Identifying Fall Risk Strategies to Prevent Falls Teri


- Slides: 37

Identifying Fall Risk: Strategies to Prevent Falls Teri Hecht, RPh Board Certified Geriatric Pharmacist February 22, 2018
Learning Objectives • Identify potential fall risk factors • Determine high risk medication that may contribute to falls • Implement key fall interventions • When to refer to pharmacist for review • Use national fall prevention programs to assist with patient/family education 2
What is the leading cause of fatal and nonfatal injury among adults 65 years of age and older? A. Motor vehicle accidents B. Suffocation C. Falls D. Fires/burns
Huge impact on quality of life Among people who fall, less than half talk to their healthcare provider about it.
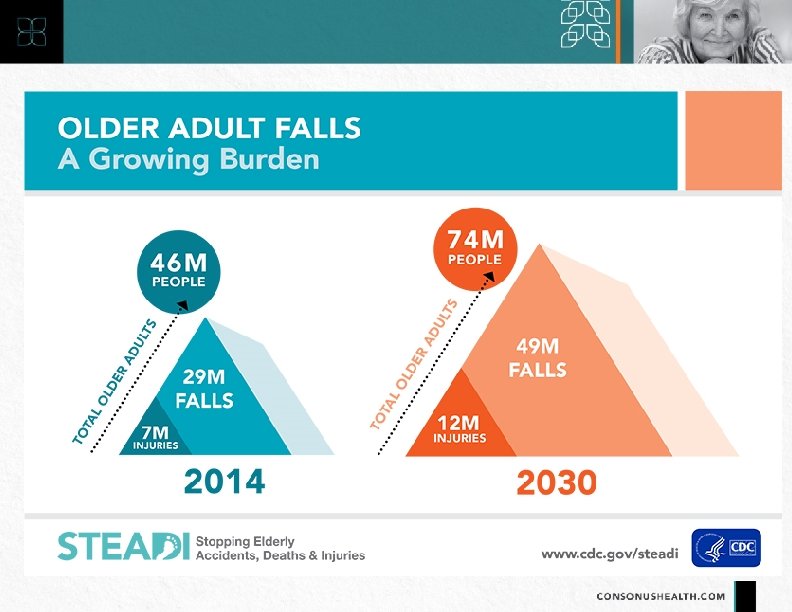
Resources for Fall Prevention • https: //www. cdc. gov/steadi/materials. html
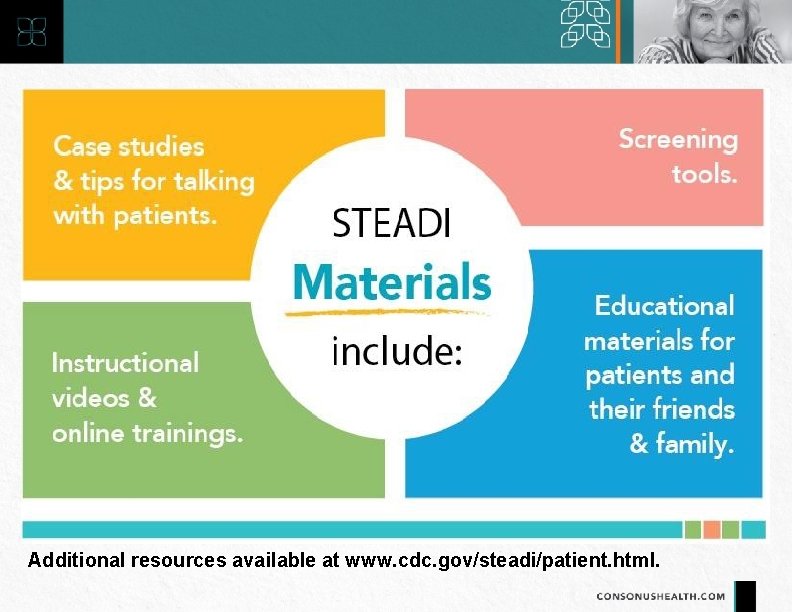
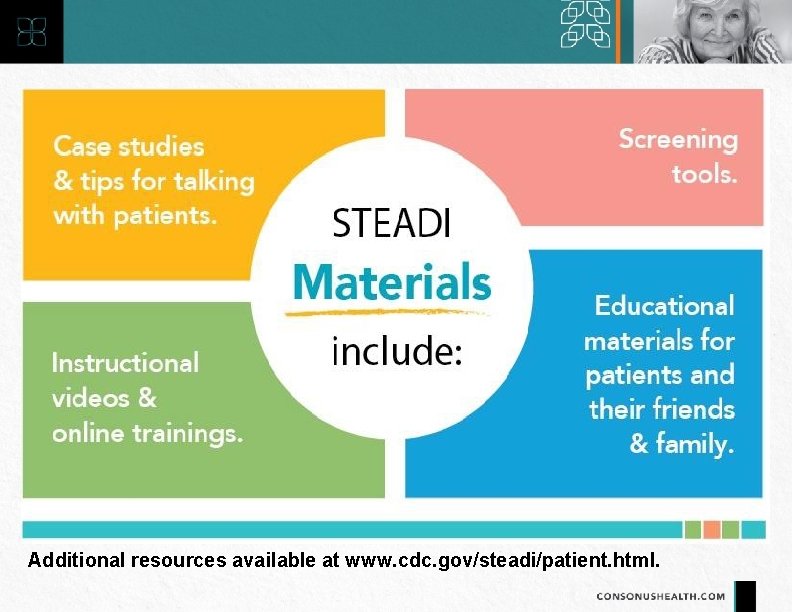
Additional resources available at www. cdc. gov/steadi/patient. html.
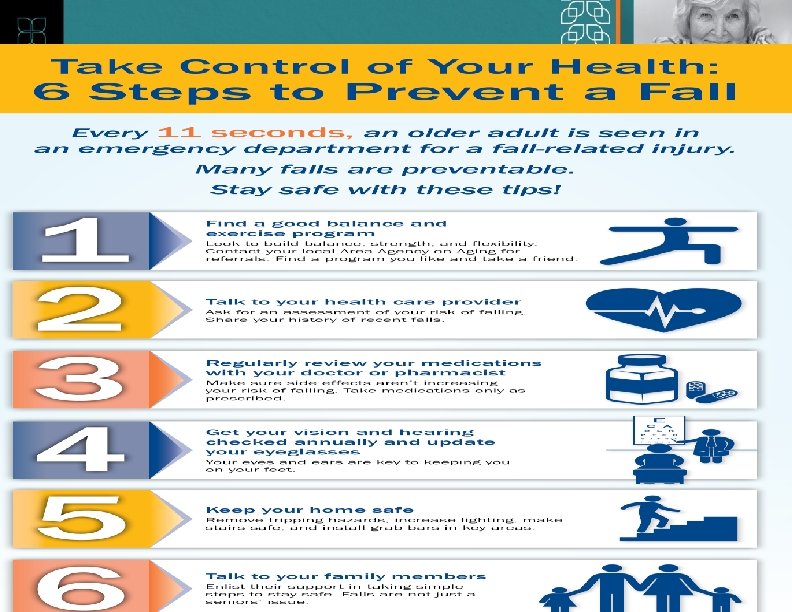
ncoa. org/healthy-aging/falls-prevention/fallsprevention-awareness-day/generalresources/infographics-handouts/
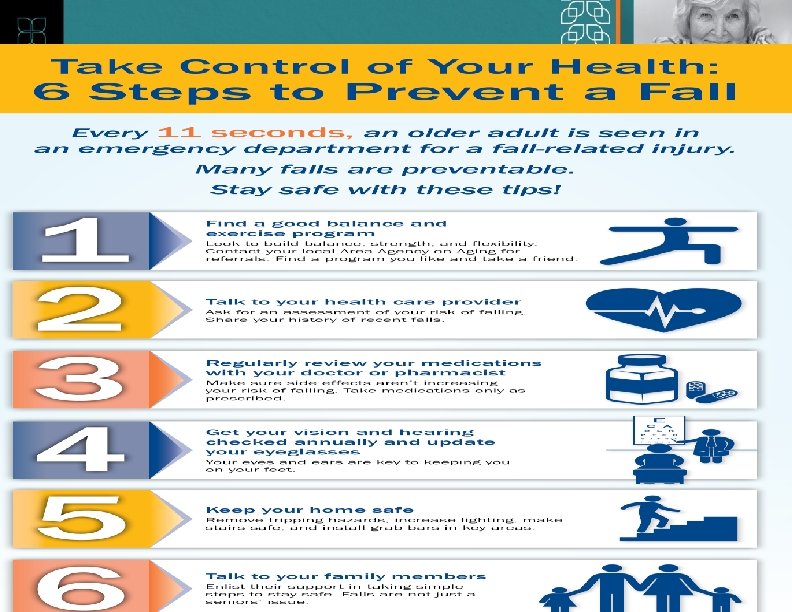
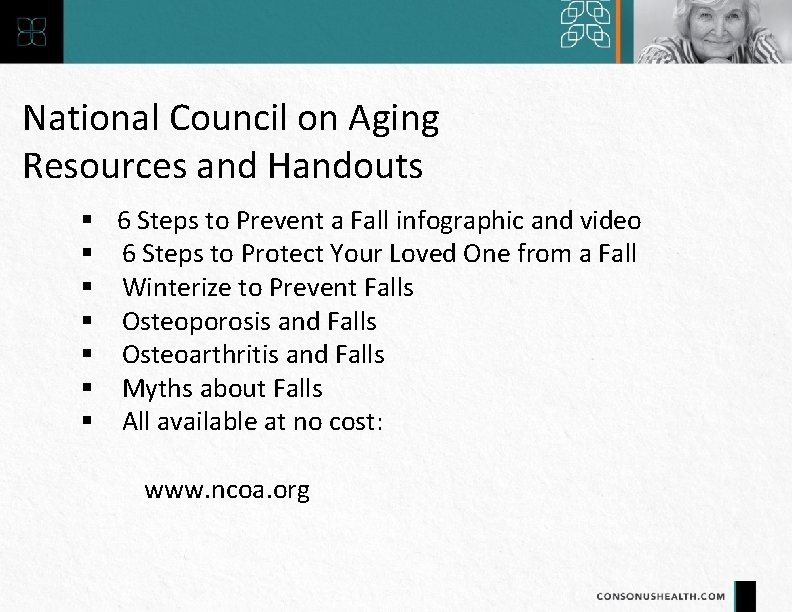
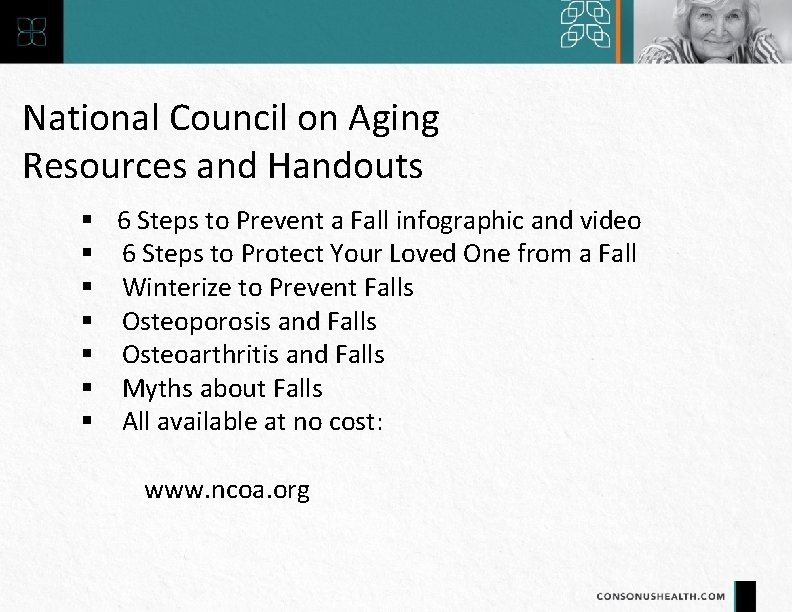
National Council on Aging Resources and Handouts 6 Steps to Prevent a Fall infographic and video 6 Steps to Protect Your Loved One from a Fall Winterize to Prevent Falls Osteoporosis and Falls Osteoarthritis and Falls Myths about Falls All available at no cost: www. ncoa. org
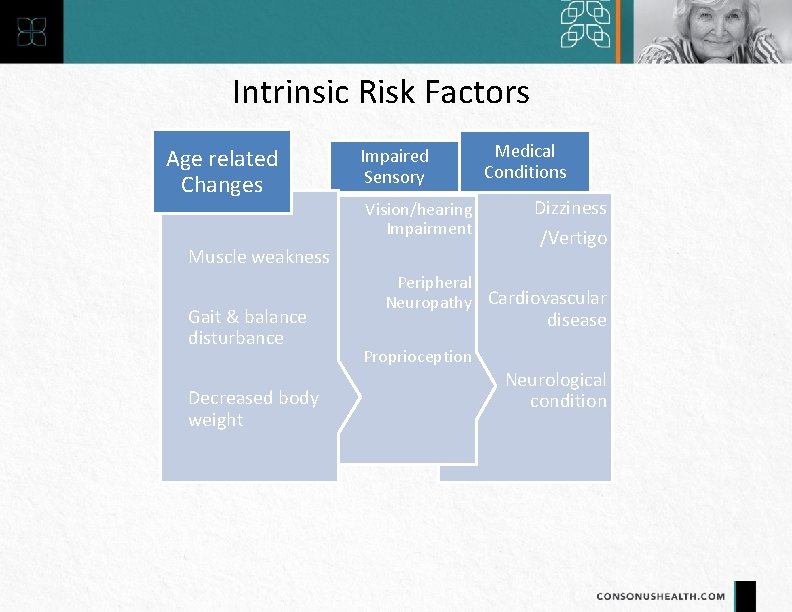
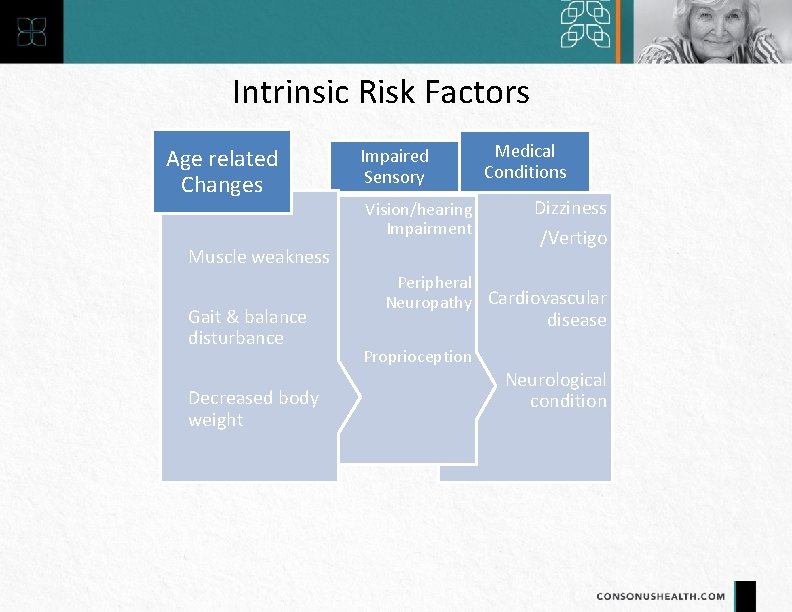
Intrinsic Risk Factors Age related Changes Impaired Sensory Vision/hearing Impairment Muscle weakness Gait & balance disturbance Decreased body weight Medical Conditions Dizziness /Vertigo Peripheral Neuropathy Cardiovascular disease Proprioception Neurological condition
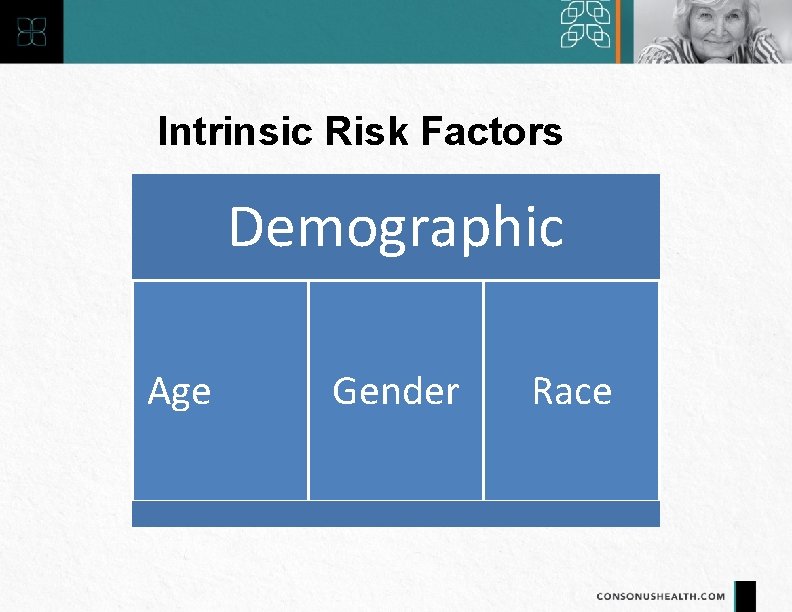
Intrinsic Risk Factors Demographic Age Gender Race
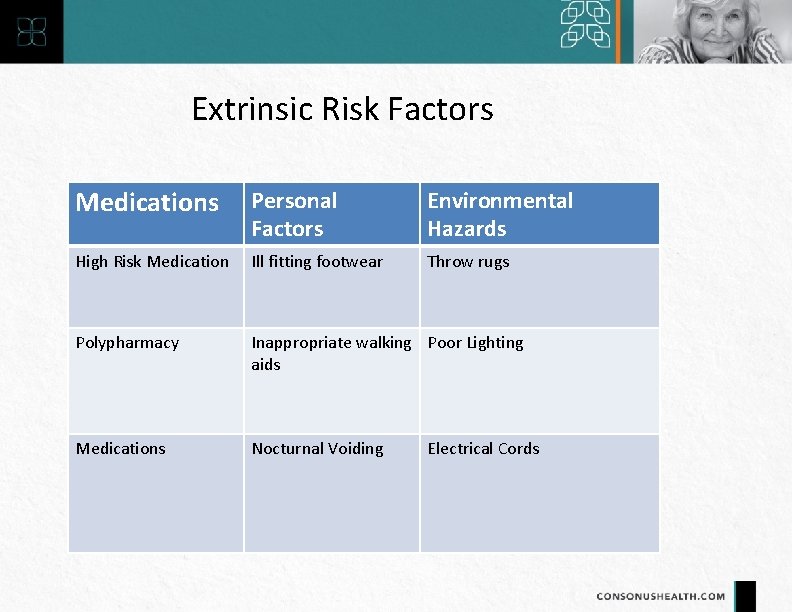
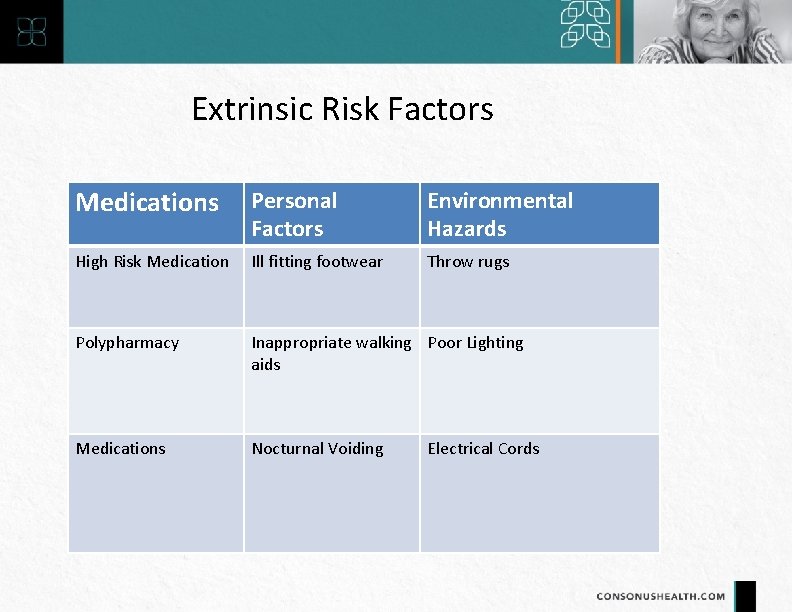
Extrinsic Risk Factors Medications Personal Factors Environmental Hazards High Risk Medication Ill fitting footwear Throw rugs Polypharmacy Inappropriate walking Poor Lighting aids Medications Nocturnal Voiding Electrical Cords
Medication and Fall Risk • Psychotropics • Anti-diabetic • Opioid analgesics • Cardiovascular agents • Antiepileptics • Antidepressants
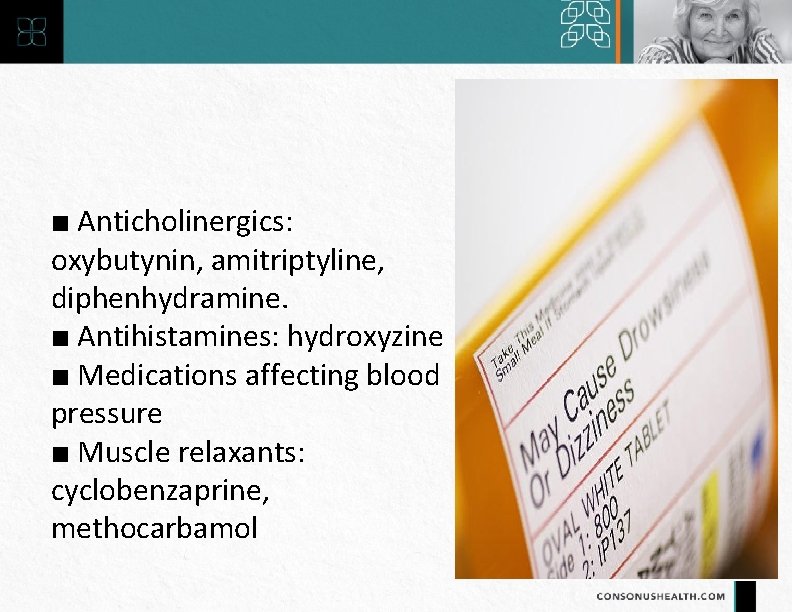
■ Anticholinergics: oxybutynin, amitriptyline, diphenhydramine. ■ Antihistamines: hydroxyzine ■ Medications affecting blood pressure ■ Muscle relaxants: cyclobenzaprine, methocarbamol
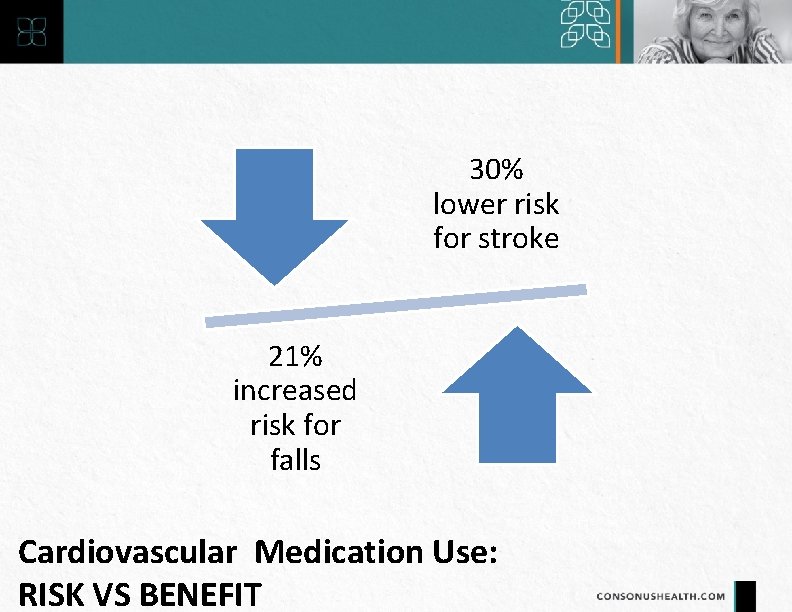
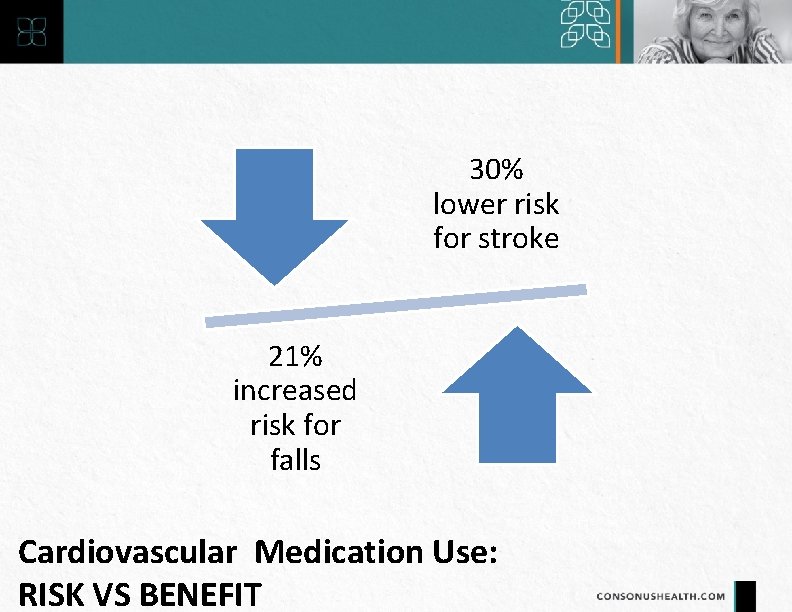
30% lower risk for stroke 21% increased risk for falls Cardiovascular Medication Use: RISK VS BENEFIT
Mrs. Doubtfire is 81 year old female
Case Study Her Son indicates she has had “too many falls to count. ” Mrs. Doubtfire agrees that she falls a lot, but she’s pessimistic. “Old people fall, that’s just how it is, ” she says. Mrs. Doubtfire is an outgoing 81 -year-old Caucasian woman She lives in an assisted living community. Her son reports that she was just seen in the hospital’s emergency room a week ago because she fell when she was getting out of the shower. Mrs. Doubtfire has a history of hypertension, hyperlipidemia, diabetes, CAD, and CHF.
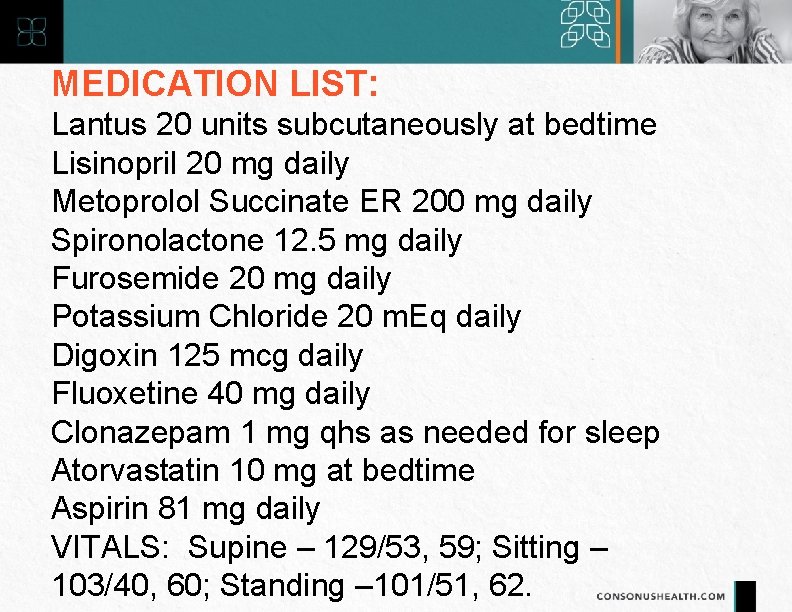
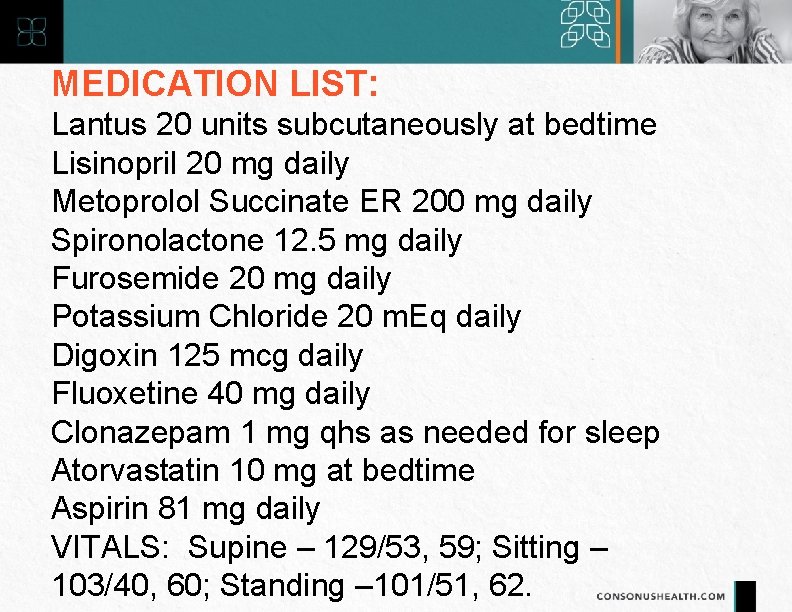
MEDICATION LIST: Lantus 20 units subcutaneously at bedtime Lisinopril 20 mg daily Metoprolol Succinate ER 200 mg daily Spironolactone 12. 5 mg daily Furosemide 20 mg daily Potassium Chloride 20 m. Eq daily Digoxin 125 mcg daily Fluoxetine 40 mg daily Clonazepam 1 mg qhs as needed for sleep Atorvastatin 10 mg at bedtime Aspirin 81 mg daily VITALS: Supine – 129/53, 59; Sitting – 103/40, 60; Standing – 101/51, 62.
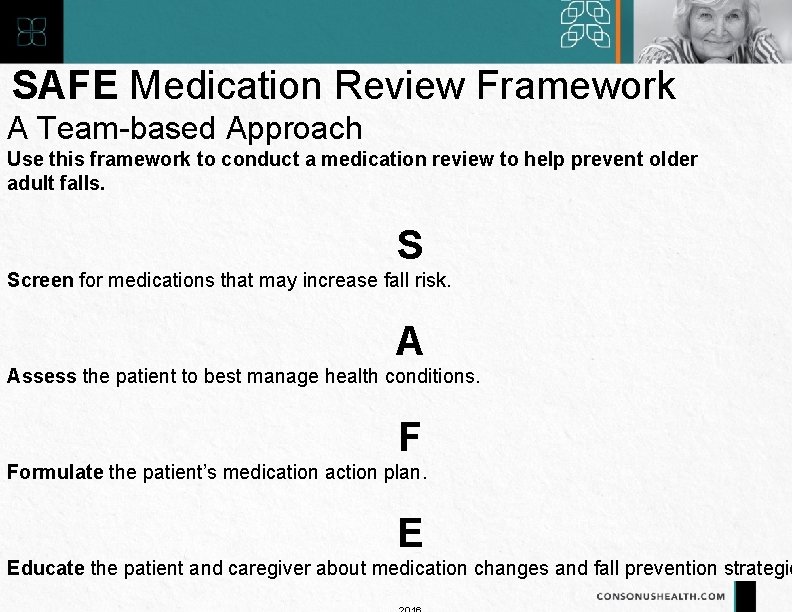
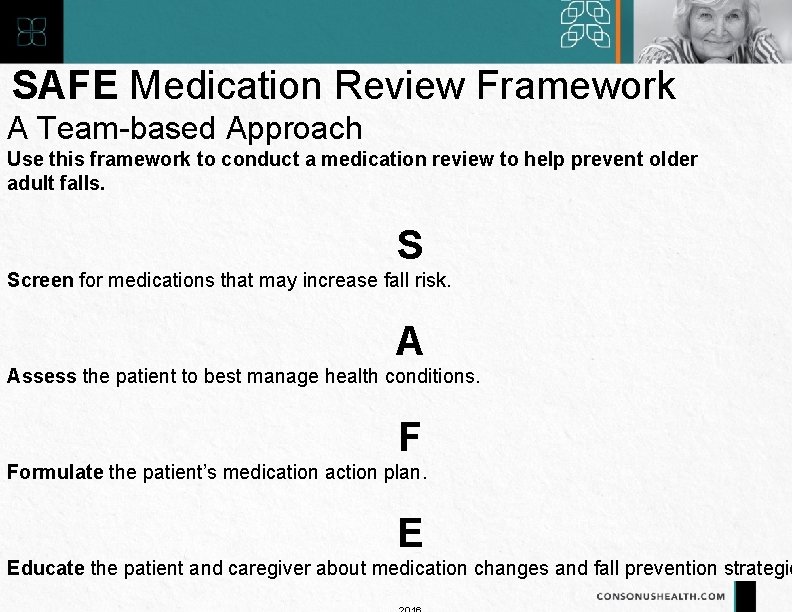
SAFE Medication Review Framework A Team-based Approach Use this framework to conduct a medication review to help prevent older adult falls. S Screen for medications that may increase fall risk. A Assess the patient to best manage health conditions. F Formulate the patient’s medication action plan. E Educate the patient and caregiver about medication changes and fall prevention strategie
Formulate the patient’s medication action plan. ■ Stop medications when possible

Formulate the patient’s medication action plan. ■ Switch to safer alternatives
Formulate the patient’s medication action plan.
Educate the patient and/or caregiver about medication changes and fall prevention strategies. Discuss the following: ■ Reasons for medication changes ■ Steps for implementing action plan ■ Other approaches to reduce fall risk ■ Importance of referrals to specialists such as PT/OT/vision check
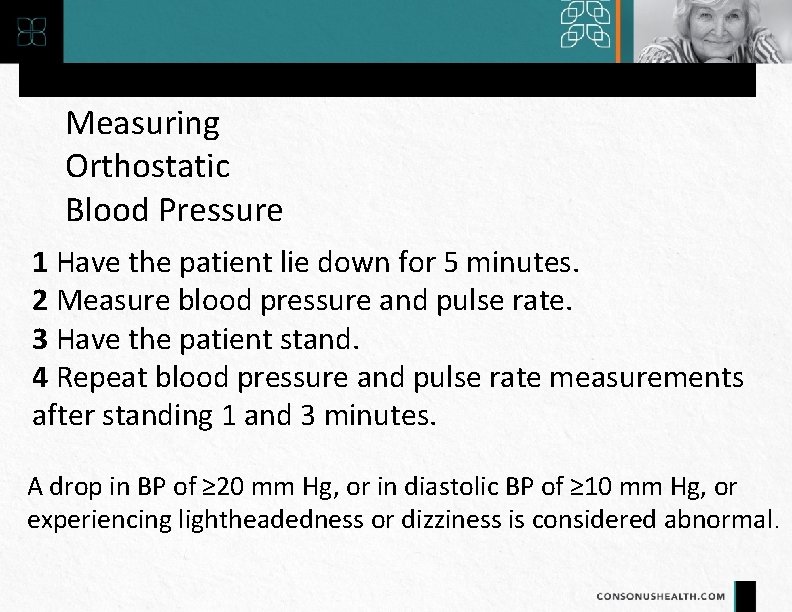
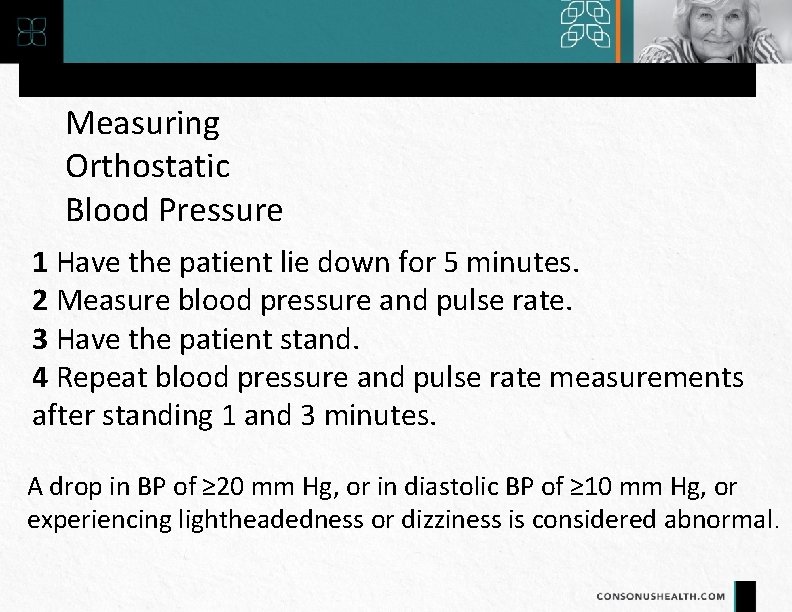
Measuring Orthostatic Blood Pressure 1 Have the patient lie down for 5 minutes. 2 Measure blood pressure and pulse rate. 3 Have the patient stand. 4 Repeat blood pressure and pulse rate measurements after standing 1 and 3 minutes. A drop in BP of ≥ 20 mm Hg, or in diastolic BP of ≥ 10 mm Hg, or experiencing lightheadedness or dizziness is considered abnormal.
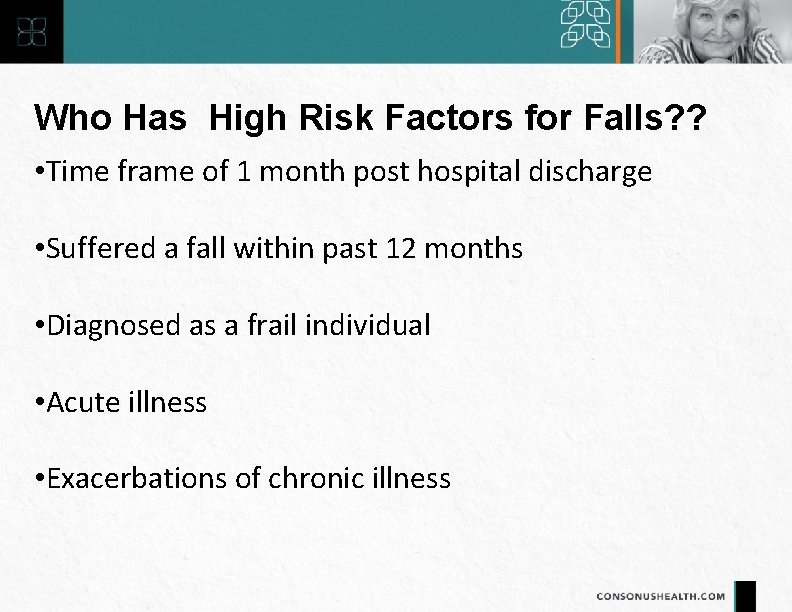
Who Has High Risk Factors for Falls? ? • Time frame of 1 month post hospital discharge • Suffered a fall within past 12 months • Diagnosed as a frail individual • Acute illness • Exacerbations of chronic illness
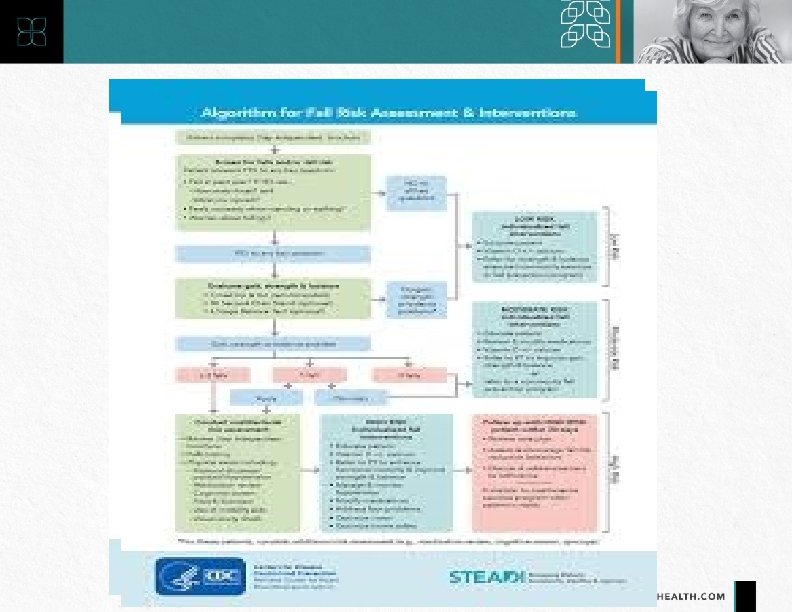
KEY STEPS FOR FALL PREVENTION Identify and address fall risk factors Refer as needed to specialists or community programs Follow up with patient in 30 days
KEY FALL INTERVENTIONS • • Add Vitamin D supplementation Modify medication Manage hypotension Address foot and vision problems Enhance strength and balance Educate patient and family Optimize safety
“Any new symptom in an older patient should be considered a drug side effect until proven otherwise”
Questions?
(425) 308 -0400 thecht@consonushealth. com 36
Sources • www. cdc. gov/steadi • ncoa. org/healthy-aging/falls-preventionawareness-day/general-resources/infographics-handouts/ • https: //www. medscape. com/viewarticle/841020 • https: //www. medscape. com/viewarticle/831517 • https: //www. youtube. com/watch? v=o 54 v_tu. Evpw