ICU Key Performance Indicators MOH Journey Towards Standardization
- Slides: 38
ICU Key Performance Indicators: MOH Journey Towards Standardization of Care Zohair Al Aseri, MD, FRCPC, FCEM
ICU Key Performance Indicators: MOH Journey Towards Standardization of Care Objectives 1. Introduction 2. KPI Accuracy & challenges 3. Ongoing projects 1. Clinical Outcome KPI 2. Structural & Process KPI 3. Quality projects NASAM 4. Future and Plan 5. Q & A
ICU Key Performance Indicators: MOH Journey Towards Standardization of Care Pros: Benchmarking against other ICUs: • Provide ICU staff and hospital managers with a broader view. • Clearer perspectives of targets for improvement. Cons: Self-reflection can lead to excessive optimism or criticism. What should we benchmark? ? ? What you measure is not nearly as important as what you do with what you measure Gordon D. Rubenfeld, MD MSc Professor of Medicine, University of Toronto Chief, Program in Trauma, Emergency, and Critical Care Sunnybrook Health Sciences Centre
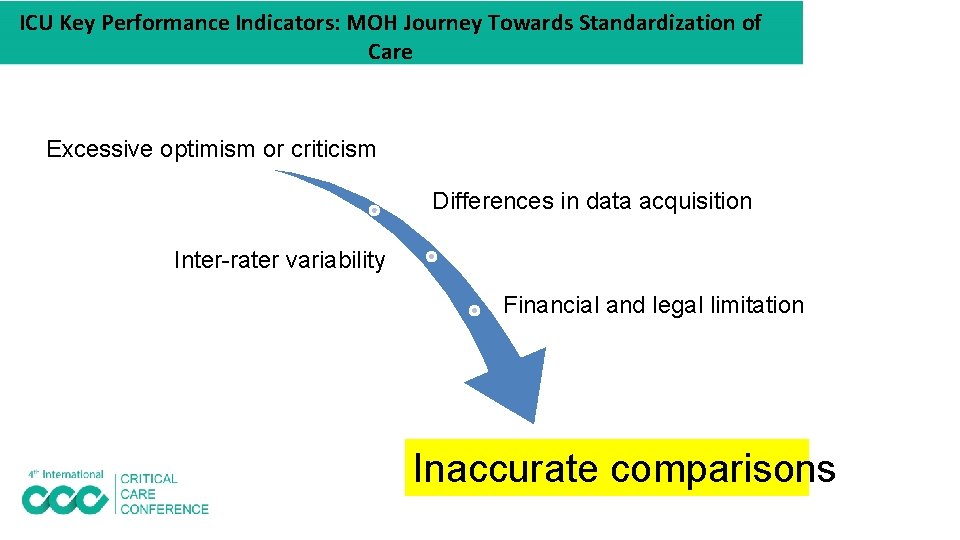
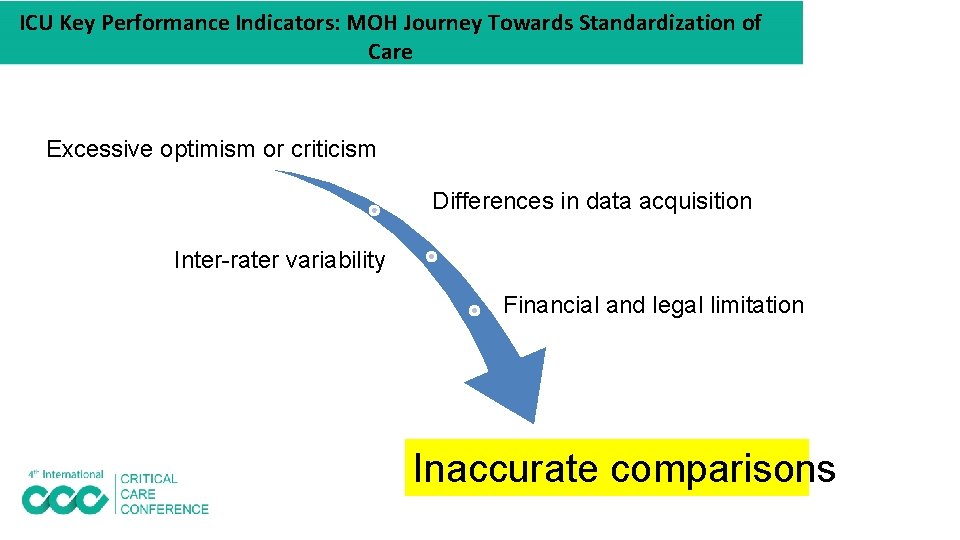
ICU Key Performance Indicators: MOH Journey Towards Standardization of Care Excessive optimism or criticism Differences in data acquisition Inter-rater variability Financial and legal limitation Inaccurate comparisons
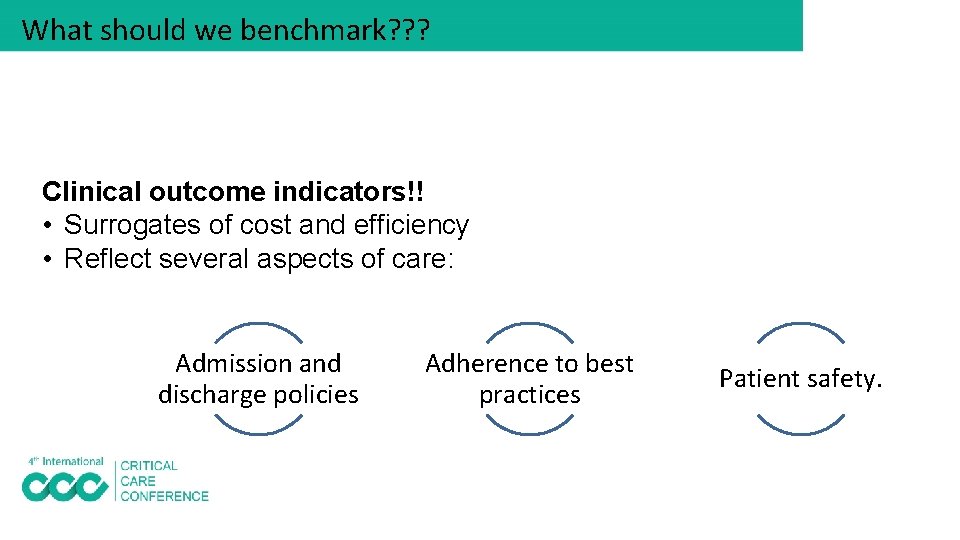
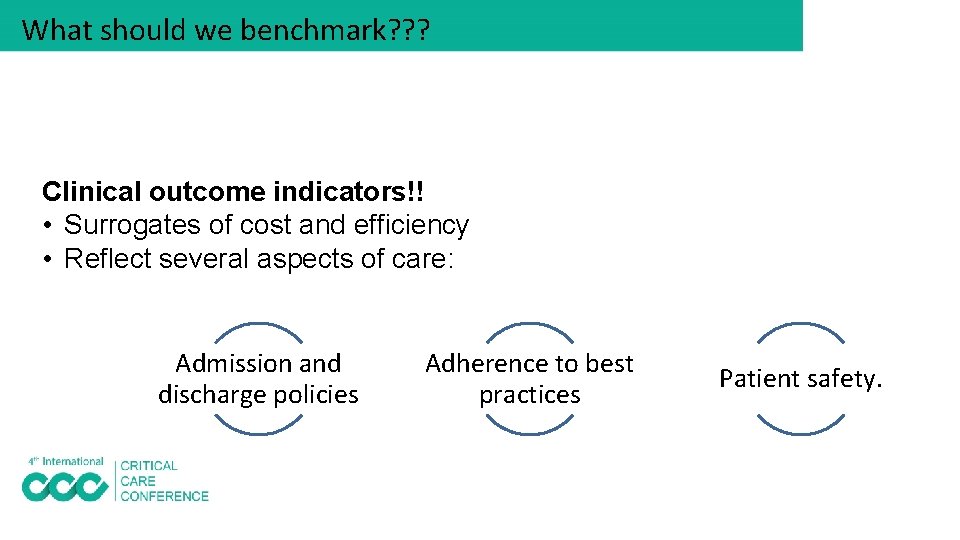
What should we benchmark? ? ? Clinical outcome indicators!! • Surrogates of cost and efficiency • Reflect several aspects of care: Admission and discharge policies Adherence to best practices Patient safety.
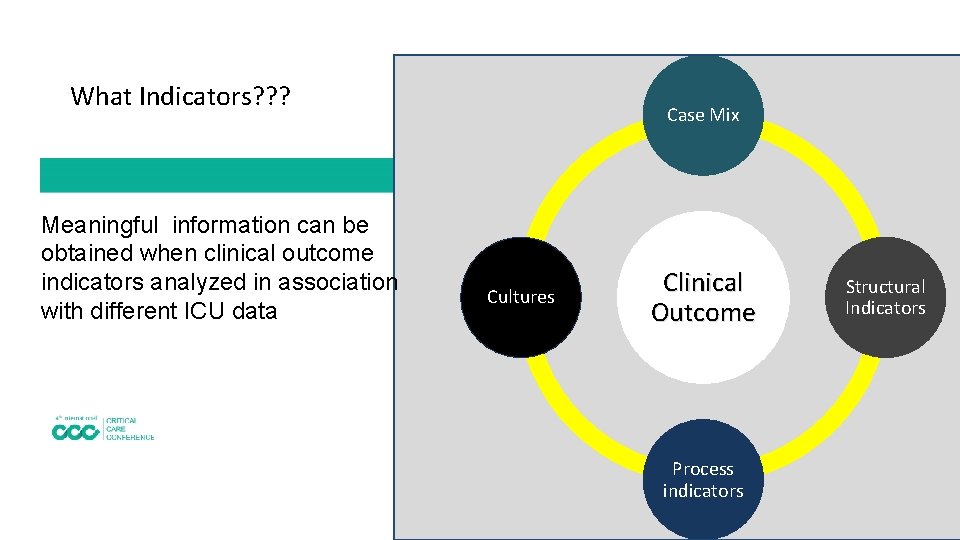
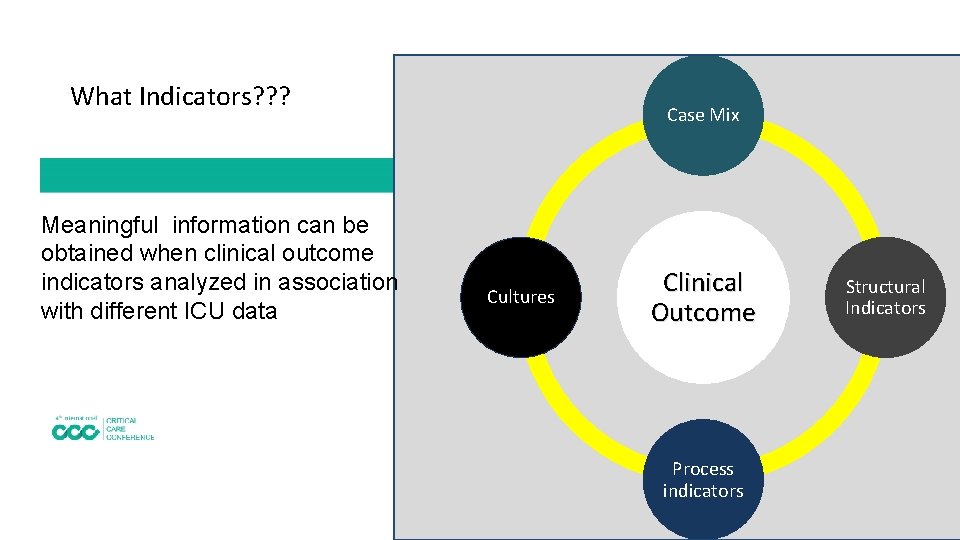
What Indicators? ? ? Meaningful information can be obtained when clinical outcome indicators analyzed in association with different ICU data Case Mix Cultures Clinical Outcome Process indicators Structural Indicators
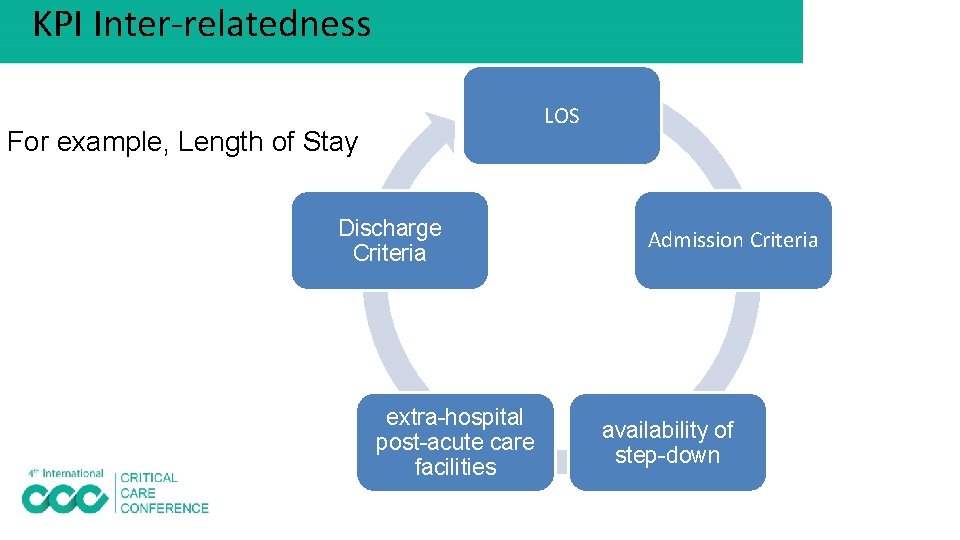
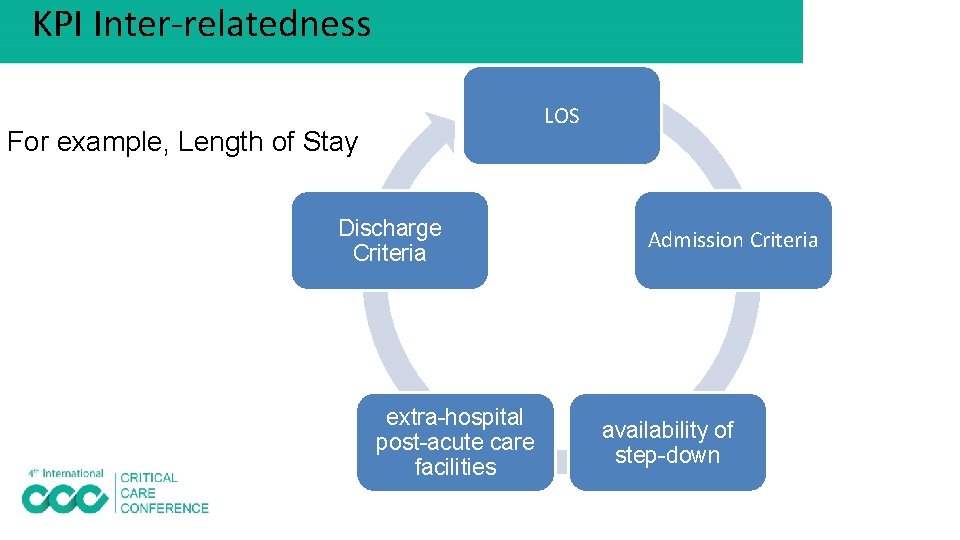
KPI Inter-relatedness LOS For example, Length of Stay Discharge Criteria extra-hospital post-acute care facilities Admission Criteria availability of step-down
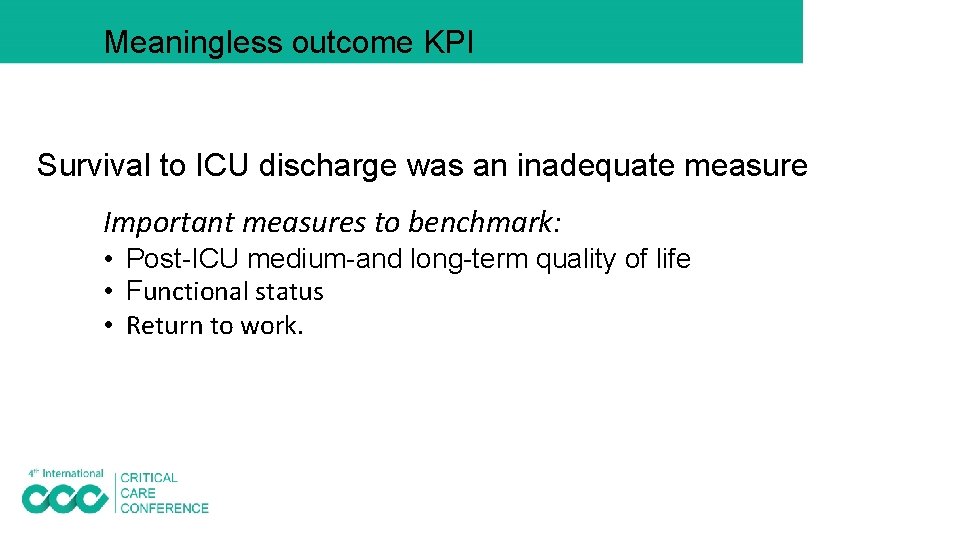
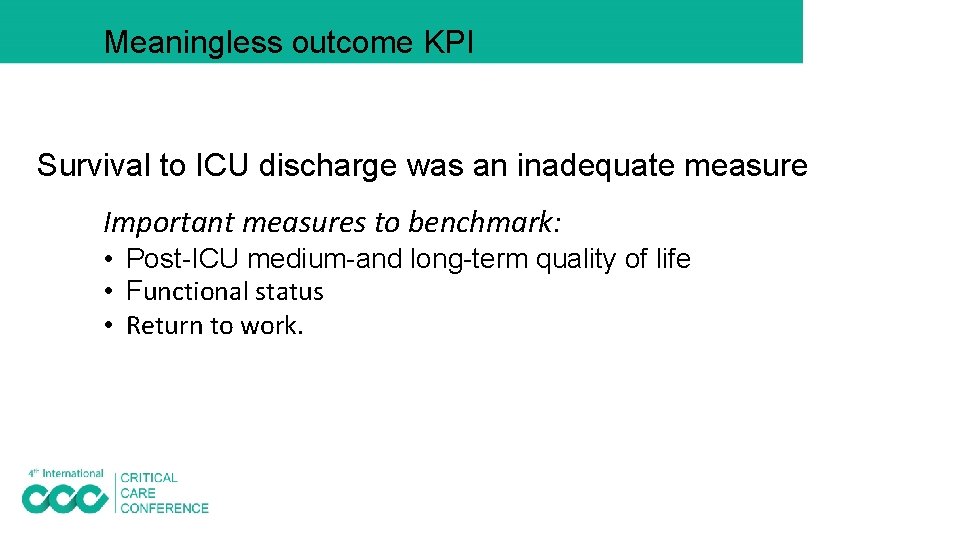
Meaningless outcome KPI Survival to ICU discharge was an inadequate measure Important measures to benchmark: • Post-ICU medium-and long-term quality of life • Functional status • Return to work.
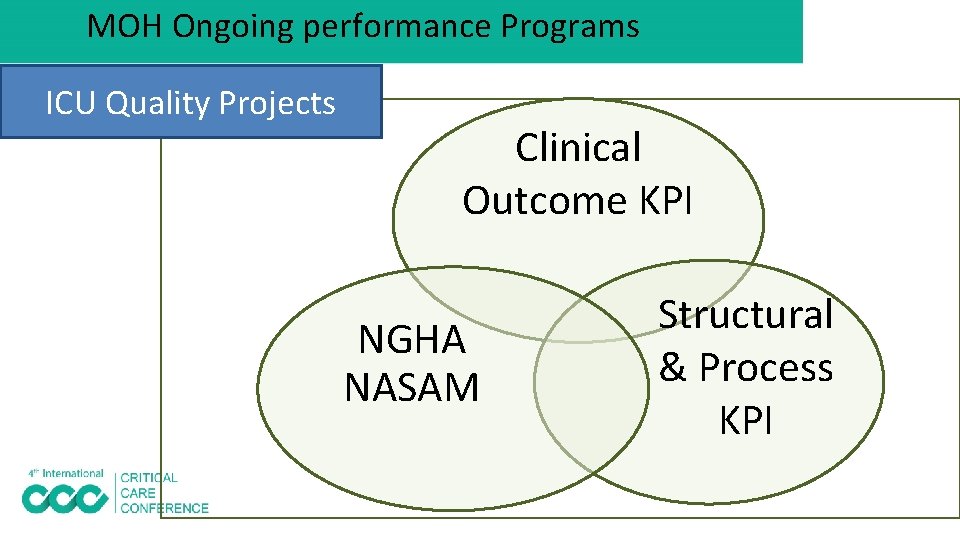
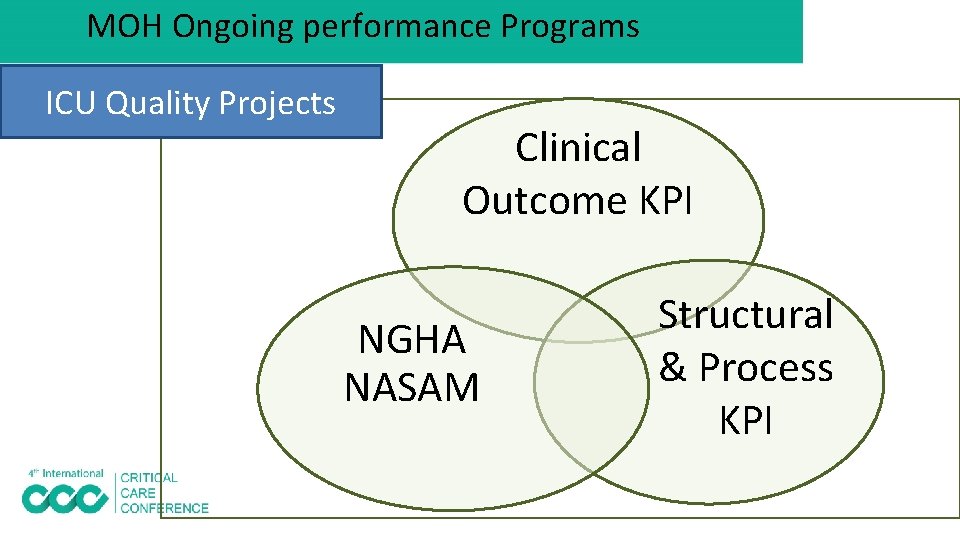
MOH Ongoing performance Programs ICU Quality Projects Clinical Outcome KPI NGHA NASAM Structural & Process KPI
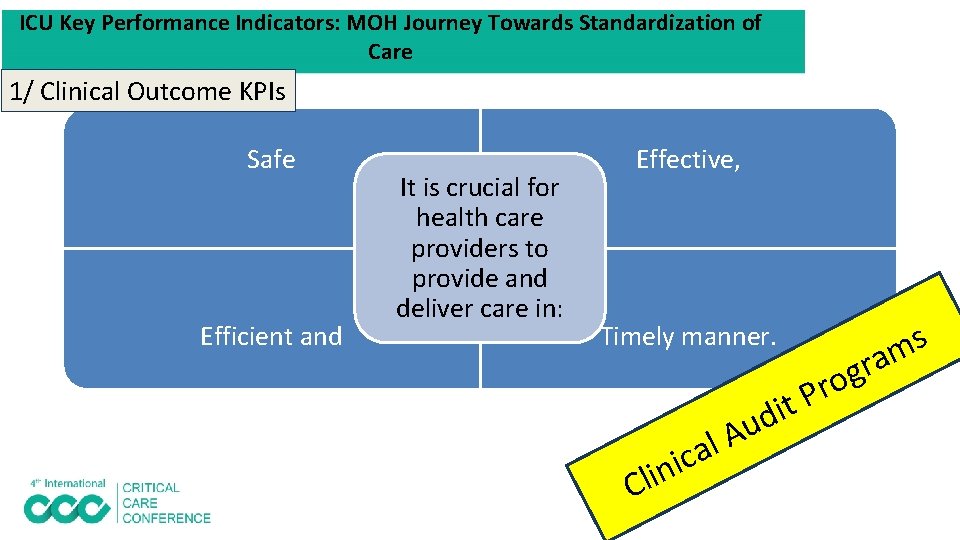
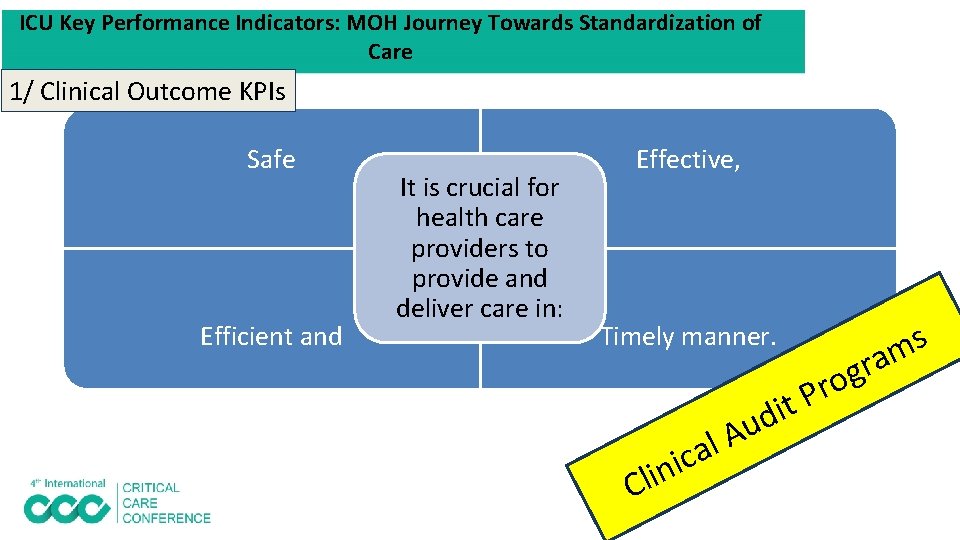
ICU Key Performance Indicators: MOH Journey Towards Standardization of Care 1/ Clinical Outcome KPIs Safe Efficient and It is crucial for health care providers to provide and deliver care in: Effective, Timely manner. i n i Cl A l ca g o r P t i d u s m ra
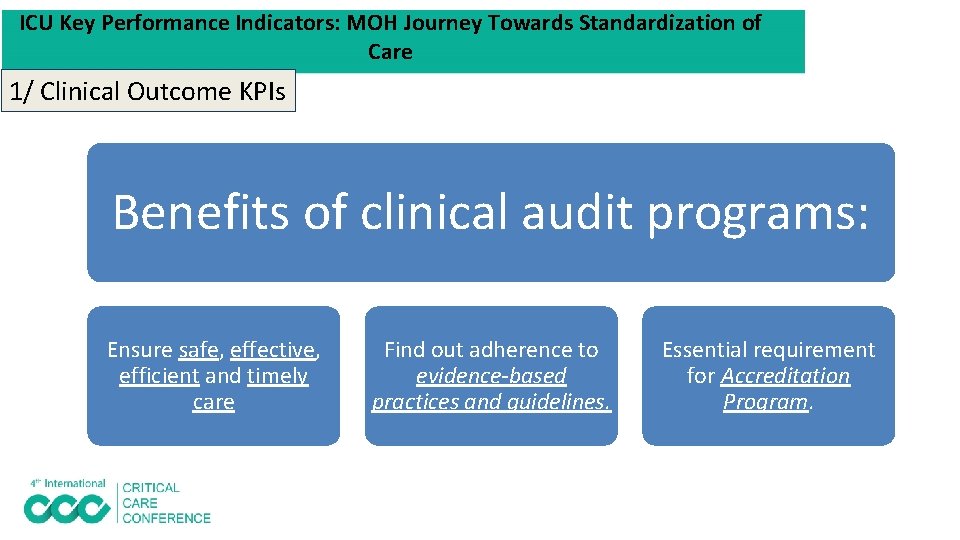
ICU Key Performance Indicators: MOH Journey Towards Standardization of Care 1/ Clinical Outcome KPIs Benefits of clinical audit programs: Ensure safe, effective, efficient and timely care Find out adherence to evidence-based practices and guidelines. Essential requirement for Accreditation Program.
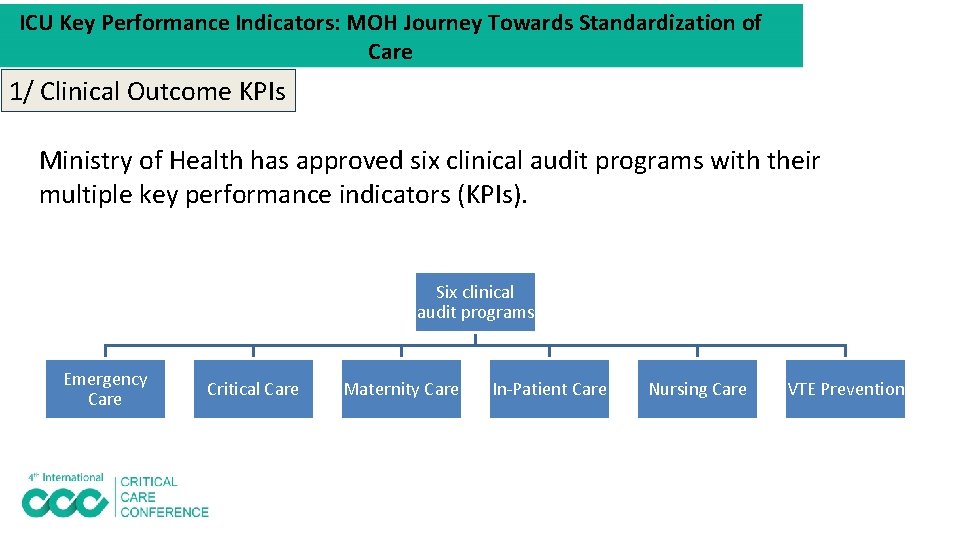
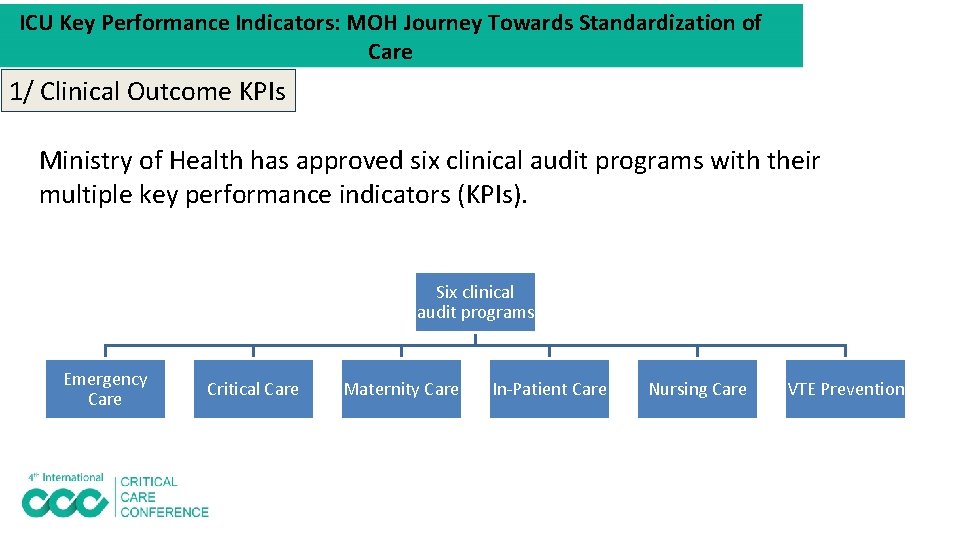
ICU Key Performance Indicators: MOH Journey Towards Standardization of Care 1/ Clinical Outcome KPIs Ministry of Health has approved six clinical audit programs with their multiple key performance indicators (KPIs). Six clinical audit programs Emergency Care Critical Care Maternity Care In-Patient Care Nursing Care VTE Prevention
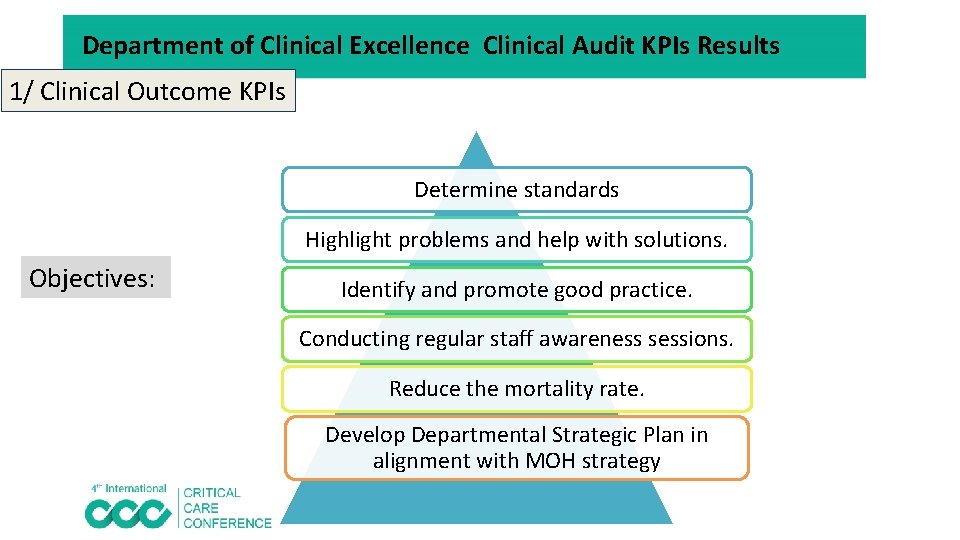
Department of Clinical Excellence Clinical Audit KPIs Results 1/ Clinical Outcome KPIs Determine standards Highlight problems and help with solutions. Objectives: Identify and promote good practice. Conducting regular staff awareness sessions. Reduce the mortality rate. Develop Departmental Strategic Plan in alignment with MOH strategy
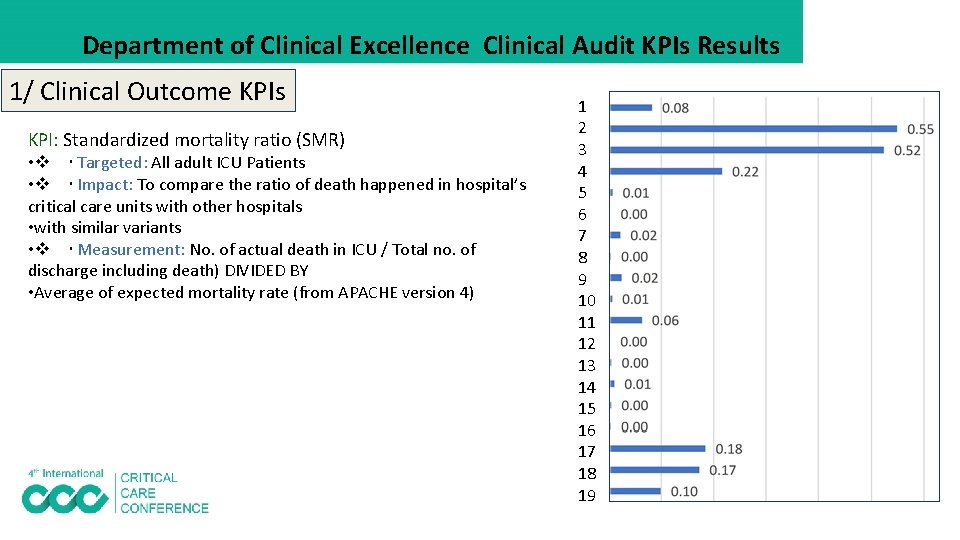
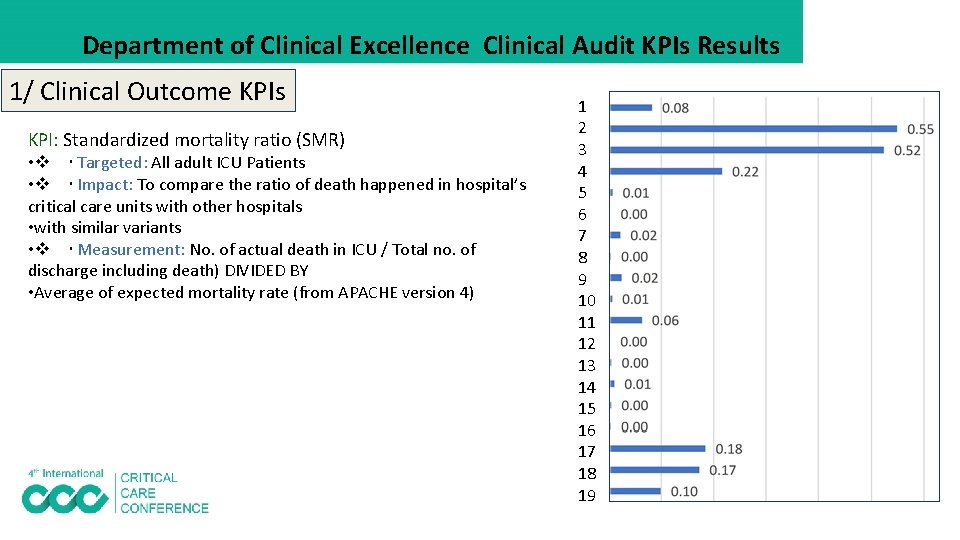
Department of Clinical Excellence Clinical Audit KPIs Results 1/ Clinical Outcome KPIs KPI: Standardized mortality ratio (SMR) • Targeted: All adult ICU Patients • Impact: To compare the ratio of death happened in hospital’s critical care units with other hospitals • with similar variants • Measurement: No. of actual death in ICU / Total no. of discharge including death) DIVIDED BY • Average of expected mortality rate (from APACHE version 4) 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19
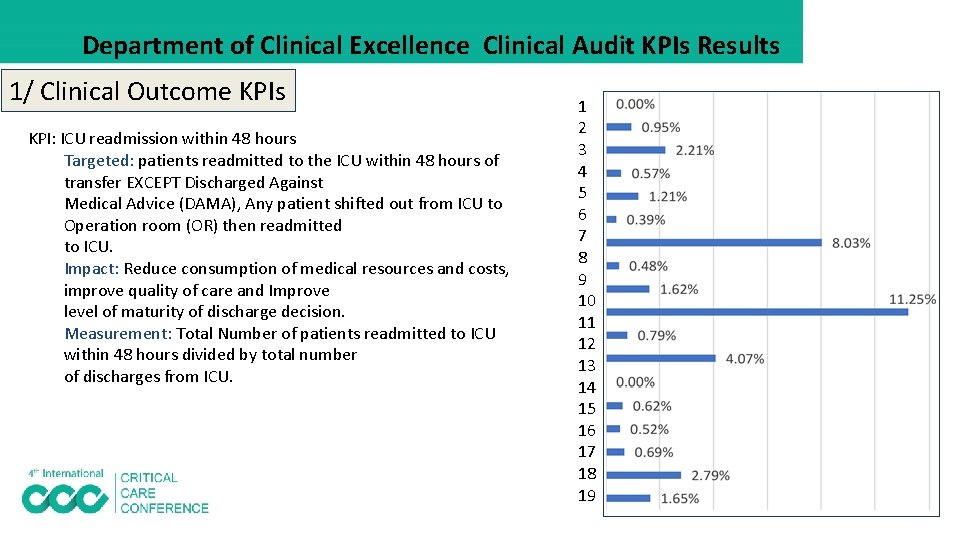
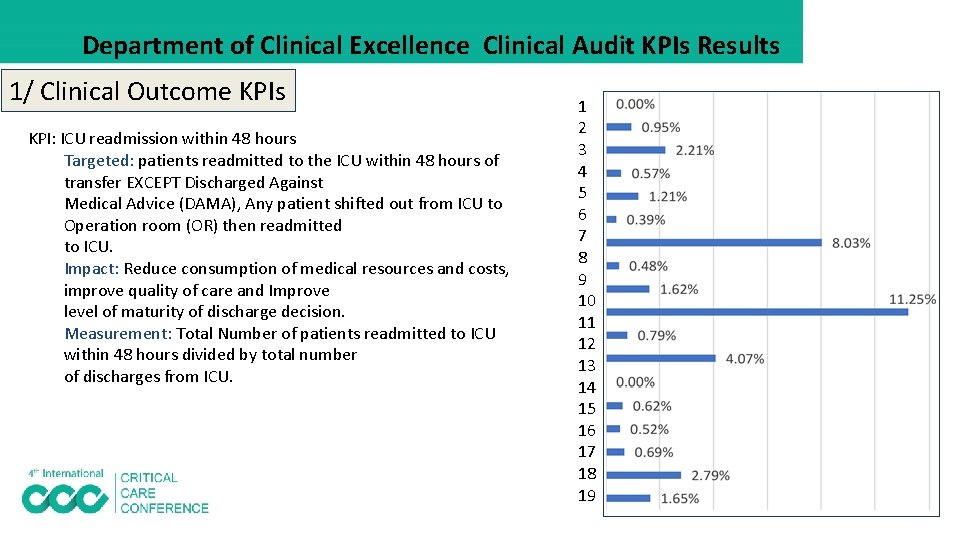
Department of Clinical Excellence Clinical Audit KPIs Results 1/ Clinical Outcome KPIs KPI: ICU readmission within 48 hours Targeted: patients readmitted to the ICU within 48 hours of transfer EXCEPT Discharged Against Medical Advice (DAMA), Any patient shifted out from ICU to Operation room (OR) then readmitted to ICU. Impact: Reduce consumption of medical resources and costs, improve quality of care and Improve level of maturity of discharge decision. Measurement: Total Number of patients readmitted to ICU within 48 hours divided by total number of discharges from ICU. 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19
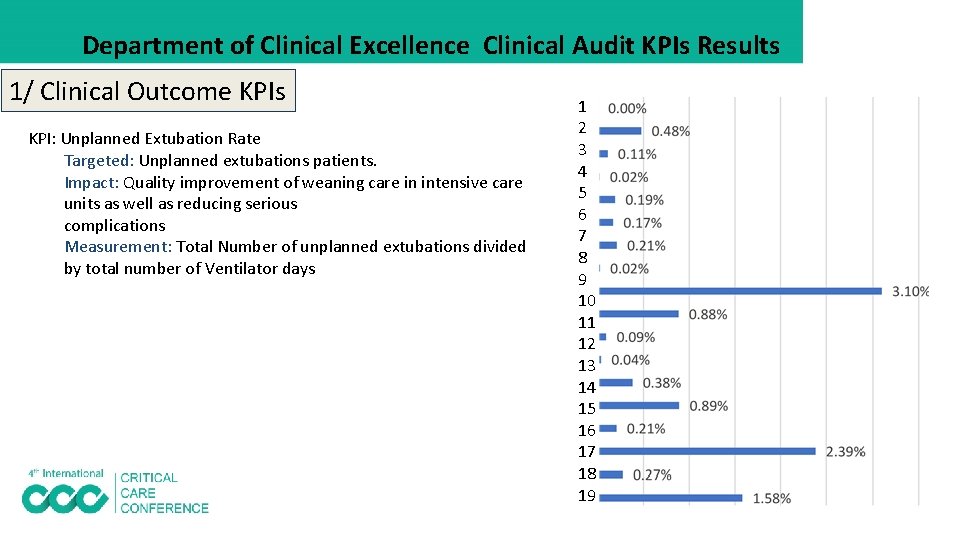
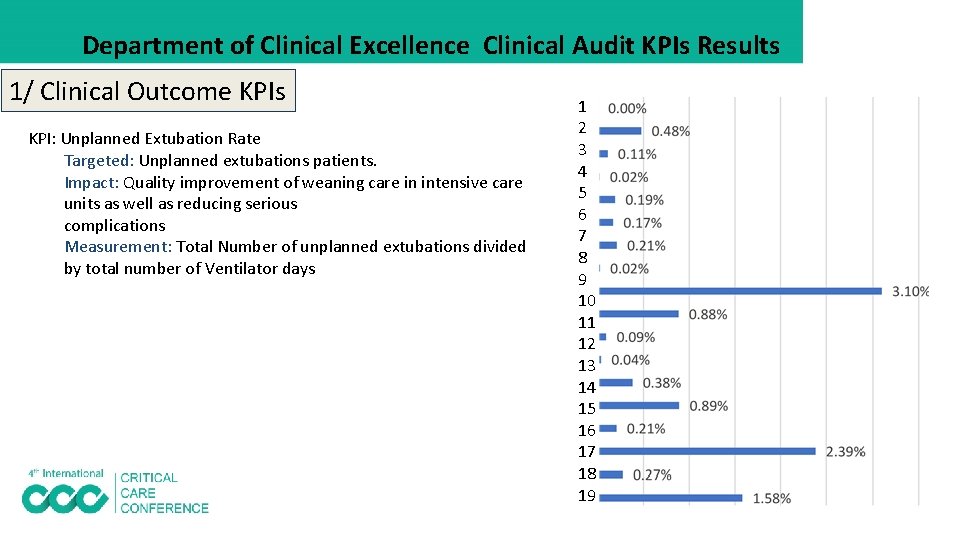
Department of Clinical Excellence Clinical Audit KPIs Results 1/ Clinical Outcome KPIs KPI: Unplanned Extubation Rate Targeted: Unplanned extubations patients. Impact: Quality improvement of weaning care in intensive care units as well as reducing serious complications Measurement: Total Number of unplanned extubations divided by total number of Ventilator days 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19
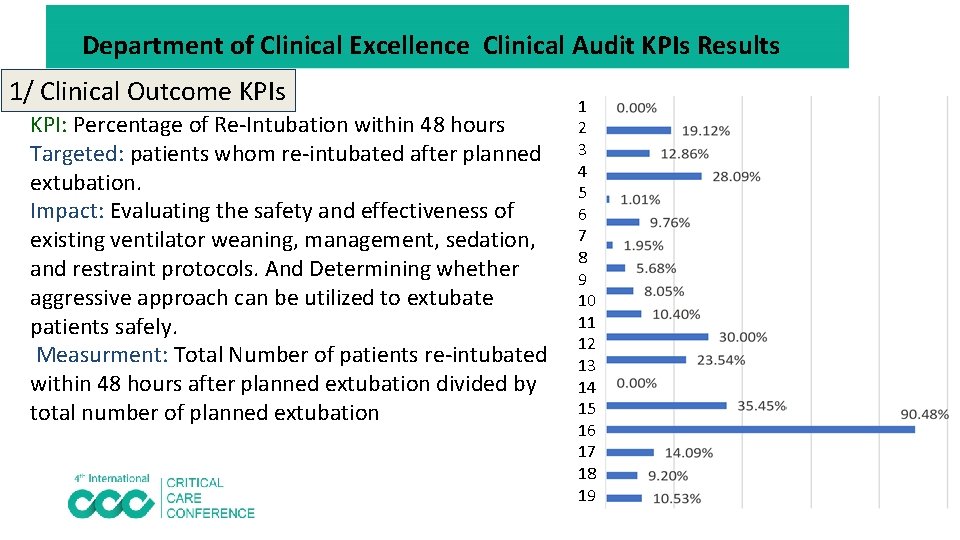
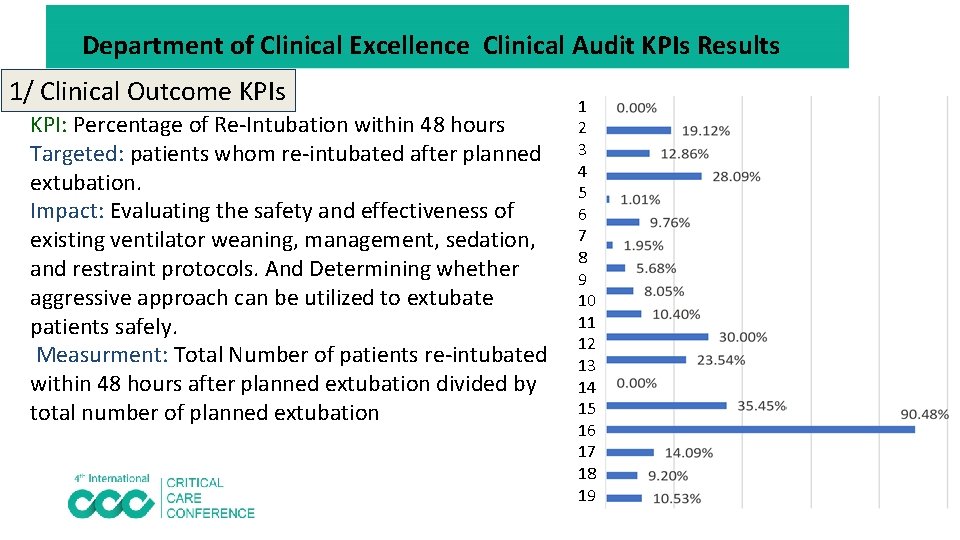
Department of Clinical Excellence Clinical Audit KPIs Results 1/ Clinical Outcome KPIs KPI: Percentage of Re-Intubation within 48 hours Targeted: patients whom re-intubated after planned extubation. Impact: Evaluating the safety and effectiveness of existing ventilator weaning, management, sedation, and restraint protocols. And Determining whether aggressive approach can be utilized to extubate patients safely. Measurment: Total Number of patients re-intubated within 48 hours after planned extubation divided by total number of planned extubation 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19
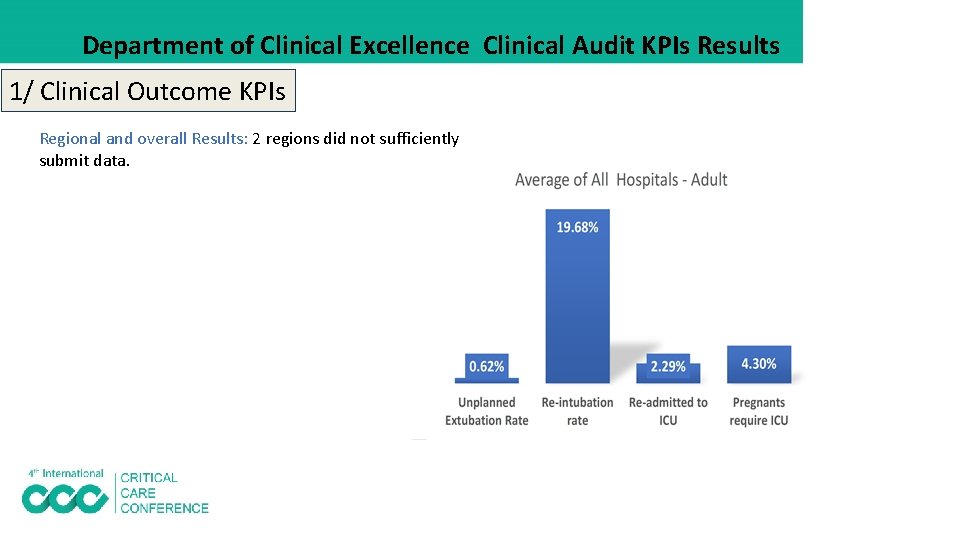
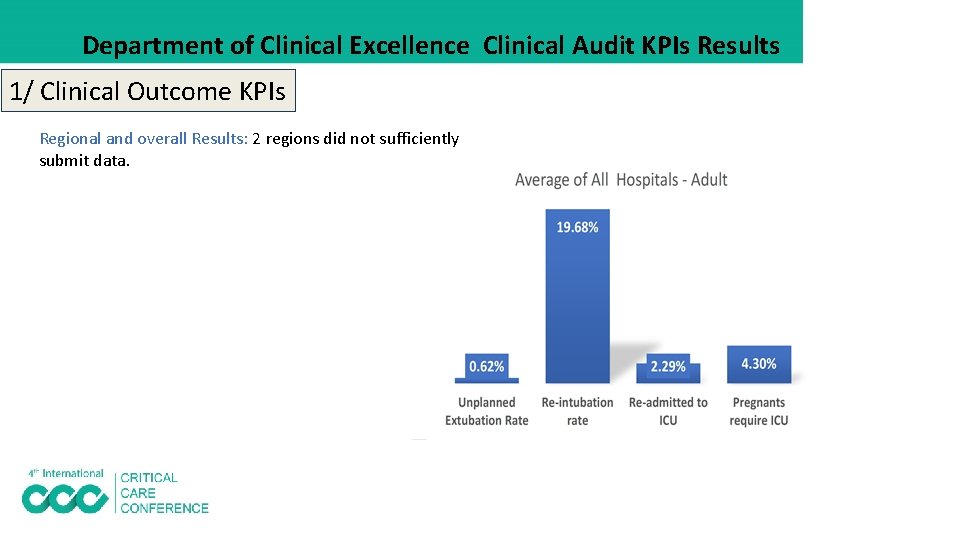
Department of Clinical Excellence Clinical Audit KPIs Results 1/ Clinical Outcome KPIs Regional and overall Results: 2 regions did not sufficiently submit data.
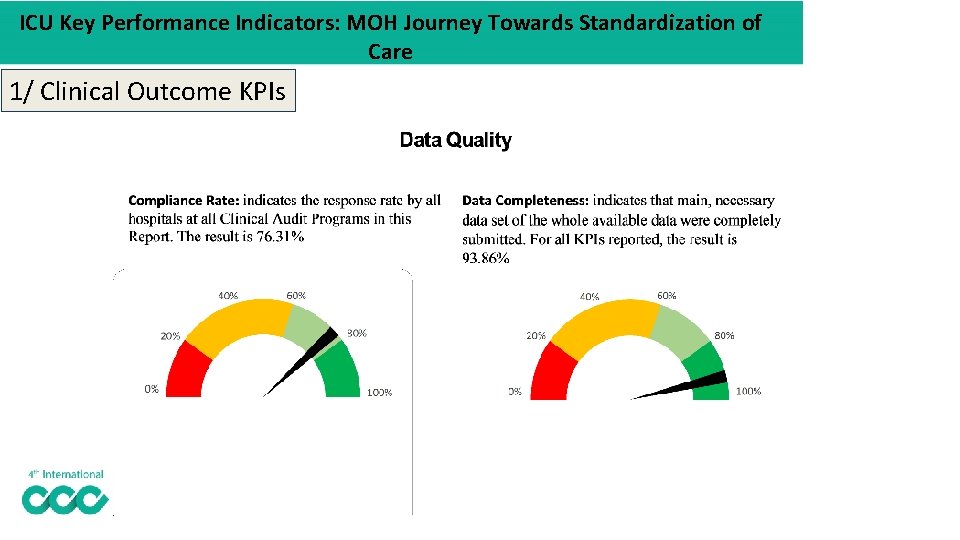
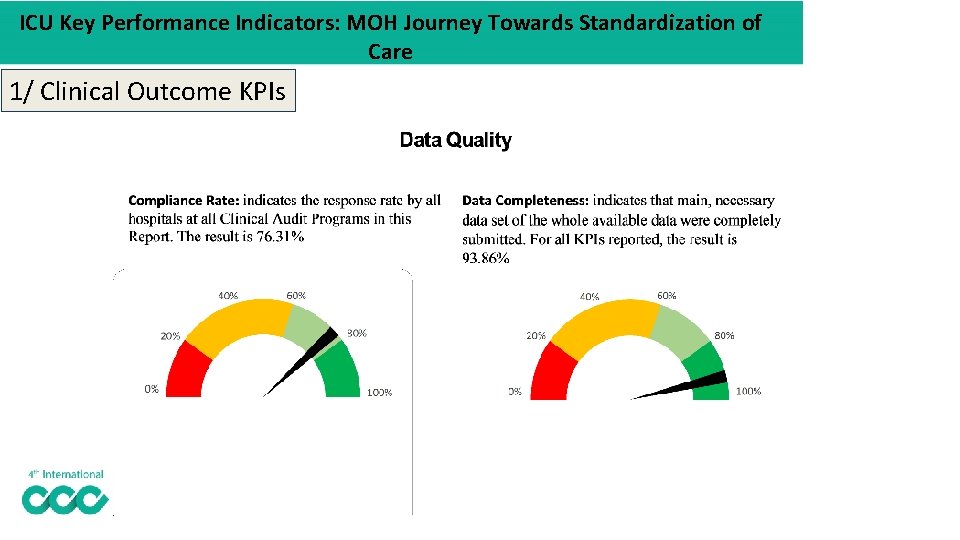
ICU Key Performance Indicators: MOH Journey Towards Standardization of Care 1/ Clinical Outcome KPIs
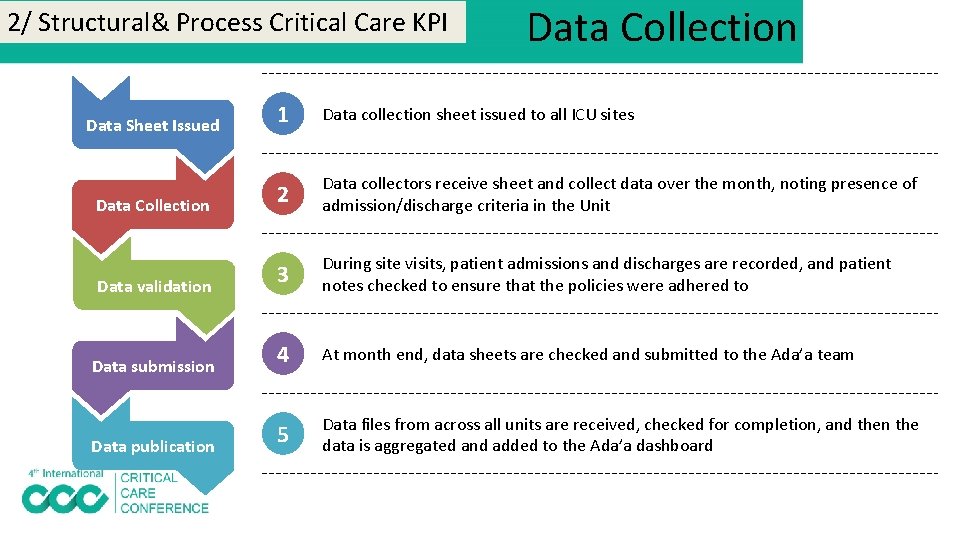
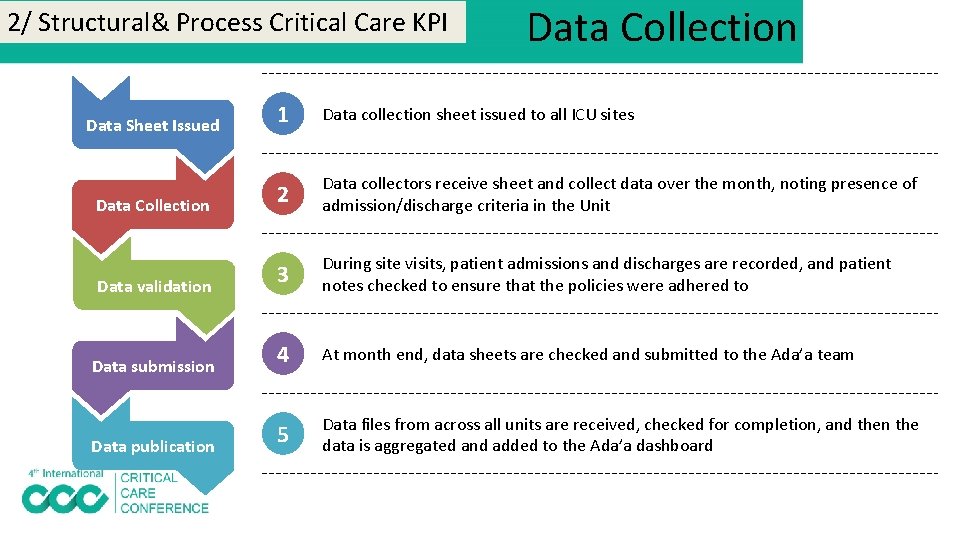
2/ Structural& Process Critical Care KPI Data Collection Data Sheet Issued 1 Data collection sheet issued to all ICU sites Data Collection 2 Data collectors receive sheet and collect data over the month, noting presence of admission/discharge criteria in the Unit Data validation 3 During site visits, patient admissions and discharges are recorded, and patient notes checked to ensure that the policies were adhered to Data submission 4 At month end, data sheets are checked and submitted to the Ada’a team 5 Data files from across all units are received, checked for completion, and then the data is aggregated and added to the Ada’a dashboard Data publication
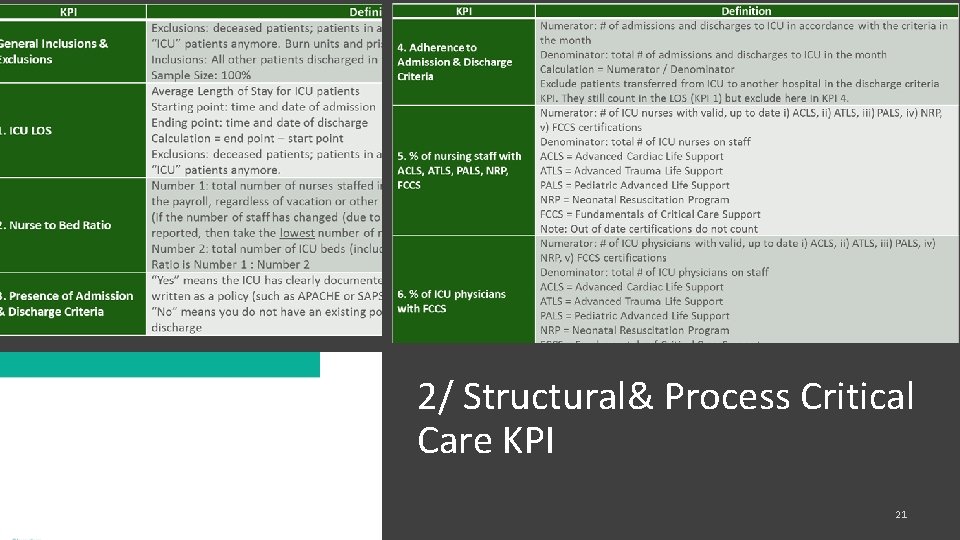
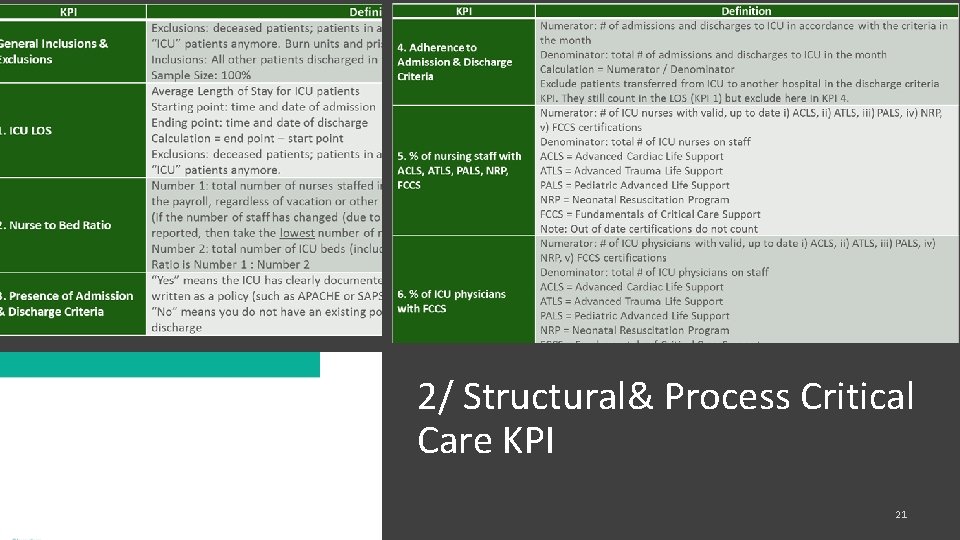
2/ Structural& Process Critical Care KPI 21
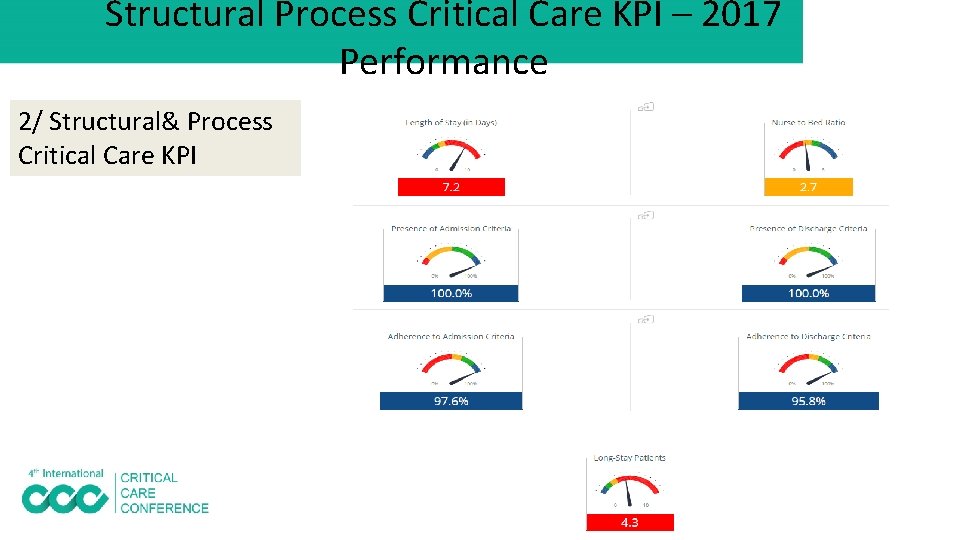
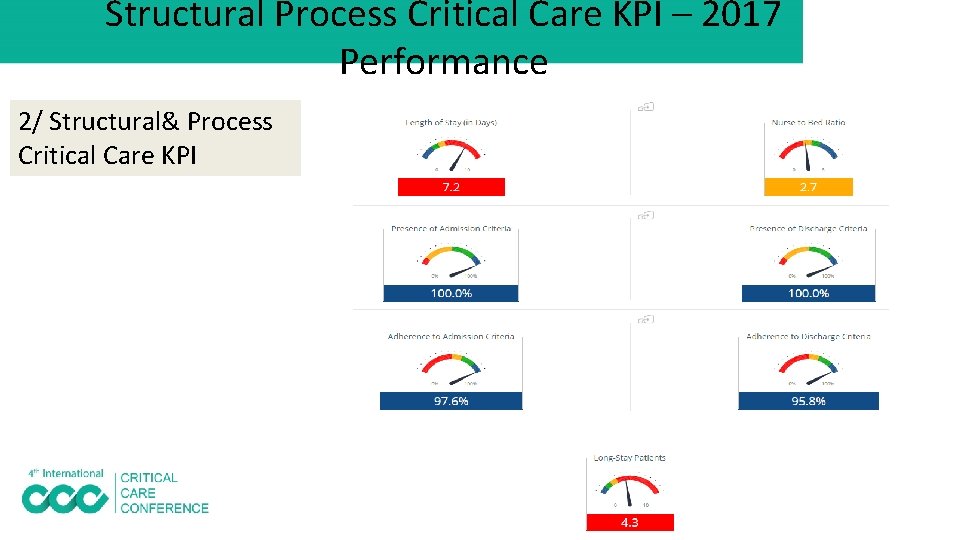
Structural Process Critical Care KPI – 2017 Performance 2/ Structural& Process Critical Care KPI 22
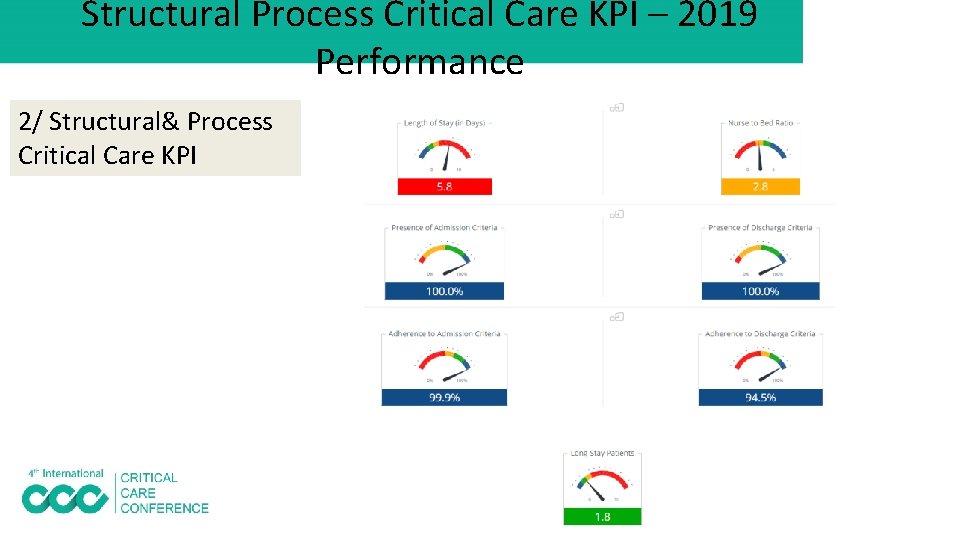
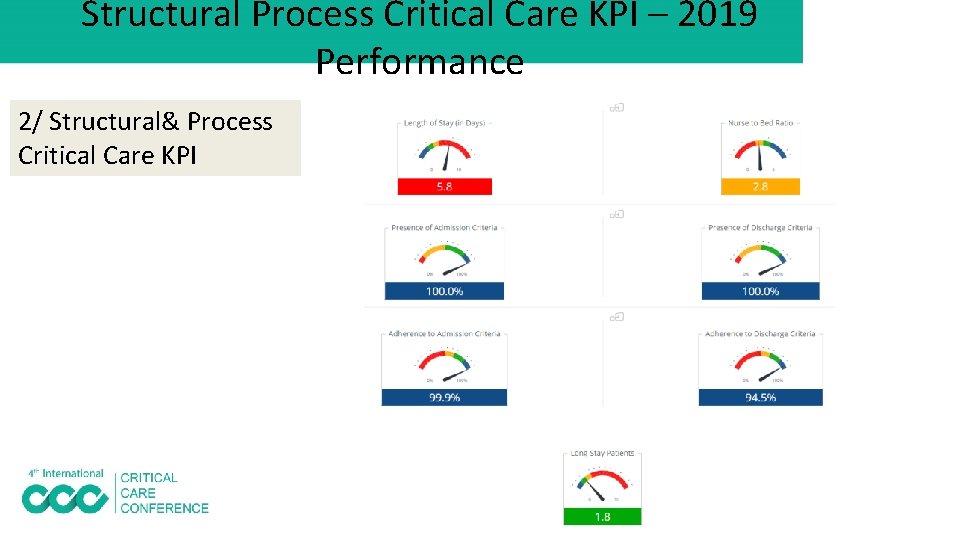
Structural Process Critical Care KPI – 2019 Performance 2/ Structural& Process Critical Care KPI
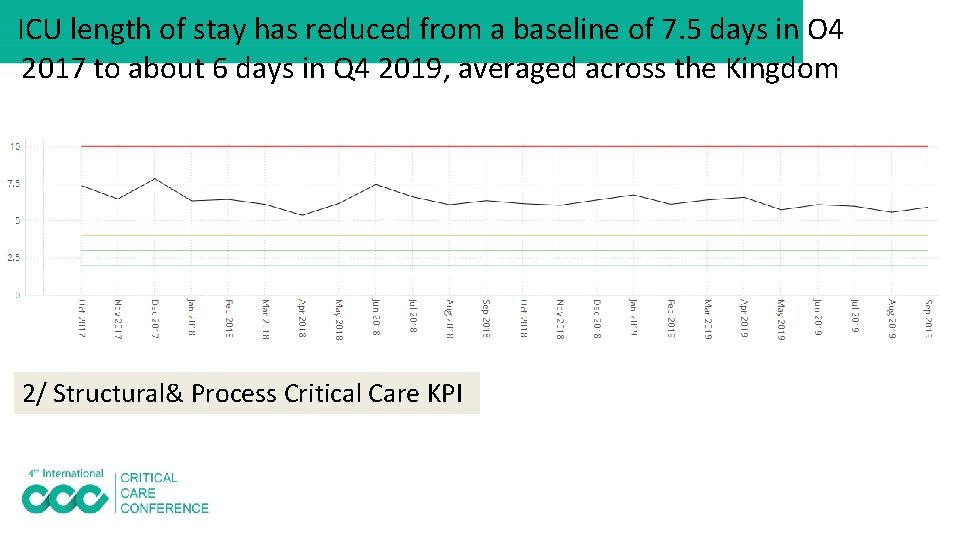
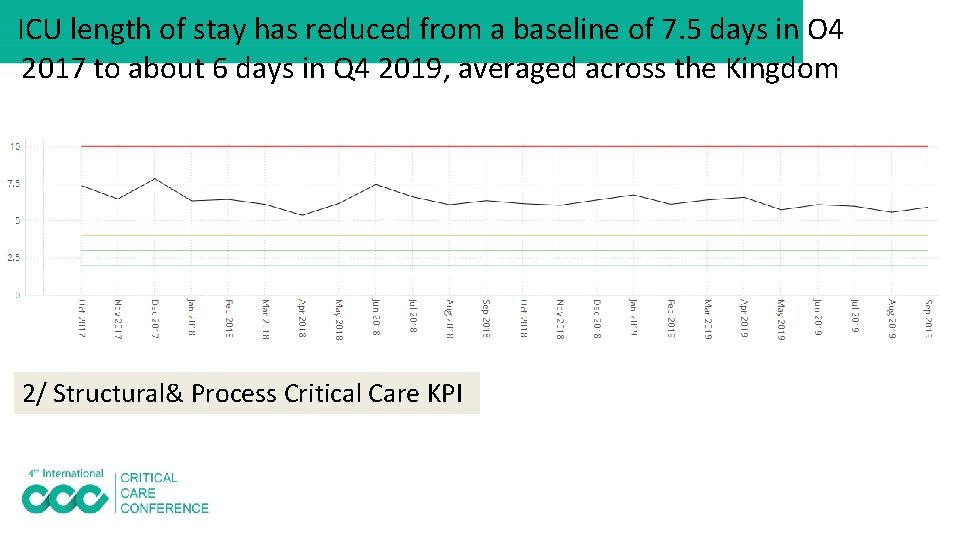
ICU length of stay has reduced from a baseline of 7. 5 days in O 4 2017 to about 6 days in Q 4 2019, averaged across the Kingdom 2/ Structural& Process Critical Care KPI
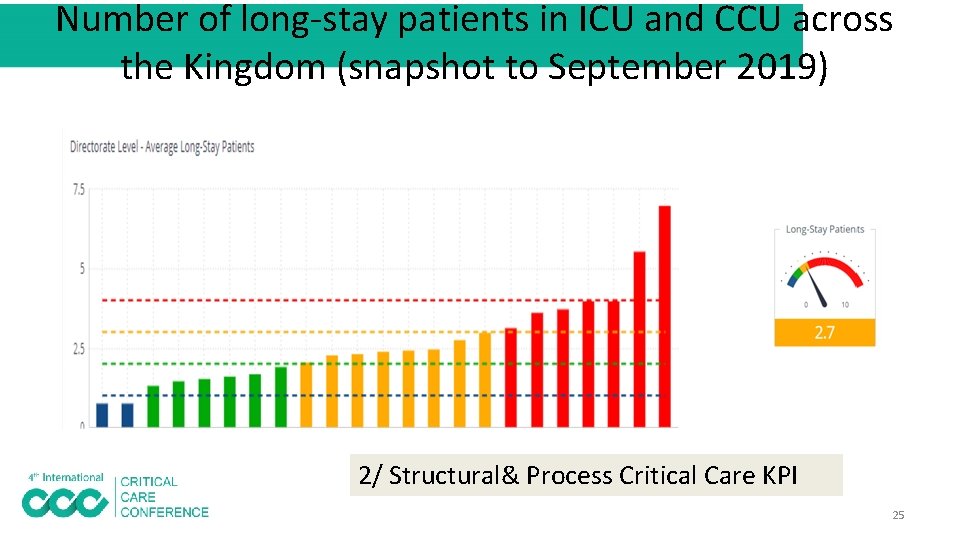
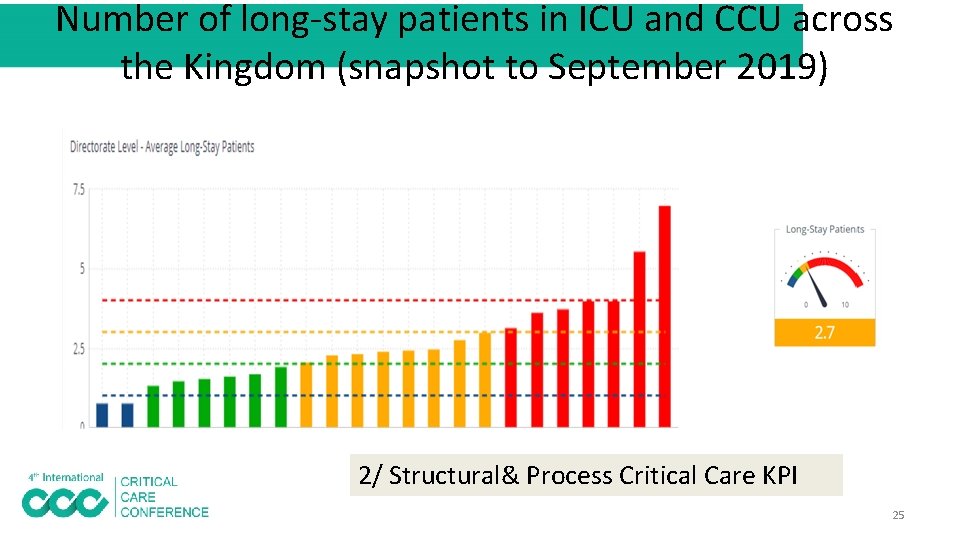
Number of long-stay patients in ICU and CCU across the Kingdom (snapshot to September 2019) 2/ Structural& Process Critical Care KPI 25
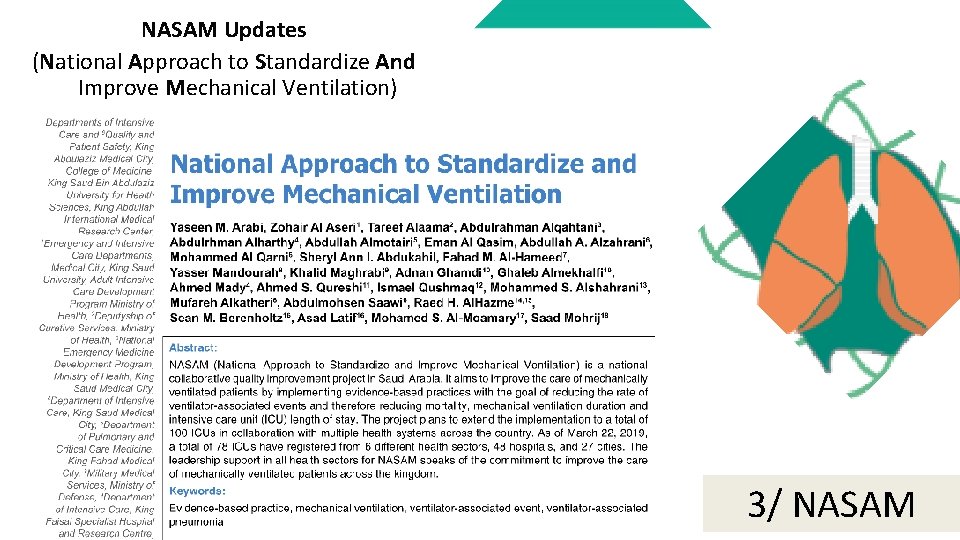
NASAM Updates (National Approach to Standardize And Improve Mechanical Ventilation) 3/ NASAM
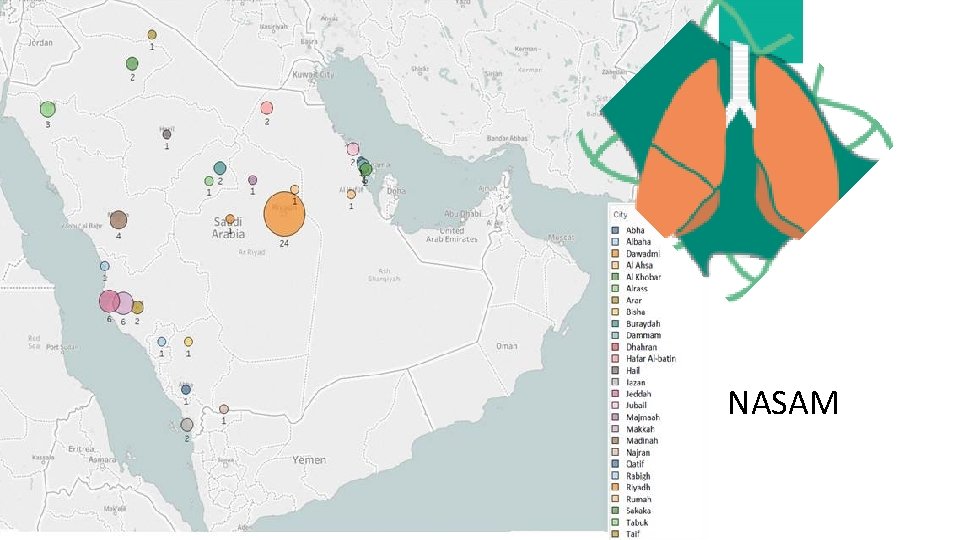
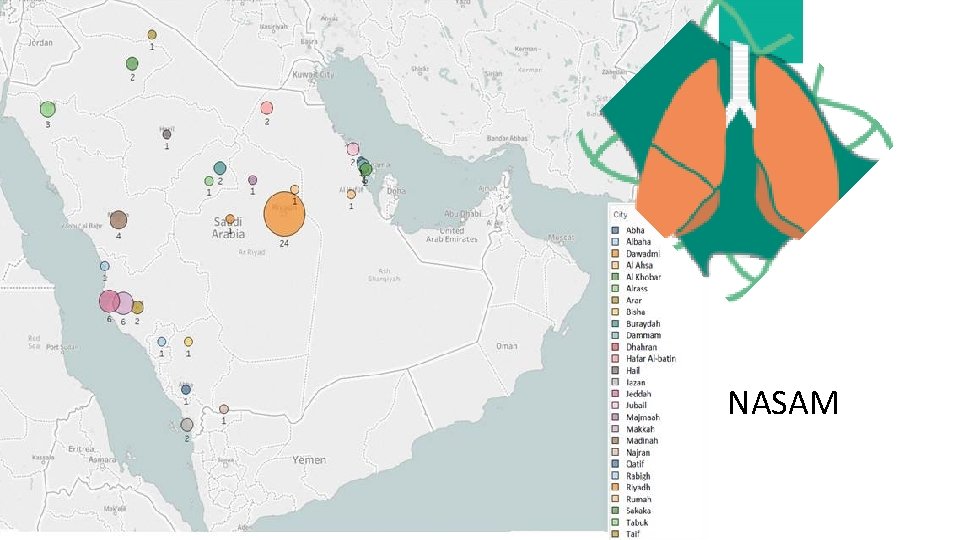
NASAM
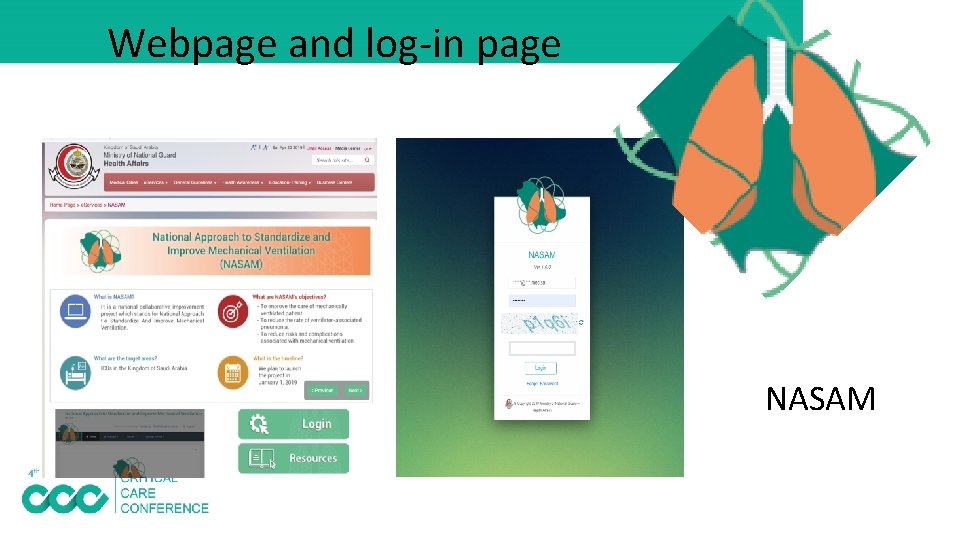
Webpage and log-in page NASAM
NASAM
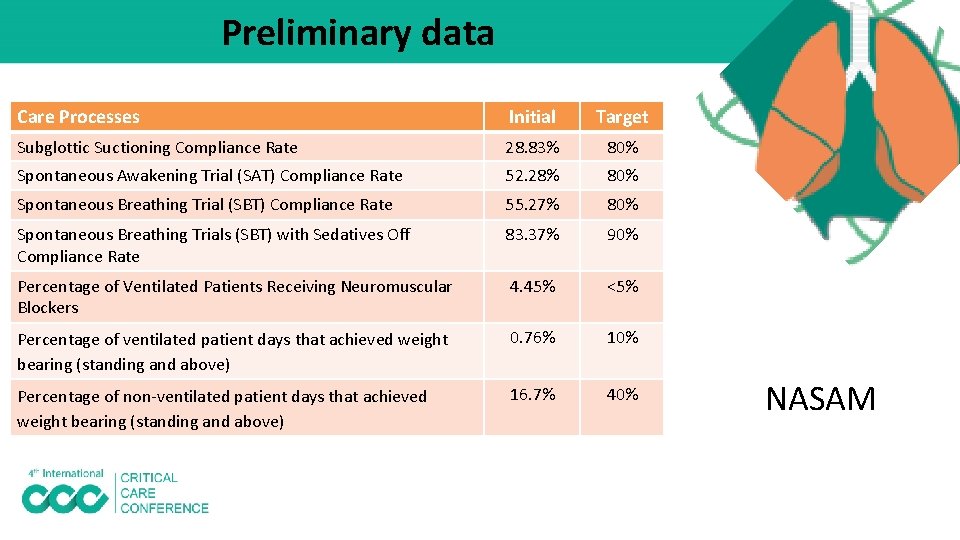
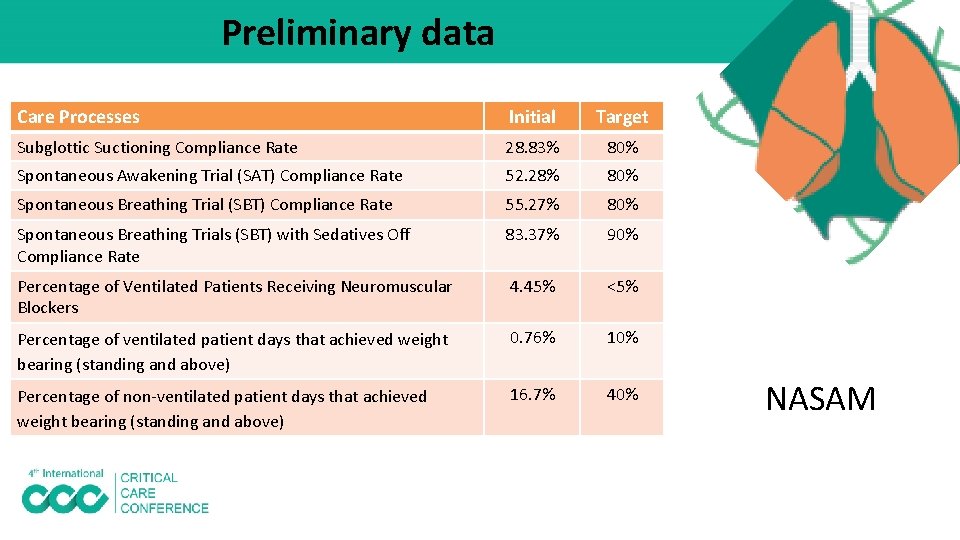
Preliminary data Care Processes Initial Target Subglottic Suctioning Compliance Rate 28. 83% 80% Spontaneous Awakening Trial (SAT) Compliance Rate 52. 28% 80% Spontaneous Breathing Trial (SBT) Compliance Rate 55. 27% 80% Spontaneous Breathing Trials (SBT) with Sedatives Off Compliance Rate 83. 37% 90% Percentage of Ventilated Patients Receiving Neuromuscular Blockers 4. 45% <5% Percentage of ventilated patient days that achieved weight bearing (standing and above) 0. 76% 10% Percentage of non-ventilated patient days that achieved weight bearing (standing and above) 16. 7% 40% NASAM
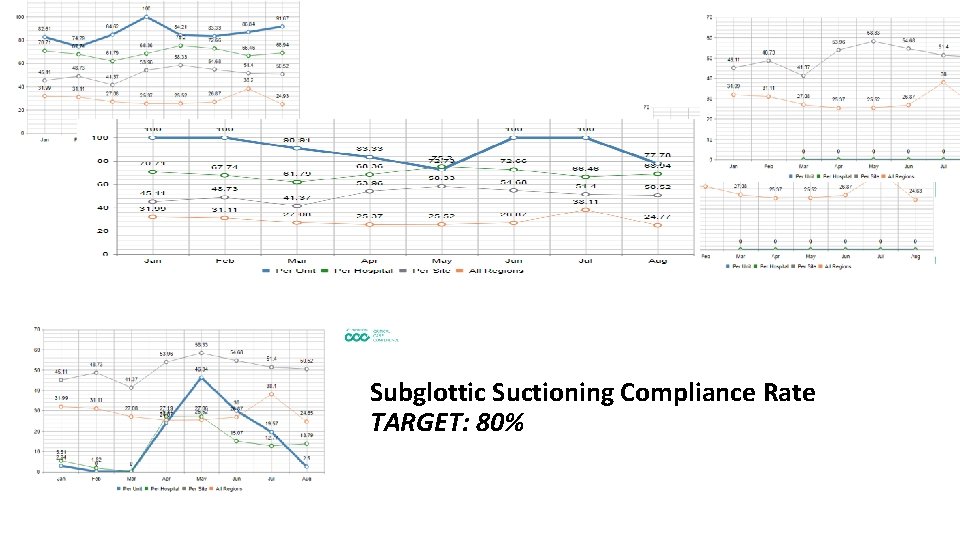
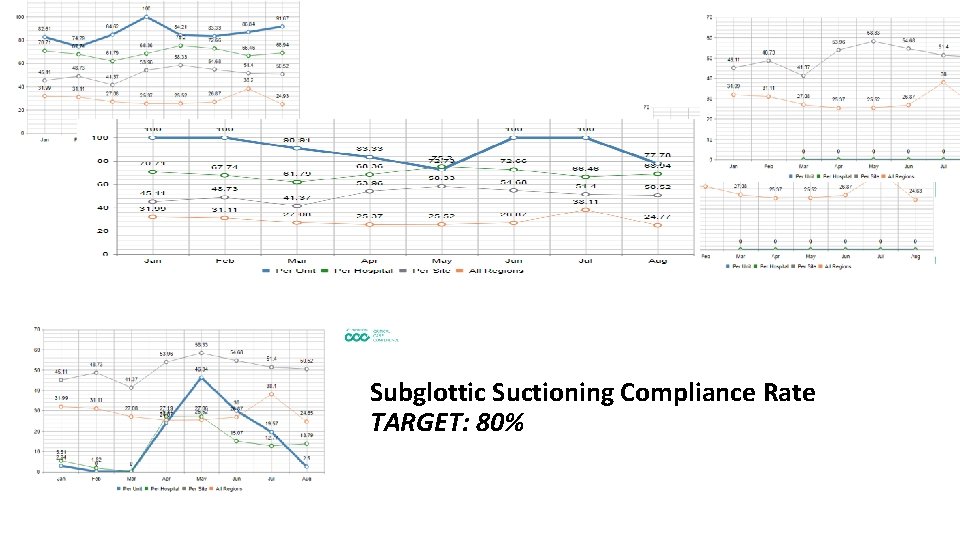
Subglottic Suctioning Compliance Rate TARGET: 80%
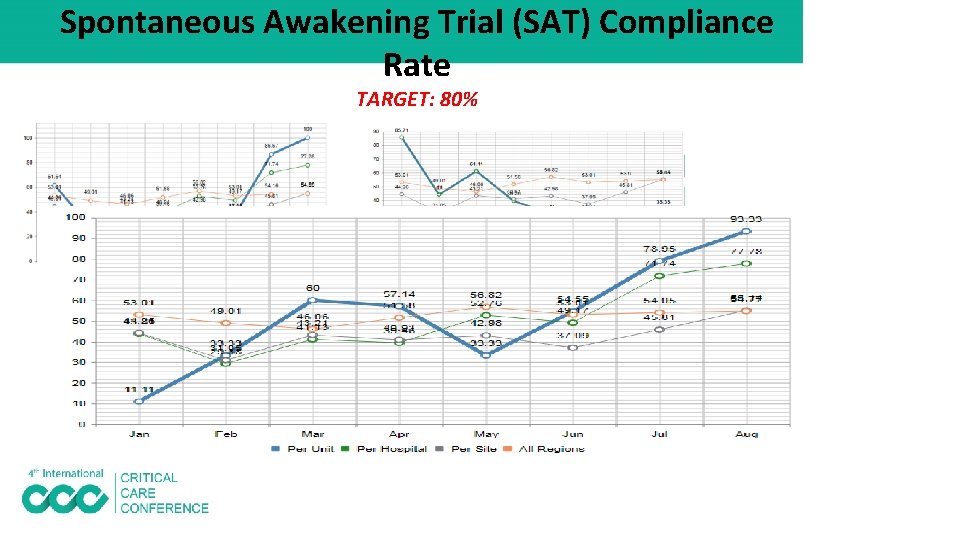
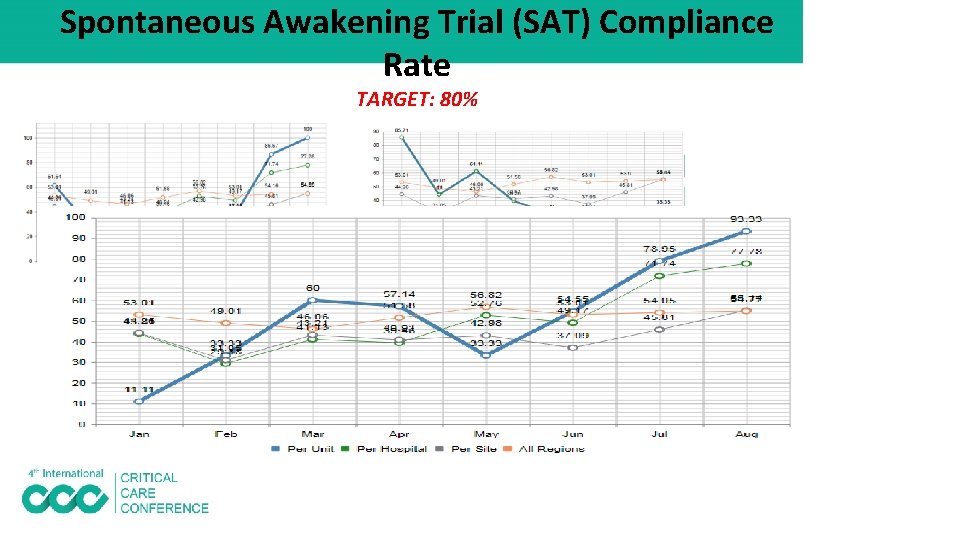
Spontaneous Awakening Trial (SAT) Compliance Rate TARGET: 80%
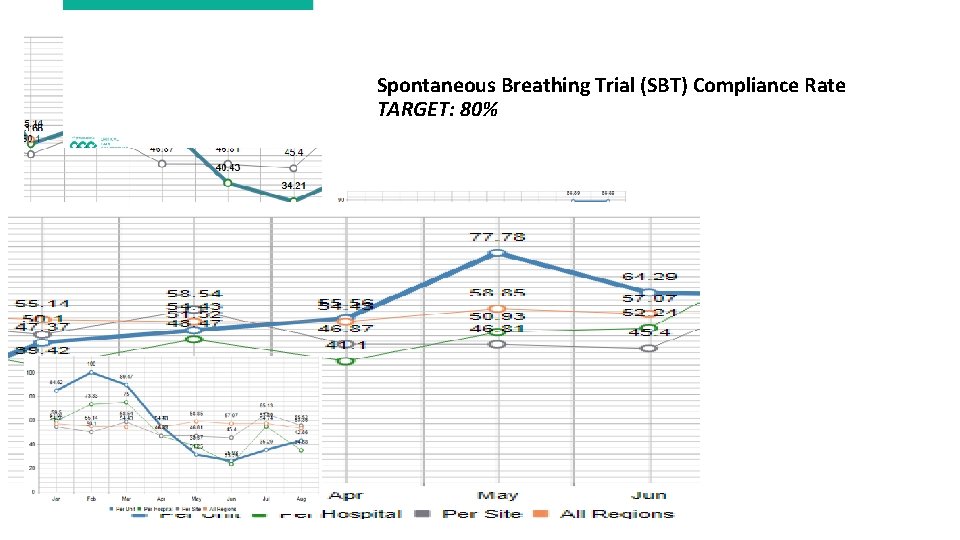
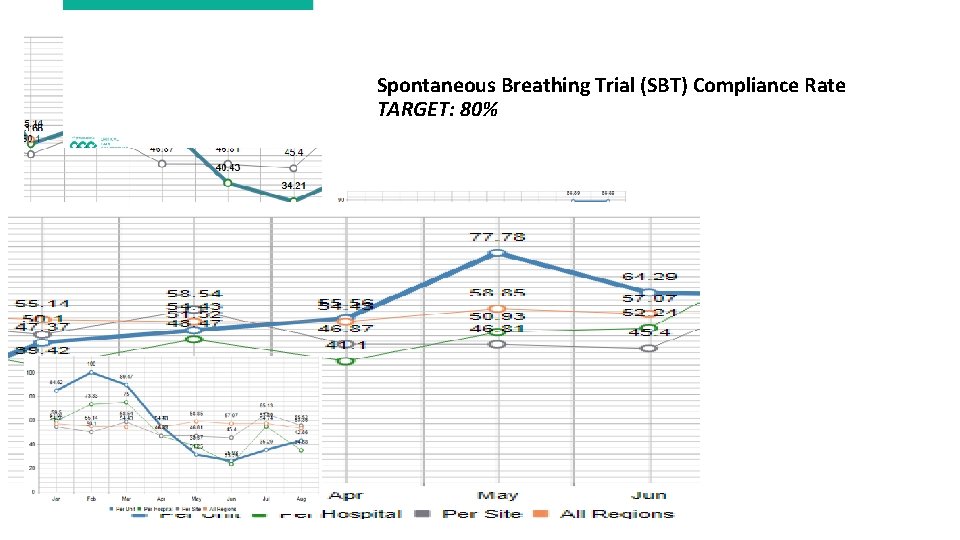
Spontaneous Breathing Trial (SBT) Compliance Rate TARGET: 80%
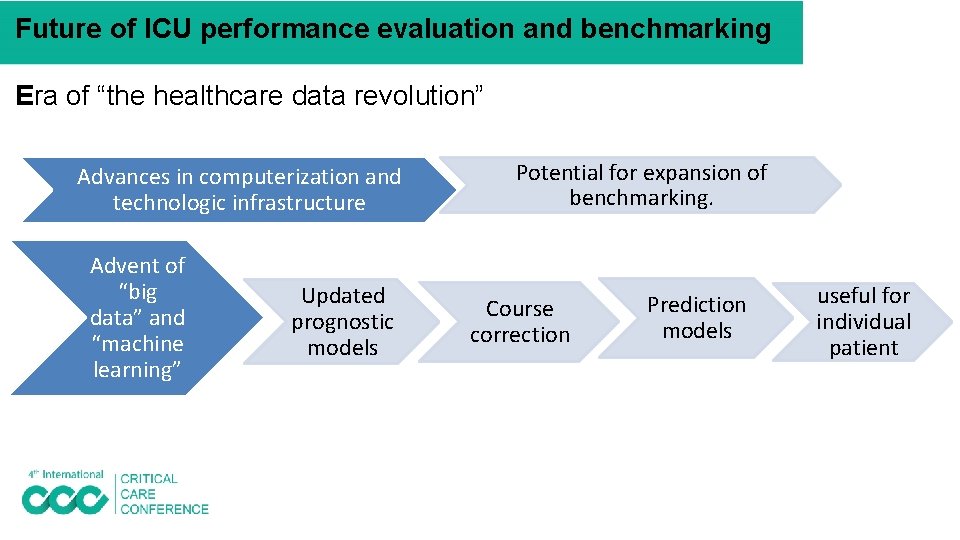
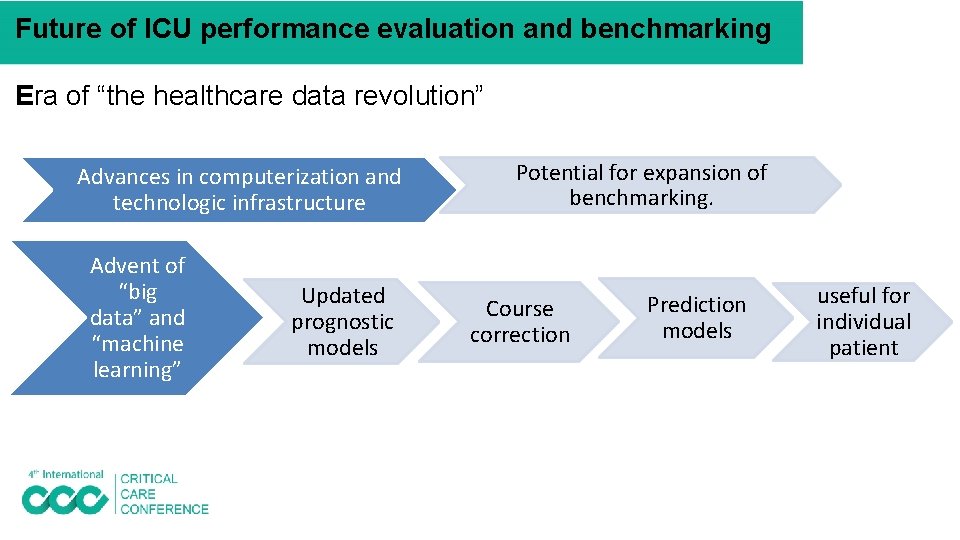
Future of ICU performance evaluation and benchmarking Era of “the healthcare data revolution” Advances in computerization and technologic infrastructure Advent of “big data” and “machine learning” Updated prognostic models Potential for expansion of benchmarking. Course correction Prediction models useful for individual patient
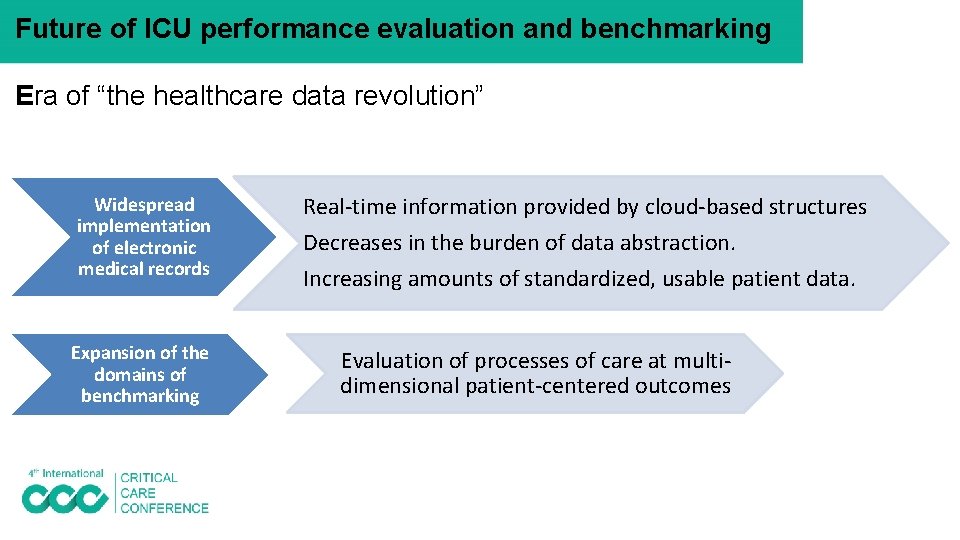
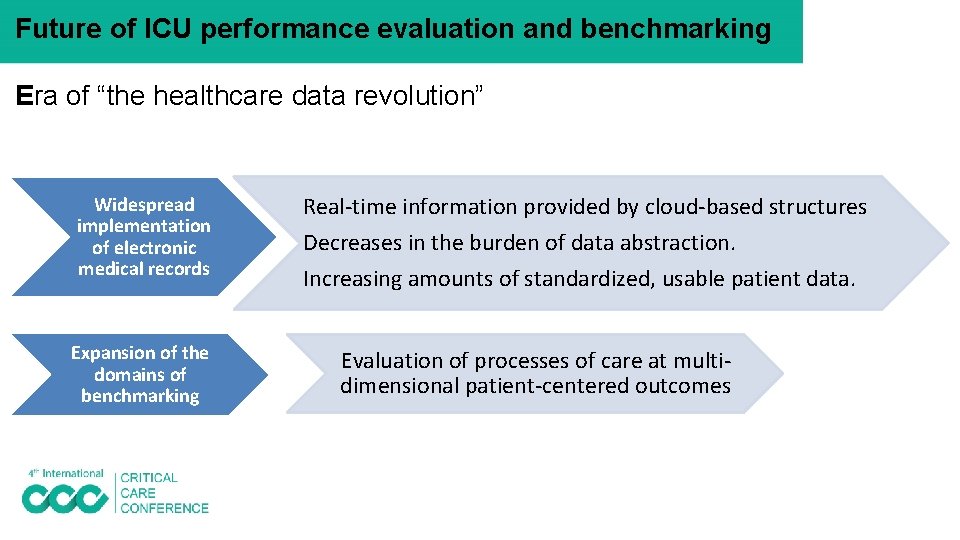
Future of ICU performance evaluation and benchmarking Era of “the healthcare data revolution” Widespread implementation of electronic medical records Expansion of the domains of benchmarking Real-time information provided by cloud-based structures Decreases in the burden of data abstraction. Increasing amounts of standardized, usable patient data. Evaluation of processes of care at multidimensional patient-centered outcomes
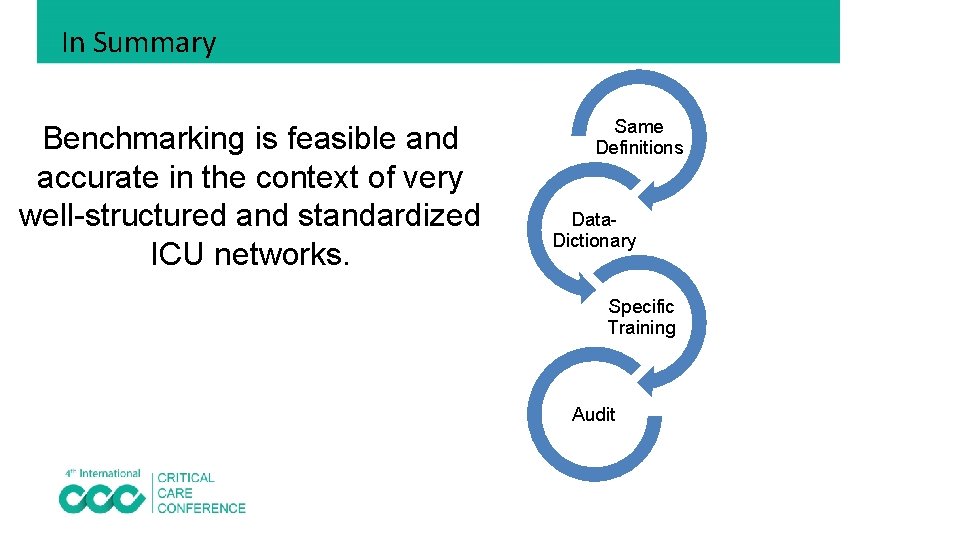
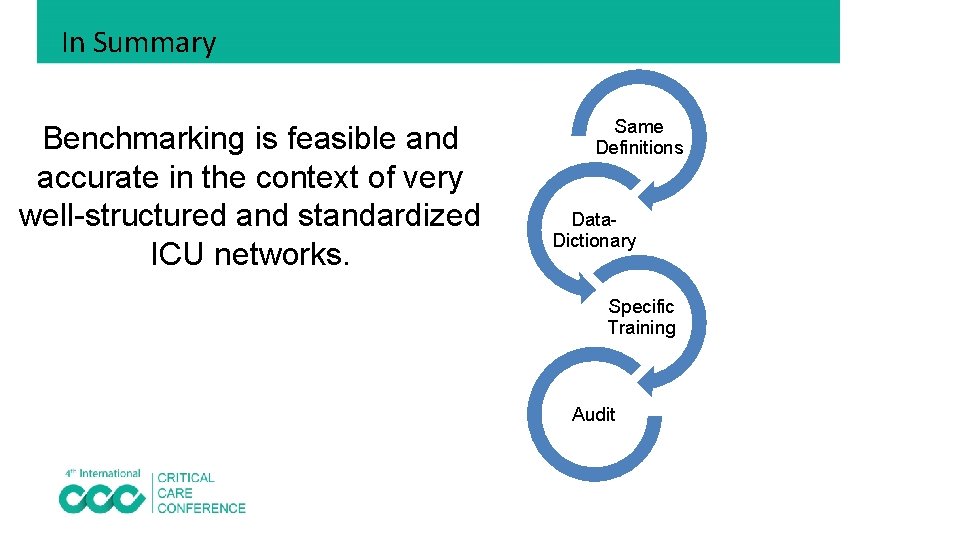
In Summary Benchmarking is feasible and accurate in the context of very well-structured and standardized ICU networks. Same Definitions Data. Dictionary Specific Training Audit
In Summary Benchmarking processes of care • A complementary approach • Evaluate the adherence to evidence-based practices that are associated with improved outcomes • NASAM & MOH KPI Projects are good examples
Thank You Q&A