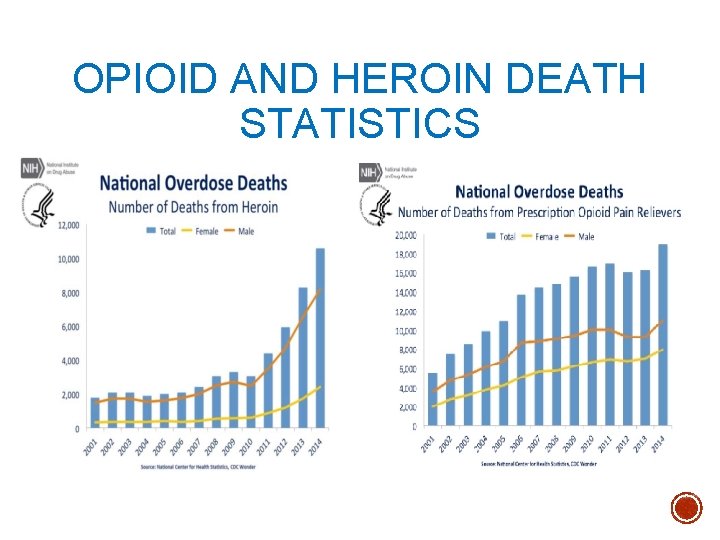
OPIOID AND HEROIN DEATH STATISTICS
IN ILLINOIS – THE OPIATE CRISIS 2013 - 2015 § Illinois was one of 14 states with statistically significant increases in overall drug overdose deaths between 2013 and 2014. § Opioid drug overdoses killed 45% more people than homicides § The Chicago Metropolitan area ranks first nationwide in emergency departmentions for heroin use. § Cook County ranks first in the nation for percentage of arrestees testing positive for opiates. Source: Illinois Department of Public Health
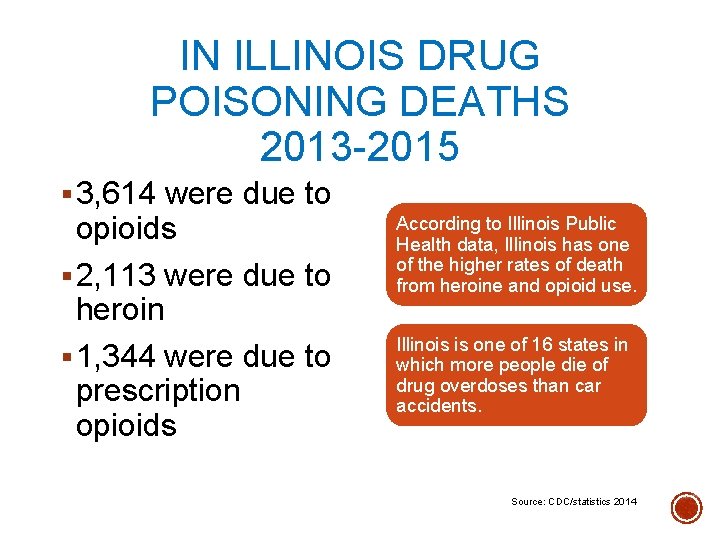
IN ILLINOIS DRUG POISONING DEATHS 2013 -2015 § 3, 614 were due to opioids § 2, 113 were due to heroin § 1, 344 were due to prescription opioids According to Illinois Public Health data, Illinois has one of the higher rates of death from heroine and opioid use. Illinois is one of 16 states in which more people die of drug overdoses than car accidents. Source: CDC/statistics 2014
WHO IS AT RISK OF AN OVERDOSE? Anyone who may use opioids for chronic cancer pain or non-cancer § pain, as well as people who use heroin, may be at risk for opioid overdose Some situations that may increase a person’s risk include: § § § § Switching between opioids Mixing opioids with depressants, such as alcohol or benzodiazepines; such as oxycodone and xanax and alcohol. People with chronic medical conditions (Substance Use Disorders, HIV, cardiovascular or respiratory disease, mental illnesses) or homeless conditions; Recently released from incarceration and in-patient tx programs. Recently completing a mandatory opioid detoxification or having abstained from use for a period of time; the person’s tolerance has decreased but they have a high risk of relapse Discharge from emergency medical care after opioid intoxication
HOW TO REDUCE THE RISK OVERDOSE Talk to people and caregivers about ways to avoid an accidental overdose, especially at discharge: § Do not adjust prescribed dosage, skip doses, or take any extra doses § Do not mix with other dugs and/or alcohol (i. e. antianxiety drugs like benzodiazepines, antidepressants, or cocaine) § Abstain from use of opioids unless prescribed, and attempt abstinence from heroin.

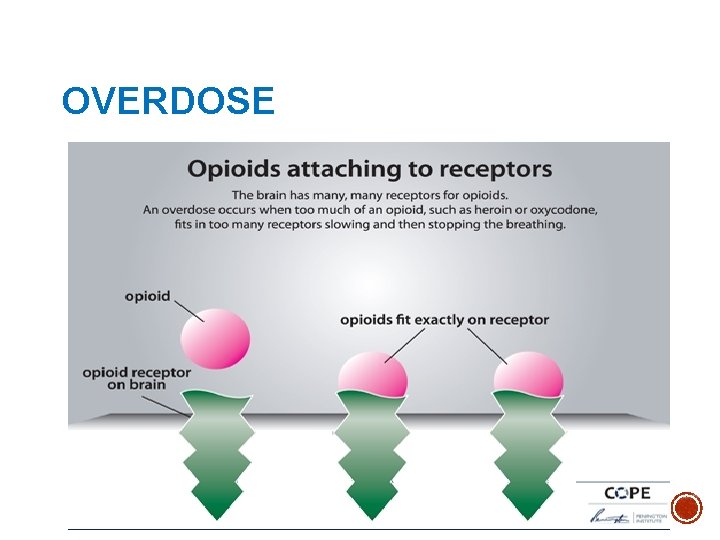
OVERDOSE § Overdose is an acute condition that usually occurs over 1 -3 hours § May be caused by: § Excess intake of opioids § Combination of opioid and a Central Nervous System depressant § Opioid use in someone with a compromised respiratory system or metabolic condition
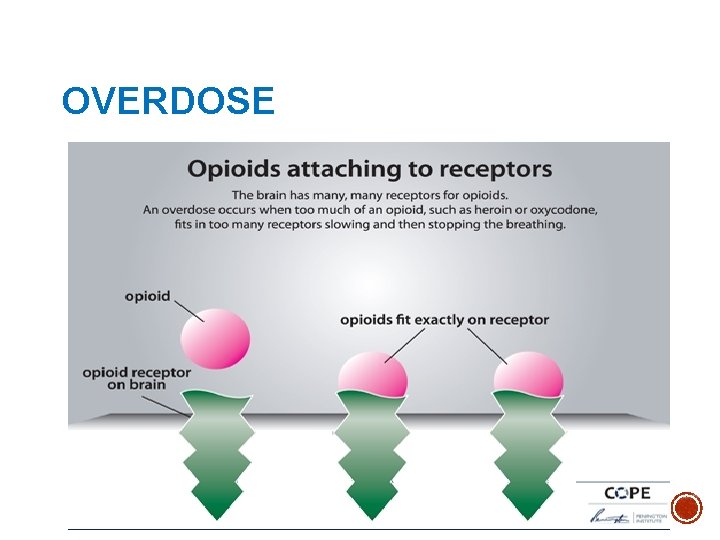
OVERDOSE
Slow Breathing Stops Lack of oxygen may cause brain damage Heart Stops Seizure, stroke, or even death Mechanisms of overdose
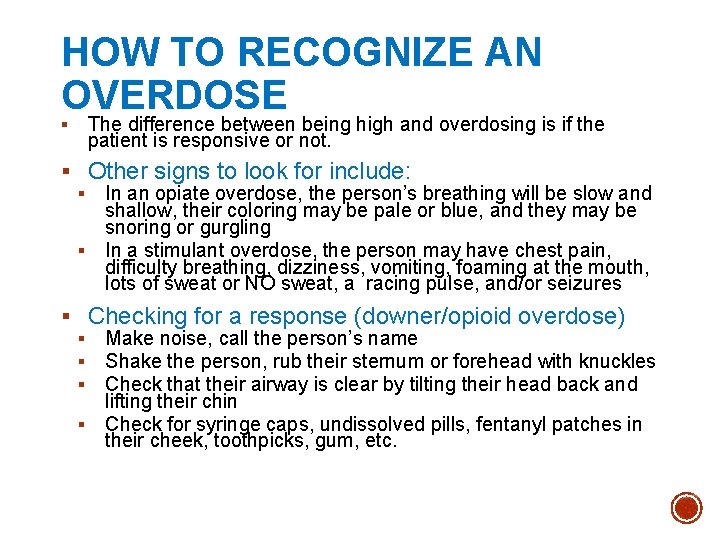
HOW TO RECOGNIZE AN OVERDOSE § The difference between being high and overdosing is if the patient is responsive or not. § Other signs to look for include: § In an opiate overdose, the person’s breathing will be slow and shallow, their coloring may be pale or blue, and they may be snoring or gurgling § In a stimulant overdose, the person may have chest pain, difficulty breathing, dizziness, vomiting, foaming at the mouth, lots of sweat or NO sweat, a racing pulse, and/or seizures § Checking for a response (downer/opioid overdose) § Make noise, call the person’s name § Shake the person, rub their sternum or forehead with knuckles § Check that their airway is clear by tilting their head back and lifting their chin § Check for syringe caps, undissolved pills, fentanyl patches in their cheek, toothpicks, gum, etc.

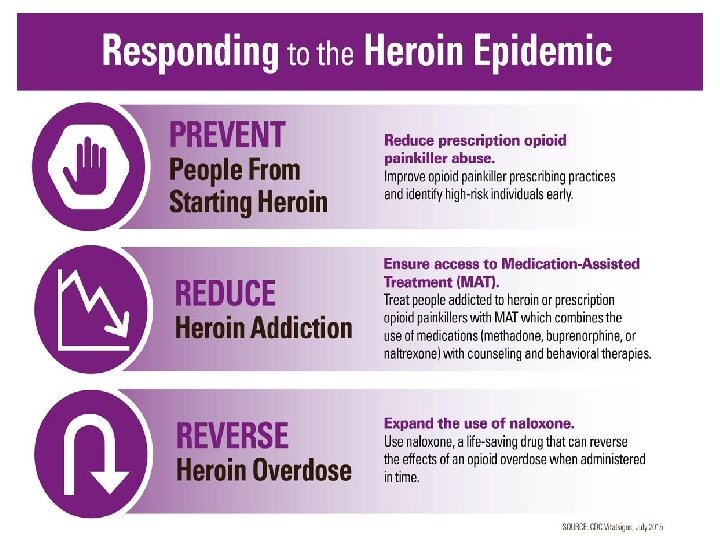
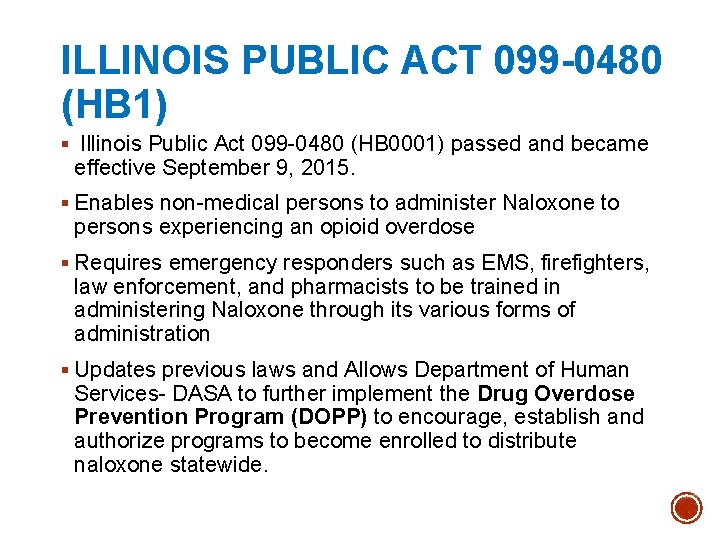
ILLINOIS PUBLIC ACT 099 -0480 (HB 1) § Illinois Public Act 099 -0480 (HB 0001) passed and became effective September 9, 2015. § Enables non-medical persons to administer Naloxone to persons experiencing an opioid overdose § Requires emergency responders such as EMS, firefighters, law enforcement, and pharmacists to be trained in administering Naloxone through its various forms of administration § Updates previous laws and Allows Department of Human Services- DASA to further implement the Drug Overdose Prevention Program (DOPP) to encourage, establish and authorize programs to become enrolled to distribute naloxone statewide.
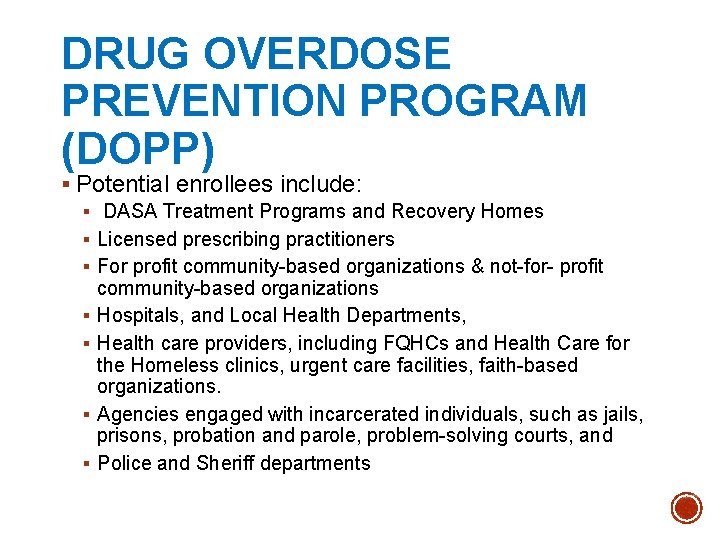
DRUG OVERDOSE PREVENTION PROGRAM (DOPP) § Potential enrollees include: § DASA Treatment Programs and Recovery Homes § Licensed prescribing practitioners § For profit community-based organizations & not-for- profit community-based organizations § Hospitals, and Local Health Departments, § Health care providers, including FQHCs and Health Care for the Homeless clinics, urgent care facilities, faith-based organizations. § Agencies engaged with incarcerated individuals, such as jails, prisons, probation and parole, problem-solving courts, and § Police and Sheriff departments
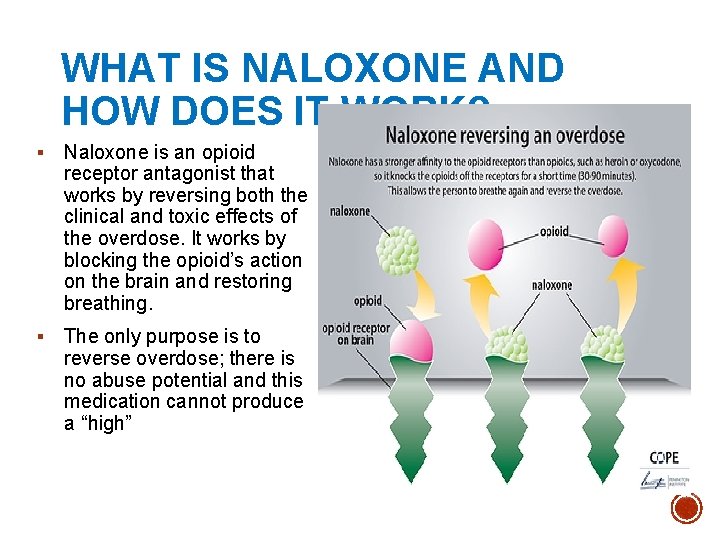
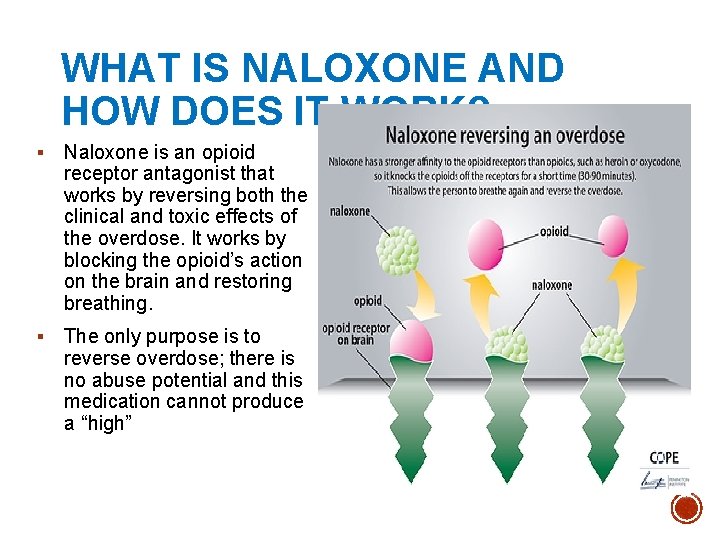
WHAT IS NALOXONE AND HOW DOES IT WORK? § Naloxone is an opioid receptor antagonist that works by reversing both the clinical and toxic effects of the overdose. It works by blocking the opioid’s action on the brain and restoring breathing. § The only purpose is to reverse overdose; there is no abuse potential and this medication cannot produce a “high”
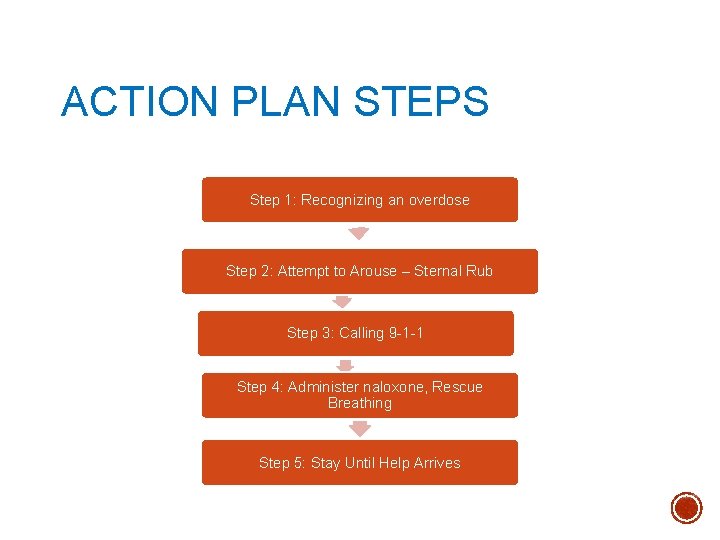
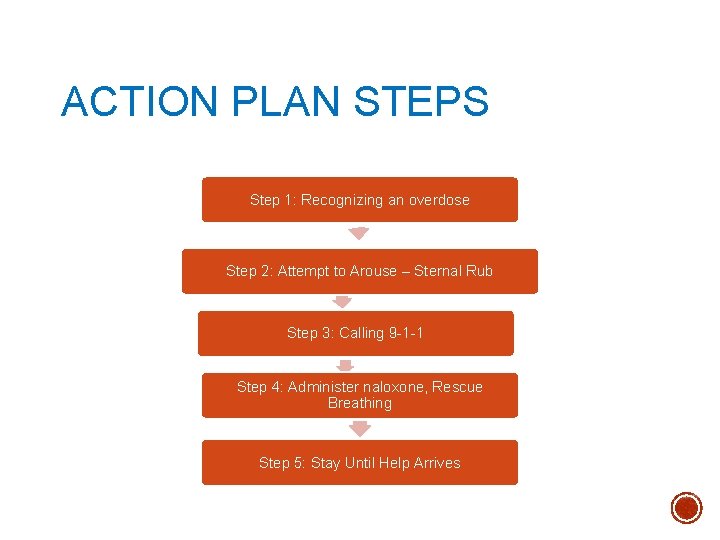
ACTION PLAN STEPS Step 1: Recognizing an overdose Step 2: Attempt to Arouse – Sternal Rub Step 3: Calling 9 -1 -1 Step 4: Administer naloxone, Rescue Breathing Step 5: Stay Until Help Arrives
ACTION PLAN 1. Stay Calm 2. Give Sternal Rub (Call out persons name and shake shoulders) 3. Call 911 for Emergency Rescue Responder Services 4. Perform Rescue Breathing and Chest Compression Techniques 5. Administer Naloxone either through muscular injection or nasal spray. 6. Continue rescue breathing for 3 -5 mins, if person is still not responding administer second dose of Naloxone 7. Goal is to restore adequate breathing, but not necessarily complete arousal 8. Stay with person until Emergency Responders arrive. If person is still unconscious but breathing on his/her own, put him or her in recovery position.
TIPS FOR CALLING 9 -1 -1 & NALOXONE § Whichever you can do the quickest – DO FIRST! § Tell the dispatcher the person has stopped breathing § The dispatcher may give instructions on rescue breathing or chest compressions § Have the address and location ready § The dispatcher may connect you with the paramedics who will ask you the same questions – this is a normal process.
RESCUE BREATHING § Please review the steps below to perfect your rescue breathing technique: 1. Be sure the person’s airway is clear (check that nothing inside the person’s mouth or throat is blocking the airway 2. Place one hand on the person’s chin, tilt the head back. 3. Pinch the nose closed. 4. Place your mouth over the person’s mouth to make a seal and give 2 slow breaths. 5. The person’s chest should rise (but not the stomach). 6. Follow up with one breath every 5 seconds until the person can breath on their own
WHY NALOXONE? § Naloxone is an opioid overdose antidote. § Naloxone counteracts the effects of prescription opioids like hydrocodone, oxycodone, morphine, methadone and fentanyl and illegal opioids like heroin. § Naloxone is safe. It is as nontoxic as water and has no potential for addiction. If a person has not taken opioids, naloxone will not hurt them. § Naloxone is cost effective. § In Illinois anyone can be trained to administer naloxone.
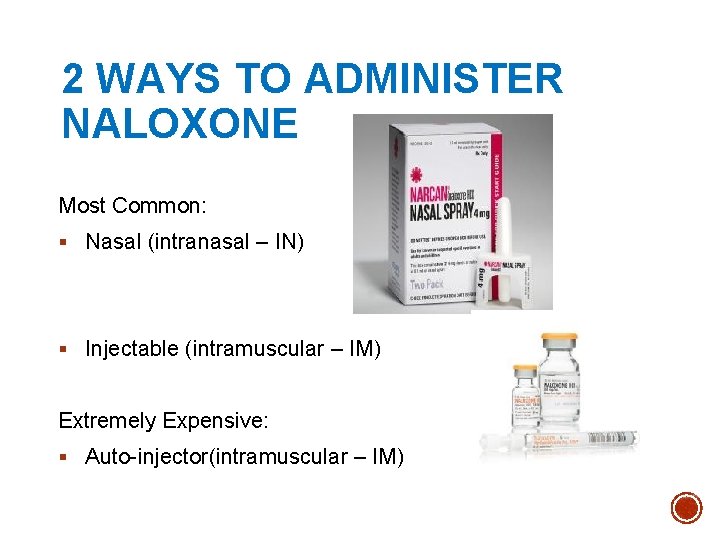
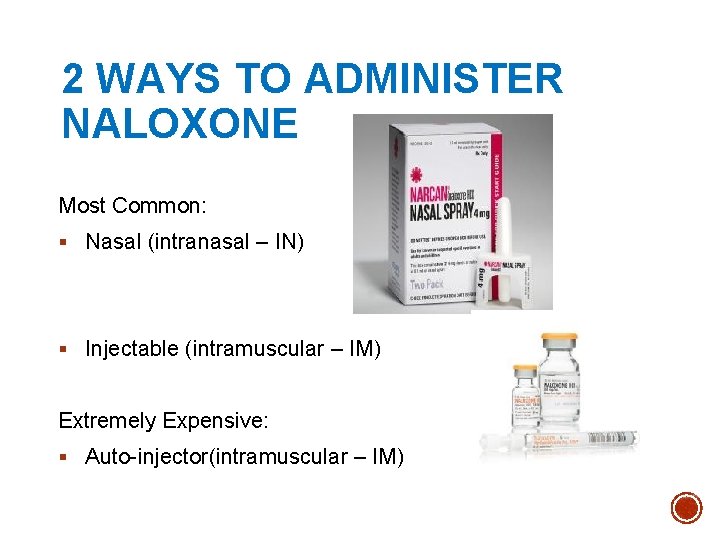
2 WAYS TO ADMINISTER NALOXONE Most Common: § Nasal (intranasal – IN) § Injectable (intramuscular – IM) Extremely Expensive: § Auto-injector(intramuscular – IM)
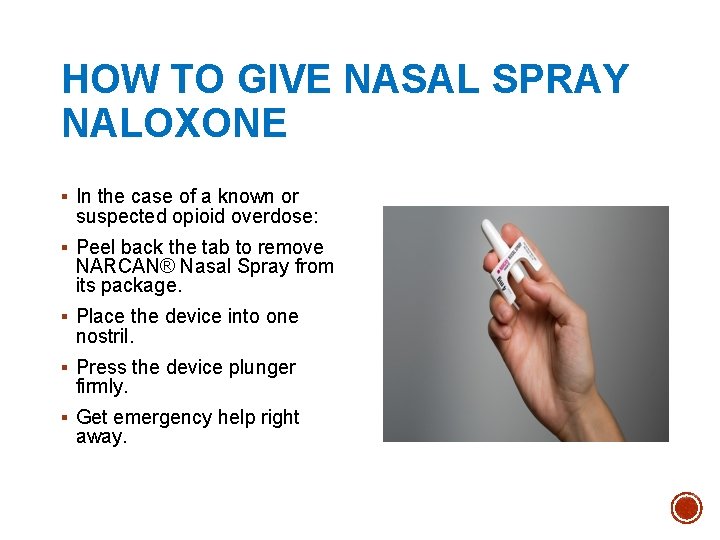
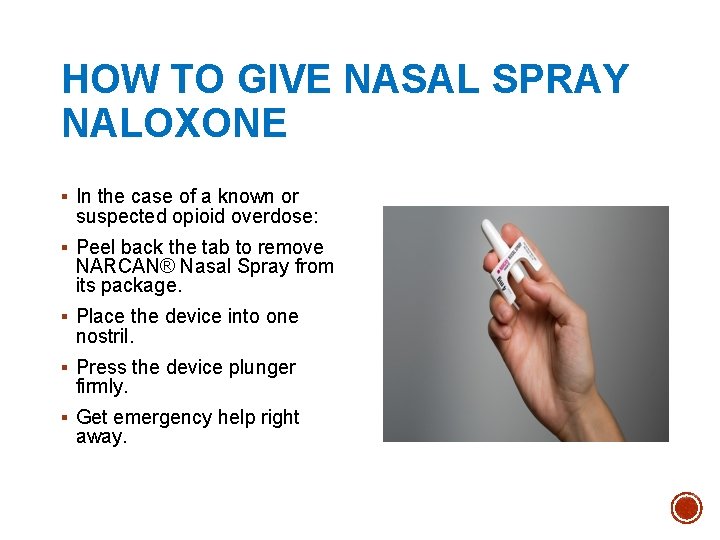
HOW TO GIVE NASAL SPRAY NALOXONE § In the case of a known or suspected opioid overdose: § Peel back the tab to remove NARCAN® Nasal Spray from its package. § Place the device into one nostril. § Press the device plunger firmly. § Get emergency help right away.
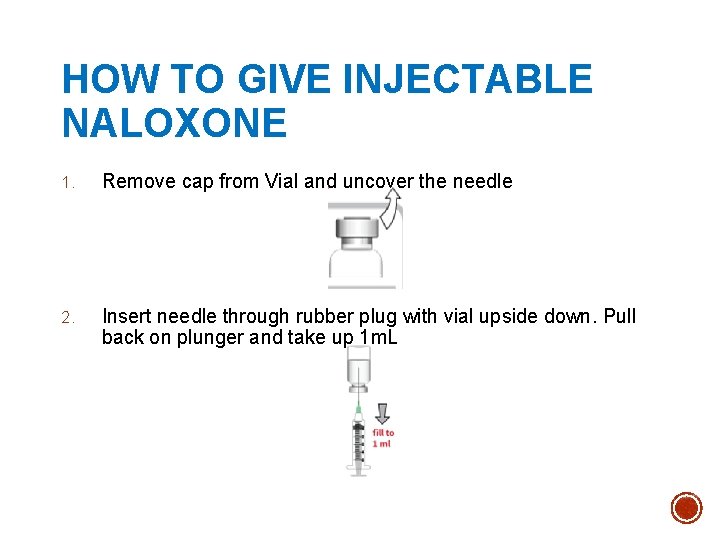
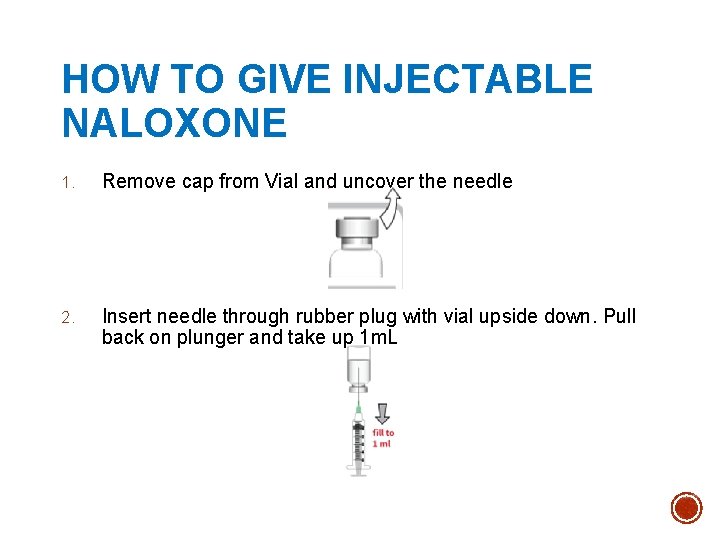
HOW TO GIVE INJECTABLE NALOXONE 1. Remove cap from Vial and uncover the needle 2. Insert needle through rubber plug with vial upside down. Pull back on plunger and take up 1 m. L
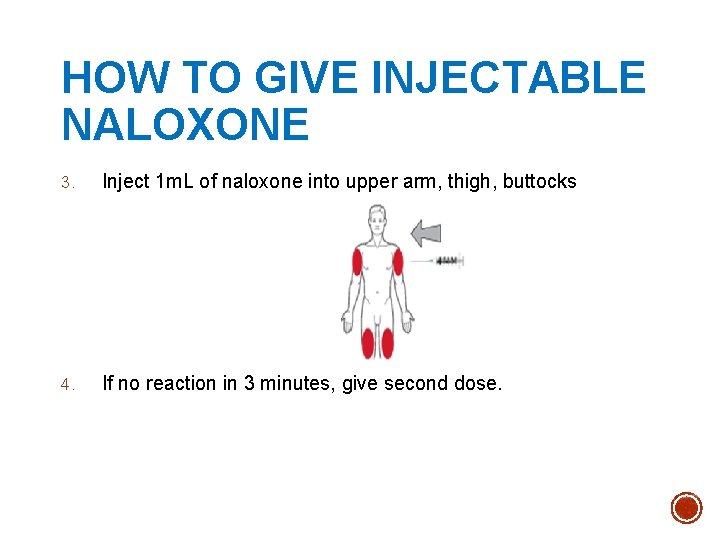
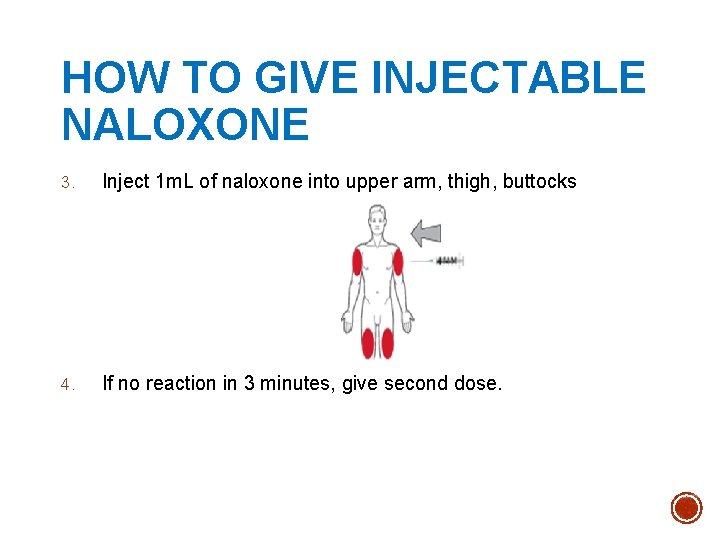
HOW TO GIVE INJECTABLE NALOXONE 3. Inject 1 m. L of naloxone into upper arm, thigh, buttocks 4. If no reaction in 3 minutes, give second dose.
WHILE YOU’RE WAITING FOR NALOXONE TO KICK IN… § Start rescue breathing again until you see the person start to breathe on their own. § Wait 2 -3 minutes (longer if administering IN naloxone) to give the medication a chance to work. § If no response after 2 -3 minutes, give a second dose of naloxone and begin rescue breathing again. § If still no response, continue rescue breathing until paramedics arrive and let them take over. § Note: naloxone will only work if the individual has taken an opioid. If they overdosed on a non-opioid, naloxone will not have an effect on them.
WHAT TO EXPECT AFTER ADMINISTRATION OF NALOXONE… § Stay with the person for as long as you can or until help arrives § If the person is still unresponsive, make sure to lay them in the recovery position to prevent choking and wait for help. § If the person is responsive, they will be confused about what is happening and will probably not remember overdosing. § Explain what has happened § Comfort the person; withdrawal symptoms triggered by naloxone can feel unpleasant. § Some people may become agitated or combative and will need help remaining calm. § Don’t allow the person to take more opioids, as they can overdose again.
NALOXONE FACTS § Onset of action is about 2 -3 minute § Duration of action is 30 -120 minutes depending on method of administration § It will not reverse an overdose caused by other drugs, only opioids § May be used in children and pregnant women § Naloxone should be stored in its original packaging, while avoiding light, at room temperature. § It can be left in the car glove box overnight, but not as a permanent storage option § Pay attention to the expiration date for any naloxone product. Most have an expiration date of about 12 -18 months. § Expired naloxone can still be administered if there is no other alternative available. However, it may not be as effective and a second dose may be required.
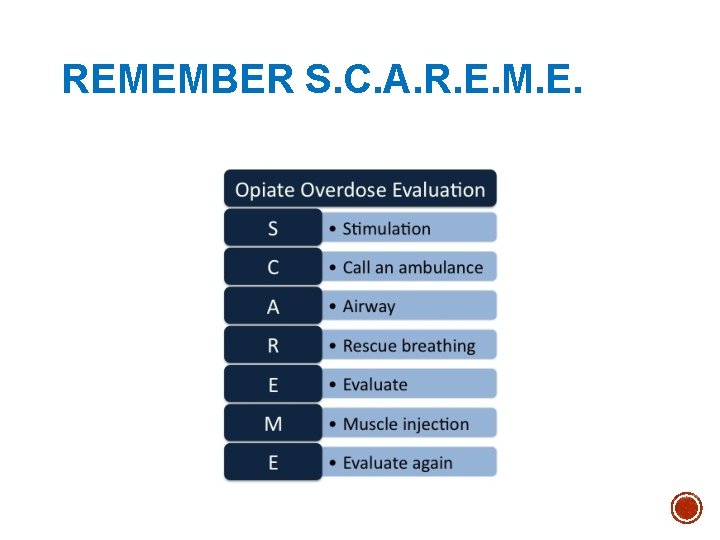
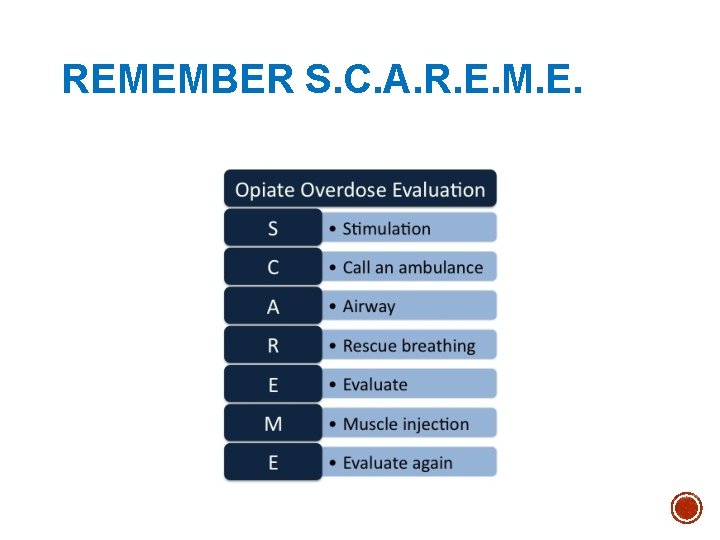
REMEMBER S. C. A. R. E. M. E.
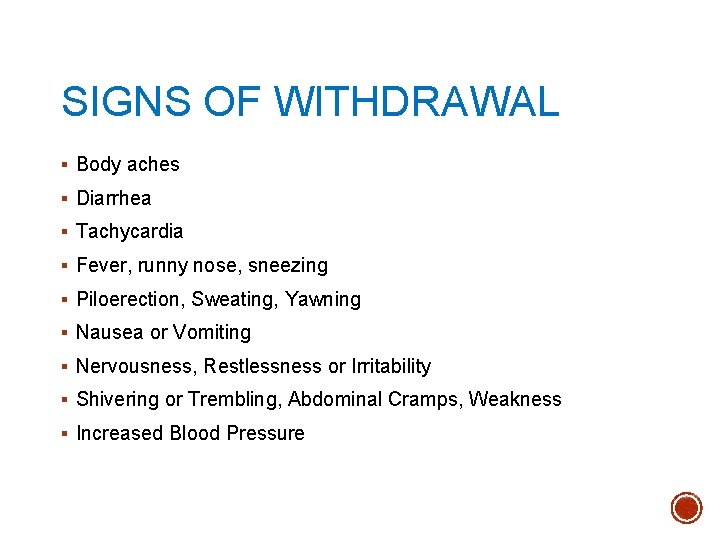
SIGNS OF WITHDRAWAL § Body aches § Diarrhea § Tachycardia § Fever, runny nose, sneezing § Piloerection, Sweating, Yawning § Nausea or Vomiting § Nervousness, Restlessness or Irritability § Shivering or Trembling, Abdominal Cramps, Weakness § Increased Blood Pressure
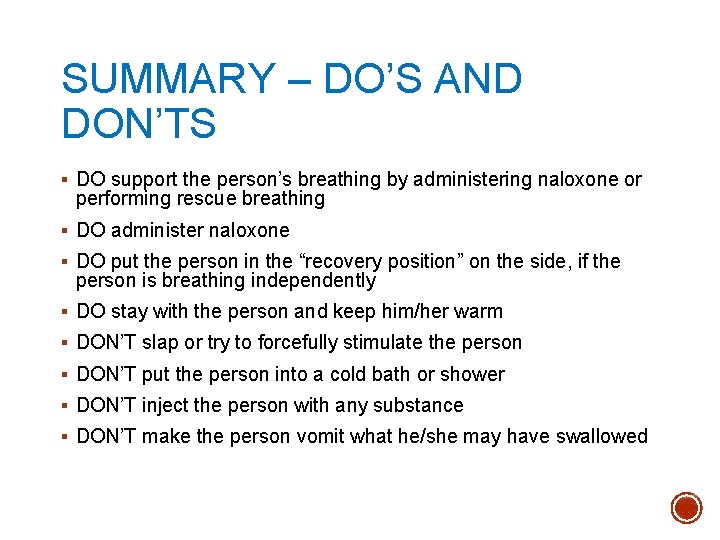
SUMMARY – DO’S AND DON’TS § DO support the person’s breathing by administering naloxone or performing rescue breathing § DO administer naloxone § DO put the person in the “recovery position” on the side, if the person is breathing independently § DO stay with the person and keep him/her warm § DON’T slap or try to forcefully stimulate the person § DON’T put the person into a cold bath or shower § DON’T inject the person with any substance § DON’T make the person vomit what he/she may have swallowed
SAMSHA Treatment Locator: Convenient and Easy to use Behavioral Health and Substance Abuse Treatment locator: https: //findtreatment. samhsa. gov/locator
M. A. T. - MEDICATION ASSISTED TREATMENT History: In the post- WWII there was a significant rise in the use of § § § opioids. The federal government became concerned with the effects this was having on communities, so they began to increase punishment for possession and distribution. At this time the psychiatric community was finding that people addicted to opioids were much more likely to relapse despite the completion of detoxification and treatment programs. When this did little to quell the problem, the medical community began to advocate for opioid maintenance programs in which people dependent on opioids were given small doses under the care of a medical professional. The initial interventions didn’t work because they used short half-life medications such as morphine. Patients quickly developed tolerance and needed increasing amounts of medication. Higher doses of morphine caused increased sedation and interfered with patients social functioning. In response the federal government began funding experimental programs to use Methadone.
FORMS OF M. A. T. § Methadone was the first successful medication used in conjunction with dependency treatment. It is a long acting agonist that is taken orally and binds with the opiate receptors. It stops withdrawal and craving while allowing the patient to function, and at appropriate dosing does not have any of euphoric or sedative effects. It is only available through approved treatment programs and is usually dispensed daily. § Buprenorphine/Naloxone combination medication contains buprenorphine (a partial agonist) and naloxone (an antagonist) designed to ward off attempts to get high through injection because if injected it can trigger withdrawal effects. In 2002 brand name Suboxone became the first form of MAT to be available by prescription from an office-based physician. § Long acting injectable naltrexone (Vivitrol) is the newest form of MAT. It is an antagonist that prevents the opioids to attaching to receptors, thus if a person takes an opioid any opioid effect is blocked. It is given monthly administered through a treatment program or office based physician.
EFFECTIVENESS § Support for MAT is on a international scale. A 2014 briefing from SAHMSA lists the following as supporters of MAT: § National Association of State Alcohol and Drug Abuse Directors § World Health Organization § National Institute of Drug Court Professionals § National Institute on Drug Abuse § This study also reviewed current literature to find the effectiveness of each type of MAT § Methadone- In 11 clinical trials of involving 1969 people, methadone improved retention and reduced use compared to non-medication treatment. § Suboxone-SAHMSA reviewed clinical trials and saw that Suboxone was more effective than placebo, but not as effective as methadone. § Vivitrol- A six month multi state study of people under legal supervision had “significantly fewer” positive urine tests.
NALOXONE FOR THOSE WHO NEED IT MOST § NUMBER ONE priority: Put naloxone in the hands of those most likely to be on the scene and first to respond, individuals who use opioids, themselves. § How best to reach this population? By making naloxone available, in these settings: § Syringe Exchange Programs § Jails § Hospital Emergency Departments § Free Clinics § First Responders § Friends and Family members § Methadone, Suboxone and Other Treatment Programs
IN TREATMENT – VULNERABLE POPULATION § People entering & exiting Treatment for Opiate Use Disorder § Effective January 1, 2017, all substance use treatment programs licensed by IDHS/DASA must provide educational information to clients identified as having or seeking treatment for opioid use disorder, including the use of a medication for the use of opioid use disorder, recognition of and response to opioid overdose, and the use and administration of naloxone (PA 99 -0553). § Ideally, each treatment program would: § Train each staff person/participant how to administer naloxone § Encourage each participant to access a dose of naloxone either through an outreach effort or with an insurance card at a pharmacy
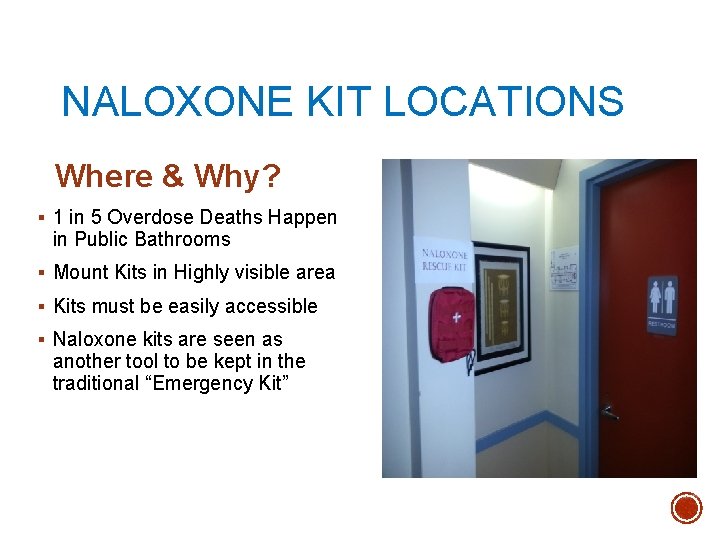
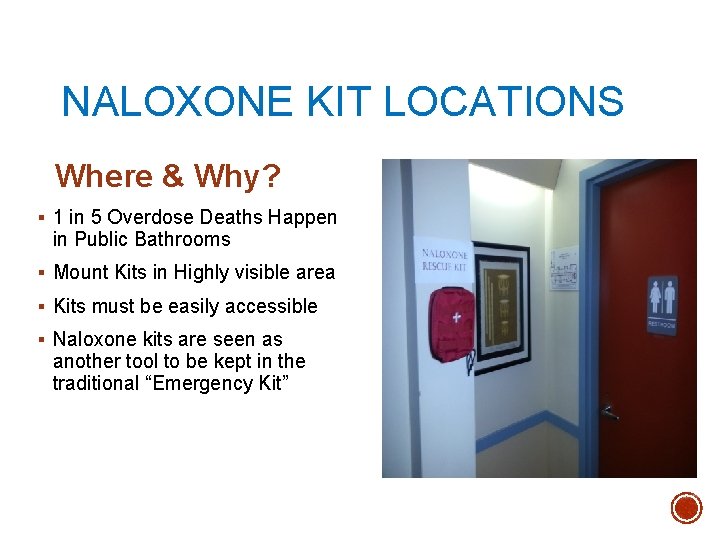
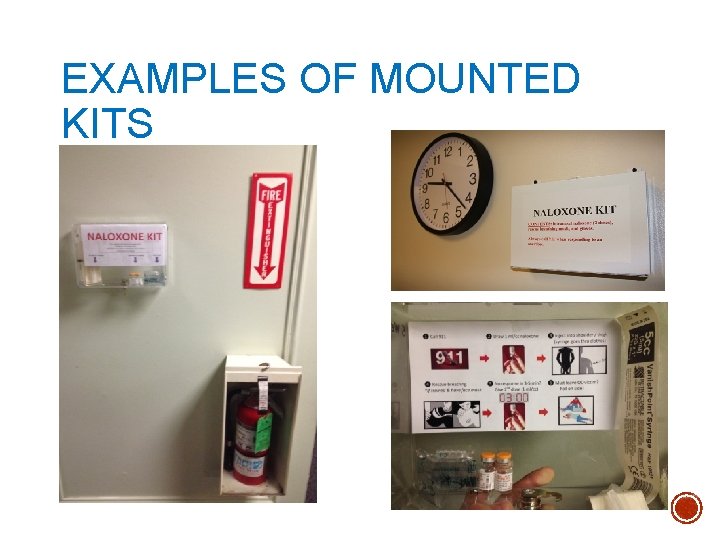
NALOXONE KIT LOCATIONS Where & Why? § 1 in 5 Overdose Deaths Happen in Public Bathrooms § Mount Kits in Highly visible area § Kits must be easily accessible § Naloxone kits are seen as another tool to be kept in the traditional “Emergency Kit”
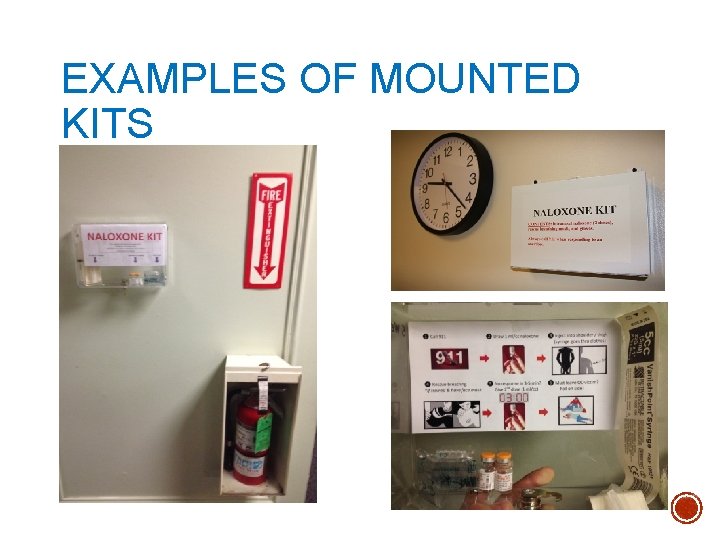
EXAMPLES OF MOUNTED KITS

DHS/DASA DRUG OVERDOSE PREVENTION PROGRAM (DOPP) Benefits of Enrolling • • Be part of the effort to reduce opioid deaths in Illinois. Gain access to innovative training; Stay informed about the most current legislation; Inform your community about naloxone and help save lives! Click here for Program Guideline Manual
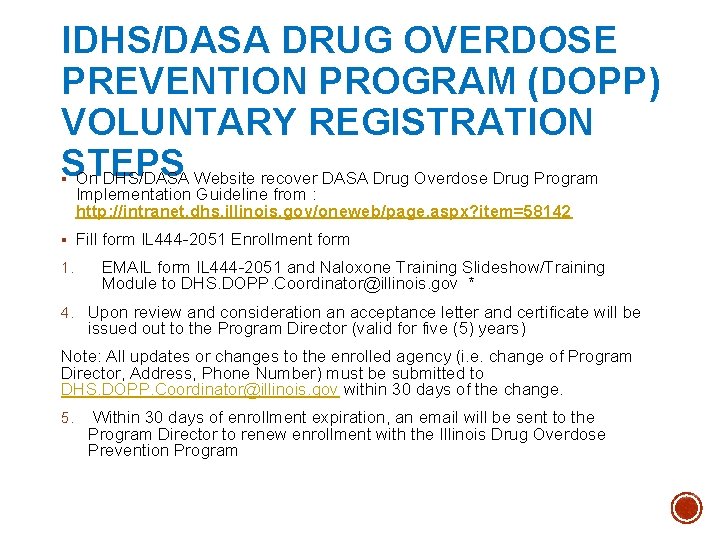
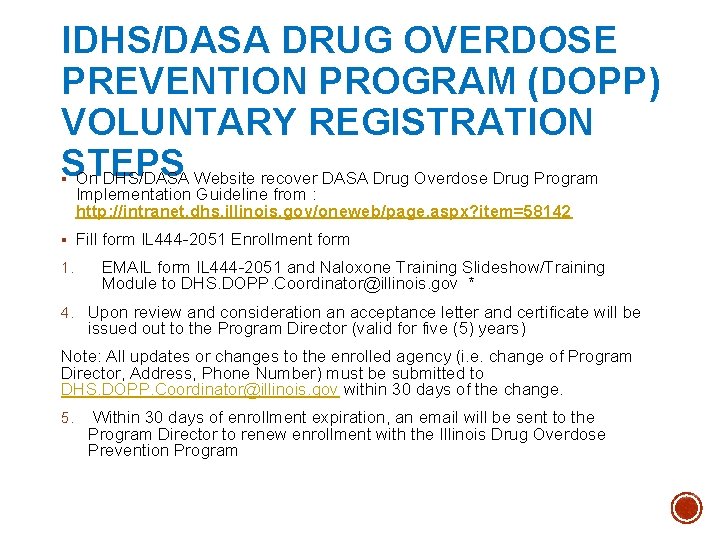
IDHS/DASA DRUG OVERDOSE PREVENTION PROGRAM (DOPP) VOLUNTARY REGISTRATION STEPS On DHS/DASA Website recover DASA Drug Overdose Drug Program § Implementation Guideline from : http: //intranet. dhs. illinois. gov/oneweb/page. aspx? item=58142 § Fill form IL 444 -2051 Enrollment form 1. EMAIL form IL 444 -2051 and Naloxone Training Slideshow/Training Module to DHS. DOPP. Coordinator@illinois. gov * 4. Upon review and consideration an acceptance letter and certificate will be issued out to the Program Director (valid for five (5) years) Note: All updates or changes to the enrolled agency (i. e. change of Program Director, Address, Phone Number) must be submitted to DHS. DOPP. Coordinator@illinois. gov within 30 days of the change. 5. Within 30 days of enrollment expiration, an email will be sent to the Program Director to renew enrollment with the Illinois Drug Overdose Prevention Program

PROGRAM ADMINISTRATION The Program Director Will: § Identify a physician, physician assistant, or advanced practice nurse to oversee the clinical aspects of the Drug Overdose Prevention Program ; § Establish the content of a training program, which is consistent with the SAMHSA toolkit and IDHS/DASA policies and procedures ; § Maintain and review Drug Overdose Prevention Program records including quarterly training records, inventory of supplies and materials, and reversal forms
PROGRAM ADMINISTRATION (CONT) § The Health Care Professional Will: § Serve as a clinical advisor and liaison concerning medical issues related to the Drug Overdose Prevention Program; § Provide consultation to ensure that all trained Overdose Responders are properly trained; § Adapt and approve training program content and protocols; § Provide liaison with local emergency medical services and emergency dispatch agencies, where appropriate; § Review reports of all administration of an opioid antagonist
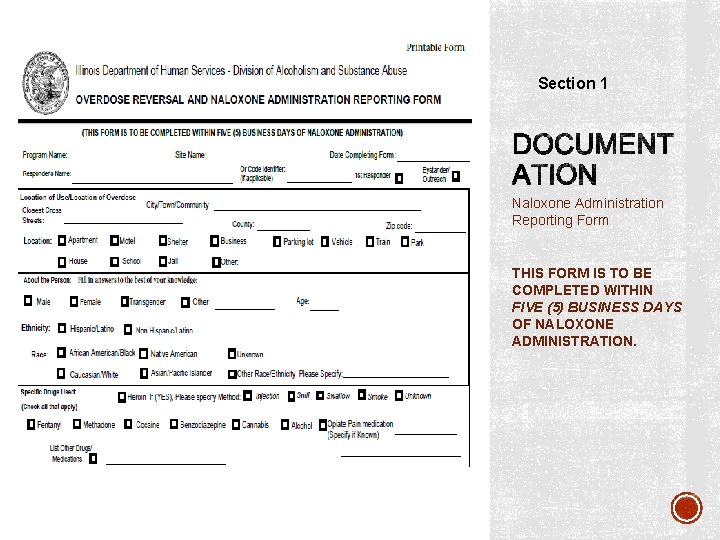
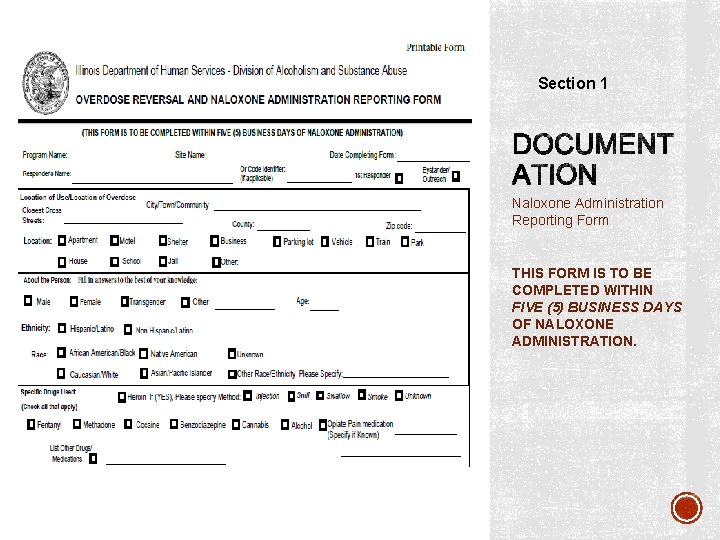
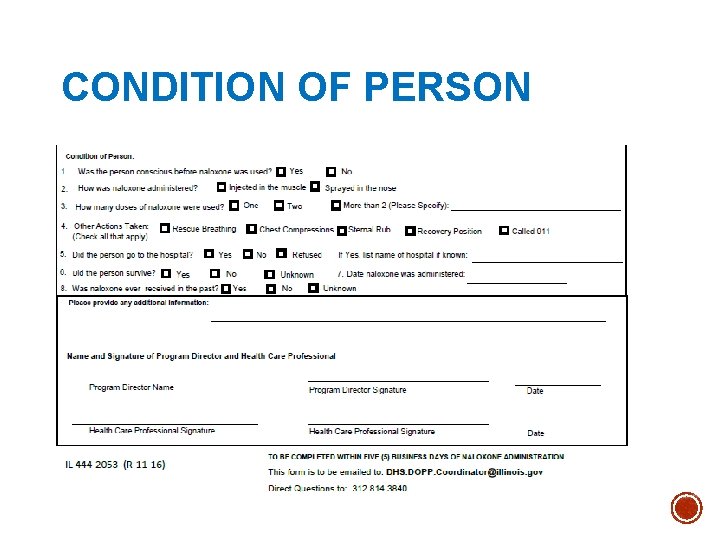
Section 1 Naloxone Administration Reporting Form THIS FORM IS TO BE COMPLETED WITHIN FIVE (5) BUSINESS DAYS OF NALOXONE ADMINISTRATION.
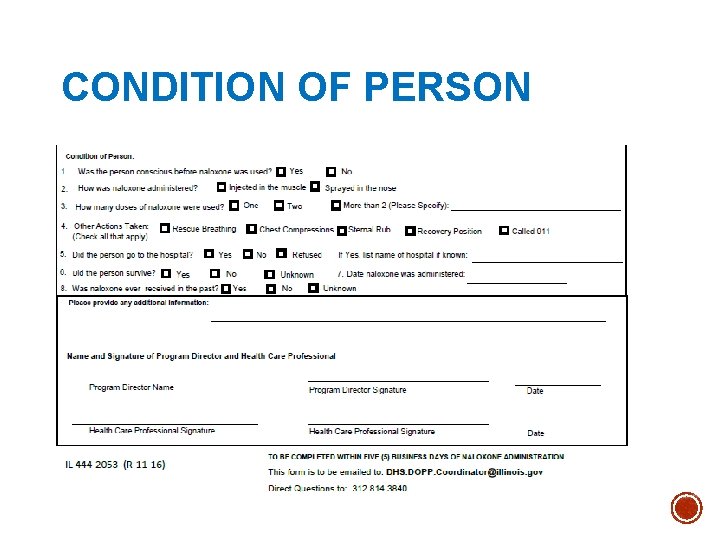
CONDITION OF PERSON
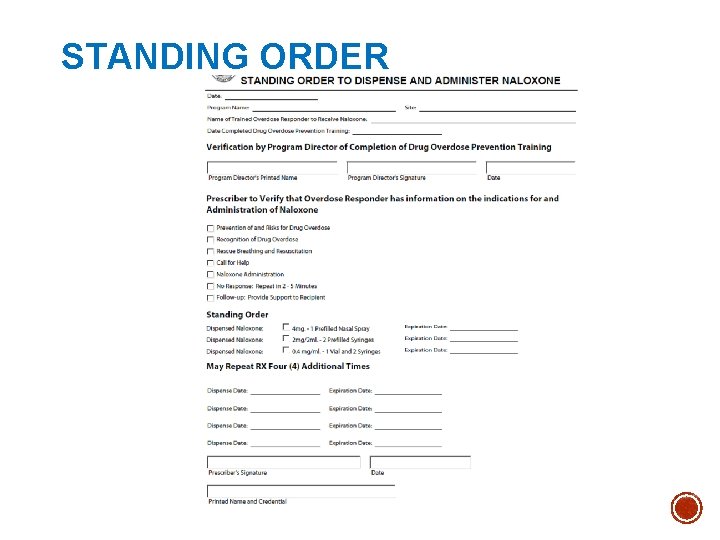
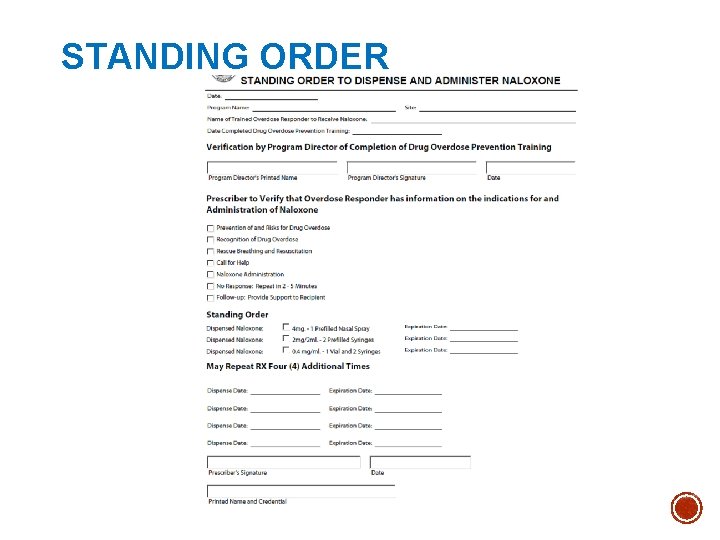
STANDING ORDER
TRAINING CURRICULUM & MATERIALS § Describe the qualifications of individuals who can provide the drug overdose prevention training ( including the use of naloxone) to potential responders; § Describe the duration and frequency requirements to training; § Describe any required supervision or monitoring of drug overdose responders and program trainers; § Use available reference material to enhance training content; § Describe the training oversight responsibilities of the program’s official designee and HCP. § Utilize resource materials on DHS/DASA website – DOPP § DOPP webinar and slides are welcomed to be copied
§ Drug Overdose Prevention Program email: § DHS. DOPP. coordinator@illinois. gov § (email all forms to this email) § Seth Eisenberg, M. D. § Seth. Eisenberg@illinois. gov § Rosie Gianforte § Rosie. m. gianforte@illinois. gov § 312 -814 -2136

§ Anatomy of an Overdose https: //www. youtube. com/watch? v=Dh. S 9 M 2 ni 2 y. E § Administering Nasal Atomizer Naloxone Bystander video § http: //adaptpharma. com/news-events/press-kit § Administering injectable naloxone § https: //vimeo. com/197652566/ce 41306803 § https: //vimeo. com/197650414/4916741 e 17 (Spanish) § Recognizing an overdose & Reversing an overdose § https: //www. youtube. com/watch? v=FZpgj. RBby_M § M. A. T. Treatment § https: //youtu. be/ht 7 Ep. K 2 UF 4 I
News + research on overdose prevention § Publications and Resources §Prescribetoprevent. org § Law Enforcement Naloxone Toolkit at the §Get. Naloxone. Now. org Bureau of Justice Assistance’s National Training and Technical Assistance Center (link is external) §preventionalliance. org § Naloxone Injection at Medline. Plus Opioid overdose prevention education § Opioid Overdose Prevention Toolkit – 2014 §Stopoverdose. org Family support GRASP: Grief Recovery After a Substance Passing § Grasphelp. org § Learn 2 cope. org
 Icg grant illinois
Icg grant illinois Raymond carver alcoholism
Raymond carver alcoholism Pes statement for alcoholism
Pes statement for alcoholism Phases of alcoholism
Phases of alcoholism Alcoholism
Alcoholism Iowa department of health and human services
Iowa department of health and human services Seattle human services department
Seattle human services department Milwaukee health and human services
Milwaukee health and human services Maine department of health and human services
Maine department of health and human services Delaware county department of human services
Delaware county department of human services Illinois department of rehabilitation
Illinois department of rehabilitation Wake county human services community services center
Wake county human services community services center Illinois healthcare lien act
Illinois healthcare lien act Siue hr forms
Siue hr forms Mohari botanical name
Mohari botanical name Division of academics department of mathematics
Division of academics department of mathematics Enterprise dedicated network
Enterprise dedicated network Imf
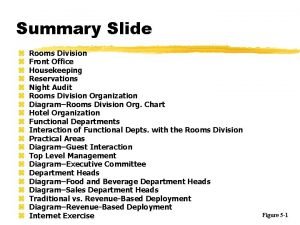
Imf Room division in hotel
Room division in hotel Room division department
Room division department Long division and short division
Long division and short division Polynomial long division definition
Polynomial long division definition 2065 divided by 5
2065 divided by 5 Synthetic diviison
Synthetic diviison Worcester building dept
Worcester building dept Washington state department of social and health services
Washington state department of social and health services Miami dade county juvenile services department
Miami dade county juvenile services department Fl dept of agriculture
Fl dept of agriculture Deshaney v. winnebago background
Deshaney v. winnebago background Caldwell county dss
Caldwell county dss Albany county dss
Albany county dss Miami dade county internal services department
Miami dade county internal services department Department of correctional services strategic plan
Department of correctional services strategic plan Virginia department of agriculture food safety
Virginia department of agriculture food safety California department of general services
California department of general services Nys division of criminal justice services
Nys division of criminal justice services Measurement units standards and services department
Measurement units standards and services department Department of health and senior services missouri
Department of health and senior services missouri Cacfp nebraska
Cacfp nebraska New hampshire department of administrative services
New hampshire department of administrative services Department management services dms
Department management services dms Veterinary services division
Veterinary services division Court support services division
Court support services division Missouri division of youth services
Missouri division of youth services Bureau of dealer services
Bureau of dealer services Division of vocational rehabilitation
Division of vocational rehabilitation Lausd recipes
Lausd recipes Division of local services
Division of local services Swot analysis introduction
Swot analysis introduction Human resource management 15th edition
Human resource management 15th edition Swot analysis for human resource department
Swot analysis for human resource department Calhr fmla
Calhr fmla Georgia department of human resources
Georgia department of human resources Human resources department adalah
Human resources department adalah Human resorces department
Human resorces department Pfizer human resources department
Pfizer human resources department Merck human health division
Merck human health division Integrated and differentiated services in computer networks
Integrated and differentiated services in computer networks Siskiyou county human services
Siskiyou county human services Health and human services milwaukee
Health and human services milwaukee Anna y reed and eli weaver
Anna y reed and eli weaver