IGA DEFICIENCY BY BRITTNI MCCLELLAN IGA DEFICIENCY DESCRIPTION

IGA DEFICIENCY BY: BRITTNI MCCLELLAN
IGA DEFICIENCY - DESCRIPTION Description: Serum Ig. A <5 mg/d. L Normal serum Ig. G and Ig. M Patients >1 year Genetics: Autosomal Dominant Abnormalities on Chromosome 18 Associated with HLA-A 1, HLA-A 2, B 8, and Dw 3
IGA DEFICIENCY - PATHOPHYSIOLOGY Increased incidence of the following: Atopy Sinopulmonary infections GI infections (especially Giardia lamblia) Crohn disease Ulcerative colitis Celiac disease Autoimmune illnesses: Arthritis Lupus Immune Endocrinopathies Autoimmune Hematologic Conditions Chronic Active Hepatitis
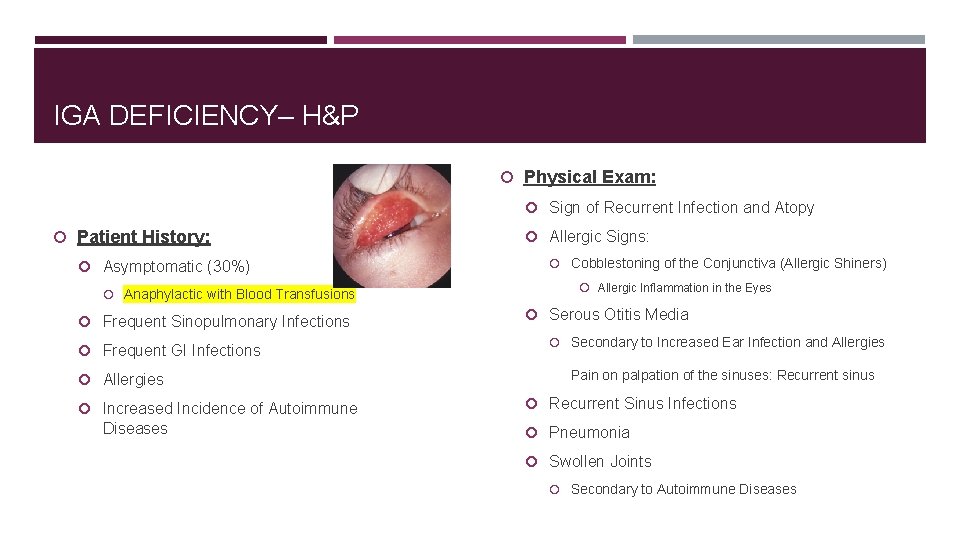
IGA DEFICIENCY– H&P Physical Exam: Sign of Recurrent Infection and Atopy Patient History: Asymptomatic (30%) Anaphylactic with Blood Transfusions Frequent Sinopulmonary Infections Frequent GI Infections Allergies Increased Incidence of Autoimmune Diseases Allergic Signs: Cobblestoning of the Conjunctiva (Allergic Shiners) Allergic Inflammation in the Eyes Serous Otitis Media Secondary to Increased Ear Infection and Allergies Pain on palpation of the sinuses: Recurrent sinus Recurrent Sinus Infections Pneumonia Swollen Joints Secondary to Autoimmune Diseases

IGA DEFICIENCY - DIAGNOSIS Diagnosis: Normal CBC Measure Serum Ig. A Level: Deficiency: Serum Ig. A level is <5 mg/d. L. Total Immunoglobulins: Normal: Rules Out X-Linked Agammaglobulinemia, Common Variable Immunodeficiency, and Severe Combined Immunodeficiency Lymphocyte Mitogens: Normal: Rules Out Common Variable Immunodeficiency, Severe Combined Immunodeficiency, Ataxia Telangiectasia, Di. George Syndrome, and Nezelof Syndrome

IGA DEFICIENCY– TREATMENT Medication There is no specific drug therapy. Recurrent infections should be treated aggressively with broad-spectrum antibiotics. Antibiotic prophylaxis to prevent recurrent sinopulmonary infections is often indicated. Patients with Ig. A deficiency may develop antibodies against Ig. A in transfused blood products. These patients are at risk for anaphylactic transfusion reactions. To avoid these reactions, these patients may receive: Packed RBCs (only if these cells have been washed 3 times) Plasma Products from Ig. A-Deficient Donors Autologous Banked Blood
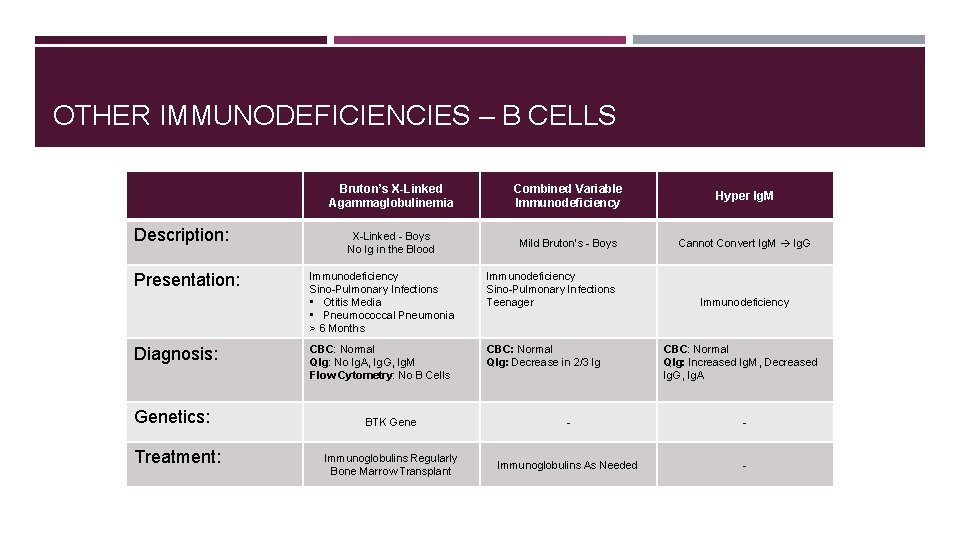
OTHER IMMUNODEFICIENCIES – B CELLS Description: Presentation: Diagnosis: Genetics: Treatment: Bruton’s X-Linked Agammaglobulinemia Combined Variable Immunodeficiency Hyper Ig. M X-Linked - Boys No Ig in the Blood Mild Bruton’s - Boys Cannot Convert Ig. M Ig. G Immunodeficiency Sino-Pulmonary Infections • Otitis Media • Pneumococcal Pneumonia > 6 Months Immunodeficiency Sino-Pulmonary Infections Teenager CBC: Normal QIg: No Ig. A, Ig. G, Ig. M Flow Cytometry: No B Cells CBC: Normal QIg: Decrease in 2/3 Ig Immunodeficiency CBC: Normal QIg: Increased Ig. M, Decreased Ig. G, Ig. A BTK Gene - - Immunoglobulins Regularly Bone Marrow Transplant Immunoglobulins As Needed -
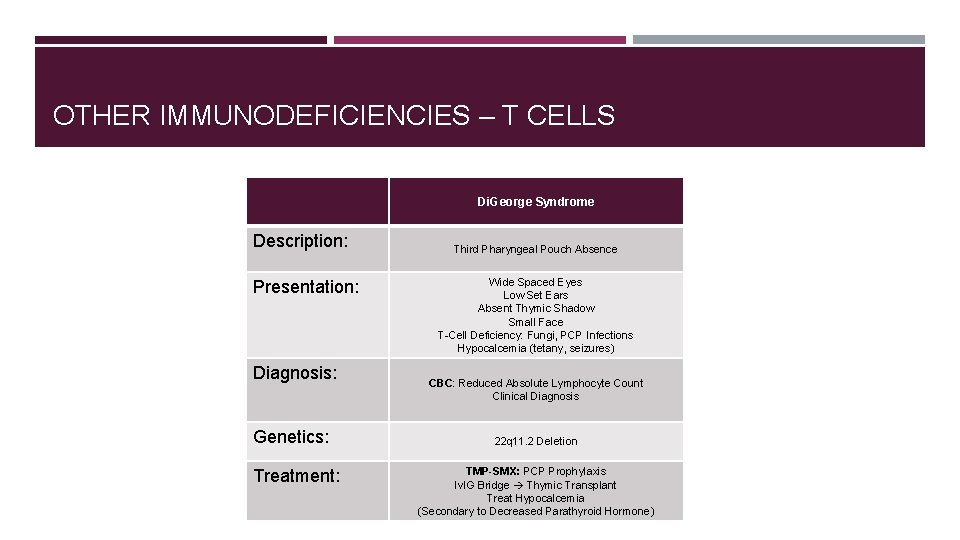
OTHER IMMUNODEFICIENCIES – T CELLS Di. George Syndrome Description: Presentation: Diagnosis: Genetics: Treatment: Third Pharyngeal Pouch Absence Wide Spaced Eyes Low Set Ears Absent Thymic Shadow Small Face T-Cell Deficiency: Fungi, PCP Infections Hypocalcemia (tetany, seizures) CBC: Reduced Absolute Lymphocyte Count Clinical Diagnosis 22 q 11. 2 Deletion TMP-SMX: PCP Prophylaxis Iv. IG Bridge Thymic Transplant Treat Hypocalcemia (Secondary to Decreased Parathyroid Hormone)
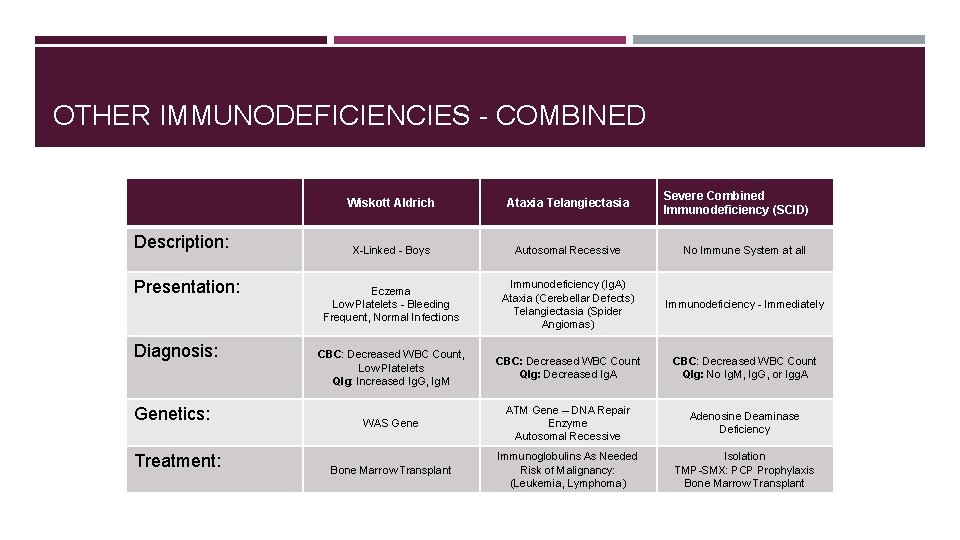
OTHER IMMUNODEFICIENCIES - COMBINED Description: Presentation: Diagnosis: Genetics: Treatment: Severe Combined Immunodeficiency (SCID) Wiskott Aldrich Ataxia Telangiectasia X-Linked - Boys Autosomal Recessive No Immune System at all Eczema Low Platelets - Bleeding Frequent, Normal Infections Immunodeficiency (Ig. A) Ataxia (Cerebellar Defects) Telangiectasia (Spider Angiomas) Immunodeficiency - Immediately CBC: Decreased WBC Count, Low Platelets QIg: Increased Ig. G, Ig. M CBC: Decreased WBC Count QIg: Decreased Ig. A CBC: Decreased WBC Count QIg: No Ig. M, Ig. G, or Igg. A WAS Gene ATM Gene – DNA Repair Enzyme Autosomal Recessive Adenosine Deaminase Deficiency Bone Marrow Transplant Immunoglobulins As Needed Risk of Malignancy: (Leukemia, Lymphoma) Isolation TMP-SMX: PCP Prophylaxis Bone Marrow Transplant

OTHER IMMUNODEFICIENCIES – PHAGOCYTES Description: Presentation: Diagnosis: Genetics: Treatment: Chronic Granulomatous Disease Leukocyte Adhesion Deficiency Chediak Higashi Macrophage Problem Can Eat Bacteria, but Cannot Kill Catalase + Organisms No Respiratory Burst WBCs cannot leave bloodstream and attack infection. Microtubule Dysfunction Failure of Phagolysosome Formation Defective Melanization High Fever High WBC Count No Pus Delayed Separate of the Cord Immunodeficiency - Neutropenia Albinism Neuropathy Nitro. Blue CBC: Increased WBC Count QIg: All Elevated CBC: Increased WBC Count Flow Cytometry: Absence of CD 18 on Leukocytes Peripheral Smear: Giant Granules in Neutrophils Eosinophilic-Peroxidase + NADPH Oxidase Deficiency X-Linked Recessive LFA-1 Integrin (CD 11 a/CD 18) LYST Gene Autosomal Recessive Bone Marrow Transplant Recurrent Staph Infections
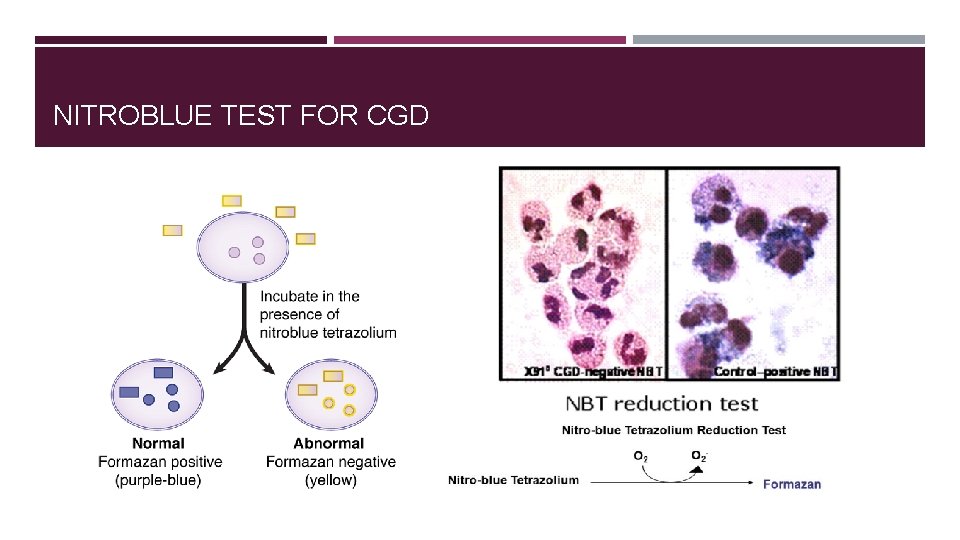
NITROBLUE TEST FOR CGD
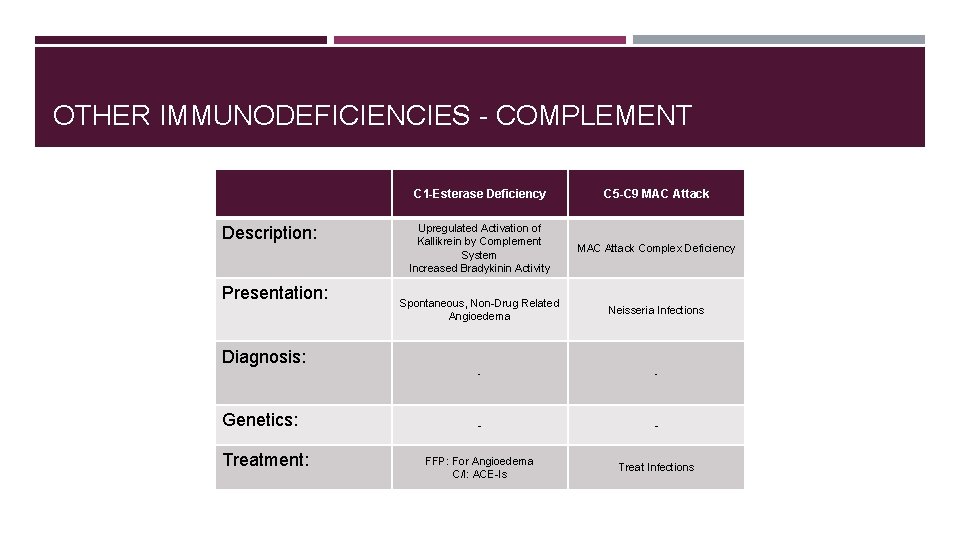
OTHER IMMUNODEFICIENCIES - COMPLEMENT Description: Presentation: C 1 -Esterase Deficiency C 5 -C 9 MAC Attack Upregulated Activation of Kallikrein by Complement System Increased Bradykinin Activity MAC Attack Complex Deficiency Spontaneous, Non-Drug Related Angioedema Neisseria Infections - - FFP: For Angioedema C/I: ACE-Is Treat Infections Diagnosis: Genetics: Treatment:
QUESTION 1 Two anxious parents bring their 5 -month-old male baby to your clinic for evaluation. They report that he has had "continuous" sinus a) No treatment needed; patient's infections for the past several months, has been condition will resolve spontaneously hospitalized twice for lobar pneumonia, and has b) Hematopoetic cell transplantation chronic diarrhea. Although the patient's vital signs are within normal limits, he is at the 5 th c) Intravenous piperacillin-tazobactam percentile for age in both height and weight. d) Immune globulin administration Your physical exam reveals oral thrush, tenderness upon maxillary sinus palpation, and e) Highly active antiretroviral therapy absent cervical lymph nodes and tonsils. Which of the following interventions is curative for this patient's condition? a) Hematopoetic cell transplantation

QUESTION 1 a) A 15 -month-old girl who has had repeated otitis media, pneumonia, and progressive clumsiness since beginning to walk in the past three months b) A 10 -month-old boy who has had recurrent viral infections as well as hypocalcemia during neonatal period Which of the following patient presentations seen in a pediatric immunology clinic is most consistent with a diagnosis of Bruton's agammaglobulinemia? d) A 9 -month-old boy who has had recurrent otitis media and pneumococcal pneumonia in the past three months c) A 4 -year-old girl who has had repeated oral candidasis in the past nine months d) A 9 -month-old boy who has had recurrent otitis media and pneumococcal pneumonia in the past three months e) A 7 -month-old boy who has had recurrent pneumococcal pneumonia, eczema, and easy bruising in the past four months
QUESTION 1 An 18 -year-old male presents to the emergency room after a stab wound. His wound is repaired surgically and he is resuscitated appropriately. Two days later, he is transferred to the floor where he receives a transfusion. He has no prior history of transfusions. Minutes after beginning the transfusion, the patient complains of shortness of breath. Vital signs are temperature 37 degrees Celsius, heart rate 110, blood pressure 90/60, respiratory rate 20, and oxygen saturation of 99% on room air. Physical examination reveals bilateral wheezes. The transfusion is stopped, epinephrine and intravenous fluids are administered, and his vital signs stabilize. You glance at his chart and see that he has a history of recurrent pneumonias and seasonal allergies. If a congenital disorder has increased this patient’s risk of an anaphylactic transfusion reaction, one would expect serum studies to reveal: a) Decreased Ig. A b) Increased Ig. M, decreased Ig. G, Ig. A, and Ig. E c) Increased Ig. E d) Increased Ig. E and Ig. A, and decreased Ig. M e) Decreased IFN-gamma a) Decreased Ig. A
QUESTION 1 A 3 -year-old boy is brought to the family physician by his parents. They are concerned that he has had multiple nosebleeds in the last 6 months and is always sick compared to other children. During this time period they have also noticed the formation of multiple bruises on his extremities and dry-itching skin on his hands, feet and elbow. On physical exam the physician notes moderate splenomegaly. What is the most likely diagnosis in this child? a) X-linked Agammaglobulinemia b) Severe Combined Immunodefiency c) Wiskott-Aldrich Syndrome d) Primary Eczema e) Hyperimmunoglobulin E syndrome c) Wiskott Aldrich
- Slides: 16