IHP Dementia Knowledge Day LOROS Hospice 14 th


















- Slides: 87
IHP Dementia Knowledge Day LOROS Hospice, 14 th July 2010
Welcome Alan Heron, Senior Commercial Manager, IHP.
Achieving the National Dementia Strategy: Prof. Jane Gilliard, National Dementia Strategy Programme Manager, Dept. of Health.
The National Dementia Strategy Professor Jane Gilliard NDS National Programme Manager (Implementation) Social Care, Local Government and Care Partnerships
National dementia strategy Launched Feb 2009 The 3 themes • Public and professional awareness • Early diagnosis • Quality of care 17 (+1) recommendations
Why a National Dementia Strategy? • Currently 570, 000 people with dementia in England (700, 000 in UK) • Numbers likely to double in the next 30 years • Cost currently is £ 17 billion • Costs likely to treble to more than £ 50 billion Ø Ø Ø Dementia is one of the main causes of disability later in life, ahead of some cancers, cardiovascular disease and stroke 40% of people admitted to hospital have dementia 30% of older people develop delirium during their stay in hospital 50% of hip fracture patients have dementia At least 50% of long term care residents have dementia 40% of the work of community matrons is focussed on people with dementias a co-morbid condition Need to improve range and quality of support and services
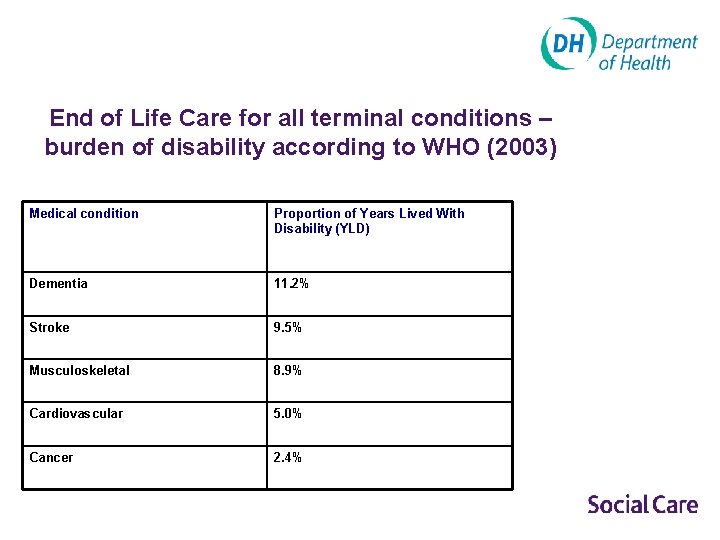
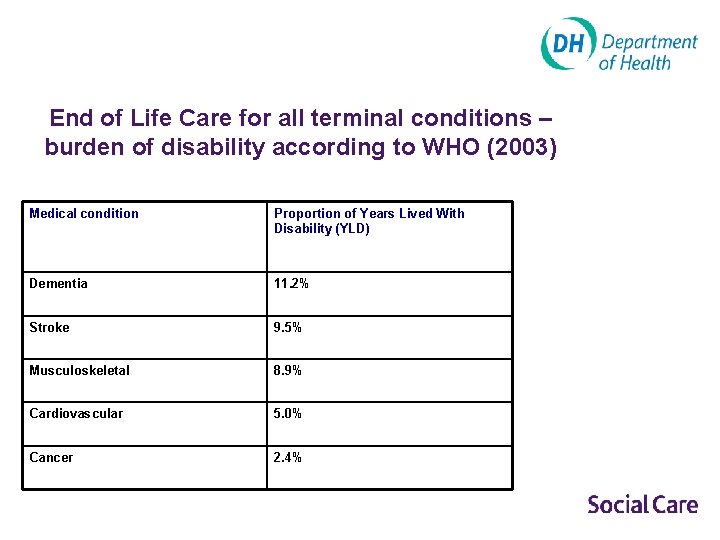
End of Life Care for all terminal conditions – burden of disability according to WHO (2003) Medical condition Proportion of Years Lived With Disability (YLD) Dementia 11. 2% Stroke 9. 5% Musculoskeletal 8. 9% Cardiovascular 5. 0% Cancer 2. 4%
Dying from and with dementia • 60, 000 die directly of dementia yearly Knapp & Prince 2007 • A common contributor or accompaniment to dying: 1 in 3 of over 65 s will die with dementia Byrne 2006
Objective 12 - improved end of life care for people with dementia People with dementia and their carers to be involved in planning end of life care which recognises the principles outlined in the Department of Health End of Life Care Strategy. Local work on the End of Life Care Strategy to consider dementia.
Priorities for implementation 17 Objectives, of which seven are priorities: • Good-quality early diagnosis and intervention for all • Improved community personal support services • Implementing the Carers’ Strategy • Improved quality of care for people with dementia in general hospitals • Living well with dementia in care homes • An informed and effective workforce for people with dementia • A joint commissioning strategy.

Year 1: Building the foundations • Leadership – – – People with dementia and carers Prof Alistair Burns, National Clinical Director, Dementia Sir Ian Carruthers, CE South West Strategic Health Authority Jenny Owen and Simon Williams, Association Directors Adult Social Services (ADASS) Martin Green, ECCA, Care Homes • National and Regional Programmes in place and working – Central implementation team: policy and implementation • A lead and implementation programme for each priority Objective – Regional implementation team • Making Connections – Policy: embedding dementia with Dignity, Carers and working with other key policy areas eg Personalisation – Professional bodies eg Royal Colleges – Other work programmes eg Enhancing the Healing Environment • Implementation projects – Advisory/project groups in place for the Objectives: building partnerships and buy-in – Projects commissioned and underway

Key events in the last year • 40 Demonstrator Sites for Dementia Advisors (22) and Peer Support (18) • Joint Commissioning Framework published June and national conference October 2009 • Cause, Care and Cure - major national research summit • Regional leadership network established • Skills for Health/Care mapping training and education • Pocket guides issued for care home managers issued in October • 1 st national memory assessment conference Nov 2009 • Anti-psychotics Review published November
Antipsychotics in dementia 11 recommendations • Reducing use is a priority backed up by audit and explicit goals • Curricula needed • In reach to homes • Care Quality Commission • Access to Psychological Therapies Programme • People with dementia in their own homes.
Objective 12 – improving end of life care • Established partnerships with Eo. LC Strategy team and National Eo. LC programme • Links with NCPC and Dying Matters • NEo. LC newsletter – Issue 17, Dec 2009 • NICE Commissioning Guidance – published ? ? • Established a reference group to advise and steer work • Developing online web-based resource guide • Due to launch in August • www. endoflifecareforadults. nhs. uk
Eo. LC innovative practice • Haringey audit tool • Palliative care for people with dementia in Croydon • Gables Nursing Home in Peterborough • Southwark modernisation initiative • Greater Manchester and Cheshire Cancer Network
Implementing best practice • Need to spread and adopt models of best practice • Dementia Portal to diffuse best examples • We all need to innovate - a challenge for us all, but we all can • But avoid re-inventing of wheels, and learn from the best • Remember, always be ready to replicate.
Conclusions • Strategy widely welcomed • National and regional support in place • Range of national initiatives to support implementation • High profile in terms media and other interest • Priority indicated from the centre • Clinical leadership provided by new National Clinical Director • Focus on disseminating best practice • Are changes really happening on the ground?
Contacts Jane. Gilliard@dh. gsi. gov. uk Claire. Goodchild@dh. gsi. gov. uk www. dementia. dh. gov. uk www. endoflifecareforadults. nhs. uk
Implementing end of life care: Dr Sanjana Nyatsanza, MBBS, MD (Psychiatry), MRCPsych, Cambridgeshire & Peterborough NHS Foundation Trust.
Implementing End of Life Care in Dementia 14 th July 2010 Dr Sanjana Nyatsanza Consultant Old Age Psychiatrist Cambridgeshire & Peterborough NHS Foundation Trust
Outline Ø What is Palliative Care Ø Government guidelines Ø How to improve end-of-life care Ø Application of Mental Capacity Act Ø CQC Regulations
What is Palliative Care? An approach that improves the quality of life of patients and their families facing the problems associated with life -threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual. (WHO) “palliare” – to cloak or cover
Recent Reports Ø Dementia is a terminal condition l Prognosis 3 -9 yrs from diagnosis; avg - 4. 5 yrs Ø 60, 000 deaths pa attributable to dementia - Dementia 2010 – Ø RCP Report – Palliative Care Services: Meeting the Needs of Patients (2007) Alzheimer’s Research Trust l l Encourages move from charity-based hospices to mainstream NHS To ensure standards & equitable services *D Jolley & M Tapley - Due respect & professional care in death - The Psychiatrist - April 2010
Who does Palliative Care apply to? Ø Previously reserved for malignancy Ø Government policies encourage application of palliative care principles in all terminal conditions, including dementia Ø Traditional models may not be appropriate Ø Changes in service provision, attitude & education are needed

Challenges in providing good palliative care in Dementia Difficulty viewing dementia as a terminal illness Ø Lack of awareness among staff / carers Ø l l l Myths that patients do not experience pain or distressing symptoms Agitation attributed to ‘normal’ progression of dementia Unrecognised symptoms Lack of knowledge of assessment & symptom management Ø Difficulty in predicting start of the terminal phase Ø *S Bell - Peterborough Palliative Care in Dementia Group
Complex palliative care needs of people with dementia Ø Ø Ø Tend to be older; experience more pain in last months than cancer patients & spend last year of life in care homes Symptoms progress from memory impairment, to behavioural change Physical problems increase with falls, incontinence, difficulty swallowing & inanition. Terminal phase may include immobility, contractures, decubitus ulcers and recurrent infections; with behaviour that seems to indicate distress and is unresponsive to most approaches to reassurance * National Council for Palliative Care - Exploring palliative care for people with dementia * The Regional Study of Care of the Dying

Terminal phase of care in dementia is less than optimal Symptoms of distress unresolved, sometimes with no attempt to ameliorate them. Ø Repeated admissions to acute hospitals for assessment Ø Given ill-informed, inappropriate, life-sustaining treatment that only prolongs suffering & adds to confusion & distress Ø Development of additional complications - decubitus ulcers or colonisation with MRSA. Ø Carers are rarely informed of the likely outcomes for patients with dementia Ø *RCP Report – Palliative Care Services: Meeting the Needs of Patients
NICE-SCIE Guidance on palliative care in dementia ‘Dementia care should incorporate a palliative care approach from the time of diagnosis until death. The aim should be to support the quality of life of people with dementia and to enable them to die with dignity and in the place of their choosing, while also supporting carers during their bereavement, which may both anticipate and follow death. ’
Living well with dementia: A National Dementia Strategy Do. H, 2009 Objective 12: Improved end of life care for people with dementia. Ø People with dementia and their carers to be involved in planning care Ø Department of Health’s End of Life Care Strategy 2004 : requires integration of care across primary, secondary and tertiary healthcare and social services Ø Local work on the End of Life Care Strategy to consider dementia Ø
“Good” palliative care in dementia? (WHO 2002) A team approach: to relieve distressing symptoms; to affirm life and to see dying as a normal process, to be neither hastened nor postponed; to integrate the psychological and the spiritual; to offer a support system to help patients live as actively as possible and to help the family cope, including during bereavement; to enhance quality of life, which might positively influence the course of the illness; to become involved early in the course of the illness and to work in conjunction with otherapeutic approaches *J Hughes - Dementias 2010 Conference
CQC Regulations Ø involvement and information Ø personalised care and treatment Ø safety and safeguarding
What’s the evidence that a palliative care approach works? (Sampson, Ritchie, Lai, et al. 2005) Retrospective case-note studies demonstrate inadequate palliative care in both psychiatric and acute hospital wards (Lloyd-Williams, 1996; Sampson et al, 2006) Ø Equivocal evidence of the efficacy of a palliative model of care in dementia Ø Increased interest, but little evidence: ethical difficulties, prognostic uncertainty, lack of clear outcome measures Ø *J Hughes - Dementias 2010 Conference
Solutions Ø Cross-specialty training Ø Increased awareness – professionals, carers & public Ø Co-ordination of multi-agency care Ø Development of specialist hospice-style services, within the framework of continuing NHS care
The PEACE* programme physical and psychological symptoms advance care planning education about disease connections to community resources coordination of care with an interdisciplinary team lead by a clinical nurse specialist Ø patient-family centred care Ø use hospice services for end-stage patients Ø Ø Ø *Palliative Excellence in Alzheimer Care Efforts - Shega JW, Sachs GA. (2010) Offering supportive care in dementia: reflections on the PEACE programme. In: Supportive Care for the Person with Dementia

Application of Mental Capacity Act Ø Ø Ø Ø Five principles: l Presumption of capacity l Support to individual to reach the decision l The right to make unwise or eccentric decisions l Decisions should be in patients “Best Interests” l Least restrictive decision or action Be mindful of fluctuations in capacity Respect patient’s past wishes & feelings and valid / applicable advance decisions Involve IMCA, in case of serious medical treatment, esp. if harm or risks outweighs benefit (PEG) LPA or court appointed deputy Ultimate arbiter – Court of Protection - declaration Preferred place of care disputes; with holding life-sustaining treatment If subject to DOLS – death in custody
Advance Care Planning Ø Patients may still retain capacity to make informed choices Ø Involve patient and carers as far as possible, in care plans, in advance Ø Carers can plan for the future and feel more supported in making decisions Ø Better resolution of carers’ bereavement Ø Reduction in admissions from care homes to hospital
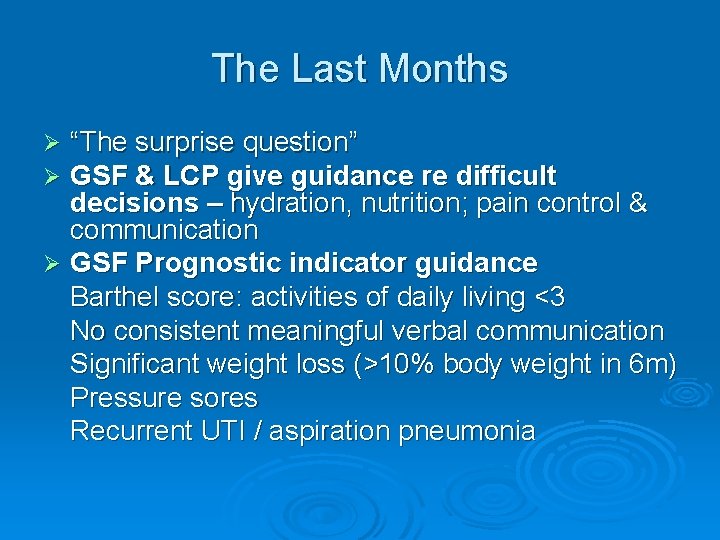
The Last Months “The surprise question” GSF & LCP give guidance re difficult decisions – hydration, nutrition; pain control & communication Ø GSF Prognostic indicator guidance Barthel score: activities of daily living <3 No consistent meaningful verbal communication Significant weight loss (>10% body weight in 6 m) Pressure sores Recurrent UTI / aspiration pneumonia Ø Ø
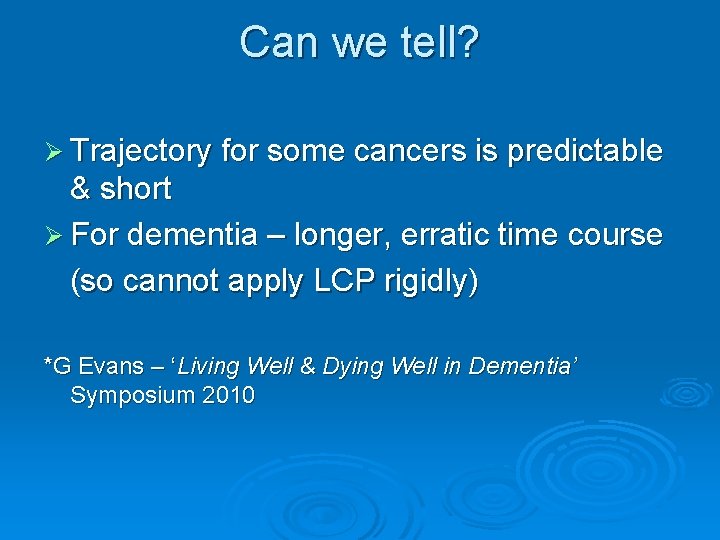
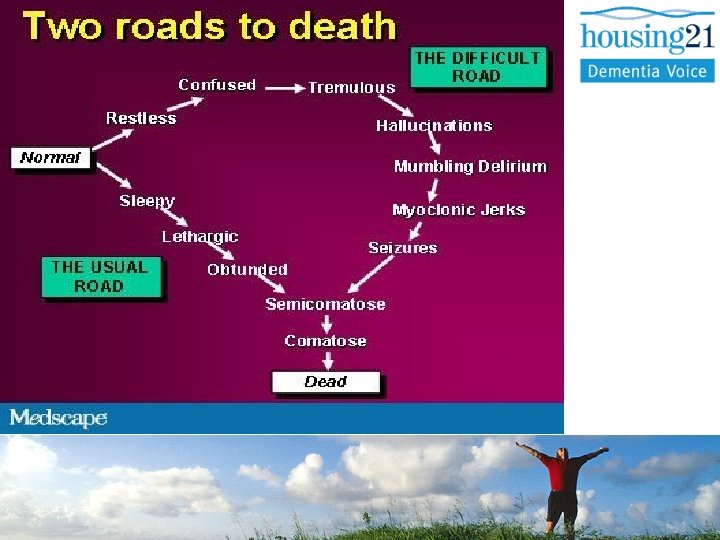
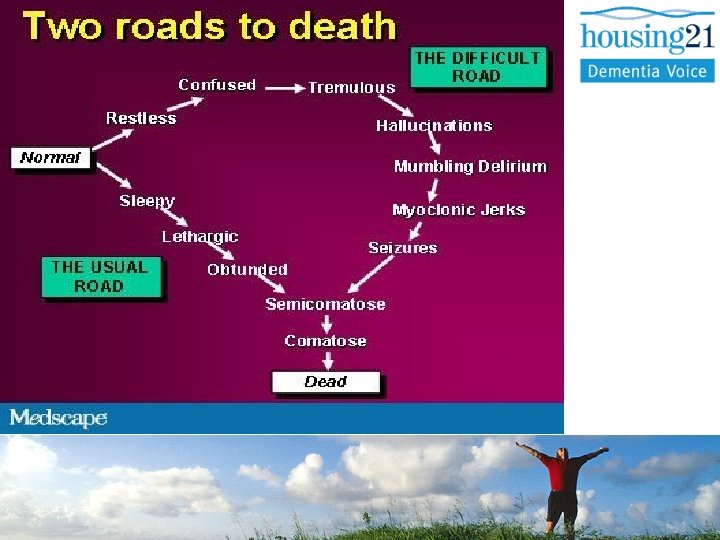
Can we tell? Ø Trajectory for some cancers is predictable & short Ø For dementia – longer, erratic time course (so cannot apply LCP rigidly) *G Evans – ‘Living Well & Dying Well in Dementia’ Symposium 2010
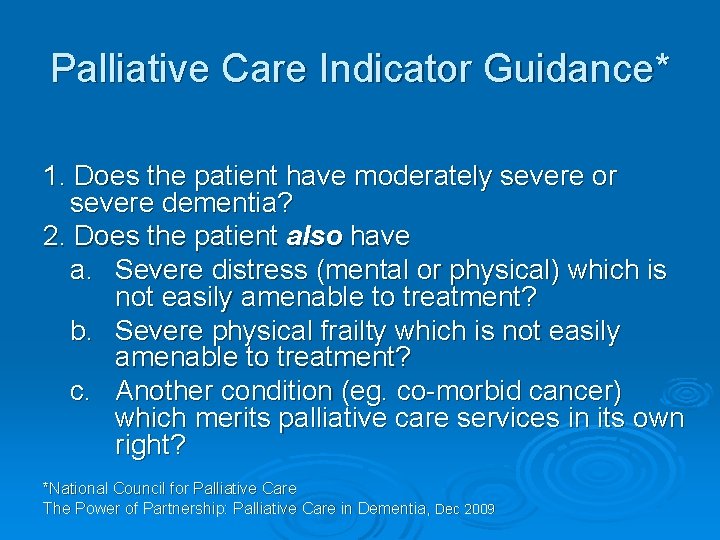
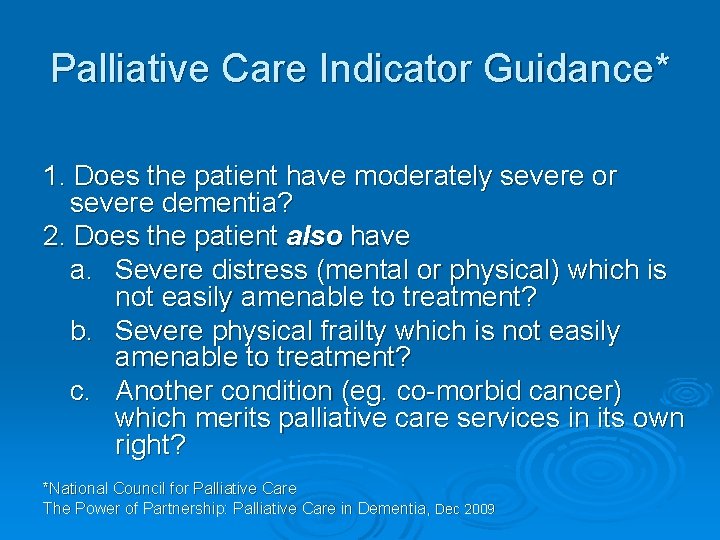
Palliative Care Indicator Guidance* 1. Does the patient have moderately severe or severe dementia? 2. Does the patient also have a. Severe distress (mental or physical) which is not easily amenable to treatment? b. Severe physical frailty which is not easily amenable to treatment? c. Another condition (eg. co-morbid cancer) which merits palliative care services in its own right? *National Council for Palliative Care The Power of Partnership: Palliative Care in Dementia, Dec 2009
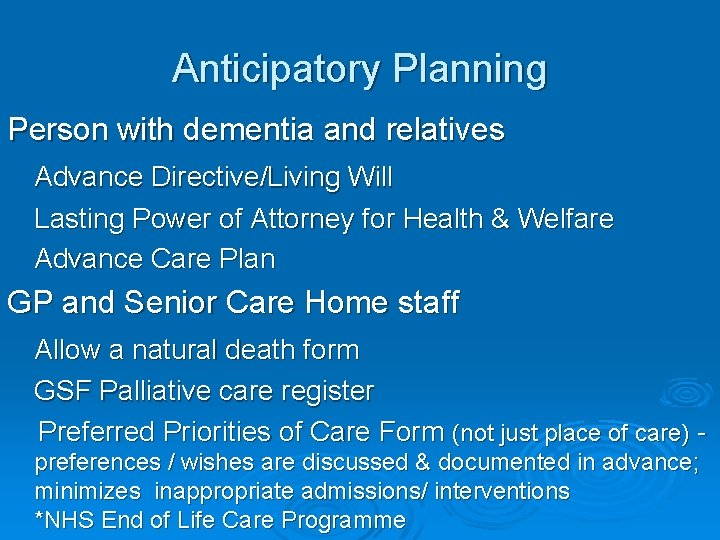
Anticipatory Planning Person with dementia and relatives Advance Directive/Living Will Lasting Power of Attorney for Health & Welfare Advance Care Plan GP and Senior Care Home staff Allow a natural death form GSF Palliative care register Preferred Priorities of Care Form (not just place of care) - preferences / wishes are discussed & documented in advance; minimizes inappropriate admissions/ interventions *NHS End of Life Care Programme
Contingency Plans Ø Ø Ø Ø Ø Active management of pain and distress Cardiopulmonary resuscitation Cancer chemotherapy Complex surgical procedures Hospital admission for injuries such as fractures Hospital admission for stroke Hospital admission for chest or other severe infections Swallowing difficulties Dehydration Terminal care

The Greenwich Care Home Illness Plan (GCHIP) Examples from the GCHIP: Use of Acute hospitals Ø We do/ do not recommend that hospital admission may be appropriate for injuries such as fractures Ø We do/ do not recommend that hospital admission may be appropriate for illness such as chest infections Terminal care Ø When dying is imminent and the patient is distressed we would expect that medication (e. g. antibiotics) will be given to alleviate the distress that may occur during death Patient has/ lacks capacity for this decision Patient aware Next of kin/ advocate aware GP initials Date
Common symptoms in the terminal phase Pain Ø Nausea & vomiting Ø Breathlessness Ø Distress/ restlessness/ agitation Ø Respiratory secretions (‘death rattle’) Ø *S Bell - Peterborough Palliative Care in Dementia Group
Diagnosing dying Ø Profound weakness Ø Drowsy or reduced cognition Ø Diminished intake of food/fluids Ø Difficulty swallowing medication Ø Abnormal breathing patterns Ø Reduced peripheral perfusion with skin colour and temperature changes

General considerations Ø Review of all medication and other interventions: l l l Can any drugs be stopped? Do routine obs need to continue? Can important drugs be given via an alternative route or changed to ones that can? e. g. syringe driver for SC drugs, PR NSAIDs l Is enteral feeding/ fluids continuing to offer benefit or can they be stopped?
Nursing care Quality nursing care is the basis of terminal care management Ø Try and involve the family Ø Attention to detail Ø Anticipate and prevent problems Ø l l l Careful positioning Skin care Pressure area care Mouth care Bowel & bladder care Eye care
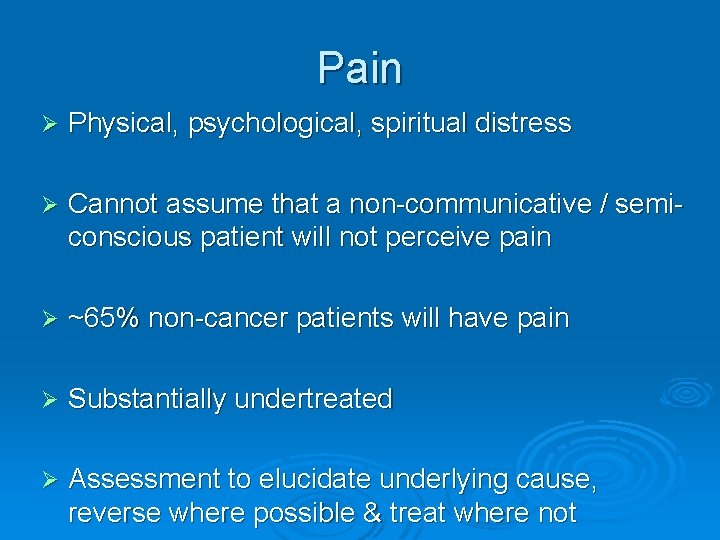
Pain Ø Physical, psychological, spiritual distress Ø Cannot assume that a non-communicative / semiconscious patient will not perceive pain Ø ~65% non-cancer patients will have pain Ø Substantially undertreated Ø Assessment to elucidate underlying cause, reverse where possible & treat where not

Pain Assessment Tools (PAINAD and Dis. DAT) to identify pain & monitor outcome of intervention in people with severe dementia Ø In terminal phase, oral route can be lost Ø Follow the WHO analgesic ladder & titrate carefully Ø Do not withhold strong analgesics if needed Ø Do not remove patch - continue to change as previously; give additional analgesia via CSCI Ø Opioid naive likely to need very small doses Ø l l Suppositories (Paracetamol, Diclofenac) Sublingual (Fentanyl, alfentanil) Parenteral (Morphine, Diamorphine, Oxycodone) Transdermal (Fentanyl & Buprenorphine)
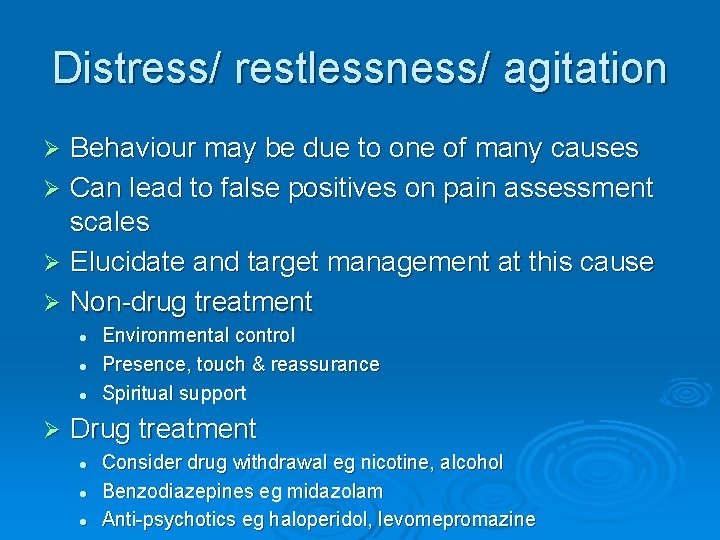
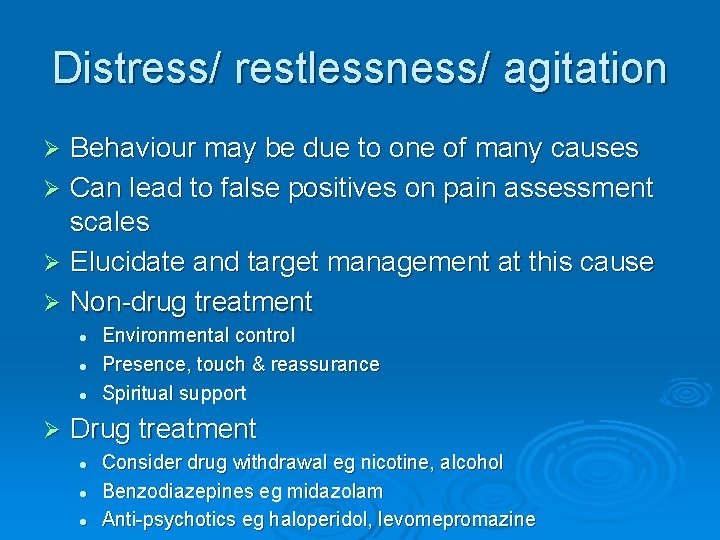
Distress/ restlessness/ agitation Behaviour may be due to one of many causes Ø Can lead to false positives on pain assessment scales Ø Elucidate and target management at this cause Ø Non-drug treatment Ø l l l Ø Environmental control Presence, touch & reassurance Spiritual support Drug treatment l l l Consider drug withdrawal eg nicotine, alcohol Benzodiazepines eg midazolam Anti-psychotics eg haloperidol, levomepromazine
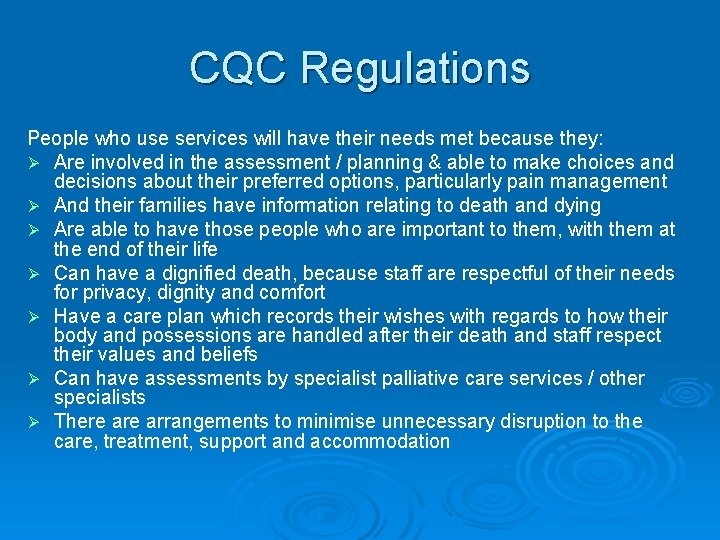
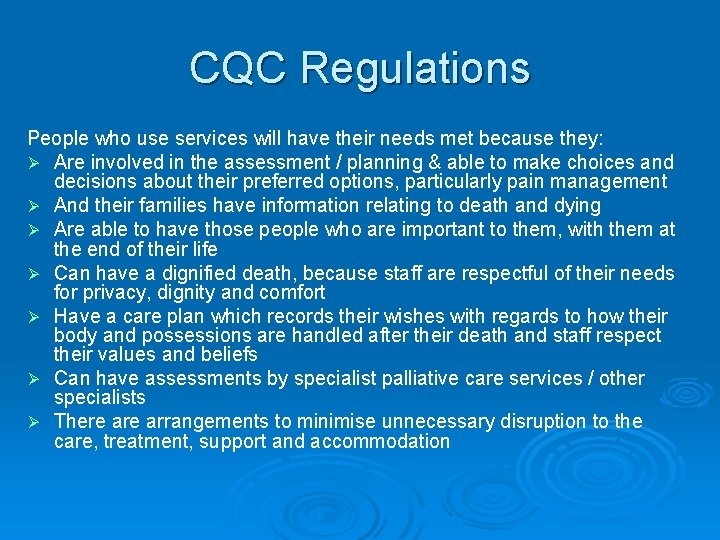
CQC Regulations People who use services will have their needs met because they: Ø Are involved in the assessment / planning & able to make choices and decisions about their preferred options, particularly pain management Ø And their families have information relating to death and dying Ø Are able to have those people who are important to them, with them at the end of their life Ø Can have a dignified death, because staff are respectful of their needs for privacy, dignity and comfort Ø Have a care plan which records their wishes with regards to how their body and possessions are handled after their death and staff respect their values and beliefs Ø Can have assessments by specialist palliative care services / other specialists Ø There arrangements to minimise unnecessary disruption to the care, treatment, support and accommodation

‘How people die remains in the memory of those who live on. ’ Dame Cicely Saunders - Founder of Modern Hospice Movement “Slowly, I learn about the importance of powerlessness. I experience it in my own life and I live with it in my work. The secret is not to be afraid of it – not to run away. The dying know that we are not God, All they ask is that we do not desert them. ” Cassidy S. Sharing the Darkness; the Spirituality of Caring.

How can collective procurement help? Tracey Allford, Operations Manager, LOROS.

LOROS Hospice • • Member since mid-2009 Local registered Charity providing care and support in Leicestershire & Rutland A specialist centre providing skilled nursing and medical focused on patient and relatives’ needs 31 in-patient Hospice and Day Centre with outreach facilities in the community
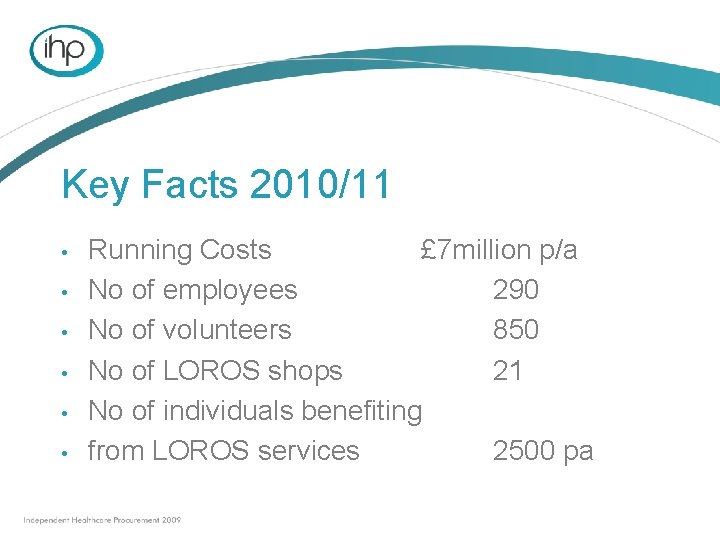
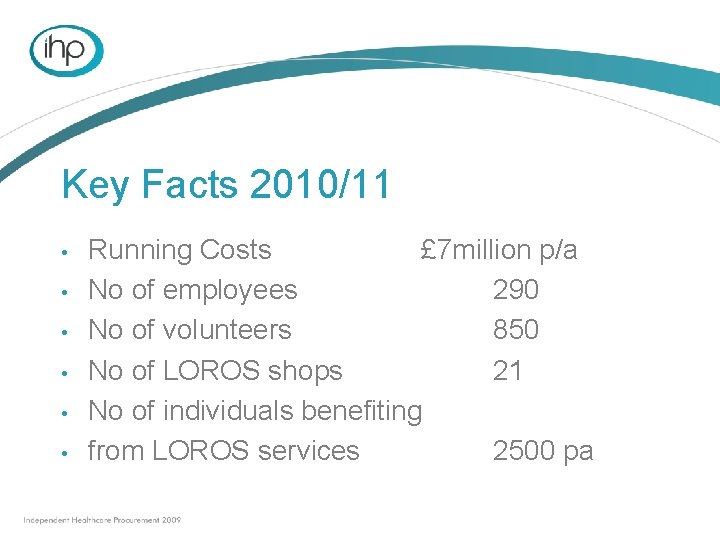
Key Facts 2010/11 • • • Running Costs £ 7 million p/a No of employees 290 No of volunteers 850 No of LOROS shops 21 No of individuals benefiting from LOROS services 2500 pa

Why did LOROS join? • • To save money = more money for patient and family needs To work with similar independent health care providers to benefit from joint purchasing

What did we do? • • • Stationery – Office depot Energy – 20 Charity shops Linen – Hospice Catering Kitchen Equipment
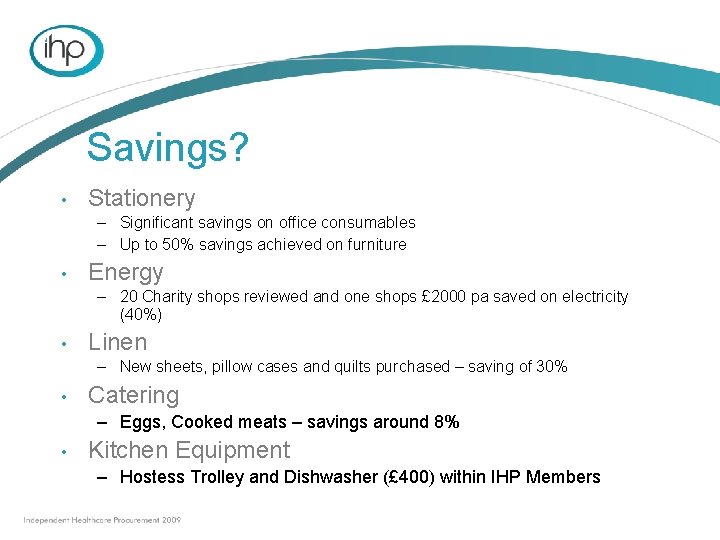
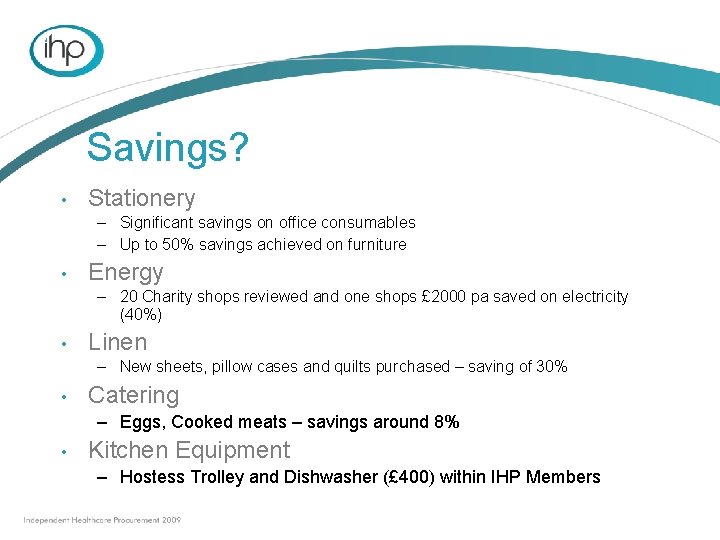
Savings? • Stationery – Significant savings on office consumables – Up to 50% savings achieved on furniture • Energy – 20 Charity shops reviewed and one shops £ 2000 pa saved on electricity (40%) • Linen – New sheets, pillow cases and quilts purchased – saving of 30% • Catering – Eggs, Cooked meats – savings around 8% • Kitchen Equipment – Hostess Trolley and Dishwasher (£ 400) within IHP Members
Improving the quality of dementia services: Jackie Crowther, Researcher, Academic Palliative and Supportive Care Studies Group (APSCSG).
Dementia: what care do patients and carers need in the last year of life? Jackie Crowther Ph. D Student Professor Mari Lloyd-Williams Academic Palliative and Supportive Care Studies Group (APSCSG) University of Liverpool Academic Palliative and Supportive Care Studies Group
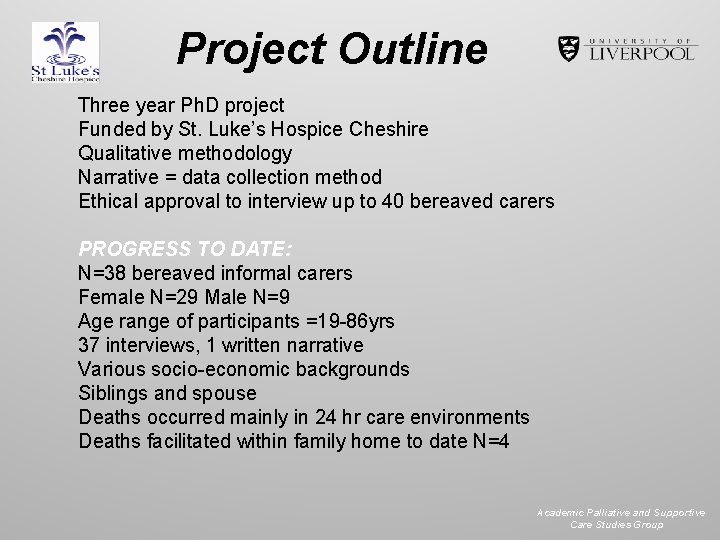
Project Outline Three year Ph. D project Funded by St. Luke’s Hospice Cheshire Qualitative methodology Narrative = data collection method Ethical approval to interview up to 40 bereaved carers PROGRESS TO DATE: N=38 bereaved informal carers Female N=29 Male N=9 Age range of participants =19 -86 yrs 37 interviews, 1 written narrative Various socio-economic backgrounds Siblings and spouse Deaths occurred mainly in 24 hr care environments Deaths facilitated within family home to date N=4 Academic Palliative and Supportive Care Studies Group
Aims and Objectives ØCommunicate with carers of people with dementia ØInclusion not exclusion ØCarers = experts ØNeed to provide care people “want” and not care we think we think they “need” ØSupport development and implementation of guidelines/ directives ØOngoing and continued research needed to facilitate this
Preliminary Analysis ØDied in hospital environments N= 21 Ø Died in care homes N=13 Ø Died at home N=4 ØInterview recordings re-visited on several occasions ØTranscripts read and re-read on several occasions ØInitial coding: 15 -30 per transcript ØSearched for similarities across all Academic Palliative and Supportive Care Studies Group

Commonalities/tentative categories • Knowledge • Intuition • +ve and –ve care • Information • Spirituality • Faith • Death talk • Moving on • Coping strategies • Kindness • Guilt • Carers as experts • Practicalities • Control • Trust • Anger • Deceit • “Being” with • Communication • Cultural issues • Language issues • Abandonment • Occupation/stimulation • Trauma • Release/relief • Life history • 1 st and 2 nd death • Religion • Carer stress/burden • Physical health (both) • Finances Academic palliative and Supportive Care Studies Group
Potential Themes Emerging ØCommunication: ability for everyone to listen (more importantly to “hear” what is said). Vital to know life history of person e. g. loss of a child, war veteran, personal habits and preferences ØSupport for families: at transitions of care e. g. decision to place relative in care home or admit to hospital, burden of guilt, lies and deceit Academic Palliative and Supportive Care Studies Group
ØKindness and humanity: appears to outweigh knowledge, examples of excellent care across all settings but also examples of very poor care even within family home, issues with co-ordination of care increasing stress on families, kindness of strangers Ø“Being with”: support to “be with” the pwd at difficult times, emphasis is on “doing”, when the “doing” is “done” nobody is with the pwd, results in stress for families, isolation for pwd, carers find this difficult but can be supported with finding a way to connect Academic Palliative and Supportive Care Studies Group
ØKnowledge of carers: informal carers believe they have intimate and best knowledge of pwd, however this can be dismissed by formal carers ØKnowledge of disease process: knowing when to treat, when to admit to hospital appropriately, when to withdraw, lack of continuity and consistency across settings, uncertainty contributing to stress for carers ØLanguage/cultural issues: differing languages and cultural backgrounds of formal carers impacting upon care and informal carers Academic palliative and Supportive Care Studies Group

THANK YOU ! Jackie Crowther crowther@liverpool. ac. uk Tel: 01517948047 Academic Palliative and Supportive Care Studies Group
A joined up approach to dealing with dementia palliative care: Morejoy Saineti, Dementia Palliative Voice Nurse, Housing 21.
Morejoy Saineti Dementia Voice Nurse

Dementia Voice Nurse Palliative care for people with Dementia; • • Employed By: Housing 21 Funded By: Kings Fund and Friends Period: Two years Borough: London, Westminster
The drivers of the post End of life Care strategy Dementia Care Strategy Carers like Barbra Pointon
Why Palliative care? A home for life? Preferred place of death?
The difference between dementia and any other condition during end of life stage • Capacity to make decision • Communication problems • Behavioural problem versus pain reaction or distress versus pain • Other people making decisions for you • Co-occurring conditions • Coordination of services • Effective advocacy services • Accessible care plans and regular caring services
What Dementia Palliative care does • Affirms life and regards dying as a normal process • Neither hastens nor postpones death • Relief from pain and other distressing symptoms • Integrates psychological and spiritual aspects of care • Coordinates services • Multi professional support • Support system for the family

DVN First year engagements • Planning • Networking • Raising awareness • Communication • Partnership working
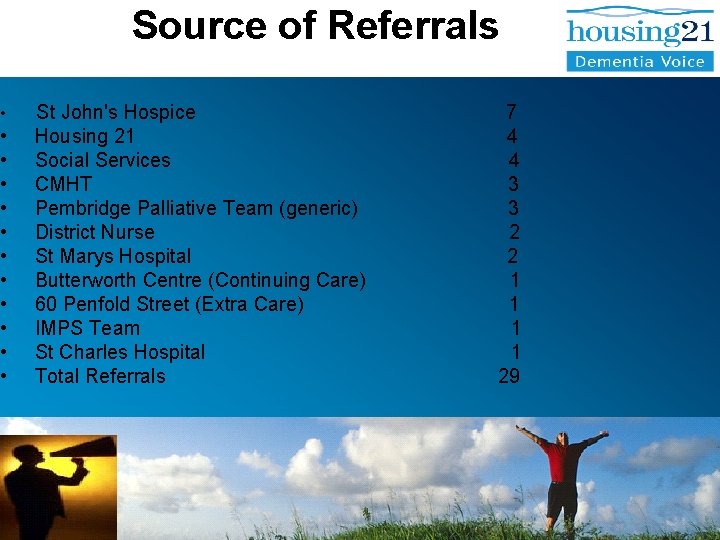
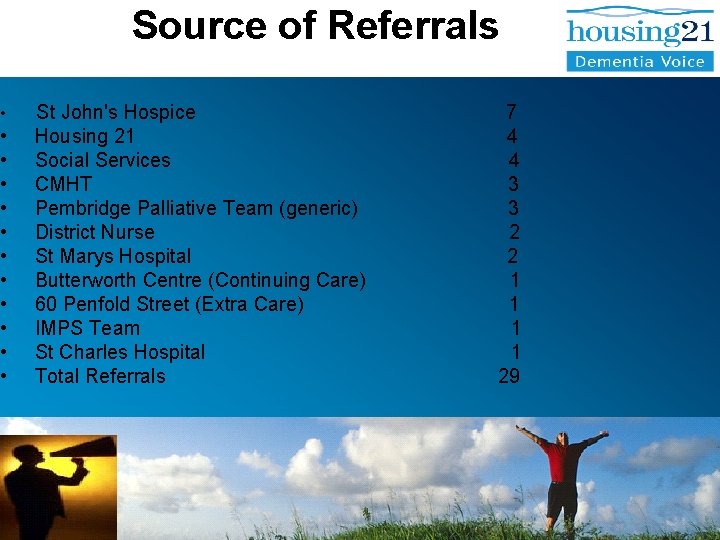
Source of Referrals • St John's Hospice 7 • Housing 21 4 • Social Services 4 • CMHT 3 • Pembridge Palliative Team (generic) 3 • District Nurse 2 • St Marys Hospital 2 • Butterworth Centre (Continuing Care) 1 • 60 Penfold Street (Extra Care) 1 • IMPS Team 1 • St Charles Hospital 1 • Total Referrals 29

What Joint up working does • Reduces waiting time • non bureaucratic referral system • Standardises care plans and practice • Continuity of care • Holistic care • Fast and friendly • Sharing information and expertise • Seamlessness
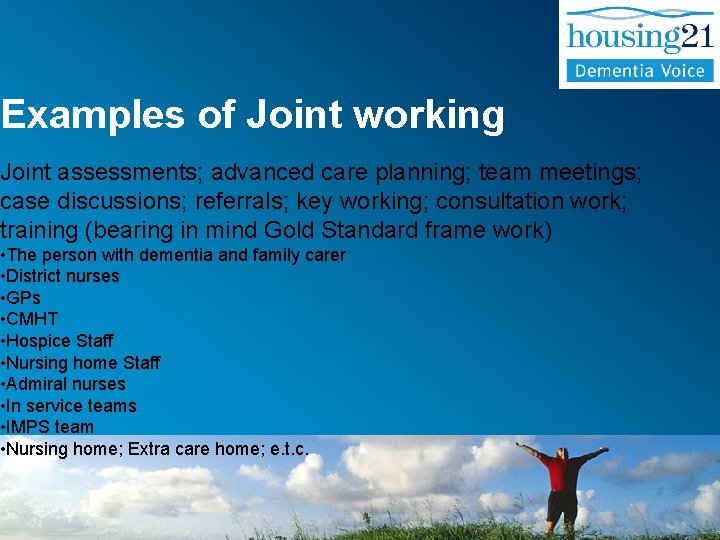
Examples of Joint working Joint assessments; advanced care planning; team meetings; case discussions; referrals; key working; consultation work; training (bearing in mind Gold Standard frame work) • The person with dementia and family carer • District nurses • GPs • CMHT • Hospice Staff • Nursing home Staff • Admiral nurses • In service teams • IMPS team • Nursing home; Extra care home; e. t. c.
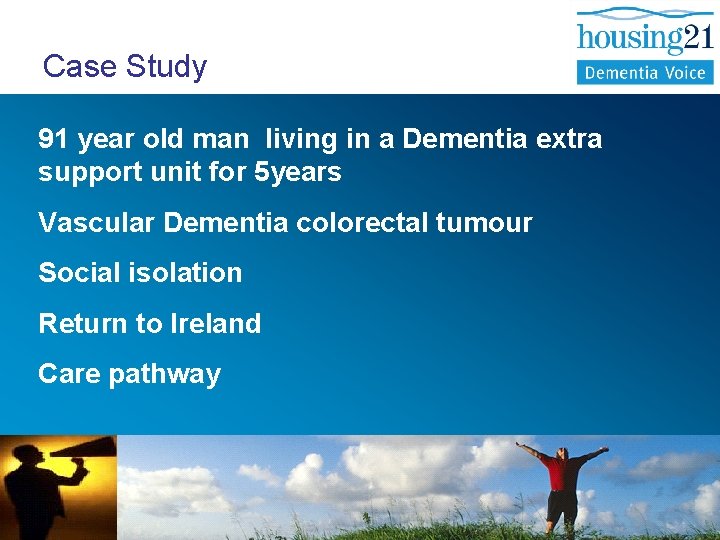
Case Study 91 year old man living in a Dementia extra support unit for 5 years Vascular Dementia colorectal tumour Social isolation Return to Ireland Care pathway
People Involved • IMCA (independent mental capacity act advocate • Extra care housing staff • Community nurses • DVN, Mc. Millan nurses • Care manager • In services care teams
Continuing Care Action Plan Palliation A continuing care package Community Mc. Millan Nurses/ Hospice @ Home Continence assessment. Rapid response Community Nursing Service Top up transfusions Brisker bleeds Infections Carers’ awareness / training
Outcome Discharged from hospital back to the Extra support care home Unachievable wishes of visiting Ireland due to advanced illness Died peacefully at home with support from professionals.
DVN Service Success: • improving quality of life, and quality of dying • improving availability of support, services and equipments • support to Housing 21 and staff from other organizations, • improving staffs’ skills.
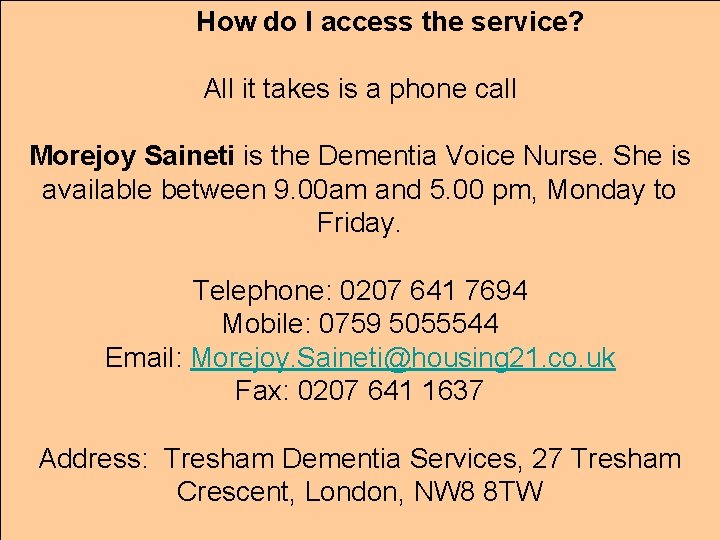
How do I access the service? All it takes is a phone call Morejoy Saineti is the Dementia Voice Nurse. She is available between 9. 00 am and 5. 00 pm, Monday to Friday. Telephone: 0207 641 7694 Mobile: 0759 5055544 Email: Morejoy. Saineti@housing 21. co. uk Fax: 0207 641 1637 Address: Tresham Dementia Services, 27 Tresham Crescent, London, NW 8 8 TW
Questions?