Hyperthyroidism Hypothyroidism Dr Megangela Christi Amores Thyroid Hormones
- Slides: 23
Hyperthyroidism Hypothyroidism Dr. Meg-angela Christi Amores
Thyroid Hormones • Thyroxine (T 4) • Triiodothyronine (T 3) • Secreted by the THYROID G: AMD • Regulated by the PITUITARY GLAND • TSH – secreted by the PITUITARY GLAND
Normal levels • T 4 = • T 3 = • TSH • T 4 and T 3 greater than normal: HYPERTHYROIDISM • T 4 and T 3 lesser than normal: HYPOTHYROIDISM
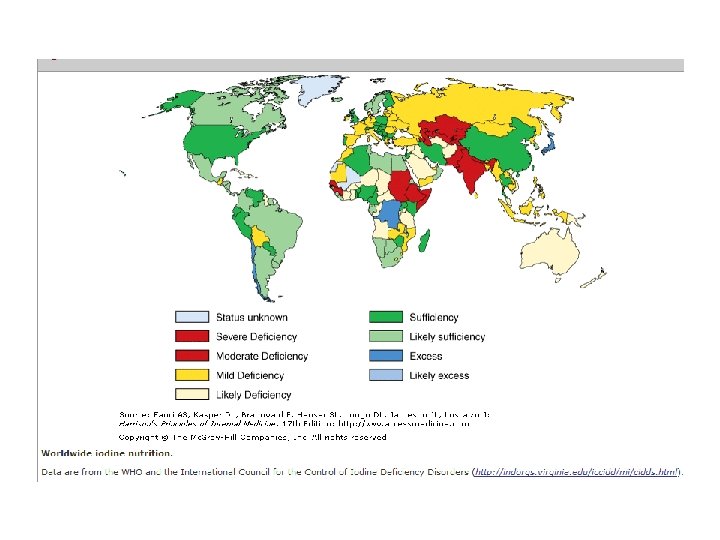
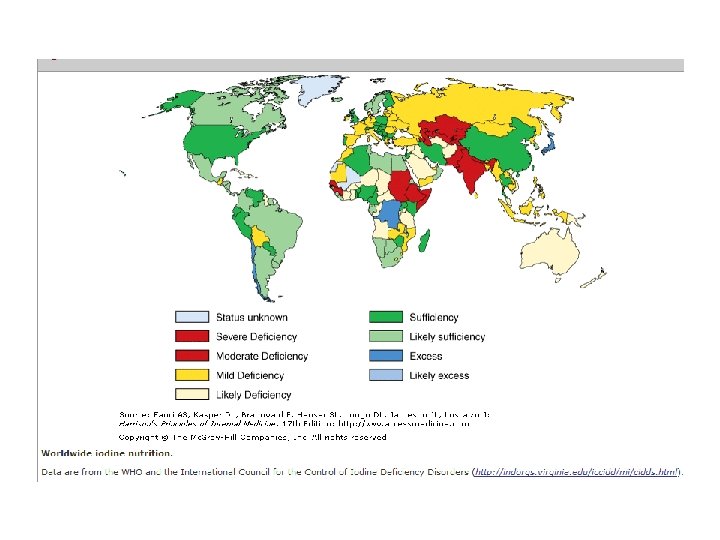
Thyroid Hormone Synthesis • Iodide uptake is a critical first step in thyroid hormone synthesis • In areas of relative iodine deficiency, there is an increased prevalence of goiter • iodine deficiency remains the most common cause of preventable mental deficiency
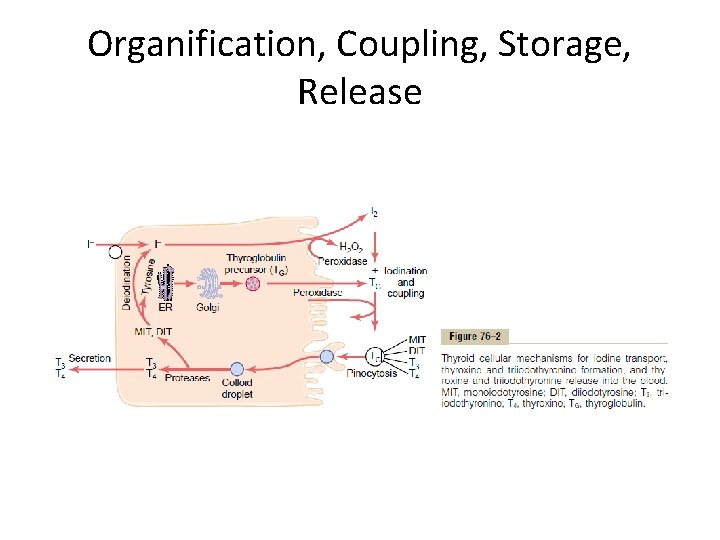
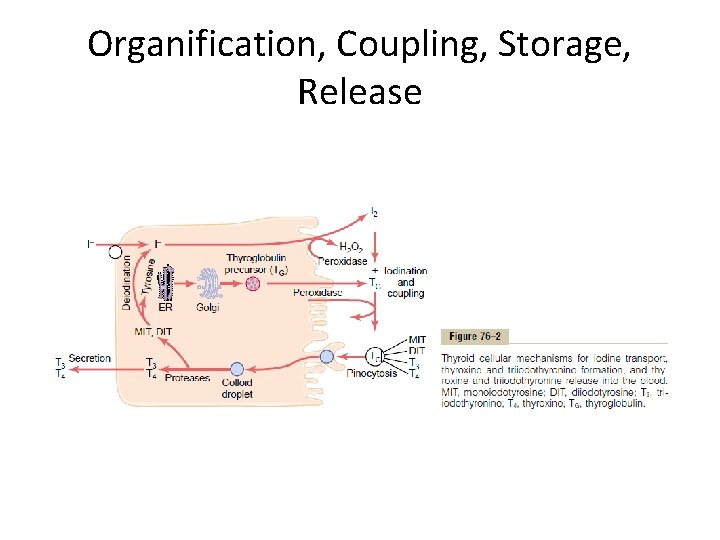
Organification, Coupling, Storage, Release
Hypothyroidism • Iodine deficiency remains the most common cause of hypothyroidism worldwide • In areas of iodine sufficiency, autoimmune disease (Hashimoto's thyroiditis) and iatrogenic causes (treatment of hyperthyroidism) are most common
Congenital Hypothyroidism • occurs in about 1 in 4000 newborns • due to thyroid gland dysgenesis in 80– 85% • due to inborn errors of thyroid hormone synthesis in 10– 15% • TSH-R antibody-mediated in 5% of affected newborns
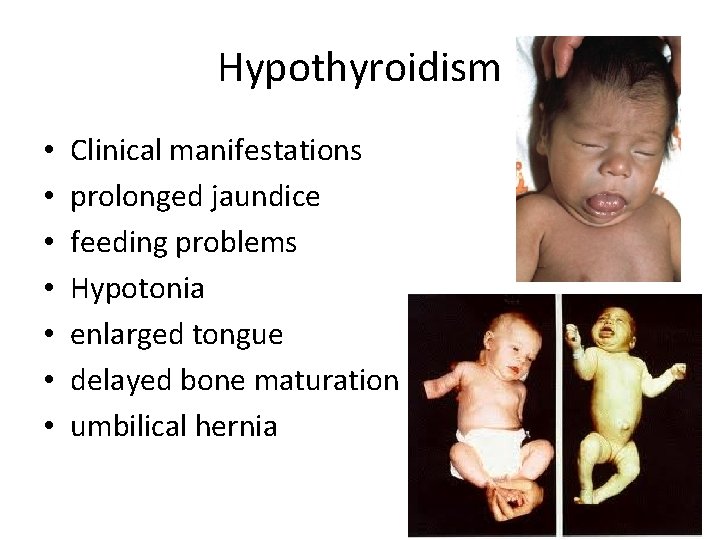
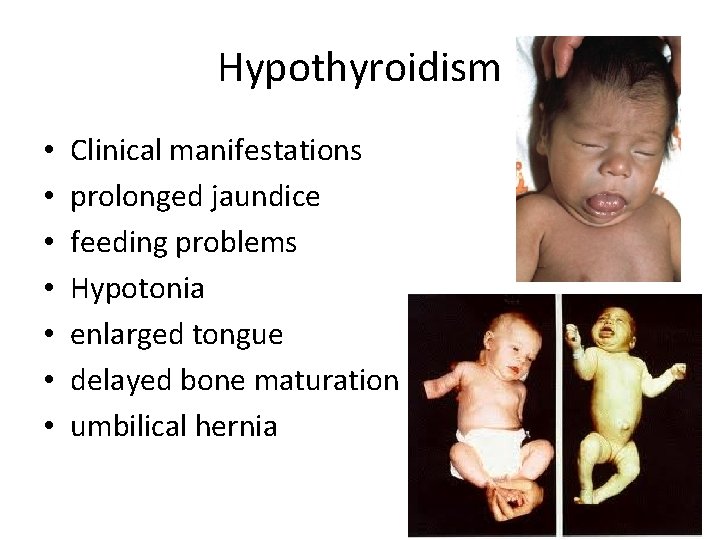
Hypothyroidism • • Clinical manifestations prolonged jaundice feeding problems Hypotonia enlarged tongue delayed bone maturation umbilical hernia
Diagnosis and Treatment • Diagnosis – neonatal screening programs – based on measurement of TSH or T 4 levels in heelprick blood specimens • Treatment – T 4 is instituted at a dose of 10– 15 g/kg per day, and the dose is adjusted by close monitoring of TSH levels. T 4 requirements are relatively great during the first year of life – Early treatment with T 4 results in normal IQ levels
Autoimmune Hypothyroidism • may be associated with a goiter (Hashimoto's, or goitrous thyroiditis) • or, at the later stages of the disease, minimal residual thyroid tissue (atrophic thyroiditis)
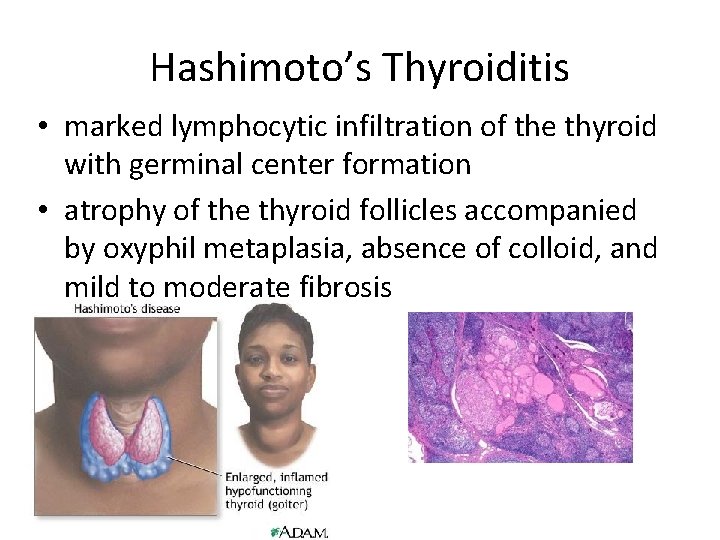
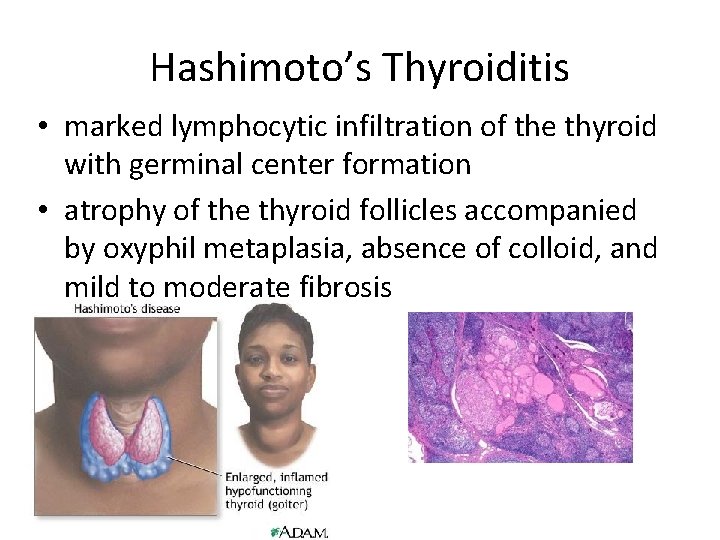
Hashimoto’s Thyroiditis • marked lymphocytic infiltration of the thyroid with germinal center formation • atrophy of the thyroid follicles accompanied by oxyphil metaplasia, absence of colloid, and mild to moderate fibrosis
Atrophic thyroiditis • fibrosis is much more extensive, lymphocyte infiltration is less pronounced, and thyroid follicles are almost completely absent
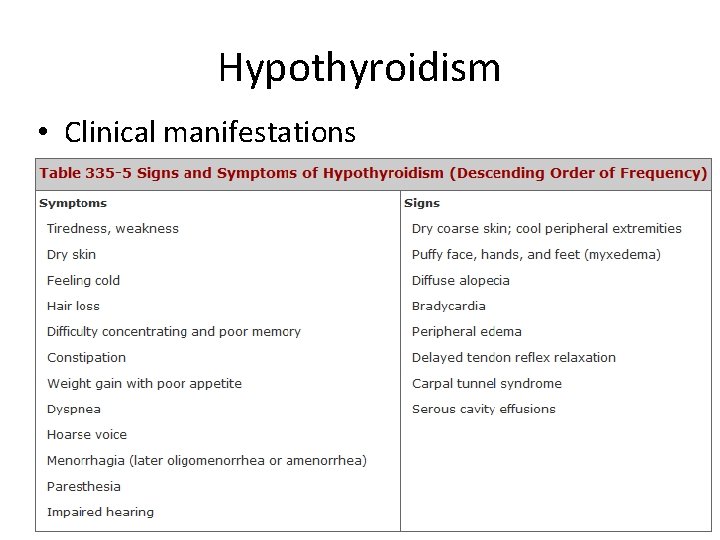
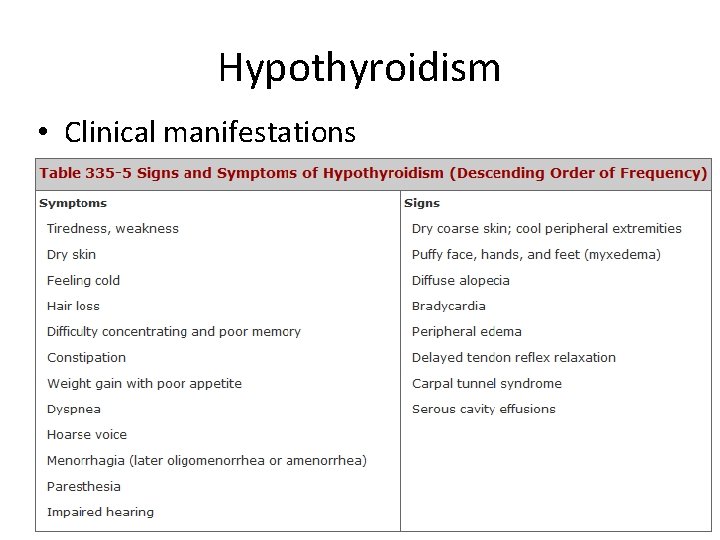
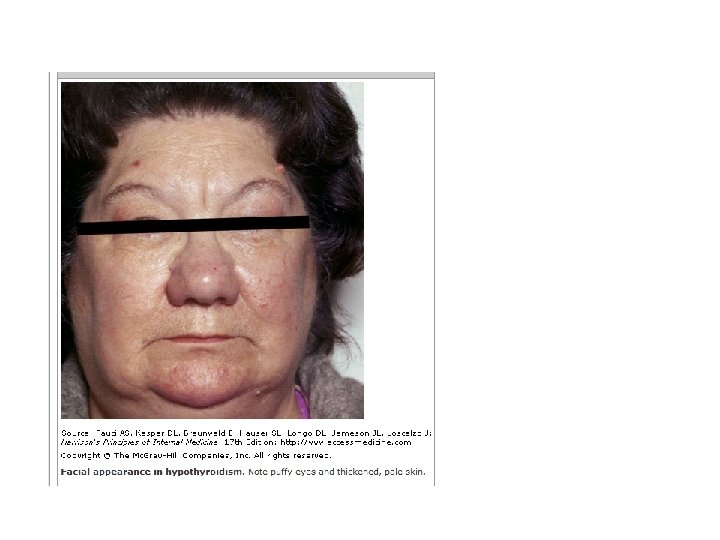
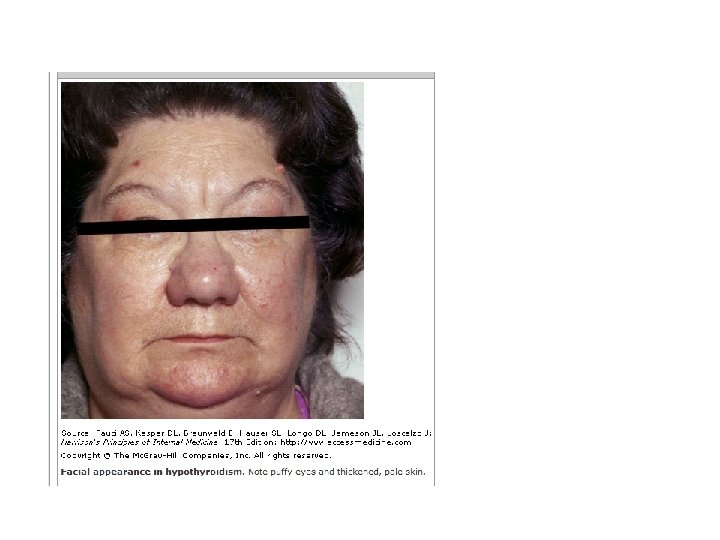
Hypothyroidism • Clinical manifestations
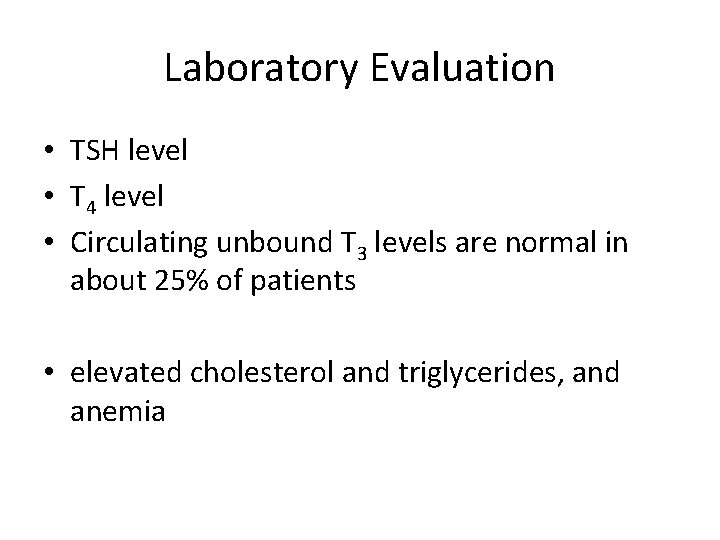
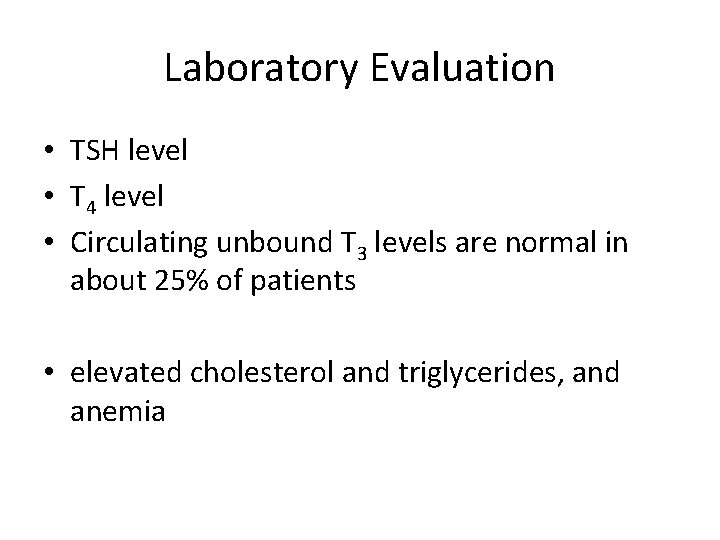
Laboratory Evaluation • TSH level • T 4 level • Circulating unbound T 3 levels are normal in about 25% of patients • elevated cholesterol and triglycerides, and anemia
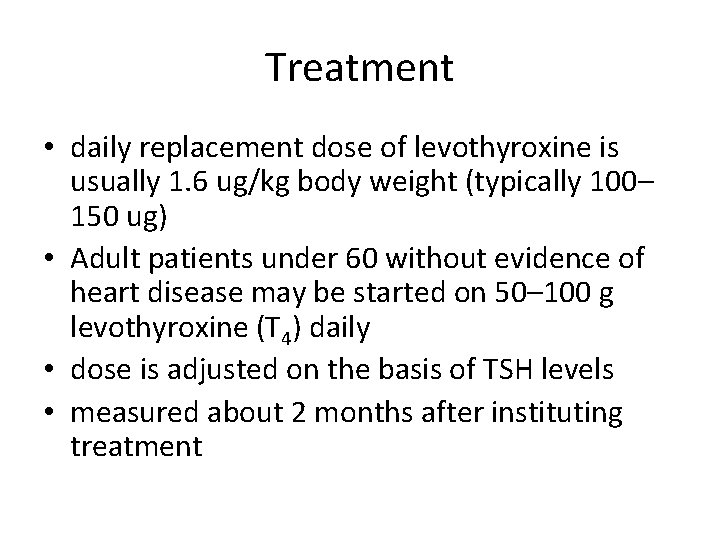
Treatment • daily replacement dose of levothyroxine is usually 1. 6 ug/kg body weight (typically 100– 150 ug) • Adult patients under 60 without evidence of heart disease may be started on 50– 100 g levothyroxine (T 4) daily • dose is adjusted on the basis of TSH levels • measured about 2 months after instituting treatment
Treatment • Patients may not experience full relief from symptoms until 3– 6 months after normal TSH levels are restored • Once full replacement is achieved and TSH levels are stable, follow-up measurement of TSH is recommended at annual intervals
Hyperthyroidism • Causes: – Graves' disease – Toxic multinodular goiter – Toxic adenoma – Functioning thyroid carcinoma metastases – Activating mutation of the TSH receptor – Activating mutation of Gsa (Mc. Cune-Albright syndrome) – Struma ovarii – Drugs: iodine excess (Jod-Basedow phenomenon)
Graves disease • combination of environmental and genetic factors • stress is an important environmental factor, presumably operating through neuroendocrine effects • Due to TSI synthesized in the thyroid gland as well as in bone marrow and lymph nodes
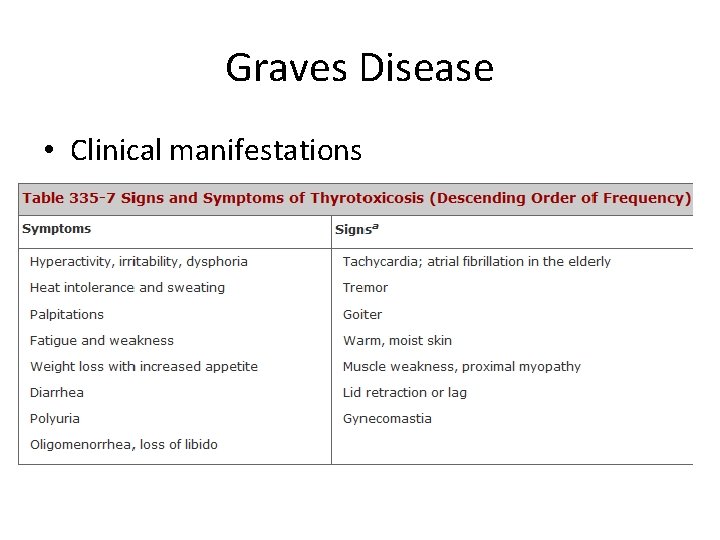
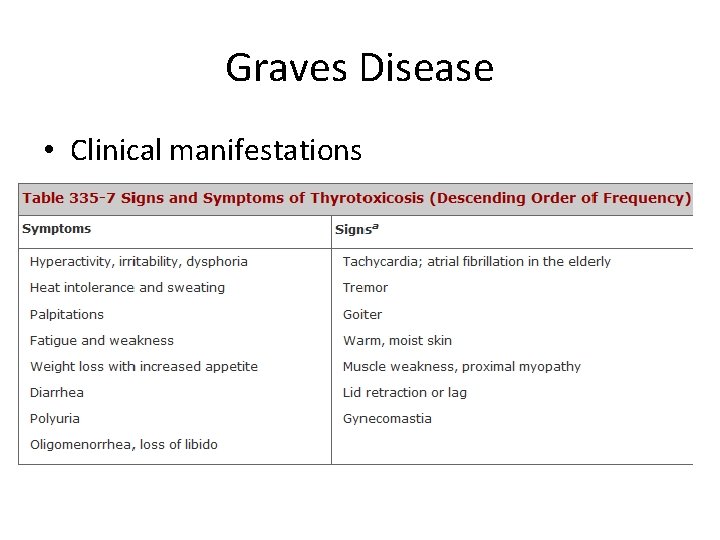
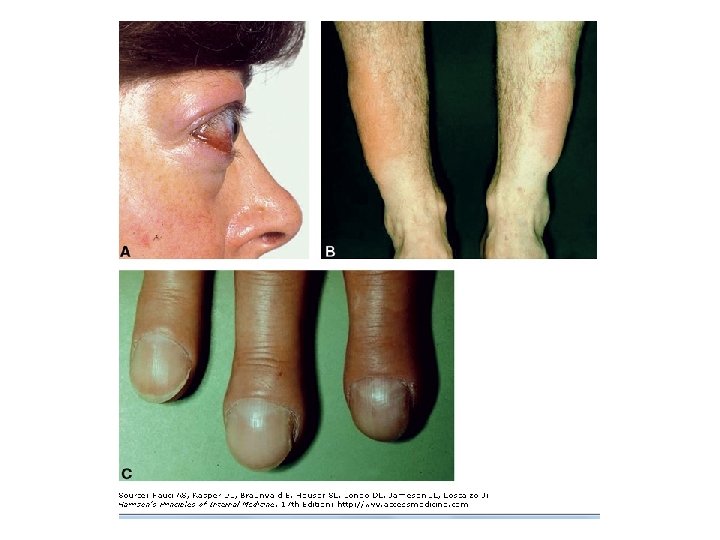
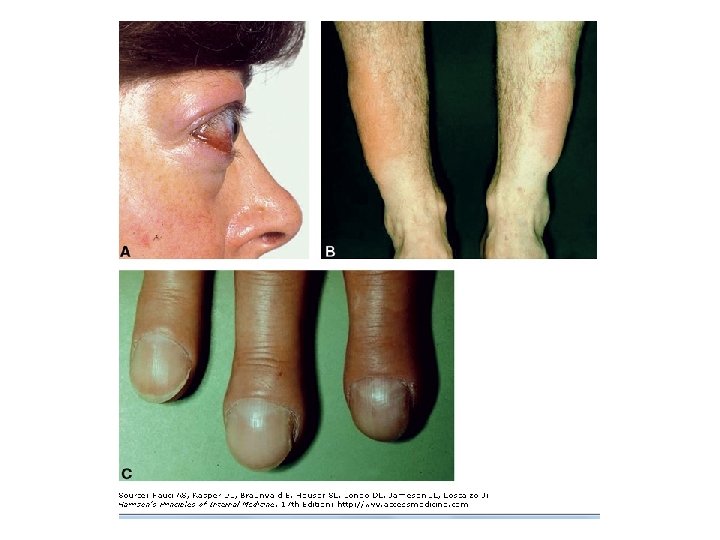
Graves Disease • Clinical manifestations
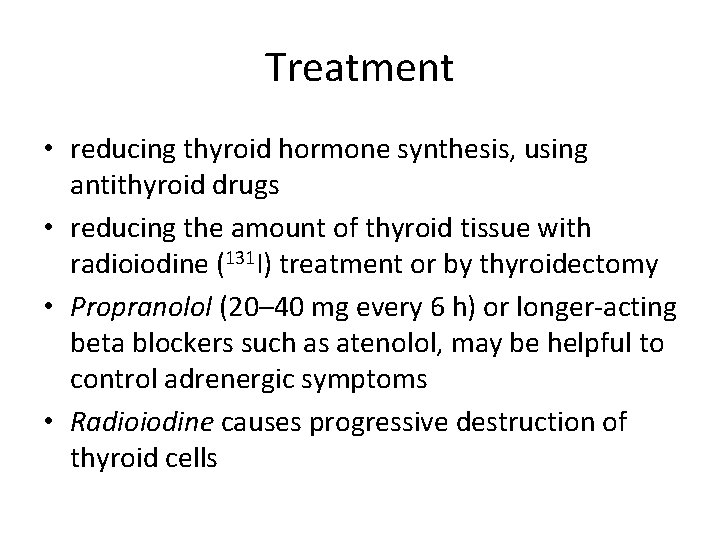
Treatment • reducing thyroid hormone synthesis, using antithyroid drugs • reducing the amount of thyroid tissue with radioiodine (131 I) treatment or by thyroidectomy • Propranolol (20– 40 mg every 6 h) or longer-acting beta blockers such as atenolol, may be helpful to control adrenergic symptoms • Radioiodine causes progressive destruction of thyroid cells