Hypothalamic and Pituitary Hormones 1 These hormones are
- Slides: 19
Hypothalamic and Pituitary Hormones 1
These hormones are used for : n 1. Diagnostic purposes n 2. Therapeutic purposes : Replacement These hormone are peptides or glycoproteins, so destroyed by proteolysis by GIT secretions. Thus used usually parenterally, usually by injection; some also by nasal spray
From Posterior pituitary: Vasopressin(ADH: anti-diuretic hormone) and Oxytocin: these peptide hormones are released from nerve endings of neurons located in supraoptic & paraventricular nuclei of hypothalamus. d-Arginine-Vasopressin (d-a. VP): Nonapeptide (9 -aminoacid peptide) 1. Acts on V 2 receptors on cell membrane of collecting ducts in renal medulla causing water reabsorption (by increasing c. AMP formation inside these cells leading to formation & insertion of aquaporins in their plasma membrane). It is secreted in response to : A. increase in plasma osmolality (>295 mosmol) B. decrease in volume of ECF (at least by 7%).
2. Acts on V 1 receptors on smooth muscle of BV (& intestine) to cause contraction (by increasing IP 3). This occurs at large non-physiological plasma level. Deficiency of ADH secretion leads to CDI (cranial diabetes insipidus): there is loss of renal concentrating power with excessive water loss in urine presenting as polyuria with very low urine osmolality, and polydipsia due to excessive thirst, with high plasma osmolality.
Therapeutic uses of vasopressin: A. Replacement therapy in CDI: Preparations: 1. Aqueous vasopressin : SC or IM every 4 -6 h for transient CDI e. g. after head injury. 2. Desmopressin (DDa. VP : Desmethyl-d-a. VP) : inj. 1 -4 ug every 12 -24 hours; at night, intranasal spray is used at bedtime but has less bioavailability than inj. Adverse effects: water retention and increase in BP with excessive doses; avoid aqueous vasopressin in angina since it can cause coronary vasospasm
B. Other uses : 1. To Produce vasoconstriction: a. Local topical application following dental extraction to stop bleeding, OR b. may be mixed with local anaesthetic drugs to prolong their action in infiltration or nerve block anaesthesia. This is esp. when catecholamines are contra-indicated for this purpose. Vasopressin may be used locally, but felypressin (which has no V 2 action) may be preferred.
c. Bleeding oesophageal varices in portal hypertension: here, IV infusion of vasopressin is used; it may cause angina, and intestinal colic or diarrhea as side effects ; longer acting preparations e. g. terlipressin may be preferred 2. Mild Haemophilia A and von Willebrand disease : IV or oral use of desmopressin is employed; desmopressin can release v. WF and factor VIII from endothelial stores; it is used to prevent bleeding due to minor surgery if needed for any reason in these conditions
n Nephrogenic diabetes insipidus (NDI) : - usually hereditary, but may be acquired due to drugs, chronic renal failure, and in severe hypokalemia Treated by : 1. Treat or remove cause, if possible 2. Thiazides
n Excessive ADH production (SIADH : Syndrome of inappropriate ADH secretion) occurs in 1. Lung cancer 2. CNS infections: encephalitis; meningitis esp. TB 3. Pneumonia 4. Drugs e. g. cytotoxic drugs like vincristine and cyclophosphamide; carbamazepine chlorpropamide Treated by : a. Treat cause , if possible b. Demeclocycline: antagonize ADH effect on kidney c. Lithium: not usually used because of unpredictable toxicity
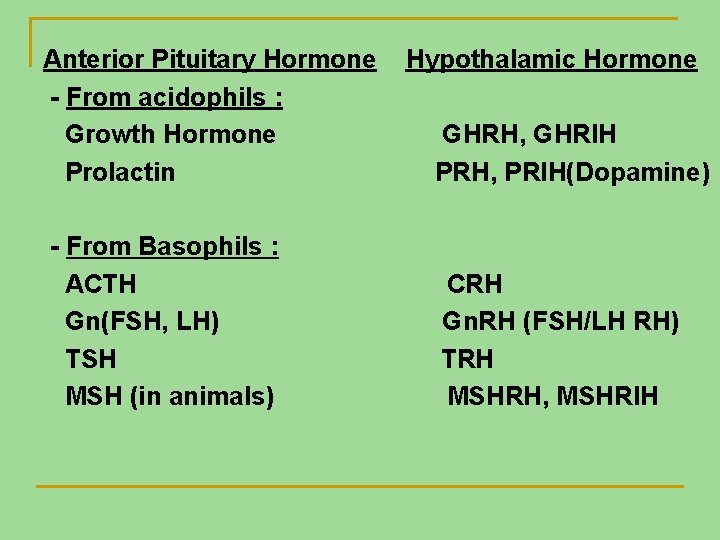
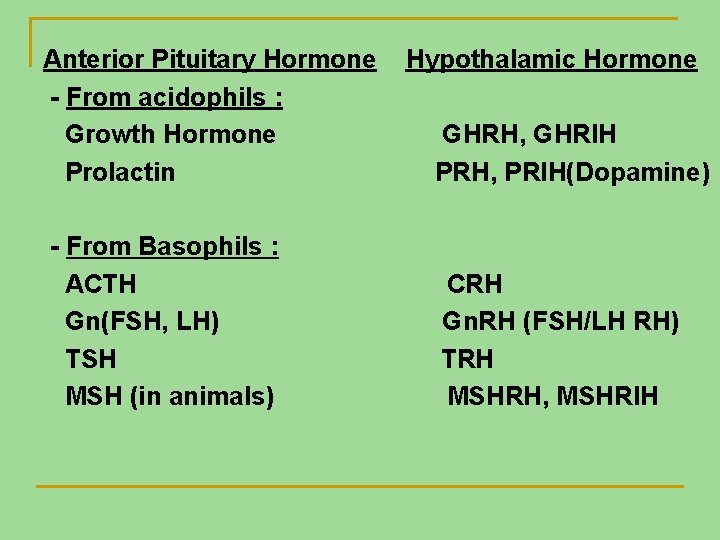
Anterior Pituitary Hormone - From acidophils : Growth Hormone Prolactin - From Basophils : ACTH Gn(FSH, LH) TSH MSH (in animals) Hypothalamic Hormone GHRH, GHRIH PRH, PRIH(Dopamine) CRH Gn. RH (FSH/LH RH) TRH MSHRH, MSHRIH
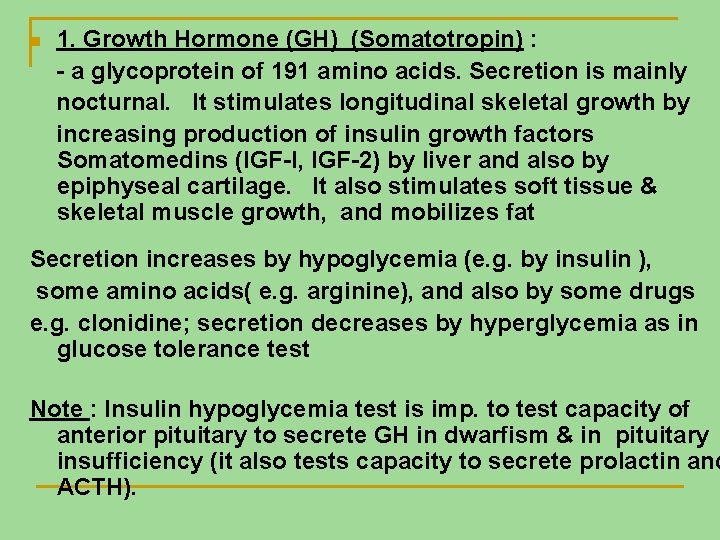
n 1. Growth Hormone (GH) (Somatotropin) : - a glycoprotein of 191 amino acids. Secretion is mainly nocturnal. It stimulates longitudinal skeletal growth by increasing production of insulin growth factors Somatomedins (IGF-I, IGF-2) by liver and also by epiphyseal cartilage. It also stimulates soft tissue & skeletal muscle growth, and mobilizes fat Secretion increases by hypoglycemia (e. g. by insulin ), some amino acids( e. g. arginine), and also by some drugs e. g. clonidine; secretion decreases by hyperglycemia as in glucose tolerance test Note : Insulin hypoglycemia test is imp. to test capacity of anterior pituitary to secrete GH in dwarfism & in pituitary insufficiency (it also tests capacity to secrete prolactin and ACTH).
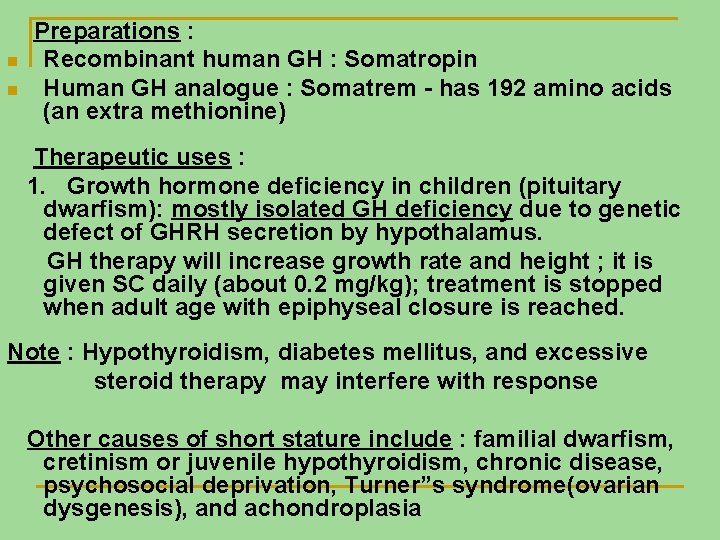
n n Preparations : Recombinant human GH : Somatropin Human GH analogue : Somatrem - has 192 amino acids (an extra methionine) Therapeutic uses : 1. Growth hormone deficiency in children (pituitary dwarfism): mostly isolated GH deficiency due to genetic defect of GHRH secretion by hypothalamus. GH therapy will increase growth rate and height ; it is given SC daily (about 0. 2 mg/kg); treatment is stopped when adult age with epiphyseal closure is reached. Note : Hypothyroidism, diabetes mellitus, and excessive steroid therapy may interfere with response Other causes of short stature include : familial dwarfism, cretinism or juvenile hypothyroidism, chronic disease, psychosocial deprivation, Turner”s syndrome(ovarian dysgenesis), and achondroplasia
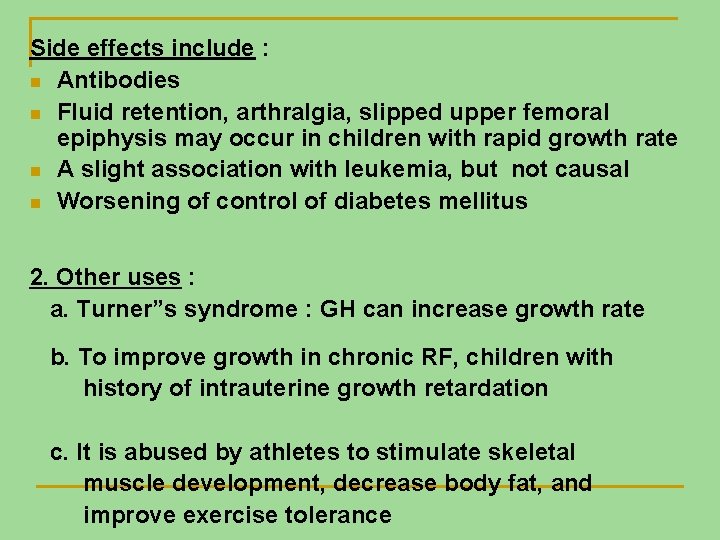
Side effects include : n Antibodies n Fluid retention, arthralgia, slipped upper femoral epiphysis may occur in children with rapid growth rate n A slight association with leukemia, but not causal n Worsening of control of diabetes mellitus 2. Other uses : a. Turner”s syndrome : GH can increase growth rate b. To improve growth in chronic RF, children with history of intrauterine growth retardation c. It is abused by athletes to stimulate skeletal muscle development, decrease body fat, and improve exercise tolerance
n n Hypothalamic GHRH: consists of several large peptides. Sermorelin is a synthetic analogue with a shorter peptide; it is used to determine if GH deficiency in dwarfs is due to pituitary or hypothalamic cause. Hypothalamic GHRIH : Somatostatin: this is a 14 -amino acid peptide; also found in pancreas (delta(D)cells of islets of Langerhans) and other parts of GIT. It decreases release of GH from anterior pituitary as well as that of TSH; it also decreases secretion of insulin and glucagon from pancreas, and of gastrin from stomach as well as serotonin from carcinoid tumor of intestine It is short-acting, and was used by IV infusion to produce splanchnic vasoconstriction and decrease bleeding from oesophageal varices in patients with portal hypertension, but it inhibits platelet aggregation
n Octreotide is a synthetic 10 -aminoacid analogue peptide that is more potent and longer acting than somatostatin. It is used clinically in: 1. Acromegally: to decrease excessive GH secretion from acidophil adenoma. Bromocryptine and other DA 2 -receptor agonists e. g. cabergoline also partially decrease GH secretion in acromegally. Acromegally is usually treated by pituitary irradiation or surgical removal of the acidophil adenoma.
Octreotide is given SC 50 ug tid at beginning, and dose gradually increased; once effective dose is found , a slow-release preparation of this dose is then given SC or IM each month. Lanreotide is a longer acting analogue than octreotide; it is given once or twice each month. Side effects include: local pain, bowel dysfunctiuon and increased incidence of cholelithiasis. 2. Other uses of octreotide include carcinoid tumour of intestine, VIPoma, & insulinoma.
2. Prolactin (PRL) : a glycoprotein hormone. It acts on the breast , primed by oestogen and other hormones, to stimulate milk production; also has other biological effects. No clinical use is available for it yet. Its secretion is controlled by hypothalamic: a. PRH: No clinical use for it. b. PRIH: now known to be dopamine; it acts on DA 2 receptors on acidophils to inhibit PRL release. It exerts a tonic physiological inhibition on PRL release from anterior pituitary
Hyperprolactinemia is a common endocrine disorder. It causes galactorrhea, menstrual abnormality (even amenorrhea), and infertility in women. It is caused by: a. Hypothalamic dysfunction : decreasing PRIH production, so leading to galactorrhea-amenorrhea syndrome in women b. Pituitary adenoma : micro- or macro-prolactinoma c. Disease: Damage to pituitary stalk, Hypothyroidism d. Drugs: DA 2 receptor antagonists (phenothiazines, butyrophenones, and metoclopramide) ; drugs that depletes monoamines in CNS ( reserpine or tetrabenazine, and alpha-methyldopa); Other drugs are oestrogens and cimetidine. e. Pregnancy
Treatmentof hyperprolactinemia is by : 1. Removal of cause, if possible 2. In cases of prolactinomas and hypothalamic causes, plasma PRL is lowered by DA 2 agonists like: a. Bromocryptine: oral 1. 25 -5 mg daily. Its side effects include nausea, fatique, postural hypotension , and worsening of psychosis b. Cabergoline : more potent , longer acting (dose is very small & once or twice per week) and has less side effects than bromocryptine 70 -80% of patients with macro-prolactinomas respond, and tumour decreases in size; in microprolactinomas, the results may be better than surgery which is successful in 50 -60% of cases.