IBD Dr Samantha Chambers FY 2 Aims What
IBD Dr Samantha Chambers FY 2
Aims �What is IBD �Differences between UC and Crohn’s �Presentation �Extra-intestinal manifestations �Investigations �Management �Case scenario
What is IBD? The boring bit � Inflammatory bowel disease: a group of idiopathic inflammatory conditions affecting the gastrointestinal tract � Usually affect 15 -30 age group, but any age, UC shows bimodal incidence(>60) � No major sex difference � More common in Western world � Mainly Crohn’s disease and UC � Crohn’s 50 -100 cases/ 100, 000 population � UC twice as common as Crohn’s � Multifactorial aetiology: � Crohn’s – NOD 2 susceptibility gene � NSAIDs and stress exacerbate disease � Other types � Indeterminate colitis � Microscopic colitis which you DO NOT need to worry about!!
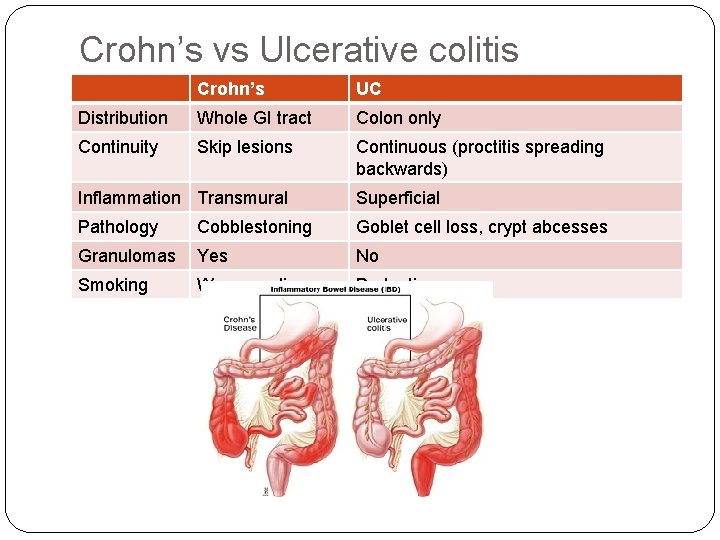
Crohn’s vs Ulcerative colitis Crohn’s UC Distribution Whole GI tract Colon only Continuity Skip lesions Continuous (proctitis spreading backwards) Inflammation Transmural Superficial Pathology Cobblestoning Goblet cell loss, crypt abcesses Granulomas Yes No Smoking Worsens disease Protective Picture here
Presentation � Can be hard to distinguish the 2 from history – there a few clues � Diarrhoea (nocturnal diarrhoea is always pathological) � +++ in UC �+/- blood �+/- mucus � Crampy abdominal pain � Weight loss � Tenesmus, urgency – rectal disease � Fever, malaise, anorexia – active disease � Perianal disease (commoner in Crohn’s) – fistulas, fissures � RIF mass (Crohn’s) � Oral apthous ulcers (commoner in Crohn’s) � Clubbing (commoner in Crohn’s)
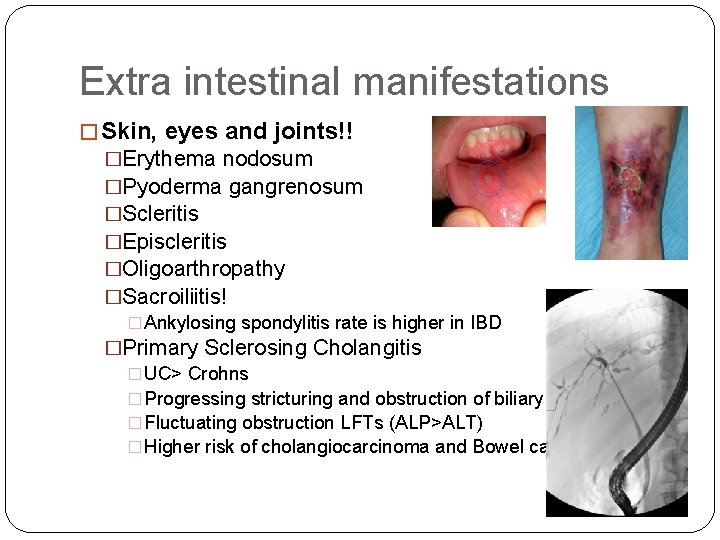
Extra intestinal manifestations � Skin, eyes and joints!! �Erythema nodosum �Pyoderma gangrenosum �Scleritis �Episcleritis �Oligoarthropathy �Sacroiliitis! � Ankylosing spondylitis rate is higher in IBD �Primary Sclerosing Cholangitis � UC> Crohns � Progressing stricturing and obstruction of biliary tree � Fluctuating obstruction LFTs (ALP>ALT) � Higher risk of cholangiocarcinoma and Bowel cancer
Differential diagnoses � Inflammatory � UC � Crohn’s disease � Infective colitis � Acute abdomen � Appendicitis � � � � Diverticular disease Cancer Pseudomembranous colitis Radiation colitis Ischaemic colitis Lymphoma Don’t forget Gynae! � Ectopic pregnancy � Ovarian cyst
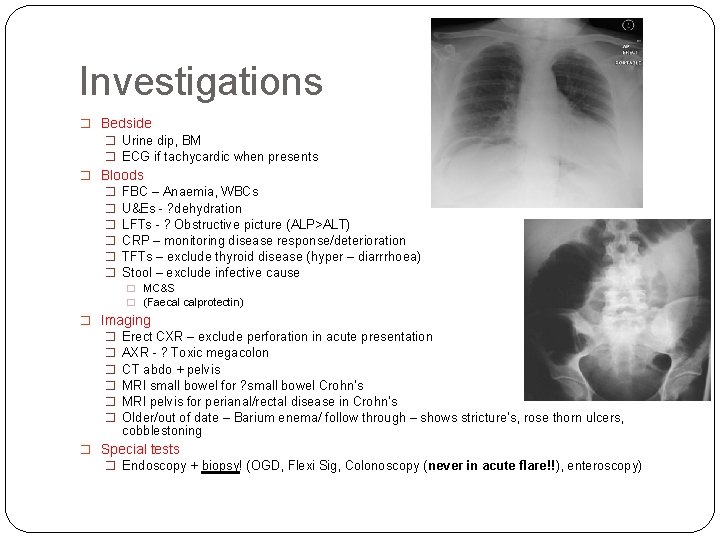
Investigations � Bedside � Urine dip, BM � ECG if tachycardic when presents � Bloods � FBC – Anaemia, WBCs � U&Es - ? dehydration � LFTs - ? Obstructive picture (ALP>ALT) � CRP – monitoring disease response/deterioration � TFTs – exclude thyroid disease (hyper – diarrrhoea) � Stool – exclude infective cause � MC&S � (Faecal calprotectin) � Imaging � Erect CXR – exclude perforation in acute presentation � AXR - ? Toxic megacolon � CT abdo + pelvis � MRI small bowel for ? small bowel Crohn’s � MRI pelvis for perianal/rectal disease in Crohn’s � Older/out of date – Barium enema/ follow through – shows stricture’s, rose thorn ulcers, cobblestoning � Special tests � Endoscopy + biopsy! (OGD, Flexi Sig, Colonoscopy (never in acute flare!!), enteroscopy)
Management � Acute presentation: ABCDE!! � Conservative � Patient education (reduce non-complicance), diet advice (eg. low residue if strictures), smoking cessation advice (!) � MDT involvement – IBD nurse specialist, nutritionist, stoma nurse � Medical � Acute - to induce remission � Corticosteroids inc IV hydrocortisone � Infliximab as rescue therapy � Symptomatic – treat anaemia � Chronic - to maintain remission � � � 5 ASAs (Mesalazine) – cornerstone of disease management – take time to work Localised – suppositories/foam enemas to treat proctitis Steroids – out of fashion due to side effects Steroid sparing agents (immunosuppressants e. g. azathioprine, methotrexate) Biologics; � Infliximab – anti-TNF alpha; Adalimumab (Humira) � Surgical � Acute – for toxic megacolon, failure of medical therapy, perforation � Resection/ colectomy (usually Hartmann’s procedure) � Panproctocolectomy is curative for UC � Chronic – resection of Crohn’s strictures � Local surgery in perianal disease � Elective panproctocolectomy for UC – cancer risk
Prognosis �Crohn’s may need several operations (increases adhesions) �Prone to strictures and fistulas �Considerable morbidity, 15% mortality rate �UC – panproctocolectomy is curative �UC patients have higher risk of bowel cancer (>10 yrs) �Need surveillance colonoscopies �N. b. UC + PSC = even higher bowel ca risk
Case scenario � 29 year old female, one month history of loose watery stools, increasing in frequency to 12 times per day now. Occasionally stools have blood and slime mixed in with them. Cramping left iliac fossa pain. Feels unwell and lethargic. On examination, febrile at 38. 2. Has a soft abdomen but slightly distended and tender in the left iliac fossa. PR examination is very painful and reveals fresh blood and mucus on the glove
29 year old female, one month history of loose watery stools, increasing in frequency to 12 times per day now. Occasionally stools have blood and slime mixed in with them. Cramping left iliac fossa pain. Feels unwell and lethargic. On examination, febrile at 38. 2. Has a soft abdomen but slightly distended and tender in the left iliac fossa. PR examination is very painful and reveals fresh blood and mucus on the glove � What are your main differential diagnoses for this lady? � How would you investigate this patient acutely and long term? � Initial management in acute setting? � Long-term management? � Can you compare the clinical presentation and pathological findings for Crohns and UC? � Can you tell me the effect of smoking on UC and Crohns? � What scoring system is used for acute UC? � What are the extra-intestinal manifestations of IBD
Questions ?
- Slides: 13