Identifying Early Warning Signs Medical Emergency Team Training




- Slides: 26

Identifying Early Warning Signs Medical Emergency Team Training
WHAT IS A MET TEAM? • Medical Emergency Team (MET) is a multidisciplinary team which purpose is to provide expert assessment, early intervention and stabilization of patients to prevent clinical deterioration or cardiopulmonary arrest. 2
WHY DO WE NEED AMET TEAM? According to the Institute for Healthcare Improvement • 48% of all hospital deaths were “unexpected” • All of the patients were admitted to non-ICU setting When a MET team is implemented • Non-ICU arrests reduced by 50% • Mortality rates reduced by 37 -50% 3
SIGNS OF PATIENT DETERIORATION • Studies show that 70% of patients show evidence of respiratory deterioration within 8 hours of arrest • 66% show abnormal vital signs within 6 hours of arrest and the MD was only notified 25% of the time Why does this happen? • Failure to adequately plan care – Assessments, goals, placement of the patient at the appropriate level of care • Failure to communicate – Patient to staff – Between healthcare providers • Failure to recognize patient deterioration 4
WHAT IS THE ROLE OF THE MET TEAM? The MET team is expected to: • Respond to the location as soon as possible and should be at the bedside within 5 minutes • • Perform a thorough assessment to determine patient status • Support and include the primary RN in all assessments and interventions performed so that he/she may increase his/her level of knowledge • • Stabilize or assist with transfer of the patient Assist with communication between nursing personnel and the MD using the SBAR format Document on the physician’s progress notes the reason and results for the consult, as well as in the nursing notes 5
MET TEAM RESPONSIBILITIES PER CHSB POLICY • Respond to the MET call location • Perform a thorough assessment • Consult with the assigned nurse throughout the patient care process • Call the attending physician and make recommendations using SBAR • Document on Physician Progress Notes and Nurses Notes utilizing SBAR the reason for the call and the result • RT will perform a thorough respiratory assessment 6
CRITERIA FOR CALLING THE MET AT CHSB • Respiratory distress, threatened airway, change in breathing pattern • Acute change in respiratory rate (less than 10 breaths/min or greater than 24 breaths/min) • Acute change in blood pressure (systolic BP less than 90 mm. Hg) • Acute change in heart rate (less than 50 beats/min or greater than 120 beats/min) 7
CRITERIA FOR CALLING THE MET AT CHSB – CONT’D • Decreased urine output (less than 50 ml in 4 hours - not on dialysis) • New, repeated, or prolonged seizures • Failure to respond to treatment • Staff “intuition” or concern 8
CRITERIA FOR CALLING PEDIATRIC MET RESPONSE • Altered level of consciousness • Respiratory distress • New onset of seizure OTHER PEDIATRIC CONSIDERATIONS • Children’s vital signs vary as the child matures • A single threshold for activation does not exist 9

COMPOSITION OF THE CHSB MET TEAM • ICCU Charge RN • Lead Respiratory Therapist • House Supervisor • ICCU Medical Director – Provide informational assistance – attendance not required ***Adult first responders include the ICU RN and Resp Therapist ***Pediatric first responders include ED RN and Resp Therapist 10

IMPORTANT MET TEAM TRAITS • Must be available to respond immediately when called • Must be onsite and accessible • Must have critical care skills • Must have good customer service skills – – Respond with a smile “Thank you for calling. How may I help you” Staff must feel comfortable in order to call If they feel ridiculed or condescended to they will be reluctant to call 11
IMPORTANT TO REMEMBER • The MET team does not work independently of the patient’s assigned nurse or physician – No Pre-printed orders! – ACLS Guidelines may be followed • Care should be taken to include both the patient’s nurse and the patient’s physician early and throughout the process of caring for the deteriorating patient 12
ACTIVATING THE MET TEAM Due to the nature of the services, the MET Team will respond to all departments with the exception of the following: a) Pediatrics – call ED RN (MET may be called for concerns regarding parent/visitor or other adult emergency b) Couplet Care – call L&D RN (L&D RN to assist MET Responders) c) Children’s Subacute Center – Call 911 13
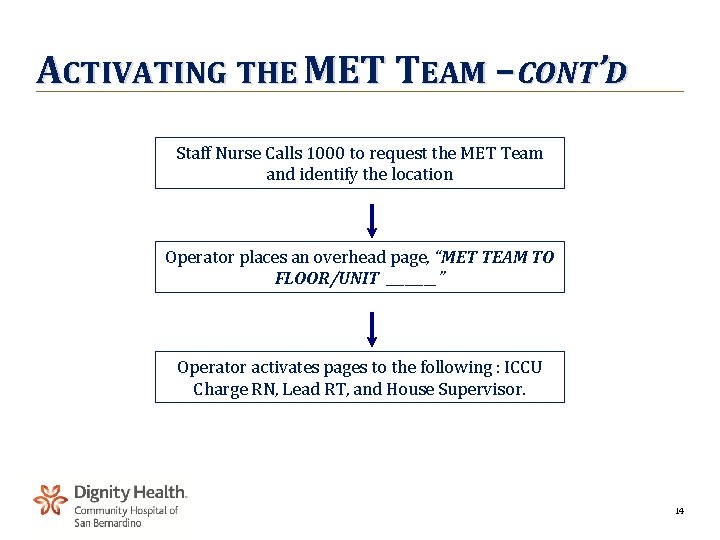
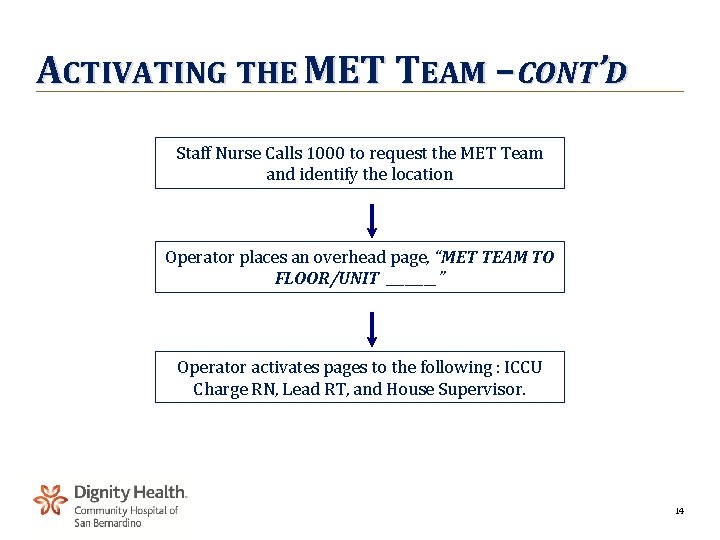
ACTIVATING THE MET TEAM – CONT’D Staff Nurse Calls 1000 to request the MET Team and identify the location Operator places an overhead page, “MET TEAM TO FLOOR/UNIT ____” Operator activates pages to the following : ICCU Charge RN, Lead RT, and House Supervisor. 14
INTERVENTIONS BY MET : REGISTERED NURSE • Perform a thorough assessment to determine the status of the patient • A sepsis screening will be performed on all patients – If patient screens positive for sepsis, lactic acid level and blood cultures are drawn – If patient screens positive for sepsis and has a systolic BP of <90 mm. Hg, the MET RN will administer a 20 ml/kg fluid bolus utilizing normal saline – The MET RN will contact the primary physician and inform him of the positive sepsis screen and obtain orders 15
INTERVENTIONS BY MET : REGISTERED NURSE – CONT’D • Consider initiating a 500 ml normal saline bolus for patients with an SBP ≤ 70 mm. Hg with signs/symptoms of shock while awaiting physician call back • Evaluate and assess the need to transfer to a higher level of care. – In the event the physician cannot be reached, the MET team has the authority to move the patient to the appropriate level of care • Document on MET documentation for PI/review and fax to House Supervisor 16
INTERVENTIONS BY MET : RESPIRATORY THERAPIST • Oxygen may be initiated for: – ALOC – Moderate to severe dyspnea – Moderate cyanosis – Pallor – Moderate to severe hypotension • Aerosol bronchodilator therapy may be initiated as defined in RT protocol based on assessment • ABGs may be obtained to assess acid-base balance 17
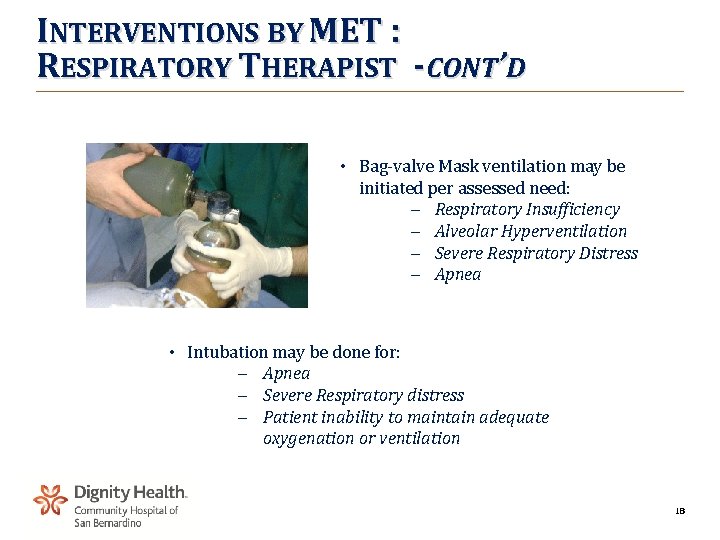
INTERVENTIONS BY MET : RESPIRATORY THERAPIST -CONT’D • Bag-valve Mask ventilation may be initiated per assessed need: - Respiratory Insufficiency - Alveolar Hyperventilation - Severe Respiratory Distress - Apnea • Intubation may be done for: - Apnea - Severe Respiratory distress - Patient inability to maintain adequate oxygenation or ventilation 18
RESPONSIBILITY OF THE PATIENT’S NURSE • Provide the team with a status report upon team arrival • Make the medical record available • Ensure that any ordered therapy is available on the unit before calling the Team • Assist in transfer of the patient if required. • The accepting RN will check for IV patency or assist with establishing an IV site • Document in the Nursing Notes reason for MET call and patient’s response to the intervention 19
MET TEAM RESPONDERS : WHAT TO AVOID • • MET Team responders should avoid “lateral violence” or “horizontal violence” – Nurses who overtly or covertly direct their dissatisfaction toward each other, toward themselves, and/or toward those less powerful – Considered behavior of an “oppressed population” Lateral violence stops nurses from asking questions or seeking help when it is needed out of fear 20
EXAMPLES OF LATERAL VIOLENCE • Non-verbal innuendo – Raising eyebrows, face-making • Verbal remarks – Snide comments, abrupt responses • Undermining – Turning away, ignoring questions • Scapegoating – Attributing patient condition to the nurse • Backstabbing – Complaining about the nurse to other individuals 21
AVOIDING LATERAL VIOLENCE • Be cooperative, despite feelings of dislike • Don’t denigrate co-workers to superiors • Don’t engage in negative conversations about co-workers • Don’t criticize another nurse publicly • Look a co-worker in the eye when talking with them 22
MET PROCESS MONITORING • Feed back from the MET team and initiating nurses will be collected and examined using the “MET Documentation Form” • The form includes: – – – • Type of event, location , and patient outcome Evaluation of MET procedure Response time Competency of team members Availability and functioning of equipment Accurate completion of forms Data is evaluated by Code Blue and ICCU subcommittees 23
RESPONSIBILITY OF THE PATIENT’S NURSE • Provide the team with a status report upon team arrival • Make the medical record available • Ensure that any ordered therapy is available on the unit before calling the Team • Assist in transfer of the patient if required. • The accepting RN will check for IV patency or assist with establishing an IV site • Document in the Nursing Notes reason for MET call and patient’s response to the intervention 24
IMPORTANT TO REMEMBER • The MET responders should be on the floor for interventions 30 minutes or less • Collaboration with the physician or triage to a higher level of care will usually be made within 30 minutes • However, patient safety comes first and the MET responders will assist in the safe transport of the patient to a higher level of care if required. 25

26