Hypokalemia and Hyperkalemia Dr Madhukar Mittal Medical Endocrinology
- Slides: 27
Hypokalemia and Hyperkalemia Dr Madhukar Mittal Medical Endocrinology
Hypokalemia 1. Spurious − Extreme leukocytosis • (WBC uptake of K+ in the test tube)
2. Transcellular shift – Stress induced catecholamine release • – Drugs • • – Insulin Theophylline, β 2 agonists Anabolic state • • • – Asthma, COPD exacerbation, CHF, MI/Angina, Drug withdrawal syndrome Vit B 12 or Folate treatment GM-CSF TPN Hypokalemic periodic paralysis 3. Decreased Total Body K+
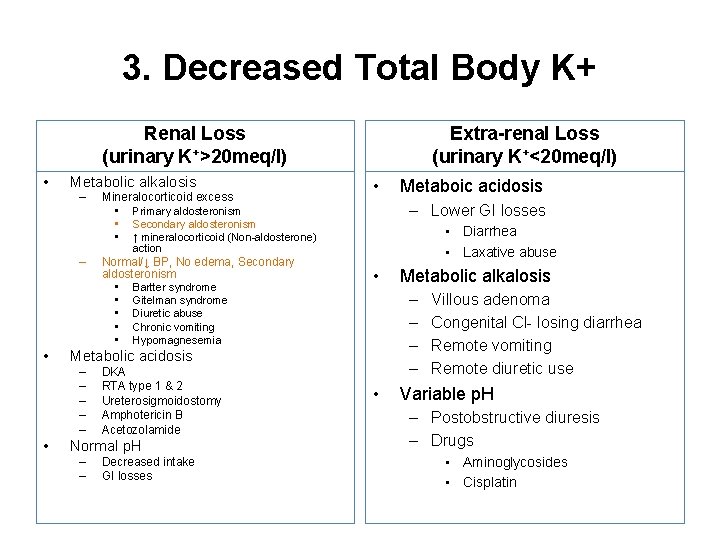
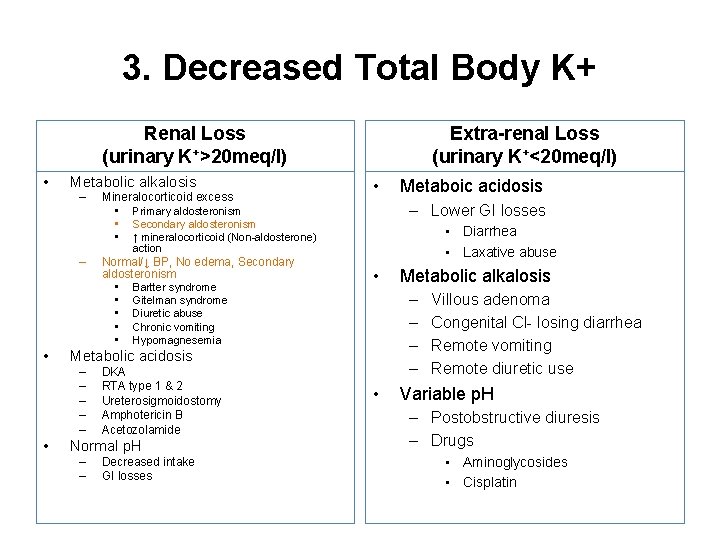
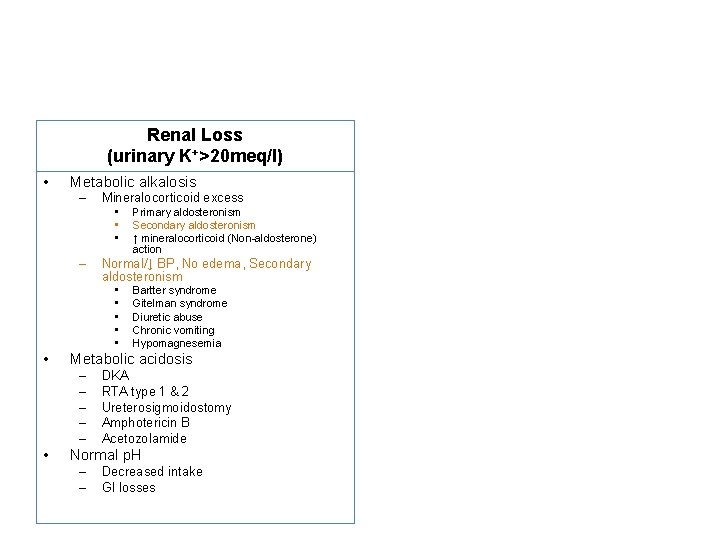
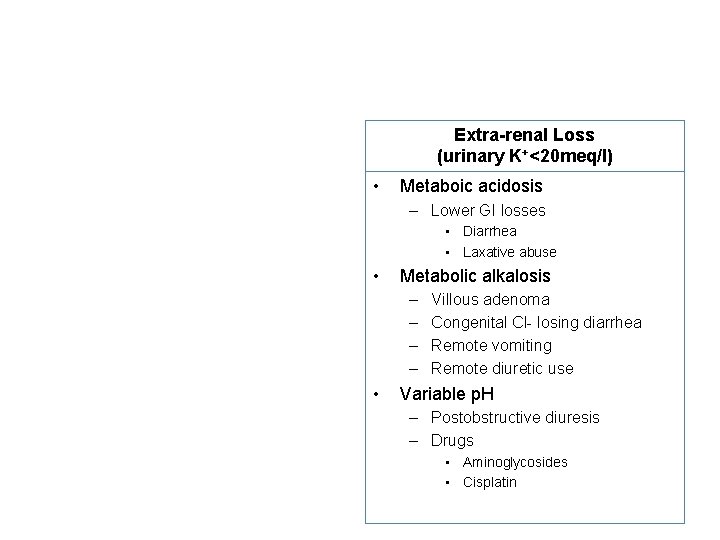
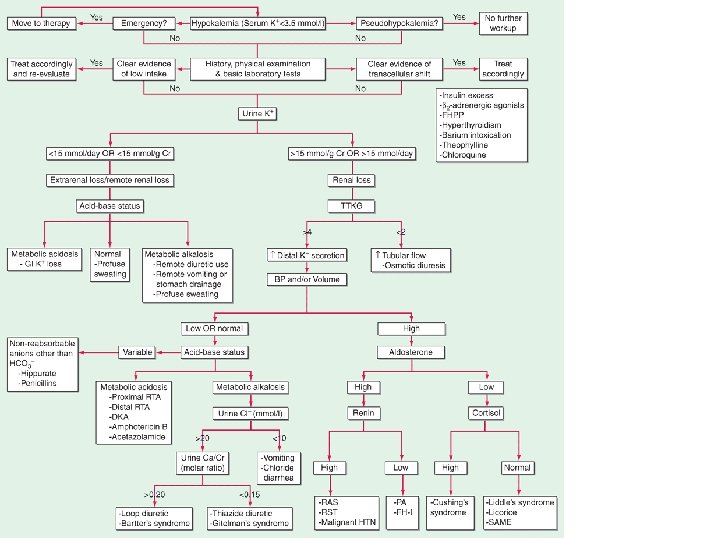
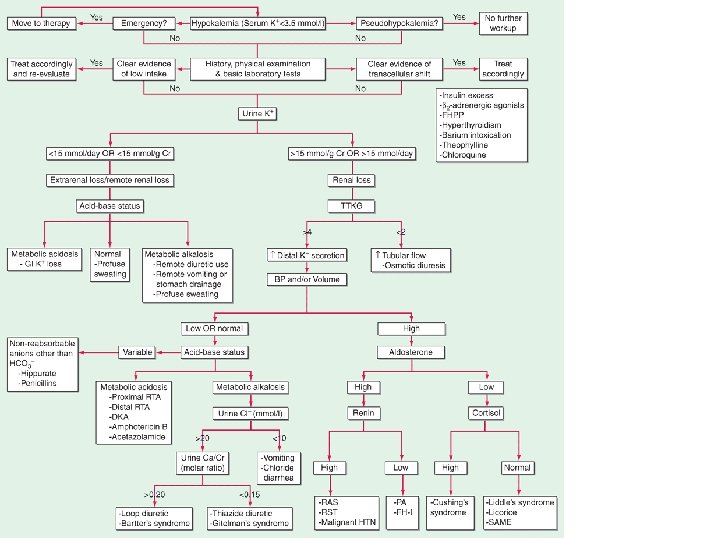
3. Decreased Total Body K+ Renal Loss (urinary K+>20 meq/l) • Metabolic alkalosis – Mineralocorticoid excess • Primary aldosteronism • Secondary aldosteronism • ↑ mineralocorticoid (Non-aldosterone) Extra-renal Loss (urinary K+<20 meq/l) • Metaboic acidosis – Lower GI losses • Diarrhea • Laxative abuse action – • • DKA RTA type 1 & 2 Ureterosigmoidostomy Amphotericin B Acetozolamide Normal p. H – – Decreased intake GI losses Metabolic alkalosis – – Metabolic acidosis – – – • Normal/↓ BP, No edema, Secondary aldosteronism • Bartter syndrome • Gitelman syndrome • Diuretic abuse • Chronic vomiting • Hypomagnesemia • Villous adenoma Congenital Cl- losing diarrhea Remote vomiting Remote diuretic use Variable p. H – Postobstructive diuresis – Drugs • Aminoglycosides • Cisplatin
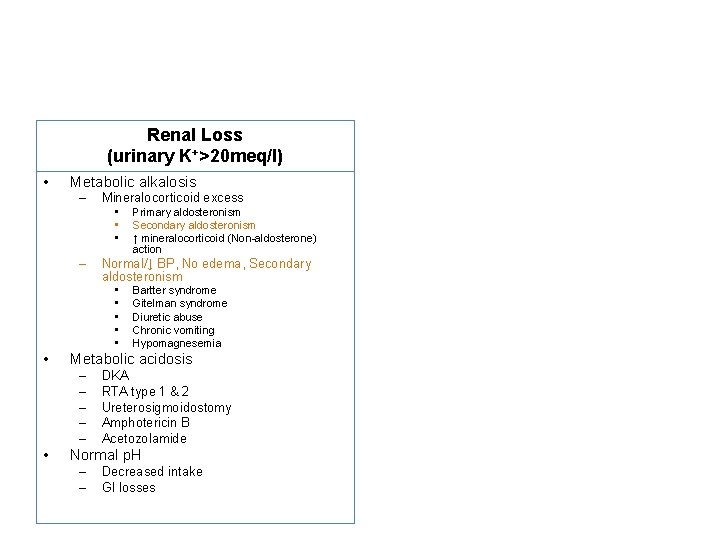
Renal Loss (urinary K+>20 meq/l) • Metabolic alkalosis – Mineralocorticoid excess • • • – Normal/↓ BP, No edema, Secondary aldosteronism • • • Bartter syndrome Gitelman syndrome Diuretic abuse Chronic vomiting Hypomagnesemia Metabolic acidosis – – – • Primary aldosteronism Secondary aldosteronism ↑ mineralocorticoid (Non-aldosterone) action DKA RTA type 1 & 2 Ureterosigmoidostomy Amphotericin B Acetozolamide Normal p. H – – Decreased intake GI losses
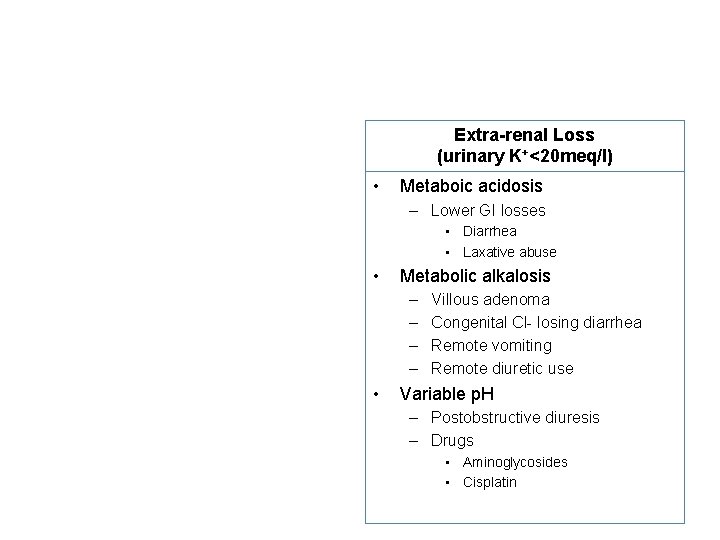
Extra-renal Loss (urinary K+<20 meq/l) • Metaboic acidosis – Lower GI losses • Diarrhea • Laxative abuse • Metabolic alkalosis – – • Villous adenoma Congenital Cl- losing diarrhea Remote vomiting Remote diuretic use Variable p. H – Postobstructive diuresis – Drugs • Aminoglycosides • Cisplatin
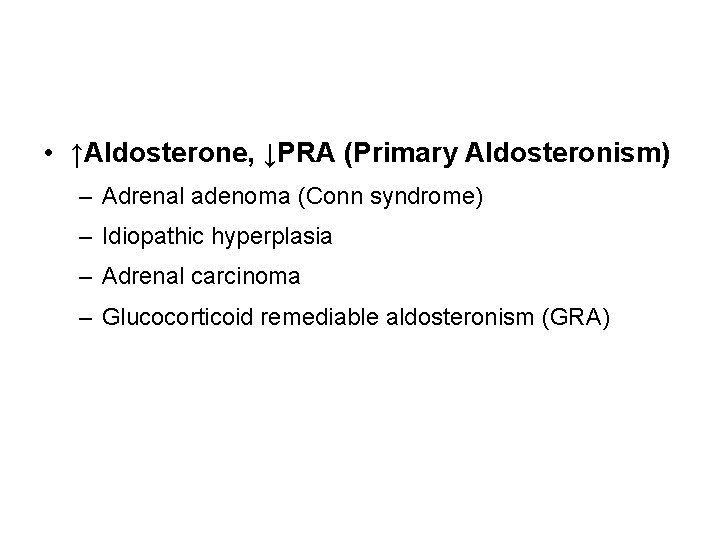
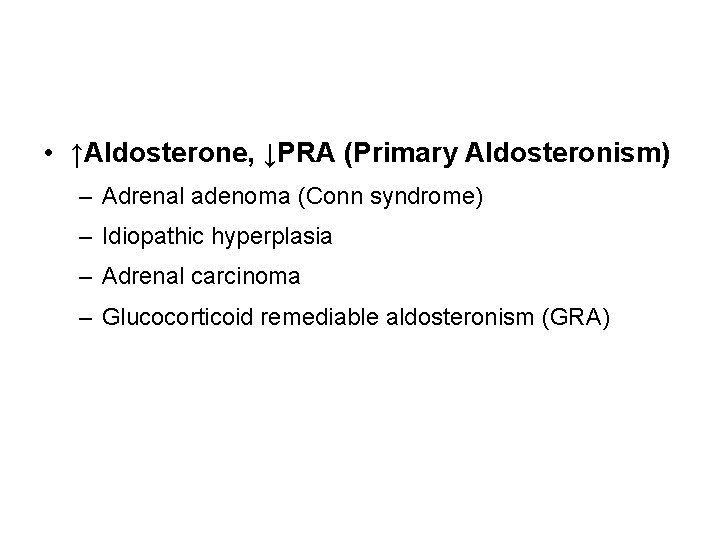
• ↑Aldosterone, ↓PRA (Primary Aldosteronism) – Adrenal adenoma (Conn syndrome) – Idiopathic hyperplasia – Adrenal carcinoma – Glucocorticoid remediable aldosteronism (GRA)
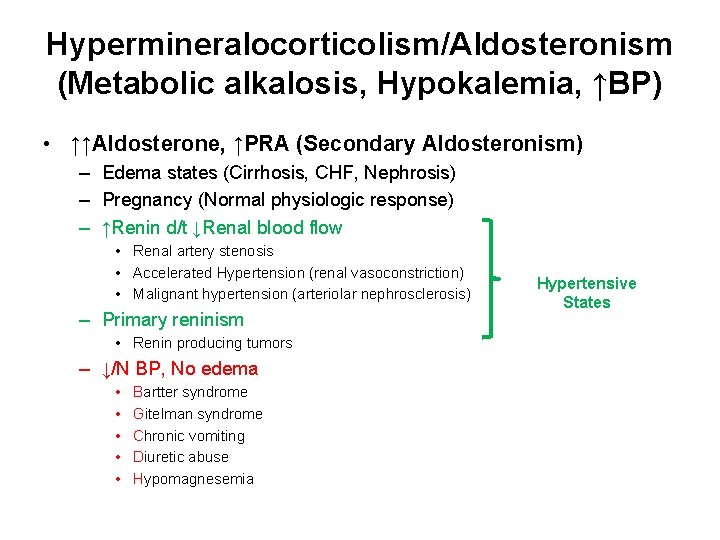
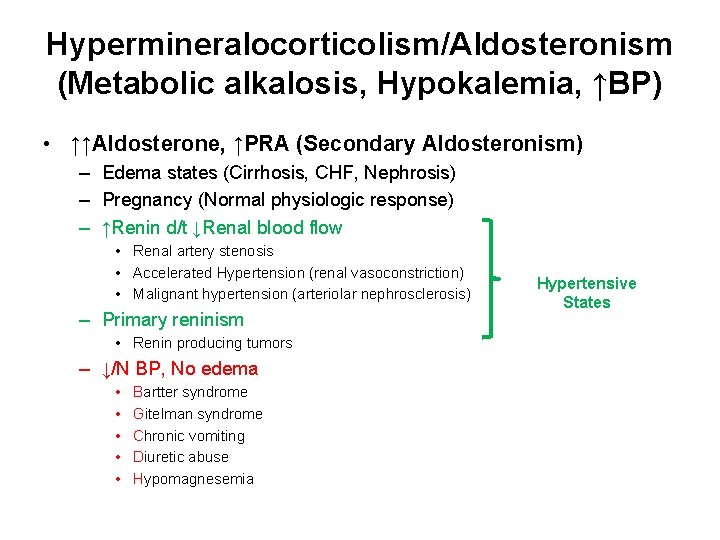
Hypermineralocorticolism/Aldosteronism (Metabolic alkalosis, Hypokalemia, ↑BP) • ↑↑Aldosterone, ↑PRA (Secondary Aldosteronism) – Edema states (Cirrhosis, CHF, Nephrosis) – Pregnancy (Normal physiologic response) – ↑Renin d/t ↓Renal blood flow • Renal artery stenosis • Accelerated Hypertension (renal vasoconstriction) • Malignant hypertension (arteriolar nephrosclerosis) – Primary reninism • Renin producing tumors – ↓/N BP, No edema • • • Bartter syndrome Gitelman syndrome Chronic vomiting Diuretic abuse Hypomagnesemia Hypertensive States
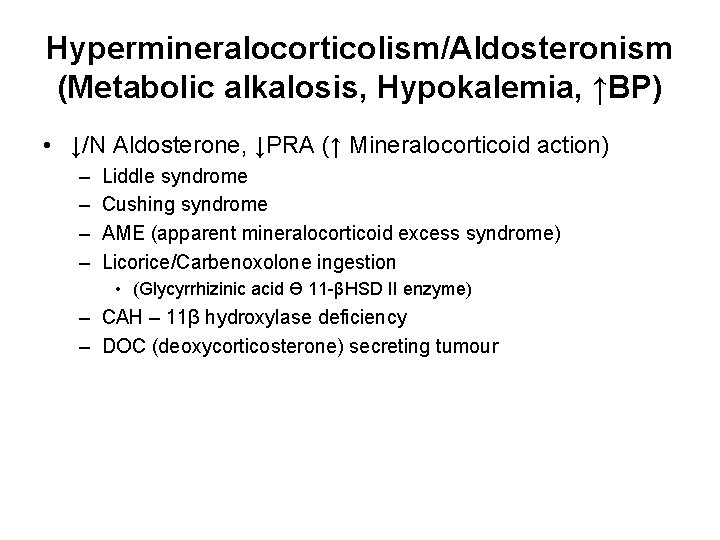
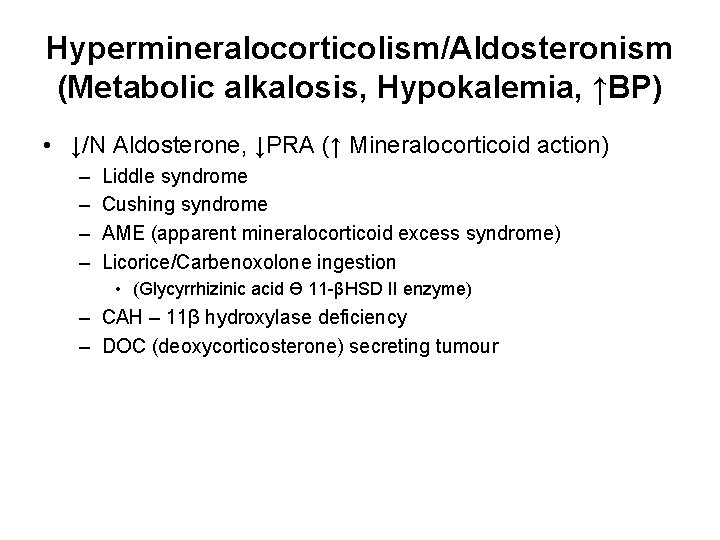
Hypermineralocorticolism/Aldosteronism (Metabolic alkalosis, Hypokalemia, ↑BP) • ↓/N Aldosterone, ↓PRA (↑ Mineralocorticoid action) – – Liddle syndrome Cushing syndrome AME (apparent mineralocorticoid excess syndrome) Licorice/Carbenoxolone ingestion • (Glycyrrhizinic acid Ɵ 11 -βHSD II enzyme) – CAH – 11β hydroxylase deficiency – DOC (deoxycorticosterone) secreting tumour
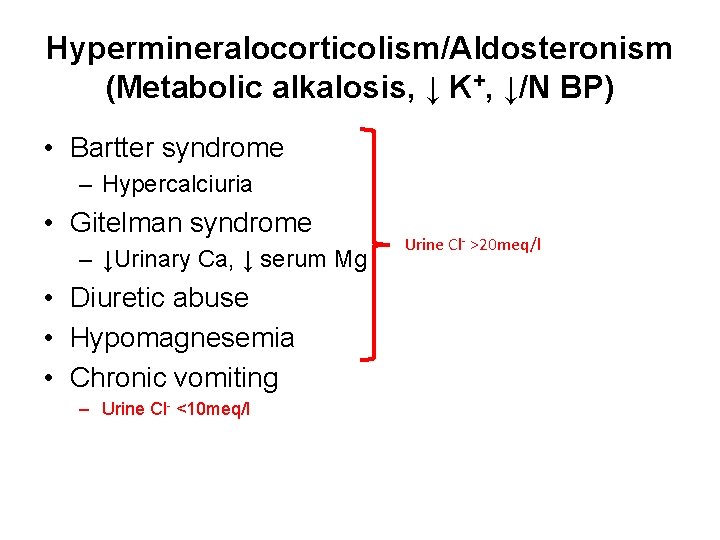
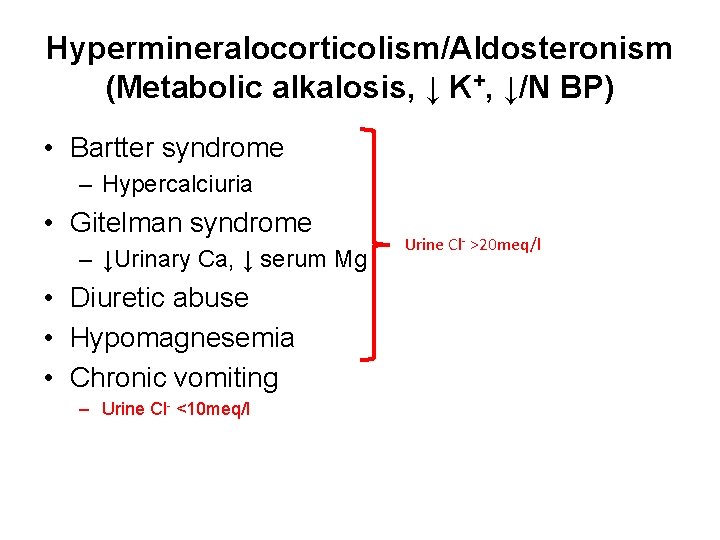
Hypermineralocorticolism/Aldosteronism (Metabolic alkalosis, ↓ K+, ↓/N BP) • Bartter syndrome – Hypercalciuria • Gitelman syndrome – ↓Urinary Ca, ↓ serum Mg • Diuretic abuse • Hypomagnesemia • Chronic vomiting – Urine Cl- <10 meq/l Urine Cl- >20 meq/l
CVS - ECG • Flattening or inversion of T wave with ST depression • Prominent U waves • Prolonged QT (QU) interval • + prolonged PR interval, wide QRS complex • Atrial and ventricular arrhythmias • Predisposition to digitalis toxicity
Clinical • Neuro. Ms – Weakness, flaccid paralysis – Cramps, tetany, rhabdomyolysis – Ileus, constipation, urinary retention • Endocrine – Glucose intolerance – Growth retardation, ↓ aldosterone • Renal – – ↓ renal blood flow, ↓ GFR Nephrogenic diabetes insipidus Increased ammoniagenesis (hepatic encephalopathy) Chloride wasting/metabolic alkalosis
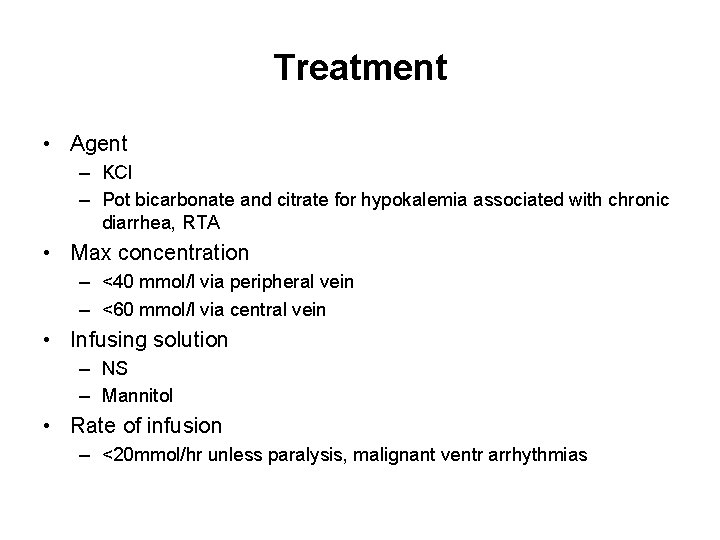
Treatment • Agent – KCl – Pot bicarbonate and citrate for hypokalemia associated with chronic diarrhea, RTA • Max concentration – <40 mmol/l via peripheral vein – <60 mmol/l via central vein • Infusing solution – NS – Mannitol • Rate of infusion – <20 mmol/hr unless paralysis, malignant ventr arrhythmias
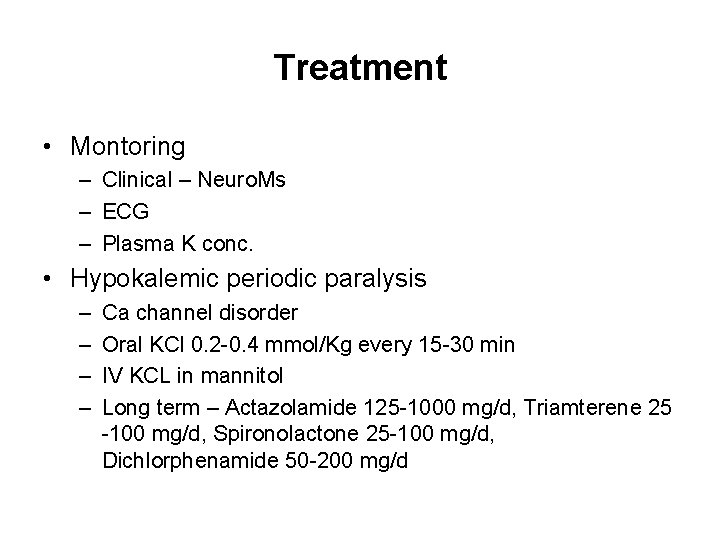
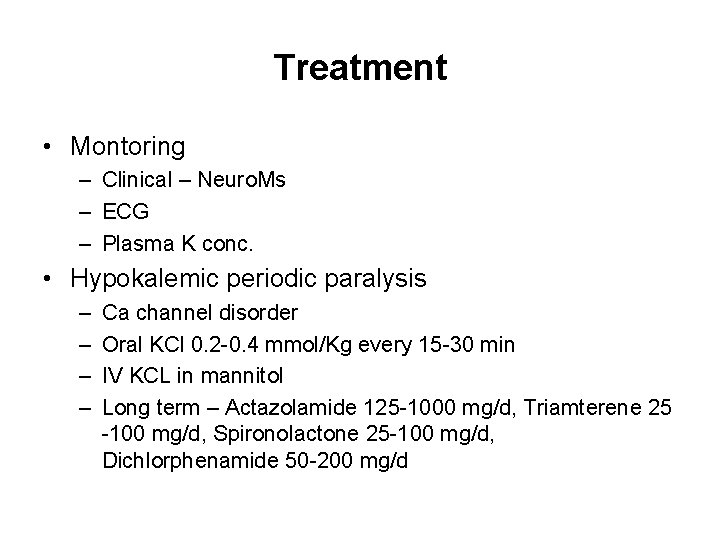
Treatment • Montoring – Clinical – Neuro. Ms – ECG – Plasma K conc. • Hypokalemic periodic paralysis – – Ca channel disorder Oral KCl 0. 2 -0. 4 mmol/Kg every 15 -30 min IV KCL in mannitol Long term – Actazolamide 125 -1000 mg/d, Triamterene 25 -100 mg/d, Spironolactone 25 -100 mg/d, Dichlorphenamide 50 -200 mg/d
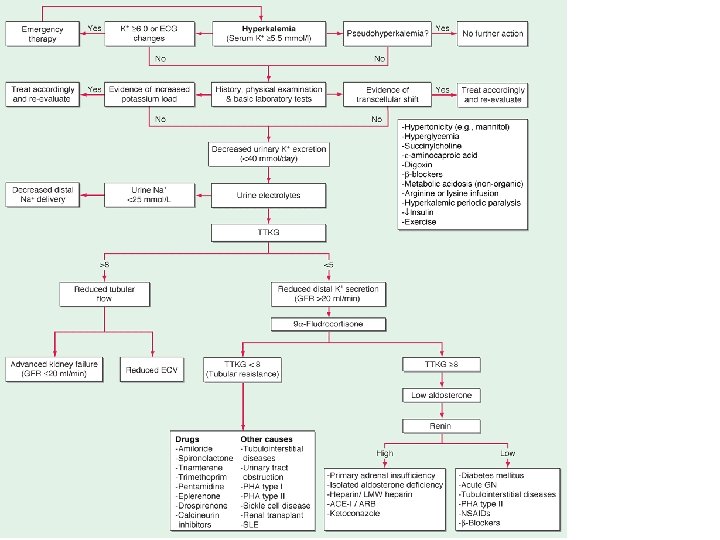
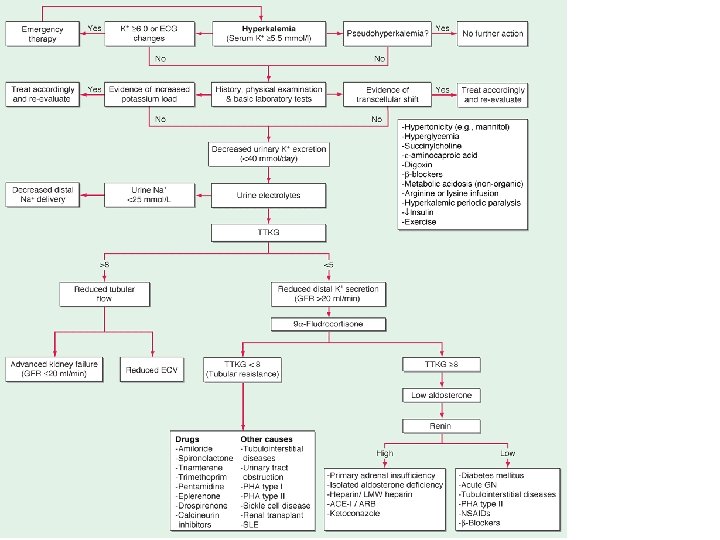
Hyperkalemia 1. Spurious (Pseudo) − Prolonged use of tourniquet − Ischemic blood draws − RBC hemolysis in test tubes − Marked thrombocytosis or leukocytosis
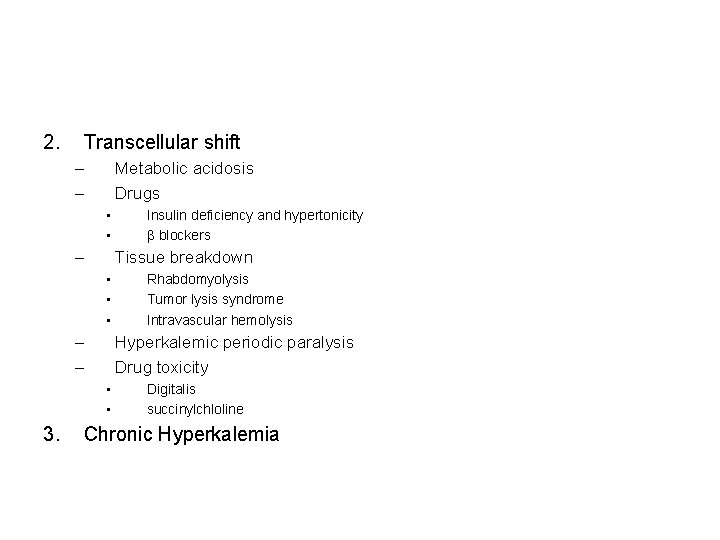
2. Transcellular shift – – Metabolic acidosis Drugs • • – Tissue breakdown • • • – – Rhabdomyolysis Tumor lysis syndrome Intravascular hemolysis Hyperkalemic periodic paralysis Drug toxicity • • 3. Insulin deficiency and hypertonicity β blockers Digitalis succinylchloline Chronic Hyperkalemia
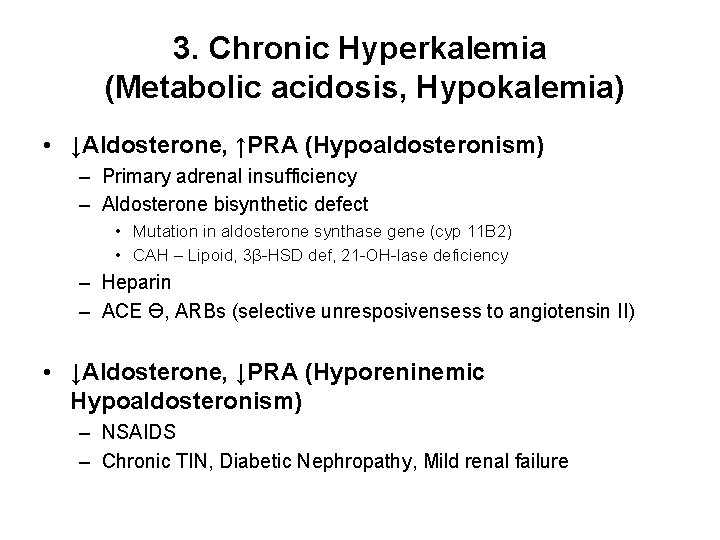
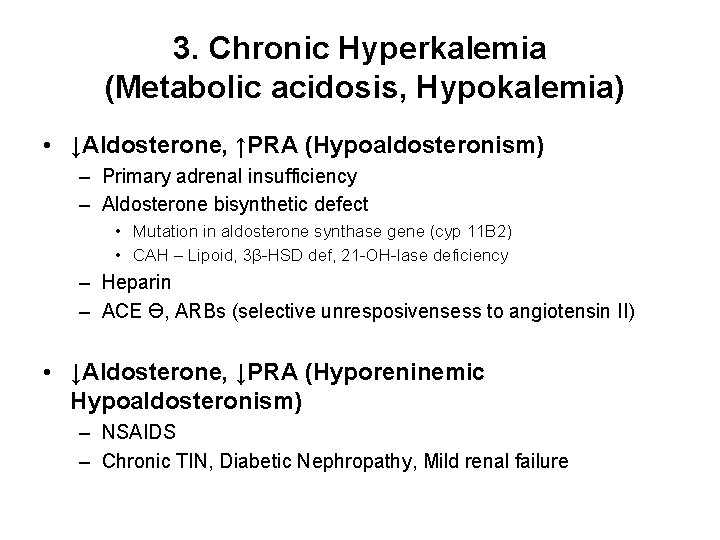
3. Chronic Hyperkalemia (Metabolic acidosis, Hypokalemia) • ↓Aldosterone, ↑PRA (Hypoaldosteronism) – Primary adrenal insufficiency – Aldosterone bisynthetic defect • Mutation in aldosterone synthase gene (cyp 11 B 2) • CAH – Lipoid, 3β-HSD def, 21 -OH-lase deficiency – Heparin – ACE Ɵ, ARBs (selective unresposivensess to angiotensin II) • ↓Aldosterone, ↓PRA (Hyporeninemic Hypoaldosteronism) – NSAIDS – Chronic TIN, Diabetic Nephropathy, Mild renal failure
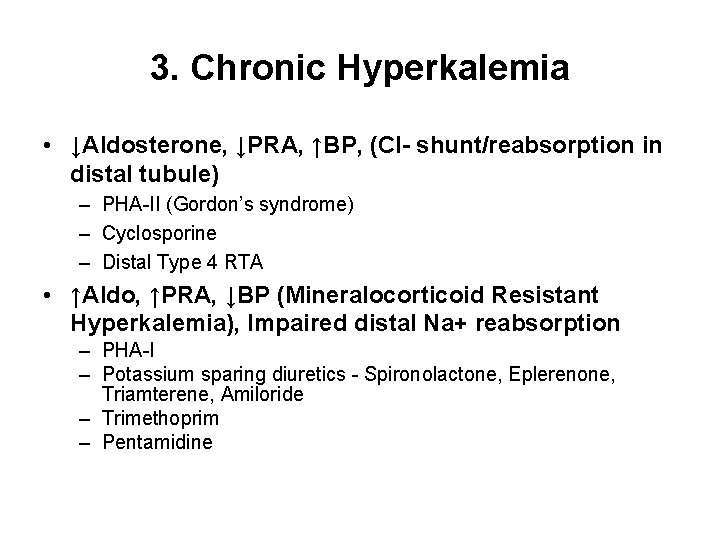
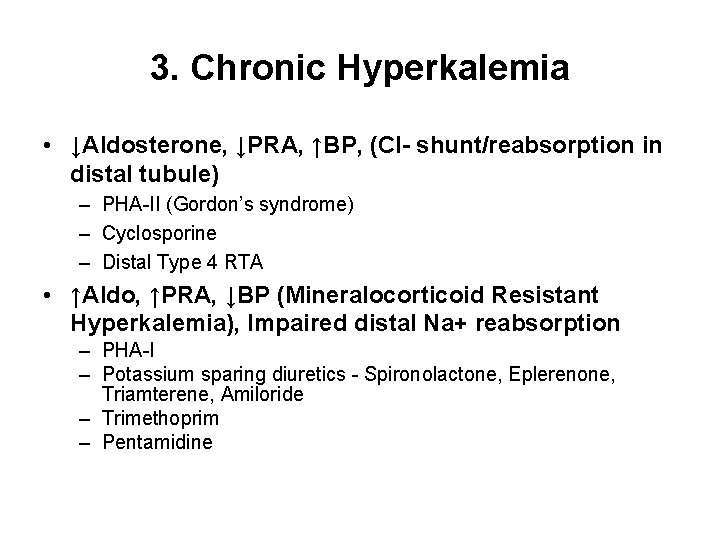
3. Chronic Hyperkalemia • ↓Aldosterone, ↓PRA, ↑BP, (Cl- shunt/reabsorption in distal tubule) – PHA-II (Gordon’s syndrome) – Cyclosporine – Distal Type 4 RTA • ↑Aldo, ↑PRA, ↓BP (Mineralocorticoid Resistant Hyperkalemia), Impaired distal Na+ reabsorption – PHA-I – Potassium sparing diuretics - Spironolactone, Eplerenone, Triamterene, Amiloride – Trimethoprim – Pentamidine
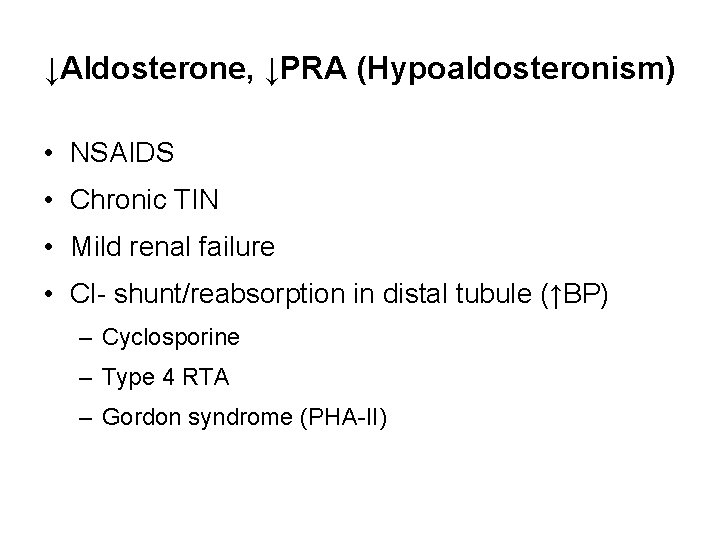
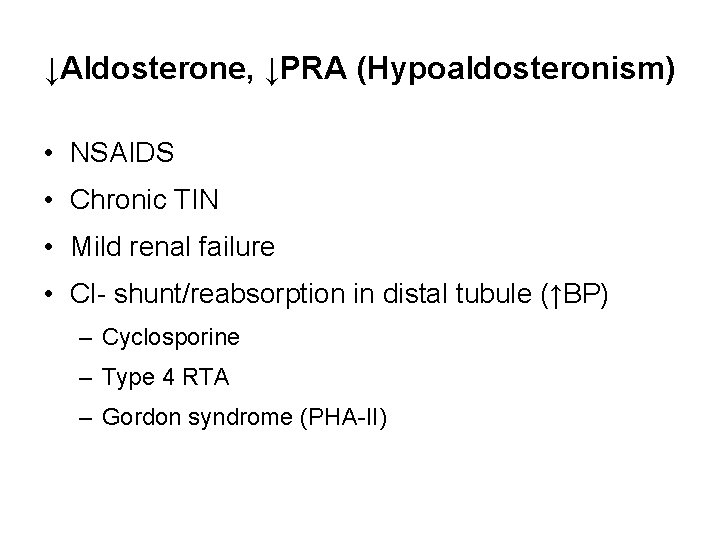
↓Aldosterone, ↓PRA (Hypoaldosteronism) • NSAIDS • Chronic TIN • Mild renal failure • Cl- shunt/reabsorption in distal tubule (↑BP) – Cyclosporine – Type 4 RTA – Gordon syndrome (PHA-II)
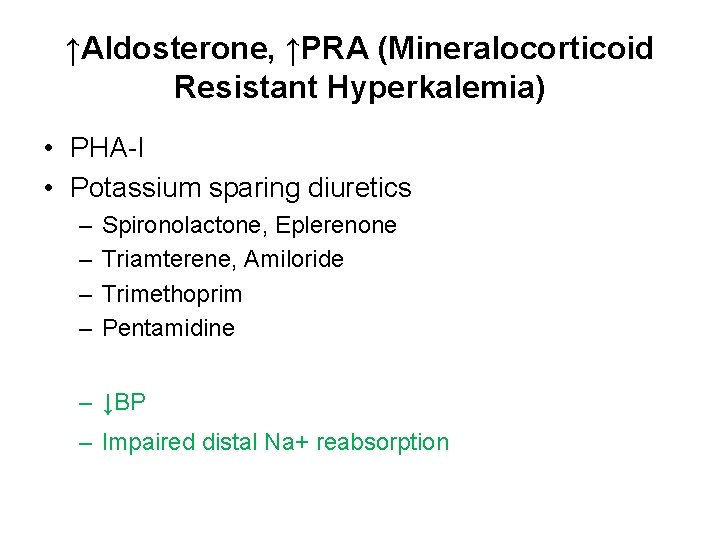
↑Aldosterone, ↑PRA (Mineralocorticoid Resistant Hyperkalemia) • PHA-I • Potassium sparing diuretics – – Spironolactone, Eplerenone Triamterene, Amiloride Trimethoprim Pentamidine – ↓BP – Impaired distal Na+ reabsorption
CVS - ECG • Tall peaked (tented) T waves (earliest change) • Short QT interval • Wide QRS, PR interval prolongs → 20 or 30 AV block • ↓ P wave amplitude → complete loss of P waves with associated junctional rhythm • QRS widens → sine wave (ventr. flutter-like) pattern • Eventual asystole
Treatment 1. Restrict K intake to <40 mmol/day 2. Stop K supplements 3. Stop K sparing diuretics
Treatment 1. Ca gluconate (10%) – 10 ml over 1 -3 min IV – Repeat if no change in ECG after 5 -10 min 2. 10 -20 U regular insulin + 25 -50 g glucose IVI 3. Na. HCO 3 3 amp (50 -150 mmol) in 1 L of 5%D 4. Nebulized β 2 agonist (albuterol 20 mg in 4 ml NS)
Treatment 5. Diuretics – furosemide 60 -80 mg/day 6. Resins (sodium polysterene sulfonate) – 25 -50 g in 100 ml of 20% sorbitol – Retention enema 50 g in 50 ml of 70% sorbitol in 150 ml tap water 7. Dialysis – For patients with renal failure – Severe life-threatening hyperkalemia unresponsive to conservative treatment – Hemodialysis – most rapid and effective way – Peritoneal dialysis – only 15 -20% as effective as hemodialysis
Thank You