ICCS enewsletter CSI Sean R Mc Master and






- Slides: 30
ICCS e-newsletter CSI Sean R Mc. Master and George Deeb Department of Pathology & Laboratory Medicine Emory University School of Medicine Emory University Hospital 1364 Clifton Road NE Atlanta, GA 30322
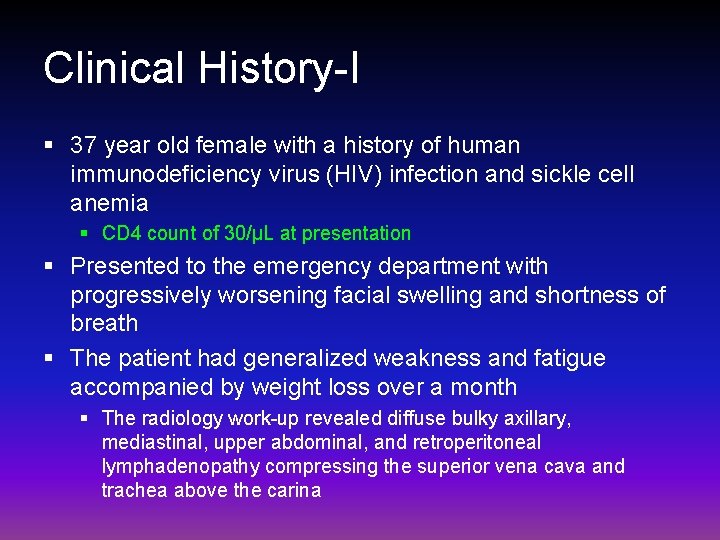
Clinical History-I § 37 year old female with a history of human immunodeficiency virus (HIV) infection and sickle cell anemia § CD 4 count of 30/µL at presentation § Presented to the emergency department with progressively worsening facial swelling and shortness of breath § The patient had generalized weakness and fatigue accompanied by weight loss over a month § The radiology work-up revealed diffuse bulky axillary, mediastinal, upper abdominal, and retroperitoneal lymphadenopathy compressing the superior vena cava and trachea above the carina

Complete blood counts Results Reference range White Blood Cell Count 6. 3 10^3/µL 4. 0 - 10. 0 Red Blood Cell Count 4. 25 10^3/µL 3. 93 - 5. 22 Hemoglobin 10. 1 gm/d. L 11. 4 - 14. 4 Hematocrit 32. 2 % 33. 3 - 41. 4 MCV 75. 8 f. L 79. 4 - 94. 8 Red Cell Distribution Width-CV 18. 4 % 11. 7 - 14. 4 Platelet Count 261 10^3/µL 150. 0 - 400. 0 A bone marrow biopsy and mediastinal mass fine needle aspiration and core needle biopsy were performed.

Flow cytometry analysis § Four-color multiparameter flow cytometry analysis were performed on submitted samples: § Samples were acquired as FCS 3. 0 files and analyzed using BD FACSDIVA software on a BD FACS Canto II cytometer § Selected relevant antibody combinations Tube 1 Tube 2 Tube 3 Per-CP FITC PE APC CD 45 CD 16 CD 56 CD 38 CD 45 intracellular kappa light chain CD 38 ----- CD 45 intracellular lambda light chain CD 38 -----
Flow cytometry analysis-I Overview § The flow cytometric immunophenotyping of samples suspected of harboring hematological malignancies emphasizes the identification and characterization of both normal and abnormal cell populations § A “pattern recognition” approach is utilized whereby normal cells exhibit a predictable antigen expression pattern and abnormal populations are obviously deviated from such § Analysis requires familiarity with normal patterns in various sample types
Flow cytometry analysis-II Overview § 14 (lymphoma/leukemia) and 16 (plasma cell myeloma) four-color tubes are usually performed on blood and bone marrow samples submitted for suspected hematolymphoid malignancies § The initial analysis begins with an overview of the principal cell populations expected to be seen in these samples (e. g. granulocytes, monocytes, and lymphocytes in a blood sample) § Thereafter, the assessment of each antibody combination focuses mainly on the mononuclear cells (mononuclear cell gate) § The cell population of interest will be gated on to be highlighted as needed § CD 45 is a backbone marker in all tubes
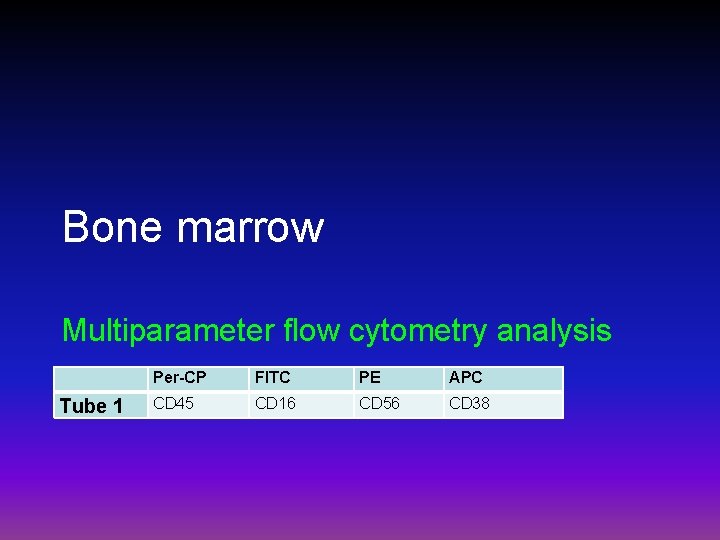
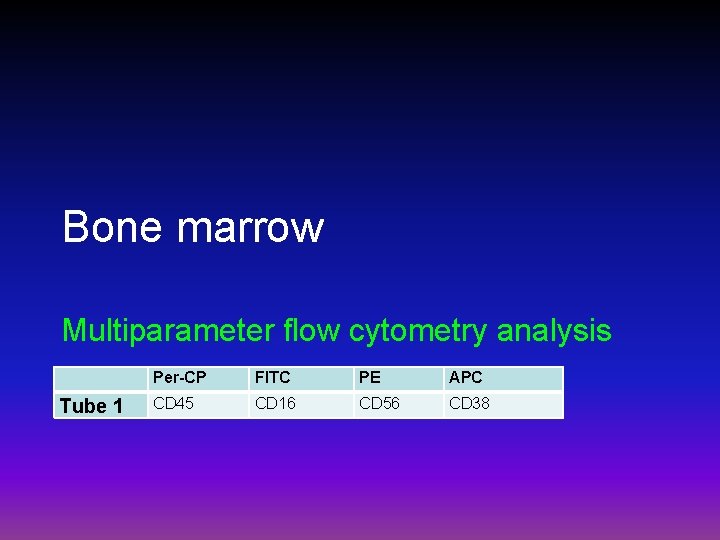
Bone marrow Multiparameter flow cytometry analysis Tube 1 Per-CP FITC PE APC CD 45 CD 16 CD 56 CD 38
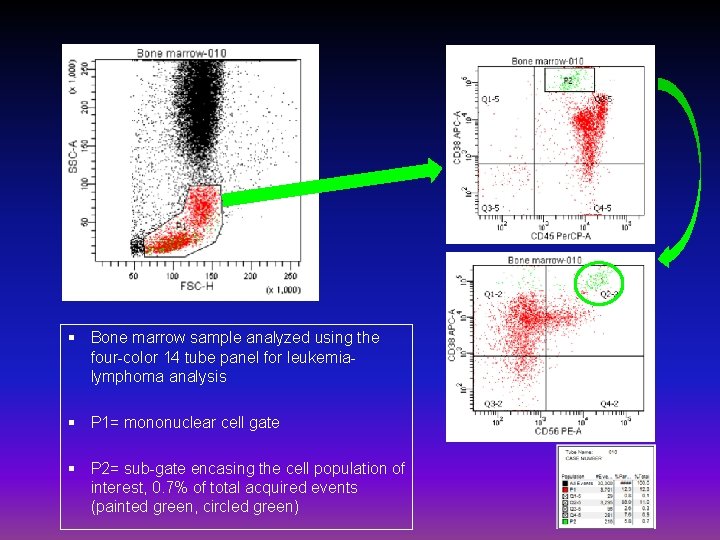
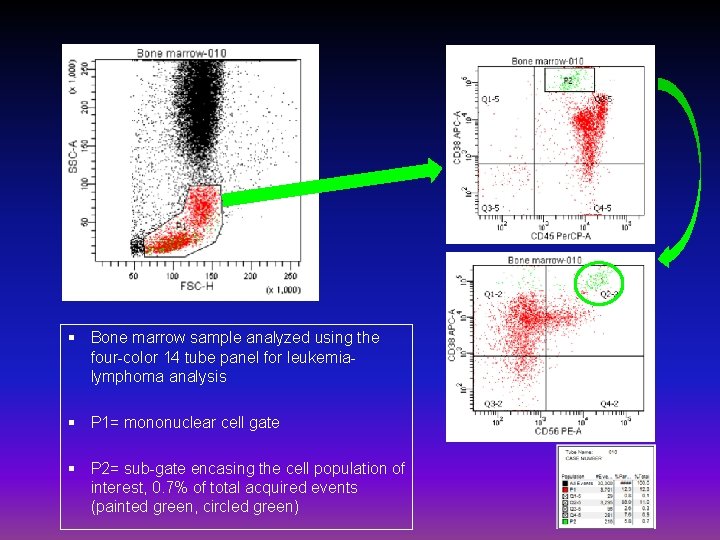
§ Bone marrow sample analyzed using the four-color 14 tube panel for leukemialymphoma analysis § P 1= mononuclear cell gate § P 2= sub-gate encasing the cell population of interest, 0. 7% of total acquired events (painted green, circled green)

Mediastinal mass Multiparameter flow cytometry analysis Tube 1 Per-CP FITC PE APC CD 45 CD 16 CD 56 CD 38
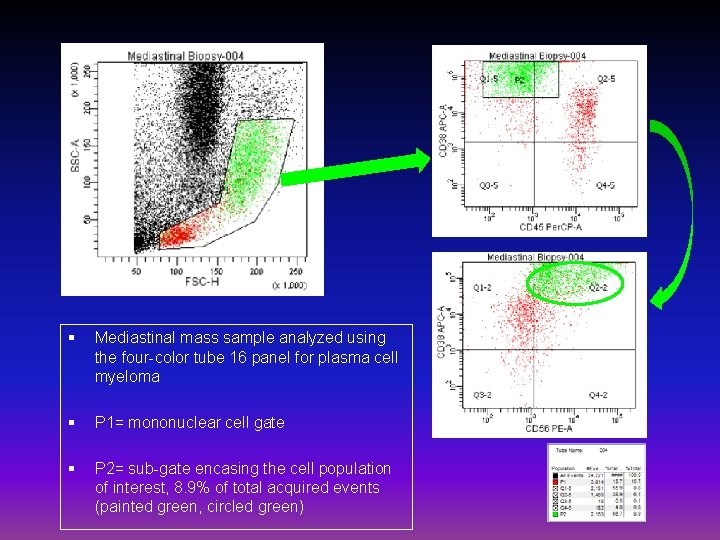
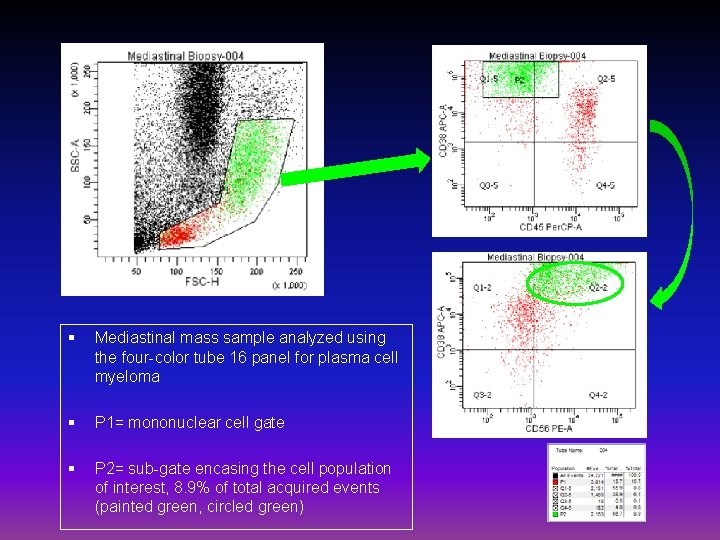
§ Mediastinal mass sample analyzed using the four-color tube 16 panel for plasma cell myeloma § P 1= mononuclear cell gate § P 2= sub-gate encasing the cell population of interest, 8. 9% of total acquired events (painted green, circled green)
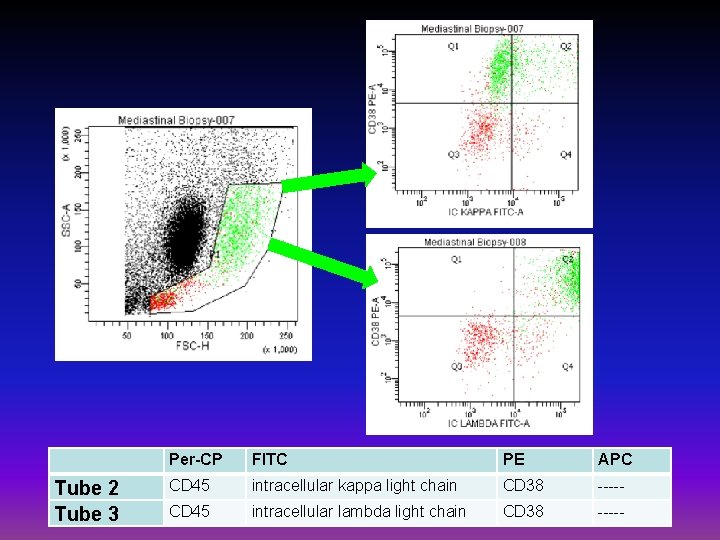
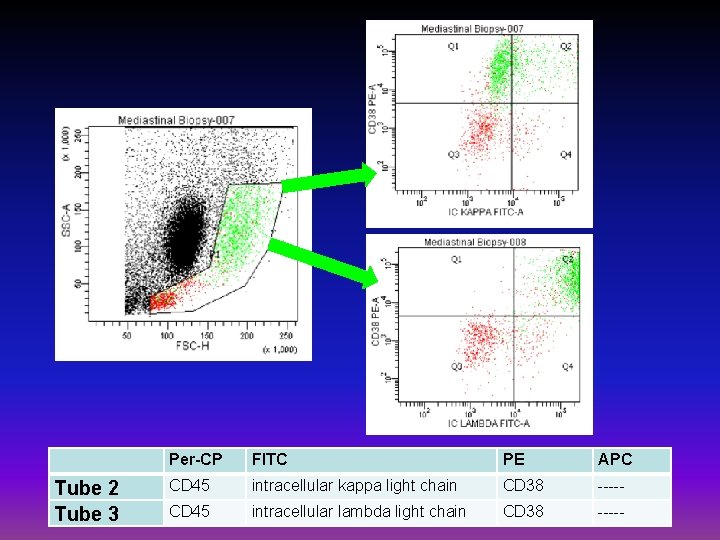
Tube 2 Tube 3 Per-CP FITC PE APC CD 45 intracellular kappa light chain CD 38 ----- CD 45 intracellular lambda light chain CD 38 -----
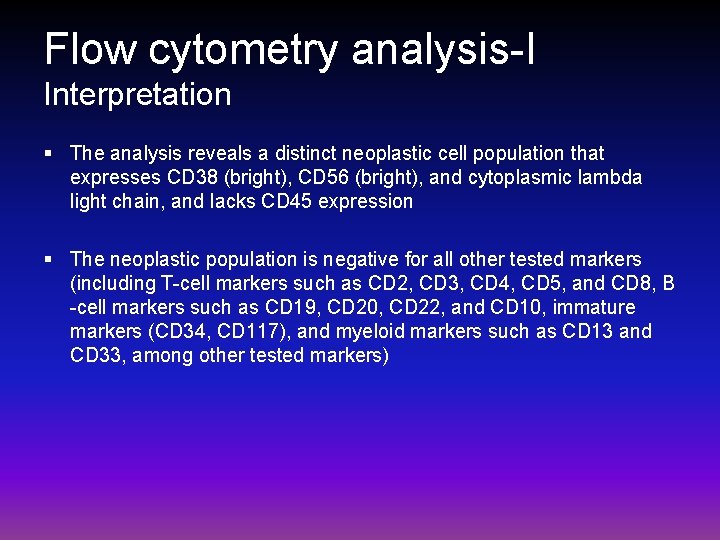
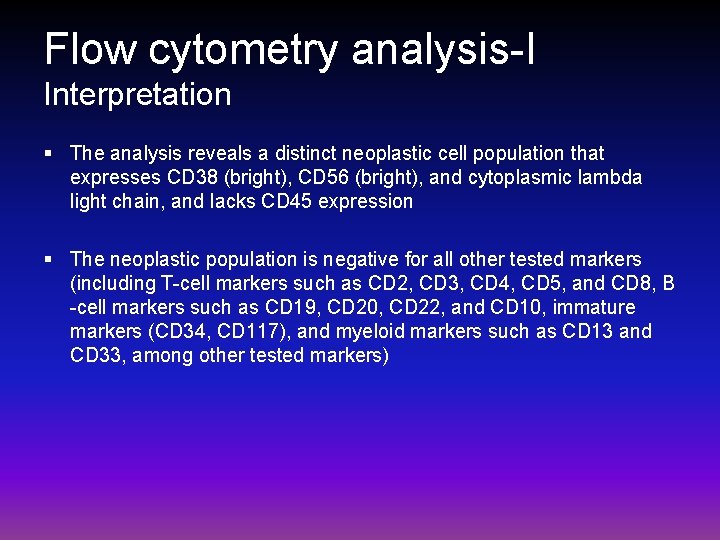
Flow cytometry analysis-I Interpretation § The analysis reveals a distinct neoplastic cell population that expresses CD 38 (bright), CD 56 (bright), and cytoplasmic lambda light chain, and lacks CD 45 expression § The neoplastic population is negative for all other tested markers (including T-cell markers such as CD 2, CD 3, CD 4, CD 5, and CD 8, B -cell markers such as CD 19, CD 20, CD 22, and CD 10, immature markers (CD 34, CD 117), and myeloid markers such as CD 13 and CD 33, among other tested markers)
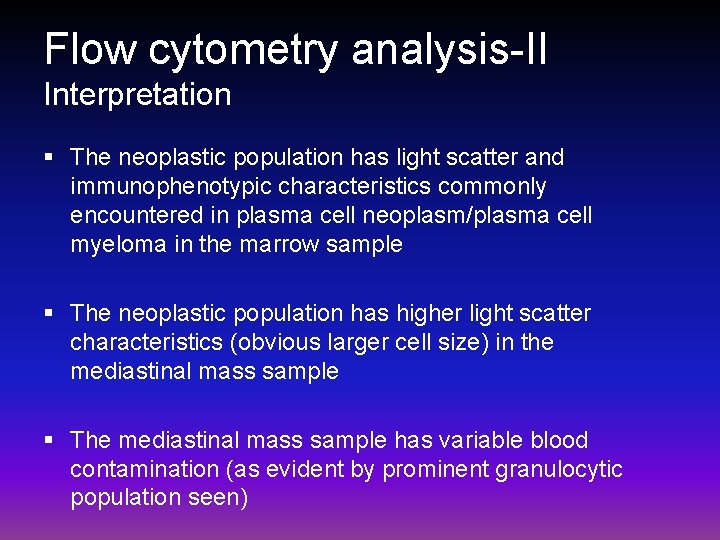
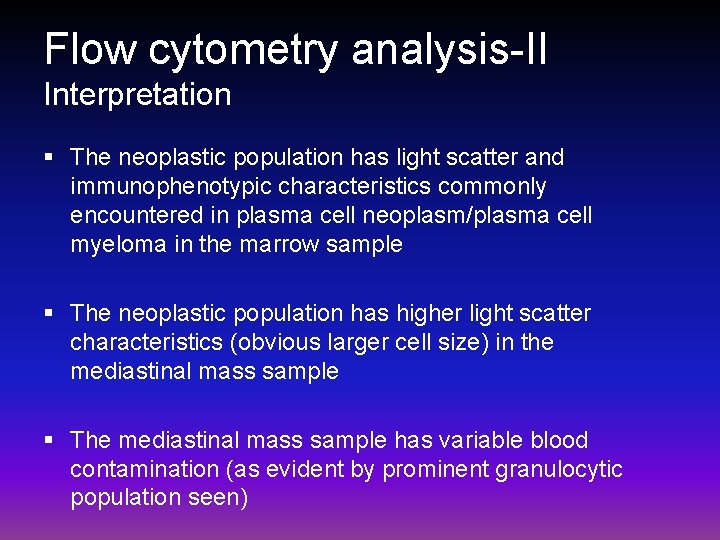
Flow cytometry analysis-II Interpretation § The neoplastic population has light scatter and immunophenotypic characteristics commonly encountered in plasma cell neoplasm/plasma cell myeloma in the marrow sample § The neoplastic population has higher light scatter characteristics (obvious larger cell size) in the mediastinal mass sample § The mediastinal mass sample has variable blood contamination (as evident by prominent granulocytic population seen)
Bone marrow Morphologic assessment
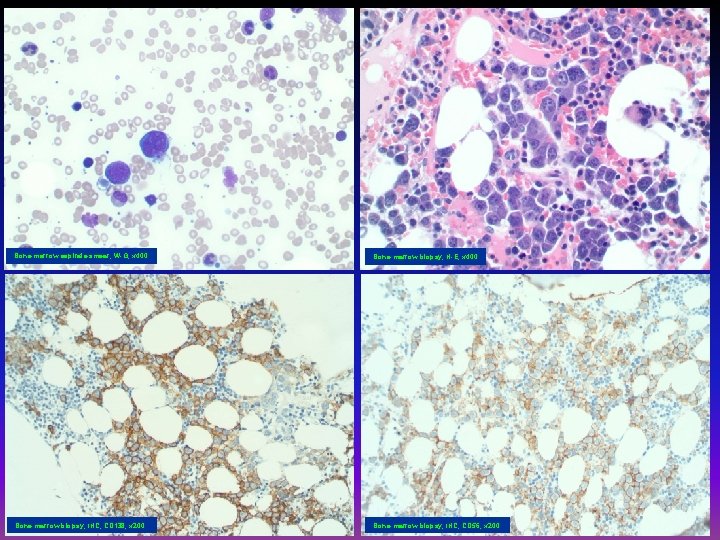
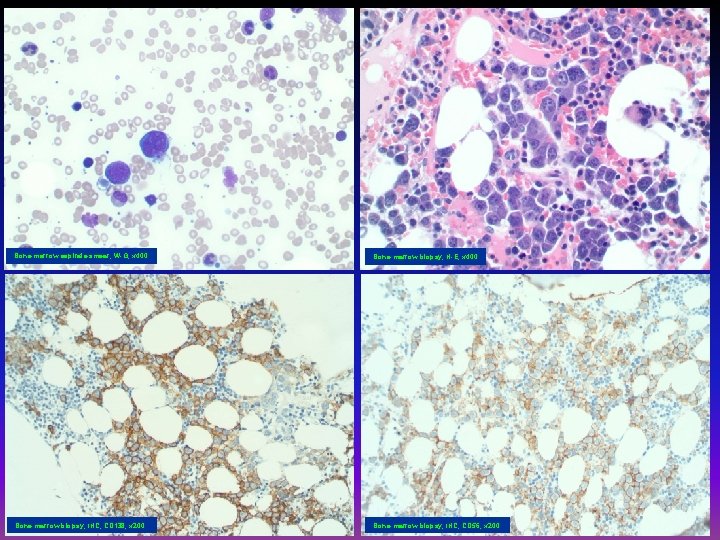
Bone marrow aspirate smear, W-G, x 400 Bone marrow biopsy, H-E, x 400 Bone marrow biopsy, IHC, CD 138, x 200 Bone marrow biopsy, IHC, CD 56, x 200
§ The bone marrow aspirate smears show trilineage hematopoiesis and large neoplastic mononuclear cells with plasmablastic features § The core biopsy sections show 50% cellularity with trilineage hematopoiesis and involvement by neoplastic plasmablastic cells
Immunohistochemistry § Immunostains on core biopsy sections § The neoplastic cells are: § Positive for CD 138, CD 56, MUM 1, and lambda § Negative for kappa, CD 20, CD 3, cyclin-D 1, CD 30, EMA, ALK 1, HHV 8, and EBV-LMP

Mediastinal mass Morphologic assessment

Mediastinal tissue, H-E, x 200 Mediastinal tissue, H-E, x 400 Mediastinal tissue, IHC, CD 138, x 200 Mediastinal tissue, IHC, CD 56, x 200
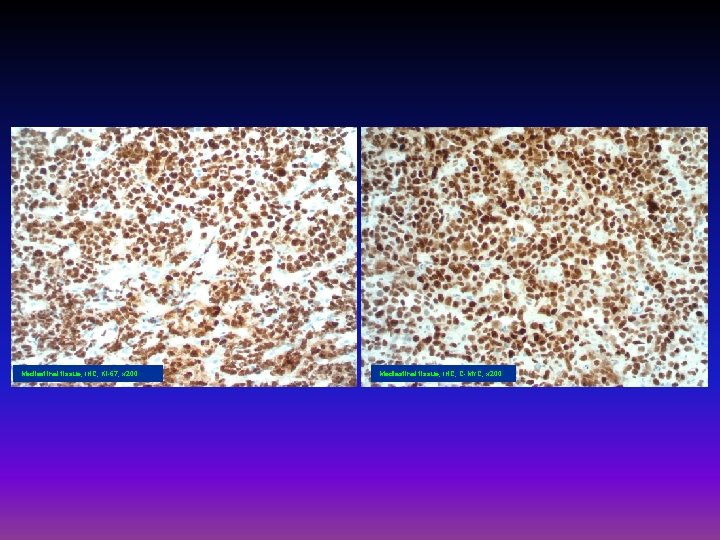
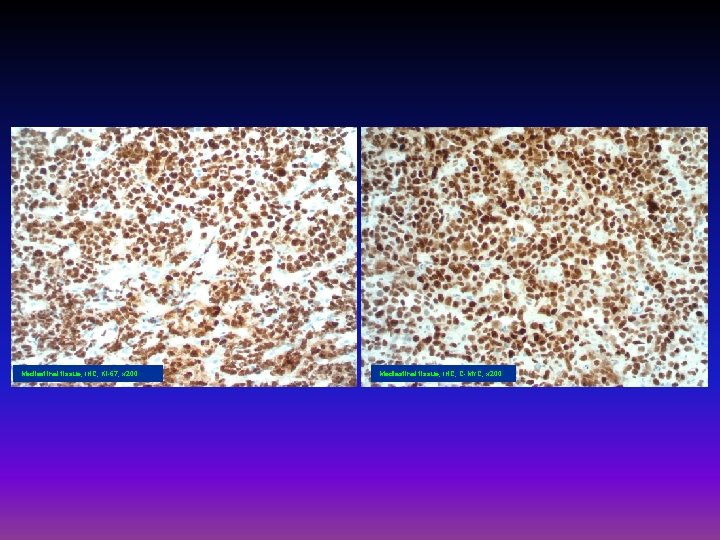
Mediastinal tissue, IHC, Ki-67, x 200 Mediastinal tissue, IHC, C-MYC, x 200
§ The mediastinal biopsy tissue sections show extensive involvement by neoplastic large cells with plasmablastic and plasmacytic features

Immunohistochemistry § Immunostains on mediastinal tissue sections § The neoplastic cells are: § Positive for CD 138, MUM 1, lambda, CD 56 (partial), C-MYC (90%), and Ki-67 (~ 100%) § Negative for CD 20, PAX 5, kappa, CD 30, BCL 6 and ALK 1 § In-situ hybridization for EBER is negative.
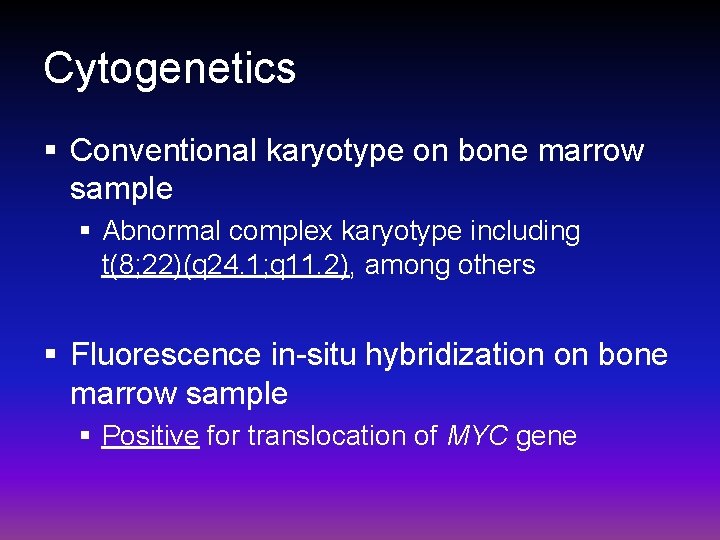
Cytogenetics § Conventional karyotype on bone marrow sample § Abnormal complex karyotype including t(8; 22)(q 24. 1; q 11. 2), among others § Fluorescence in-situ hybridization on bone marrow sample § Positive for translocation of MYC gene
Differential diagnosis § The major differential: § Plasmablastic plasma cell myeloma (PCM) versus § Plasmablastic lymphoma (PBL) v. Primary effusion lymphoma (extracavitary) is less likely based on the immunophenotypic features and the negative HHV 8 status
§ The clinical (the presence of massive nodal involvement in an HIV-positive patient), morphologic (prominent plasmablastic morphology), immunophenotypic (mainly excluding B and T-cell neoplasms and acute leukemia by flow cytometry and high proliferation rate and C-MYC expression by immunohistochemistry), and cytogenetic (C-MYC translocation) findings are in support of plasmablastic lymphoma
Final diagnosis § Plasmablastic lymphoma involving bone marrow and extramedullary tissue (lymph node), EBVnegative, HHV 8 -negative, and C-MYC-positive with C-MYC gene rearrangement and t(8; 22) [IGL/C-MYC] translocation, in HIV-positive patient
Conclusions-I § It is difficult without comprehensive clinicopathologic correlation to differentiate between plasmablastic plasma cell myeloma and plasmablastic lymphoma § The anatomic distribution of the disease is in support of the PBL § Mediastinal mass and generalized lymphadenopathy, bone marrow involvement, and absence of obvious PCM involvement pattern (e. g. lytic bone lesions)
Conclusions-II § In the bone marrow sample of this case, the neoplastic cells exhibit immunophenotypic features usually characteristic of plasma cell myeloma (CD 38+ bright, CD 56+ bright, and CD 45 -) § CD 56 expression is encountered in about 25% of all PBL and in 27% of those occur in HIV+ patients § Blood. 2015; 125(15): 2323 -2330
Conclusions-III § C-MYC gene rearrangement is seen in PBL and reported in those occuring in HIV+ patients § It could be also seen in aggressive PCM or with PCM with plasmablastic evolution § PBL is more commonly seen in HIV+ patients than PCM § The presence of Epstein-Barr virus (EBV) is in support of PBL over PCM § EBV status is negative in this case study and therefore of noncontributory diagnostic value
References § Castillo JJ, et al. The biology and treatment of plasmablastic lymphoma. Blood 2015, 125: 2323 -30. § Lorsbach RB, et al. Plasma cell myeloma and related neoplasms. Am J Clin Pathol 2011, 136: 168 -82. § Valera A, et al. IG/MYC rearrangements are the main cytogenetic alteration in plasmablastic lymphomas. Am J Surg Pathol 2010, 34: 1686 -94. § Taddesse-Heath L, et al. Plasmablastic lymphoma with MYC translocation: evidence for a common pathway in the generation of plasmablastic features. Mod Pathol 2010, 23: 991 -9. § Bogusz AM, et al. Plasmablastic lymphomas with MYC/Ig. H rearrangement: report of three cases and review of the literature. Am J Clin Pathol 2009, 132: 597 -605.
 Iccs
Iccs Iccs 2016 cytometry
Iccs 2016 cytometry Iccs denver
Iccs denver Cbc normal range
Cbc normal range Iata iccs
Iata iccs Master csi
Master csi Law & order: criminal mind
Law & order: criminal mind Csi computer crime and security survey
Csi computer crime and security survey Csi 3120
Csi 3120 Csi 3120
Csi 3120 Csi 321
Csi 321 Csi in project management
Csi in project management Csi handwriting analysis
Csi handwriting analysis Csi varese
Csi varese Csi framework
Csi framework Csi
Csi Csi 3140
Csi 3140 Csi 3140
Csi 3140 Csi 3140
Csi 3140 Csi 3140
Csi 3140 Csi 3131
Csi 3131 Csi 2911
Csi 2911 Csi 2911
Csi 2911 While the csi team is searching the crime scene, _____.
While the csi team is searching the crime scene, _____. Csi great lakes region
Csi great lakes region Bnl csi
Bnl csi Csi uottawa
Csi uottawa Csi global v card
Csi global v card Mario marchand
Mario marchand Csi dinner edition answers
Csi dinner edition answers Csi 2132
Csi 2132