Identifying the Deteriorating Patient Sara Blakeley Portsmouth Hospitals
Identifying the Deteriorating Patient Sara Blakeley Portsmouth Hospitals University NHS Trust sara. blakeley@porthosp. nhs. uk
Identifying, responding (& proving) What do we mean by a deteriorating patient? What can we do to improve response and recognition? Data collection and analysis
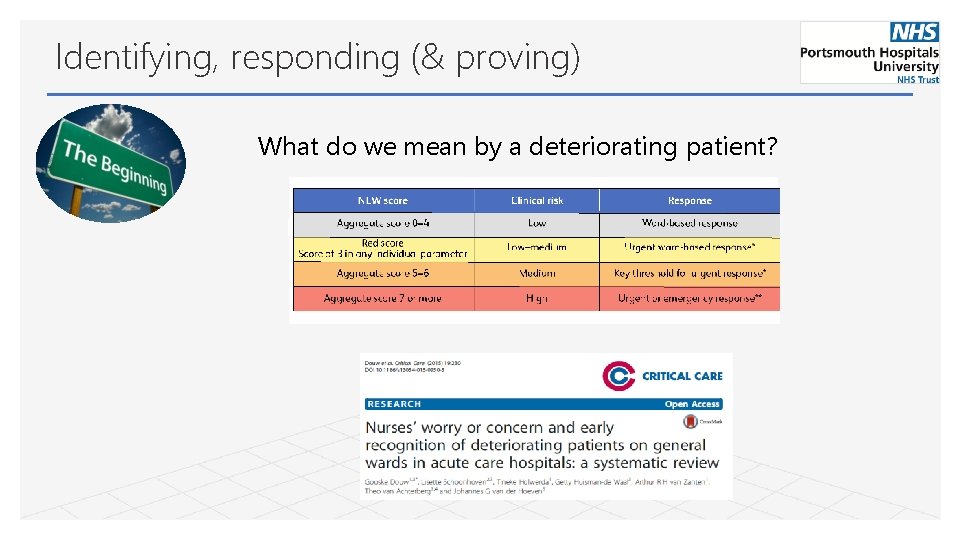
Identifying, responding (& proving) What do we mean by a deteriorating patient?
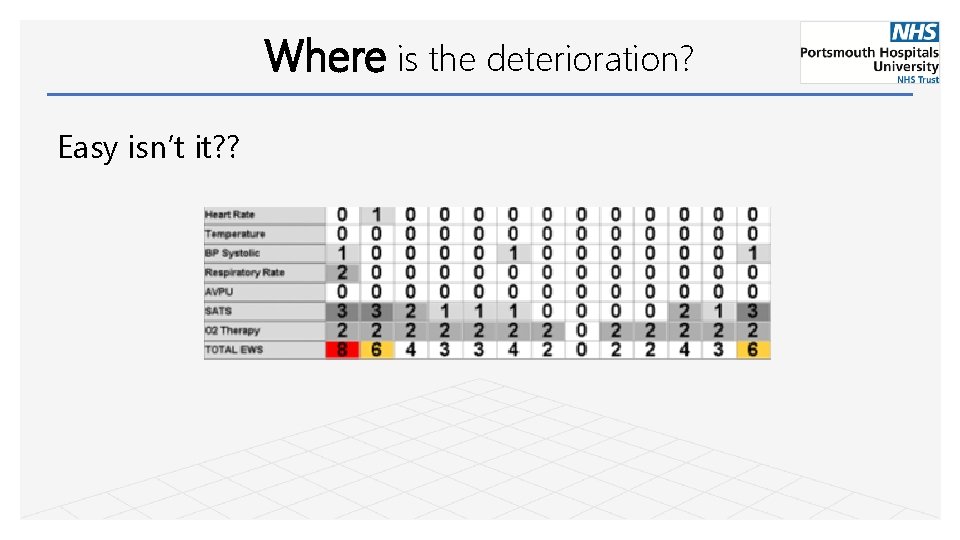
Where is the deterioration? Easy isn’t it? ?

Where is the deterioration?
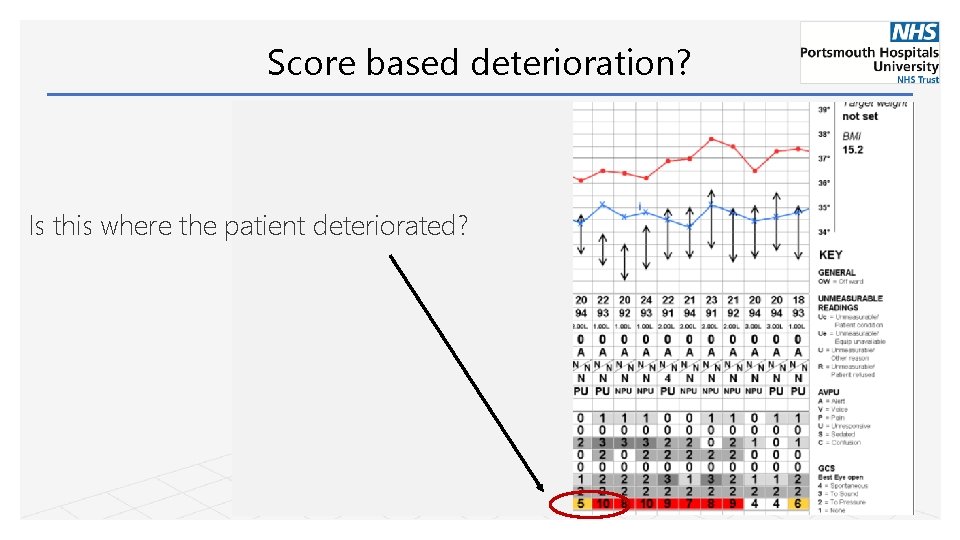
Score based deterioration? Is this where the patient deteriorated?
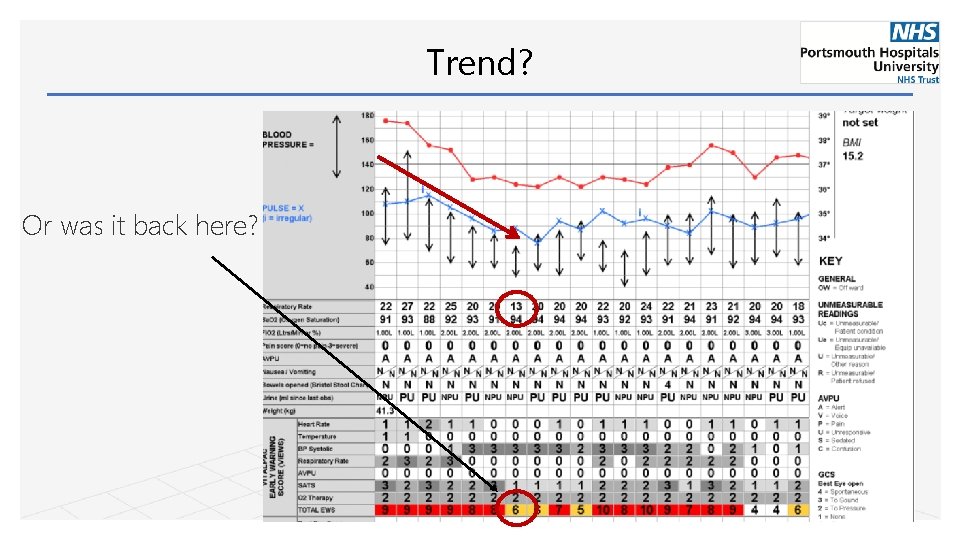
Trend? Or was it back here?
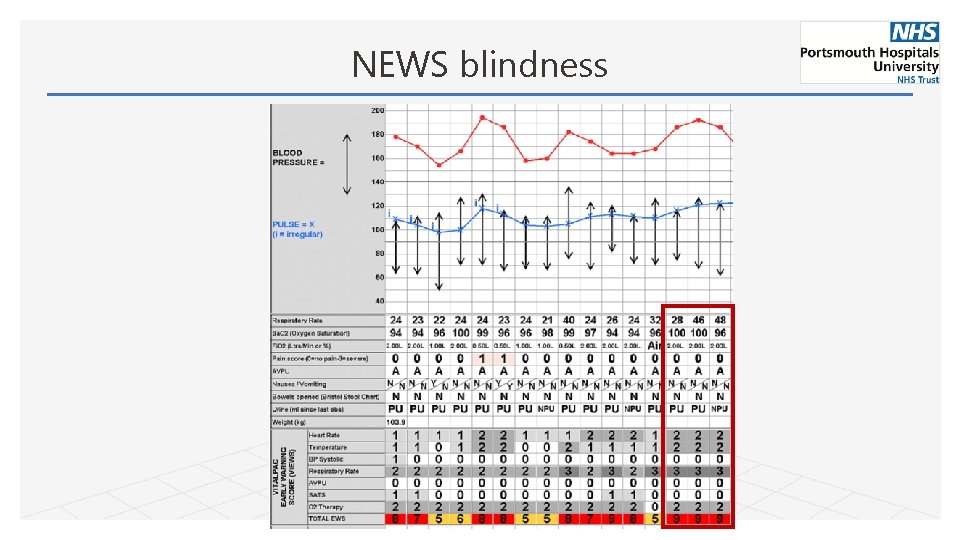
NEWS blindness
Identifying, responding (& proving) What do we mean by a deteriorating patient? What can we do to improve response and recognition? Data collection and analysis
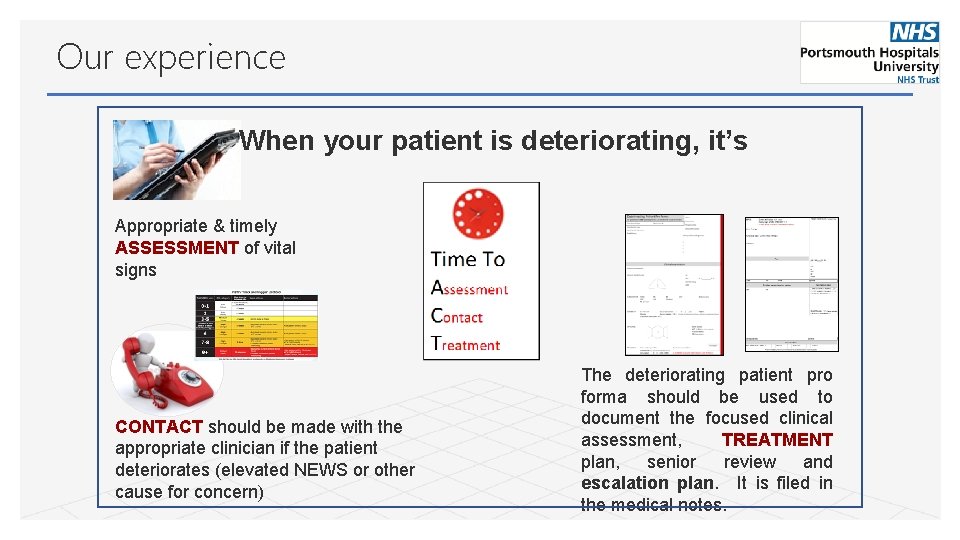
Our experience When your patient is deteriorating, it’s Appropriate & timely ASSESSMENT of vital signs CONTACT should be made with the appropriate clinician if the patient deteriorates (elevated NEWS or other cause for concern) The deteriorating patient pro forma should be used to document the focused clinical assessment, TREATMENT plan, senior review and escalation plan. It is filed in the medical notes.
“I could have done with this at 2 am when I was starting to flag” Junior Doctor “Why don’t we have this in obstetrics? ” Registrar “This is a very good way of escalating deteriorating patients as it can be very difficult at times” Staff nurse
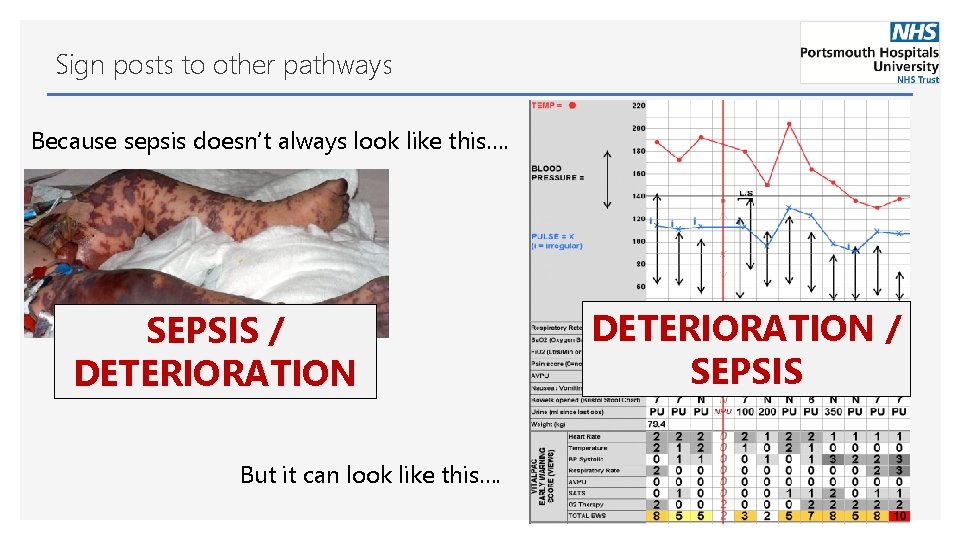
Sign posts to other pathways Because sepsis doesn’t always look like this…. SEPSIS / DETERIORATION But it can look like this…. DETERIORATION / SEPSIS
Identifying, responding (& proving) What do we mean by a deteriorating patient? What can we do to improve response and recognition? Data collection and analysis

Data capture - considerations Definition of a deteriorating patient • • • NEWS 2: What level? Delta NEWS? What about cause for concern? What about high scoring baseline? How can you capture data? • • • What data can you collect? • • Identification? Escalation by nursing staff? Clinical response? Is response appropriate? Electronic vs paper? Real time vs retrospective? Clinician vs ‘data collector’? Outcome and balancing data? • • Cardiac arrest rate? Mortality? Unplanned ICU admission? Outreach referrals?

How did/do we capture data How we capture data Our definition of a deteriorating patient • • New NEWS 5 and above OR cause for concern by the nursing staff Initiation of the deteriorating patient pro forma Data we collect • • • Appropriate frequency of vital signs monitoring Number of patients escalated by staff Clinical review by appropriate clinician in appropriate time frame (local policy) Actions following clinical review Night vs day, by ward area and by score Grading of response • • • Vital. PAC sweep identifying all NEWS 5 + Real time review of notes (+ feedback) Data collection by a clinician Emergency (ward) admissions to ICU 45 -50 deteriorations monthly March 19 Feb 20 (quarterly since) Outcome and balancing data • • Bed occupancy & nursing shifts covered Cardiac arrest calls • • • Sepsis mortality Emergency ICU admission rate Number of outreach referrals
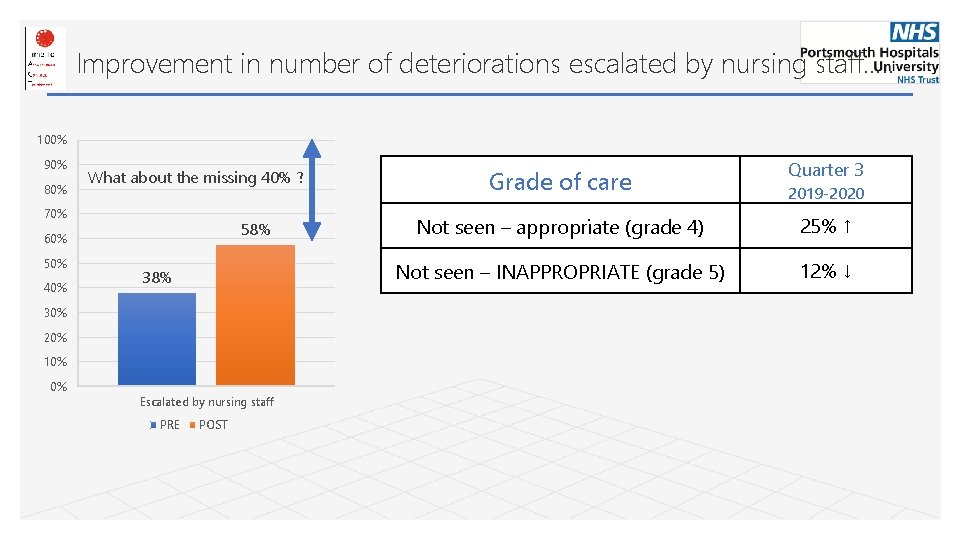
Improvement in number of deteriorations escalated by nursing staff…. . 100% 90% 80% What about the missing 40% ? 70% 58% 60% 50% 40% 38% 30% 20% 10% 0% Escalated by nursing staff PRE POST Grade of care Quarter 3 Not seen – appropriate (grade 4) 25% ↑ Not seen – INAPPROPRIATE (grade 5) 12% ↓ 2019 -2020
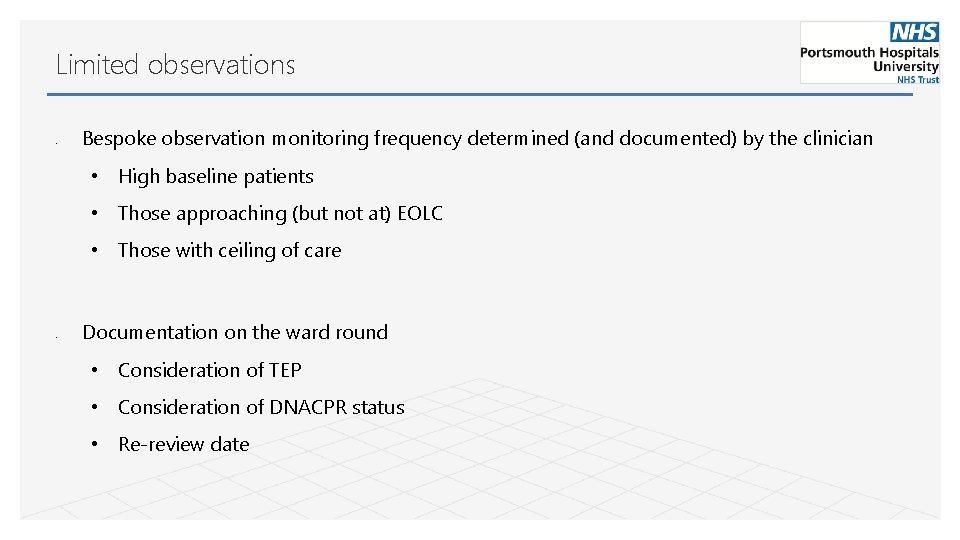
Limited observations • Bespoke observation monitoring frequency determined (and documented) by the clinician • High baseline patients • Those approaching (but not at) EOLC • Those with ceiling of care • Documentation on the ward round • Consideration of TEP • Consideration of DNACPR status • Re-review date
Identifying, responding (& proving) What do we mean by a deteriorating patient? What can we do to improve response and recognition? Data collection and analysis
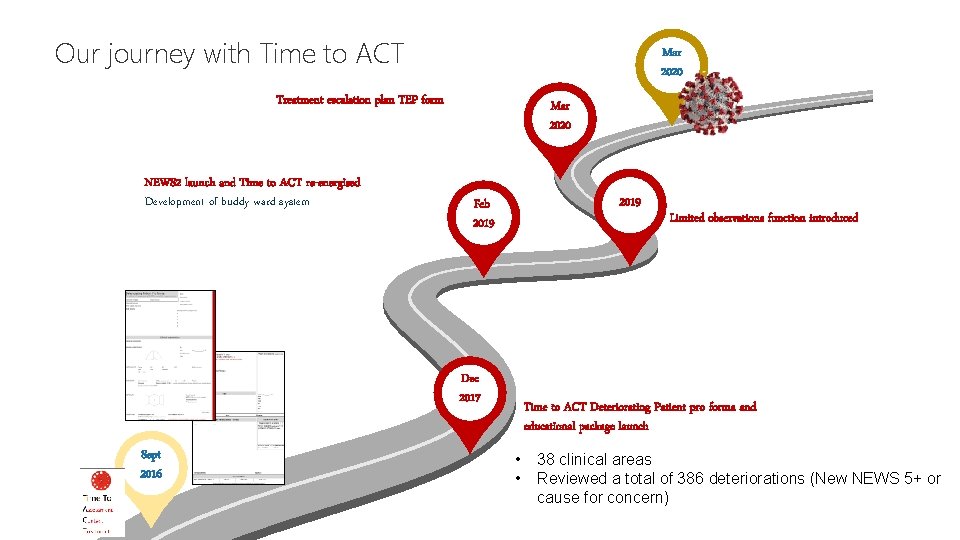
Our journey with Time to ACT Mar 2020 Treatment escalation plan TEP form NEWS 2 launch and Time to ACT re-energised Development of buddy ward system Mar 2020 2019 Feb 2019 Dec 2017 Sept 2016 Limited observations function introduced Time to ACT Deteriorating Patient pro forma and educational package launch • • 38 clinical areas Reviewed a total of 386 deteriorations (New NEWS 5+ or cause for concern)
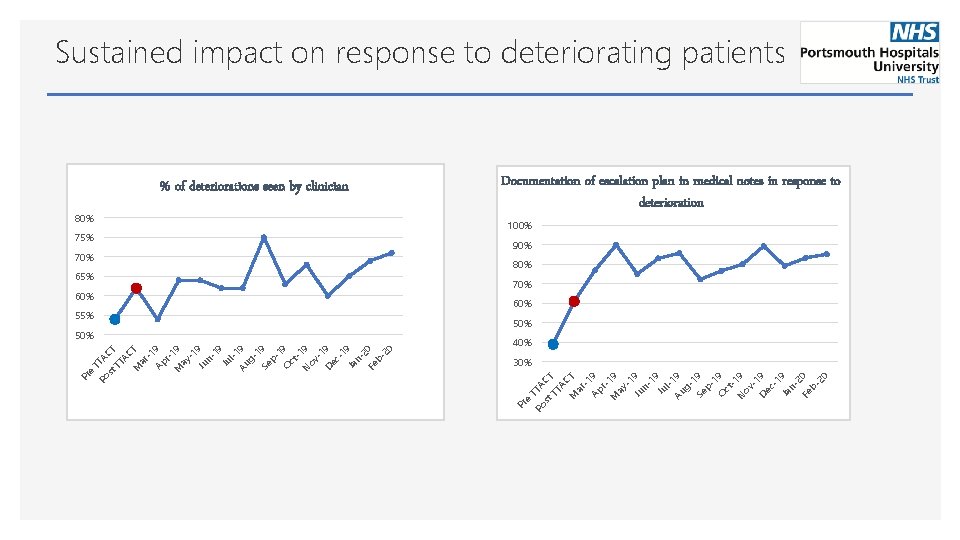
Sustained impact on response to deteriorating patients % of deteriorations seen by clinician 80% 100% 75% 90% 70% 80% 65% 70% 60% 55% 50% e Po TTA st CT TT AC M T ar -1 Ap 9 r. M 19 ay -1 Ju 9 n 19 Ju l. Au 19 g 1 Se 9 p 1 O 9 ct N 19 ov -1 De 9 c 1 Ja 9 n 2 Fe 0 b 20 30% Pr st e TT AC TT T AC M T ar -1 Ap 9 r 1 M 9 ay -1 Ju 9 n 19 Ju l-1 Au 9 g 1 Se 9 p 1 O 9 ct -1 N 9 ov -1 De 9 c 1 Ja 9 n 2 Fe 0 b 20 40% Po Pr Documentation of escalation plan in medical notes in response to deterioration
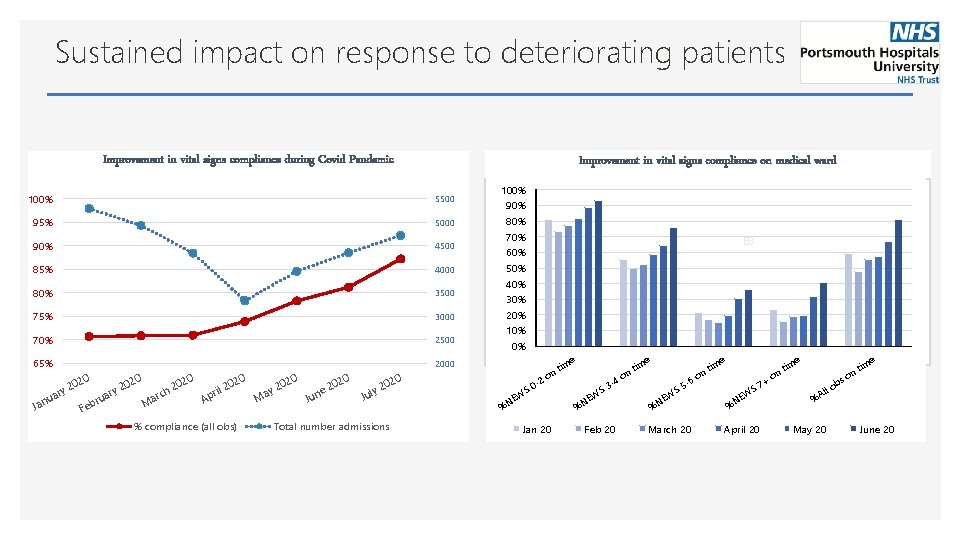
Sustained impact on response to deteriorating patients Improvement in vital signs compliance during Covid Pandemic Improvement in vital signs compliance on medical ward 100% 5500 95% 5000 90% 4500 85% 4000 80% 3500 75% 3000 70% 2500 65% 2000 u Jan 0 02 2 ary ru Feb 0 02 2 ary Ma 0 0 02 02 2 rch l 2 pri A % compliance (all obs) M 0 02 2 ay 0 02 e 2 Jun Total number admissions E 8 e im 0 02 2 uly J 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% %N -2 S 0 EW t on Jan 20 S 3 EW %N -4 Feb 20 tim on e im -6 S 5 EW %N March 20 t on e e S 7 EW %N April 20 + tim on im ll %A May 20 s ob t on e June 20
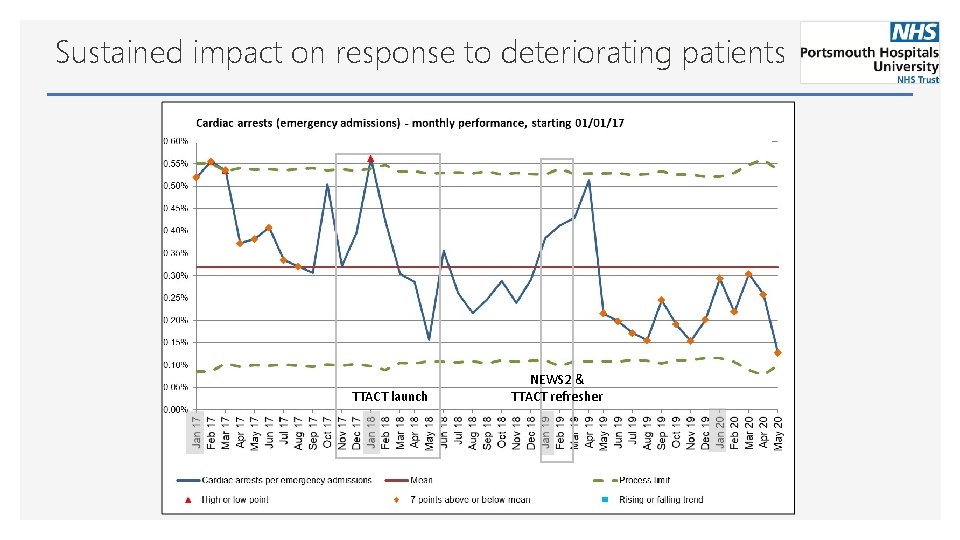
Sustained impact on response to deteriorating patients 01 TTACT launch NEWS 2 & TTACT refresher
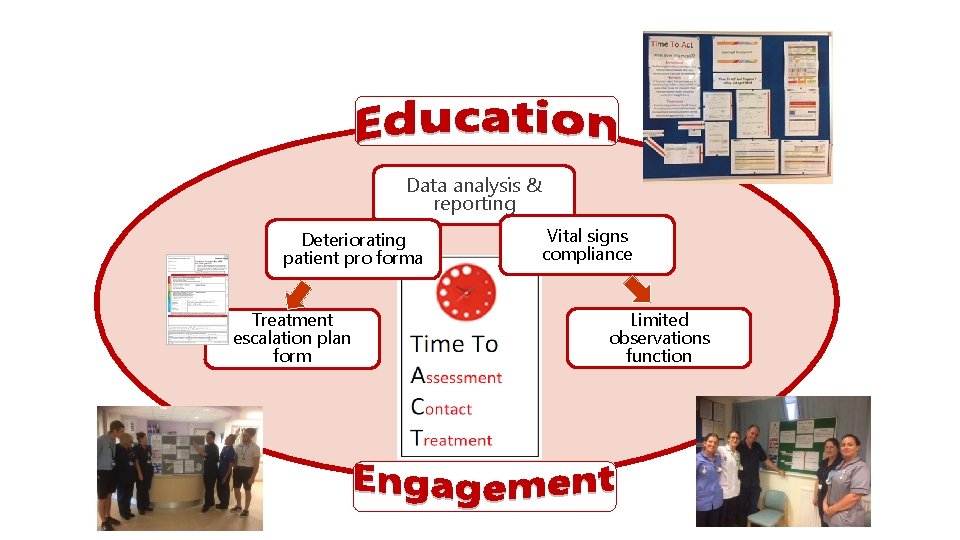
Data analysis & reporting Deteriorating patient pro forma Treatment escalation plan form Vital signs compliance Limited observations function
Conclusion • Decide what deterioration looks like in your setting • Educate on the reason for the number, not just the number • Give staff tools to escalate on NEWS and also cause for concern • Look at who you are not responding to (and why) • Data should be collected to help you shape your service • Collect data for yourself, not just because you have to • Human AND automated data collection

Questions?
- Slides: 26