Hypotension Shock Hemorrhage and IV Fluid Resuscitation Ziad






- Slides: 65
Hypotension, Shock, Hemorrhage and IV Fluid Resuscitation Ziad Sifri, MD Surgical Fundamentals and Algorithmic Approach to Patient Care Session#7: August 17, 2007
Learning Objectives 1. Definition, diagnosis and types of shock 2. Hemorrhagic shock ( I-IV ) 3. Initial management of patients in Hemorrhagic shock – Algorithm for the identifying of the location of bleeding – IV access and resuscitation of Trauma patients 4. Initial assessment of patients in non-Hemorrhagic shock 5. Diagnosis of the various types of non-Hemorrhagic shock 6. Management of non-Hemorrhagic shock 7. Case Scenarios
The real goal however……. is to avoid ….
“Shock” • Definition: Inadequate tissue Perfusion and Oxygenation • Effect: Cellular injury, Organ failure, Death • Causes: hemorrhagic and non-hemorrhagic
Types of Shock ?
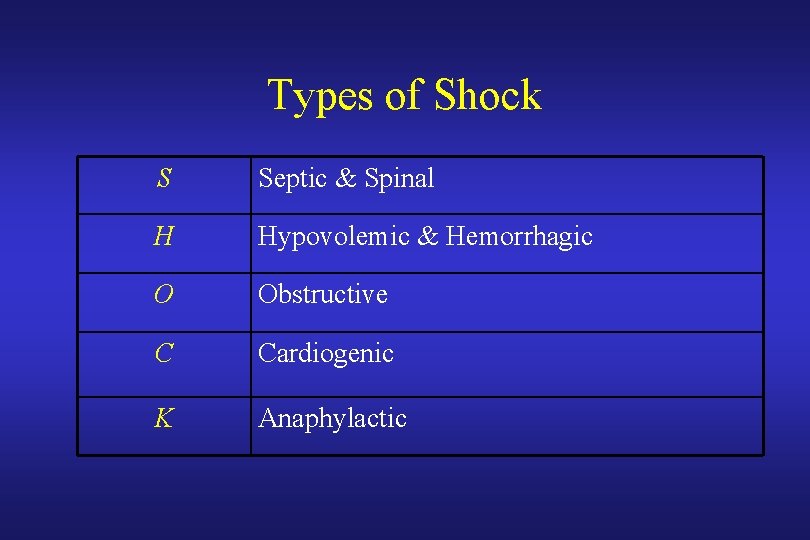
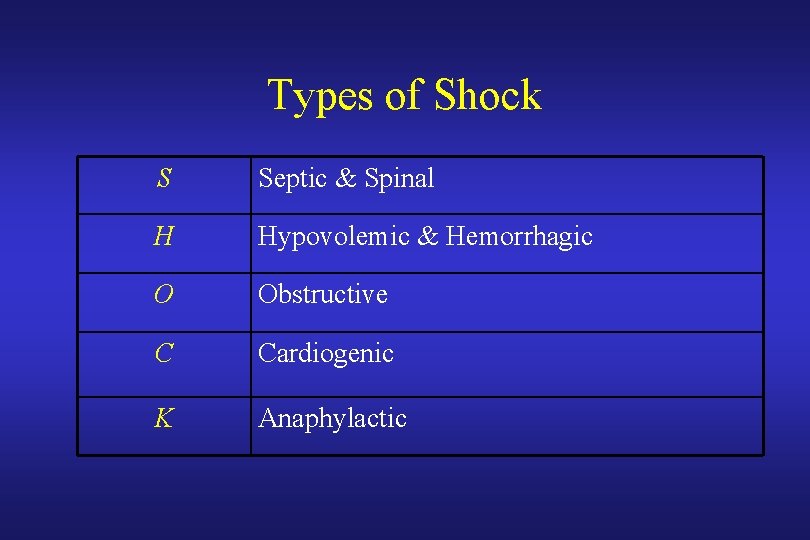
Types of Shock S Septic & Spinal H Hypovolemic & Hemorrhagic O Obstructive C Cardiogenic K Anaphylactic
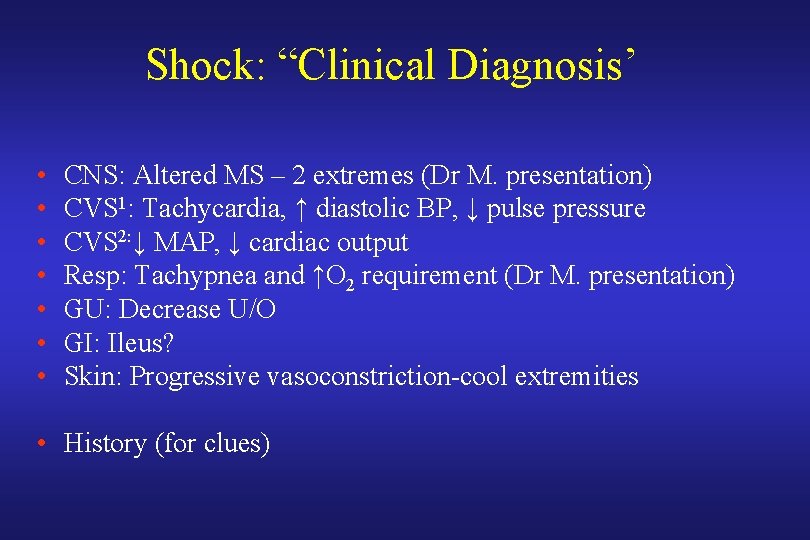
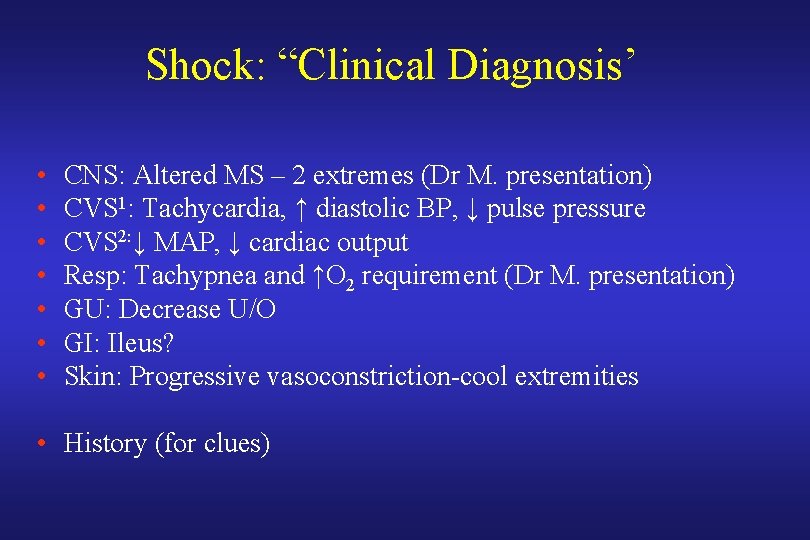
Shock: “Clinical Diagnosis’ • • CNS: Altered MS – 2 extremes (Dr M. presentation) CVS 1: Tachycardia, ↑ diastolic BP, ↓ pulse pressure CVS 2: ↓ MAP, ↓ cardiac output Resp: Tachypnea and ↑O 2 requirement (Dr M. presentation) GU: Decrease U/O GI: Ileus? Skin: Progressive vasoconstriction-cool extremities • History (for clues)
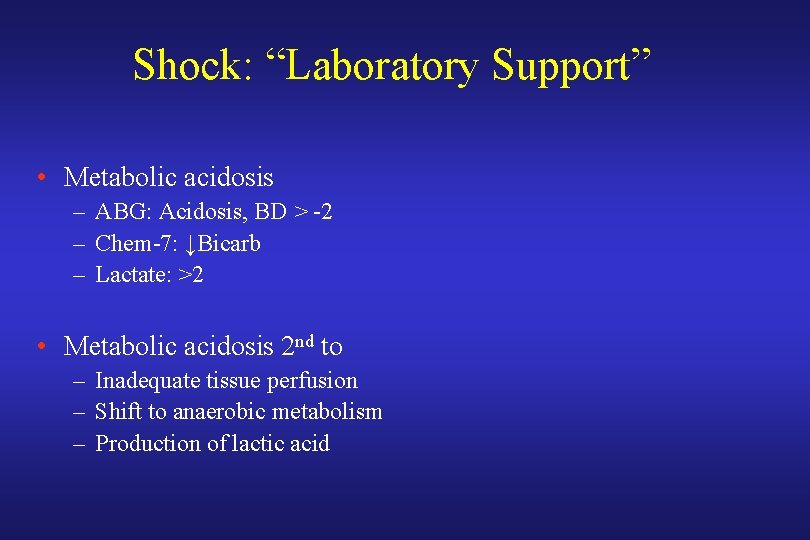
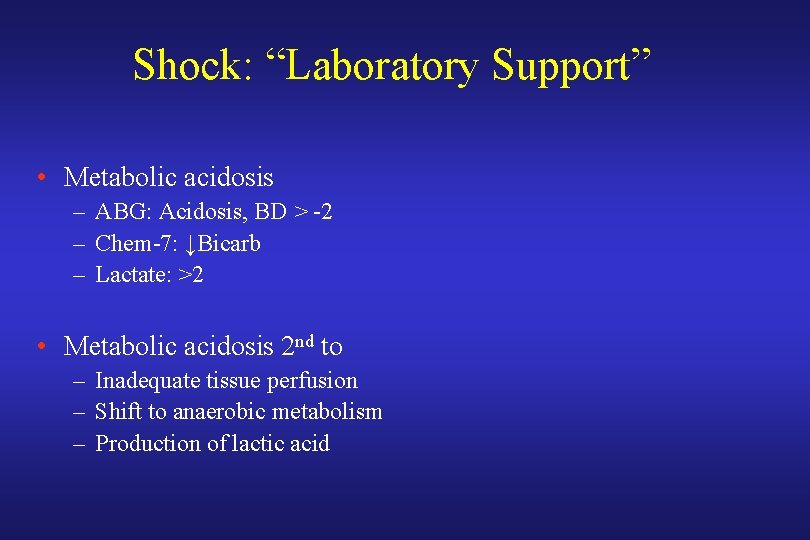
Shock: “Laboratory Support” • Metabolic acidosis – ABG: Acidosis, BD > -2 – Chem-7: ↓Bicarb – Lactate: >2 • Metabolic acidosis 2 nd to – Inadequate tissue perfusion – Shift to anaerobic metabolism – Production of lactic acid
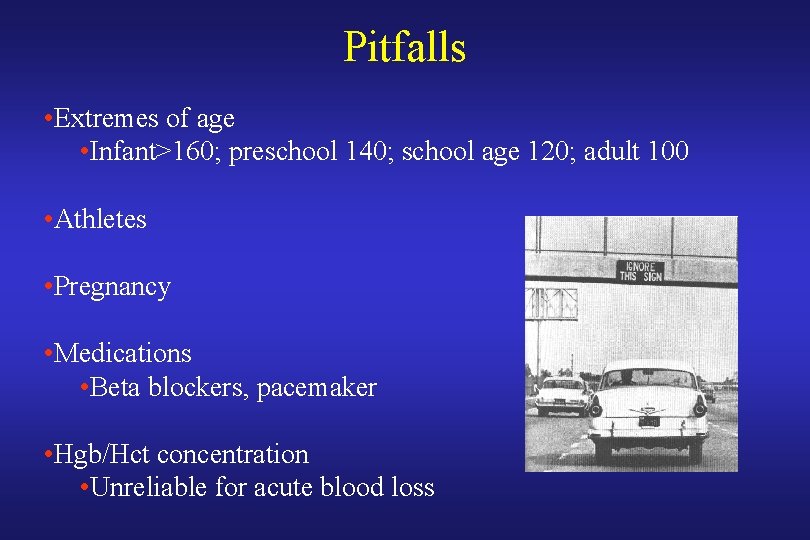
Pitfalls • Extremes of age • Infant>160; preschool 140; school age 120; adult 100 • Athletes • Pregnancy • Medications • Beta blockers, pacemaker • Hgb/Hct concentration • Unreliable for acute blood loss
Other Pitfalls…. Urine output adequate despite shock • Alcohol • Hyperglycemia • Home medication: diuretics. . • Therapeutic intervention: Mannitol • IV contrast: CT, Angio • Residual urine… • DI • Etc…
General Outline • Definition, diagnosis and types of shock • Hemorrhagic shock: Classes and Resuscitation
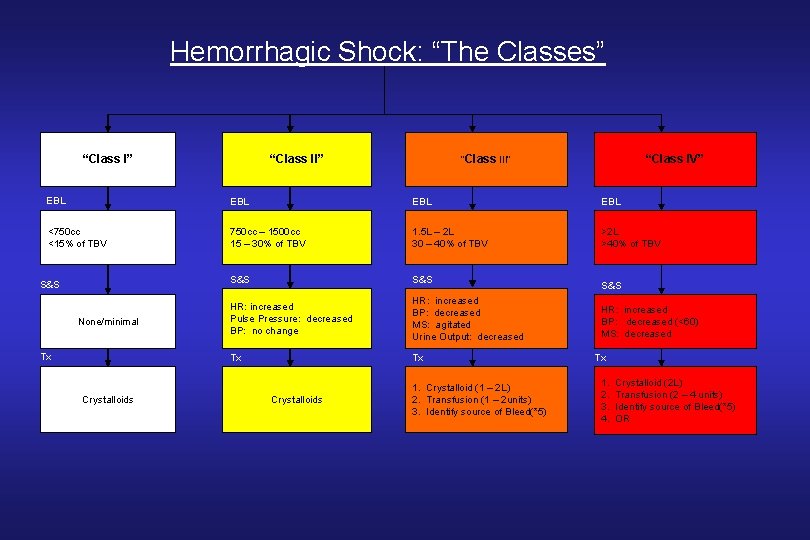
Hemorrhage & Trauma • Normal blood volume – Adults: 7% of ideal weight • 70 kg man had blood volume of 5 liters – Child: 9% of ideal weight • Hemorrhage – Loss of circulating blood volume – How much volume loss to cause shock? – Classes of hemorrhage I-IV
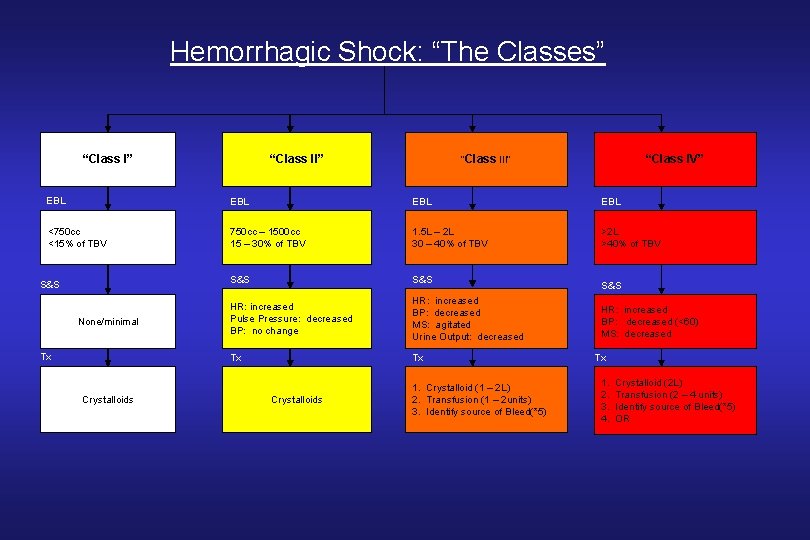
Hemorrhagic Shock: “The Classes” “Class II” “Class III” “Class IV” EBL EBL <750 cc <15% of TBV 750 cc – 1500 cc 15 – 30% of TBV 1. 5 L – 2 L 30 – 40% of TBV >2 L >40% of TBV S&S HR: increased Pulse Pressure: decreased BP: no change HR: increased BP: decreased MS: agitated Urine Output: decreased Tx Tx S&S None/minimal Tx Crystalloids 1. Crystalloid (1 – 2 L) 2. Transfusion (1 – 2 units) 3. Identify source of Bleed(*5) S&S HR: increased BP: decreased (<60) MS: decreased Tx 1. 2. 3. 4. Crystalloid (2 L) Transfusion (2 – 4 units) Identify source of Bleed(*5) OR
General Outline • Definition, diagnosis and types of shock • Classes of Hemorrhagic shock • Initial management of patients in Hemorrhagic shock
Two Goals in the management of “any” Shock GOAL #1 GOAL #2 “ID and Tx the cause” “Support the patient”
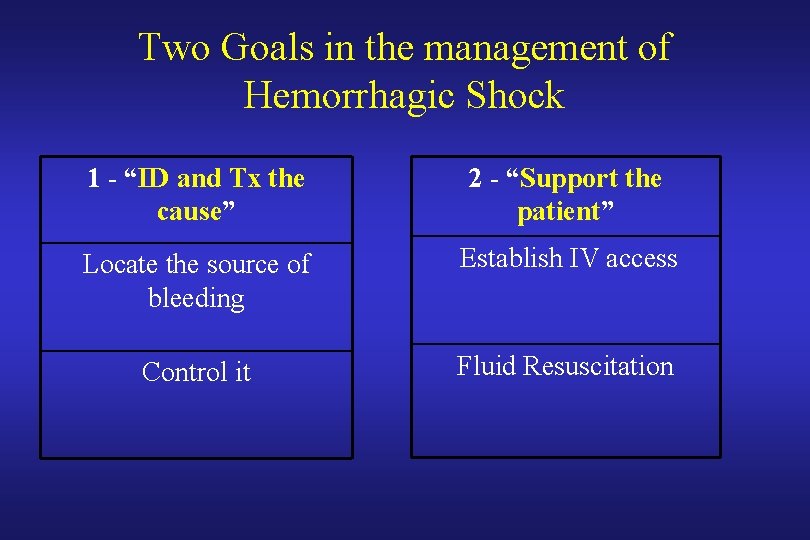
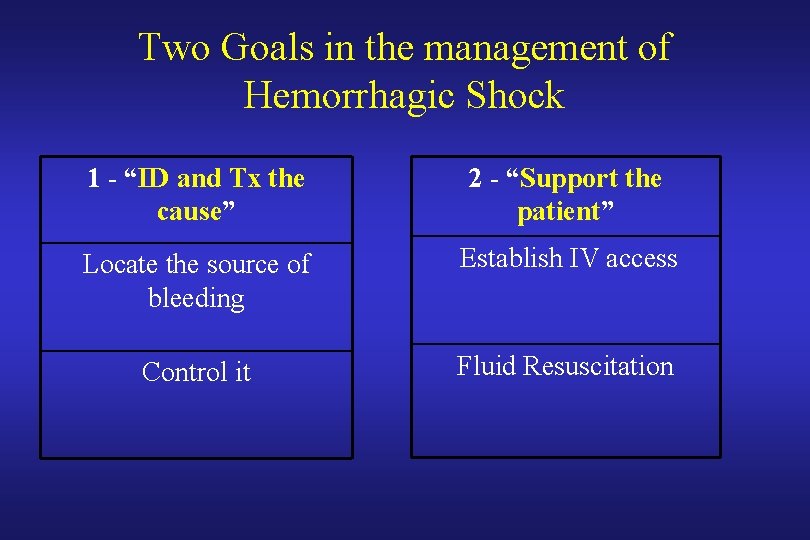
Two Goals in the management of Hemorrhagic Shock 1 - “ID and Tx the cause” 2 - “Support the patient” Locate the source of bleeding Establish IV access Control it Fluid Resuscitation
Goal #1 “Identification and Treatment of the cause” A-Locate the source of bleeding B-Control it
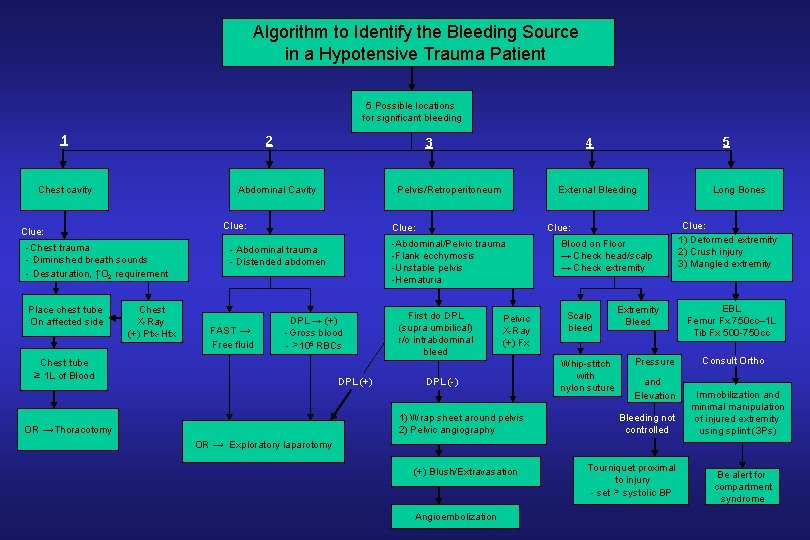
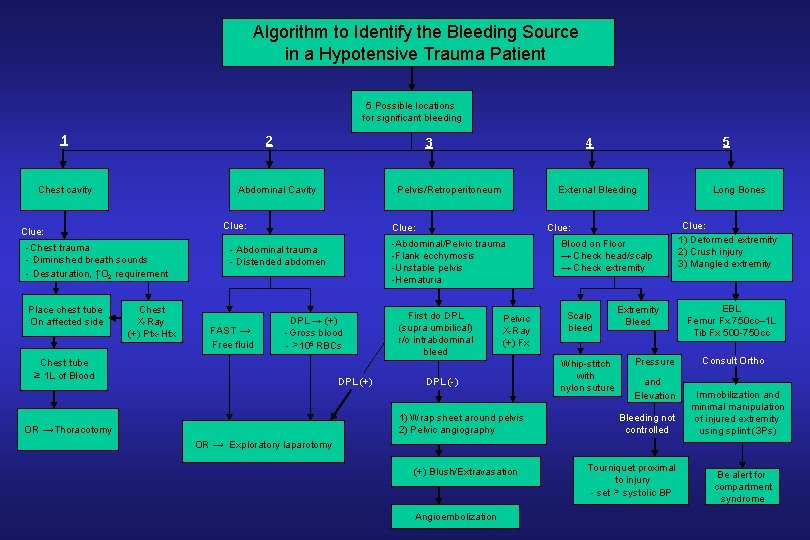
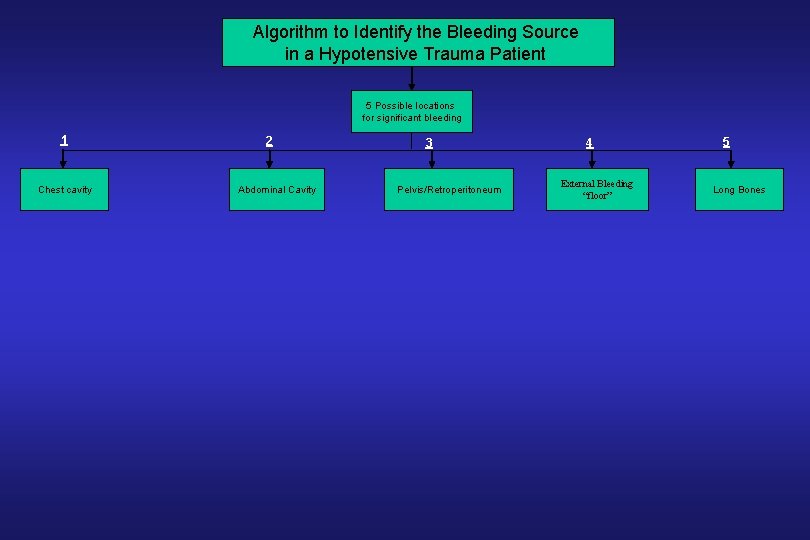
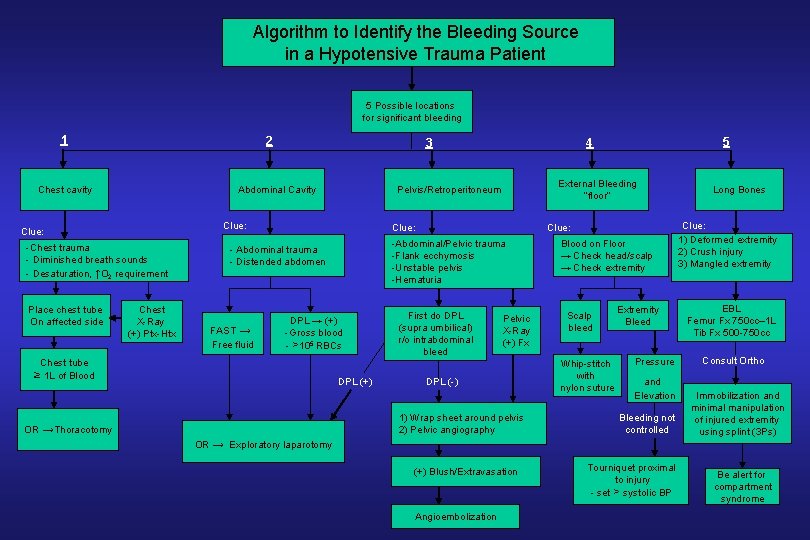
Algorithm to Identify the Bleeding Source in a Hypotensive Trauma Patient 5 Possible locations for significant bleeding 1 2 Abdominal Cavity Chest cavity -Chest trauma - Diminished breath sounds - Desaturation, ↑O 2 requirement Chest X-Ray (+) Ptx-Htx FAST → Free fluid External Bleeding Clue: DPL → (+) -Gross blood - >105 RBCs Chest tube ≥ 1 L of Blood Clue: -Abdominal/Pelvic trauma -Flank ecchymosis -Unstable pelvis -Hematuria - Abdominal trauma - Distended abdomen DPL (+) First do DPL (supra umbilical) r/o intrabdominal bleed Pelvic X-Ray (+) Fx DPL (-) 1) Wrap sheet around pelvis 2) Pelvic angiography OR →Thoracotomy 5 4 Pelvis/Retroperitoneum Clue: Place chest tube On affected side 3 Blood on Floor → Check head/scalp → Check extremity Scalp bleed Whip-stitch with nylon suture Extremity Bleed Pressure and Elevation Bleeding not controlled Long Bones Clue: 1) Deformed extremity 2) Crush injury 3) Mangled extremity EBL Femur Fx 750 cc– 1 L Tib Fx 500 -750 cc Consult Ortho Immobilization and minimal manipulation of injured extremity using splint (3 Ps) OR → Exploratory laparotomy (+) Blush/Extravasation Angioembolization Tourniquet proximal to injury - set > systolic BP Be alert for compartment syndrome
Algorithm to Identify the Bleeding Source in a Hypotensive Trauma Patient 5 Possible locations for significant bleeding 1 Chest cavity 2 Abdominal Cavity 3 Pelvis/Retroperitoneum 4 External Bleeding “floor” 5 Long Bones
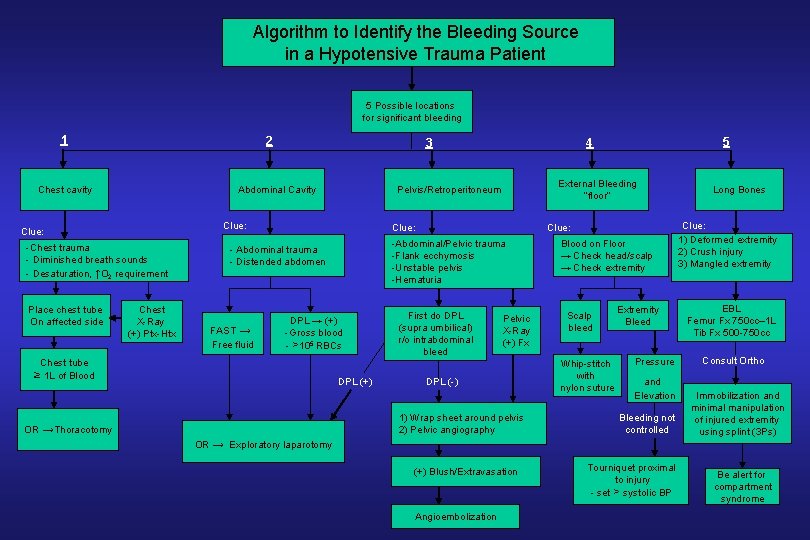
Algorithm to Identify the Bleeding Source in a Hypotensive Trauma Patient 5 Possible locations for significant bleeding 1 2 Abdominal Cavity Chest cavity -Chest trauma - Diminished breath sounds - Desaturation, ↑O 2 requirement Chest X-Ray (+) Ptx-Htx FAST → Free fluid External Bleeding “floor” Clue: DPL → (+) -Gross blood - >105 RBCs Chest tube ≥ 1 L of Blood Clue: -Abdominal/Pelvic trauma -Flank ecchymosis -Unstable pelvis -Hematuria - Abdominal trauma - Distended abdomen DPL (+) First do DPL (supra umbilical) r/o intrabdominal bleed Pelvic X-Ray (+) Fx DPL (-) 1) Wrap sheet around pelvis 2) Pelvic angiography OR →Thoracotomy 5 4 Pelvis/Retroperitoneum Clue: Place chest tube On affected side 3 Blood on Floor → Check head/scalp → Check extremity Scalp bleed Whip-stitch with nylon suture Extremity Bleed Pressure and Elevation Bleeding not controlled OR → Exploratory laparotomy (+) Blush/Extravasation Angioembolization Tourniquet proximal to injury - set > systolic BP Long Bones Clue: 1) Deformed extremity 2) Crush injury 3) Mangled extremity EBL Femur Fx 750 cc– 1 L Tib Fx 500 -750 cc Consult Ortho Immobilization and minimal manipulation of injured extremity using splint (3 Ps) Be alert for compartment syndrome
Goal #2 “Support the patient” A-Establish IV access B-Fluid Resuscitation
Establish IV access before it is too late
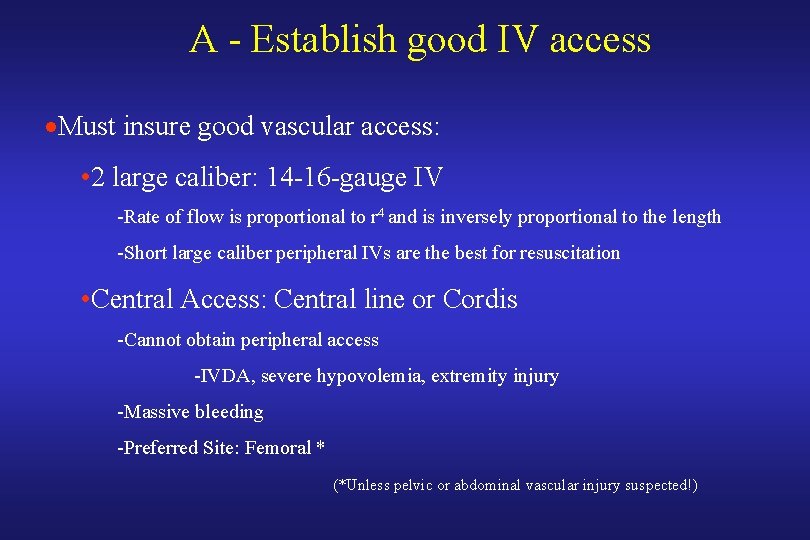
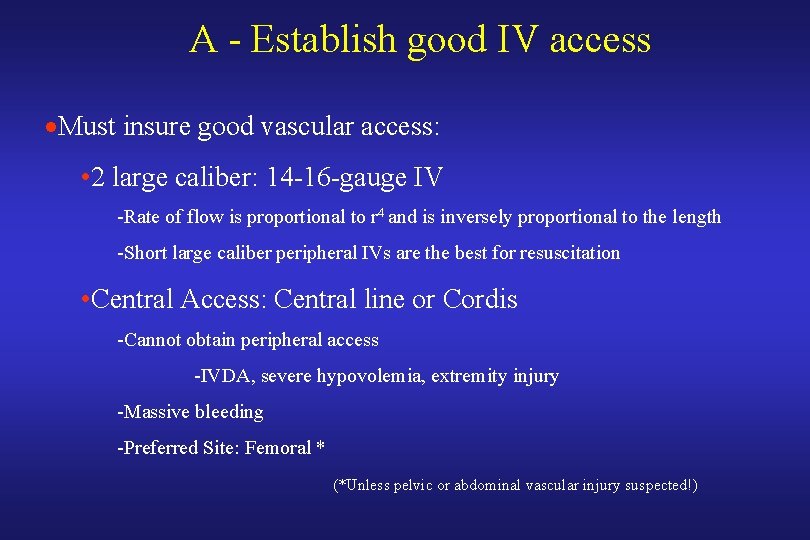
A - Establish good IV access ·Must insure good vascular access: • 2 large caliber: 14 -16 -gauge IV -Rate of flow is proportional to r 4 and is inversely proportional to the length -Short large caliber peripheral IVs are the best for resuscitation • Central Access: Central line or Cordis -Cannot obtain peripheral access -IVDA, severe hypovolemia, extremity injury -Massive bleeding -Preferred Site: Femoral * (*Unless pelvic or abdominal vascular injury suspected!)
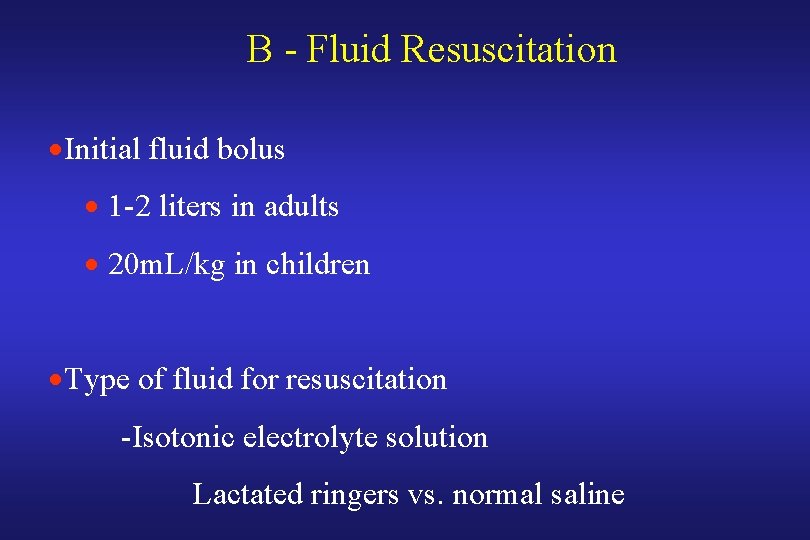
B - Fluid Resuscitation ·Initial fluid bolus · 1 -2 liters in adults · 20 m. L/kg in children ·Type of fluid for resuscitation -Isotonic electrolyte solution Lactated ringers vs. normal saline
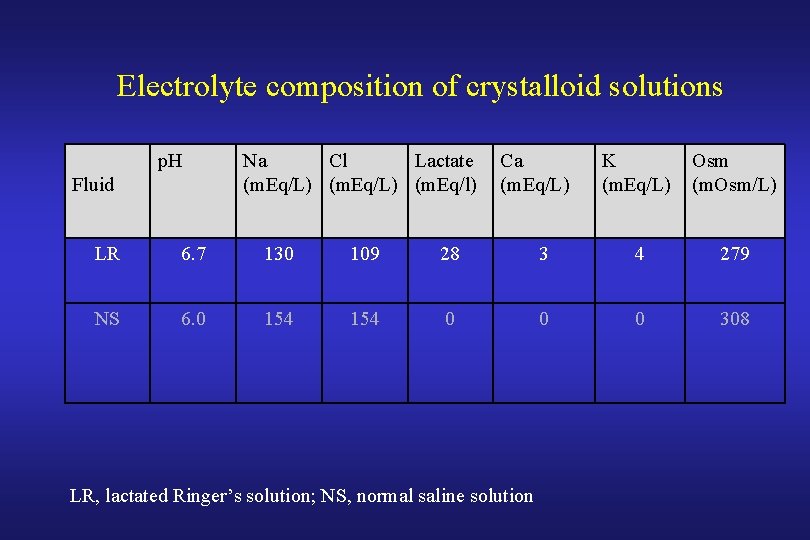
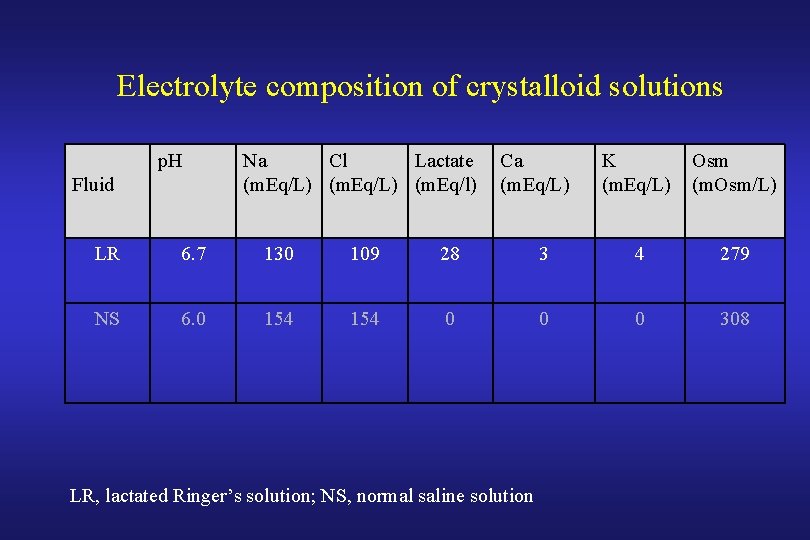
Electrolyte composition of crystalloid solutions p. H Fluid Na Cl Lactate (m. Eq/L) (m. Eq/l) Ca (m. Eq/L) K (m. Eq/L) Osm (m. Osm/L) LR 6. 7 130 109 28 3 4 279 NS 6. 0 154 0 0 0 308 LR, lactated Ringer’s solution; NS, normal saline solution
B - Fluid Resuscitation · Intravascular effect · 3 for 1 rule of Volume replacement: Volume lost
The effect of the 3: 1 Rule
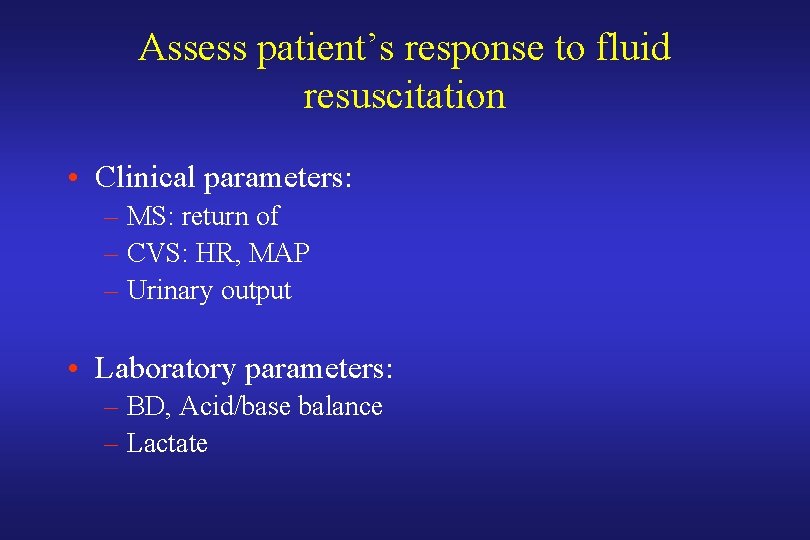
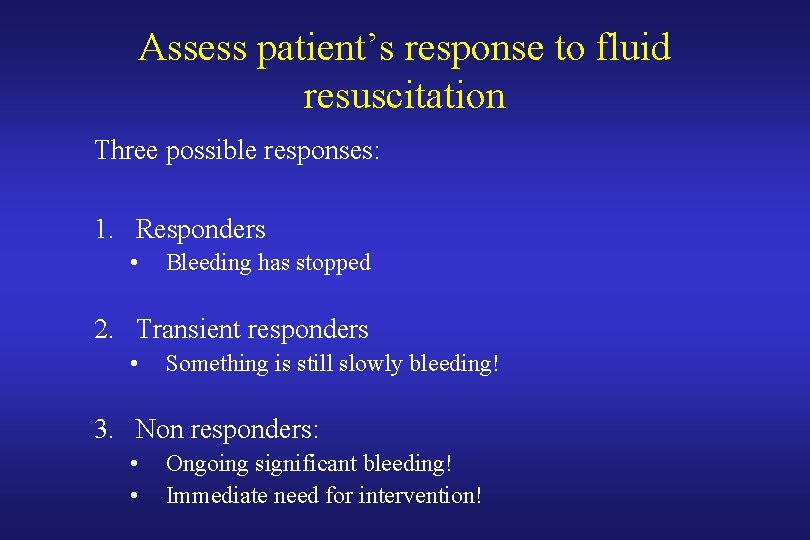
Assess patient’s response to fluid resuscitation • Clinical parameters: – MS: return of – CVS: HR, MAP – Urinary output • Laboratory parameters: – BD, Acid/base balance – Lactate
Assess patient’s response to fluid resuscitation Three possible responses: 1. Responders • Bleeding has stopped 2. Transient responders • Something is still slowly bleeding! 3. Non responders: • • Ongoing significant bleeding! Immediate need for intervention!
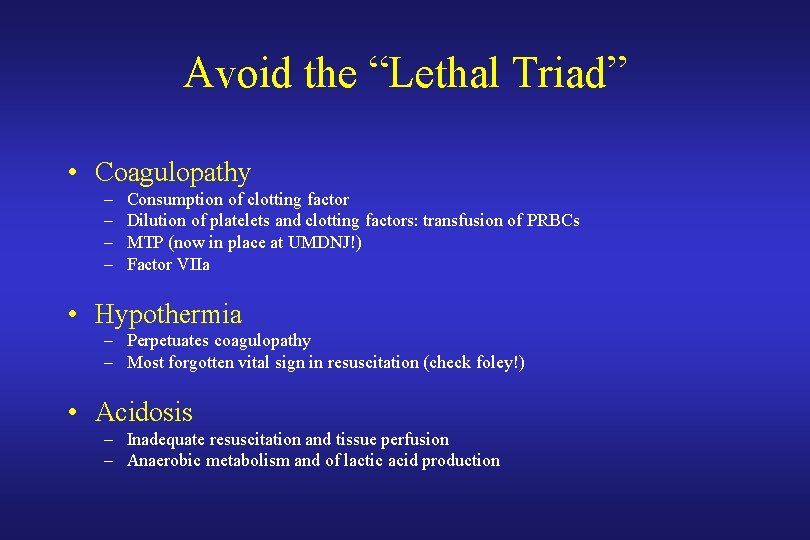
Avoid the “Lethal Triad” • Coagulopathy – – Consumption of clotting factor Dilution of platelets and clotting factors: transfusion of PRBCs MTP (now in place at UMDNJ!) Factor VIIa • Hypothermia – Perpetuates coagulopathy – Most forgotten vital sign in resuscitation (check foley!) • Acidosis – Inadequate resuscitation and tissue perfusion – Anaerobic metabolism and of lactic acid production
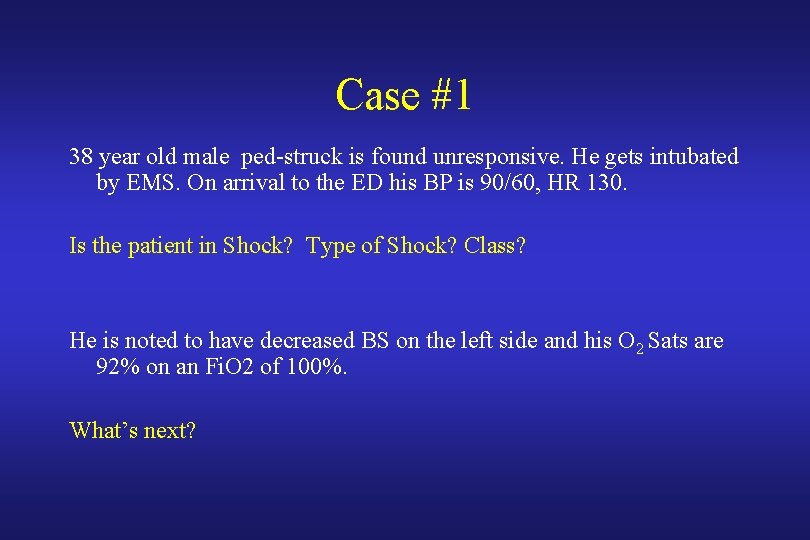
Case #1 38 year old male ped-struck is found unresponsive. He gets intubated by EMS. On arrival to the ED his BP is 90/60, HR 130. Is the patient in Shock? Type of Shock? Class? He is noted to have decreased BS on the left side and his O 2 Sats are 92% on an Fi. O 2 of 100%. What’s next?
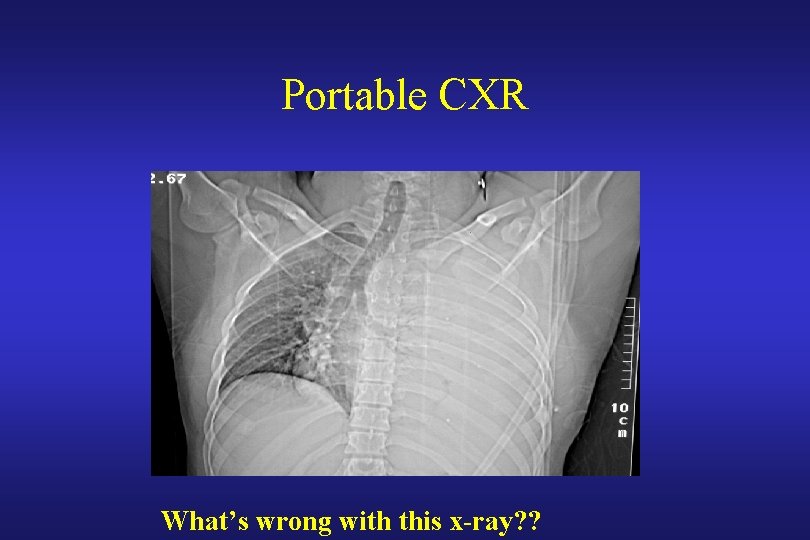
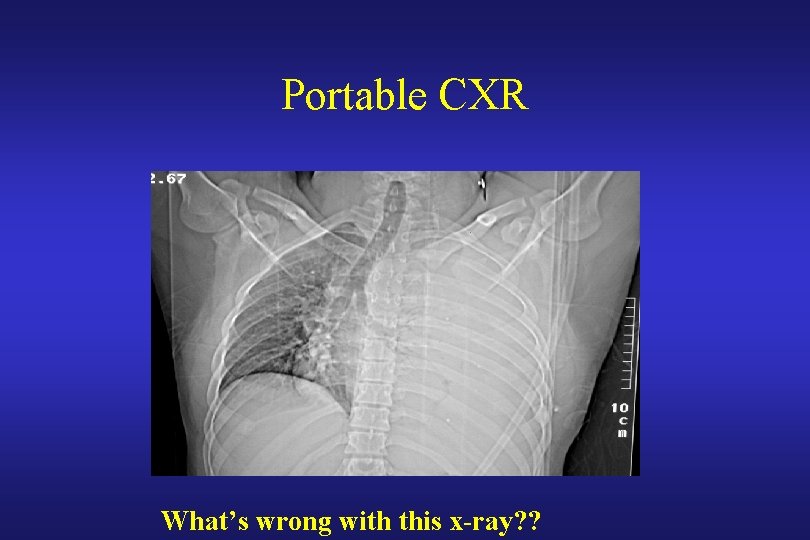
Portable CXR What’s wrong with this x-ray? ?
Case #1 • What’s next? Chest tube puts out 1 liter of blood. • What’s next?
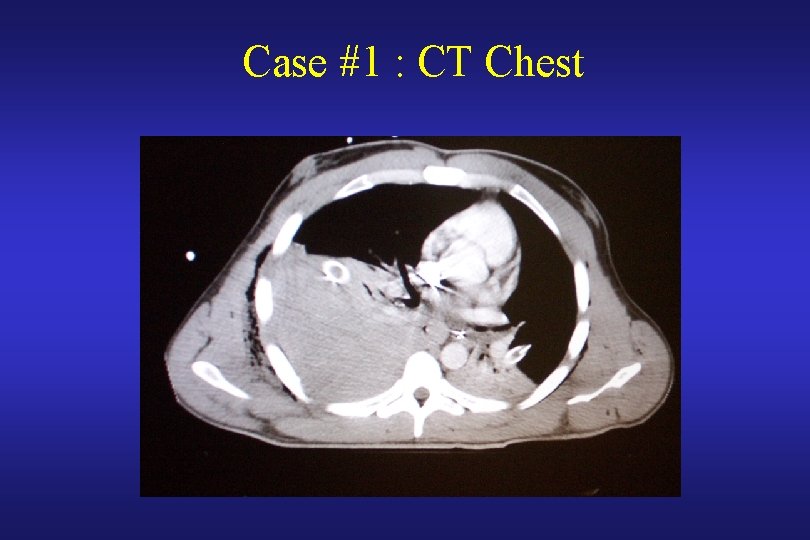
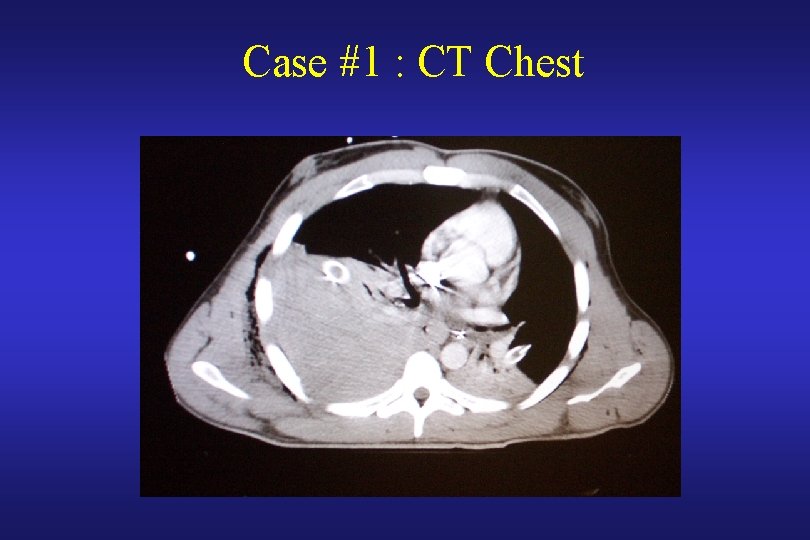
Case #1 : CT Chest

Case #2 18 year old male involved in a high speed MVC found unresponsive with a BP of 60/P at the scene. He has a large head laceration that is actively bleeding, an obvious abrasions over the pelvis and bilateral mangled lower extremities. In the ED, he is immediately intubated, he has equal BS, his sats are 100%. He is actively bleeding from his scalp and legs. His pelvis is unstable. BP 70/40 P 150. Is the patient in Shock? Type of Shock? Class?
Case #2 Management ? – Goal #1 A- Locate the source of bleeding B- Control it – Goal #2 A- Establish IV access B- Fluid Resuscitation
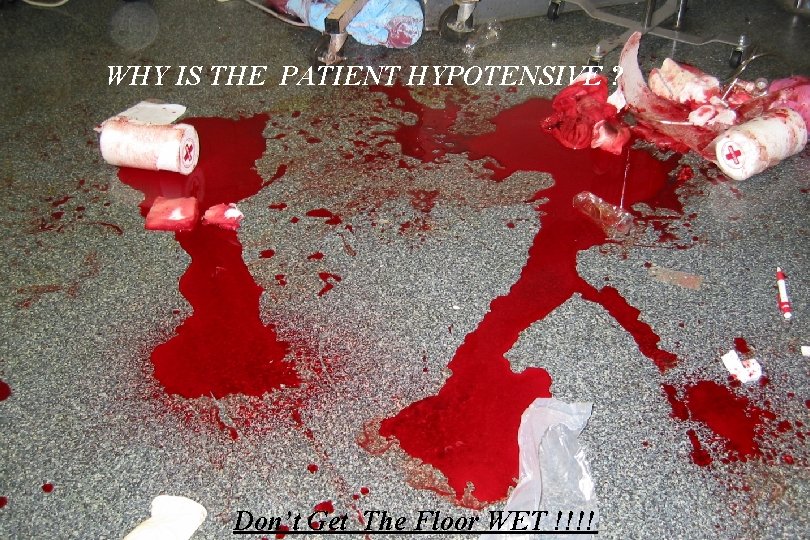
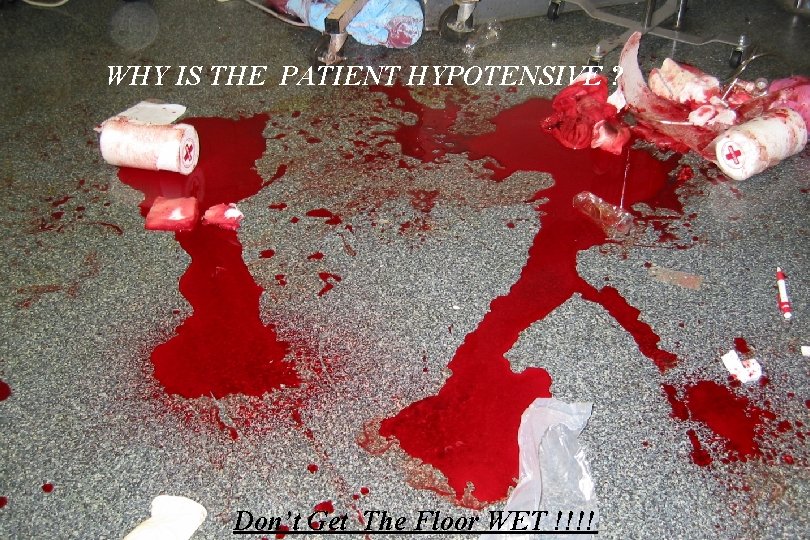
WHY IS THE PATIENT HYPOTENSIVE ? ? ? ? Don’t Get The Floor WET !!!!
Case #2 SOURCE of BLEEDING ? ? ?

Whip Stitch scalp laceration

What is missing ?

Bilateral Tourniquets
Case #2 • Still hypotensive despite bilateral tourniquets and despite whipstiching the scalp laceration • He has received: 2 L crystalloids 2 units PRBCs • CXR: Normal
NEXT? ? ? • DPL? FAST? • Pelvic X-ray?
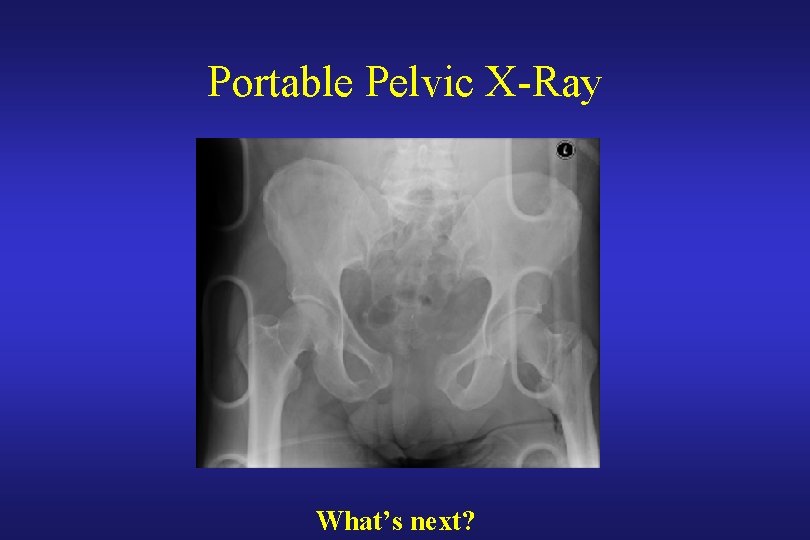
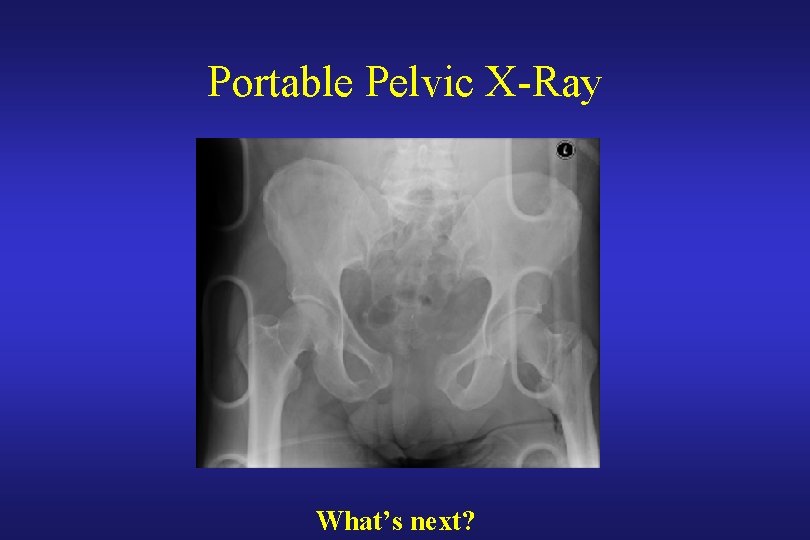
Portable Pelvic X-Ray What’s next?
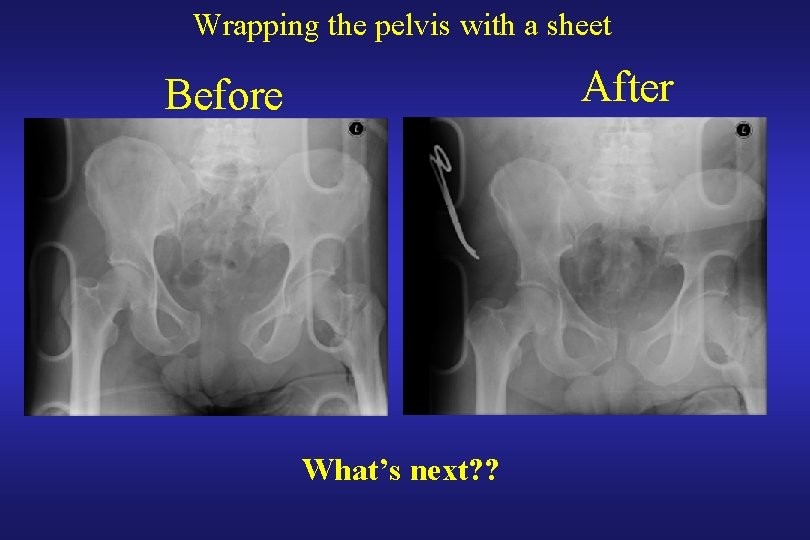
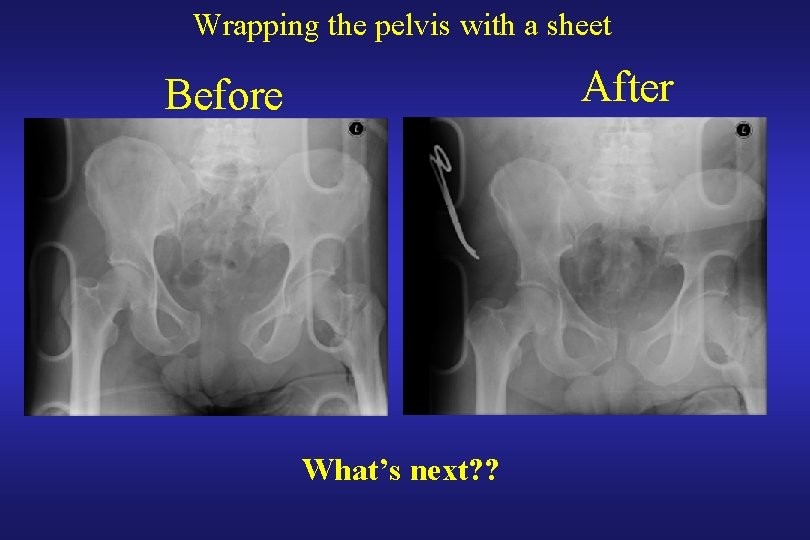
Wrapping the pelvis with a sheet After Before What’s next? ?
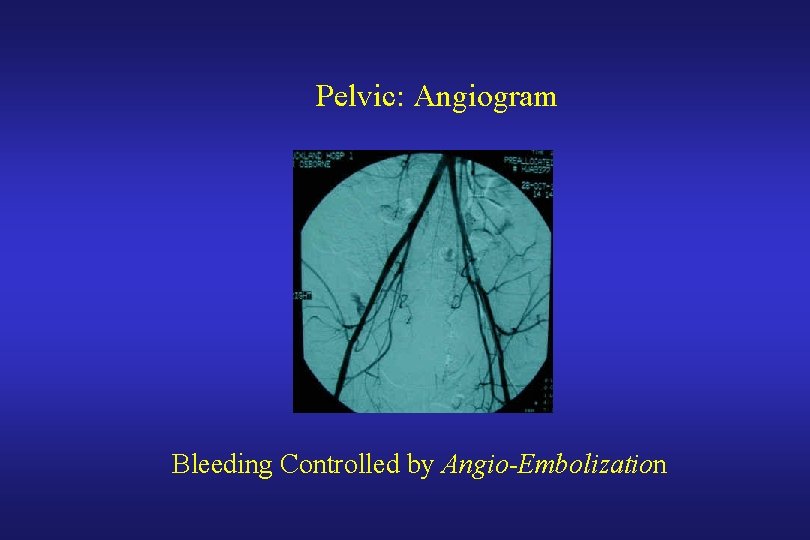
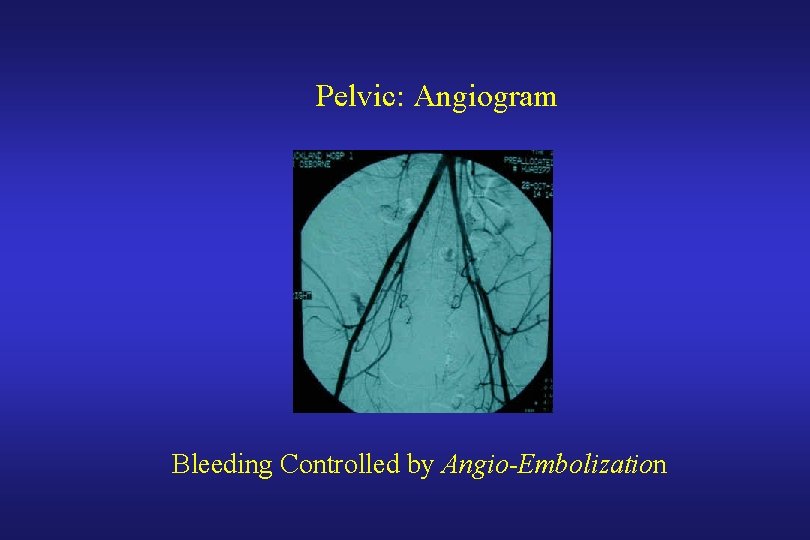
Pelvic: Angiogram Bleeding Controlled by Angio-Embolization
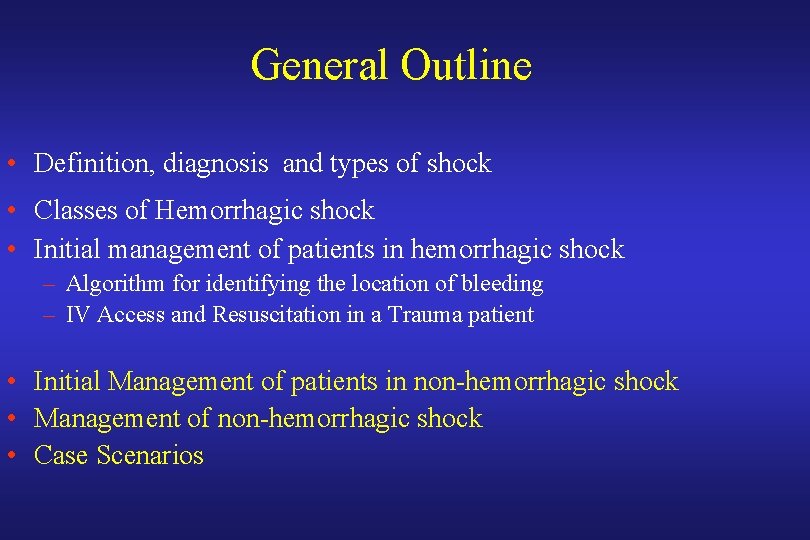
General Outline • Definition, diagnosis and types of shock • Classes of Hemorrhagic shock • Initial management of patients in hemorrhagic shock – Algorithm for identifying the location of bleeding – IV Access and Resuscitation in a Trauma patient • Initial Management of patients in non-hemorrhagic shock • Management of non-hemorrhagic shock • Case Scenarios
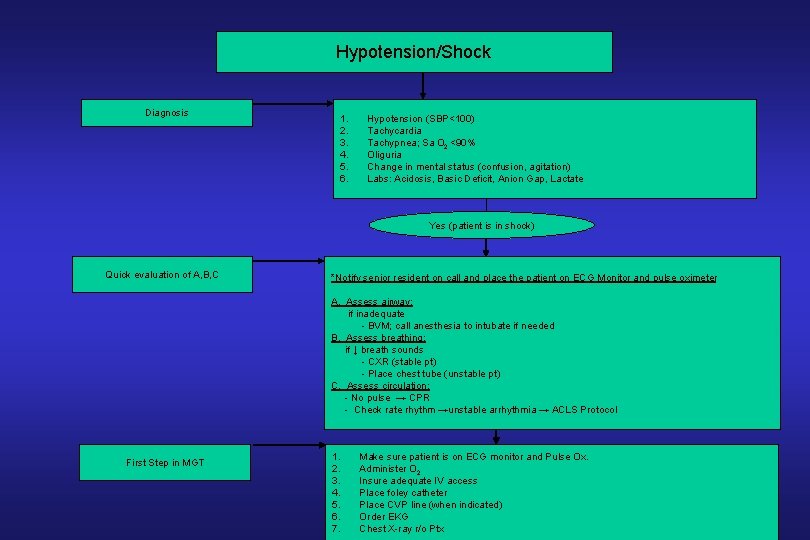
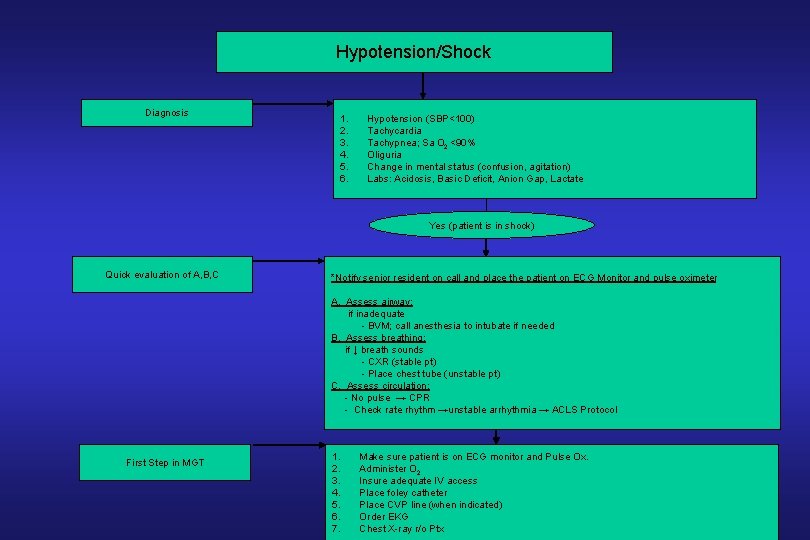
Hypotension/Shock Diagnosis 1. 2. 3. 4. 5. 6. Hypotension (SBP<100) Tachycardia Tachypnea; Sa O 2 <90% Oliguria Change in mental status (confusion, agitation) Labs: Acidosis, Basic Deficit, Anion Gap, Lactate Yes (patient is in shock) Quick evaluation of A, B, C *Notify senior resident on call and place the patient on ECG Monitor and pulse oximeter A. Assess airway: if inadequate - BVM; call anesthesia to intubate if needed B. Assess breathing: if ↓ breath sounds - CXR (stable pt) - Place chest tube (unstable pt) C. Assess circulation: - No pulse → CPR - Check rate rhythm →unstable arrhythmia → ACLS Protocol First Step in MGT 1. 2. 3. 4. 5. 6. 7. Make sure patient is on ECG monitor and Pulse Ox. Administer O 2 Insure adequate IV access Place foley catheter Place CVP line (when indicated) Order EKG Chest X-ray r/o Ptx
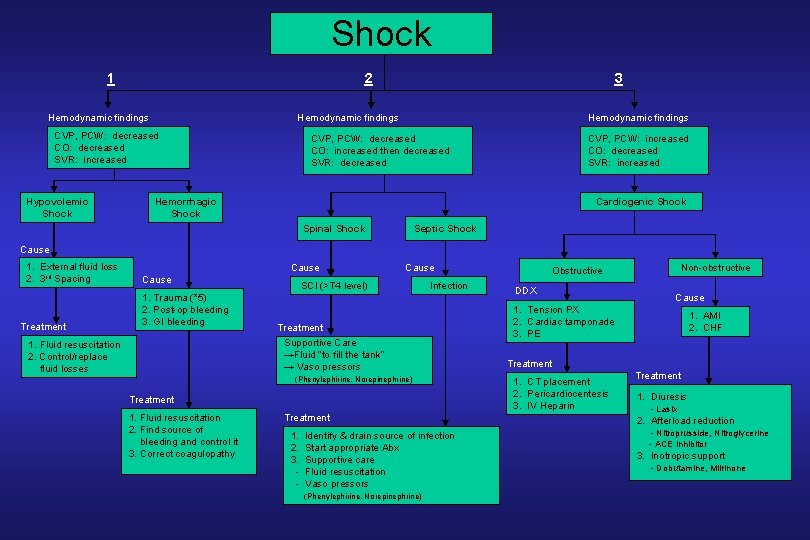
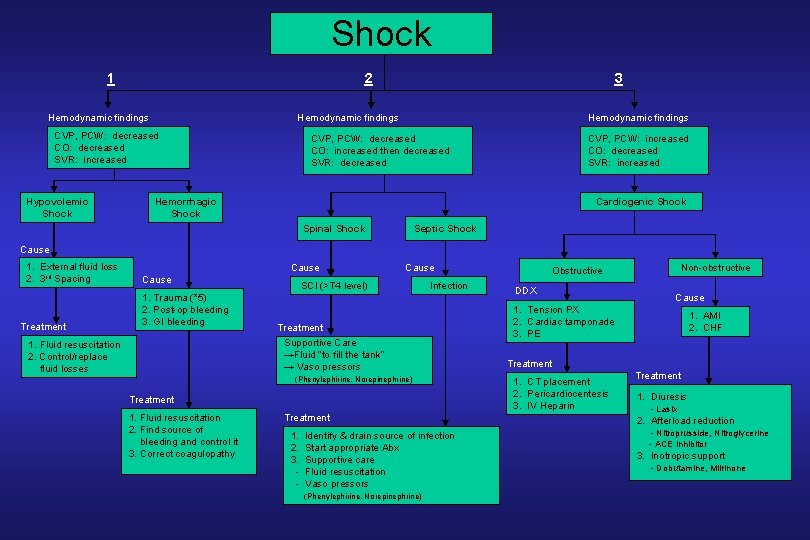
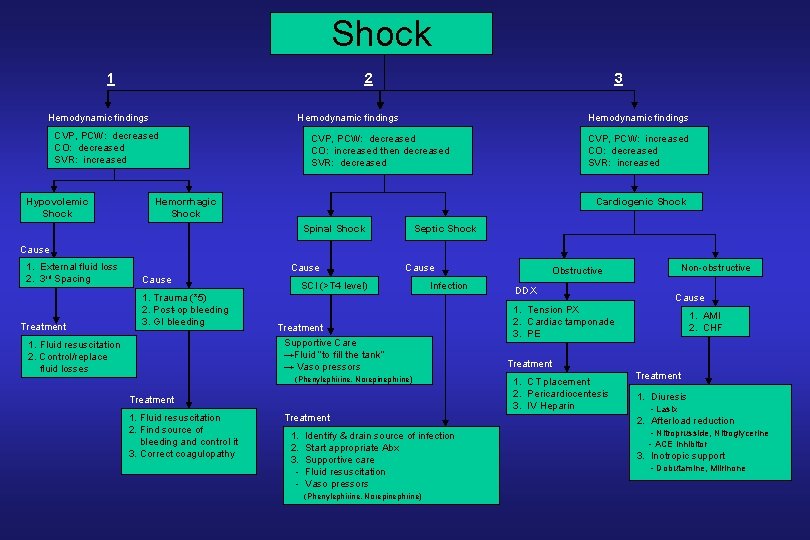
Shock 1 2 Hemodynamic findings CVP, PCW: decreased CO: decreased SVR: increased Hypovolemic Shock 3 Hemodynamic findings CVP, PCW: decreased CO: increased then decreased SVR: decreased CVP, PCW: increased CO: decreased SVR: increased Hemorrhagic Shock Cardiogenic Shock Spinal Shock Septic Shock Cause 1. External fluid loss 2. 3 rd Spacing Treatment Cause 1. Trauma (*5) 2. Post-op bleeding 3. GI bleeding 1. Fluid resuscitation 2. Control/replace fluid losses Cause SCI (>T 4 level) Infection Treatment Supportive Care →Fluid “to fill the tank” → Vaso pressors (Phenylephirine, Norepinephrine) Treatment 1. Fluid resuscitation 2. Find source of bleeding and control it 3. Correct coagulopathy Treatment 1. 2. 3. - Identify & drain source of infection Start appropriate Abx Supportive care Fluid resuscitation Vaso pressors (Phenylephirine, Norepinephrine) Non-obstructive Obstructive DDX Cause 1. Tension PX 2. Cardiac tamponade 3. PE 1. AMI 2. CHF Treatment 1. CT placement 2. Pericardiocentesis 3. IV Heparin Treatment 1. Diuresis - Lasix 2. Afterload reduction - Nitroprusside, Nitroglycerine - ACE inhibitor 3. Inotropic support - Dobutamine, Milrinone
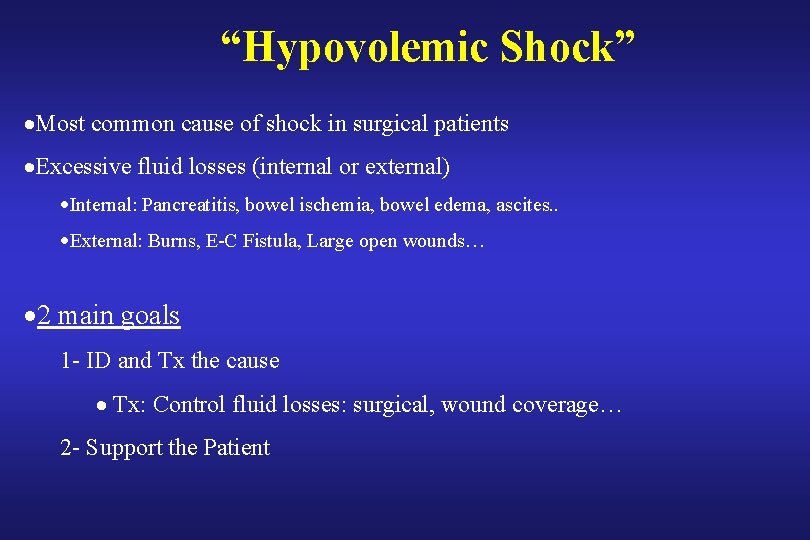
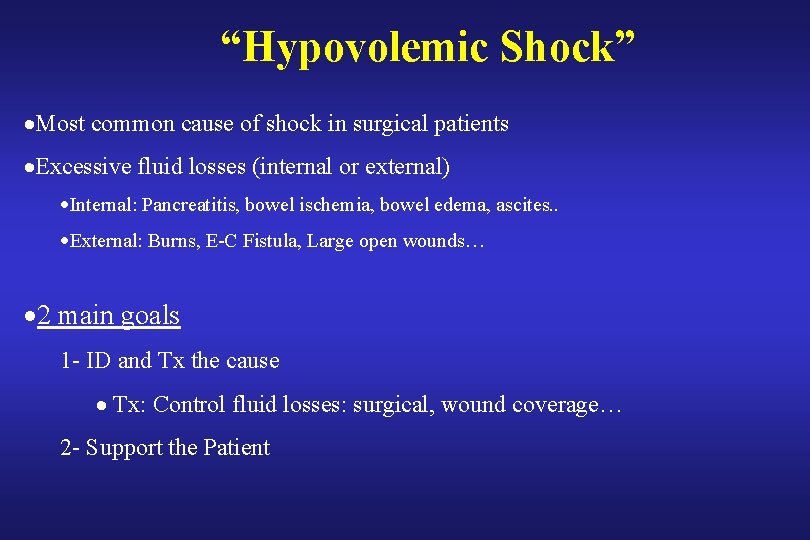
“Hypovolemic Shock” ·Most common cause of shock in surgical patients ·Excessive fluid losses (internal or external) ·Internal: Pancreatitis, bowel ischemia, bowel edema, ascites. . ·External: Burns, E-C Fistula, Large open wounds… · 2 main goals 1 - ID and Tx the cause · Tx: Control fluid losses: surgical, wound coverage… 2 - Support the Patient
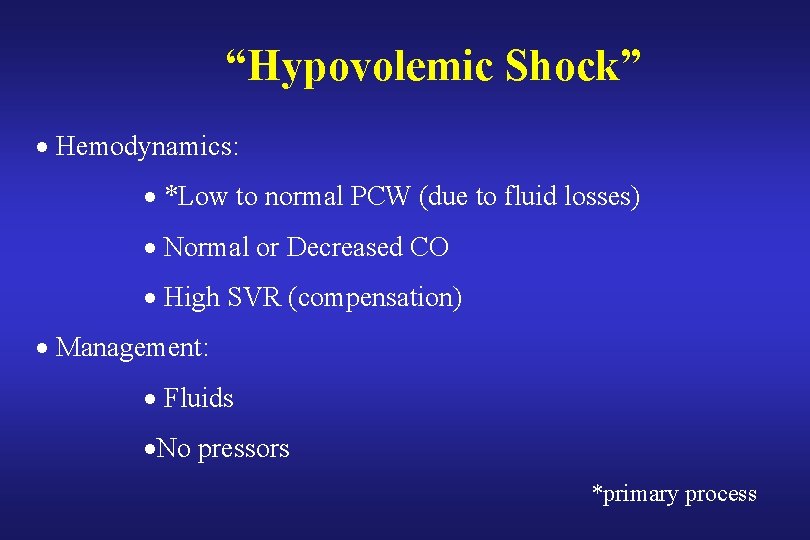
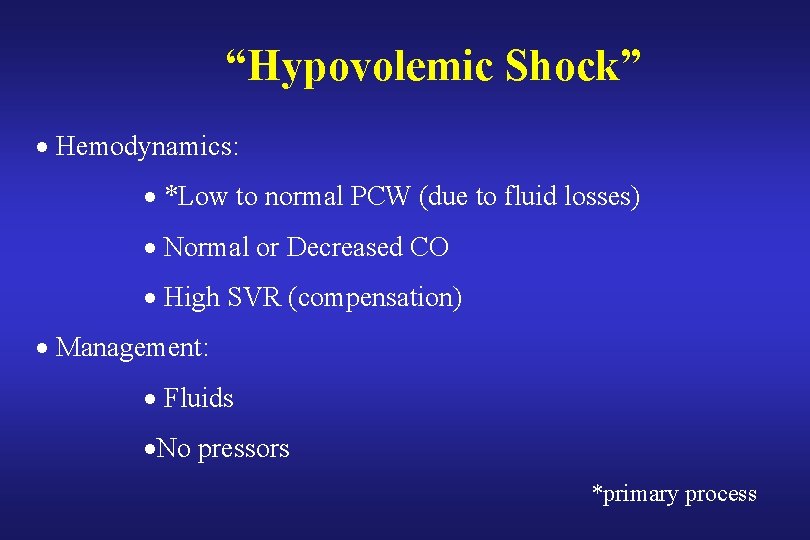
“Hypovolemic Shock” · Hemodynamics: · *Low to normal PCW (due to fluid losses) · Normal or Decreased CO · High SVR (compensation) · Management: · Fluids ·No pressors *primary process
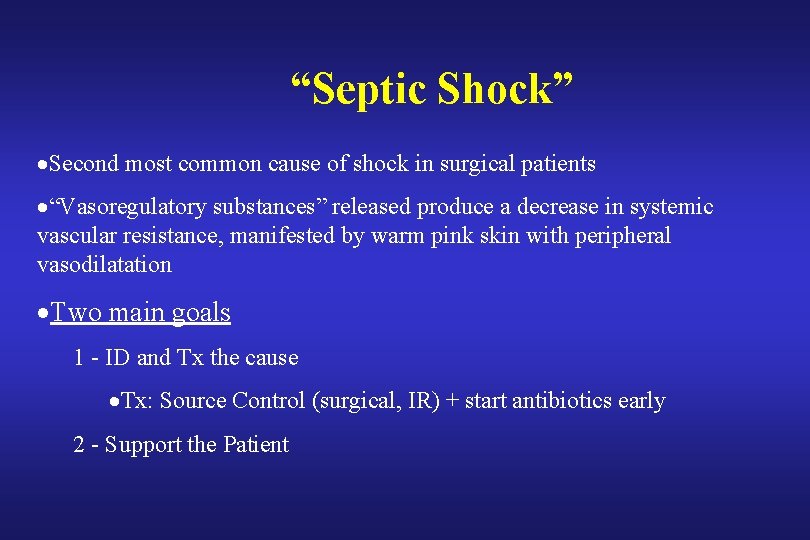
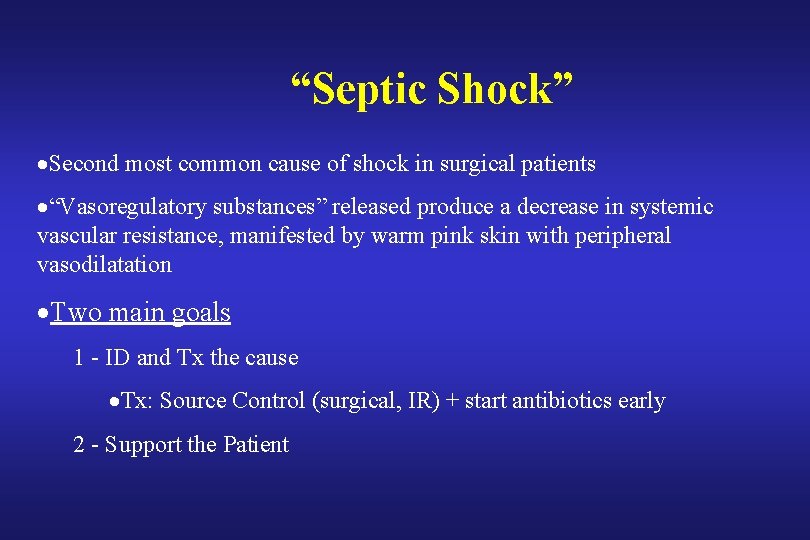
“Septic Shock” ·Second most common cause of shock in surgical patients ·“Vasoregulatory substances” released produce a decrease in systemic vascular resistance, manifested by warm pink skin with peripheral vasodilatation ·Two main goals 1 - ID and Tx the cause ·Tx: Source Control (surgical, IR) + start antibiotics early 2 - Support the Patient
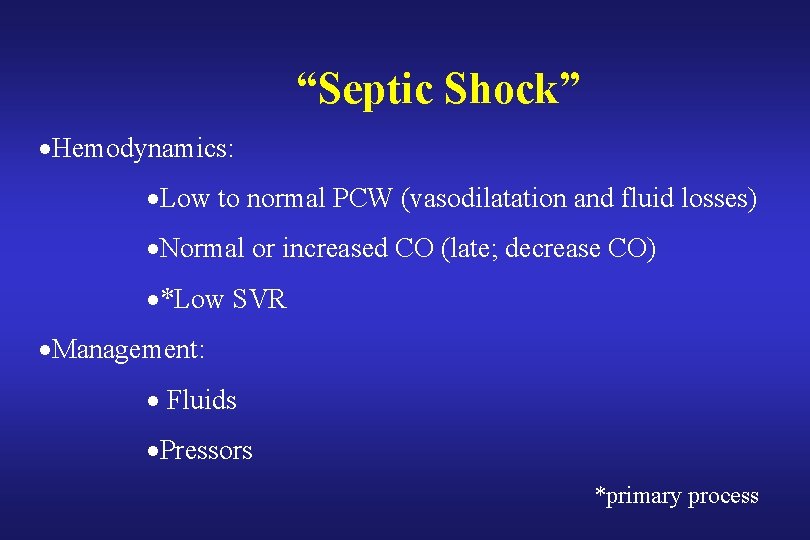
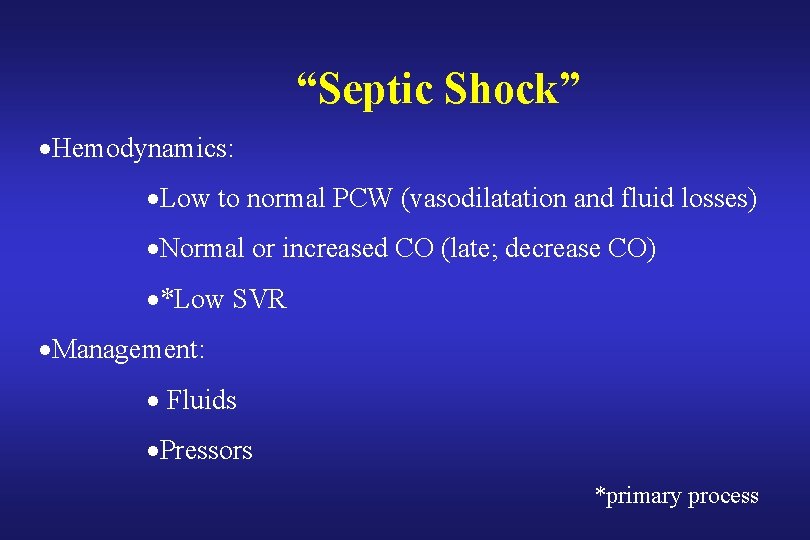
“Septic Shock” ·Hemodynamics: ·Low to normal PCW (vasodilatation and fluid losses) ·Normal or increased CO (late; decrease CO) ·*Low SVR ·Management: · Fluids ·Pressors *primary process
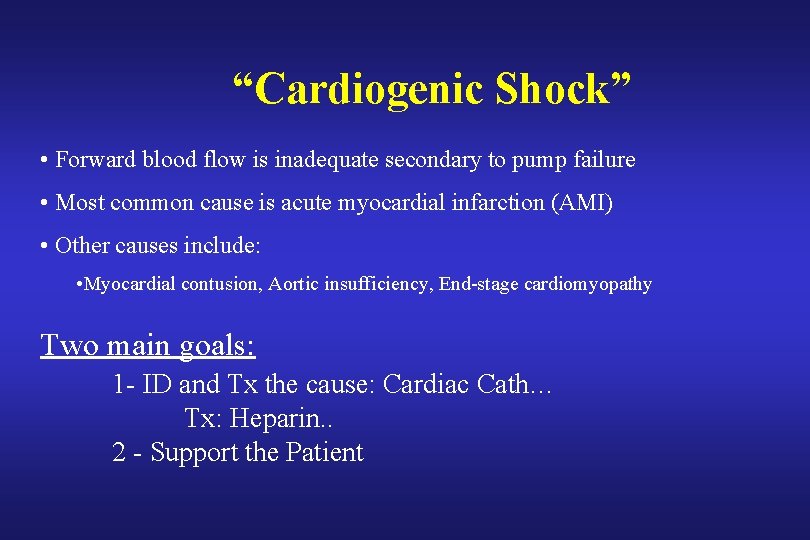
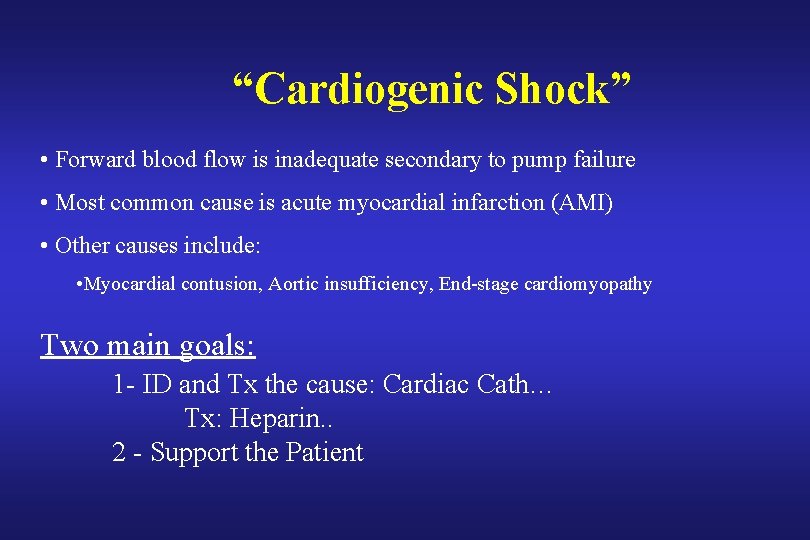
“Cardiogenic Shock” • Forward blood flow is inadequate secondary to pump failure • Most common cause is acute myocardial infarction (AMI) • Other causes include: • Myocardial contusion, Aortic insufficiency, End-stage cardiomyopathy Two main goals: 1 - ID and Tx the cause: Cardiac Cath… Tx: Heparin. . 2 - Support the Patient
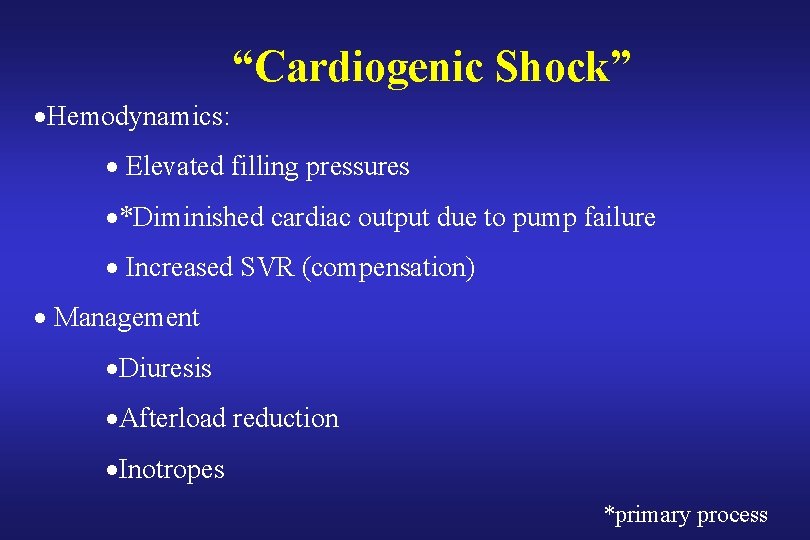
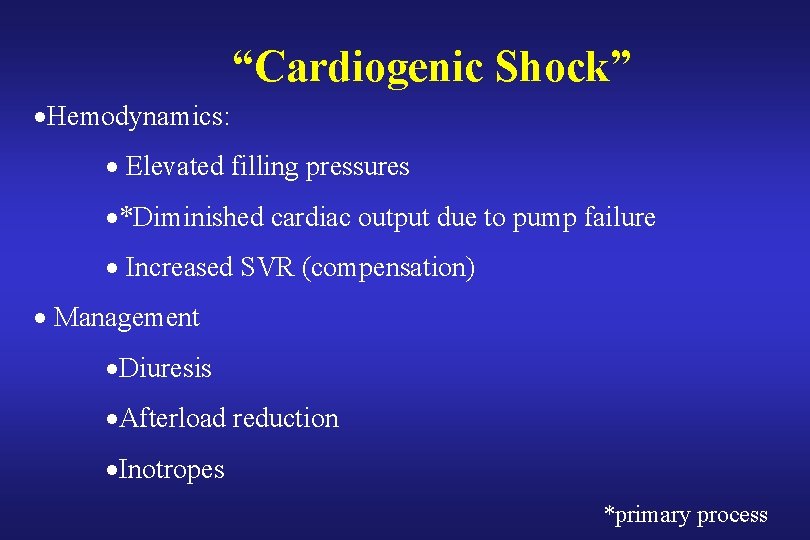
“Cardiogenic Shock” ·Hemodynamics: · Elevated filling pressures ·*Diminished cardiac output due to pump failure · Increased SVR (compensation) · Management ·Diuresis ·Afterload reduction ·Inotropes *primary process
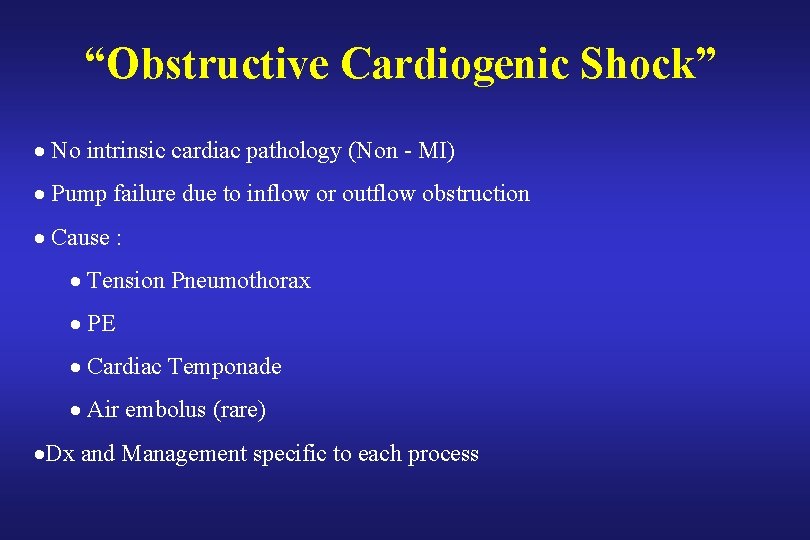
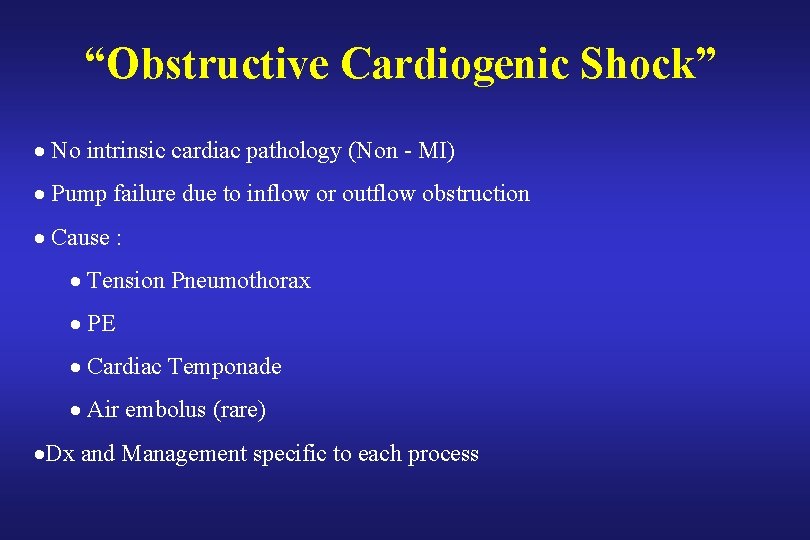
“Obstructive Cardiogenic Shock” · No intrinsic cardiac pathology (Non - MI) · Pump failure due to inflow or outflow obstruction · Cause : · Tension Pneumothorax · PE · Cardiac Temponade · Air embolus (rare) ·Dx and Management specific to each process
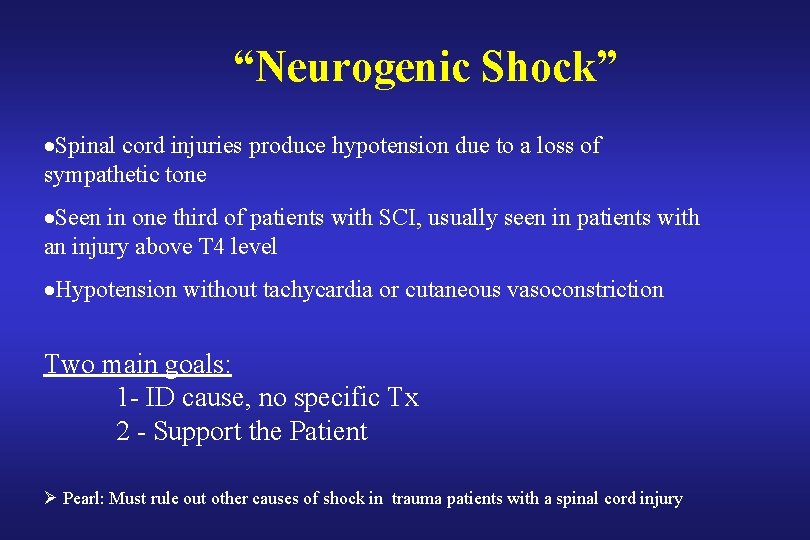
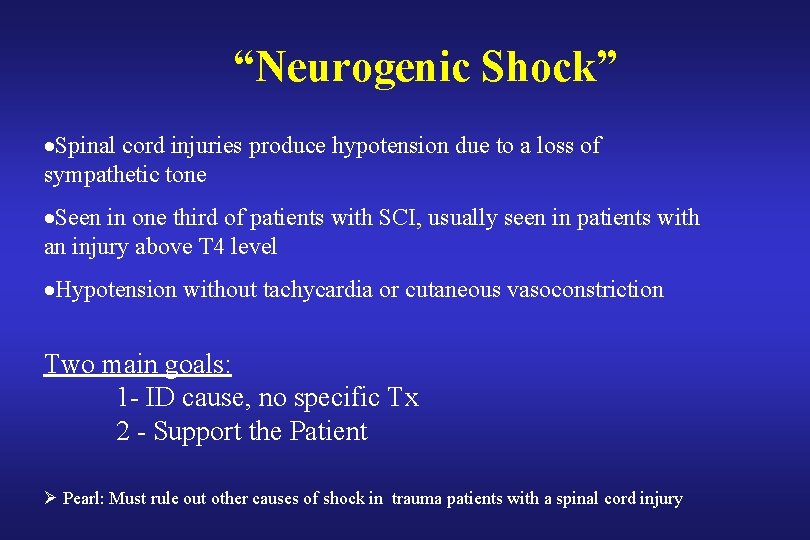
“Neurogenic Shock” ·Spinal cord injuries produce hypotension due to a loss of sympathetic tone ·Seen in one third of patients with SCI, usually seen in patients with an injury above T 4 level ·Hypotension without tachycardia or cutaneous vasoconstriction Two main goals: 1 - ID cause, no specific Tx 2 - Support the Patient Ø Pearl: Must rule out other causes of shock in trauma patients with a spinal cord injury
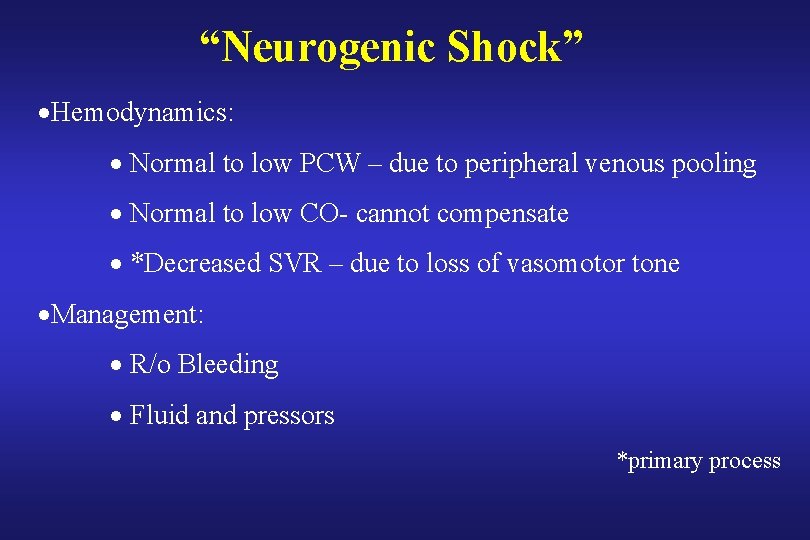
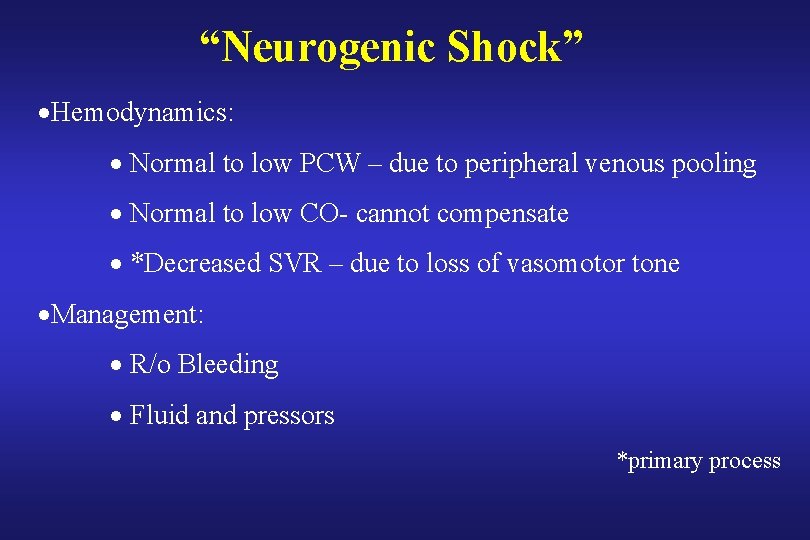
“Neurogenic Shock” ·Hemodynamics: · Normal to low PCW – due to peripheral venous pooling · Normal to low CO- cannot compensate · *Decreased SVR – due to loss of vasomotor tone ·Management: · R/o Bleeding · Fluid and pressors *primary process
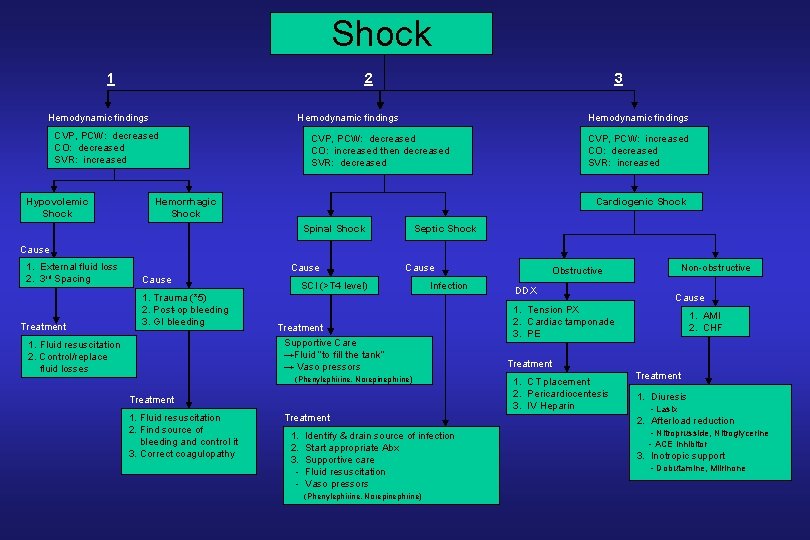
Shock 1 2 Hemodynamic findings CVP, PCW: decreased CO: decreased SVR: increased Hypovolemic Shock 3 Hemodynamic findings CVP, PCW: decreased CO: increased then decreased SVR: decreased CVP, PCW: increased CO: decreased SVR: increased Hemorrhagic Shock Cardiogenic Shock Spinal Shock Septic Shock Cause 1. External fluid loss 2. 3 rd Spacing Treatment Cause 1. Trauma (*5) 2. Post-op bleeding 3. GI bleeding 1. Fluid resuscitation 2. Control/replace fluid losses Cause SCI (>T 4 level) Infection Treatment Supportive Care →Fluid “to fill the tank” → Vaso pressors (Phenylephirine, Norepinephrine) Treatment 1. Fluid resuscitation 2. Find source of bleeding and control it 3. Correct coagulopathy Treatment 1. 2. 3. - Identify & drain source of infection Start appropriate Abx Supportive care Fluid resuscitation Vaso pressors (Phenylephirine, Norepinephrine) Non-obstructive Obstructive DDX Cause 1. Tension PX 2. Cardiac tamponade 3. PE 1. AMI 2. CHF Treatment 1. CT placement 2. Pericardiocentesis 3. IV Heparin Treatment 1. Diuresis - Lasix 2. Afterload reduction - Nitroprusside, Nitroglycerine - ACE inhibitor 3. Inotropic support - Dobutamine, Milrinone
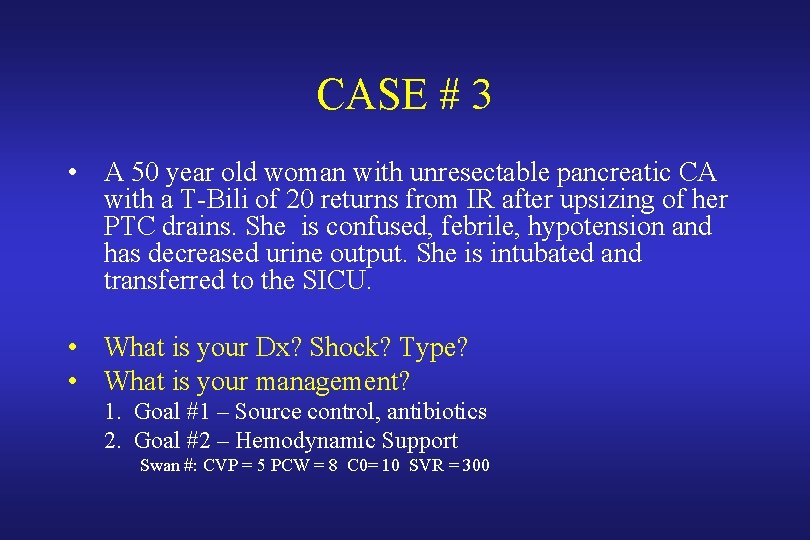
CASE # 3 • A 50 year old woman with unresectable pancreatic CA with a T-Bili of 20 returns from IR after upsizing of her PTC drains. She is confused, febrile, hypotension and has decreased urine output. She is intubated and transferred to the SICU. • What is your Dx? Shock? Type? • What is your management? 1. Goal #1 – Source control, antibiotics 2. Goal #2 – Hemodynamic Support Swan #: CVP = 5 PCW = 8 C 0= 10 SVR = 300
CASE # 4 • A 88 y/o F s/p AAA repair, post-op day 1 in the ICU, she is intubated. The nurse reports that she is hypotensive, BP 80/40, pulse 120 and her urine output is equal to less than 10 cc/H for the past 2 hours. She remains hypotensive despite 2 liters of fluid, labs; hemoglobin is 10, Hgb 10, Cr 1. 0 and lactate 4, BD -5. CVP is 15. • What is your Dx? Shock? Type? • What is your management? 1. Goal #1 – r/o MI & start appropriate treatment for MI 2. Goal #2 – Hemodynamic Support Swan #: CVP = 15 PCW = 18 C 0= 3 SVR = 1300
Conclusion: 1. How to recognize and diagnose shock 2. Types of shock (SHOCK): hemorrhagic & non-hemorrhagic 3. Hemorrhagic Shock: • Classes of hemorrhagic shock • Algorithm to find the location of bleeding and control it 4. Non-hemorrhagic shocks • the 2 key Goals in the management of any shock • Hemodynamic findings and support

THANK YOU ?

THANK YOU & GOOD LUCK