I Injectable general anaesthetics 1 Barbiturates A Oxybarbiturate

I- Injectable general anaesthetics: 1 - Barbiturates: A- Oxybarbiturate: a- Short-acting: pentobarbital sodium ( Nembutal ). Secobarbital sodium. b-Ultrashort-acting: Methohexital sodium ( Brevane ). B- Thiobarbiturates: Ultrashort-acting-Thiopental sodium -Thyamylal sodium ( Surital ). 2 - Non-barbiturates: Chloral hydrate, Mag. Sulphate, Ketamine hydrochloride.
1 - Barbiturates: which are classified as hypnotic sedatives, their dose-dependent actions range from simple sedation to hypnosis to general anaesthesia. The ultrashort acting barbiturates are derivatives of barbituric acid, which is a combination of Uses: - For induction of general anaesthesia that is to be followed by maintenance with an alant anaesthetic. or short surgical and diagnostic procedures. General effects of ultra-short acting barbiturates: lity to penetrate all tissues of the body. Action of the drug only cease after tissue metabolism or excretion by the kidney. -Acidosis potentiates the action of the barbiturates, therefore, decrease the dose tic patients. - Decreased basal metabolic rate.
General anaesthetic actions: On CNS: - all degrees of depression are produced from mild sedation to coma, depends on barbiturate used, dose, route of administration and the degree of excitability of CNS at time of administration. Barbiturates depress the cerebral cortex and probably the thalamus. They are used in control of convulsion. Barbiturates ygen uptake. used to induce surgical On respiration: - They are respiratory depressants and the degree of depression is ed. On cardiovascular system: - do not produce a significant cardiovascular effect. Cardiac arrhythmias rarely occur. They may cause a transient fall in blood pressure. GIT: - depress intestinal musculature. ** No direct effect on kidney, and therapeutic doses have no effect on liver except in atients with liver damage, the large doses may cause further injury. - Uterus and Fetus: Barbiturates easily diffuse through the placenta into fetal → neonatal asphyxia. circulation - Fate and excretion: - Biotransformed in the liver by microsomal enzyme. -Their metabolites are excreted in the urine. Small amount of pentobarbital are hanged in the urine.
Contraindication: - Patients with hepatitis, renal diseases or in shock. Also, in patients that are less than one month of age does not metabolize the agents as well as older patients. An example of available drugs: Thiopental sodium: (Thiopental, Thiopentol, Nesdonal or Pentothal). - It is ultra short acting barbiturates used in short surgical procedures and as induction agent for inhalation anaesthesia. - It is supplied as powder. The solution is stable for 3 -7 days depending on temperature. - The solution is very alkaline (PH 14) and therefore, irritant if the concentration is greater than 2. 5%. Subcutaneous injection causes necrosis and sloughing of the tissue. It may be alleviated with saline or procaine 1% injection. - The drug should be used as 2. 5% or 1% solution to: -Minimize the risk of causing perivascular damage in case of perivascular seep. - Enable accurate administration, especially in small dogs and cats. - It is important to give the drug ‟ TO EFFECT” and not to give a computed dose since each individual will vary as to its requirements. - However, as a guide, in unpremedicated fit animals, a dose of around use of premedication agents. - The dose should be given slowly over 30 -40 seconds (20 -25 mg/kg may be required for dogs and about 5 mg/kg in equine individual dose). The dose is halved by the use of premedication agents, so that the injection should be stopped once the desired effect is obtained. - Overdose is best treated with continuous O 2 and controlled ventilation.
2 - Non-barbiturates: A- Chloral hydrate: can be used for general anaesthesia, but it has a low analgesic action and the anaesthetic dose approaches the minimal lethal dose. B- Magnesium sulphate: of narrow safety margin, the anaesthetic dose produces marked respiratory and cardiovascular depression. It may be used for euthanasia (one liter of saturated sol. will be sufficient for an adult horse). C- Mag. sulphate + Chloral hydrate: - used for sedation and general anaesthesia. Solutions containing 7% chloral hydrate and 3% mag. sulphate (3 ml/50 kg) in combination with 3. 0 mg/50 kg acepromazine to provide sedation in horse. D- Mag. Sulphate + Chloral hydrate + pentobarbiturate sodium: satisfactory for general anaesthesia, the recovery time may be prolonged and one dose not has good control over the depth of anaesthesia. Preparation: a- 6. 00% chloral hydrate. b- 3. 00% mag. Sulphate. c- 0. 65% pentobarbiturate. Doses: Equine: 30 ml/50 kg. , i. v. Bovine: 20 – 30 ml/50 kg. , i. v. The sedative dose is 1/4 of the anaesthetic dose.
E- Dissociative agents: - Characterized by profound somatic analgesia (complete analgesia) with light plane of unconsciousness (superficial sleep). The animals appear to be dissociated from its environment. -The eyes remain open and laryngeal and swallowing reflexes tend to persist. Stimulation of the extra-pyramidal system occurs so that muscle tone is maintained or even enhanced (malleable rigidity). -Central stimulation of the sympathetic system frequently leads to: Lacrimation and salivation. Tachycardia and increase in blood pressure and cardiac output. -All these drugs are derived from phencyclidine compound. - Examples: (Ketamine: Ketalar®, Ketamar®, Calypsol®) – Telazol®, Vetlar®). It is presented in aqueous solution 100 mg/ml multidose vials. (Tiletamine:
Clinical uses: - Ketamine is used for chemical restraint in both dogs and cats as well as in primates and the larger species (horses and calves). - The advantage of this drug includes its potency, which means that only a small volume is required. - The disadvantage centre on the very poor muscle relaxation achieved when the drug is used alone which makes its usefulness for surgery very limited. - Xylazine is a useful agent to improve muscular relaxation, the degree of visceral analgesia and recovery. It is usually administered at 0. 2 – 0. 5 mg/kg. I. m. 10 – 15 minutes before ketamine induction in small animals and 1. 1 mg/kg. i. v. in horse. Doses of ketamine: - Horse: 2. 2 mg/kg. i. v. - Cattle: 11 mg/kg. i. m. and 2 – 5 mg/kg. i. v. - Sheep &Goat: 2. 2 – 4. 4 mg/kg. i. v. after 0. 04 -0. 06 mg/kg. of xylazine i. v. - Cat: 10 – 30 mg/kg. i. m and 2 – 5 mg/kg. i. v. 10 mg/kg i. m. + xylazine 1 mg/kg i. m. - In dogs: - xylazine and ketamine usage is normally safe but has occasionally resulted in adverse responses of bradycardia, tachycardia, seizures or cardiopulmonary distress. Dose: ketamine (10 mg/kg)/xylazine (1 mg/kg).
F- Propofol (Diprivan® 1%): - It is licensed for use in dogs and cats for the induction and maintenance of short term anaesthesia. - Although relatively expensive, propofol offers certain advantages over other short term anaesthetic agents which make it the ideal choice in certain situations. - The rapid and full recovery of consciousness in some minutes (15 – 20 minutes) following a single intravenous dose means that this is a drug which can truly be used for day or post evening surgery cases.
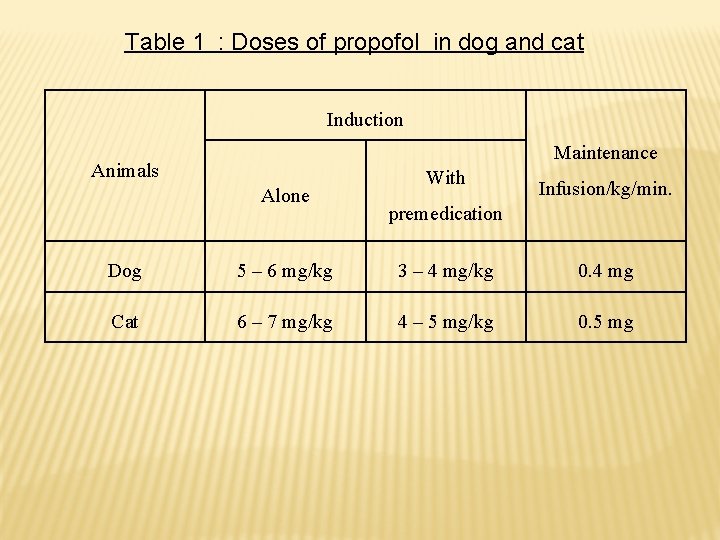
Table 1 : Doses of propofol in dog and cat Induction Maintenance Animals Alone With Infusion/kg/min. premedication Dog 5 – 6 mg/kg 3 – 4 mg/kg 0. 4 mg Cat 6 – 7 mg/kg 4 – 5 mg/kg 0. 5 mg
G- Steroid anaesthetics: Ex. , Saffan®: a mixture of 2 steroid agents is used: alphazalone/alphadolone acetate.
Inhalation anaesthesia Advantages: 1 - It is the safest one to anaesthetize the poor risk patient. 2 - The depth of the anaesthesia can be readily controlled by the anaesthetist. (Better control over the depth of anaesthesia is possible). 3 - Clinical anaesthesia by inhalation has been accomplished quiet satisfactory in all species. 4 - It can be used for essentially all types of major surgery in small animals and equine.
Disadvantages: 1 - Many are explosive and inflammable; some are irritant to body tissues. 2 - Required trained personnel to monitor the patient. 3 - More complex equipment is required that is expensive to buy and maintain rather than, it is not easily transported.
- Tidal volume: The volume of inspired or expired air in one breath. - Minute volume: Tidal volume X number of breaths per minute. - Dead space: a- Anatomical dead space: is that part of respiratory tract where there is no gas exchange. b- Physiological dead space: Some alveoli are not active (That portions of the alveoli not directly involved in gas exchange). - Gas exchange occurs in the alveoli across alveolar membrane by the process of diffusion to enter the blood stream. The rate of diffusion is controlled by the concentration gradient between the alveolus and blood ream as well as the lipid solubility of the drug.
During the induction period, the concentration of the agent in the alveolus is high and the concentration in the blood is low and this creates centration gradient. - Because of the relative high lipid solubility, inhalation agents readily leave ation and enter the brain, inducing anaesthesia oli. the - Anaesthesia is maintained as long as sufficient quantities of inhalation are delivered to alveoli → blood → brain. agent - When the concentration of inhalation agent administered is reduced or discontinued by adjusting the anaesthetic machine vaporizer, the amount of anaesthetic in the alveolus is reduced. Since blood level is still high, the concentration gradient now favors the diffusion of anaesthetic from blood
Inhalant general anaesthetics classified into: A- Gaseous: e. g. Nitrous oxide, Ethylene and Cyclopropane. All of the gaseous agents are administered by means of a closed or semiclosed system. B-Volatile liquid: Ethyl ether, Chloroform, Ethyl chloride, Halothane, Methoxyflurane, Trichloroethylene, Enflurane, Isoflurane and others. Volatile liquid agents are administered by a variety of methods which include insufflations, open nonrebreathing.
Gaseous form: Nitrous oxide (N 2 O ) - Is an odorless and colorless inert nonflammable gas. It can exist as liquid under pressure at room temperature. It can be used as adjunct to anaesthesia with other inhalation agents, particularly halothane. It is seldom used as the sole anaesthetic agent in domestic animals (analgesic action is much greater in human than in animals). Its use in veterinary medicine mainly to reduce the amount of potent inhalant anaesthetic (lowers its concentration and reduces the minimum alveolar concentration (MAC) by 20 to 30 %). - N 2 O speed the uptake of other anaesthetic gases into blood stream by the‟ second gas effect” when used at high concentrations (50 – 70 % of the total gas flow). - Nitrous oxide has an extremely low solubility coefficient and is associated duction and recovery rates. with - Nitrous oxide has little effect on cardiovascular, respiratory, hepatic, or stems and is considered to have a wide margin of safety. Nitrous oxide is contraindicated in the following conditions: eumothorax - Gastrointestinal obstruction
Halothane (Fluthane): - It is a potent inhalant anaesthetic. It posses many qualities of an ideal anaesthetic, noninflammability, nonexplosive and providing excellent muscle relaxation. It does not cause extensive irritation to mucous and mbranes. - Halothane is a potent myocardial depressant, which diminishes the contractility in proportion to the depth of anaesthesia. - Bradycardia. – otension. - Strong respiratory depressant that reduces the tidal volume. - Halothane is associated with malignant hypertension which is a fatal of thermoregulation. disorder
Isoflurane: - It is the newest inhalant anaesthetic available. Its vapour pressure closely similar to halothane (Both may reach a concentration of 30% at 20 CO), so that it can be administered in halothane type vaporizer. - Isoflurane cause small decrease in cardiac output. It has little or no depression of the myocardial cells. – It is respiratory depressant. - Isoflurane has little hepatic metabolism, and very little renal excretion of metabolites, so, it is well suited to animals with liver or kidney disease. - Isoflurane has little or no analgesic effect in the postanaesthetic period.
- Slides: 19