Iceberg Phenomenon of Diseases SCREENING of a disease

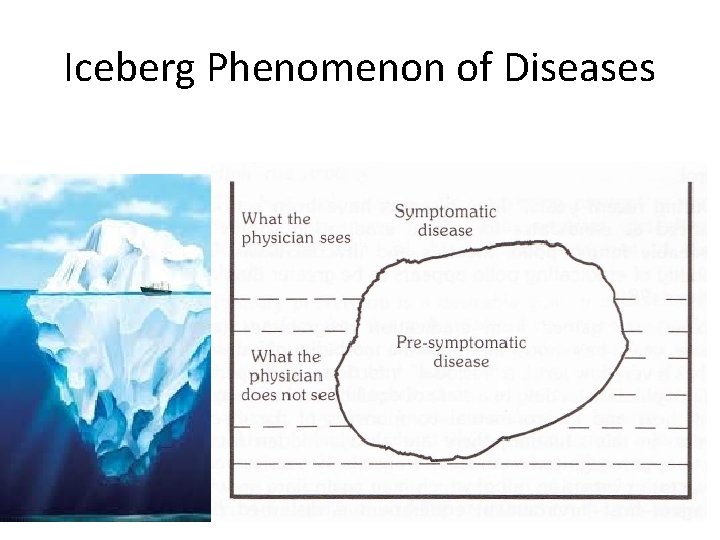
Iceberg Phenomenon of Diseases
SCREENING of a disease
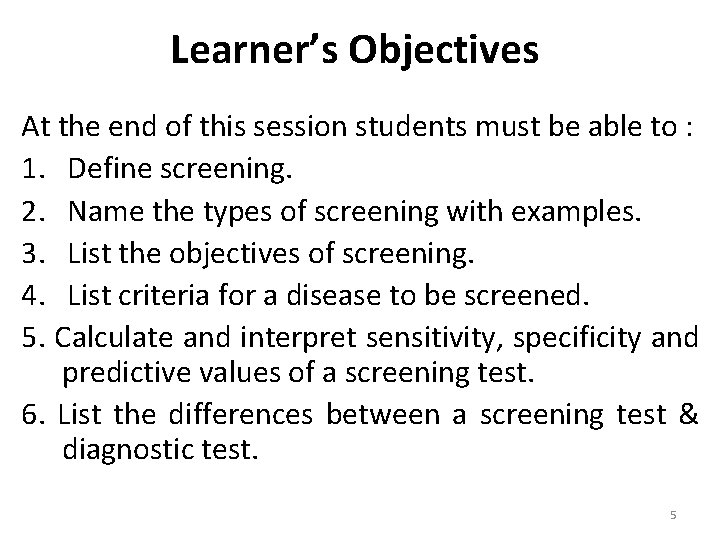
Learner’s Objectives At the end of this session students must be able to : 1. Define screening. 2. Name the types of screening with examples. 3. List the objectives of screening. 4. List criteria for a disease to be screened. 5. Calculate and interpret sensitivity, specificity and predictive values of a screening test. 6. List the differences between a screening test & diagnostic test. 5
HISTORY • Medical screening dates back to more than 60 years. • Screening for psychiatric disorders in the United States army is one of the oldest screening programmes. • Screening for syphilis used one of the earliest screening tests. • Screening for diabetes is one of the first modern forms of mass screening. • Screening for cervical cancer using the Pap test is one of the greatest successes of screening. BMJ- History of medical screening: from concepts to action 6
DEFINITION The presumptive identification of unrecognized defect or disease by the application of tests, examinations or procedures which can be applied rapidly, to sort out apparently well persons who probably have a disease, from those who probably do not. WHO-AFMC Book 7
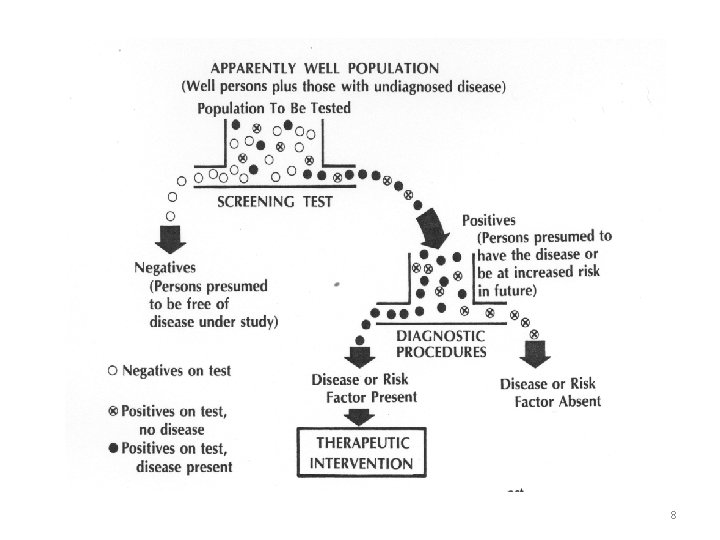
8
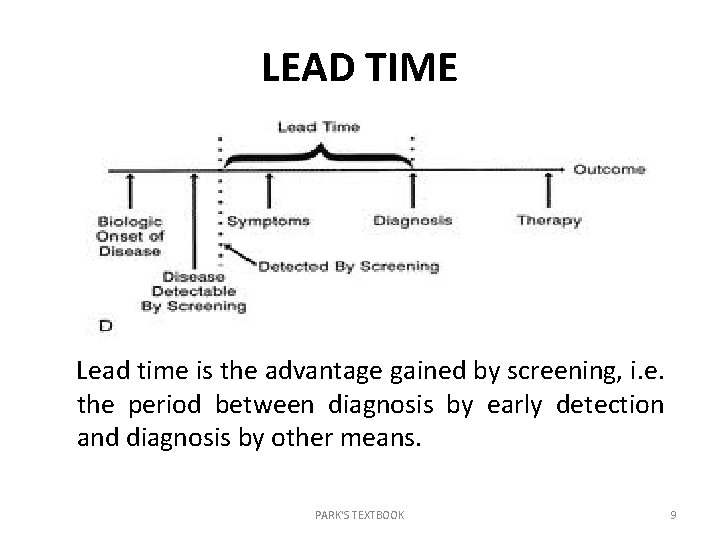
LEAD TIME Lead time is the advantage gained by screening, i. e. the period between diagnosis by early detection and diagnosis by other means. PARK'S TEXTBOOK 9
TYPES OF SCREENING Mass Screening Opportunistic Screening / Case detection Targeted Screening Multi-phasic Screening 10
OBJECTIVES OF SCREENING • Prescriptive screening : Case detection E. g. Cervical cancer / breast cancer • Prospective screening : to protect the community from the disease that person being screened has. E. g. Screening blood units for HIV/Hepatitis B • Employment : for entry into certain occupations with a view to weed out those who are unfit. E. g. . Army/ Navy/ Air force • Research and education WHO-AFMC Book 11
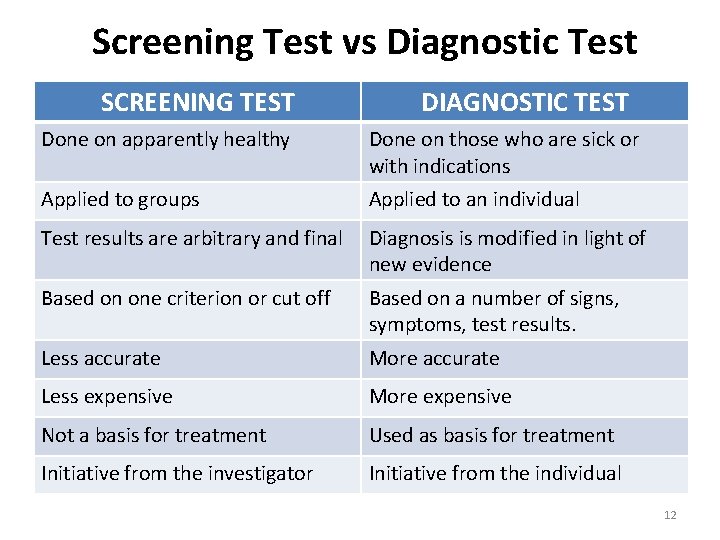
Screening Test vs Diagnostic Test SCREENING TEST DIAGNOSTIC TEST Done on apparently healthy Done on those who are sick or with indications Applied to groups Applied to an individual Test results are arbitrary and final Diagnosis is modified in light of new evidence Based on one criterion or cut off Based on a number of signs, symptoms, test results. Less accurate More accurate Less expensive More expensive Not a basis for treatment Used as basis for treatment Initiative from the investigator Initiative from the individual 12
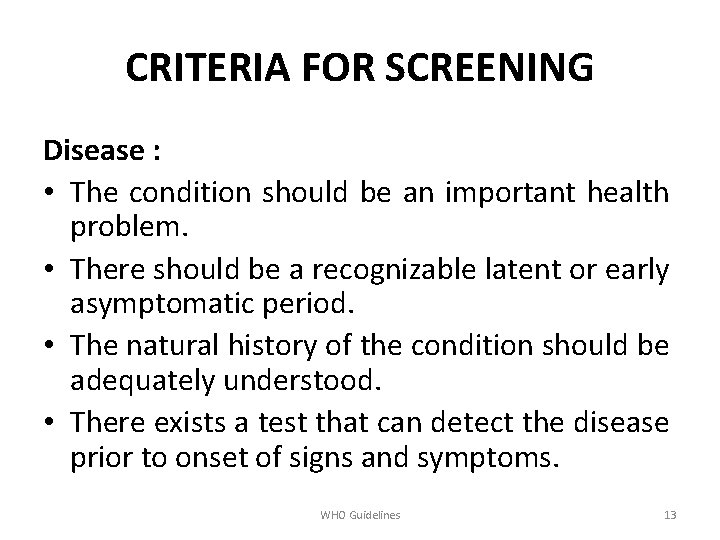
CRITERIA FOR SCREENING Disease : • The condition should be an important health problem. • There should be a recognizable latent or early asymptomatic period. • The natural history of the condition should be adequately understood. • There exists a test that can detect the disease prior to onset of signs and symptoms. WHO Guidelines 13
Contd. . • Facilities should be available for the confirmation of diagnosis. • There is an effective treatment. • There should be an agreed upon policy concerning whom to treat as a patient. • There is good evidence that early detection and treatment reduces mortality and morbidity. • The expected benefits exceed the risks and costs. WHO Guidelines 14
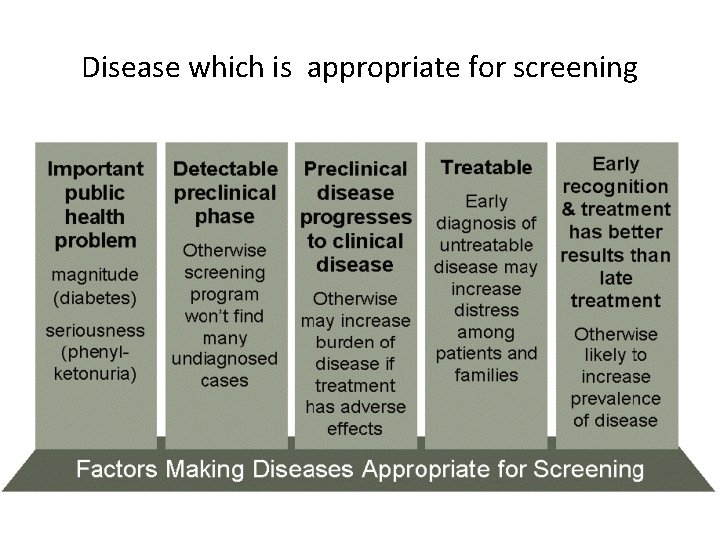
Disease which is appropriate for screening
CRITERIA FOR SCREENING Screening Test : • Acceptability • Repeatability • Validity • Yield • Simplicity • Safety • Cost • Rapidity 16
ACCEPTABILITY The test should be acceptable to the people at whom it is aimed. Tests that are painful , discomforting or embarrassing are not likely to be accepted. E. g. Rectal examination 17
REPEATABILITY Synonyms = Reproducibility , reliability, precision The test must give consistent results when repeated more than once in the same individual under the same conditions. 18
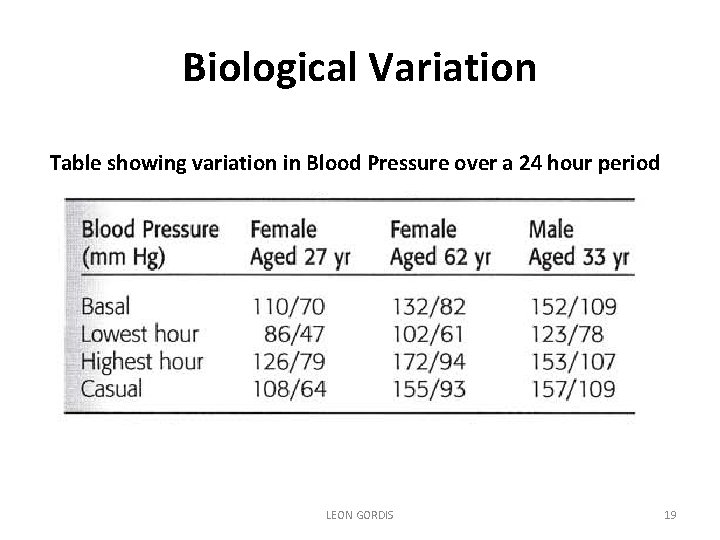
Biological Variation Table showing variation in Blood Pressure over a 24 hour period LEON GORDIS 19
Intra-observer Variation LEON GORDIS 20
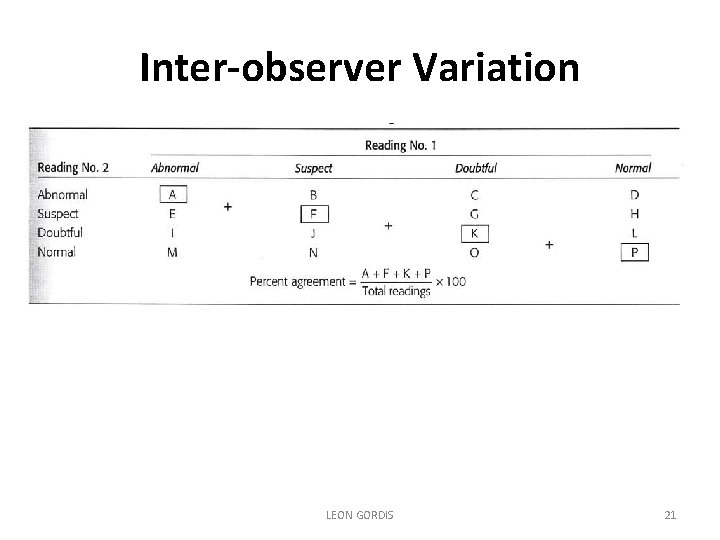
Inter-observer Variation LEON GORDIS 21
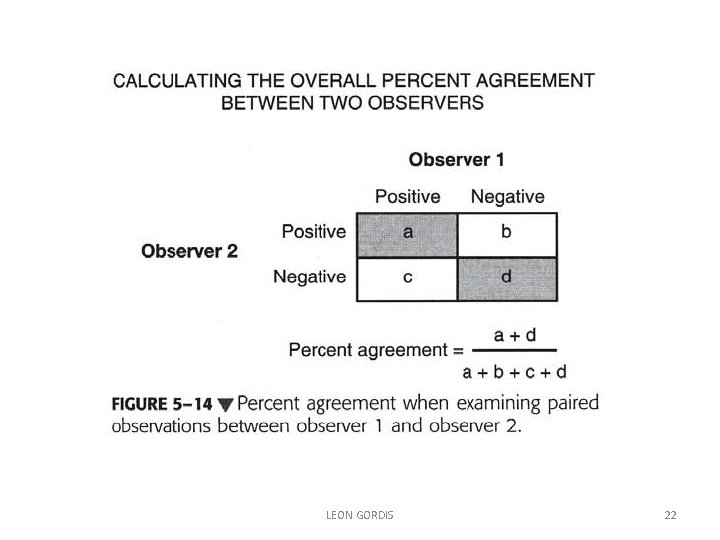
LEON GORDIS 22
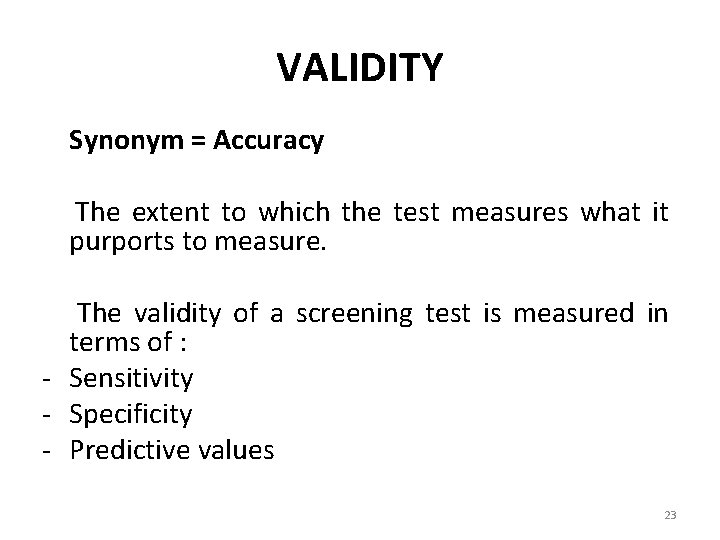
VALIDITY Synonym = Accuracy The extent to which the test measures what it purports to measure. The validity of a screening test is measured in terms of : - Sensitivity - Specificity - Predictive values 23
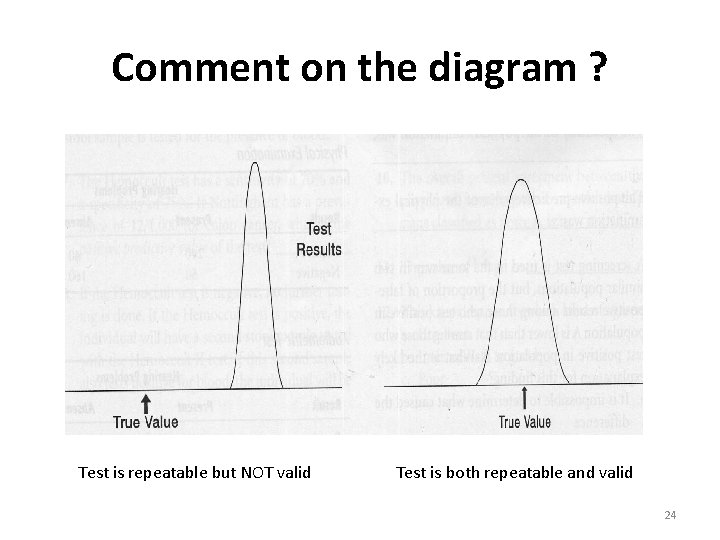
Comment on the diagram ? Test is repeatable but NOT valid Test is both repeatable and valid 24
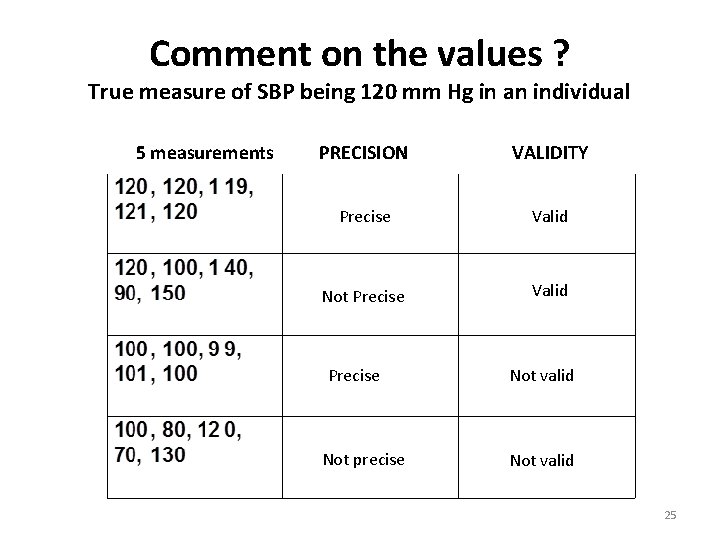
Comment on the values ? True measure of SBP being 120 mm Hg in an individual 5 measurements PRECISION VALIDITY Precise Valid Not Precise Valid Precise Not precise Not valid 25
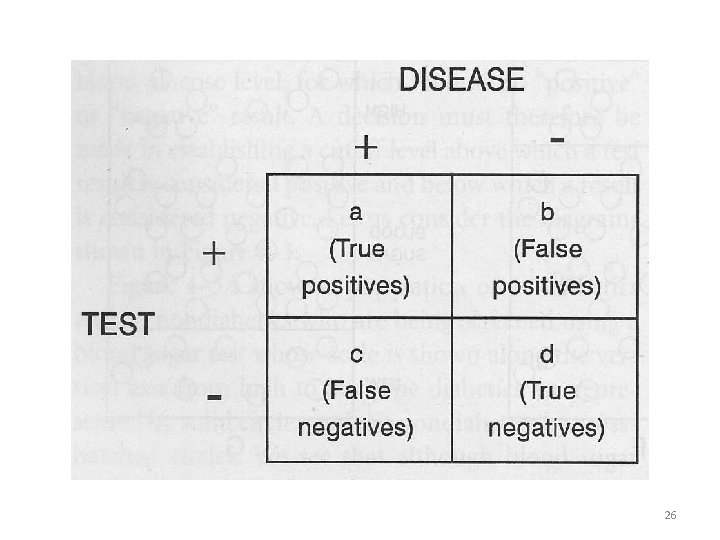
26
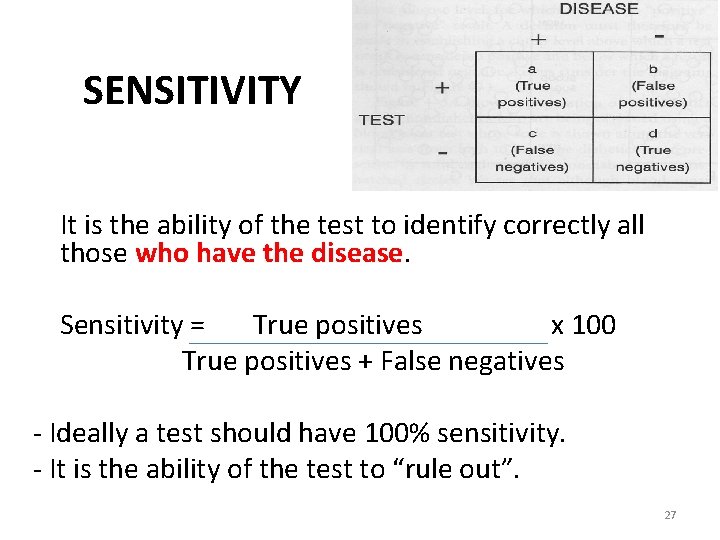
SENSITIVITY It is the ability of the test to identify correctly all those who have the disease. Sensitivity = True positives x 100 True positives + False negatives - Ideally a test should have 100% sensitivity. - It is the ability of the test to “rule out”. 27
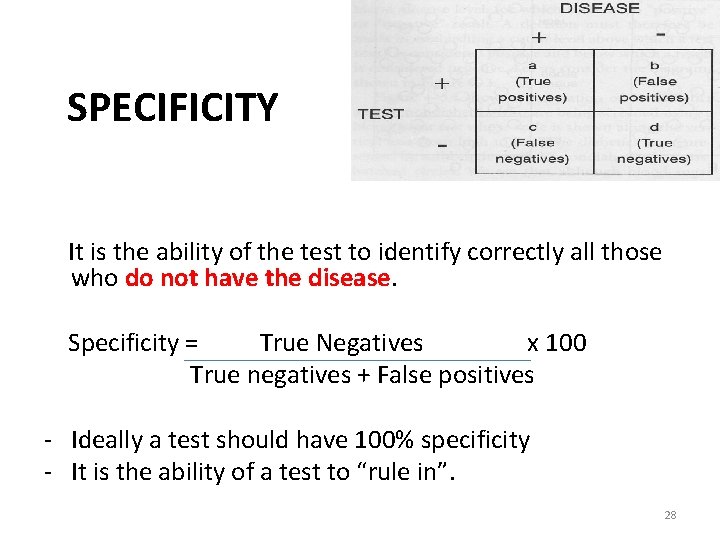
SPECIFICITY It is the ability of the test to identify correctly all those who do not have the disease. Specificity = True Negatives x 100 True negatives + False positives - Ideally a test should have 100% specificity - It is the ability of a test to “rule in”. 28
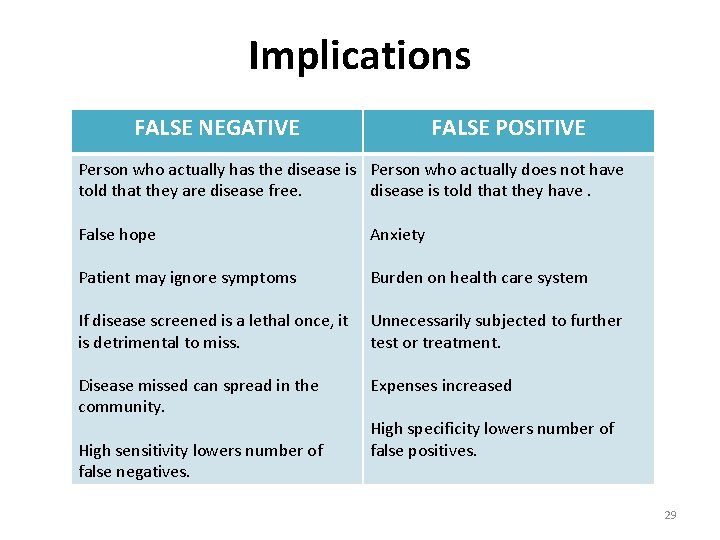
Implications FALSE NEGATIVE FALSE POSITIVE Person who actually has the disease is Person who actually does not have told that they are disease free. disease is told that they have. False hope Anxiety Patient may ignore symptoms Burden on health care system If disease screened is a lethal once, it is detrimental to miss. Unnecessarily subjected to further test or treatment. Disease missed can spread in the community. Expenses increased High sensitivity lowers number of false negatives. High specificity lowers number of false positives. 29
Question 1: Does Carcinoma cervix have a recognizable early phase in which early treatment can be shown to improve prognosis? • Early phase Yes Has early treatment been shown to improve prognosis? • Yes
Question 2: Is effective treatment available? • Is there a place nearby where the treatment can be obtained? • Visit to a gynecology – cryotherapy, loop electrosurgical excision procedure, knife-conization • Will it be affordable, i. e. will it be covered by the patient’s insurance? Yes
Question 3: Is the diagnostic/screening test relatively harmless and acceptable to patients? • The test requires only speculum examination and smear from cervix
Question 4: What is the natural history of CA Cx? • CIN 1 or Dysplasia (5 -10 years) - revert to normal/ remain the same • CIN 2&3 – 30% become ca in situ in 3 -10 years and invasive in 10 -20 years
Question 5: Does the test achieve a balance between false positives and false negatives, with an acceptable risk of wrong diagnosis for both the health system and the patient? • Need to calculate the false positive and false negative rates.
Question 6: Does the test reduce mortality • CIN 1 – if treated, do not progress to Ca • CIS – high cure rate (100% for 5 year survival)
Question 7: How effective is treatment after diagnosis? • CIN – if treated, 100% cure 5 year survival • CIS – 100% • Locally invasive 79% • Regionally invasive 45%
Uses of screening 1. Case detection: Prescriptive screening. People are screened for their own benefit. Initiate the treatment appropriately. Example: Pregnant women
2. Disease control: Prospective screening For the benefit of others. Early diagnosis: Effective treatment and implementation of control measures to prevent the spread
3. Research Purposes: 4. Educational opportunities: To the community
- Slides: 39