Ideal Practice Workflow Revenue Maximization and Cost Efficiency



- Slides: 16
Ideal Practice Workflow Revenue Maximization and Cost Efficiency Contact us : 2222 Morris Ave. 2 nd Floor, Union, NJ-07083 Ph: (908)-384 -1608 Email: info@clinicspectrum. com

About Us Clinicspectrum is a healthcare services company providing outsourcing/back office and technology solutions for 17+ medical billing companies, 600+ medical groups/healthcare facilities including hospitals, and hospital medical records departments.
Ideal Practice Workflow Patient engagement for financial purposes begins with the CALL FOR APPOINTMENT and continues thereafter until the claim is paid in full. Let's analyze an ideal practice workflow and steps in engaging the patient effectively not only for clinical reasons but for financial reasons as well. Appointment Call Received Back-End Eligibility Verification Team Physician’s Workflow Back-Office/Billing Team . Patient Front Desk Process Patient Engagement by Clinical Assistants Operation Team Clinical Reminder Team

Appointment Call Received When a patient calls to make an appointment, certain key parameters are essential to obtain over the PHONE for the success of an efficient workflow management for clinical and financial planning. Patient’s Name Phone Number Date of Birth Gender Patient’s Insurance name is noted down. Patient’s phone number is noted for future reference Patient’s date of birth is noted. Patient’s gender is recorded.
Eligibility Determination Parameters The below 3 parameters are most essential to obtain over the phone in order to determine eligibility of the patient and define a prelim care plan for the patient at the time of service Patient’s Insurance Name Patient’s name which has been recorded with the insurance. Patient’s Primary Physician Patient’s primary physician if any and reason for visit. Insurance ID Patient’s insurance ID is recorded.
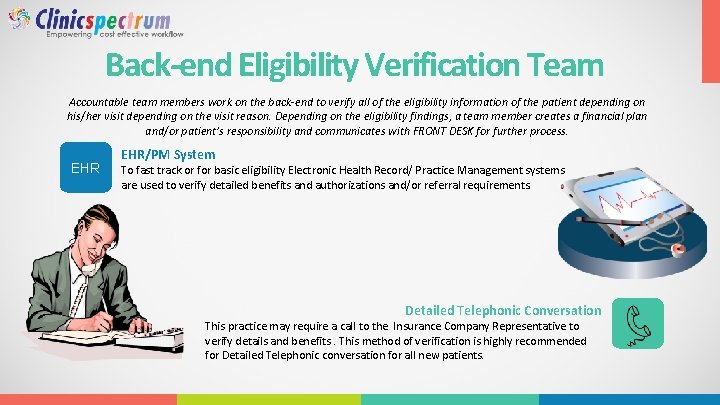
Back-end Eligibility Verification Team Accountable team members work on the back-end to verify all of the eligibility information of the patient depending on his/her visit depending on the visit reason. Depending on the eligibility findings, a team member creates a financial plan and/or patient’s responsibility and communicates with FRONT DESK for further process. EHR/PM System To fast track or for basic eligibility Electronic Health Record/ Practice Management systems are used to verify detailed benefits and authorizations and/or referral requirements. Detailed Telephonic Conversation This practice may require a call to the Insurance Company Representative to verify details and benefits. This method of verification is highly recommended for Detailed Telephonic conversation for all new patients.
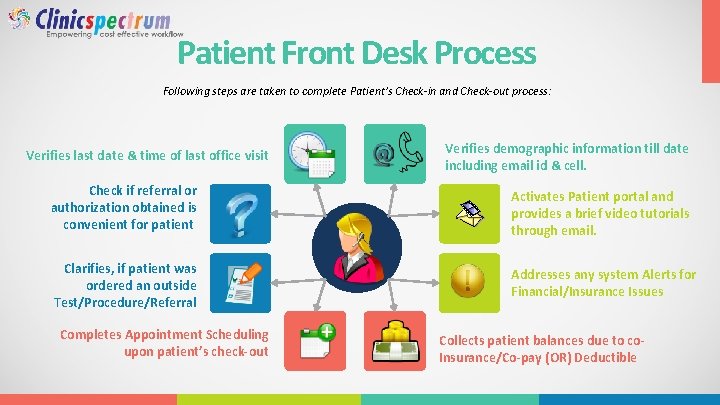
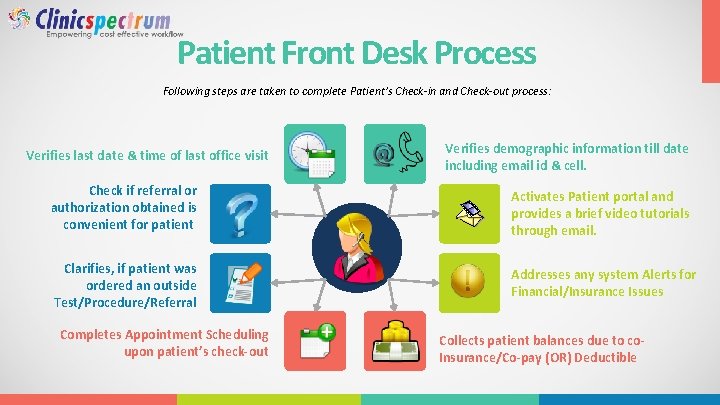
Patient Front Desk Process Following steps are taken to complete Patient’s Check-in and Check-out process: Verifies last date & time of last office visit Verifies demographic information till date including email id & cell. Check if referral or authorization obtained is convenient for patient Activates Patient portal and provides a brief video tutorials through email. Clarifies, if patient was ordered an outside Test/Procedure/Referral Addresses any system Alerts for Financial/Insurance Issues Completes Appointment Scheduling upon patient’s check-out Collects patient balances due to co. Insurance/Co-pay (OR) Deductible
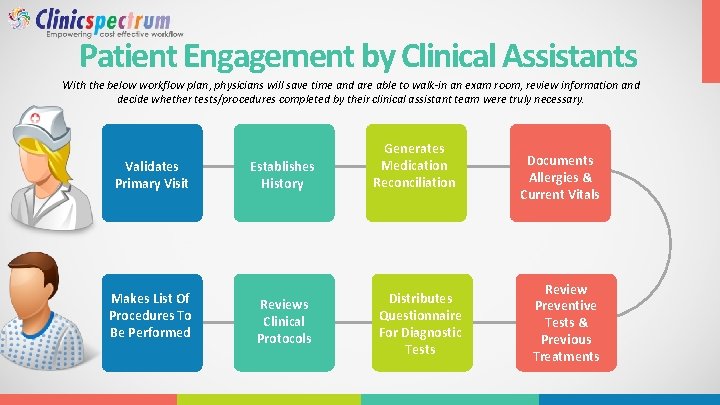
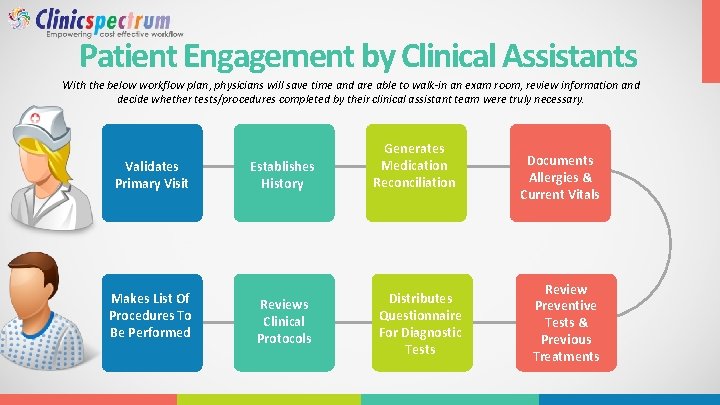
Patient Engagement by Clinical Assistants With the below workflow plan, physicians will save time and are able to walk-in an exam room, review information and decide whether tests/procedures completed by their clinical assistant team were truly necessary. Validates Primary Visit Makes List Of Procedures To Be Performed Establishes History Reviews Clinical Protocols Generates Medication Reconciliation Distributes Questionnaire For Diagnostic Tests Documents Allergies & Current Vitals Review Preventive Tests & Previous Treatments
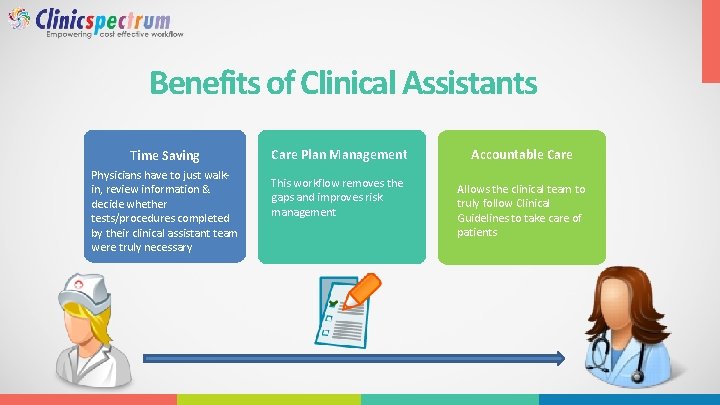
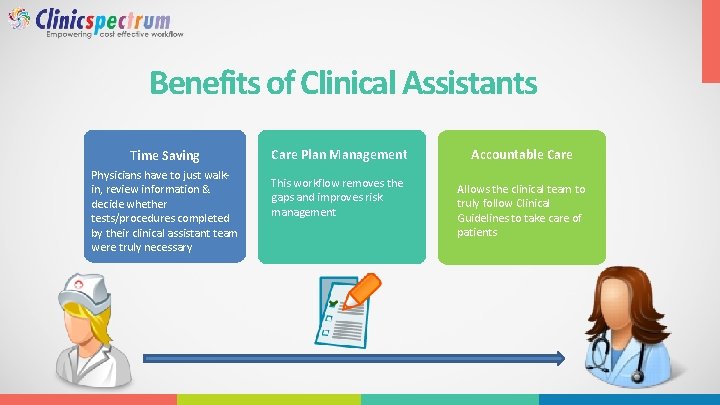
Benefits of Clinical Assistants Time Saving Physicians have to just walkin, review information & decide whether tests/procedures completed by their clinical assistant team were truly necessary Care Plan Management This workflow removes the gaps and improves risk management Accountable Care Allows the clinical team to truly follow Clinical Guidelines to take care of patients
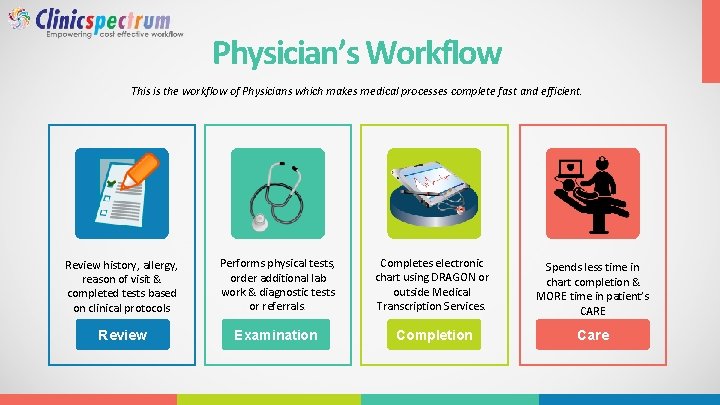
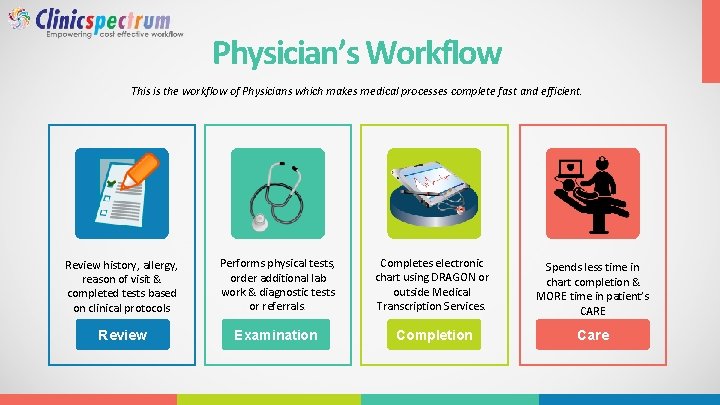
Physician’s Workflow This is the workflow of Physicians which makes medical processes complete fast and efficient. Review history, allergy, reason of visit & completed tests based on clinical protocols Performs physical tests, order additional lab work & diagnostic tests or referrals. Completes electronic chart using DRAGON or outside Medical Transcription Services. Spends less time in chart completion & MORE time in patient’s CARE Review Examination Completion Care
Back-Office/Billing Team ØPhysician sends completed chart and the information for billing and is transferred through Electronic Superbill / Paper Superbill or Autogenerated Claims through an EHR to the billing team. ØBilling team at the Medical Practice submits claims daily in order to forecast daily/weekly cash flow. They maintain a 4 day gap from date of service providing enough time for physicians to finish charts, however the cycle of billing must be kept intact.

m mu Co m de mu nica ti qu duct nica est ible te ng ion / wit na coo h p ire rd at se ina ien nt tio ts' by n o fo r he alt f ben high h p ef lan its / s. cli nic al Co Work on Denials within 72 hours & keep them in queue f or follow up in 6 -7 weeks. Managing Denials um re he (t m ini m e vic ). r e e f s rvic o ay of se r d t fo i 1 a e t w as tim n't ctions o D t le om a ll ts. r a s fr ien uire a t o a f q y r p ily da n y o sing re r a a o i d o d w con aily cl iss aims of fe e s d , to bm cl p ces month n a Su bmit be ga l he ba bill d of t Su uld d n n co ts a the e n g e ym tin s at Pos daily patement a t it Pos ing st with d sen ciated o ass Auditing Billing Team Monthly Audit team performing audit on OUTSTANDING Primary claims and creating an action plan for follow up. important to follow up on OUTSTANDING claims once in 6 weeks for optimum cash flow.
Operation Team Identify use of Technology/Outsourcing Cost Reduction Plans Discussed Monthly meetings are conducted to find available options to reduce operational costs through Automation or Outsourcing Services.
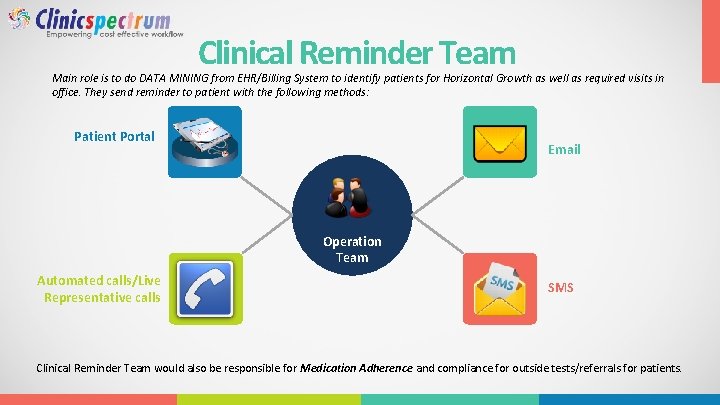
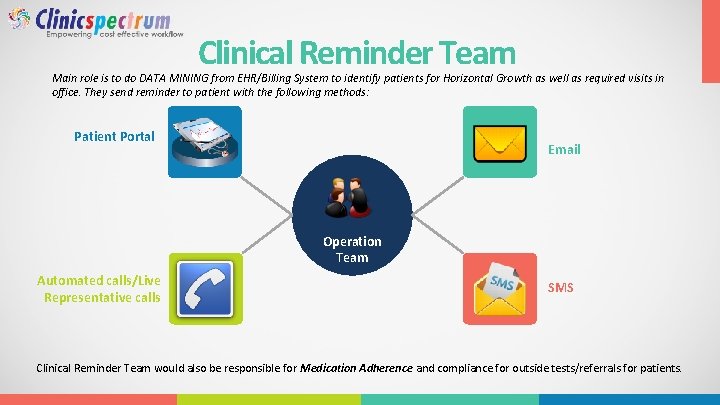
Clinical Reminder Team Main role is to do DATA MINING from EHR/Billing System to identify patients for Horizontal Growth as well as required visits in office. They send reminder to patient with the following methods: Patient Portal Email Operation Team Automated calls/Live Representative calls SMS Clinical Reminder Team would also be responsible for Medication Adherence and compliance for outside tests/referrals for patients.
This workflow plan takes a practice to next level in REVENUE / COST / RISK Management and make them truly accountable in care. REVENUE RISK COST
Contact Us 2222 Morris Ave. 2 nd Floor, Union, NJ-07083 Website http: //clinicspectrum. com/ Phone Number 908. 834. 1608 Email info@Clinicspectrum. com Clinicspectrum is a healthcare services company providing outsourcing and back office solutions for medical billing companies, medical offices, hospital billing departments, and hospital medical records departments.