Identifying and mitigating risks when providing therapy services


- Slides: 66
Identifying and mitigating risks when providing therapy services to people with ABI in the National Disability Insurance Scheme LIB BY CALLAWAY SUE SLOAN JA N MA CKEY ASSBI, WELLINGTON May 2019
Learning objectives By the end of this session, participants will: 1. Understand current risks that exist when providing therapy services within the NDIS, both for both service providers and Scheme participants 2. Identify strategies to mitigate these risks, whilst delivering outcome-focused capacity building supports 3. Consider the work of the new NDIS Quality and Safeguarding Commission Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
Workshop overview 1. NDIS roll out to date + people with ABI 2. Introduction of the NDIS Quality + Safeguards Commission 3. NDIS plan management + provider registration 4. The risks + strategies to mitigate them Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
Who are we talking about today? NDIS participants with severe acquired brain injury (ABI) Living with Supported Independent Living (SIL) +/- SDA or 1: 1 or 24/7 support in community Often limited capacity for self-advocacy or availability of family advocacy / informal supports Often ‘intensive / super intensive group’ or within new ‘complex participant pathway’, as defined by NDIA Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
1. NDIS roll out to date + people with ABI
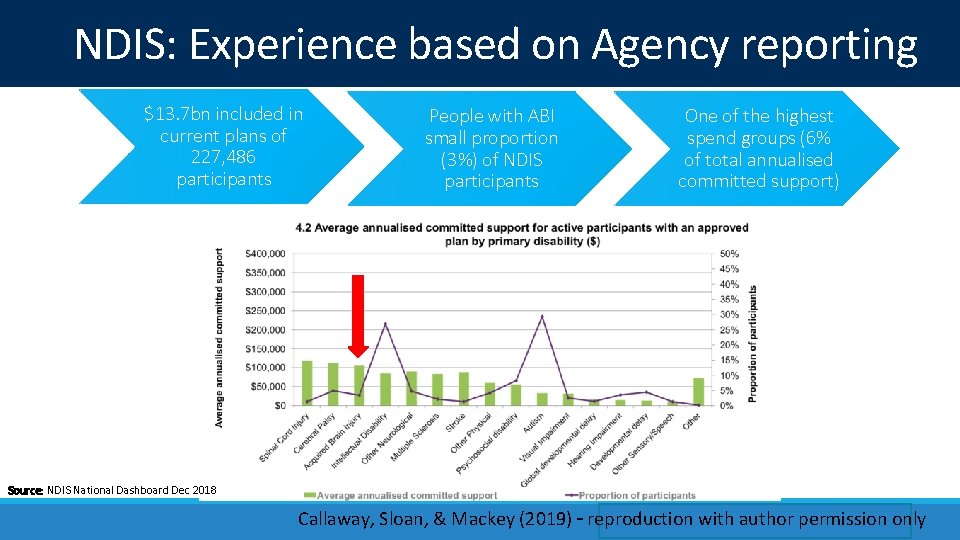
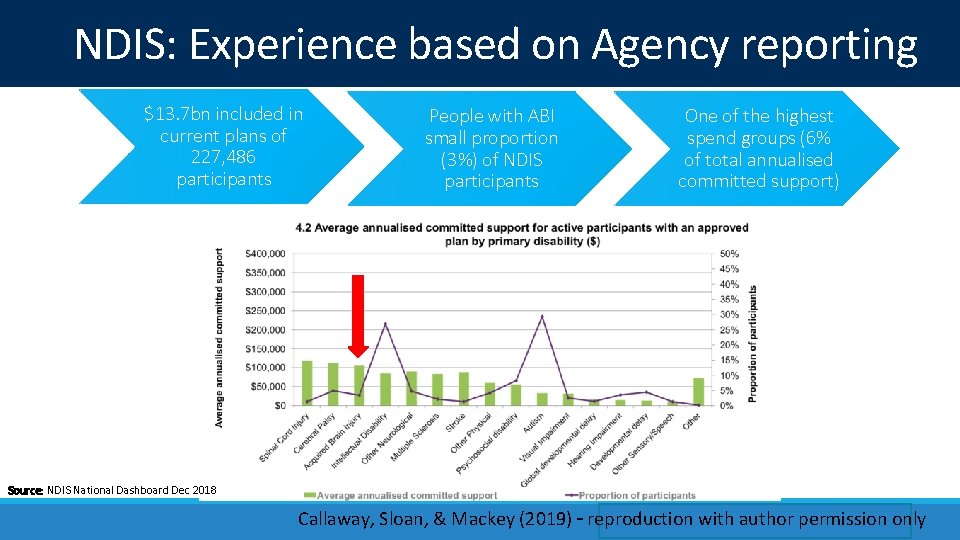
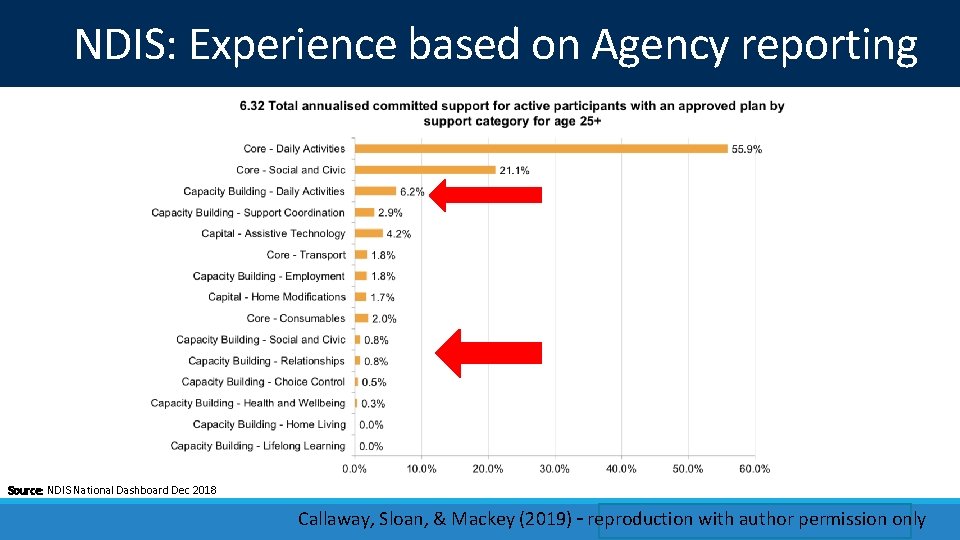
NDIS: Experience based on Agency reporting $13. 7 bn included in current plans of 227, 486 participants People with ABI small proportion (3%) of NDIS participants One of the highest spend groups (6% of total annualised committed support) Source: NDIS National Dashboard Dec 2018 Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
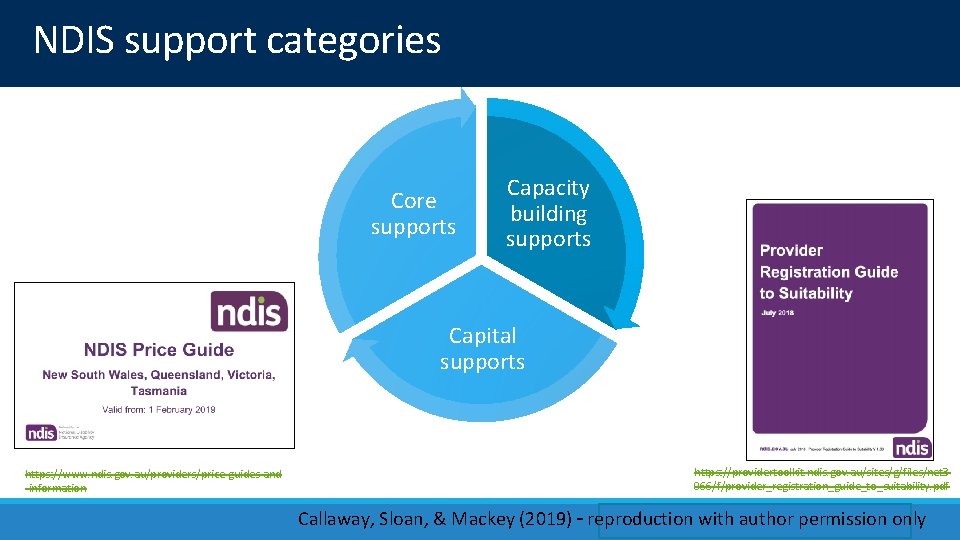
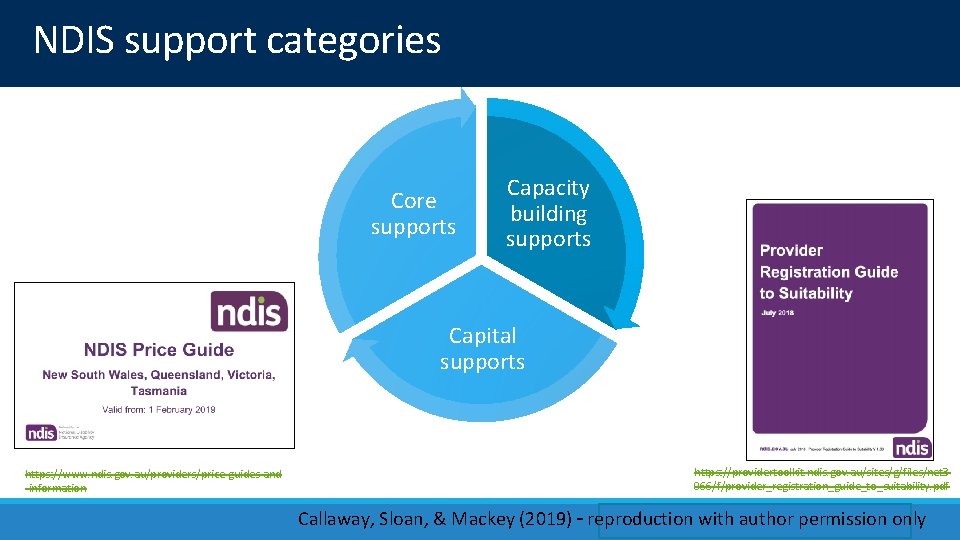
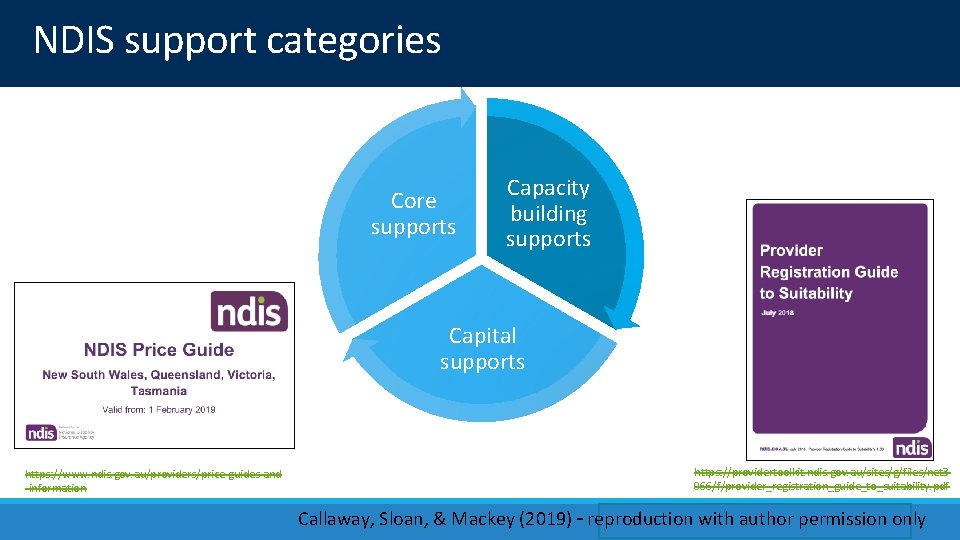
NDIS support categories Core supports Capacity building supports Capital supports https: //www. ndis. gov. au/providers/price-guides-and -information https: //providertoolkit. ndis. gov. au/sites/g/files/net 3 066/f/provider_registration_guide_to_suitability. pdf Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
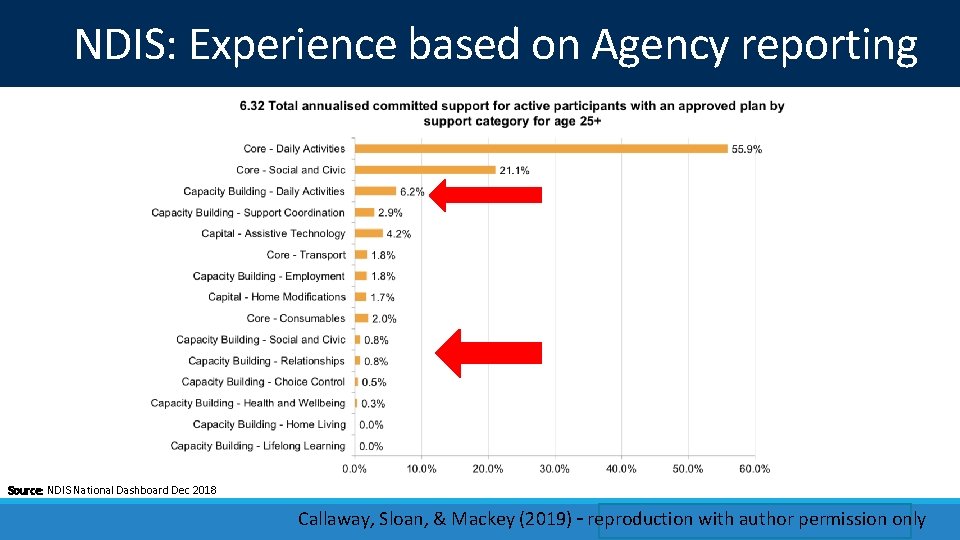
NDIS: Experience based on Agency reporting Source: NDIS National Dashboard Dec 2018 Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
Complex Support Needs pathway Established to provide specialised support for participants with disability who have other challenges impacting their lives (e. g. mental health issues, incarceration or homelessness) and need a higher level of specialised supports in their plan. Includes specialised planning teams, NDIA liaison and support coordinators with the ‘networks, skill and knowledge of government and community services to provide the support required for complex needs’. https: //www. ndis. gov. au/news/1215 -ndis-pathway-reform Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
Complex Support Needs pathway NDIS Participants identified for CSN Pathway by the complexity of their situation and personal factors (e. g. homelessness; returning to the community from aged care). Involuntary or voluntary involvement with particular government systems such as Justice or mental health would also be factors necessitating entry to the pathway. At full scheme, it is estimated around 10 to 15 per cent of NDIS participants may require complex support. https: //www. ndis. gov. au/news/1002 -improved-ndis-planning-people-complex-support-needs Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
Key features of the Complex Support Needs pathway 1. Pre-access, local engagement and strengthening connections to other services 2. Access, detailed handovers and connections 3. Specialised Planners and Complex Support Practice Lead 4. Skilled Support Coordinators and effective plan implementation 5. Ongoing monitoring and evaluation 6. Review outcomes and progress https: //www. ndis. gov. au/news/1215 -ndis-pathway-reform Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
2. Introduction of the NDIS Quality + Safeguards Commission

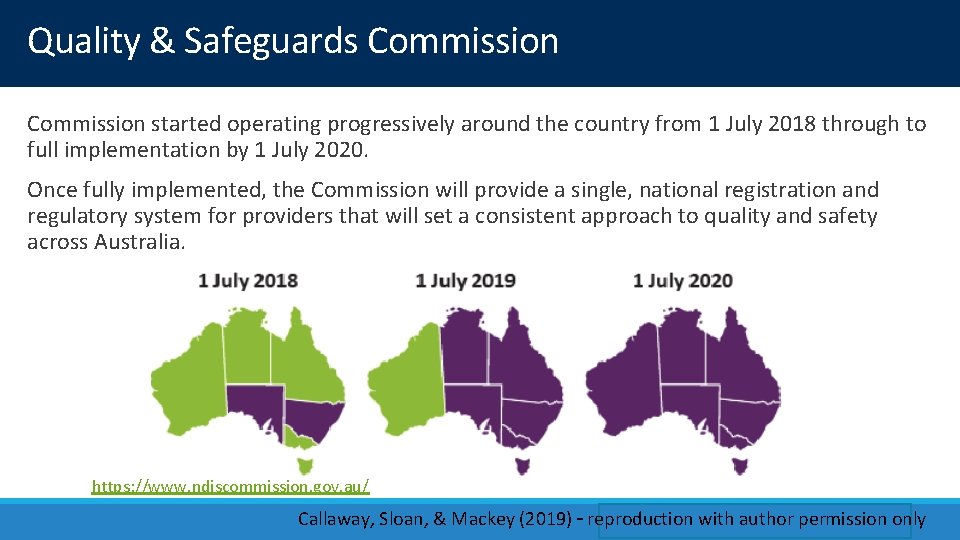
Quality & Safeguards Commission https: //www. ndiscommission. gov. au/ Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
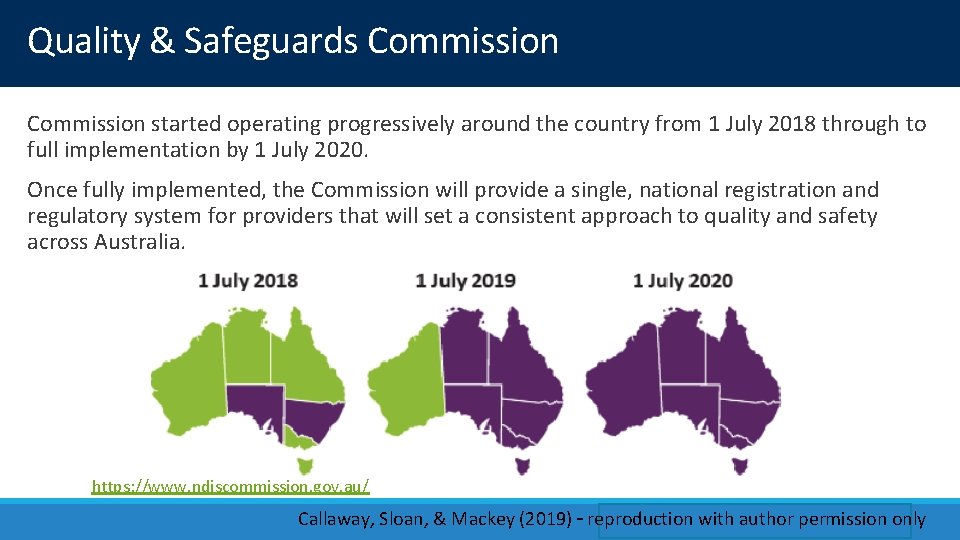
Quality & Safeguards Commission started operating progressively around the country from 1 July 2018 through to full implementation by 1 July 2020. Once fully implemented, the Commission will provide a single, national registration and regulatory system for providers that will set a consistent approach to quality and safety across Australia. https: //www. ndiscommission. gov. au/ Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
Quality & Safeguards Commission The NDIS Commission introduced several changes state-by-state, including: • a new NDIS Code of Conduct and NDIS Practice Standards, setting out expectations for the quality and safety of the services and supports providers deliver • changes to provider registration and the way complaints are made, incidents are reported, behaviour support plans are developed and checked, and worker screening is undertaken. Unregistered providers are also subject to new requirements including the NDIS Code of Conduct and complaints handling arrangements. https: //www. ndiscommission. gov. au/ Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
https: //www. ndiscommission. gov. au/ Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
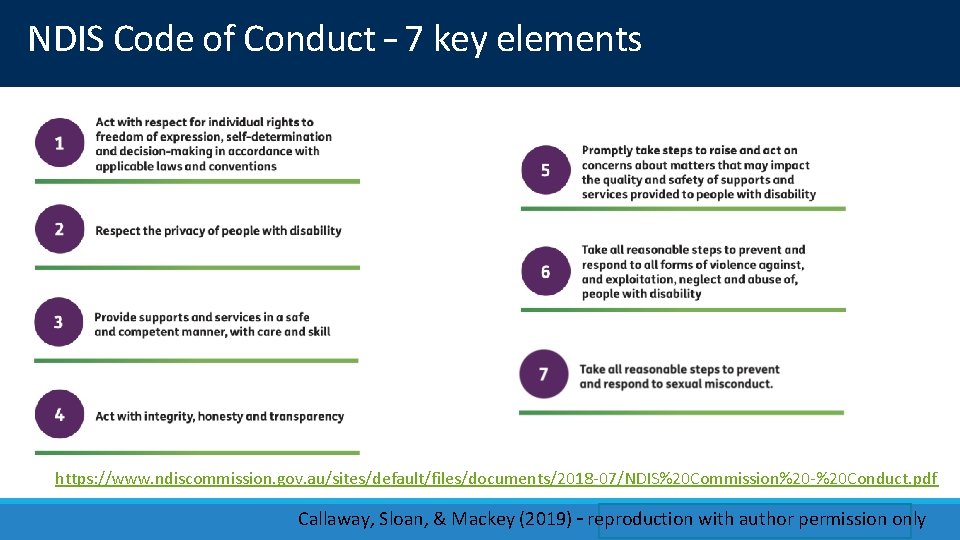
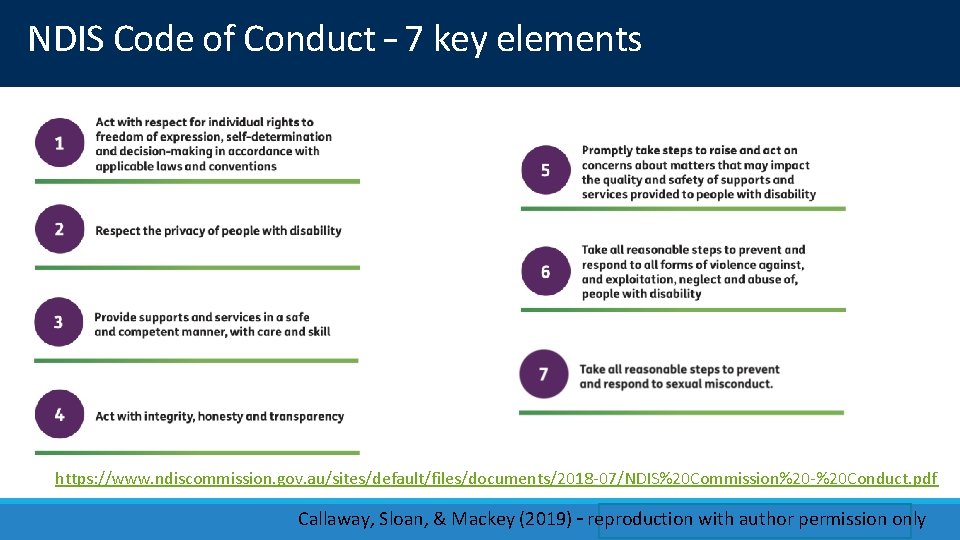
NDIS Code of Conduct – 7 key elements https: //www. ndiscommission. gov. au/sites/default/files/documents/2018 -07/NDIS%20 Commission%20 -%20 Conduct. pdf Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
Consequences of breaching the code • The NDIS Commission (independent regulator) is empowered to take a range of sanctions and remedial action if NDIS providers (or their workers) breach the Code. • Penalties for breaching the Code will depend on the nature of the breach. • Breaches of a less serious nature – training and education, warnings and directions may be used. • More serious breaches – NDIS Commission may choose different response e. g. going to court to have civil penalties imposed; deregistering NDIS providers; banning NDIS providers or workers from providing services and supports in the NDIS sector. • The Commissioner may publish on the NDIS Commission’s website the result of any action taken against an NDIS provider or person employed / engaged by an NDIS provider. https: //www. ndiscommission. gov. au/sites/default/files/documents/2018 -07/NDIS%20 Commission%20 -%20 Conduct. pdf Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
Relationship with other professional codes • Workers required to comply with an existing professional code of conduct (e. g. nurses, psychologists and health care workers) will also be required to comply with the NDIS Code of Conduct and other applicable regulatory frameworks (e. g. child protection requirements). • If a professional is found not to have complied with their own professional standards in providing NDIS supports and services, they may have also breached the NDIS Code of Conduct. The reverse may also be the case. • The NDIS Commission will, as far as practicable, coordinate any regulatory activity with the professional body or other regulator, as appropriate, to ensure there is no unnecessary duplication and manage any overlapping areas of regulation. Recommendation 17 3. 34 The committee recommends that the NDIS Quality and Safeguards Commission urgently review the impact of its regulatory requirements on sole providers and small to medium sized businesses providing disability services and report to the parliament on its findings. https: //www. ndiscommission. gov. au/sites/default/files/documents/2018 -07/NDIS%20 Commission%20 -%20 Conduct. pdf Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
https: //www. ndiscommission. gov. au/ Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
NDIS practice standards Benchmark for providers to assess their performance, and to demonstrate how they provide high quality and safe supports and services to NDIS participants. With the NDIS Code of Conduct, the NDIS Practice Standards are designed to assist NDIS participants to be aware of what quality service provision they should expect from NDIS providers. Both core and supplementary modules Each module has: 1. a series of high-level, participant-focused outcomes 2. for each outcome, quality indicators that auditors will use to assess a provider’s compliance with the Practice Standards https: //www. ndiscommission. gov. au/sites/default/files/documents/2018 -07/NDIS%20 Practice%20 Standards. pdf Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
NDIS practice standards - modules Core module covers: • rights and responsibility for participants • governance and operational management • the provision of supports, and • the support provision environment https: //www. ndiscommission. gov. au/sites/default/files/documents/2018 -07/NDIS%20 Practice%20 Standards. pdf Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
NDIS practice standards - modules Supplementary modules cover: • High intensity daily personal activities – complex bowel care; enteral feeding; tracheostomy management; urinary catheter management; ventilator management; subcutaneous injections; complex wound management • Specialist behaviour support – behaviour support; restrictive practices, behaviour assessment & support plans; behaviour support implementation, monitoring & review; reportable incidences • Implementing behaviour support plans • Early childhood supports • Specialised support co-ordination • Specialist disability accommodation https: //www. ndiscommission. gov. au/sites/default/files/documents/2018 -07/NDIS%20 Practice%20 Standards. pdf Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
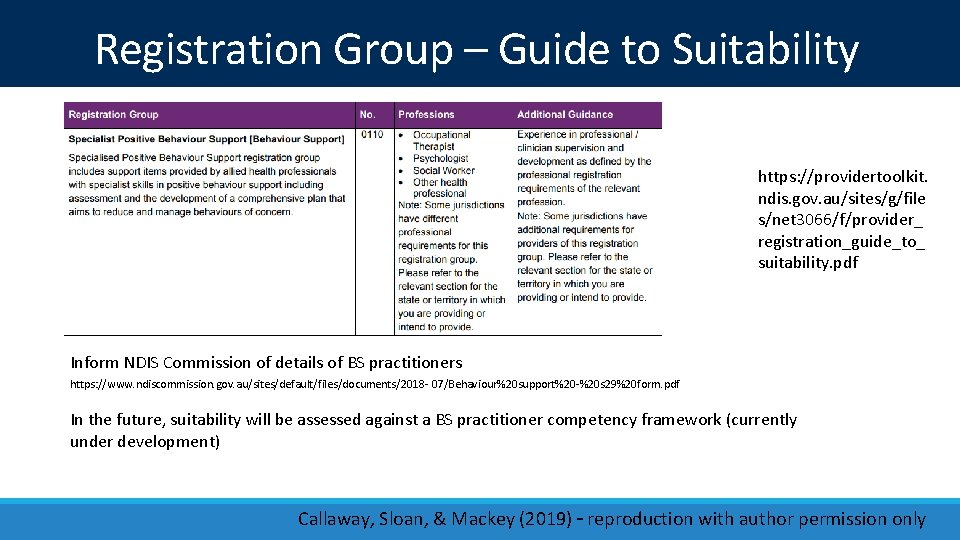
Behaviour Support Can be delivered by a range of professional groups (commonly NP, OT or other health professionals – see ‘Guide to suitability’) Need to be registered – certification process due to level of risk (funding for BS is agency managed) Two tiered auditing process – certification or verification Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
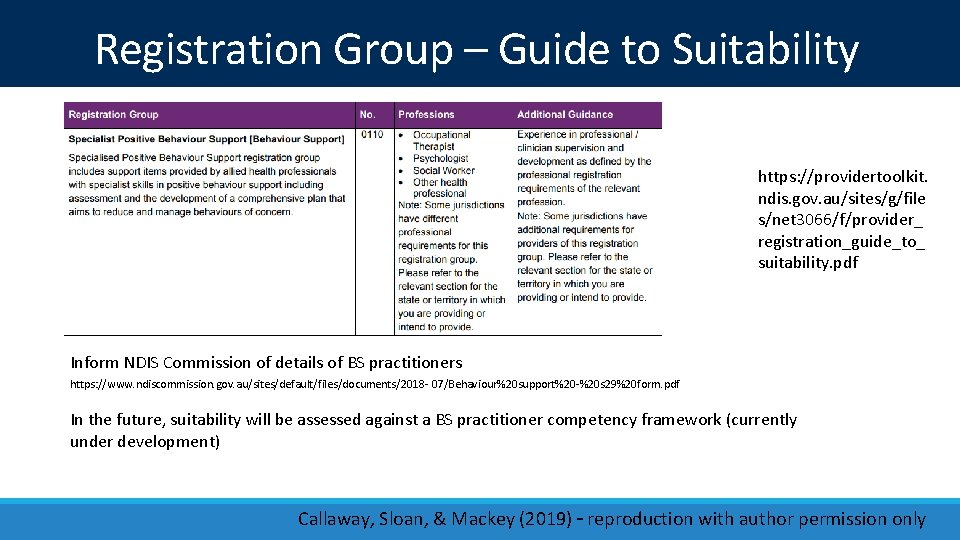
Registration Group – Guide to Suitability https: //providertoolkit. ndis. gov. au/sites/g/file s/net 3066/f/provider_ registration_guide_to_ suitability. pdf Inform NDIS Commission of details of BS practitioners https: //www. ndiscommission. gov. au/sites/default/files/documents/2018 - 07/Behaviour%20 support%20 -%20 s 29%20 form. pdf In the future, suitability will be assessed against a BS practitioner competency framework (currently under development) Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
New regulatory framework for behaviour support https: //www. legislation. gov. au/Details/F 2018 L 00632 https: //www. dss. gov. au/sites/default/files/documents/04_2017/ndis_quality_and_ safeguarding_framework_final. pdf Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
Behaviour Support Rules and framework are complex and involve both NDIS Quality and Safeguards Commission as well as State Government processes. Level of complexity and cost risks providers choosing to not register, leading to ‘thin markets’. Recent granting rounds for sector development: • NDIS Quality and Safeguarding Commission grants focused on NDIS provider readiness • NDIS granting rounds for ‘exceptionally complex support needs’ group with eligibility that applicant is a registered Provider of Supports, in ALL of the following Registration Groups: • Support Coordination (0132) • Behaviour Support (110); and • Assistance in Coordinating Or Managing Life Stages, Transitions and Supports (0106) Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
Obligations on Providers where restrictive practices are used Providers who use restrictive practices must be registered AND engage a registered specialist behaviour support practitioner, qualified to undertake behaviour support assessments and develop behaviour support plans. NDIS participants who may be subject to restrictive practices must have a behaviour support plan developed and lodged with the NDIS Commission. The use of restrictive practices will be subject to conditions, including: • the person must have a behaviour support plan in place, specifying that personcentred strategies must be applied first with restrictive practices used as a last resort in response to a risk of harm to the person or others • alignment with any state or territory authorisation and consent requirements. Providers who USE restrictive practices must provide monthly reports to the NDIS Commission. Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
Obligations on Providers where restrictive practices are used NDIS providers must understand how NDIS policies and procedures support participants with behaviour support needs. Providers will need to help staff, participants, families, and decision-makers understand the NDIS Commission’s behaviour support function. Providers implementing behaviour support plans must work closely with the NDIS behaviour support practitioner, the participant, and their family and carers on the development of the NDIS behaviour support plan. Providers must ensure that any staff involved in implementing positive behaviour strategies or restrictive practices have received appropriate training. Providers must report the unplanned or unapproved use of a restrictive practice to the NDIS Commission as a reportable incident. Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
NDIS plan management + provider registration
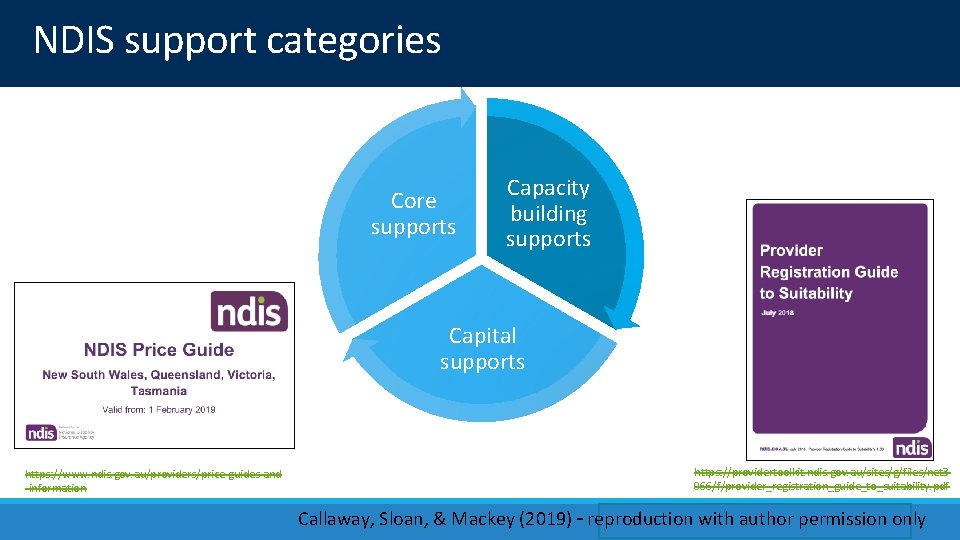
NDIS support categories Core supports Capacity building supports Capital supports https: //www. ndis. gov. au/providers/price-guides-and -information https: //providertoolkit. ndis. gov. au/sites/g/files/net 3 066/f/provider_registration_guide_to_suitability. pdf Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
NDIS – plan management Three options: • Self-managed (or Plan Nominee-managed) • NDIA-managed • Provider-managed or a mix of the above. Method of plan management is discussed in planning process (but Agency has set restrictions on some supports being self-managed). If NDIS plan is self-managed, the participant can choose any provider (except for Agency-managed budget items e. g. behaviour support; support coordination; SIL or SDA). If plan is Agency managed, the participant will need to use an NDIS registered provider. See ‘provider toolkit’– https: //providertoolkit. ndis. gov. au/ Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
NDIS – quality + safeguarding • NDIA not the regulator – will provide advice and information, but will not try and restrict expenditure • The Agency relies on existing regulatory mechanisms e. g. ACCC, Office of Fair Trading • New NDIS Quality & Safeguarding Commission is now the independent regulator (national implementation by 1/7/19) Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
NDIS provider requirements during Scheme transition Libby Callaway, March 2018
NDIS provider requirements during Scheme transition Very complex – 1 page of guidance for SA and 20 for Victoria Annual certification/verification quality audit: • Certification – required against the national disability service standards for specific provider categories • Verification – applies to NDIS providers who are individual sole traders or partnerships AND delivering lower risk or less complex NDIS supports and services Significant cost of certification $6 K+ year 1 +/- annual re -certification fees = risk of quality market failure Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
The risks + strategies to mitigate them
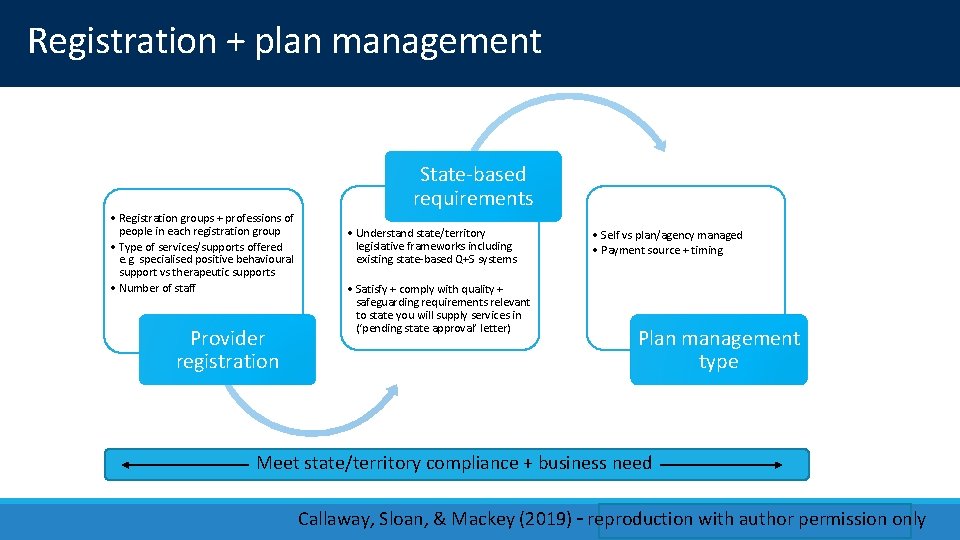
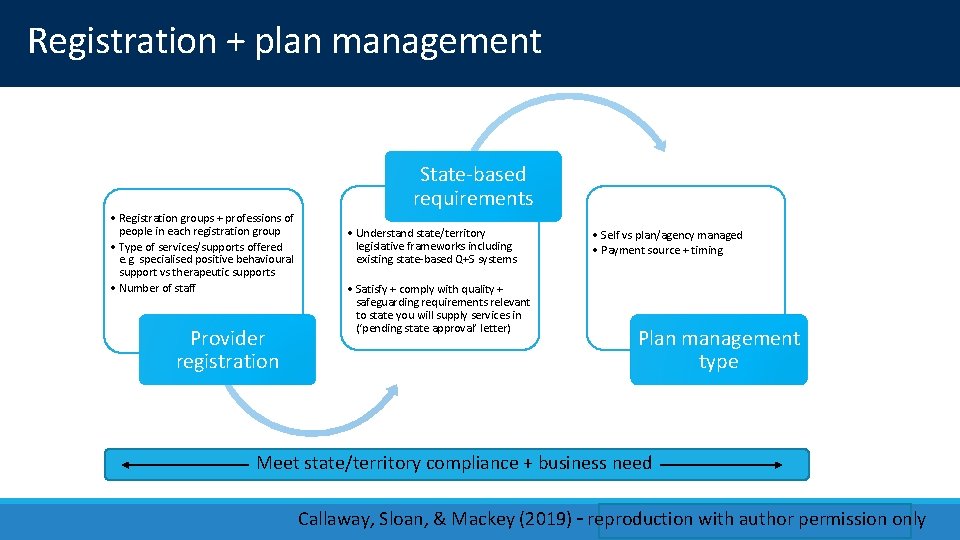
Registration + plan management • Registration groups + professions of people in each registration group • Type of services/supports offered e. g. specialised positive behavioural support vs therapeutic supports • Number of staff Provider registration State-based requirements • Understand state/territory legislative frameworks including existing state-based Q+S systems • Satisfy + comply with quality + safeguarding requirements relevant to state you will supply services in (‘pending state approval’ letter) • Self vs plan/agency managed • Payment source + timing Plan management type Meet state/territory compliance + business need Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
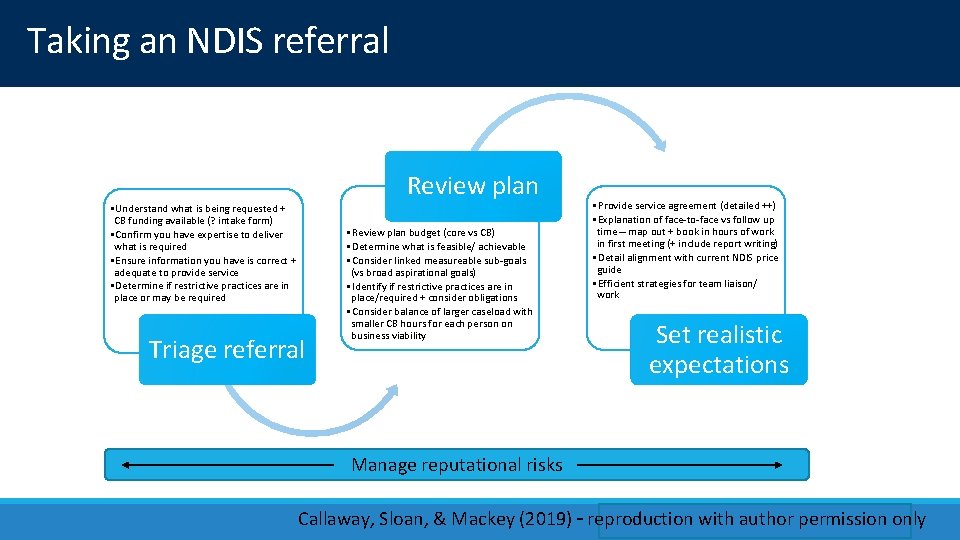
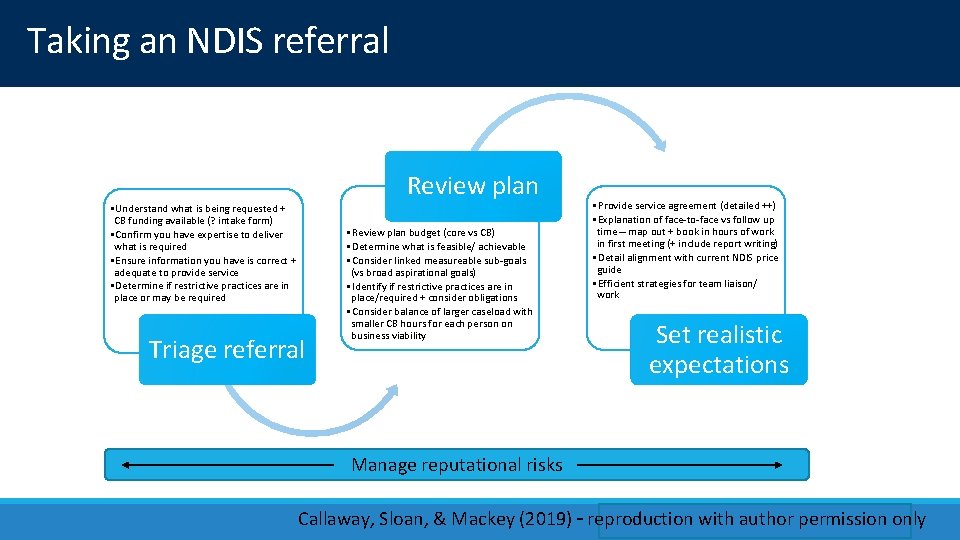
Taking an NDIS referral • Understand what is being requested + CB funding available (? intake form) • Confirm you have expertise to deliver what is required • Ensure information you have is correct + adequate to provide service • Determine if restrictive practices are in place or may be required Triage referral Review plan • Review plan budget (core vs CB) • Determine what is feasible/ achievable • Consider linked measureable sub-goals (vs broad aspirational goals) • Identify if restrictive practices are in place/required + consider obligations • Consider balance of larger caseload with smaller CB hours for each person on business viability • Provide service agreement (detailed ++) • Explanation of face-to-face vs follow up time – map out + book in hours of work in first meeting (+ include report writing) • Detail alignment with current NDIS price guide • Efficient strategies for team liaison/ work Set realistic expectations Manage reputational risks Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
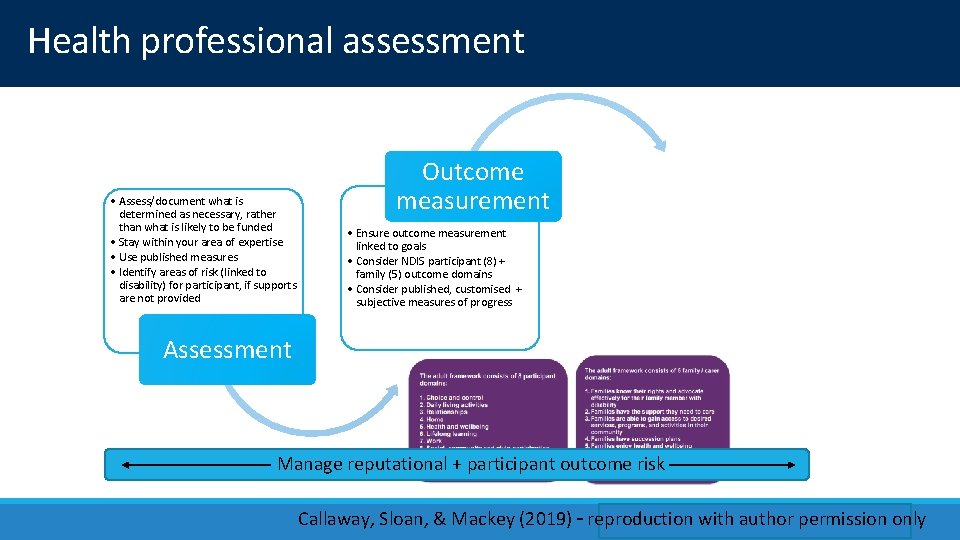
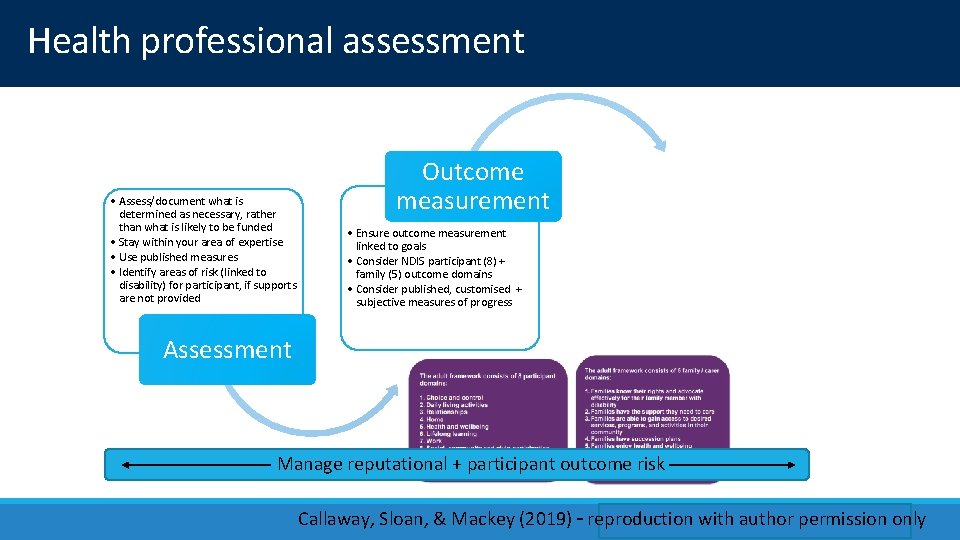
Health professional assessment • Assess/document what is determined as necessary, rather than what is likely to be funded • Stay within your area of expertise • Use published measures • Identify areas of risk (linked to disability) for participant, if supports are not provided Assessment Outcome measurement • Ensure outcome measurement linked to goals • Consider NDIS participant (8) + family (5) outcome domains • Consider published, customised + subjective measures of progress • Diarise 8 -12 weeks prior to plan review for writing review report • Identify risks occurring during plan period (e. g. falls; behaviour support needs; risk to personal safety) • Consider published, customised + subjective measures of progress Plan review Manage reputational + participant outcome risk Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
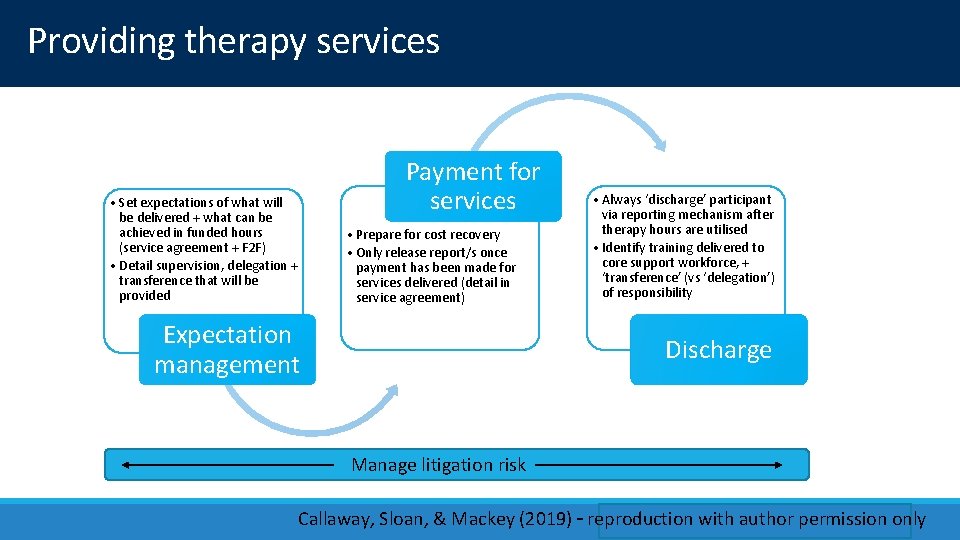
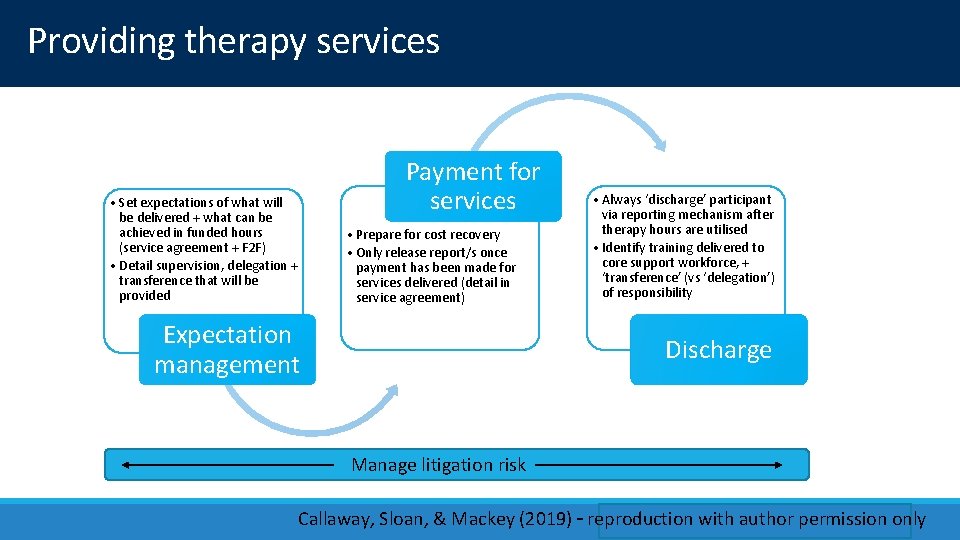
Providing therapy services • Set expectations of what will be delivered + what can be achieved in funded hours (service agreement + F 2 F) • Detail supervision, delegation + transference that will be provided Payment for services • Prepare for cost recovery • Only release report/s once payment has been made for services delivered (detail in service agreement) Expectation management • Always ‘discharge’ participant via reporting mechanism after therapy hours are utilised • Identify training delivered to core support workforce, + ‘transference’ (vs ‘delegation’) of responsibility Discharge Manage litigation risk Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
• Governance tool developed by DHHS Victoria through the NDIS Sector Development Fund • Provide information + guidance to ‘enhance the utilisation + development of the AHA role’ within disability services • Defines, delineates + operationalises AHP + AHA roles in disability including ‘delegation’ vs ‘transference’ of responsibility See https: //www 2. health. vic. gov. au/-/media/health/files/collections/policies -and-guidelines/a/allied-health-in-disability---supervision-and-delegationframework. pdf? la=en&hash=17 C 8 B 0 DA 1306 D 5944508699 B 58349590 B 1 BE 4 CCA Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
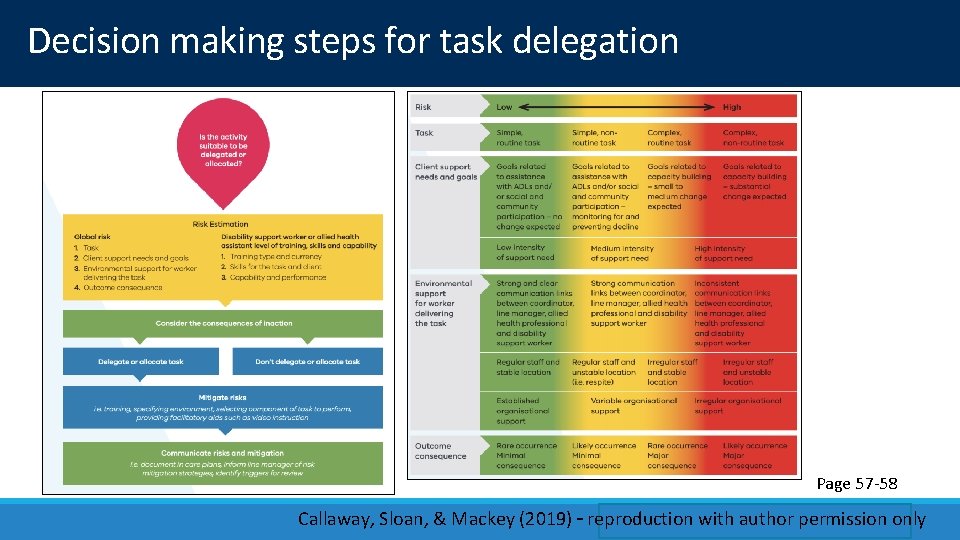
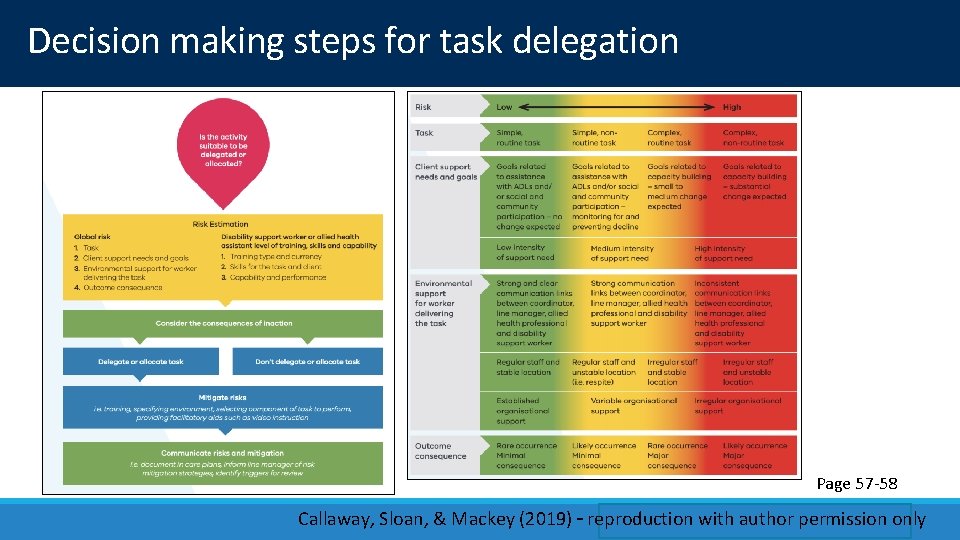
Decision making steps for task delegation Page 57 -58 Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
Resources for delegation • MOT Prac project team formalising D&S structures for PP working with NDIS providers for CB interventions • Email SS if want more detail Page 103 -117 Callaway, Sloan, & Mackey (2019) – reproduction with author permission only

Scenario – risk mitigation when working with an existing plan
Maximising therapy hours and supports Working with the Plan, where you inherit small number of pre-approved hours (typically 10 -15/annum) ◦ Triage the referral and goals / expectations carefully ◦ Identify sub-goals (use NDIS outcome domains) ◦ Plan therapy input to achieve a small sub-goal ◦ Service agreement Consider model of intervention: ◦ 1: 1 with client (+/- AHA / DSW) ◦ Secondary consultation ◦ Training to build direct workforce (DSW) capacity ◦ Or, a combination of above Sloan, Callaway & Mackey (2018) – reproduction with author permission only
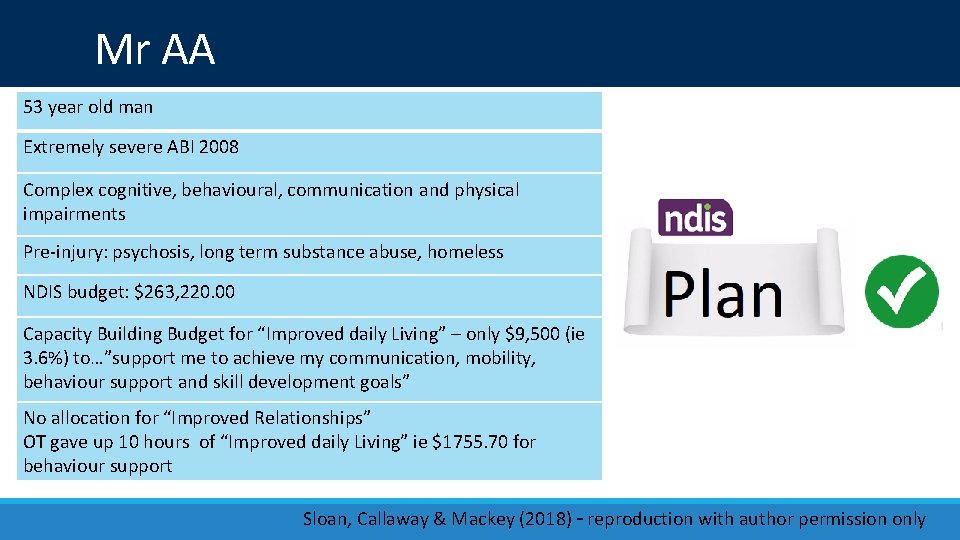
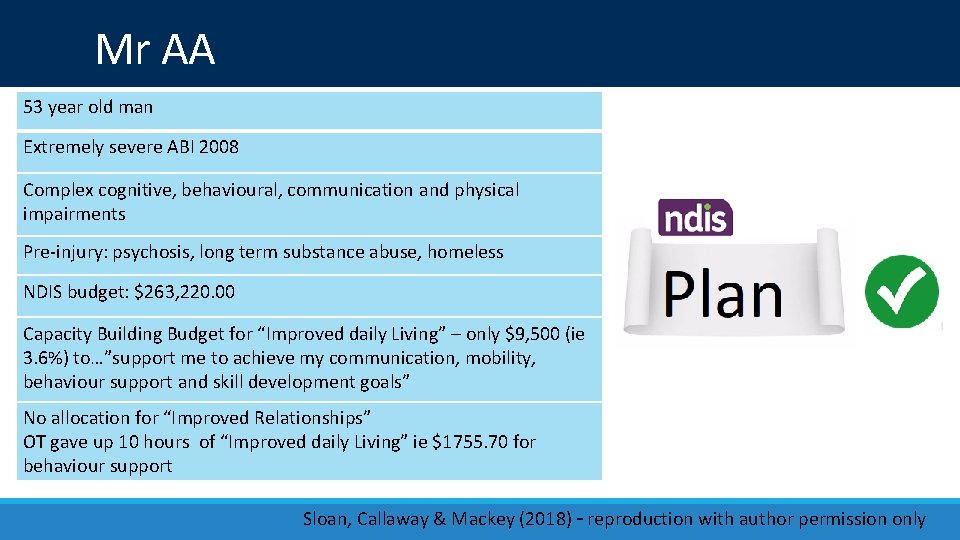
Mr AA 53 year old man Extremely severe ABI 2008 Complex cognitive, behavioural, communication and physical impairments Pre-injury: psychosis, long term substance abuse, homeless NDIS budget: $263, 220. 00 Capacity Building Budget for “Improved daily Living” – only $9, 500 (ie 3. 6%) to…”support me to achieve my communication, mobility, behaviour support and skill development goals” No allocation for “Improved Relationships” OT gave up 10 hours of “Improved daily Living” ie $1755. 70 for behaviour support Sloan, Callaway & Mackey (2018) – reproduction with author permission only
AA’s team • 24 -hour active support – Disability Support Workers (DSW) and dedicated House Manager • 15 hours / week 1: 1 DSW for community access • OT, SP, and PT 10 hours / annum each • NP for Behaviour Support 10 hours / annum Sloan, Callaway & Mackey (2018) – reproduction with author permission only
NDIS – Overt Behaviour Scale Presence, frequency + severity of 9 common behaviours after ABI See https: //www. mysupportspace. org/library/tools-andresources/support-needs Sloan, Callaway & Mackey (2018) – reproduction with author permission only
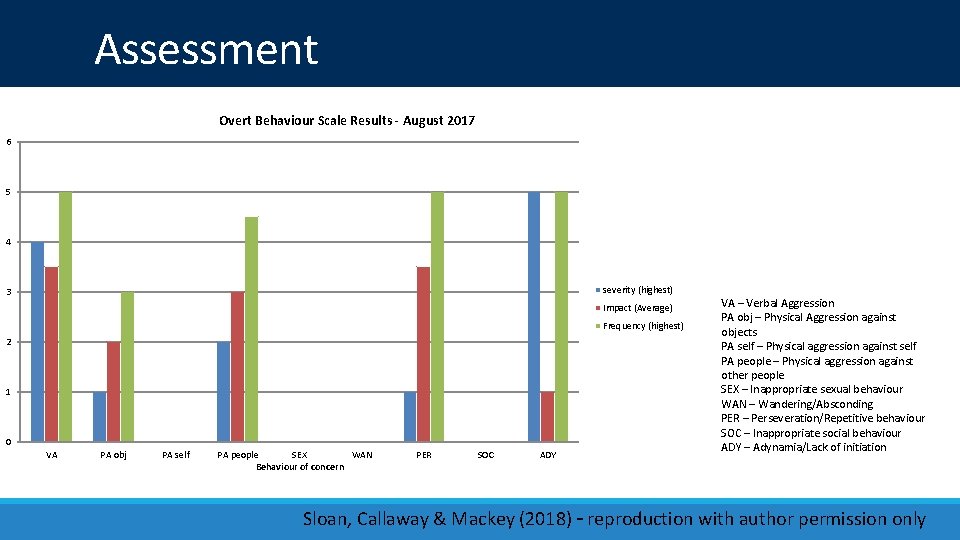
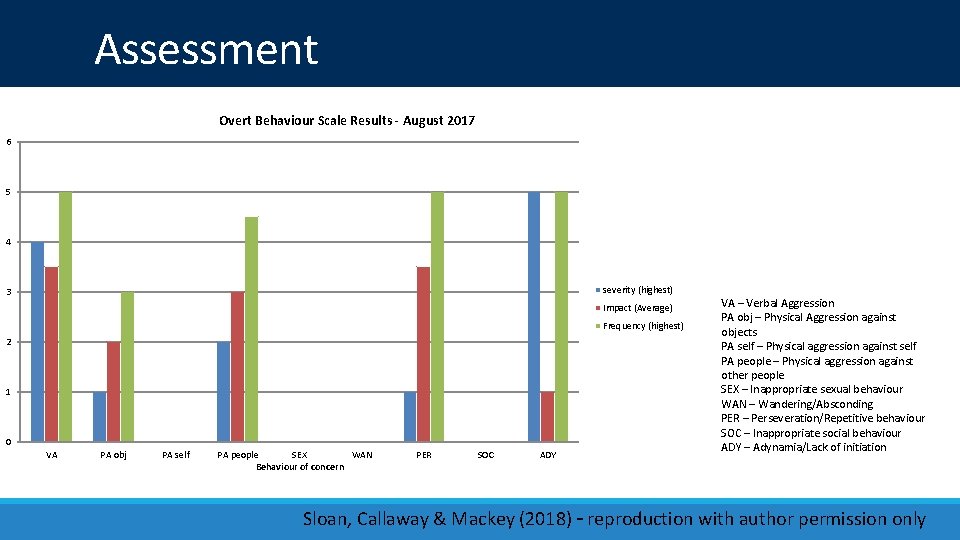
Assessment Overt Behaviour Scale Results - August 2017 6 5 4 severity (highest) 3 Impact (Average) Frequency (highest) 2 1 0 VA PA obj PA self PA people SEX WAN Behaviour of concern PER SOC ADY VA – Verbal Aggression PA obj – Physical Aggression against objects PA self – Physical aggression against self PA people – Physical aggression against other people SEX – Inappropriate sexual behaviour WAN – Wandering/Absconding PER – Perseveration/Repetitive behaviour SOC – Inappropriate social behaviour ADY – Adynamia/Lack of initiation Sloan, Callaway & Mackey (2018) – reproduction with author permission only
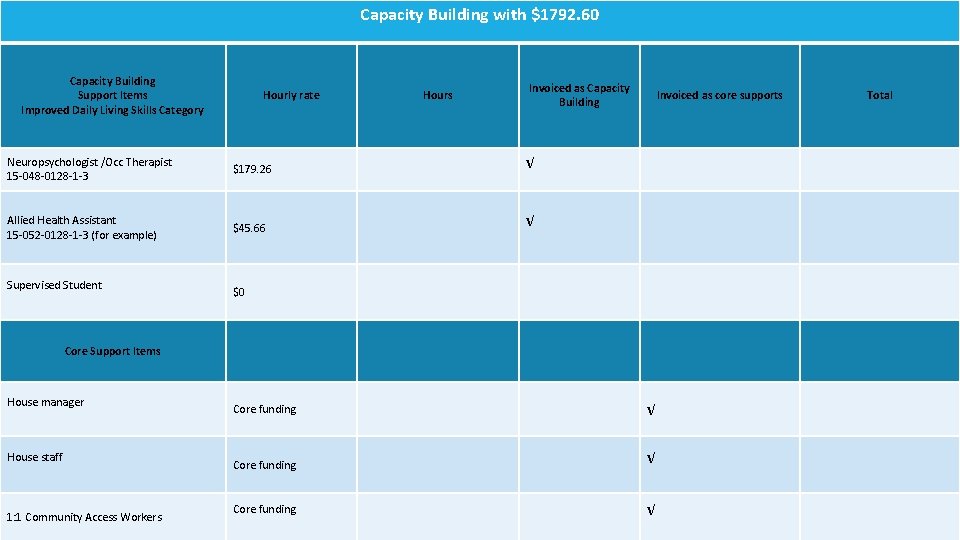
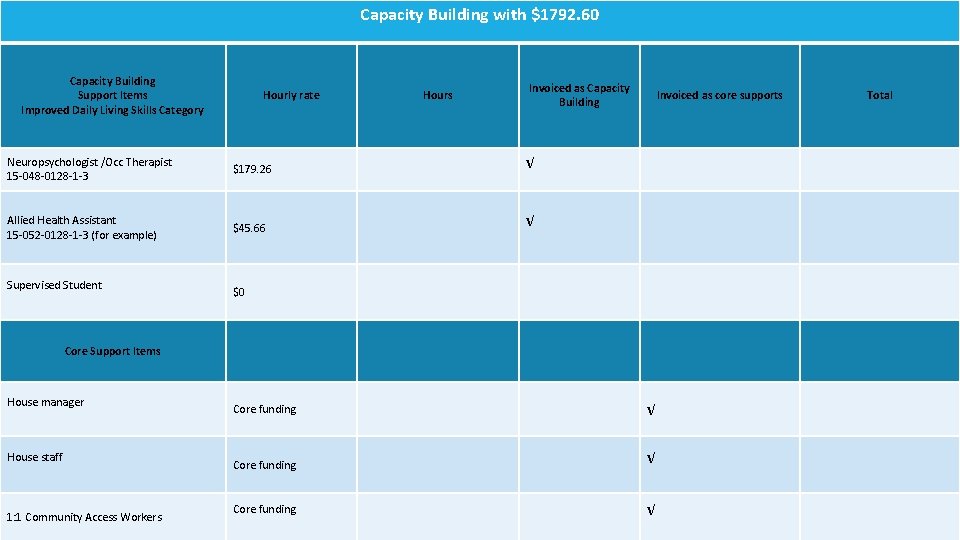
Capacity Building with $1792. 60 How to use this 10 hours funding? Capacity Building Support Items Improved Daily Living Skills Category Hourly rate Hours Invoiced as Capacity Building Neuropsychologist /Occ Therapist 15 -048 -0128 -1 -3 $179. 26 √ Allied Health Assistant 15 -052 -0128 -1 -3 (for example) $45. 66 √ Supervised Student Invoiced as core supports $0 Core Support Items House manager House staff 1: 1 Community Access Workers Core funding √ Total
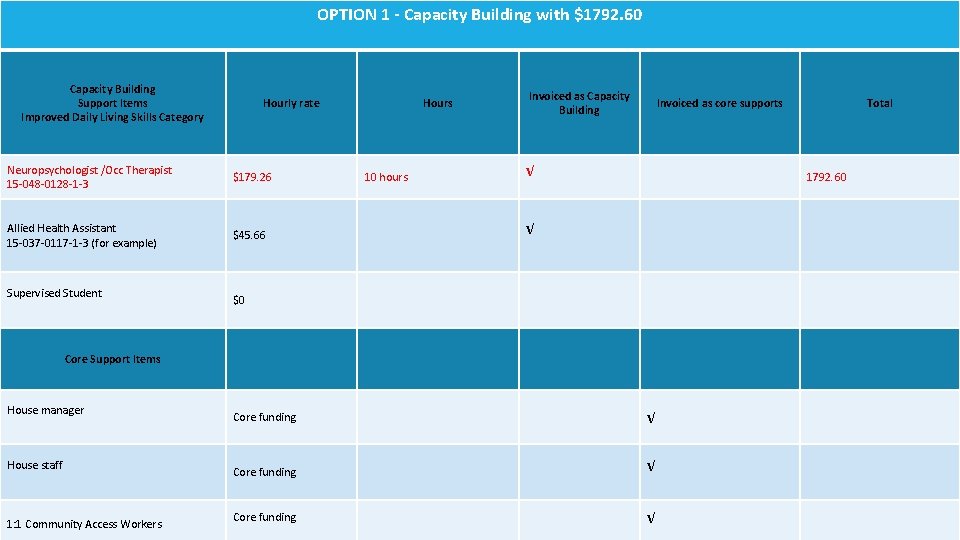
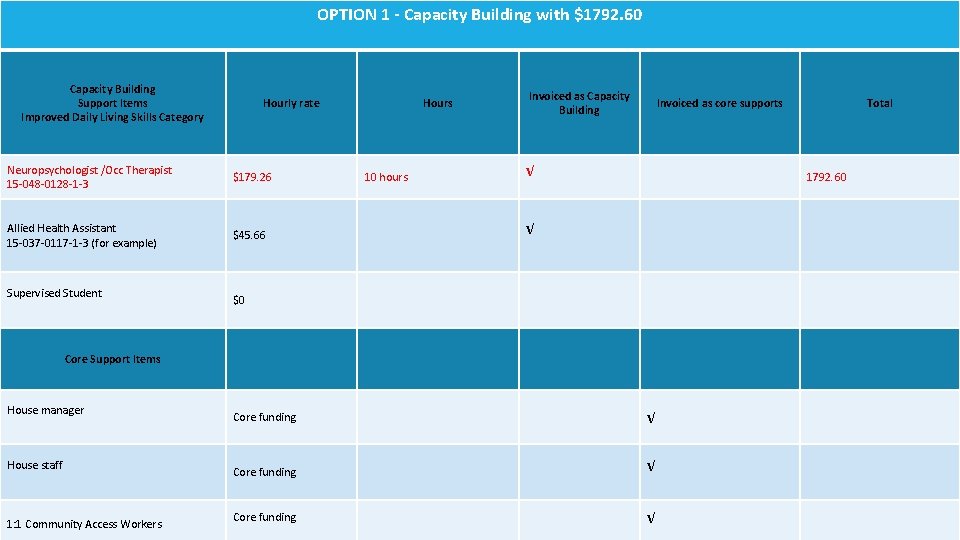
OPTION 1 - Capacity Building with $1792. 60 How to use this 10 hours funding? Capacity Building Support Items Improved Daily Living Skills Category Hourly rate Neuropsychologist /Occ Therapist 15 -048 -0128 -1 -3 $179. 26 Allied Health Assistant 15 -037 -0117 -1 -3 (for example) $45. 66 Supervised Student Hours 10 hours Invoiced as Capacity Building Invoiced as core supports √ 1792. 60 √ $0 Core Support Items House manager House staff 1: 1 Community Access Workers Total Core funding √
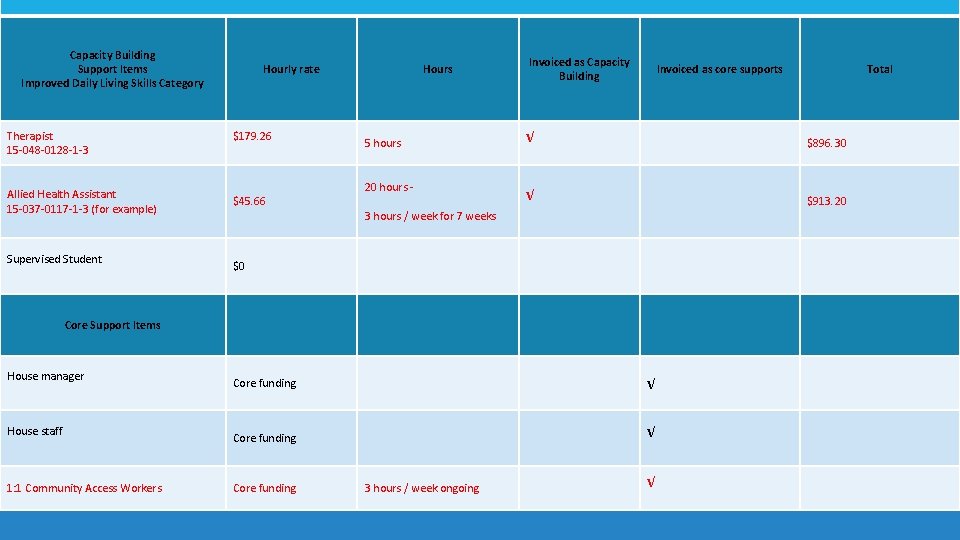
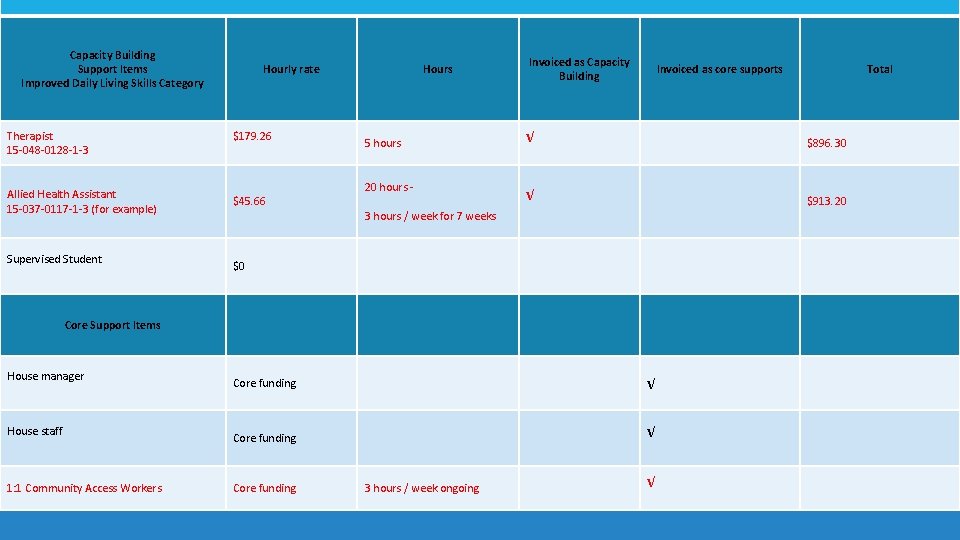
How to use this 10 hours funding? Capacity Building Support Items Improved Daily Living Skills Category Therapist 15 -048 -0128 -1 -3 Allied Health Assistant 15 -037 -0117 -1 -3 (for example) Supervised Student Hourly rate $179. 26 $45. 66 Hours 5 hours 20 hours - Invoiced as Capacity Building Invoiced as core supports √ $896. 30 √ $913. 20 3 hours / week for 7 weeks $0 Core Support Items House manager House staff 1: 1 Community Access Workers Core funding √ Core funding 3 hours / week ongoing Total √
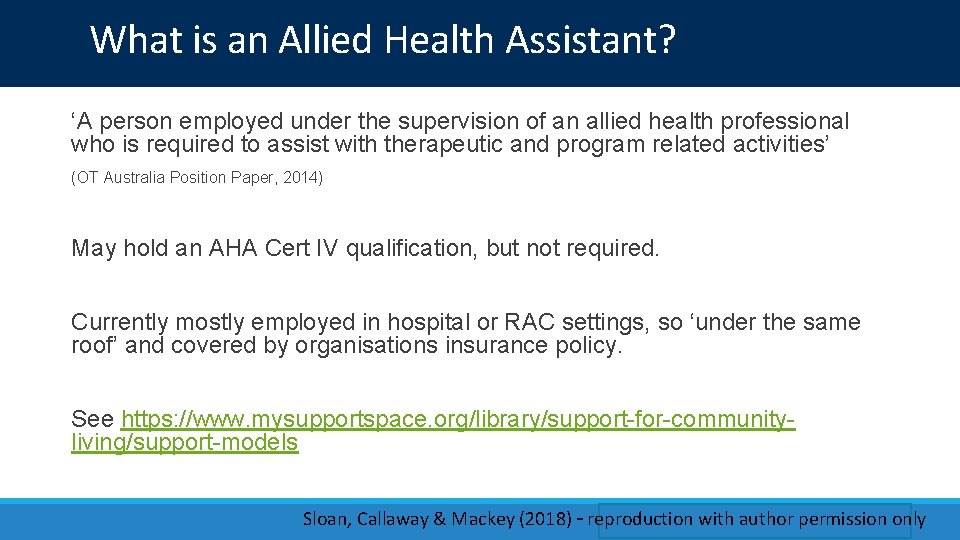
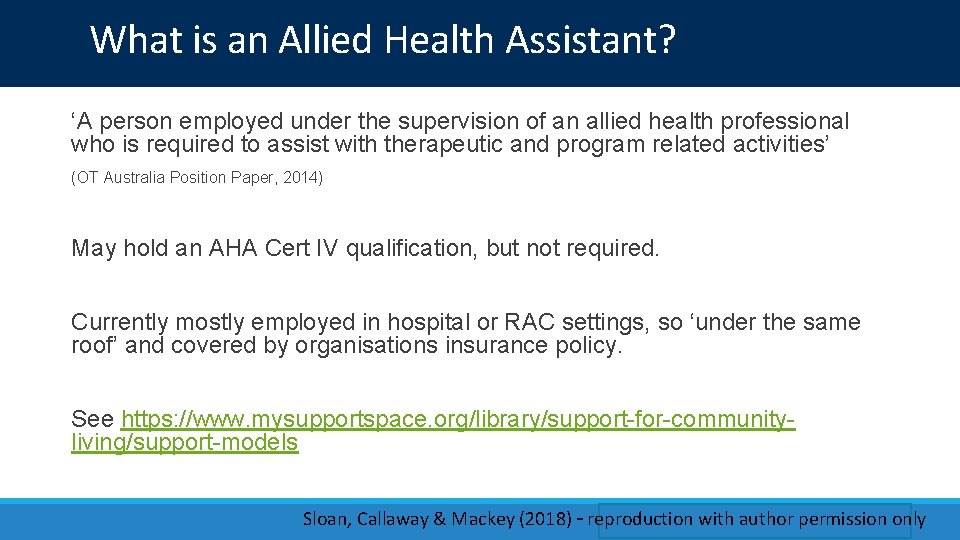
What is an Allied Health Assistant? ‘A person employed under the supervision of an allied health professional who is required to assist with therapeutic and program related activities’ (OT Australia Position Paper, 2014) May hold an AHA Cert IV qualification, but not required. Currently mostly employed in hospital or RAC settings, so ‘under the same roof’ and covered by organisations insurance policy. See https: //www. mysupportspace. org/library/support-for-communityliving/support-models Sloan, Callaway & Mackey (2018) – reproduction with author permission only
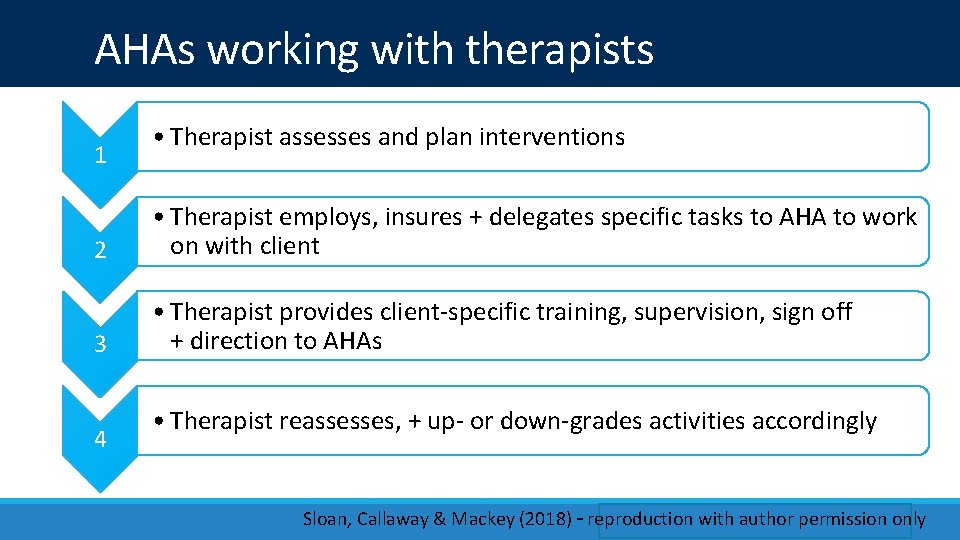
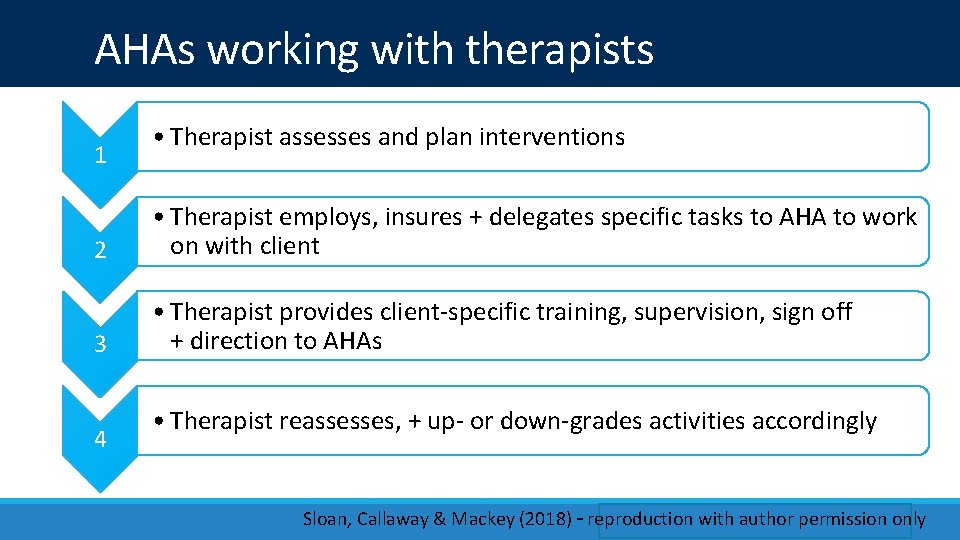
AHAs working with therapists 1 • Therapist assesses and plan interventions 2 • Therapist employs, insures + delegates specific tasks to AHA to work on with client 3 • Therapist provides client-specific training, supervision, sign off + direction to AHAs 4 • Therapist reassesses, + up- or down-grades activities accordingly Sloan, Callaway & Mackey (2018) – reproduction with author permission only
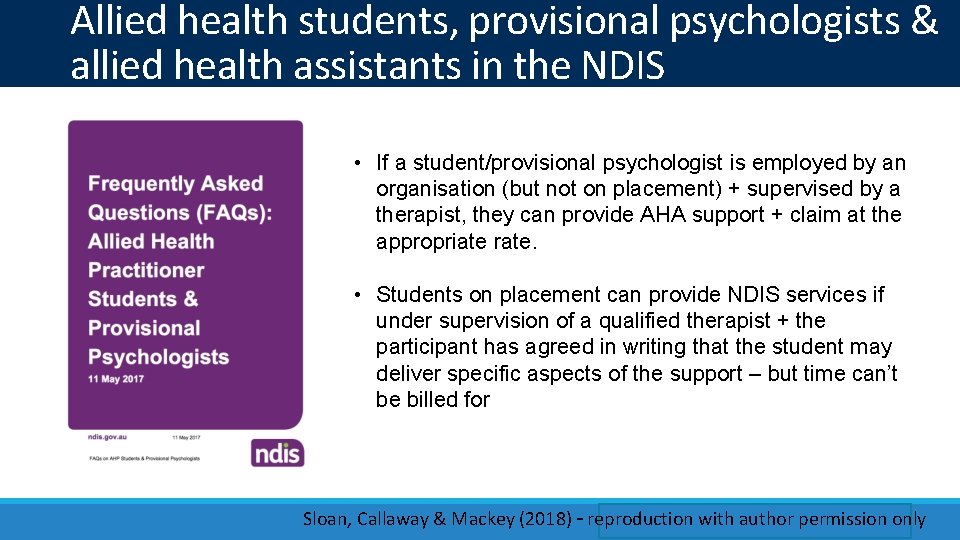
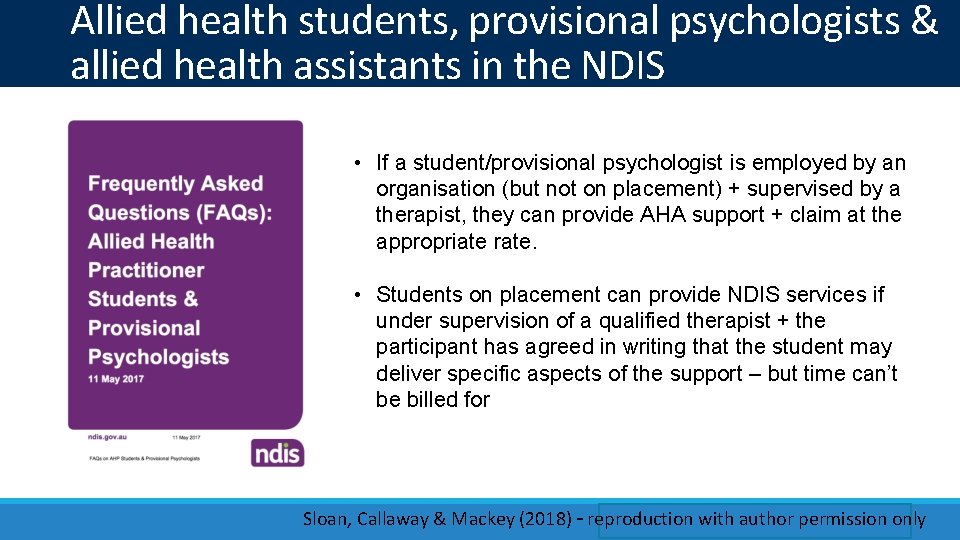
Allied health students, provisional psychologists & allied health assistants in the NDIS • If a student/provisional psychologist is employed by an organisation (but not on placement) + supervised by a therapist, they can provide AHA support + claim at the appropriate rate. • Students on placement can provide NDIS services if under supervision of a qualified therapist + the participant has agreed in writing that the student may deliver specific aspects of the support – but time can’t be billed for Sloan, Callaway & Mackey (2018) – reproduction with author permission only
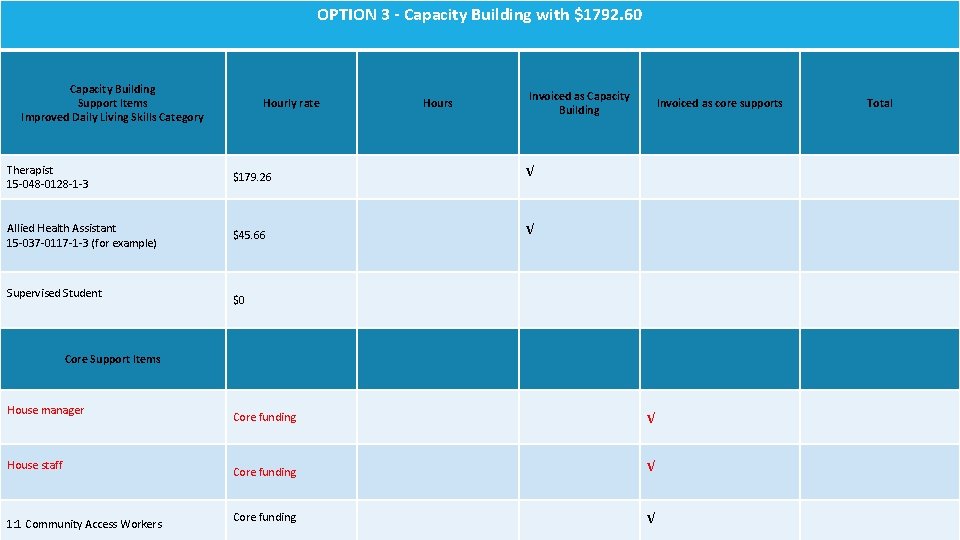
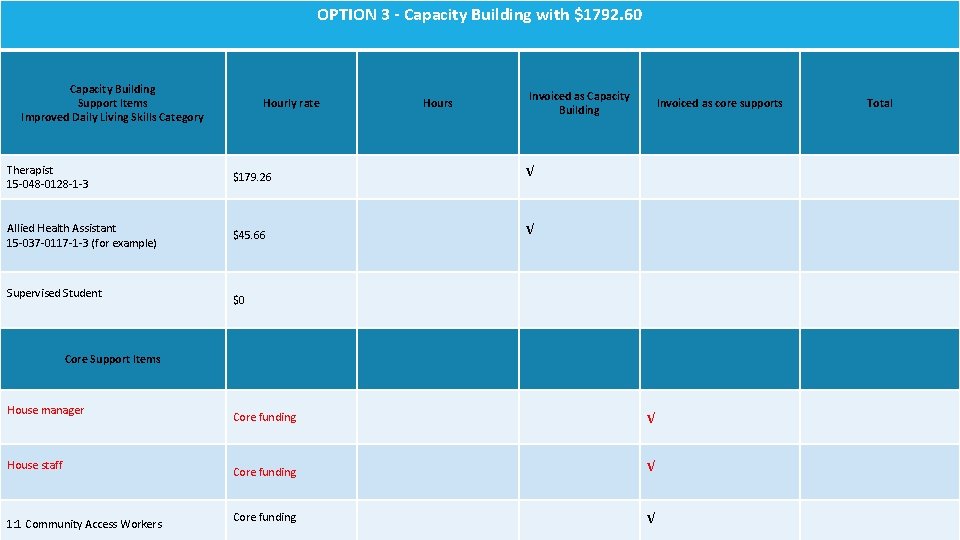
OPTION 3 - Capacity Building with $1792. 60 How to use this 10 hours funding? Capacity Building Support Items Improved Daily Living Skills Category Hourly rate Hours Invoiced as Capacity Building Therapist 15 -048 -0128 -1 -3 $179. 26 √ Allied Health Assistant 15 -037 -0117 -1 -3 (for example) $45. 66 √ Supervised Student Invoiced as core supports $0 Core Support Items House manager House staff 1: 1 Community Access Workers Core funding √ Total
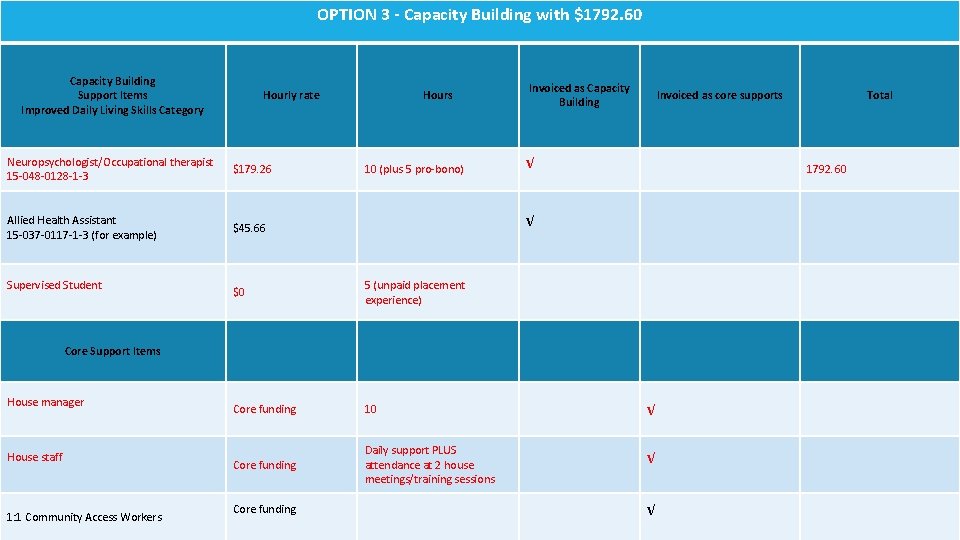
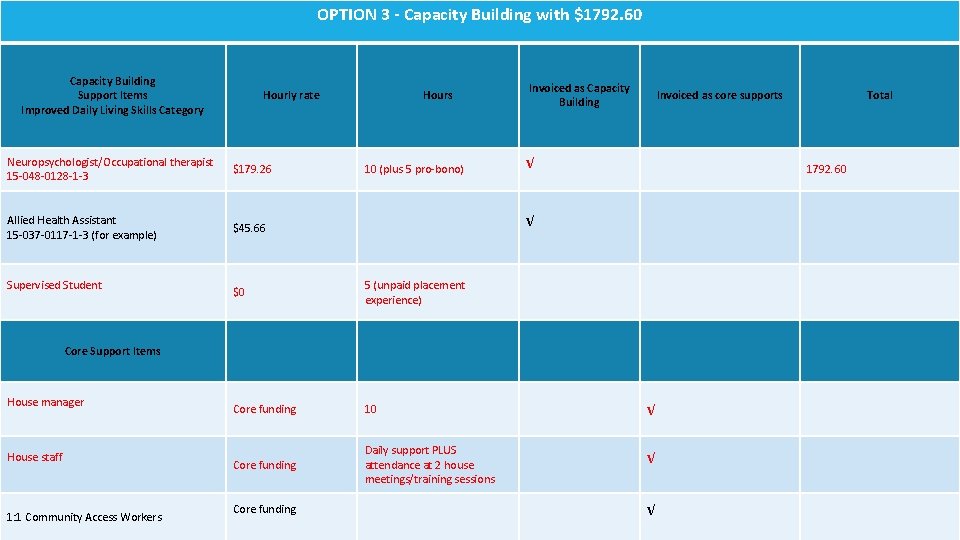
OPTION 3 - Capacity Building with $1792. 60 How to use this 10 hours funding? Capacity Building Support Items Improved Daily Living Skills Category Hourly rate Neuropsychologist/Occupational therapist 15 -048 -0128 -1 -3 $179. 26 Allied Health Assistant 15 -037 -0117 -1 -3 (for example) $45. 66 Supervised Student Hours 10 (plus 5 pro-bono) Invoiced as Capacity Building Invoiced as core supports √ 1792. 60 √ $0 5 (unpaid placement experience) Core funding 10 √ Core funding Daily support PLUS attendance at 2 house meetings/training sessions √ Core Support Items House manager House staff 1: 1 Community Access Workers Core funding Total √
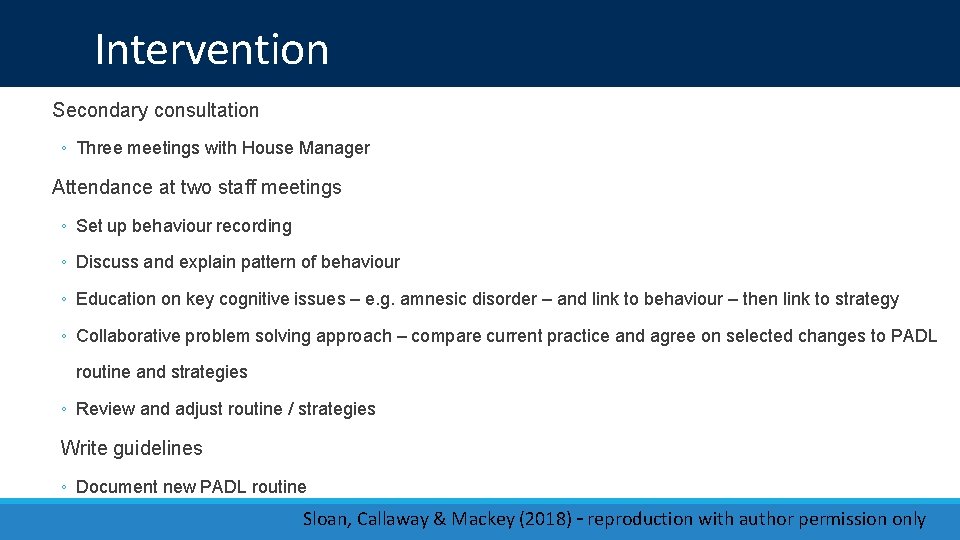
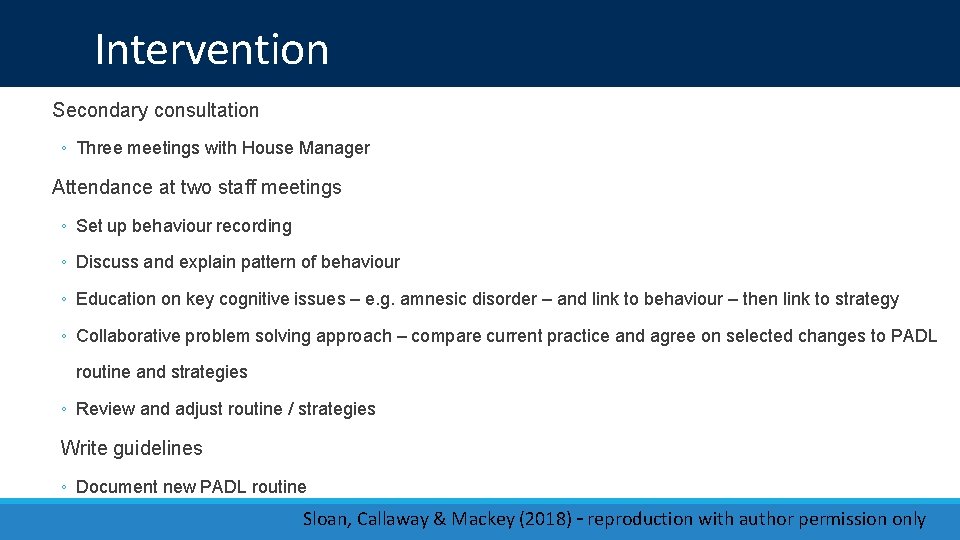
Intervention Secondary consultation ◦ Three meetings with House Manager Attendance at two staff meetings ◦ Set up behaviour recording ◦ Discuss and explain pattern of behaviour ◦ Education on key cognitive issues – e. g. amnesic disorder – and link to behaviour – then link to strategy ◦ Collaborative problem solving approach – compare current practice and agree on selected changes to PADL routine and strategies ◦ Review and adjust routine / strategies Write guidelines ◦ Document new PADL routine Sloan, Callaway & Mackey (2018) – reproduction with author permission only
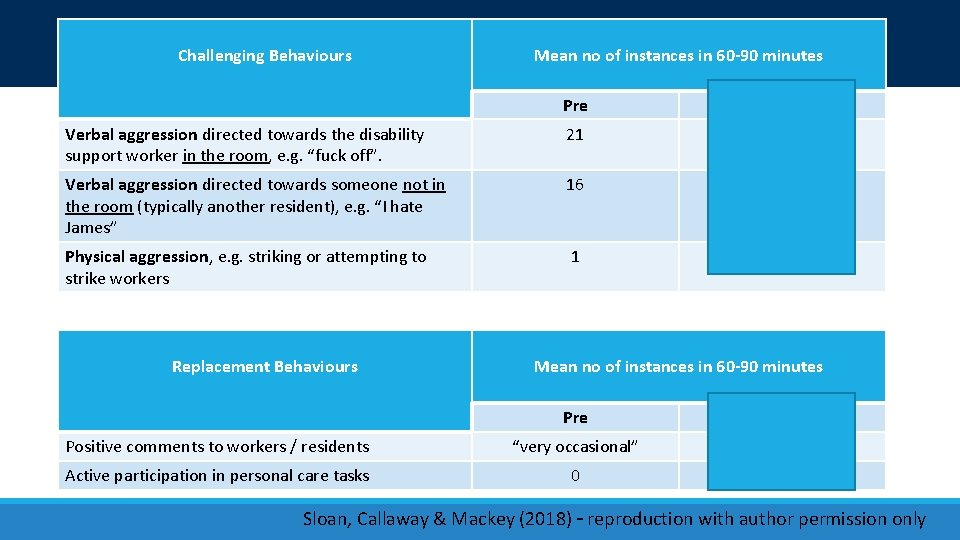
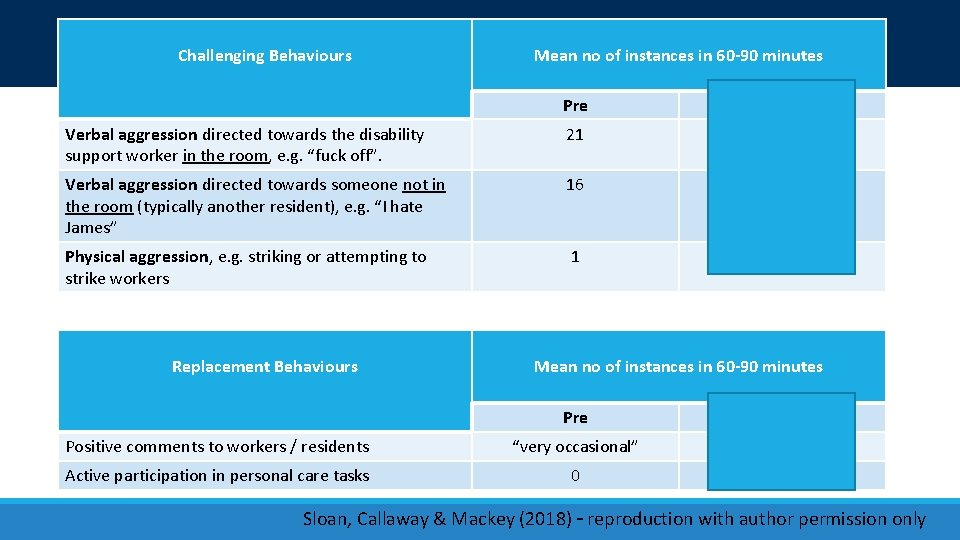
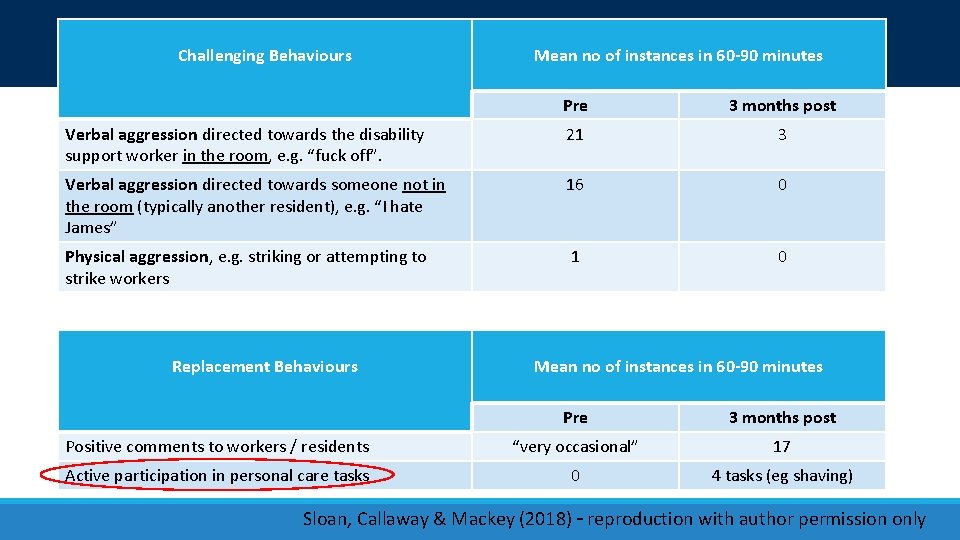
Outcome Challenging Behaviours Mean no of instances in 60 -90 minutes Pre 3 months post Verbal aggression directed towards the disability support worker in the room, e. g. “fuck off”. 21 3 Verbal aggression directed towards someone not in the room (typically another resident), e. g. “I hate James” 16 0 Physical aggression, e. g. striking or attempting to strike workers 1 0 Replacement Behaviours Mean no of instances in 60 -90 minutes Pre 3 months post Positive comments to workers / residents “very occasional” 17 Active participation in personal care tasks 0 4 tasks (eg shaving) Sloan, Callaway & Mackey (2018) – reproduction with author permission only
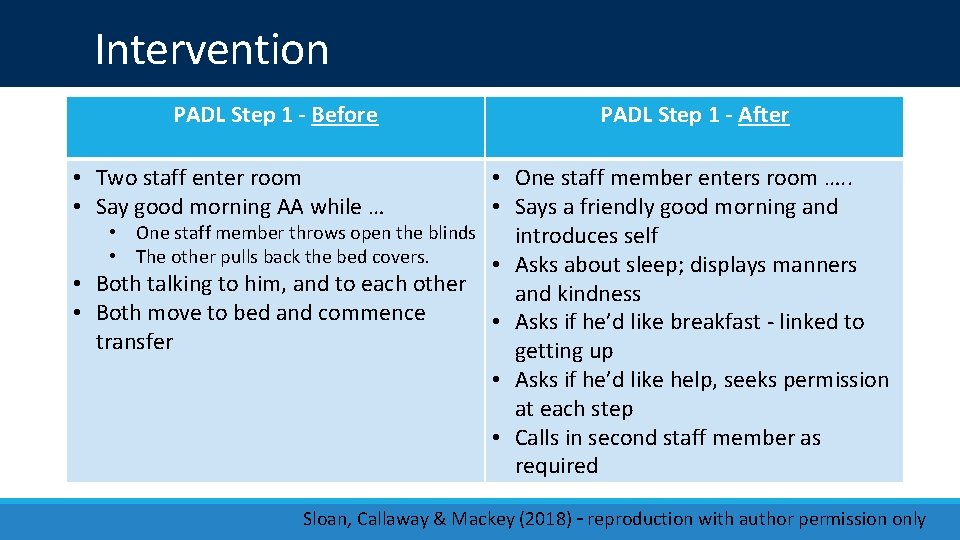
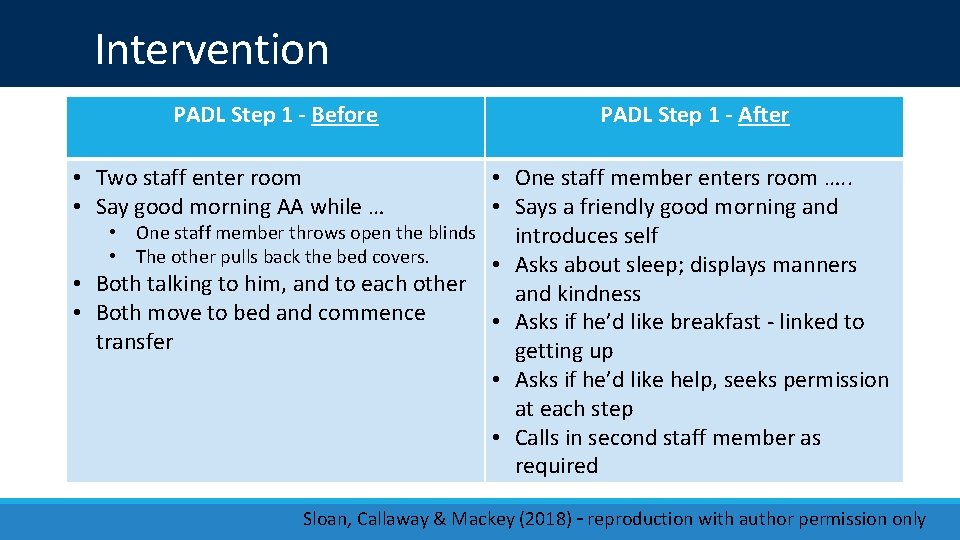
Intervention PADL Step 1 - Before PADL Step 1 - After • Two staff enter room • Say good morning AA while … • One staff member enters room …. . • Says a friendly good morning and • One staff member throws open the blinds introduces self • The other pulls back the bed covers. • Asks about sleep; displays manners • Both talking to him, and to each other and kindness • Both move to bed and commence • Asks if he’d like breakfast - linked to transfer getting up • Asks if he’d like help, seeks permission at each step • Calls in second staff member as required Sloan, Callaway & Mackey (2018) – reproduction with author permission only
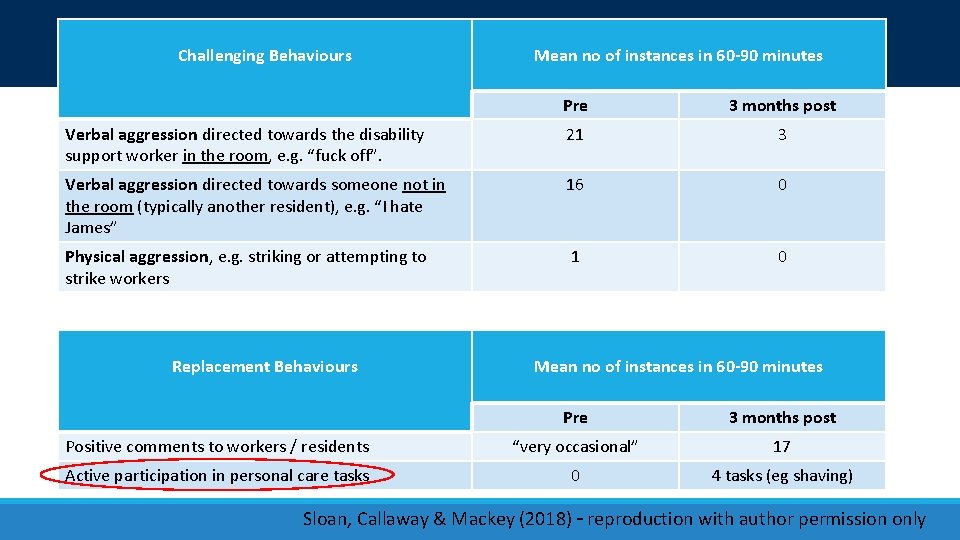
Outcome Challenging Behaviours Mean no of instances in 60 -90 minutes Pre 3 months post Verbal aggression directed towards the disability support worker in the room, e. g. “fuck off”. 21 3 Verbal aggression directed towards someone not in the room (typically another resident), e. g. “I hate James” 16 0 Physical aggression, e. g. striking or attempting to strike workers 1 0 Replacement Behaviours Mean no of instances in 60 -90 minutes Pre 3 months post Positive comments to workers / residents “very occasional” 17 Active participation in personal care tasks 0 4 tasks (eg shaving) Sloan, Callaway & Mackey (2018) – reproduction with author permission only
Conclusion
Conclusion TO BE WRITTEN WITH JAN & SUE Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
Contact details • libby. callaway@monash. edu • sue@osbornsloan. com. au • jan@appliedcommunicationskills. com. au Callaway, Sloan, & Mackey (2019) – reproduction with author permission only
Summary of risks Sue can think of Poor client outcomes due to low level of capacity building and siloed service delivery model (hardly anyone meets as teams any more!). Coupled with over-confidence in DSW ability to deliver outcomes Increased liability in this ‘consumer’ model of service. Blamed/sued/reputational risk when challenging behaviours result in adverse consequences for others eg injury to carer / public Financial risk – not getting paid for services. Plus cost of registration and audits Risk that hours of BS not sufficient given significant requirements and responsibilities on practitioner, esp as the BS practitioner is dealing with two layers of Govt to obtain approval of PBSP, where there is use of RP. Work to reduce RP is intensive and hours may be insufficient Risk that therapist oversight of AHA programs will be diminished eg if DSW agencies “reclassify workers” as AHA. Mitigate risk if AHA employed by therapy practices and overseen by therapists (as per model) Quality and Safeguards Commission – rules on Restrictive Practice – significant outcomes for clinicians not abiding by new rules. On acceptance of referral, often not known if RP in place or will need to be in place. BS clinician responsible for plans and reporting – change from the onus of reporting previously being on the service provider applying the RP Definitional risk of RP – may categorise for eg ‘limit setting’ and ‘routine’ commonly used to manage executive impairment and impulsivity as RP, esp in this current climate of “choice and control” Callaway, Sloan, & Mackey (2019) – reproduction with author permission only