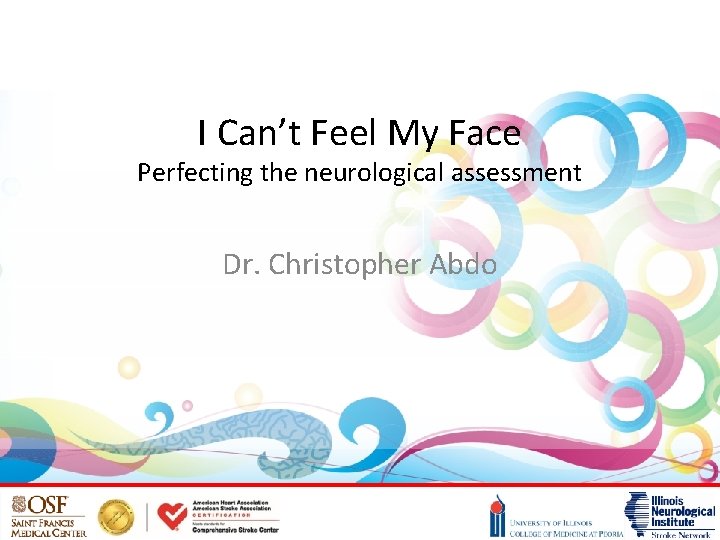
I Cant Feel My Face Perfecting the neurological




- Slides: 30
I Can’t Feel My Face Perfecting the neurological assessment Dr. Christopher Abdo
Objectives • Discuss National Institute of Health Stroke Scale (NIHSS) • Be able to perform & accurately score the NIHSS • Discuss common pitfalls
What is the NIHSS? • Standardized and repeatable assessment of stroke patients – High intra/interobserver reliability (RNs/physicians) • Clinical research and communication tool • Can predict stroke severity & outcomes
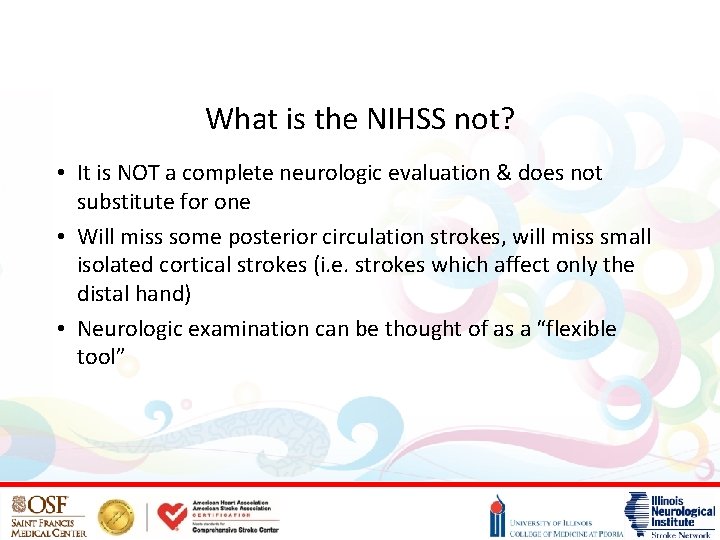
What is the NIHSS not? • It is NOT a complete neurologic evaluation & does not substitute for one • Will miss some posterior circulation strokes, will miss small isolated cortical strokes (i. e. strokes which affect only the distal hand) • Neurologic examination can be thought of as a “flexible tool”
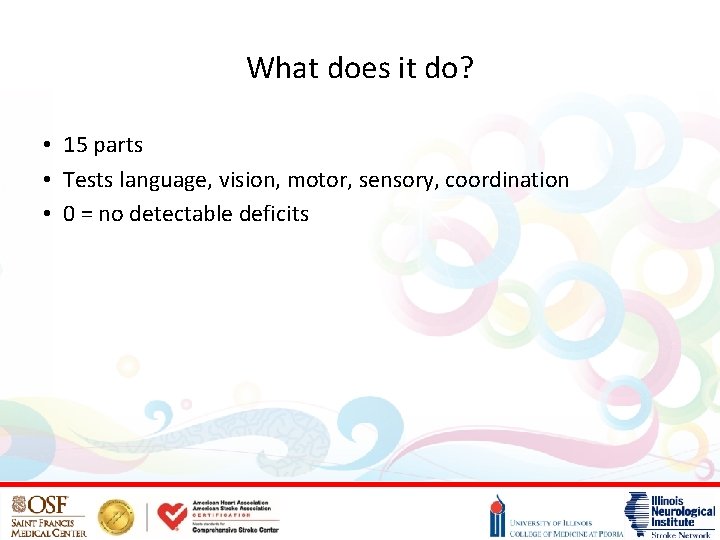
What does it do? • 15 parts • Tests language, vision, motor, sensory, coordination • 0 = no detectable deficits

Common pitfall You don’t do this every day, so you are not sure how exactly to perform or score the exam. Find one of these books in your ER. Or go to: https: //stroke. nih. gov/ This is available in pdf & Power. Point Graphics which will be needed during the exam are contained in this book. These can be used to supplement a neurologic examination.
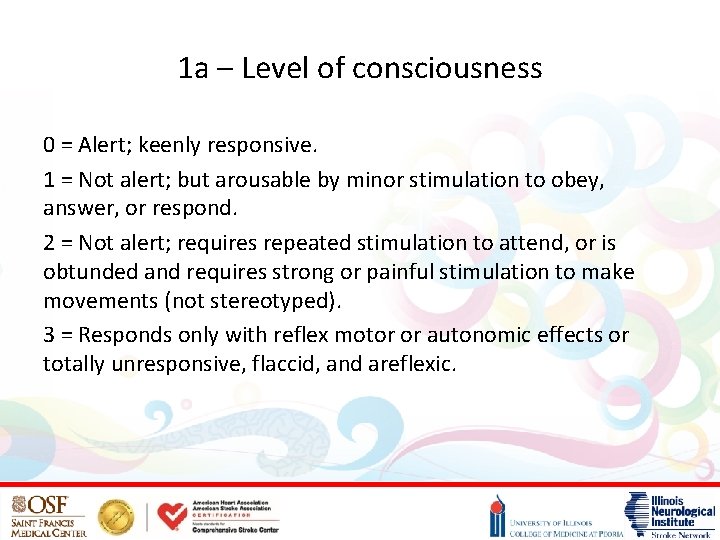
1 a – Level of consciousness 0 = Alert; keenly responsive. 1 = Not alert; but arousable by minor stimulation to obey, answer, or respond. 2 = Not alert; requires repeated stimulation to attend, or is obtunded and requires strong or painful stimulation to make movements (not stereotyped). 3 = Responds only with reflex motor or autonomic effects or totally unresponsive, flaccid, and areflexic.
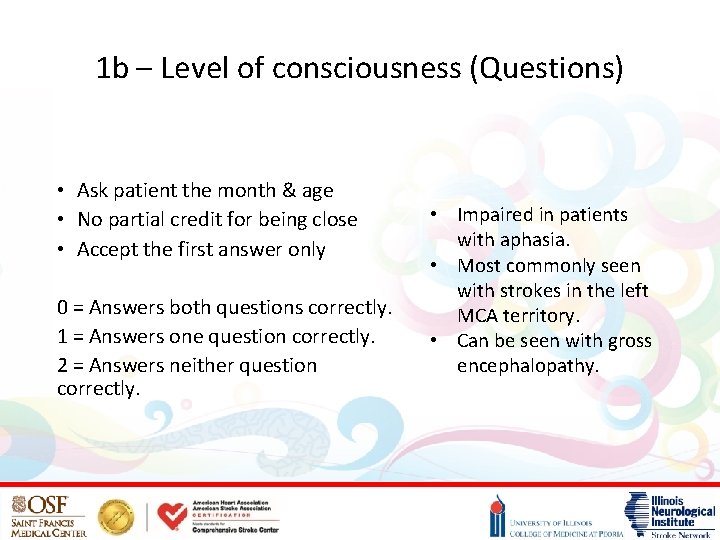
1 b – Level of consciousness (Questions) • Ask patient the month & age • No partial credit for being close • Accept the first answer only 0 = Answers both questions correctly. 1 = Answers one question correctly. 2 = Answers neither question correctly. • Impaired in patients with aphasia. • Most commonly seen with strokes in the left MCA territory. • Can be seen with gross encephalopathy.
1 c – Level of consciousness (Commands) • Ask patient to open and close eyes • Ask patient to grip and release the non-paretic hand • If the patient does not respond, demonstrate the command. • 0 = Performs both tasks correctly. • 1 = Performs one task correctly. • 2 = Performs neither task correctly. Some patients may not be able to respond to your verbal cues, but be able to mimic your demonstration. This is consistent with impaired comprehension from stroke, most commonly seen with left MCA territory strokes.

2 – Best gaze • Tests only horizontal eye movements • Can be assessed on all patients • May try moving from one side of room to the other • Attempt oculocephalic if C-spine is cleared. • We are normally taught the occulocephalic reflex in patients who are comatose. • A different response is expected in an awake patient. • Does not test for vertical eye • 0 = Normal. movement or nystagmus • 1 = Partial gaze palsy; gaze is abnormal in one or both eyes, but forced deviation or total gaze which could be seen in a paresis is not present. posterior circulation stroke • 2 = Forced deviation, or total gaze paresis not • In a stroke, the patient overcome by the oculocephalic maneuver. normally looks towards the stroke “right way eyes”

Normal in comatose patient Seen in awake patient fixating on object.
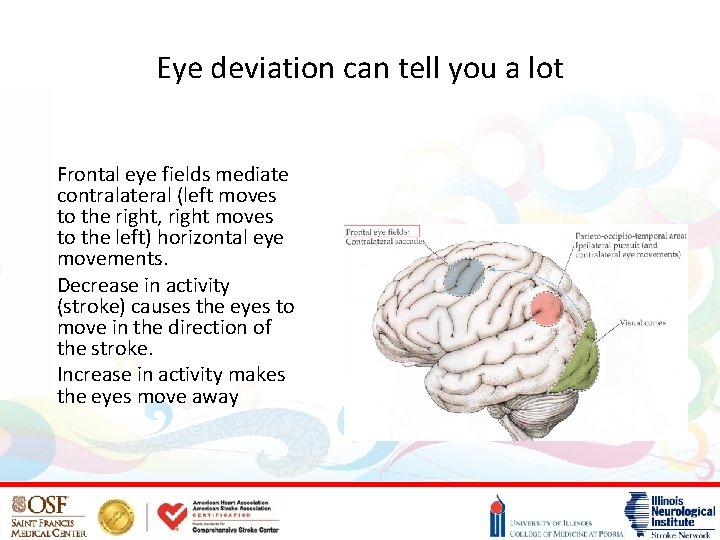
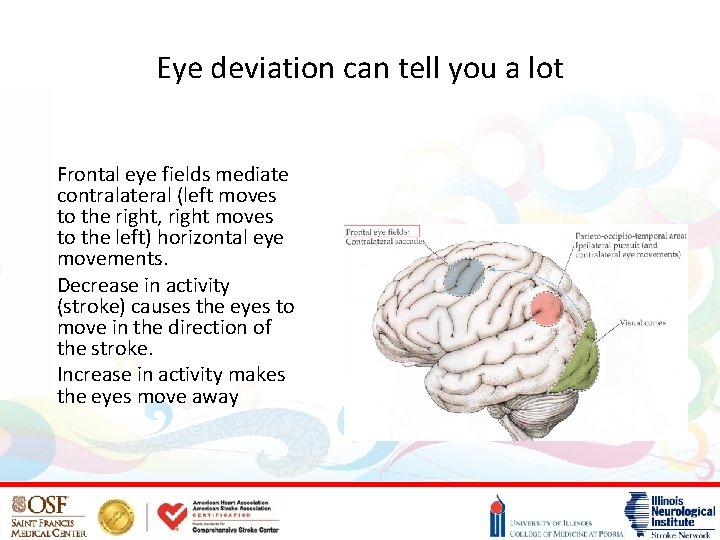
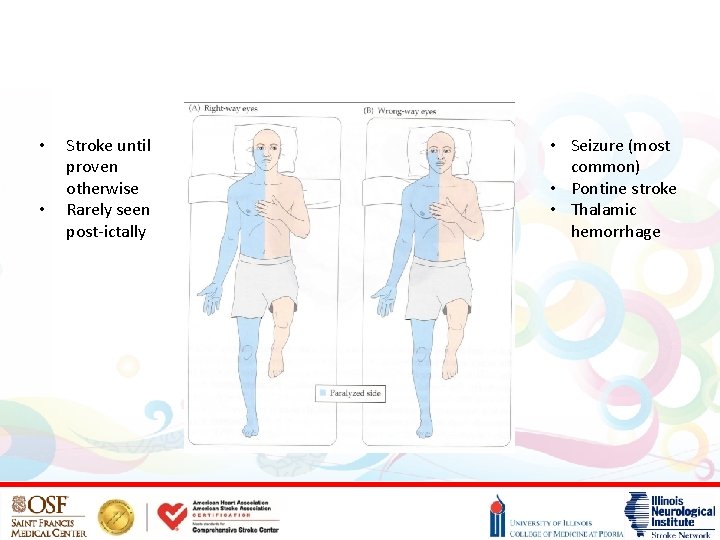
Eye deviation can tell you a lot Frontal eye fields mediate contralateral (left moves to the right, right moves to the left) horizontal eye movements. Decrease in activity (stroke) causes the eyes to move in the direction of the stroke. Increase in activity makes the eyes move away
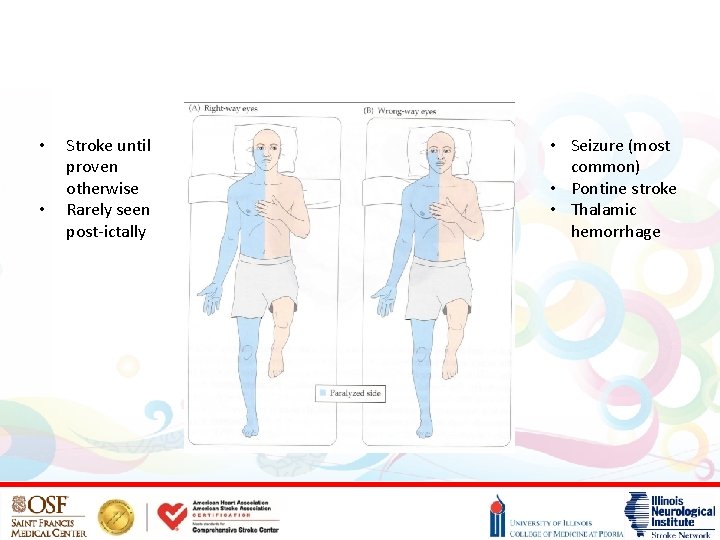
• • Stroke until proven otherwise Rarely seen post-ictally • Seizure (most common) • Pontine stroke • Thalamic hemorrhage
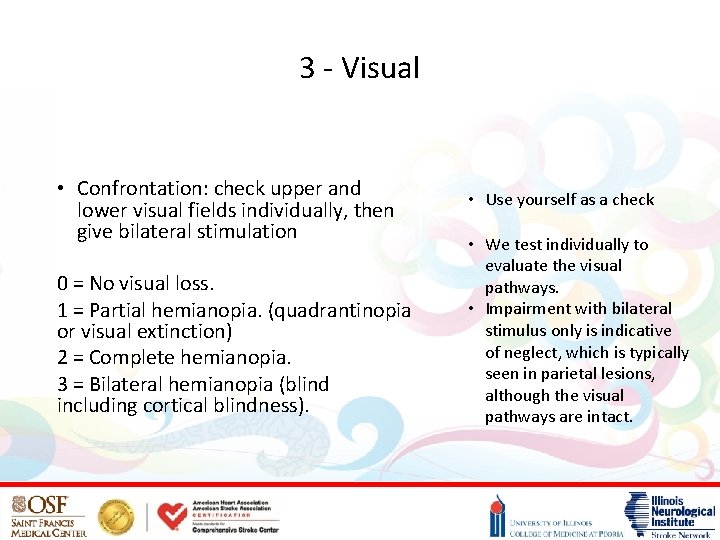
3 - Visual • Confrontation: check upper and lower visual fields individually, then give bilateral stimulation 0 = No visual loss. 1 = Partial hemianopia. (quadrantinopia or visual extinction) 2 = Complete hemianopia. 3 = Bilateral hemianopia (blind including cortical blindness). • Use yourself as a check • We test individually to evaluate the visual pathways. • Impairment with bilateral stimulus only is indicative of neglect, which is typically seen in parietal lesions, although the visual pathways are intact.
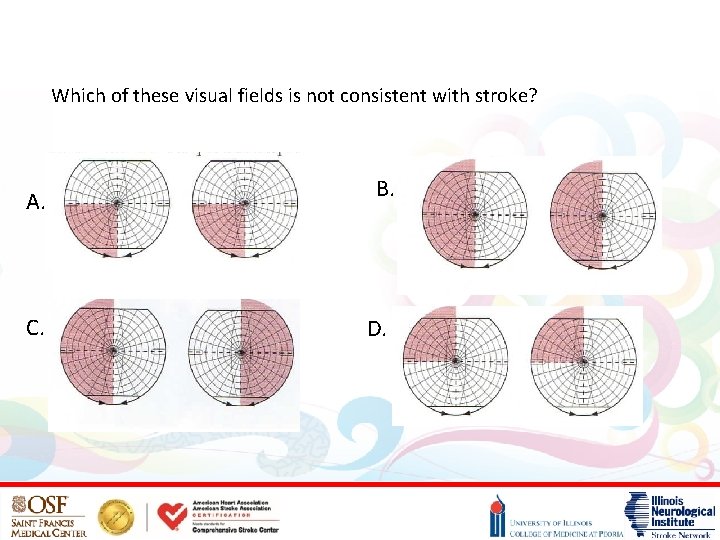
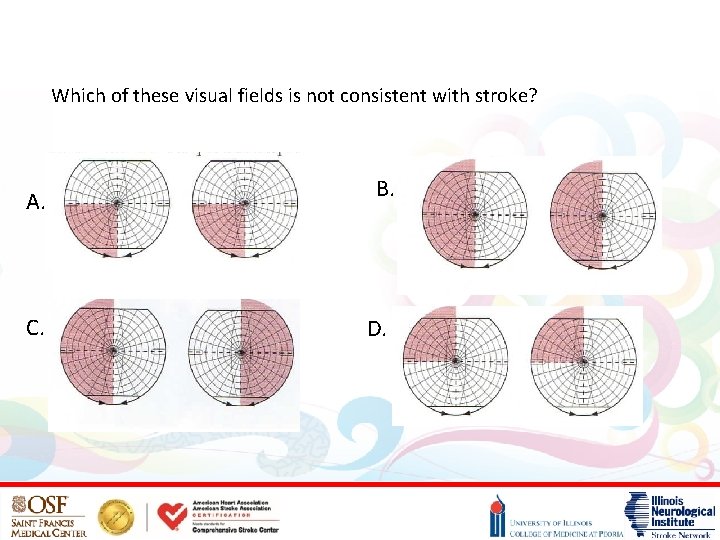
Which of these visual fields is not consistent with stroke? A. C. B. D.
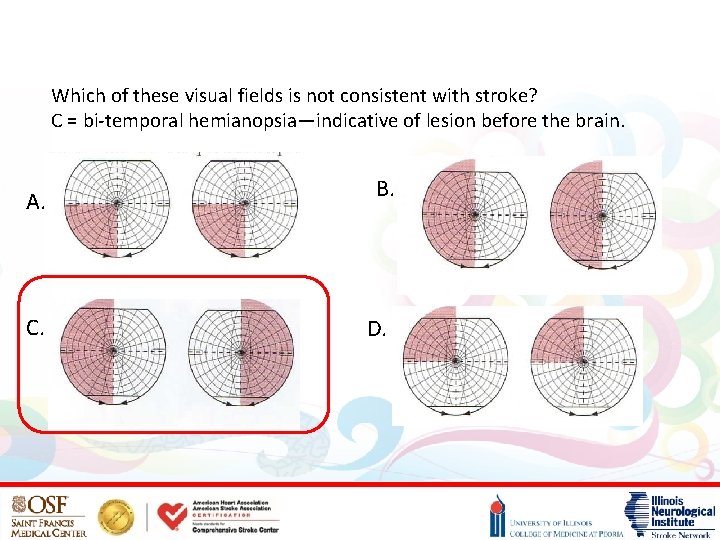
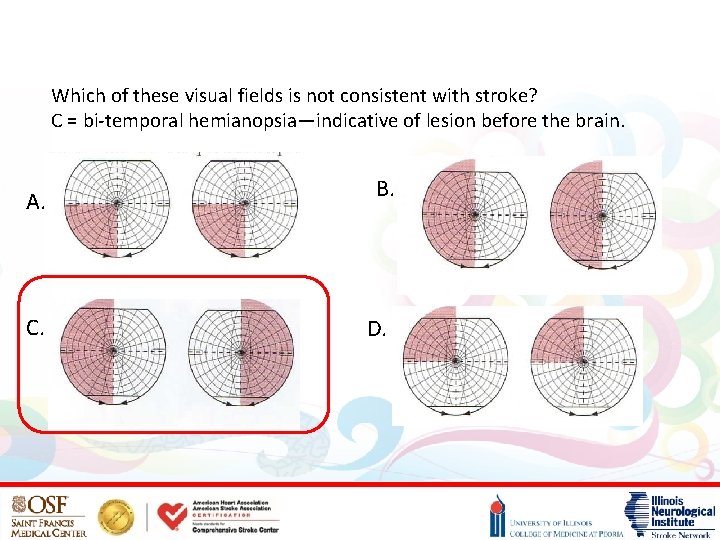
Which of these visual fields is not consistent with stroke? C = bi-temporal hemianopsia—indicative of lesion before the brain. A. C. B. D.
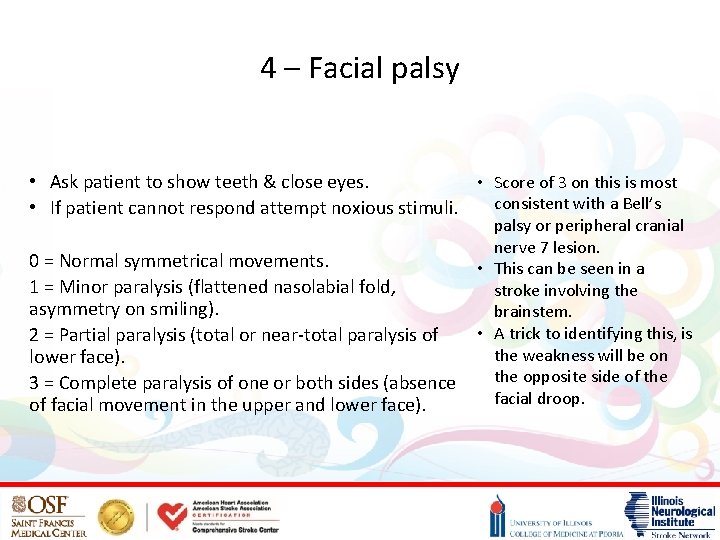
4 – Facial palsy • Ask patient to show teeth & close eyes. • Score of 3 on this is most consistent with a Bell’s • If patient cannot respond attempt noxious stimuli. palsy or peripheral cranial nerve 7 lesion. 0 = Normal symmetrical movements. • This can be seen in a 1 = Minor paralysis (flattened nasolabial fold, stroke involving the asymmetry on smiling). brainstem. • A trick to identifying this, is 2 = Partial paralysis (total or near-total paralysis of the weakness will be on lower face). the opposite side of the 3 = Complete paralysis of one or both sides (absence facial droop. of facial movement in the upper and lower face).

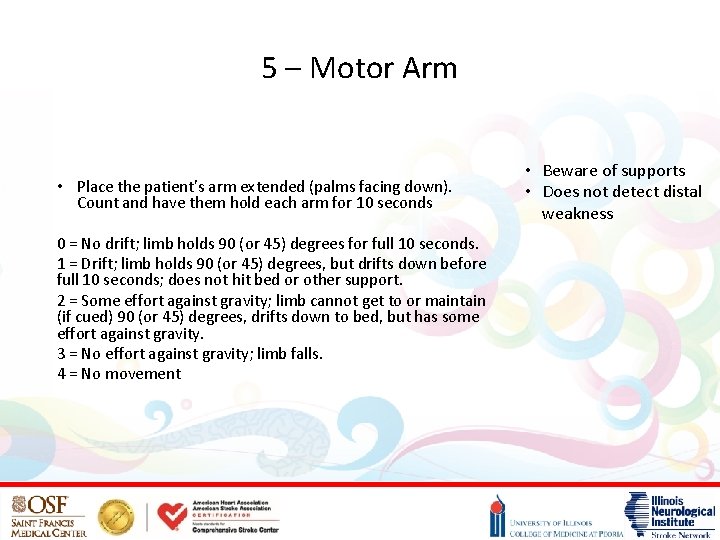
5 – Motor Arm • Place the patient’s arm extended (palms facing down). Count and have them hold each arm for 10 seconds 0 = No drift; limb holds 90 (or 45) degrees for full 10 seconds. 1 = Drift; limb holds 90 (or 45) degrees, but drifts down before full 10 seconds; does not hit bed or other support. 2 = Some effort against gravity; limb cannot get to or maintain (if cued) 90 (or 45) degrees, drifts down to bed, but has some effort against gravity. 3 = No effort against gravity; limb falls. 4 = No movement • Beware of supports • Does not detect distal weakness
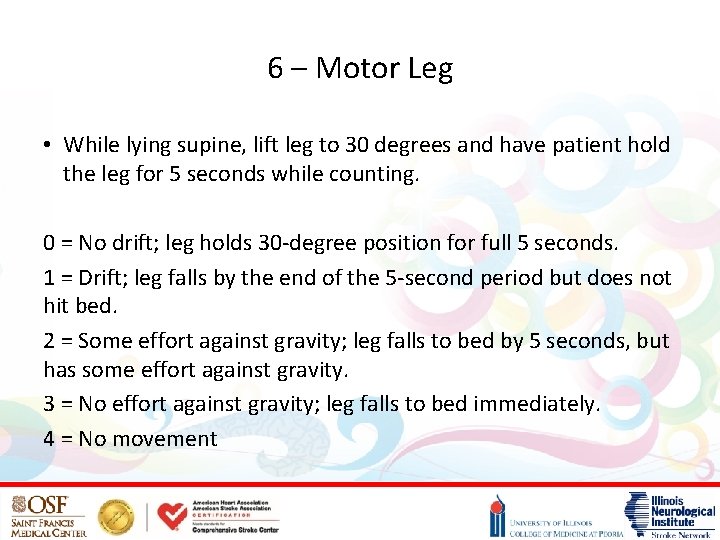
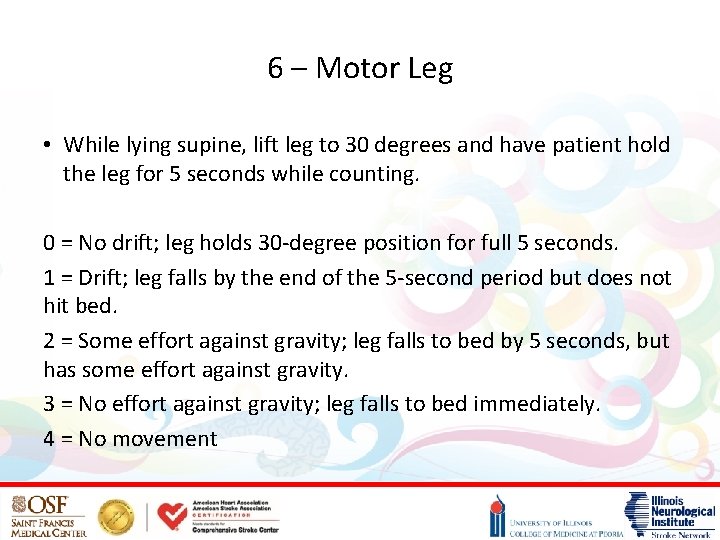
6 – Motor Leg • While lying supine, lift leg to 30 degrees and have patient hold the leg for 5 seconds while counting. 0 = No drift; leg holds 30 -degree position for full 5 seconds. 1 = Drift; leg falls by the end of the 5 -second period but does not hit bed. 2 = Some effort against gravity; leg falls to bed by 5 seconds, but has some effort against gravity. 3 = No effort against gravity; leg falls to bed immediately. 4 = No movement
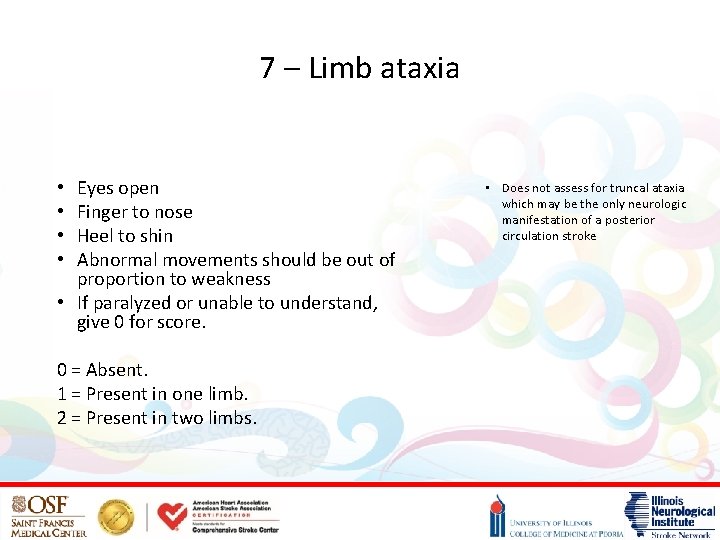
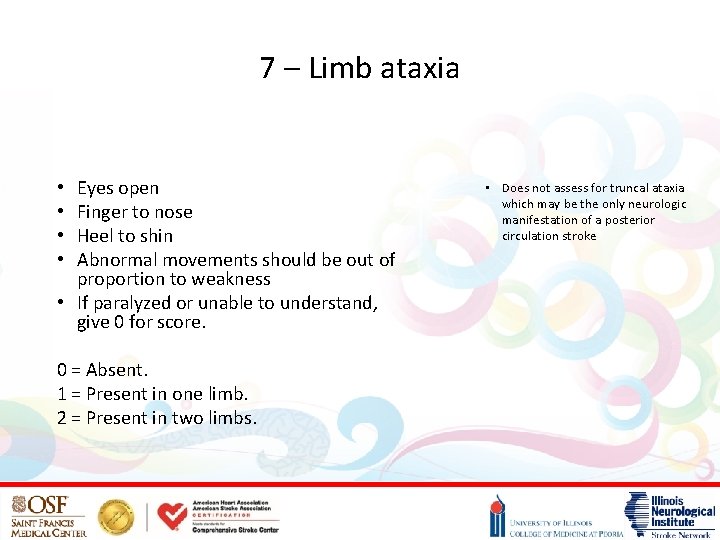
7 – Limb ataxia Eyes open Finger to nose Heel to shin Abnormal movements should be out of proportion to weakness • If paralyzed or unable to understand, give 0 for score. • • 0 = Absent. 1 = Present in one limb. 2 = Present in two limbs. • Does not assess for truncal ataxia which may be the only neurologic manifestation of a posterior circulation stroke
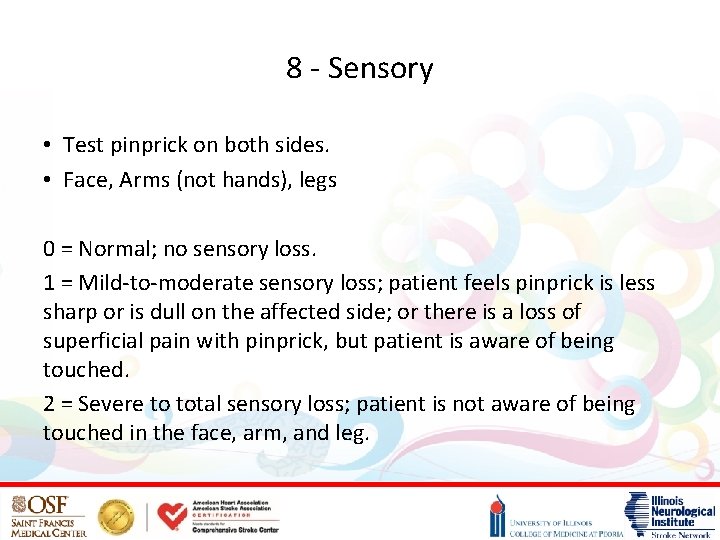
8 - Sensory • Test pinprick on both sides. • Face, Arms (not hands), legs 0 = Normal; no sensory loss. 1 = Mild-to-moderate sensory loss; patient feels pinprick is less sharp or is dull on the affected side; or there is a loss of superficial pain with pinprick, but patient is aware of being touched. 2 = Severe to total sensory loss; patient is not aware of being touched in the face, arm, and leg.
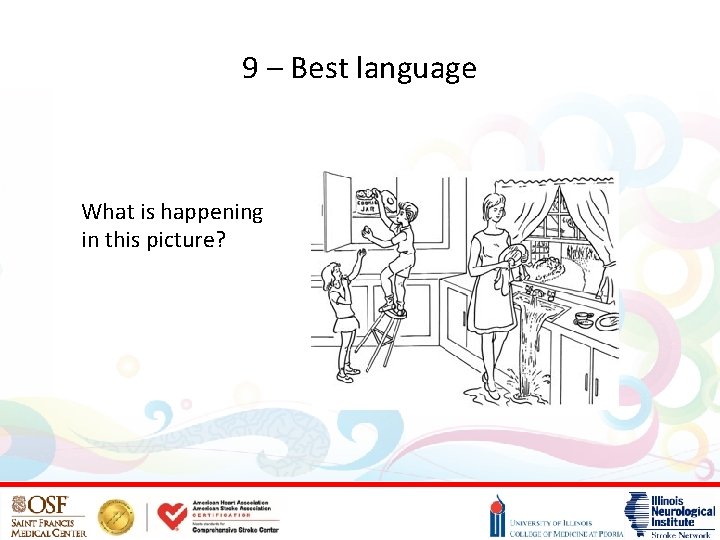
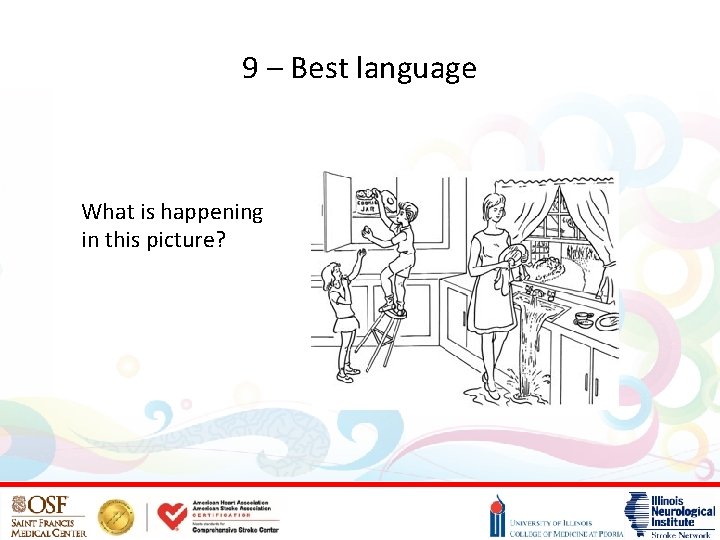
9 – Best language What is happening in this picture?
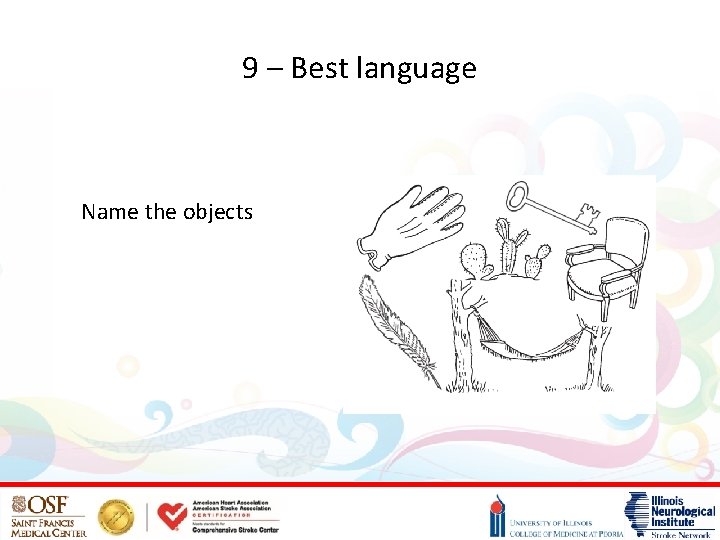
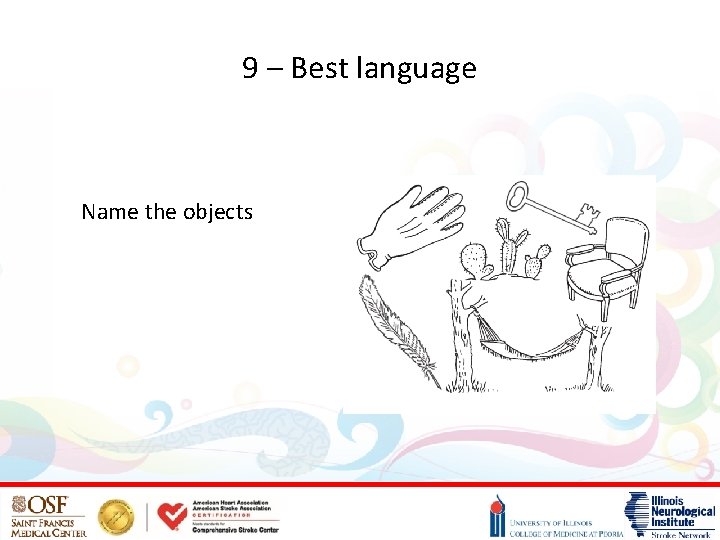
9 – Best language Name the objects
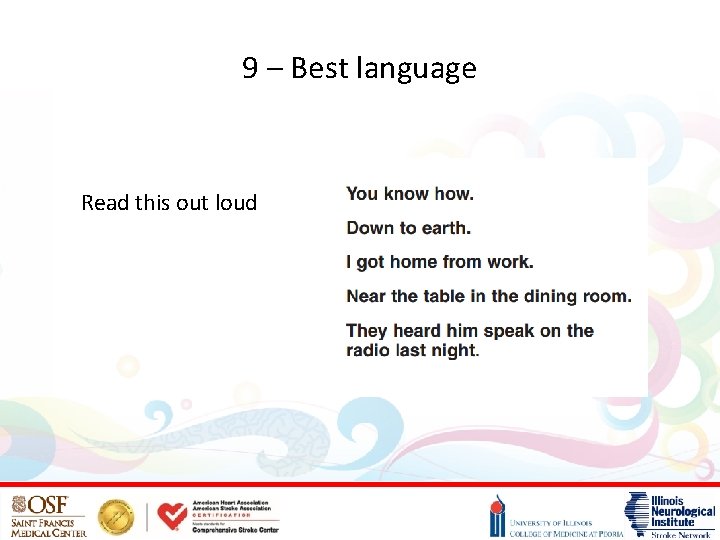
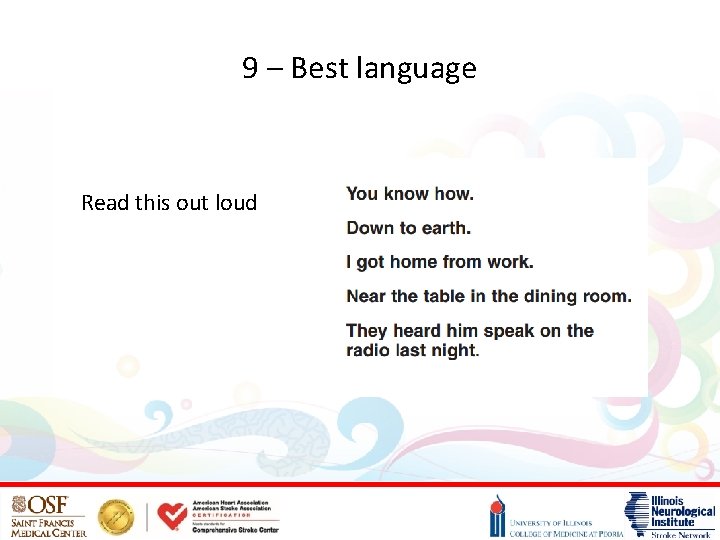
9 – Best language Read this out loud
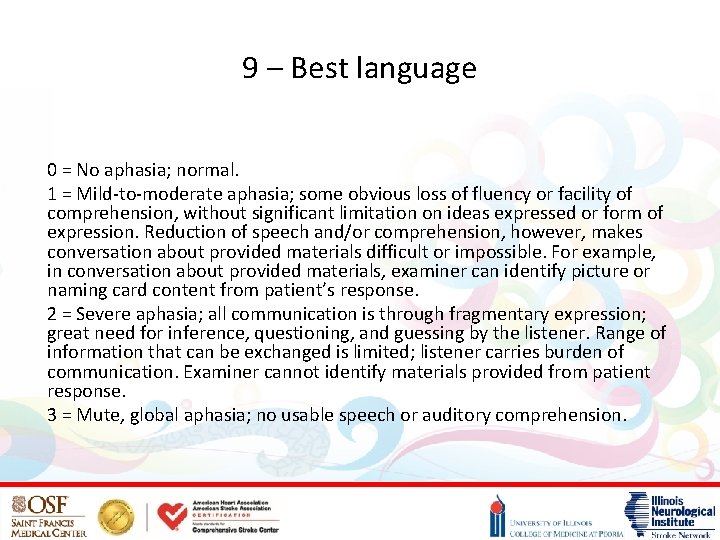
9 – Best language 0 = No aphasia; normal. 1 = Mild-to-moderate aphasia; some obvious loss of fluency or facility of comprehension, without significant limitation on ideas expressed or form of expression. Reduction of speech and/or comprehension, however, makes conversation about provided materials difficult or impossible. For example, in conversation about provided materials, examiner can identify picture or naming card content from patient’s response. 2 = Severe aphasia; all communication is through fragmentary expression; great need for inference, questioning, and guessing by the listener. Range of information that can be exchanged is limited; listener carries burden of communication. Examiner cannot identify materials provided from patient response. 3 = Mute, global aphasia; no usable speech or auditory comprehension.
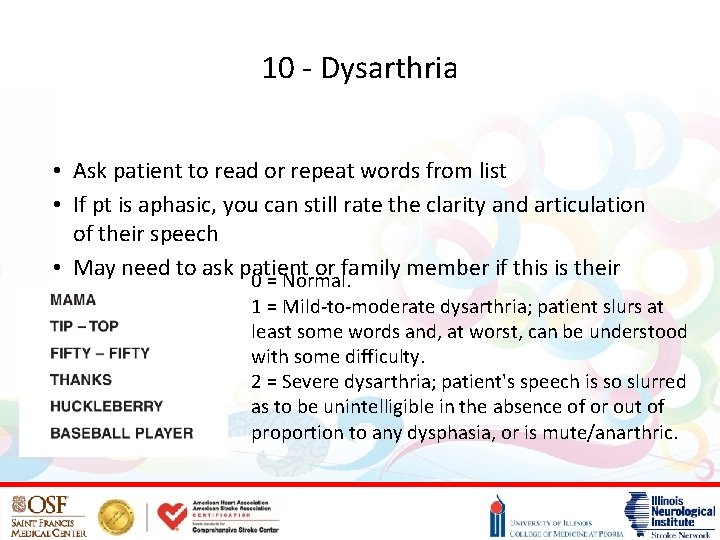
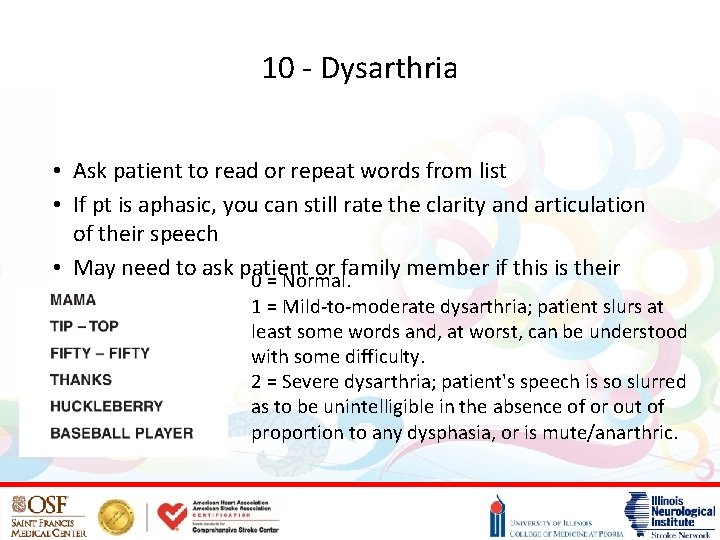
10 - Dysarthria • Ask patient to read or repeat words from list • If pt is aphasic, you can still rate the clarity and articulation of their speech • May need to ask patient or family member if this is their 0 = Normal. normal speech 1 = Mild-to-moderate dysarthria; patient slurs at least some words and, at worst, can be understood with some difficulty. 2 = Severe dysarthria; patient's speech is so slurred as to be unintelligible in the absence of or out of proportion to any dysphasia, or is mute/anarthric.
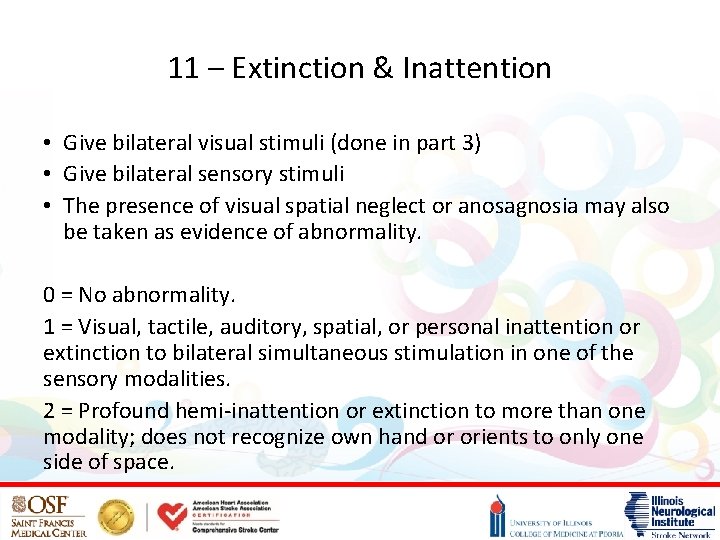
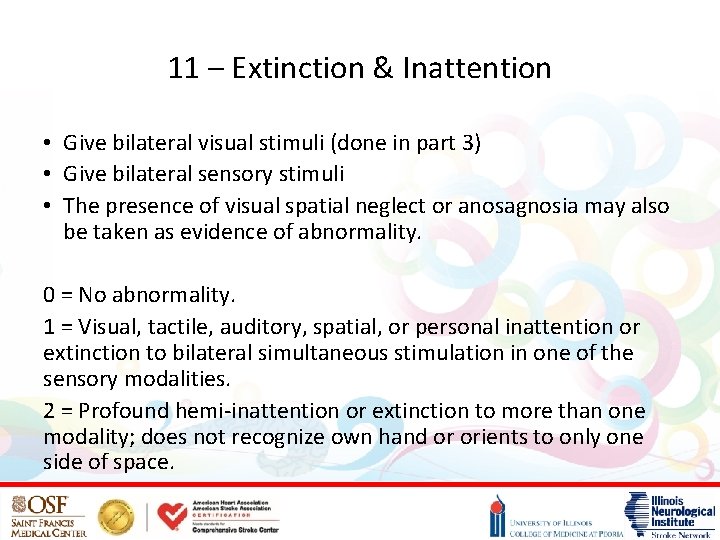
11 – Extinction & Inattention • Give bilateral visual stimuli (done in part 3) • Give bilateral sensory stimuli • The presence of visual spatial neglect or anosagnosia may also be taken as evidence of abnormality. 0 = No abnormality. 1 = Visual, tactile, auditory, spatial, or personal inattention or extinction to bilateral simultaneous stimulation in one of the sensory modalities. 2 = Profound hemi-inattention or extinction to more than one modality; does not recognize own hand or orients to only one side of space.
Questions?
References https: //www. nih. gov/ Blumenfeld, Neuroanatomy through Clinical Cases “Overview of the evaluation of stroke, ” Uptodate. com Adams H, Davis P, Hansen M, et al. "Baseline NIH Stroke Scale score strongly predicts outcome after stroke - A report of the Trial of Org 10172 in Acute Stroke Treatment (TOAST)". Muir KW, Weir CJ, Murray GD, Povey C, Lees KR (1996). "Comparison of neurological scales and scoring systems for acute stroke prognosis". Stroke. 27: 1817– 1820. Neurology, 2015. Brian Katz et all, “Interrater Reliability of the National Institutes of Health Stroke Scale: Rating by Emergency Room Physicians and Neurologists in a Population-Based Study”
 If you don't measure it you can't manage it
If you don't measure it you can't manage it Can't manage what you don't measure
Can't manage what you don't measure Root ject
Root ject What is focal neurological signs
What is focal neurological signs Neurological examination
Neurological examination Physio rehab centre
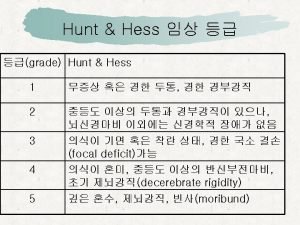
Physio rehab centre World federation of neurological surgeons scale
World federation of neurological surgeons scale Glasgow coma scale video
Glasgow coma scale video Neurological considerations in language acquisition
Neurological considerations in language acquisition Neurological exam
Neurological exam Abnormal flexion and extension
Abnormal flexion and extension Neurological disease
Neurological disease Neurological based behavior
Neurological based behavior Neuro checks pupil size
Neuro checks pupil size Biosocial trait theory
Biosocial trait theory Is adhd a neurological disorder
Is adhd a neurological disorder Uw neurosurgery residents
Uw neurosurgery residents Neurological examination
Neurological examination Motor function neurological assessment
Motor function neurological assessment Solent msk physiotherapy
Solent msk physiotherapy Grading of reflexes
Grading of reflexes Ryan waters neurosurgeon
Ryan waters neurosurgeon Muscle power neurological examination
Muscle power neurological examination Hospice face to face template
Hospice face to face template Myron b thompson academy
Myron b thompson academy I have one curved face and one flat face what am i
I have one curved face and one flat face what am i Face to face communication definition
Face to face communication definition Ecdl.com
Ecdl.com Attributable silence
Attributable silence When was romeo and juliet written
When was romeo and juliet written Barbara cons
Barbara cons