Hypoglycaemia and PrePregnancy Care Projects Dr Peter Winocour

- Slides: 23
Hypoglycaemia and Pre-Pregnancy Care Projects Dr Peter Winocour - Consultant Physician and Clinical Director for Diabetes and Endocrine Services Sarah Woodley - Clinical Nurse Educator Karen Moore-Haines - Project Manager East and North Herts Institute of Diabetes and Endocrinolgy (ENHIDE)
EAHSN Strategic goals: Innovative population based transformational models of delivery Using data to address unwarranted variations Using proven science methods and professional networks to deliver improvement in outcomes for major chronic diseases Engaging industry to deliver innovative interventions and systems Developing workforce capacity and capability
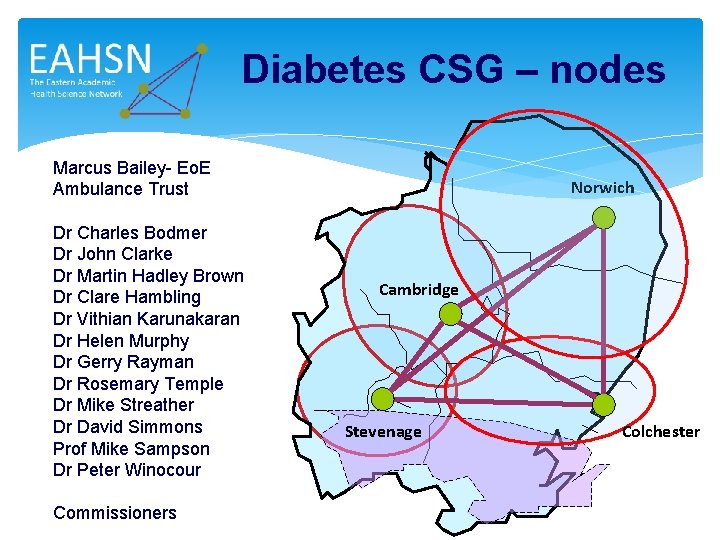
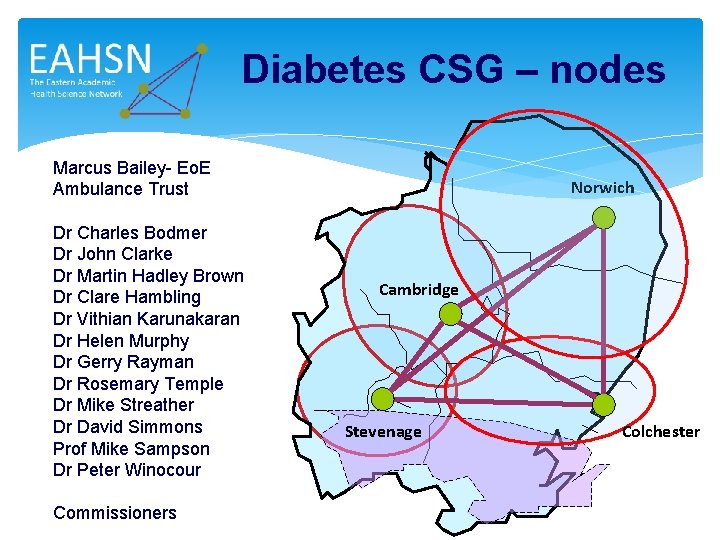
Diabetes CSG – nodes Marcus Bailey- Eo. E Ambulance Trust Dr Charles Bodmer Dr John Clarke Dr Martin Hadley Brown Dr Clare Hambling Dr Vithian Karunakaran Dr Helen Murphy Dr Gerry Rayman Dr Rosemary Temple Dr Mike Streather Dr David Simmons Prof Mike Sampson Dr Peter Winocour Commissioners Norwich Cambridge Stevenage Colchester
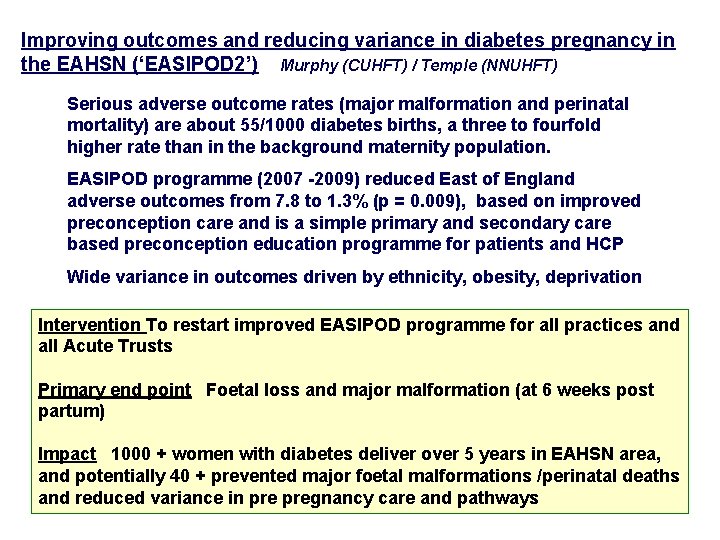
Improving outcomes and reducing variance in diabetes pregnancy in the EAHSN (‘EASIPOD 2’) Murphy (CUHFT) / Temple (NNUHFT) Serious adverse outcome rates (major malformation and perinatal mortality) are about 55/1000 diabetes births, a three to fourfold higher rate than in the background maternity population. EASIPOD programme (2007 -2009) reduced East of England adverse outcomes from 7. 8 to 1. 3% (p = 0. 009), based on improved preconception care and is a simple primary and secondary care based preconception education programme for patients and HCP Wide variance in outcomes driven by ethnicity, obesity, deprivation Intervention To restart improved EASIPOD programme for all practices and all Acute Trusts Primary end point Foetal loss and major malformation (at 6 weeks post partum) Impact 1000 + women with diabetes deliver over 5 years in EAHSN area, and potentially 40 + prevented major foetal malformations /perinatal deaths and reduced variance in pregnancy care and pathways
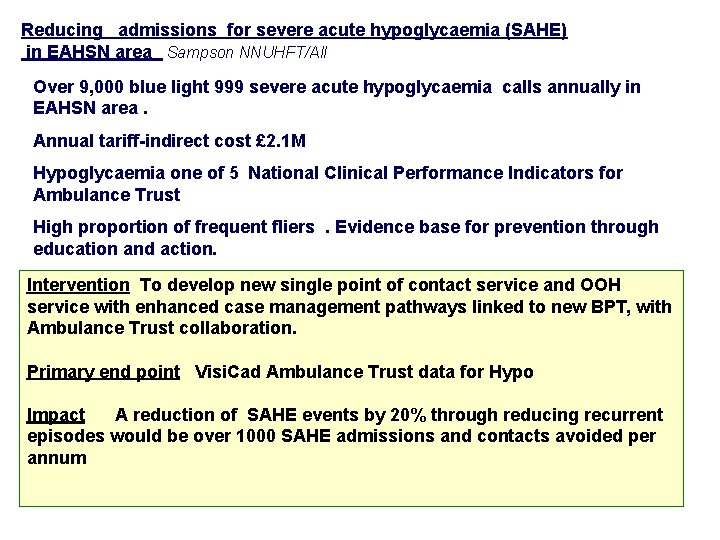
Reducing admissions for severe acute hypoglycaemia (SAHE) in EAHSN area Sampson NNUHFT/All Over 9, 000 blue light 999 severe acute hypoglycaemia calls annually in EAHSN area. Annual tariff-indirect cost £ 2. 1 M Hypoglycaemia one of 5 National Clinical Performance Indicators for Ambulance Trust High proportion of frequent fliers. Evidence base for prevention through education and action. 2 – 4 fold variance in EAHSN area for hospital conveyance admissions and Intervention To develop new single point of contact service, and OOH readmissions with hypoglycaemia service with enhanced case management pathways linked to new BPT, with Ambulance Trust collaboration. Primary end point Visi. Cad Ambulance Trust data for Hypo Impact A reduction of SAHE events by 20% through reducing recurrent episodes would be over 1000 SAHE admissions and contacts avoided per annum
Hypo Leaflet
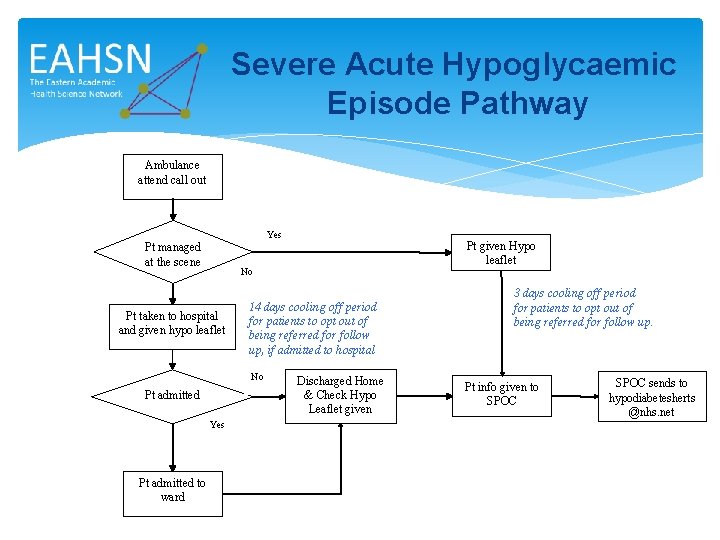
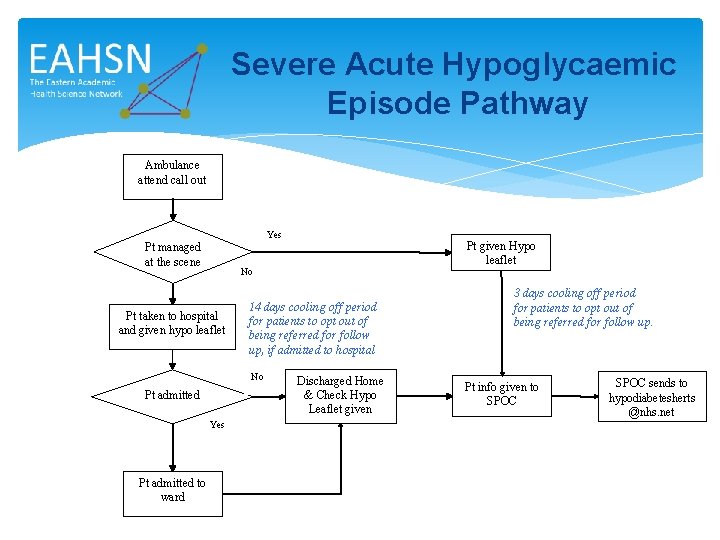
Severe Acute Hypoglycaemic Episode Pathway Ambulance attend call out Yes Pt managed at the scene No Pt taken to hospital and given hypo leaflet 14 days cooling off period for patients to opt out of being referred for follow up, if admitted to hospital No Pt admitted Yes Pt admitted to ward Pt given Hypo leaflet Discharged Home & Check Hypo Leaflet given 3 days cooling off period for patients to opt out of being referred for follow up. Pt info given to SPOC sends to hypodiabetesherts @nhs. net
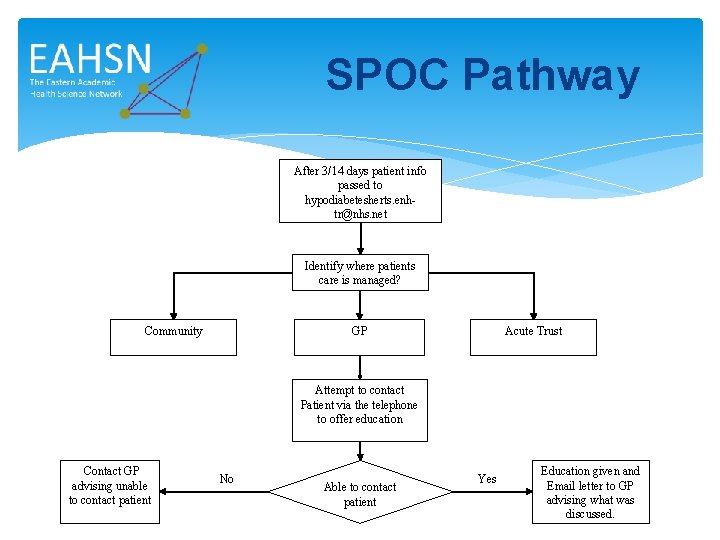
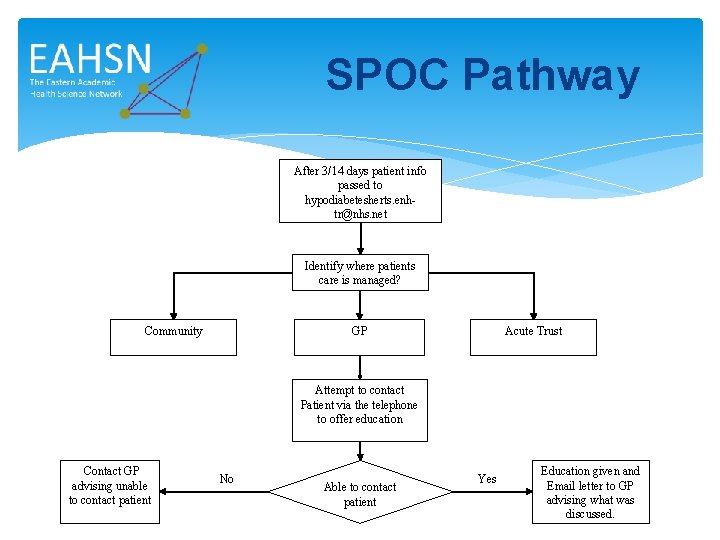
SPOC Pathway After 3/14 days patient info passed to hypodiabetesherts. enhtr@nhs. net Identify where patients care is managed? Community GP Acute Trust Attempt to contact Patient via the telephone to offer education Contact GP advising unable to contact patient No Able to contact patient Yes Education given and Email letter to GP advising what was discussed.
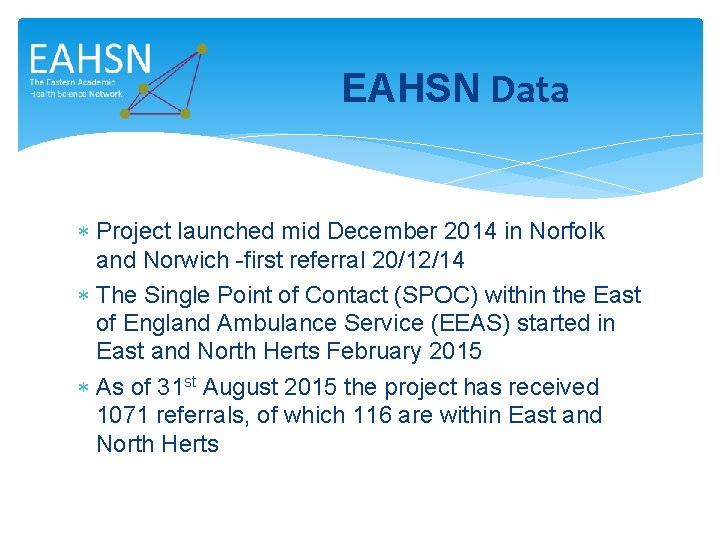
EAHSN Data Project launched mid December 2014 in Norfolk and Norwich -first referral 20/12/14 The Single Point of Contact (SPOC) within the East of England Ambulance Service (EEAS) started in East and North Herts February 2015 As of 31 st August 2015 the project has received 1071 referrals, of which 116 are within East and North Herts
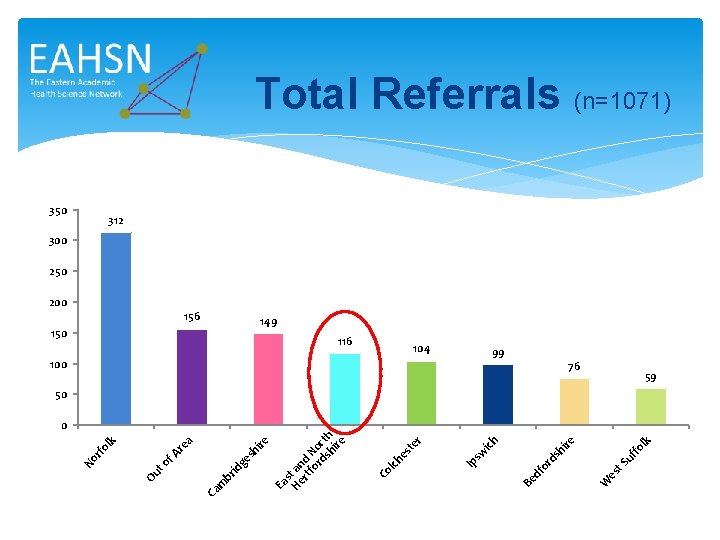
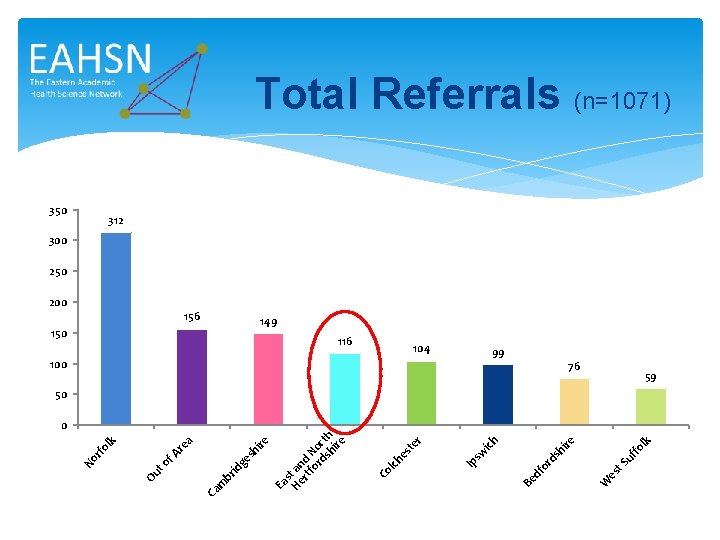
lk uf fo t. S es 99 W re hi ds 104 df or 100 Be ich sw 116 Ip r te es lch 150 Co 156 Ea s He t an rt d fo No rd rt sh h ire sh ge id br m 200 Ca a f. A re to k 350 Ou rf ol No Total Referrals (n=1071) 312 300 250 149 76 59 50 0
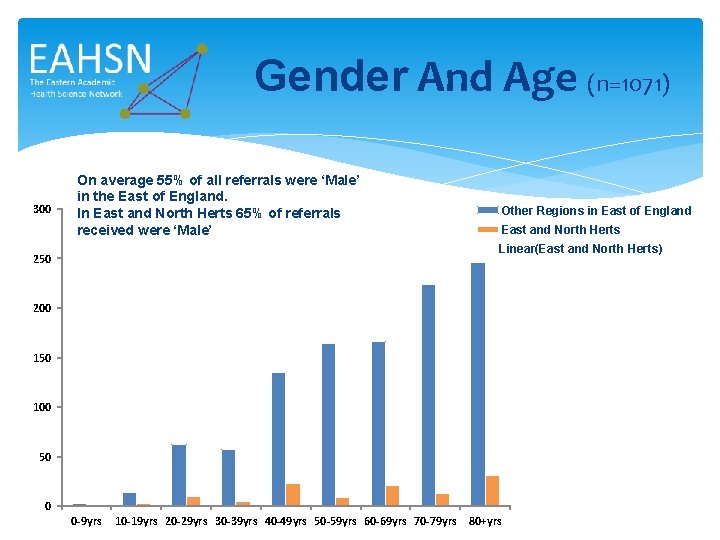
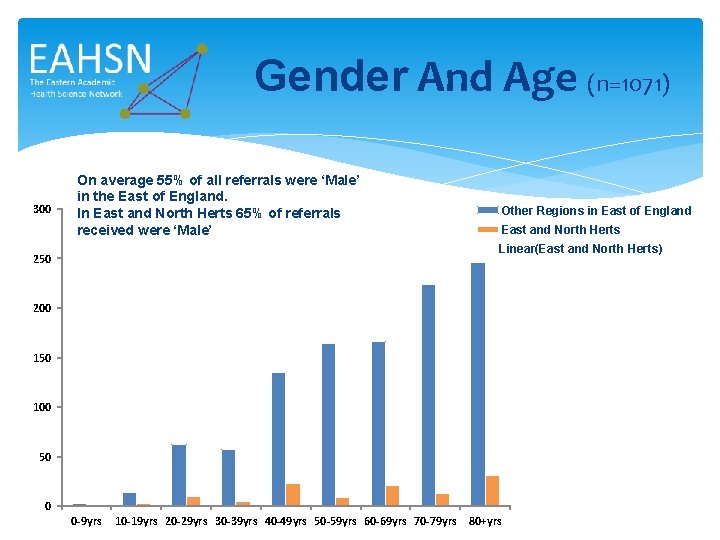
Gender And Age (n=1071) 300 On average 55% of all referrals were ‘Male’ in the East of England. In East and North Herts 65% of referrals received were ‘Male’ Other Regions in East of England East and North Herts Linear(East and North Herts) 250 200 150 100 50 0 0 -9 yrs 10 -19 yrs 20 -29 yrs 30 -39 yrs 40 -49 yrs 50 -59 yrs 60 -69 yrs 70 -79 yrs 80+yrs
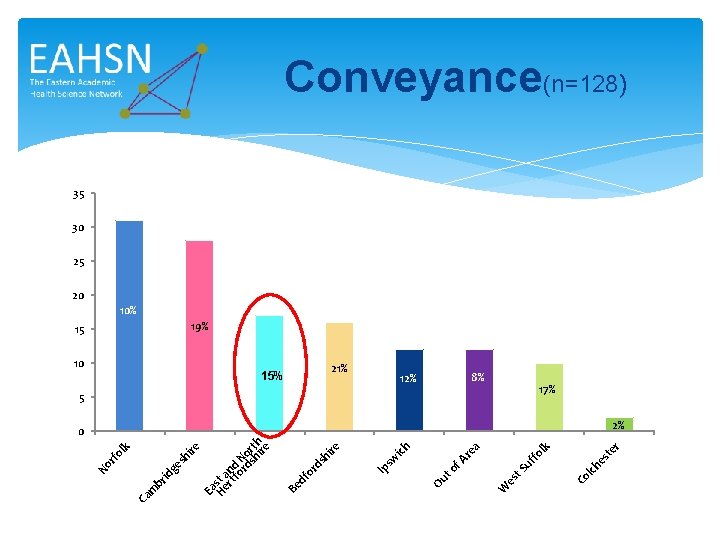
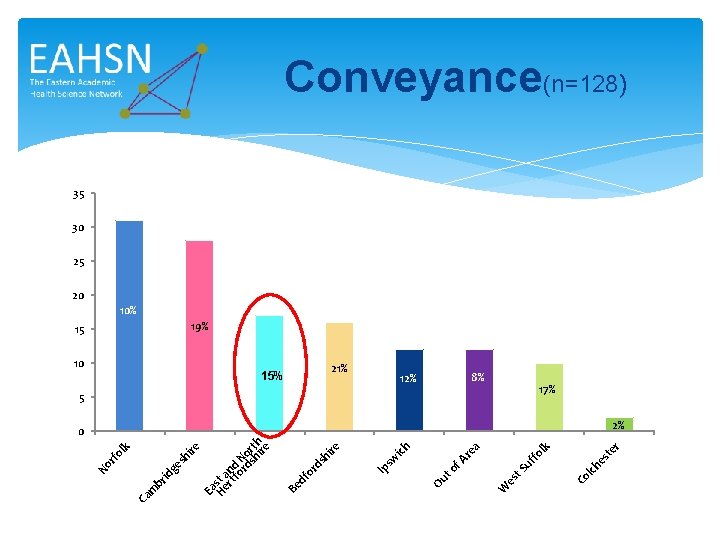
k r te es 5 lch 8% Co lk uf fo t. S es 12% W a f. A re to 21% Ou ich sw 15% Ip re hi ds df or 10 Be 15 Ea Hest a rt nd fo N rd o sh rth ire sh ge id br m Ca rf ol No Conveyance(n=128) 35 30 25 20 10% 19% 17% 0 2%
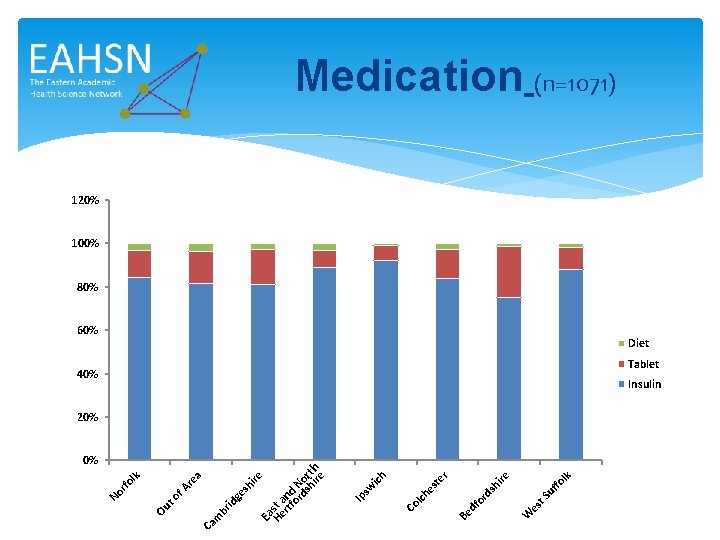
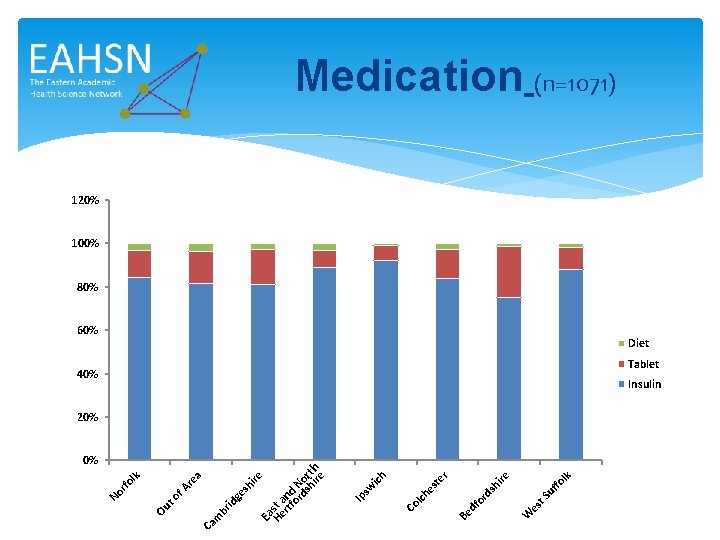
sh ge br id a re to f. A lk fo t. S uf ire sh or d W es df Be r ich es te Co lch Ip sw ire Ea He st a rtf nd or N ds or hi th re Ca m Ou lk No rfo Medication (n=1071) 120% 100% 80% 60% Diet 40% Tablet Insulin 20% 0%
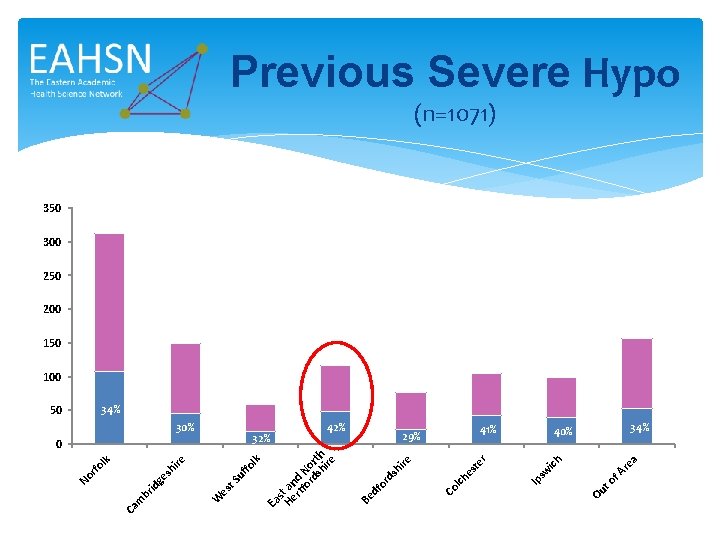
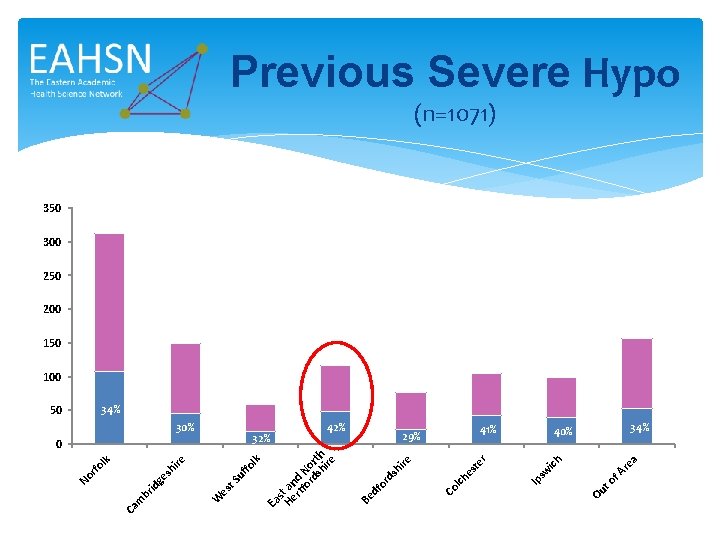
lk fo t. S uf es a re to f. A 41% Ou ich 29% Ip sw r es te ire sh or d 42% Co lch df 0 32% Be 30% Ea s He t an rtf d or No ds rt hi h re W re sh i ge id br Ca m lk 50 No rfo Previous Severe Hypo (n=1071) 350 300 250 200 150 100 34% 40% 34%
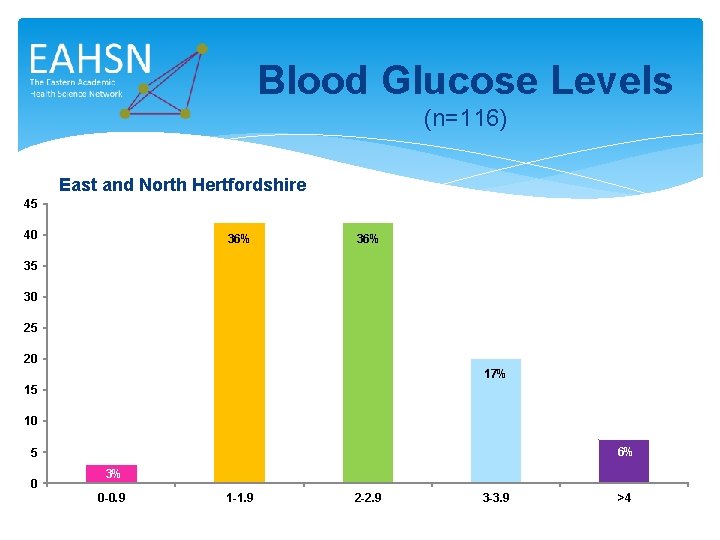
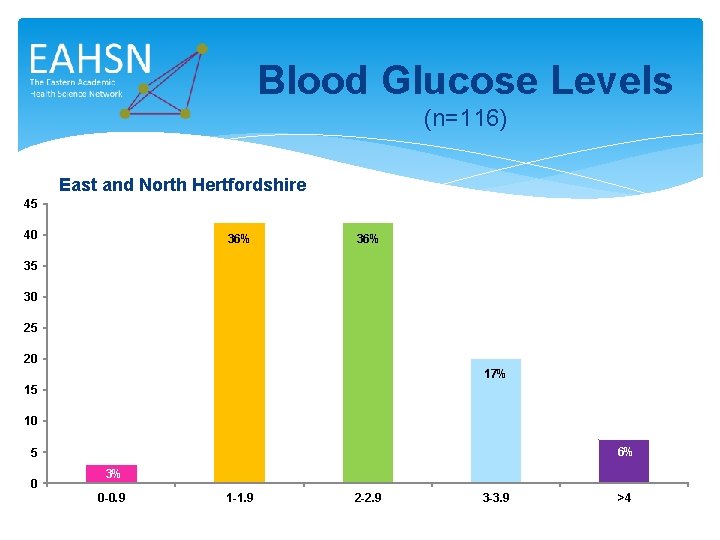
Blood Glucose Levels (n=116) East and North Hertfordshire 45 40 36% 35 30 25 20 17% 15 10 6% 5 0 3% 0 -0. 9 1 -1. 9 2 -2. 9 3 -3. 9 >4
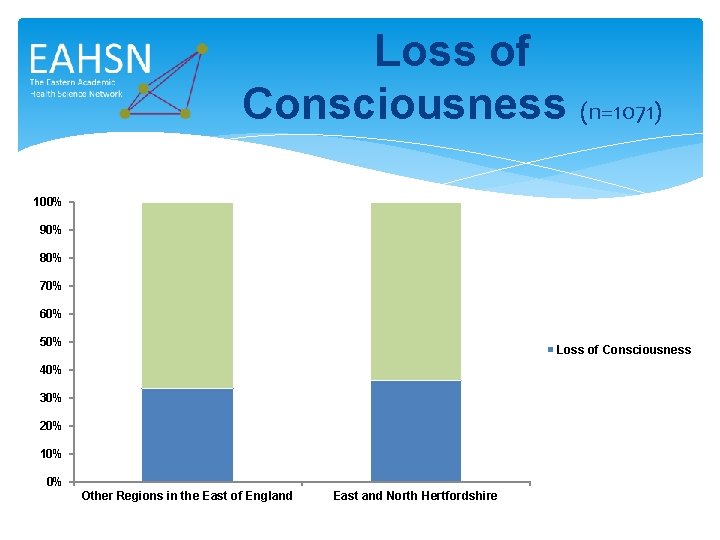
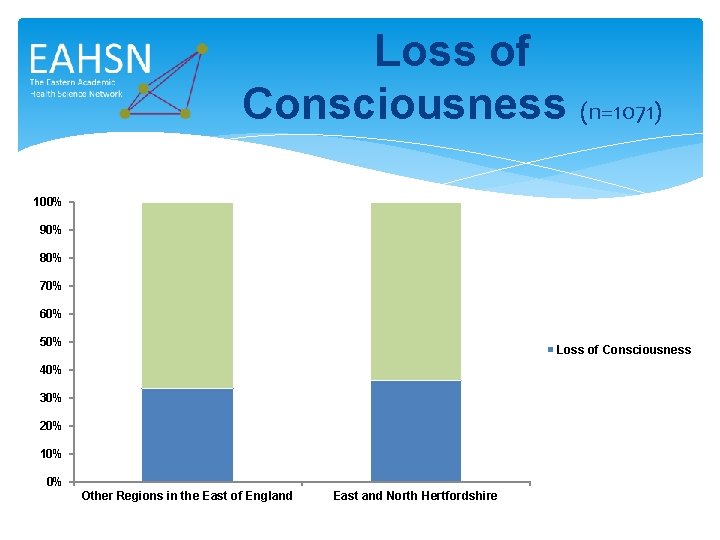
Loss of Consciousness (n=1071) 100% 90% 80% 70% 60% 50% Loss of Consciousness 40% 30% 20% 10% 0% Other Regions in the East of England East and North Hertfordshire
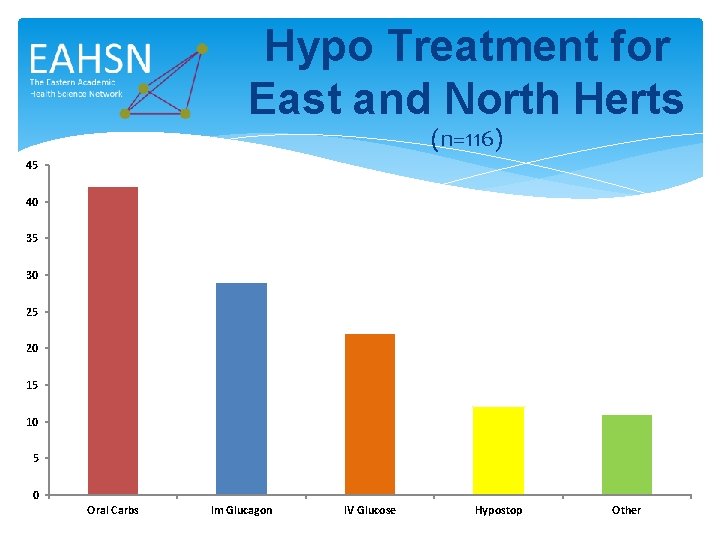
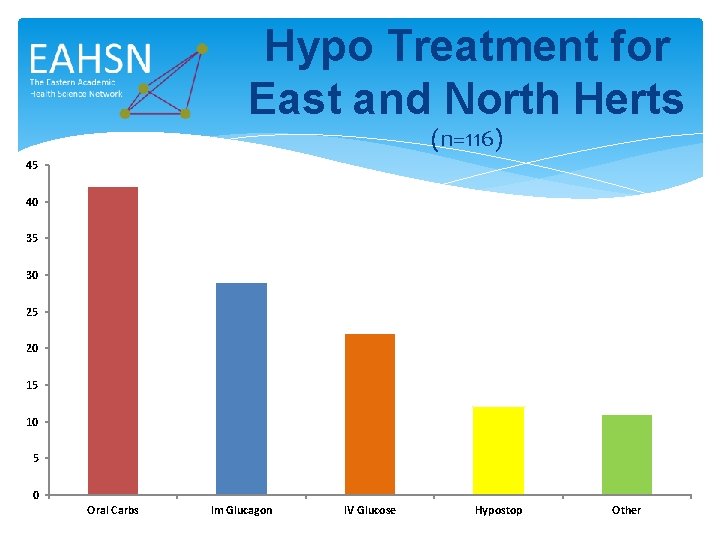
Hypo Treatment for East and North Herts (n=116) 45 40 35 30 25 20 15 10 5 0 Oral Carbs Im Glucagon IV Glucose Hypostop Other
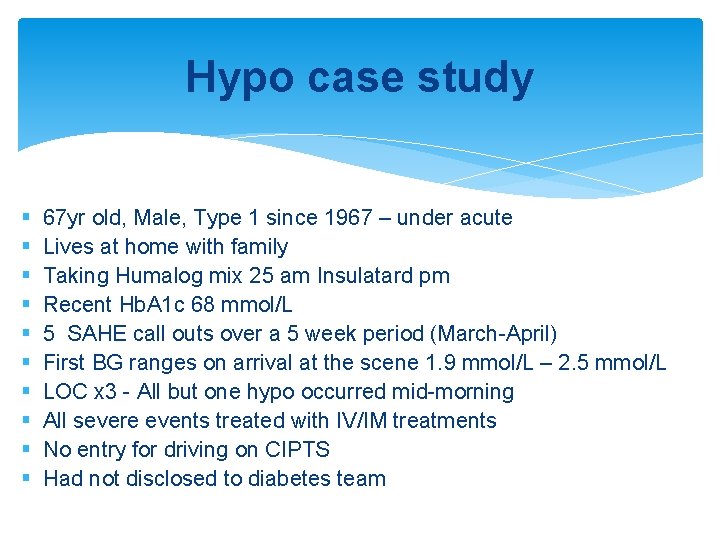
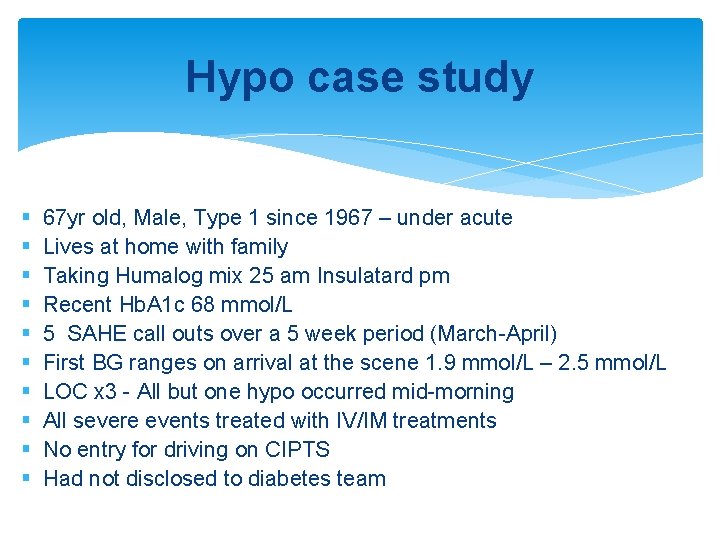
Hypo case study § § § § § 67 yr old, Male, Type 1 since 1967 – under acute Lives at home with family Taking Humalog mix 25 am Insulatard pm Recent Hb. A 1 c 68 mmol/L 5 SAHE call outs over a 5 week period (March-April) First BG ranges on arrival at the scene 1. 9 mmol/L – 2. 5 mmol/L LOC x 3 - All but one hypo occurred mid-morning All severe events treated with IV/IM treatments No entry for driving on CIPTS Had not disclosed to diabetes team
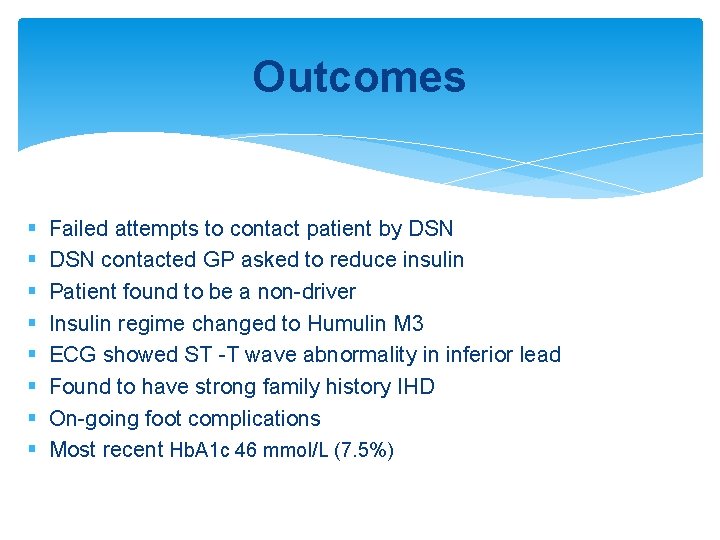
Outcomes § § § § Failed attempts to contact patient by DSN contacted GP asked to reduce insulin Patient found to be a non-driver Insulin regime changed to Humulin M 3 ECG showed ST -T wave abnormality in inferior lead Found to have strong family history IHD On-going foot complications Most recent Hb. A 1 c 46 mmol/L (7. 5%)
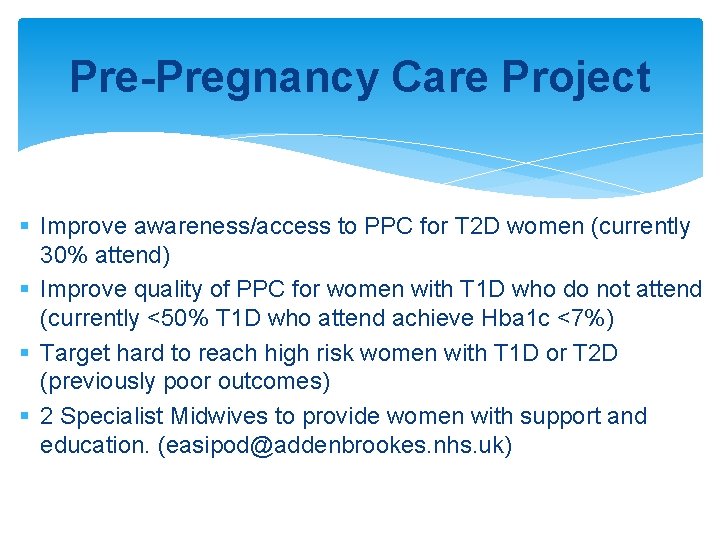
Pre-Pregnancy Care Project § Improve awareness/access to PPC for T 2 D women (currently 30% attend) § Improve quality of PPC for women with T 1 D who do not attend (currently <50% T 1 D who attend achieve Hba 1 c <7%) § Target hard to reach high risk women with T 1 D or T 2 D (previously poor outcomes) § 2 Specialist Midwives to provide women with support and education. (easipod@addenbrookes. nhs. uk)
Pre-Pregnancy Care Project Steps taken so far… § Contacted Practices in East and North Herts to ask to send a PPC leaflet out to women aged between 16 -45 yrs (short exclusion list) § In total 2118 PPC Leaflets have to sent out by GP practices in the East of England § Visited all Tesco, Sainsbury and Asda Pharmacies Superstores in area to hand out PPC leaflet with medication § Visited a number of Health Centres/Childrens Centres to display leaflets as various clinics
CDEP – What is it and who for? Please contact us for your CDEP Registration code Karen. moore-haines@nhs. net S. woodley@nhs. net

Any Questions?