Hyponatremia and Hypernatremia Satwant Singh M D Professor


- Slides: 48
Hyponatremia and Hypernatremia Satwant Singh, M. D Professor of Medicine Division of Nephrology University of Cincinnati February 2, 2018
Disclosures None
Learning Objectives • • • Learn process of making dilute urine How to calculate osmolality and total body water deficit Apply physiology to clinical scenarios of hypo and hypernatremia Diagnosis of hypo and hypernatremia Treatment of hypo and hypernatremia
Hyponatremia/Hypernatremia Definitions Osmolality – number of osmoles (or m. OSm) in 1 Kg of solvent • Osmolarity – number of osmoles (or m. OSm) in 1 L of solvent • Both – sum total of osmotically active solutes in fluid (serum/extracellular fluid /intra-cellular fluid) • Tonicity – effective osmolarity/osmolality (solute unable to freely cross the membrane) •
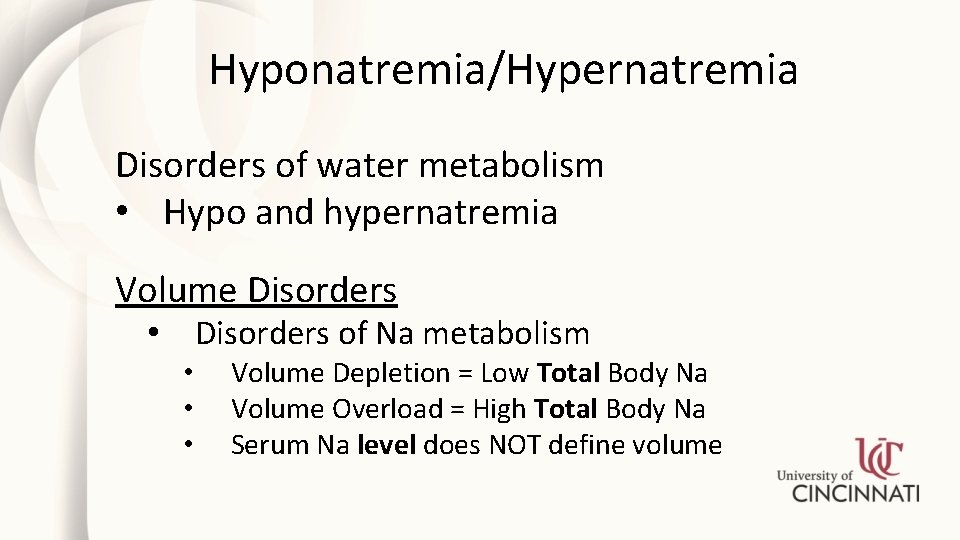
Hyponatremia/Hypernatremia Disorders of water metabolism • Hypo and hypernatremia Volume Disorders of Na metabolism • • Volume Depletion = Low Total Body Na Volume Overload = High Total Body Na Serum Na level does NOT define volume
Hyponatremia/Hypernatremia Are Disorders of water metabolism Both can be accompanied by: • • • Volume depletion – low BP/postural hypotension, tachycardia Volume expansion – edema, ascites Euvolumia
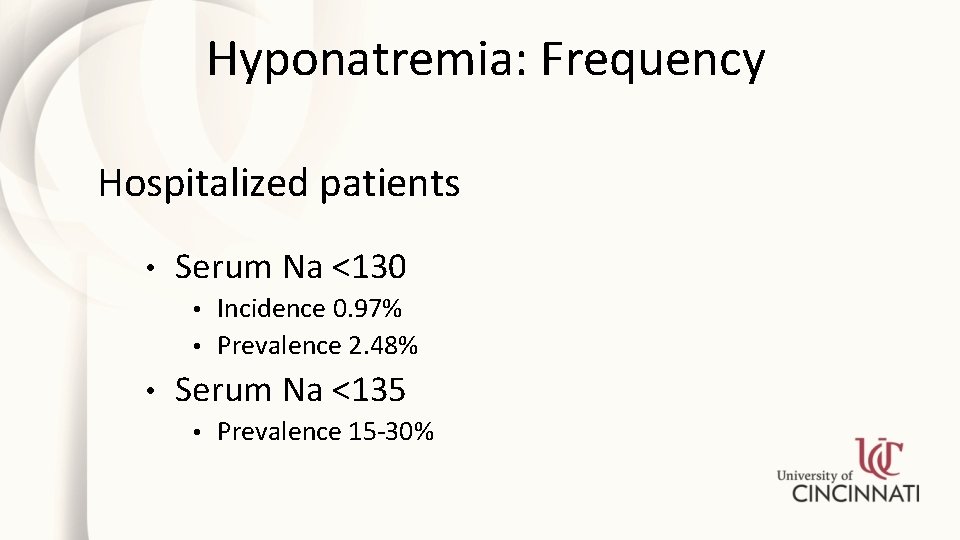
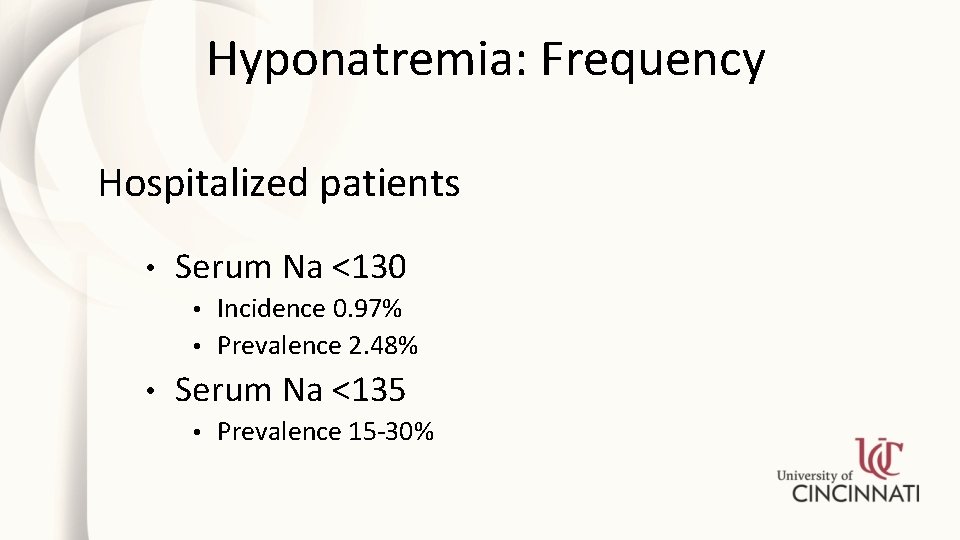
Hyponatremia: Frequency Hospitalized patients • Serum Na <130 Incidence 0. 97% • Prevalence 2. 48% • • Serum Na <135 • Prevalence 15 -30%
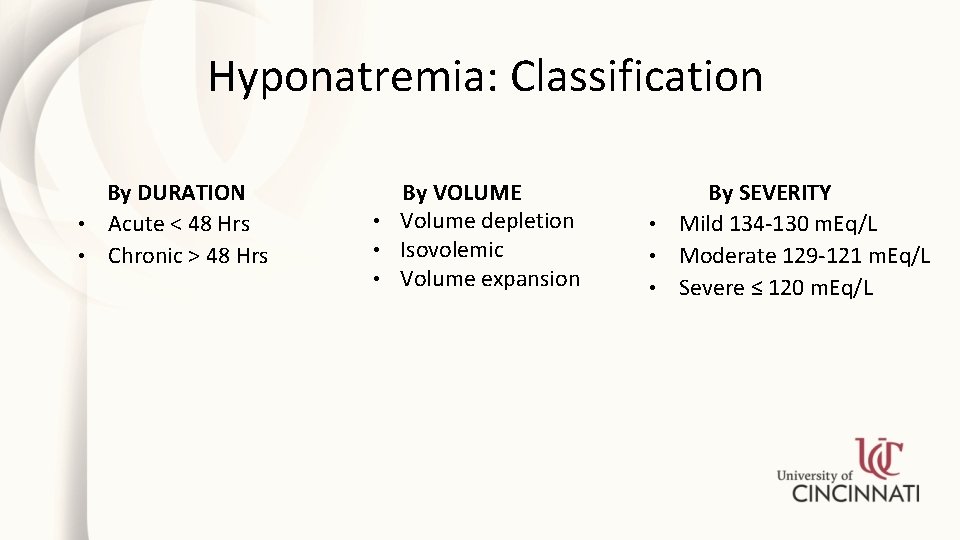
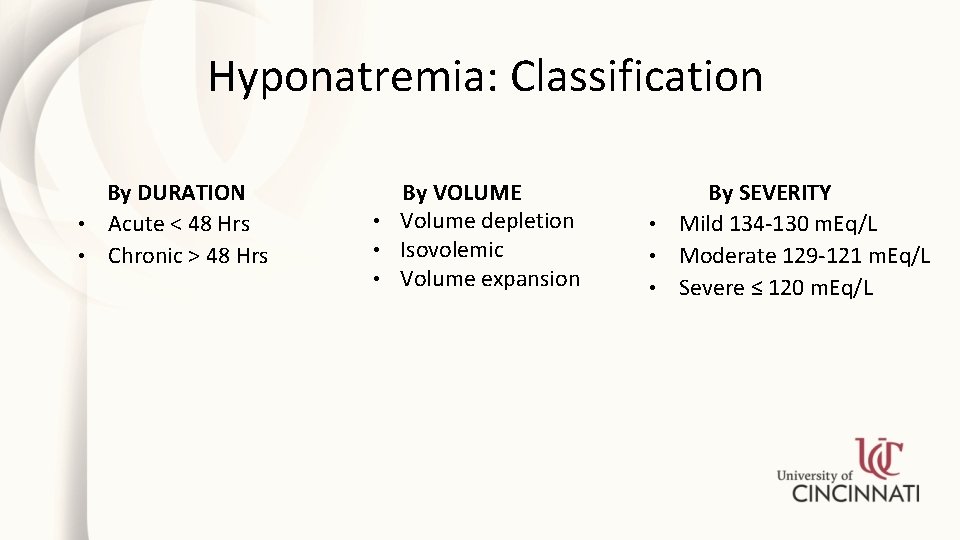
Hyponatremia: Classification By DURATION • Acute < 48 Hrs • Chronic > 48 Hrs By VOLUME • Volume depletion • Isovolemic • Volume expansion By SEVERITY • Mild 134 -130 m. Eq/L • Moderate 129 -121 m. Eq/L • Severe ≤ 120 m. Eq/L
Hyponatremia/Hypernatremia What is free water? • Electrolyte free water = Na-free water
Hyponatremia/Hypernatremia How a dilute urine is made is central to understanding Hyponatremia
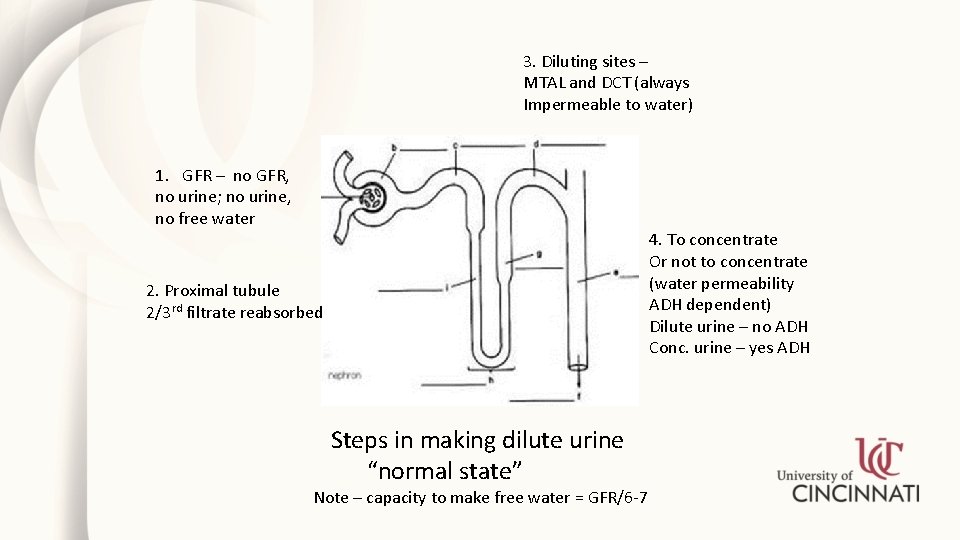
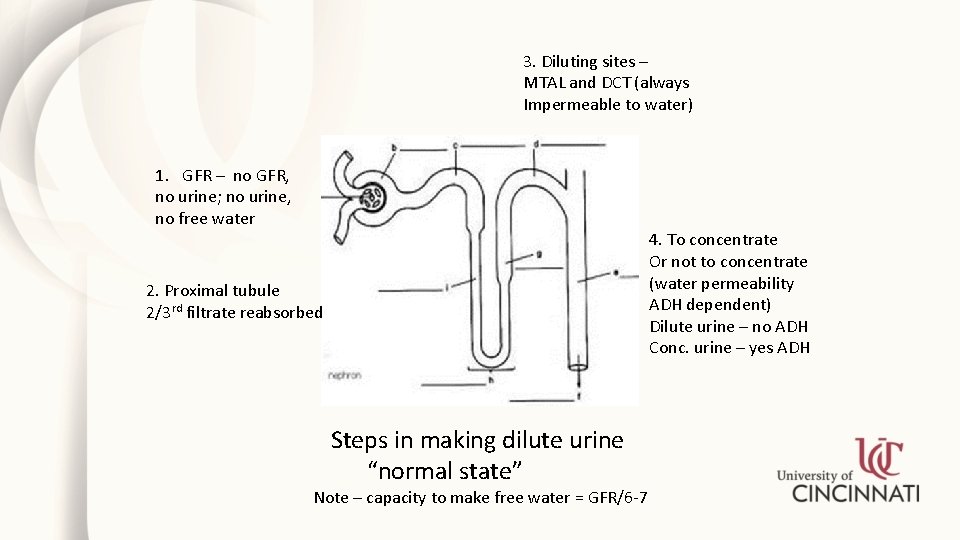
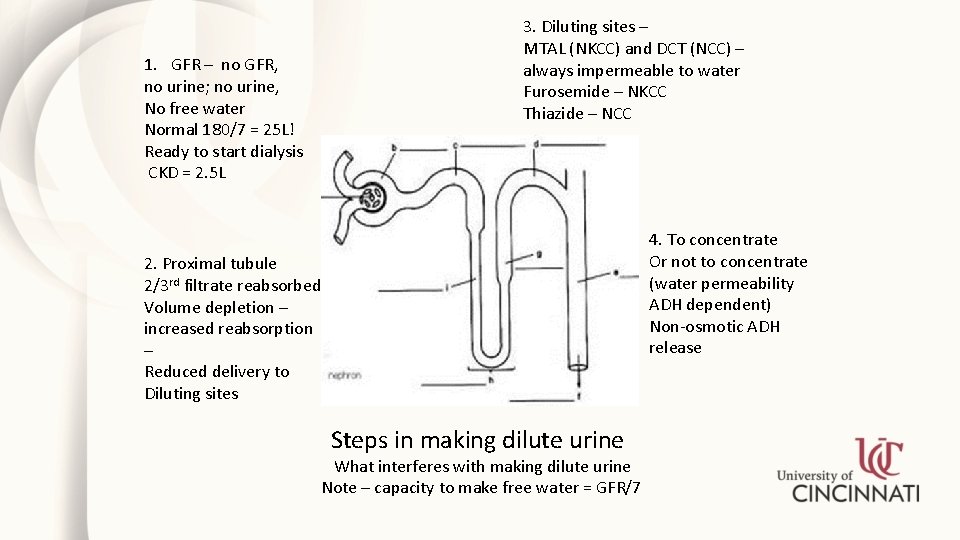
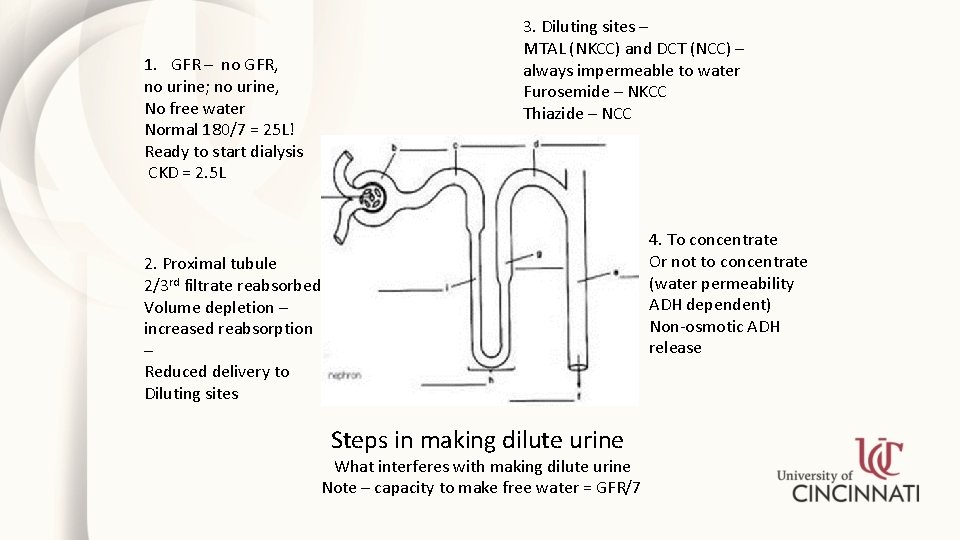
3. Diluting sites – MTAL and DCT (always Impermeable to water) 1. GFR – no GFR, no urine; no urine, no free water 4. To concentrate Or not to concentrate (water permeability ADH dependent) Dilute urine – no ADH Conc. urine – yes ADH 2. Proximal tubule 2/3 rd filtrate reabsorbed Steps in making dilute urine “normal state” Note – capacity to make free water = GFR/6 -7
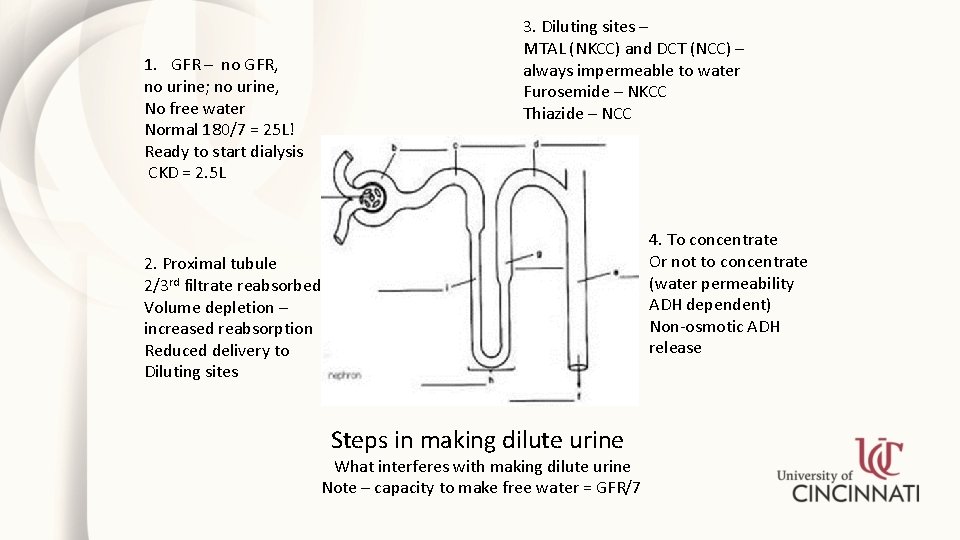
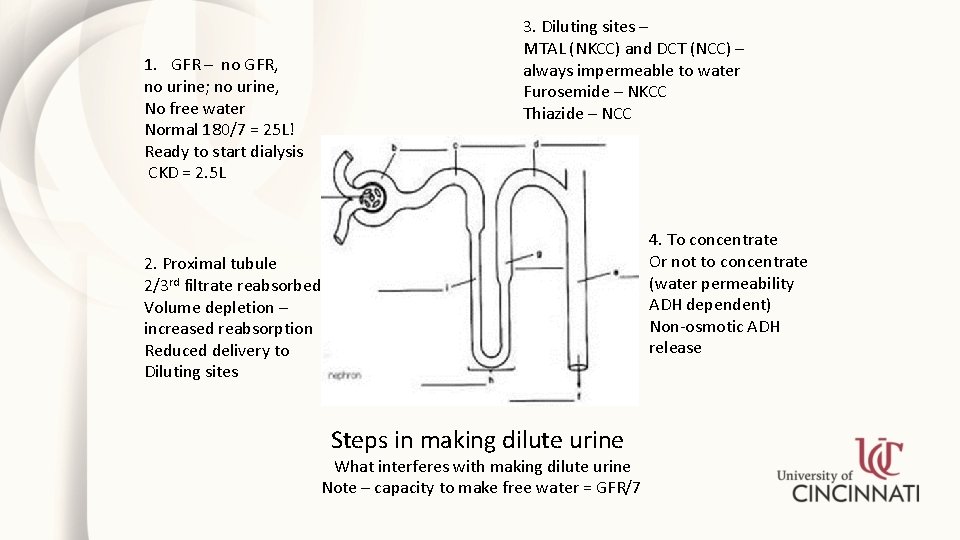
1. GFR – no GFR, no urine; no urine, No free water Normal 180/7 = 25 L! Ready to start dialysis CKD = 2. 5 L 3. Diluting sites – MTAL (NKCC) and DCT (NCC) – always impermeable to water Furosemide – NKCC Thiazide – NCC 4. To concentrate Or not to concentrate (water permeability ADH dependent) Non-osmotic ADH release 2. Proximal tubule 2/3 rd filtrate reabsorbed Volume depletion – increased reabsorption Reduced delivery to Diluting sites Steps in making dilute urine What interferes with making dilute urine Note – capacity to make free water = GFR/7
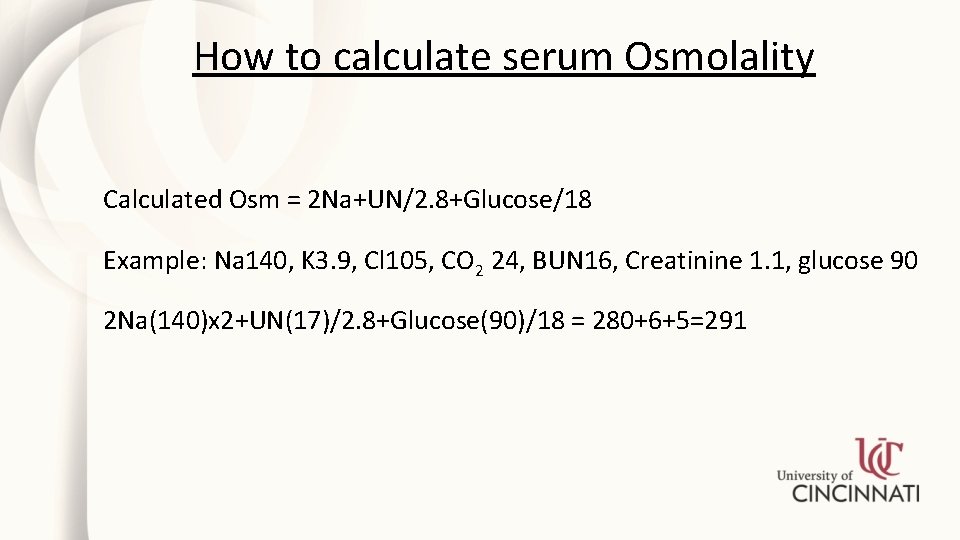
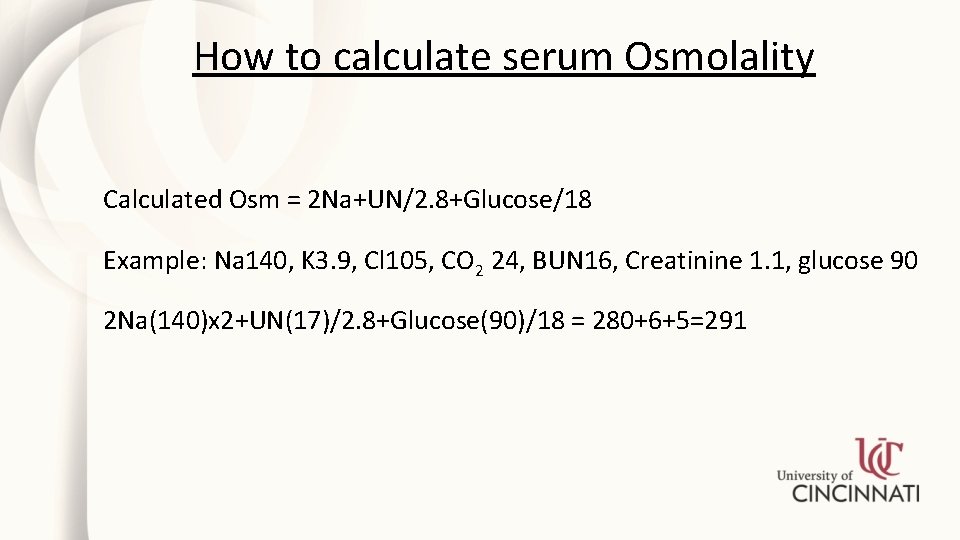
How to calculate serum Osmolality Calculated Osm = 2 Na+UN/2. 8+Glucose/18 Example: Na 140, K 3. 9, Cl 105, CO 2 24, BUN 16, Creatinine 1. 1, glucose 90 2 Na(140)x 2+UN(17)/2. 8+Glucose(90)/18 = 280+6+5=291

Total Body Water Deficit How to calculate total body water deficit Normal TBW x Normal Na = Current TBW x Current Na Example: 100 Kg male admitted with Na of 150 N TBW = C TBW x C Na/N Na = (100 x 0. 6) x 150/140 = 60 x 150/140 = 64. 3 TBW Deficit = 64. 3 -60 = 4. 3 L ____ TBW = Total Body Water
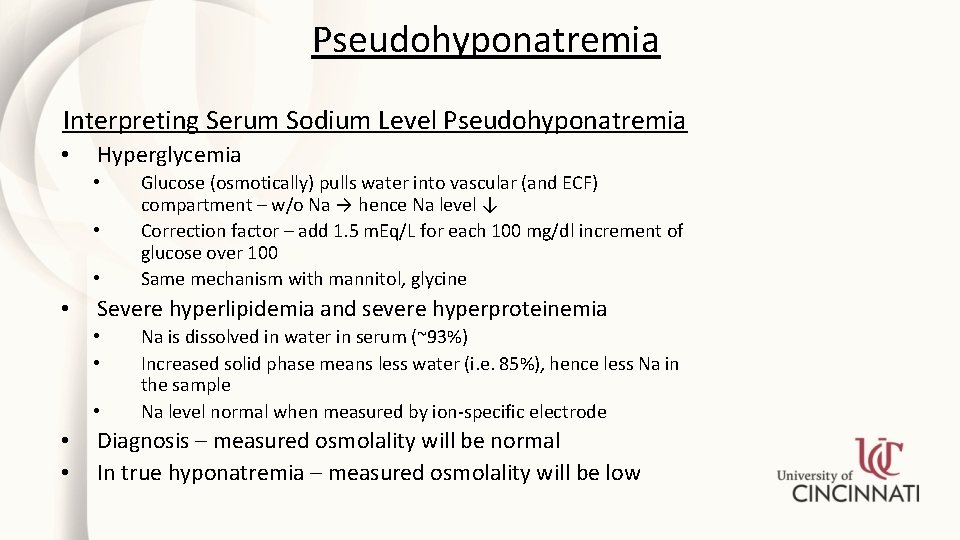
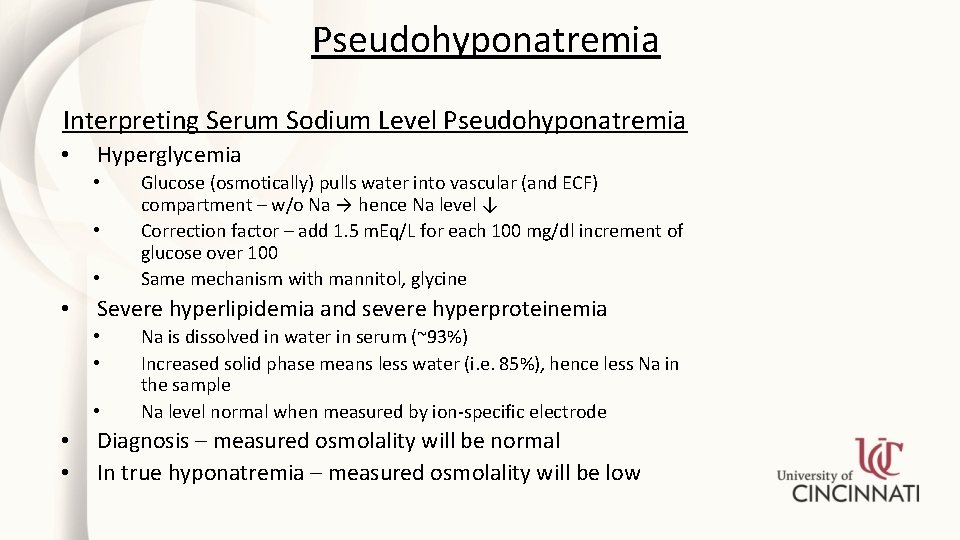
Pseudohyponatremia Interpreting Serum Sodium Level Pseudohyponatremia • Hyperglycemia • • Severe hyperlipidemia and severe hyperproteinemia • • • Glucose (osmotically) pulls water into vascular (and ECF) compartment – w/o Na → hence Na level ↓ Correction factor – add 1. 5 m. Eq/L for each 100 mg/dl increment of glucose over 100 Same mechanism with mannitol, glycine Na is dissolved in water in serum (~93%) Increased solid phase means less water (i. e. 85%), hence less Na in the sample Na level normal when measured by ion-specific electrode Diagnosis – measured osmolality will be normal In true hyponatremia – measured osmolality will be low
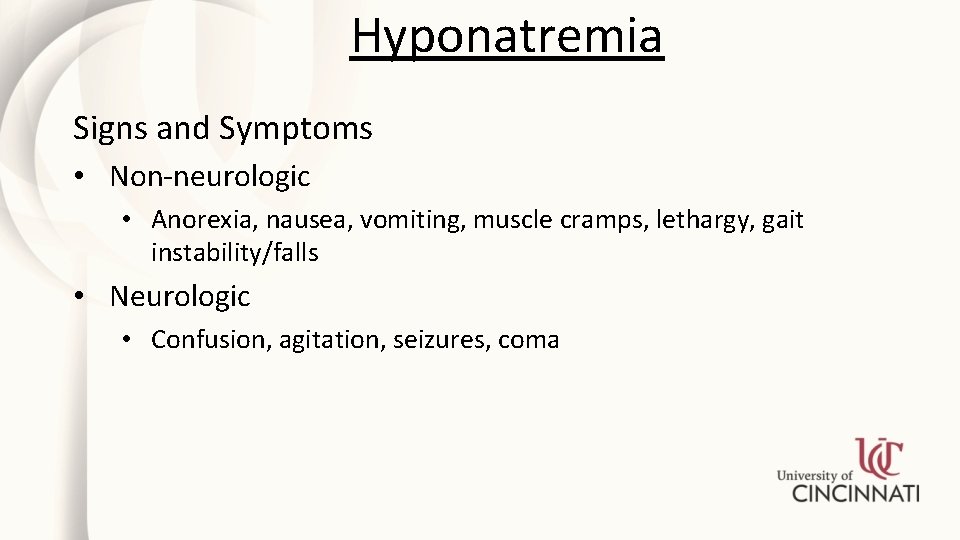
Hyponatremia Signs and Symptoms • Non-neurologic • Anorexia, nausea, vomiting, muscle cramps, lethargy, gait instability/falls • Neurologic • Confusion, agitation, seizures, coma
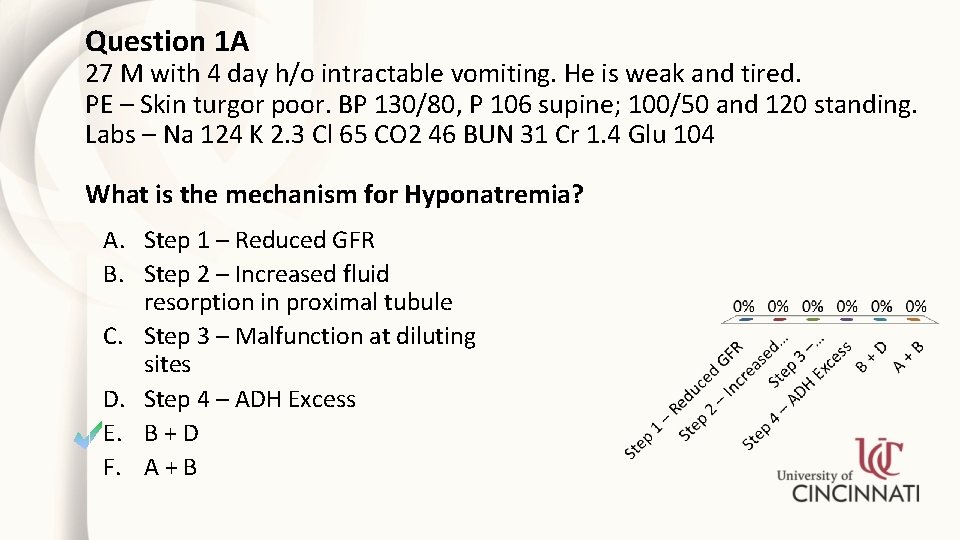
Question 1 A 27 M with 4 day h/o intractable vomiting. He is weak and tired. PE – Skin turgor poor. BP 130/80, P 106 supine; 100/50 and 120 standing. Labs – Na 124 K 2. 3 Cl 65 CO 2 46 BUN 31 Cr 1. 4 Glu 104 What is the mechanism for Hyponatremia? A. Step 1 – Reduced GFR B. Step 2 – Increased fluid resorption in proximal tubule C. Step 3 – Malfunction at diluting sites D. Step 4 – ADH Excess E. B + D F. A + B
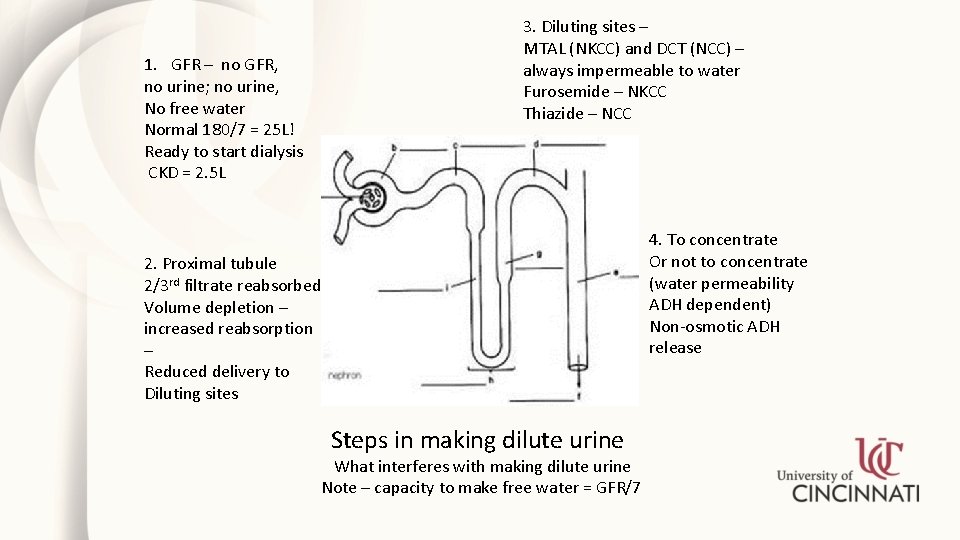
1. GFR – no GFR, no urine; no urine, No free water Normal 180/7 = 25 L! Ready to start dialysis CKD = 2. 5 L 3. Diluting sites – MTAL (NKCC) and DCT (NCC) – always impermeable to water Furosemide – NKCC Thiazide – NCC 4. To concentrate Or not to concentrate (water permeability ADH dependent) Non-osmotic ADH release 2. Proximal tubule 2/3 rd filtrate reabsorbed Volume depletion – increased reabsorption – Reduced delivery to Diluting sites Steps in making dilute urine What interferes with making dilute urine Note – capacity to make free water = GFR/7
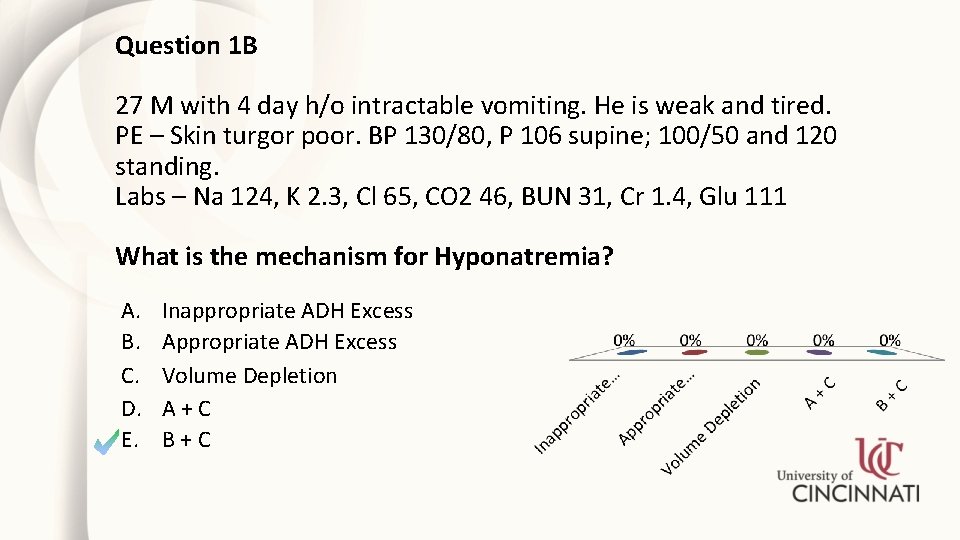
Question 1 B 27 M with 4 day h/o intractable vomiting. He is weak and tired. PE – Skin turgor poor. BP 130/80, P 106 supine; 100/50 and 120 standing. Labs – Na 124, K 2. 3, Cl 65, CO 2 46, BUN 31, Cr 1. 4, Glu 111 What is the mechanism for Hyponatremia? A. B. C. D. E. Inappropriate ADH Excess Appropriate ADH Excess Volume Depletion A+C B+C
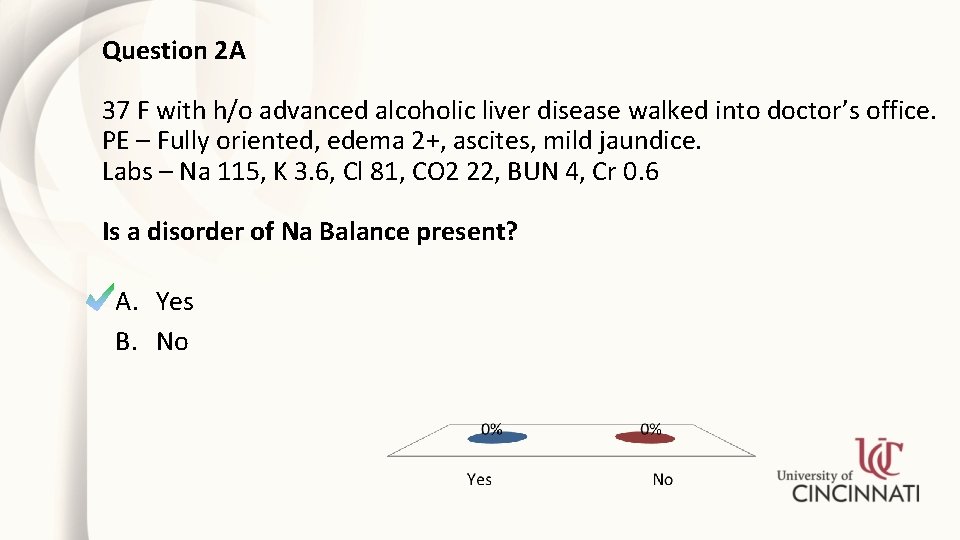
Question 2 A 37 F with h/o advanced alcoholic liver disease walked into doctor’s office. PE – Fully oriented, edema 2+, ascites, mild jaundice. Labs – Na 115, K 3. 6, Cl 81, CO 2 22, BUN 4, Cr 0. 6 Is a disorder of Na Balance present? A. Yes B. No
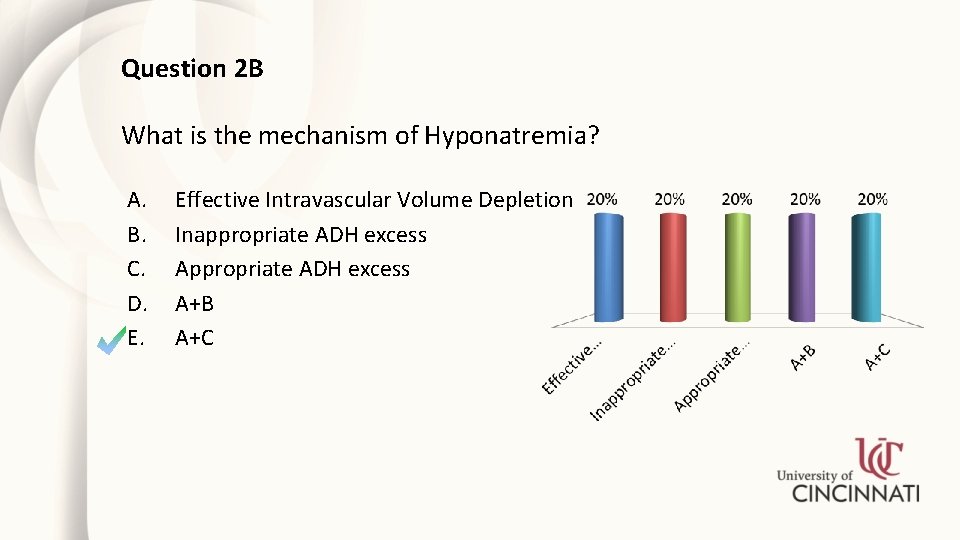
Question 2 B What is the mechanism of Hyponatremia? A. B. C. D. E. Effective Intravascular Volume Depletion Inappropriate ADH excess A+B A+C
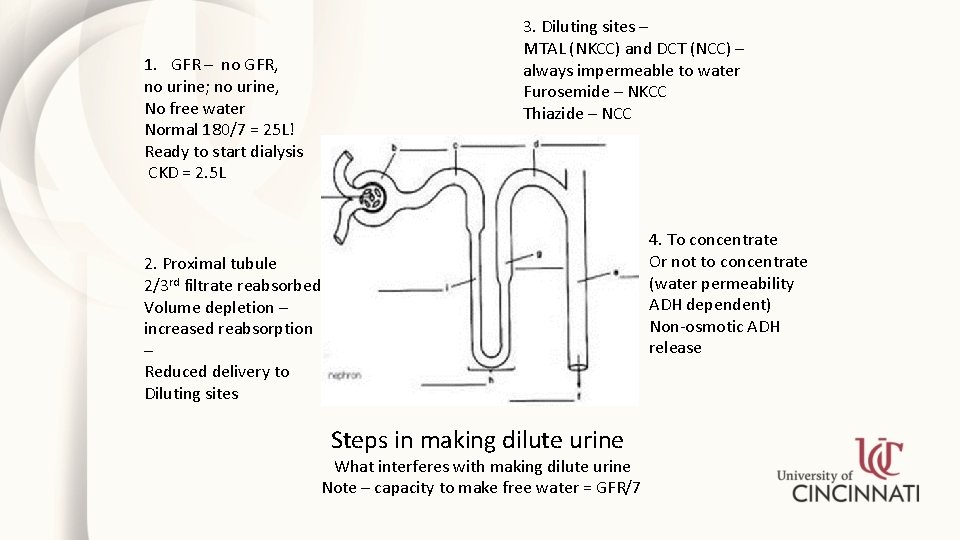
1. GFR – no GFR, no urine; no urine, No free water Normal 180/7 = 25 L! Ready to start dialysis CKD = 2. 5 L 3. Diluting sites – MTAL (NKCC) and DCT (NCC) – always impermeable to water Furosemide – NKCC Thiazide – NCC 4. To concentrate Or not to concentrate (water permeability ADH dependent) Non-osmotic ADH release 2. Proximal tubule 2/3 rd filtrate reabsorbed Volume depletion – increased reabsorption – Reduced delivery to Diluting sites Steps in making dilute urine What interferes with making dilute urine Note – capacity to make free water = GFR/7
Question 2 c • • • 37 F with h/o advanced alcoholic liver disease walked into doctor’s office. PE – Fully oriented, edema 2+, ascites, mild jaundice. Labs – Na 115 K 3. 6 Cl 81 CO 2 22 BUN 4 Cr 0. 6
Question 2 C How will you manage hyponatremia? A. I/V Normal Saline B. I/V Hypertonic Saline C. Water restriction
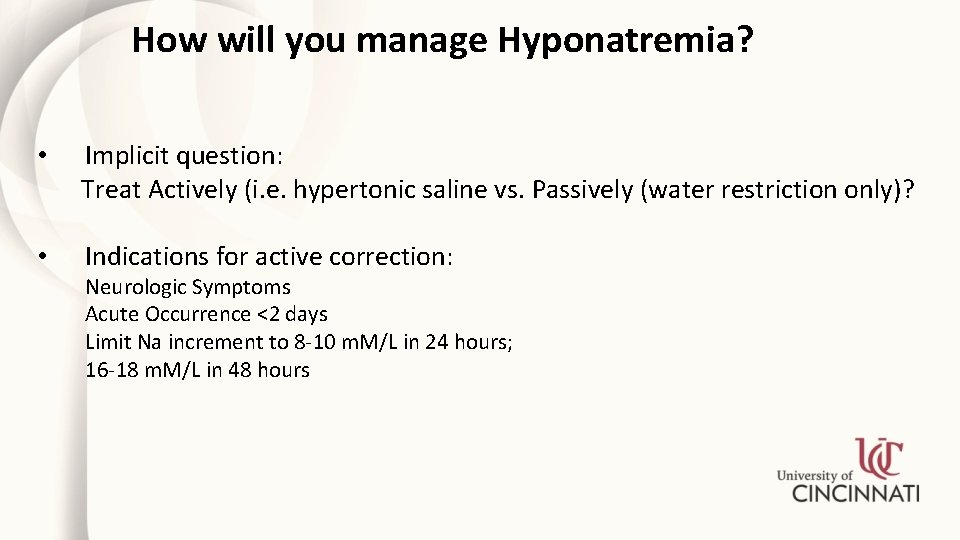
How will you manage Hyponatremia? • Implicit question: Treat Actively (i. e. hypertonic saline vs. Passively (water restriction only)? • Indications for active correction: Neurologic Symptoms Acute Occurrence <2 days Limit Na increment to 8 -10 m. M/L in 24 hours; 16 -18 m. M/L in 48 hours
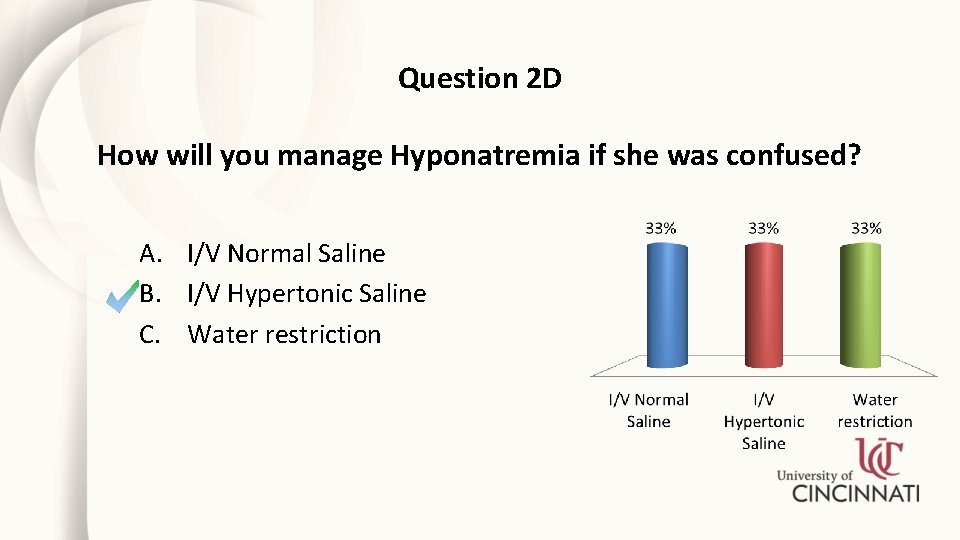
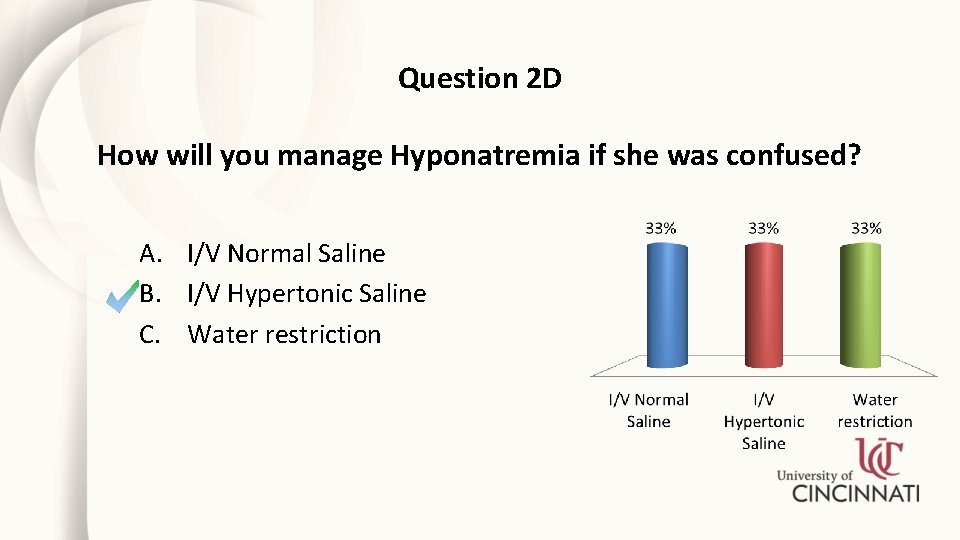
Question 2 D How will you manage Hyponatremia if she was confused? A. I/V Normal Saline B. I/V Hypertonic Saline C. Water restriction
Stimuli for ADH release • Osmolality • • Volume • • • Very sensitive; 1 -2 m. Osm change, changes ADH level ADH shuts off at serum osmolality of 280 – maximally dilute urine Maximally concentrated urine at serum osmolality of 295 Crude: ~7% volume depletion before release Very potent Miscellaneous – pain, nausea and vomiting, anesthesia, surgery, intracranial pathology, drugs
SIADH: Definition • • Hypotonic hyponatremia No renal or adrenal disease No edema or volume depletion Inability to dilute urine (Urine osm. > 100)
SIADH Helpful tests for SIADH • • • Single digit BUN UNa >30 m. Eq/L Serum uric acid ≤ 2. 5 mg/d. L FEUN >55% FEUA >12% Drop in serum Na following NS infusion
SIADH Copeptin • • • Enzymatic cleavage of vasopressin prohormone produces vasopressin, neurophysin and copeptin Copeptin is stable, easy to measure, unlike vasopressin Copeptin levels • High in SIADH • Low in polydipsia
SIADH Causes • Carcinomas: lung, duodenum, ureter, pancreas, prostate • Pulmonary: tuberculosis, pneumonia, positive pressure breathing • CNS: encephalitis, meningitis, trauma, brain abscess, SAH, Guillain-Barré syndrome, CVA, MS • Drugs: Ecstasy, SSRIs, NSAIDs, desmopressin, oxytocin, cyclophosphamide, tricyclic antidepressants, anti-psychotics, narcotics • Miscellaneous: HIV, idiopathic, nephrogenic
Hyponatremia: Considerations during treatment A balancing act between the effects of hyponatremia and its treatment • Risk of hyponatremia • • • Cerebral edema, eventually temporal herniation Risk of rapid correction • Osmotic demyelination syndrome
Hyponatremia Treatment • • Water restriction • Works if intake < ability to excrete free water Monitoring active sodium correction • Check Na level q 3 -4 Hrs initially • Most important thing to watch is urine volume • If urine volume increases abruptly, the stimulus for ADH release is gone • Stop active correction • May need reversal of over-correction (D 5 W or desmopressin)
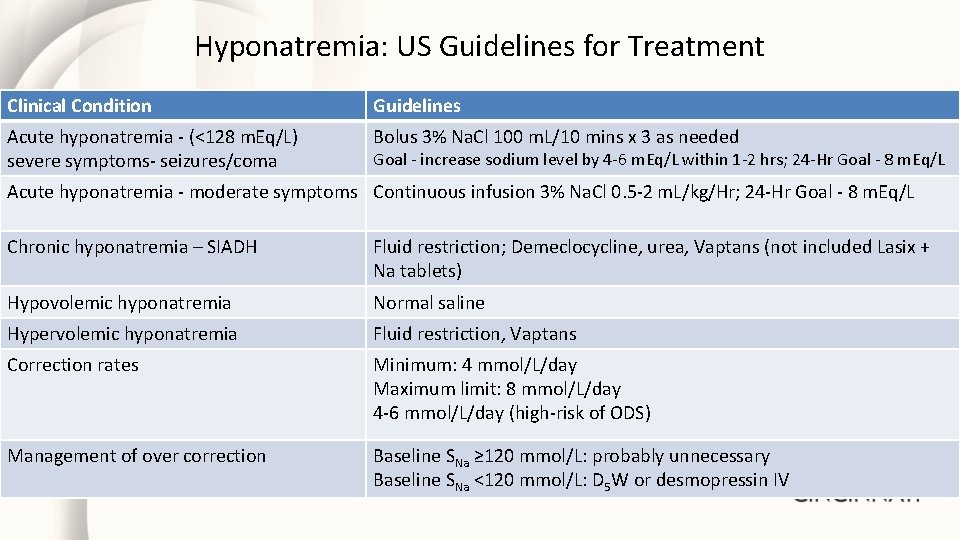
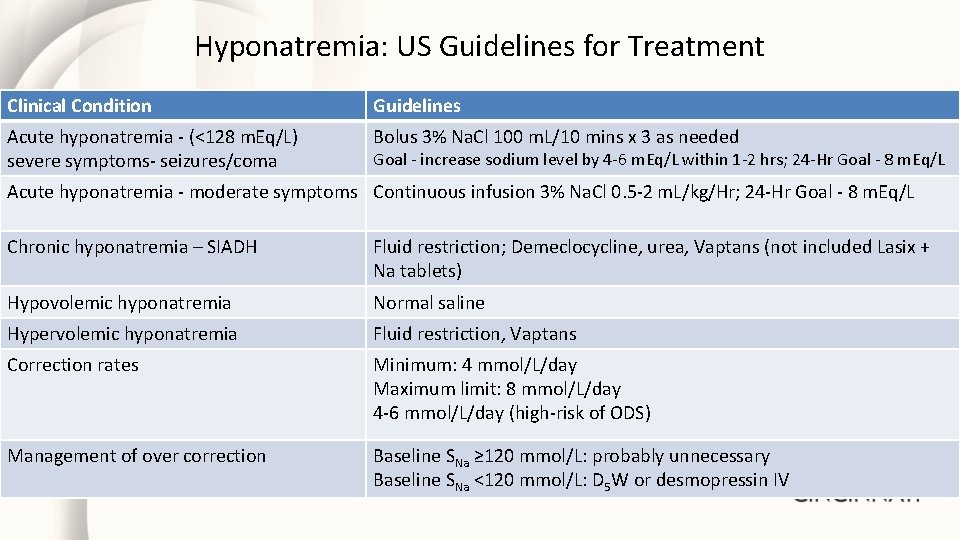
Hyponatremia: US Guidelines for Treatment Clinical Condition Guidelines Acute hyponatremia - (<128 m. Eq/L) severe symptoms- seizures/coma Bolus 3% Na. Cl 100 m. L/10 mins x 3 as needed Goal - increase sodium level by 4 -6 m. Eq/L within 1 -2 hrs; 24 -Hr Goal - 8 m. Eq/L Acute hyponatremia - moderate symptoms Continuous infusion 3% Na. Cl 0. 5 -2 m. L/kg/Hr; 24 -Hr Goal - 8 m. Eq/L Chronic hyponatremia – SIADH Fluid restriction; Demeclocycline, urea, Vaptans (not included Lasix + Na tablets) Hypovolemic hyponatremia Normal saline Hypervolemic hyponatremia Fluid restriction, Vaptans Correction rates Minimum: 4 mmol/L/day Maximum limit: 8 mmol/L/day 4 -6 mmol/L/day (high-risk of ODS) Management of over correction Baseline SNa ≥ 120 mmol/L: probably unnecessary Baseline SNa <120 mmol/L: D 5 W or desmopressin IV
Hyponatremia: High-risk for ODS Alcoholism • Liver disease • Malnutrition • Hypokalemia •
Hypernatremia: Causes • Loss of Free Water • Gain of salt (rare)
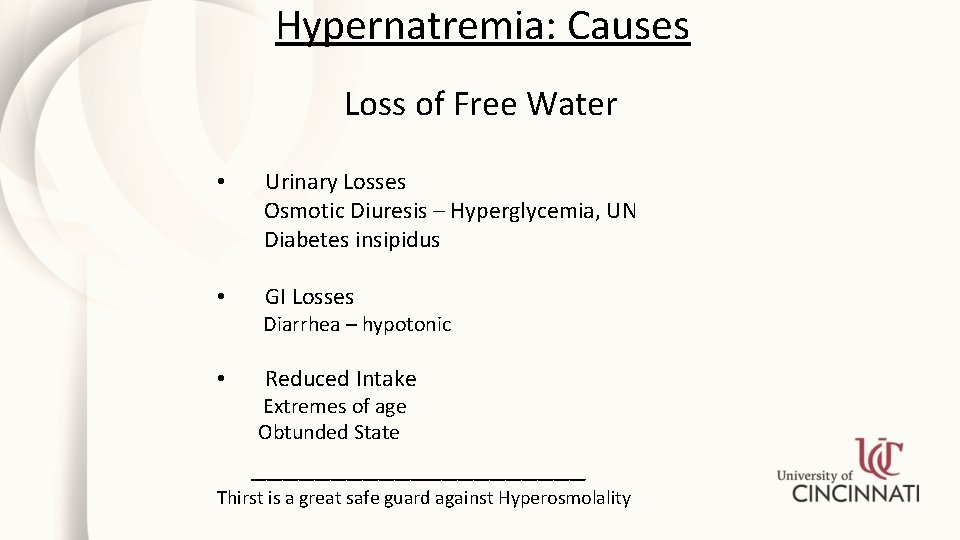
Hypernatremia: Causes Loss of Free Water • Urinary Losses Osmotic Diuresis – Hyperglycemia, UN Diabetes insipidus • GI Losses Diarrhea – hypotonic • Reduced Intake Extremes of age Obtunded State ___________ Thirst is a great safe guard against Hyperosmolality
Hypernatremia Gain of Na • • I/V Na. HCO 3 (Cardiac Resuscitation) Salt Water Drowning
Hypernatremia Signs and Symptoms • Restlessness • Lethargy • Irritability • Hyperreflexia • Spasticity • Intracranial hemorrhage
Question 3 A • 45 M with known h/o DM, CAD and HTN presents with increased thirst, polyuria, weakness and fatigue. • PE – Weight 62. 5 Kg; BP 120/70, Pulse 105 supine; BP 95/70, pulse 115 standing. Poor skin turgor, dry mucus membranes. • Labs – Na 157 K 4. 2 Cl 116 CO 2 22 BUN 76 Cr 2. 9, Glu 967
Question 3 A Is a disorder of Na balance present? A. Yes B. No
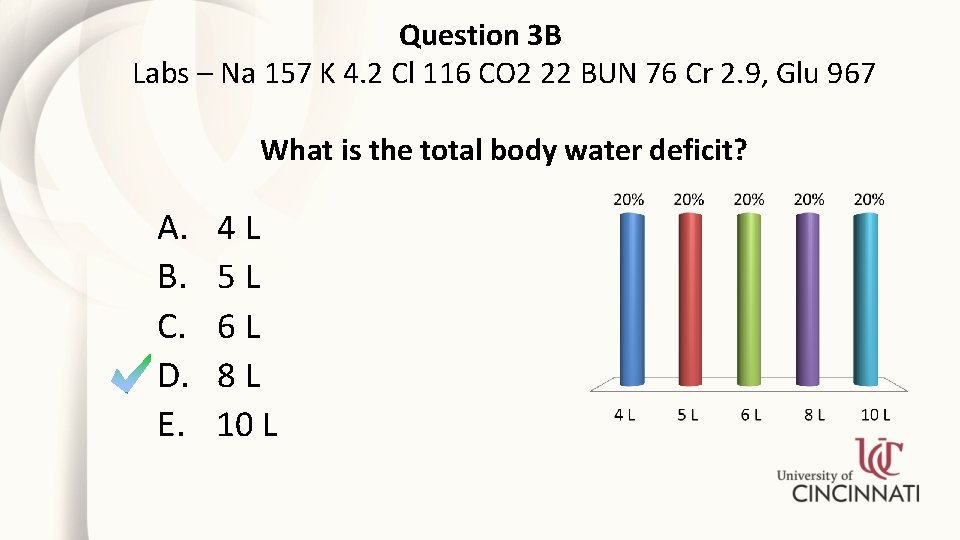
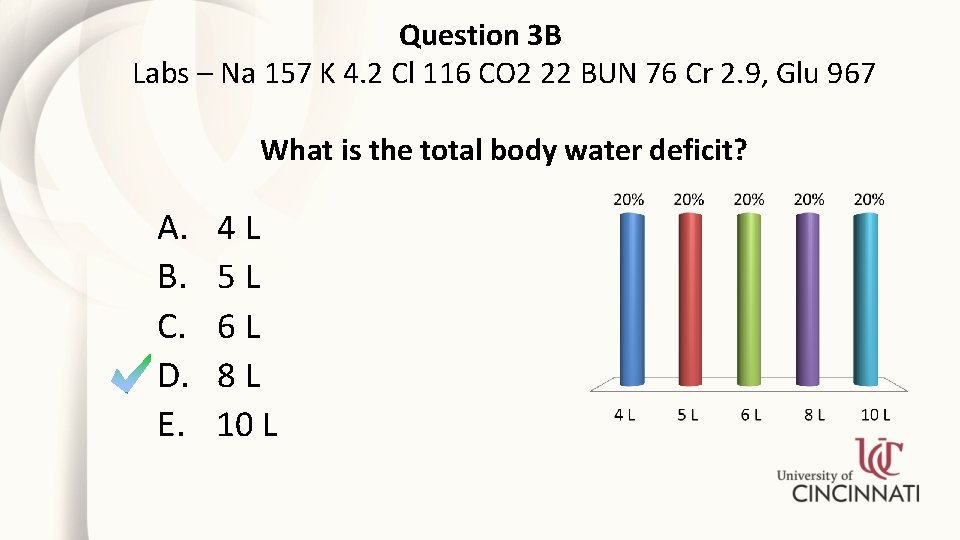
Question 3 B Labs – Na 157 K 4. 2 Cl 116 CO 2 22 BUN 76 Cr 2. 9, Glu 967 What is the total body water deficit? A. B. C. D. E. 4 L 5 L 6 L 8 L 10 L
Fluid and Electrolyte Disorders Case Study 3 How will you manage hypernatremia initially? A. Normal Saline B. Dextrose in Water C. Half-Normal Saline
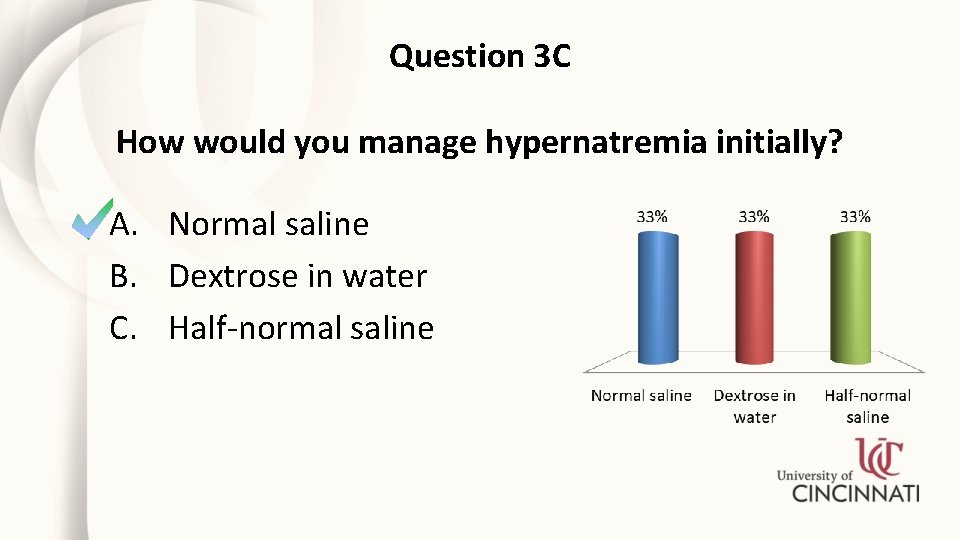
Question 3 C How would you manage hypernatremia initially? A. Normal saline B. Dextrose in water C. Half-normal saline
Question 3 c How will you manage hypernatremia? • First correct volume depletion with NS • Insulin to correct hyperglycemia • Then correct water deficit with D 5 W at the rate of 0. 5 m. Eq/L/Hr (10 -12 m. Eq/day)
Hyponatremia and Hypernatremia Summary • • • Good H & P Exclude pseudohyponatremia (serum Osm) Carefully look at the renal panel (K, UN, Creat, CO 2) Urine Na and Osm If unclear – Serum Uric Acid, FEUN, FEUA, i/v Saline
Hyponatremia and Hypernatremia Summary Diagnosis and Management need: • • • Physiologic diagnosis – what step(s) for excreting dilute urine went bad Volume Status Acute or Chronic Neurologic Symptoms Active treatment – hypertonic saline, Vaptans, Urea, Demeclocycline Passive treatment – water restriction

Thank You