Hypoglycaemia Dr Essam H Jiffri 1 INTRODUCTION Hypoglycaemia



- Slides: 23
Hypoglycaemia Dr. Essam H. Jiffri 1

INTRODUCTION -Hypoglycaemia is defined as a fasting venous whole-blood glucose level of less than 2. 2 mmol/L (plasma glucose <2. 5 mmo 1/l), when measured by a glucose-specific ( enzymatic) method. -Hypoglycaemia is dangerous because glucose is a vital primary fuel for the brain. 2
INTRODUCTION -Deficiency produces disordered function and, if prolonged or severe, can cause tissue damage or death. -In fasting, the brain still has an energy requirement equivalent to 80 g glucose 24/h, which cannot be provided by NEFA, the immediately available alternative fuel. -The brain can utilize ketone bodies but these are not produced rapidly enough to protect against acute hypoglycaemia. 3
Clinical Features -Symptoms fall into two main categories: -In early acute hypoglycaemia: include nervousness, weakness, headache, sweating, dizziness, tremor, tachycardia, palpitations, anxiety and hunger. ( 4
Clinical Features -Those caused by dysfunction of the central nervous system (neuroglycopaenia, ( include visual symptoms, headache, blunted mental, loss of motor function, confusion, abnormal behavior and loss of consciousness. 5
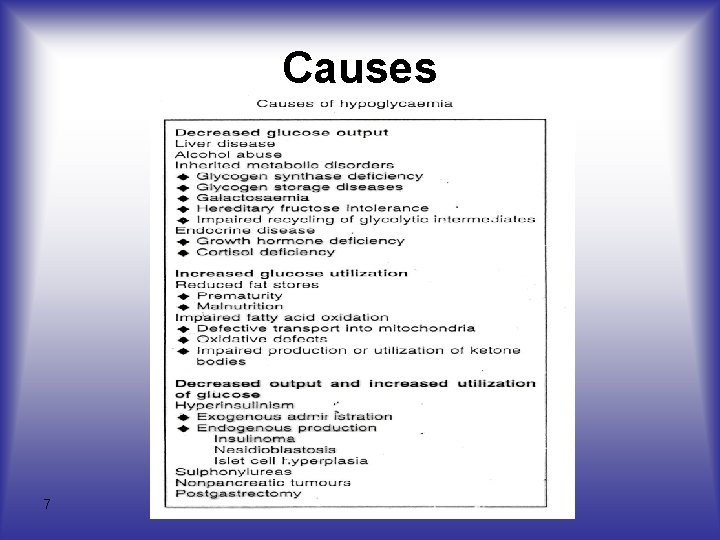
Causes -It has been traditional to classify hypoglycaemia as conditions that produce low blood glucose levels during fasting. -An alternative approach is based on the pathophysiology of hypoglycaemia, particularly reduced gluconeogenesis and increased utilization of glucose. 6
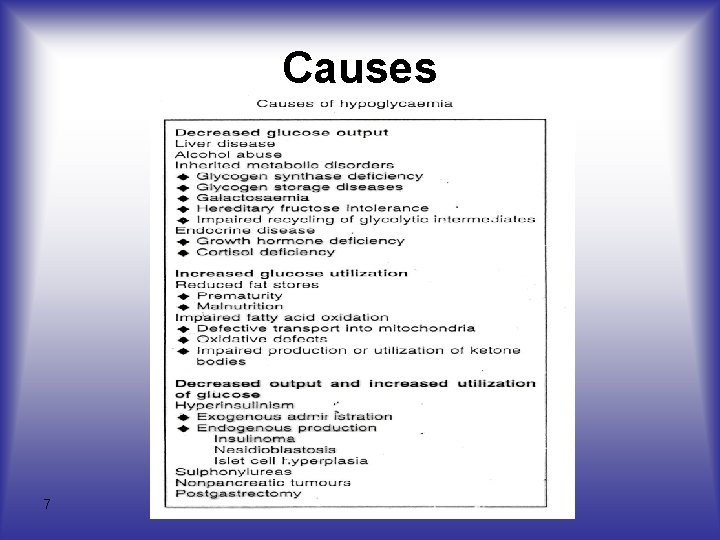
Causes 7
CAUSES I-Decreased Output of Glucose -Hypoglycaemia may result from impaired glycogenolysis or reduced gluconeogenesis. -Gluconeogenesis may be impaired because of reduced formation from amino acids and glycerol. 8
I-Decreased Output of Glucose • Liver Disease -Hypoglycaemia might be expected to be a complication of liver disease because of the role of this organ in gluconeogenesis • Alcohol Abuse -Alcohol inhibits gluconeogenesis following alcohol ingestion. 9
I-Decreased Output of Glucose • Inherited Metabolic Disorders - Endocrine Disease -Deficiency of counter-regulatory hormones is common cause of hypoglycaemia. -It occurs in cortisol deficiency, due either to: – primary adrenal failure or – secondary to adrenocorticotrophic hormone (ACTH) deficiency -In growth hormone deficiency. -Impaired gluconeogenesis is the most likely reason. 10
CAUSES 2 -lncreased Glucose Utilization • Reduced Fat Stores Low -Fat stores allow only limited ketogenesis and this may contribute to hypoglycaemia in premature infants and in malnutrition. 11

2 -lncreased Glucose Utilization • Decreased Ketone Body Production -Continued utilization of glucose by the brain cause hypoglycaemia when the production of ketone bodies is defective. 12
2 -lncreased Glucose Utilization • Impaired Fatty Acid Oxidation Activated -Long-chain fatty acids are transported by carnitine into mitochondria for oxidation, this being facilitated by two carnitine acyltransferases, deficiency or inactivity of one of these enzymes may cause impaired oxidation of long-chain fatty acids. 13
CAUSES 3 -Decreased Output and Increased Utilization of Glucose • Insulin -Insulin reduces blood glucose acutely, mainly by increasing cellular uptake and utilization; therefore excess administration causes hypoglycaemia. -Hyperinsulinaemia may also result from inappropriate endogenous production. 14
3 -Decreased Output and Increased Utilization of Glucose • Insulin -Insulinomas, which are common causes of hypoglycaemia in adults, are tumours of pancreatic beta cells. -Nesiodioblastosis is a diffuse increase in pancreatic endocrine cells and is an important cause of hypoglycaemia in infancy. 15
3 -Decreased Output and Increased Utilization of Glucose • Sulphonylureas - Sulphonylureas increase glucosestimulated insulin release and hypoglycaemia is the most commonly observed side-effect. 16
3 -Decreased Output and Increased Utilization of Glucose • Nonpancreatic Tumour - Some nonpancreatic tumours, particularly primary liver carcinomas, occasionally cause hypoglycaemia. 17
3 -Decreased Output and Increased Utilization of Glucose • Postgastrectomy - Hypoglycaemia is 2 h after a meal rich in carbohydrate is common in patients with a partial gastrectomy. - It occurs because of rapid passage of sugar into the small intestine and enhanced release of enteric hormones which augment glucosestimulated insulin release, this excess release of insulin causes hypoglycaemia. 18
Investigation of Hypoglycaemia in Adults -Once the diagnosis is considered blood glucose and insulin should be measured after an overnight fast: hypoglycaemia with inappropriately high insulin levels is being demonstrated by such a protocol in over 90% of cases of insulinoma. 19

Investigation of Hypoglycaemia in Adults - For some patients an extended fast of up to 72 h is needed, and glucose and insulin concentration should be determined every 4 -6 h, or when the patient has symptoms. - Hypoglycaemia due to non-islet cell tumours is usually very severe and tuomours may be detected by physical examination or imaging techniques. 20
Hypoglacaemia in Infancy and Childhood - Hypoglycaemia often occurs at birth, as normal blood control is established after a few days of birth. 21
Investigation of Hypoglacaemia in Infancy and Childhood - minimum investigations are: - blood glucose - serum insulin, and - blood or urinary ketone bodies. - It may be necessary to estimate: - Growth hormone - Cortisol - NEFA, and - Other intermediary metabolites 22
Hypoglacaemia in Infancy and Childhood - Most neonates with persistent hypoglycaemia have hyperinsulinism due to: -Deficiency of counter-regulatory hormone, or -An enzyme deficiency affecting gluconeogenisis or glycogenolysis. - In older children hyperinsulinism, growth hormone or cortisol deficiency are important cause. 23
 Dr. essam hamza
Dr. essam hamza Introduction paragraph structure
Introduction paragraph structure Yashpal committee report 2009
Yashpal committee report 2009 What is yacc
What is yacc What to write for a dare essay
What to write for a dare essay How to write a introduction to an essay
How to write a introduction to an essay Abstract vs introduction
Abstract vs introduction How long is an introduction
How long is an introduction Introduction in email
Introduction in email Bridge introduction paragraph
Bridge introduction paragraph Introduction answer the question
Introduction answer the question Informative essay example
Informative essay example Editorial introduction example
Editorial introduction example Disadvantages of essay writing
Disadvantages of essay writing Mla research proposal format
Mla research proposal format Daily diary writing examples
Daily diary writing examples Character analysis examples
Character analysis examples Jane schaffer introduction paragraph example
Jane schaffer introduction paragraph example Mesopotamian civilization conclusion
Mesopotamian civilization conclusion Work immersion expected behavior
Work immersion expected behavior Wireless communication introduction
Wireless communication introduction Band introduction speech
Band introduction speech Sales management introduction
Sales management introduction What is humor
What is humor