HYPERTENSIVE VASCULAR DISEASE Types and Causes of Hypertension



- Slides: 66
HYPERTENSIVE VASCULAR DISEASE

Types and Causes of Hypertension (Systolic and Diastolic) � ESSENTIAL HYPERTENSION � 90% TO 95% OF CASES � SECONDARY HYPERTENSION �Renal �Endocrine �Cardiovascular �Neurologic
Renal � Acute glomerulonephritis � Chronic renal disease � Polycystic disease � Renal artery stenosis � Renal vasculitis � Renin-producing tumors
Endocrine Adrenocortical hyperfunction � Exogenous hormones � � � Pheochromocytoma Hypothyroidism (myxedema) � � Acromegaly Hyperthyroidism (thyrotoxicosis) � Pregnancy-induced
Cardiovascular � Coarctation of aorta � Polyarteritis nodosa � Increased intravascular volume � Increased cardiac output � Rigidity of the aorta
Neurologic � Psychogenic � Increased intracranial pressure � Sleep apnea � Acute stress, including surgery
Essential hypertension � 95% � Idiopathic � Generally does not cause short-term problems.
Essential hypertension � When controlled �Compatible with long life �Asymptomatic � Unless ○ A myocardial infarction, cerebrovascular accident, or other complication supervenes.
Accelerated / Malignant Hypertension � 5% of hypertensives � Rapidly rising blood pressure � If untreated death within a year or two. � May develop in previously normotensives
Accelerated / Malignant Hypertension �Systolic pressure >200 mm hg, �Diastolic pressure >120 mm hg �Renal failure �Retinal hemorrhages and exudates �With or without papilledema.
MECHANISMS OF ESSENTIAL HYPERTENSION
a complex, multifactorial disorder � Genetic factors � Reduced renal sodium excretion � Vasoconstrictive influences � Environmental factors
Genetic factors � play a definite role � several single-gene disorders �cause relatively rare forms of hypertension (and hypotension) �through several mechanisms
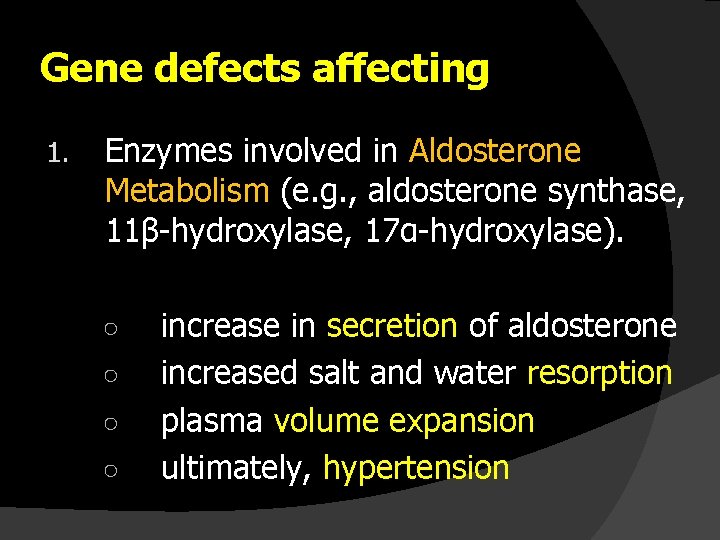
Gene defects affecting 1. Enzymes involved in Aldosterone Metabolism (e. g. , aldosterone synthase, 11β-hydroxylase, 17α-hydroxylase). ○ ○ increase in secretion of aldosterone increased salt and water resorption plasma volume expansion ultimately, hypertension
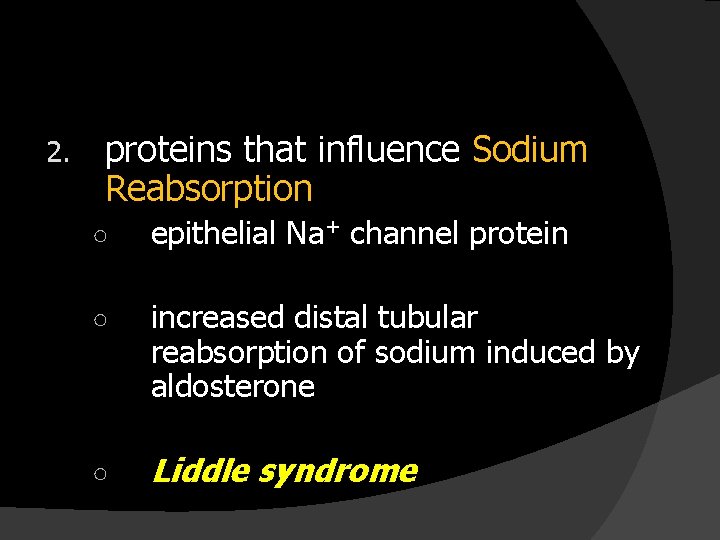
2. proteins that influence Sodium Reabsorption ○ epithelial Na+ channel protein ○ increased distal tubular reabsorption of sodium induced by aldosterone ○ Liddle syndrome
� Inherited variations in BP may also depend on the cumulative effects of polymorphisms in several genes that affect blood pressure. � For example ○ variations in the genes encoding components of the renin-angiotensin system
Reduced renal sodium excretion � may be a key initiating event in essential hypertension � may lead sequentially to an increase in �fluid volume �cardiac output �peripheral vasoconstriction �thereby elevating blood pressure.
Vasoconstrictive influences � increase peripheral resistance � chronic or repeated vasoconstrictive influences could cause thickening and rigidity of the involved vessels.
Environmental factors � can modify the impact of genetic determinants. �Stress �Obesity �Smoking �physical inactivity �heavy consumption of salt
PATHOGENESIS OF SECONDARY HYPERTENSION
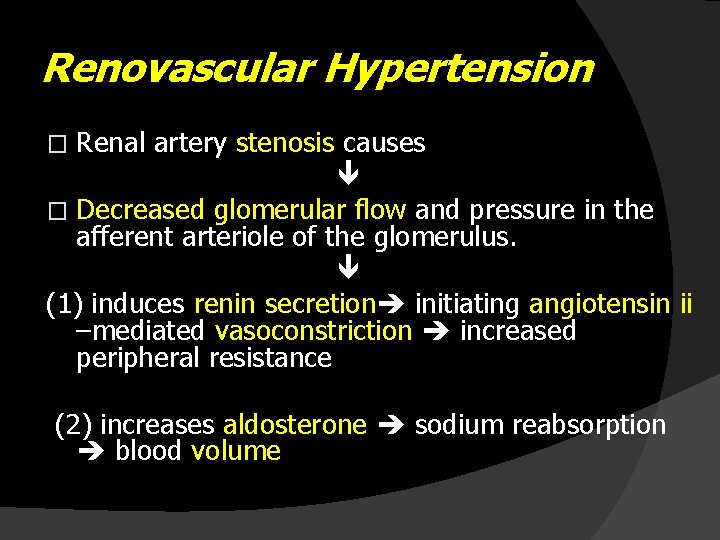
Renovascular Hypertension Renal artery stenosis causes � Decreased glomerular flow and pressure in the afferent arteriole of the glomerulus. (1) induces renin secretion initiating angiotensin ii –mediated vasoconstriction increased peripheral resistance � (2) increases aldosterone sodium reabsorption blood volume
VASCULAR PATHOLOGY IN HYPERTENSION
VASCULAR PATHOLOGY IN HYPERTENSION � Accelerates atherogenesis � Causes degenerative changes in the walls of large and medium arteries that can lead to - Aortic dissection and - Cerebrovascular hemorrhage.
Morphology � Two forms of small blood vessel disease: �Hyaline arteriolosclerosis & �Hyperplastic arteriolosclerosis.
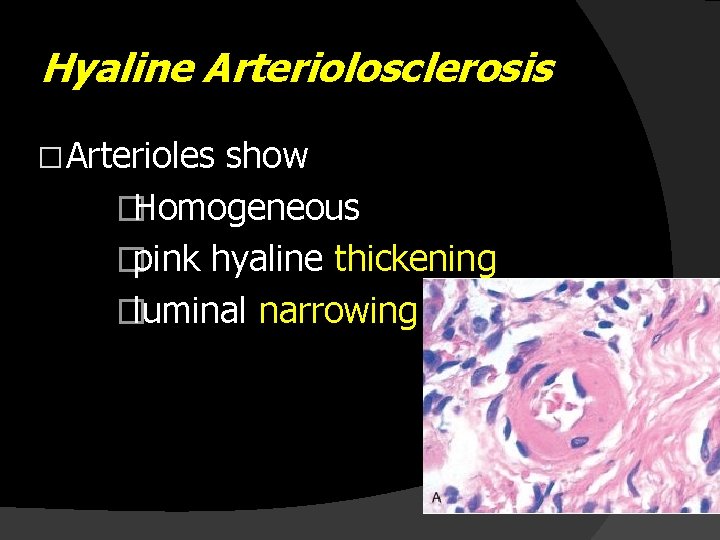
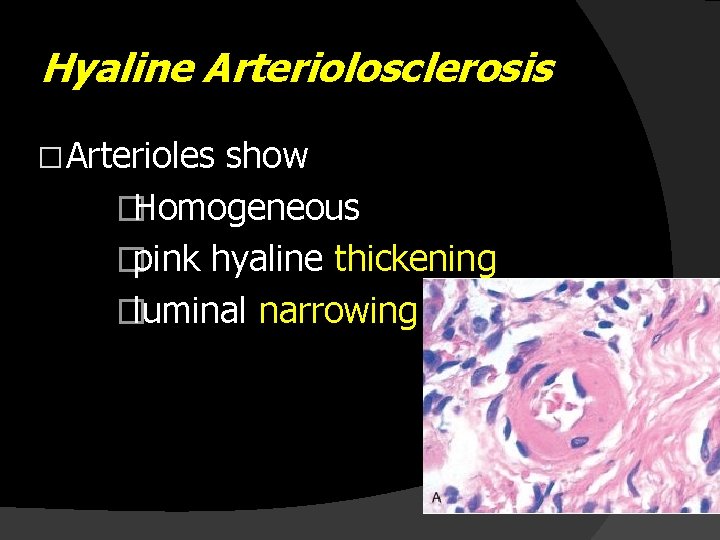
Hyaline Arteriolosclerosis � Arterioles show �Homogeneous �pink hyaline thickening �luminal narrowing
Hyaline Arteriolosclerosis � Plasma protein leakage across injured endothelial cells � Increased smooth muscle cell matrix synthesis in response to chronic hemodynamic stress.
Hyaline Arteriolosclerosis � In Nephrosclerosis due to chronic hypertension, the arteriolar narrowing of hyaline arteriosclerosis causes ○ diffuse impairment of renal blood supply ○ glomerular scarring
Hyaline Arteriolosclerosis � Vessels of elderly persons (either normo- or hypertensive) � Diabetic microangiography
Morphology � Two forms of small blood vessel disease: �Hyaline arteriolosclerosis & �Hyperplastic arteriolosclerosis.
Hyperplastic Arteriolosclerosis. � in severe (malignant) hypertension � vessels exhibit “onion-skin lesions, ” � characterized by ○ concentric ○ laminated thickening of the walls and ○ luminal narrowing
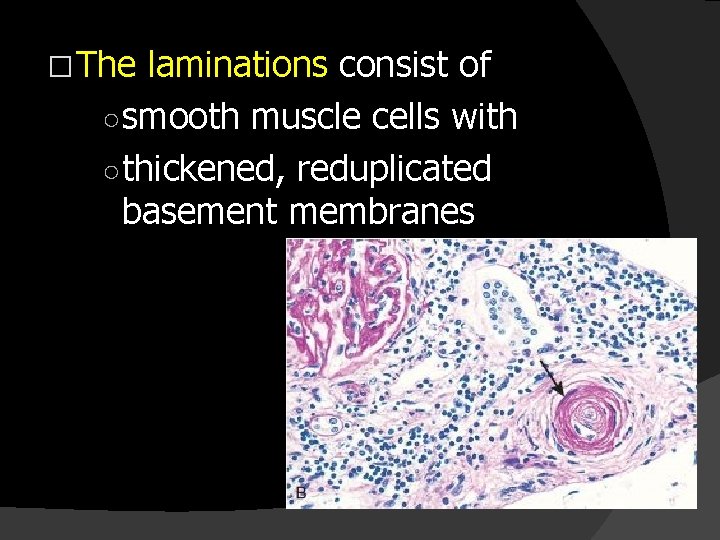
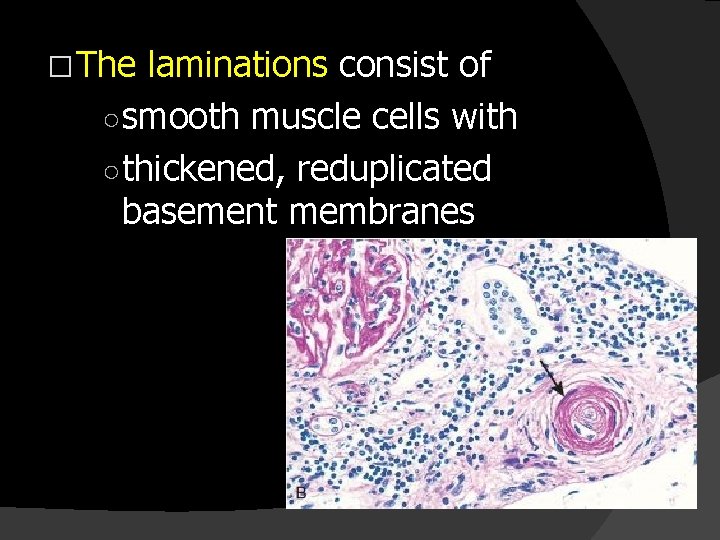
� The laminations consist of ○ smooth muscle cells with ○ thickened, reduplicated basement membranes
� In malignant hypertension they are accompanied by ○ fibrinoid deposits & ○ vessel wall necrosis (necrotizing arteriolitis), particularly in the kidney.

HYPERTENSIVE HEART DISEASE
Hypertensive Heart Disease � stems from ○ the increased demands placed on the heart by hypertension, which causes - pressure overload - ventricular hypertrophy
� Systemic (Left-sided) Hypertensive Heart Disease � Pulmonary (Right-sided) Hypertensive Heart Disease (Cor Pulmonale)
SYSTEMIC (LEFT-SIDED) HYPERTENSIVE HEART DISEASE � In hypertension, hypertrophy of the heart is an �adaptive response to pressure overload �that can lead to ümyocardial dysfunction ücardiac dilation üCHF üin some cases sudden death.
The minimal criteria for the diagnosis of systemic HHD are the following: (1) Left ventricular hypertrophy � � (2) (usually concentric) In the absence of other cardiovascular pathology A history or pathologic evidence of hypertension.

MORPHOLOGY
Morphology � Hypertension induces left ventricular pressure overload hypertrophy �Initially without ventricular dilation �Increases the weight of the heart disproportionately to the increase in overall cardiac size
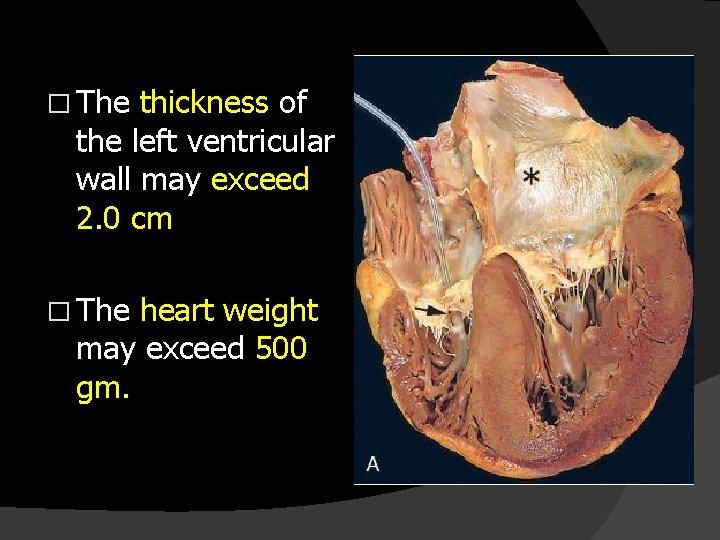
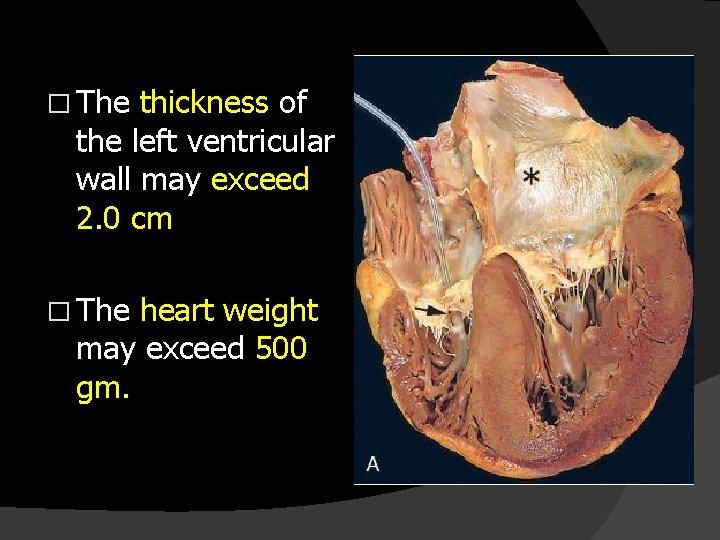
� The thickness of the left ventricular wall may exceed 2. 0 cm � The heart weight may exceed 500 gm.
� In time the increased thickness � imparts a stiffness � impairs diastolic filling � often inducing left atrial enlargement
Microscopy � The earliest change of systemic HHD ○ An increase in the transverse diameter of myocytes ○ May be difficult to appreciate on routine microscopy. � At a more advanced stage ○ cellular and nuclear enlargement become apparent ○ often accompanied by interstitial fibrosis.
Compensated systemic HHD � may be asymptomatic �producing only electrocardiographic or echocardiographic evidence of left ventricular enlargement. � In many, systemic HHD comes to attention due to new atrial fibrillation �induced by left atrial enlargement or CHF.
� Depending on the severity, duration, and underlying basis of the hypertension, and on the adequacy of therapeutic control, the patient may ○ enjoy normal longevity ○ develop IHD due to the potentiating effects of hypertension on coronary atherosclerosis ○ suffer renal damage or cerebrovascular stroke as direct effects of hypertension ○ experience progressive heart failure or SCD.
� Effective control of hypertension �can prevent or �lead to regression of cardiac hypertrophy and its associated risks
PULMONARY (RIGHT-SIDED) HYPERTENSIVE HEART DISEASE (COR PULMONALE) � stems from pressure overload of the right ventricle � characterized by ○ right ventricular hypertrophy ○ dilation ○ potentially failure � The most frequent causes are ○ disorders of the lungs
Disorders Predisposing to Cor Pulmonale � DISEASES OF THE PULMONARY PARENCHYMA �Chronic obstructive pulmonary disease �Diffuse pulmonary interstitial fibrosis �Pneumoconioses �Cystic fibrosis �Bronchiectasis
� DISEASES OF THE PULMONARY VESSELS �Recurrent pulmonary thromboembolism �Primary pulmonary hypertension �Extensive pulmonary arteritis (e. g. , Wegener granulomatosis) �Drug-, toxin-, or radiation-induced vascular obstruction �Extensive pulmonary tumor microembolism
� DISORDERS AFFECTING CHEST MOVEMENT �Kyphoscoliosis �Marked obesity (sleep apnea, pickwickian syndrome) �Neuromuscular diseases
� DISORDERS INDUCING PULMONARY ARTERIAL CONSTRICTION �Metabolic acidosis �Hypoxemia �Chronic altitude sickness �Obstruction of major airways �Idiopathic alveolar hypoventilation
� Cor pulmonale may be �acute or chronic. � Acute cor pulmonale ○ can follow massive pulmonary embolism. � Chronic cor pulmonale results from ○ right ventricular hypertrophy (and dilation) ○ secondary to prolonged pressure overload
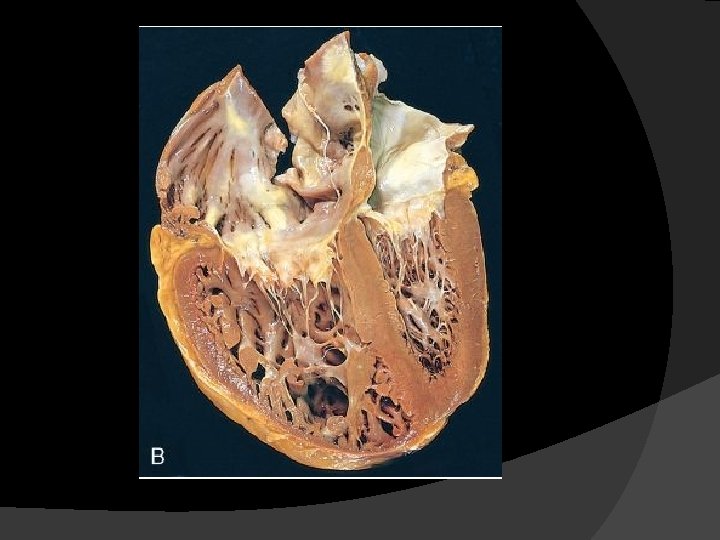
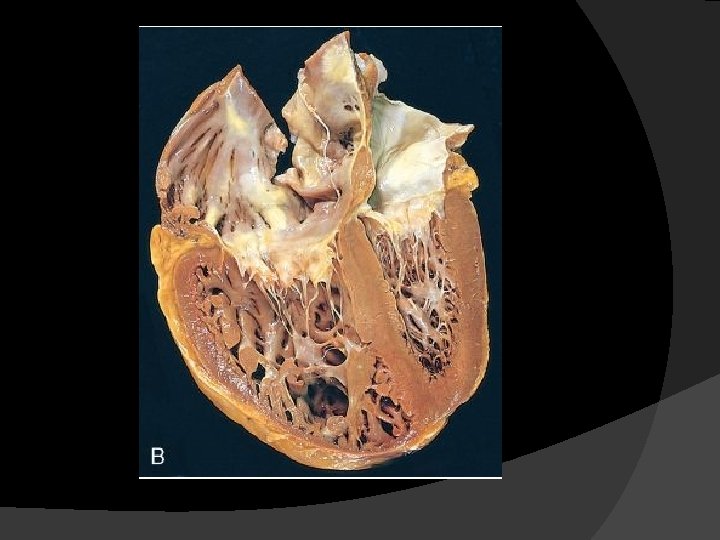
Morphology � In Acute Cor Pulmonale there is �marked dilation of the right ventricle �without hypertrophy. �On cross-section the normal crescent shape of the right ventricle is transformed to a dilated ovoid.
� In chronic cor pulmonale ○ the right ventricular wall thickens ○ sometimes up to 1. 0 cm or more � More subtle RVH may take the form of �thickening of the muscle bundles in the outflow tract, immediately below the pulmonary valve, or �thickening of the moderator band
� Sometimes, the hypertrophied right ventricle ○ compresses the left ventricular chamber, or ○ leads to regurgitation and fibrous thickening of the tricuspid valve.
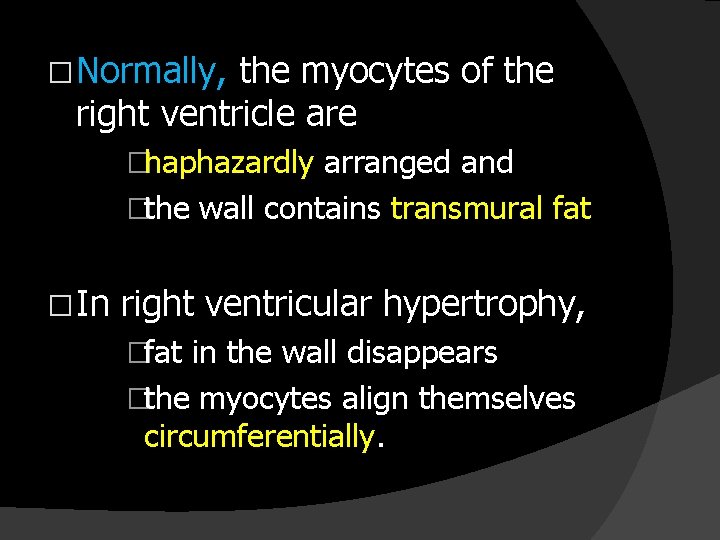
� Normally, the myocytes of the right ventricle are �haphazardly arranged and �the wall contains transmural fat � In right ventricular hypertrophy, �fat in the wall disappears �the myocytes align themselves circumferentially.
Renal changes Benign Nephrosclerosis � Associated with long-standing hypertension and diabetes. Patients are usually old. � This infrequently causes Uremia and death � A mild proteinuria is present. � GFR mildly diminished.
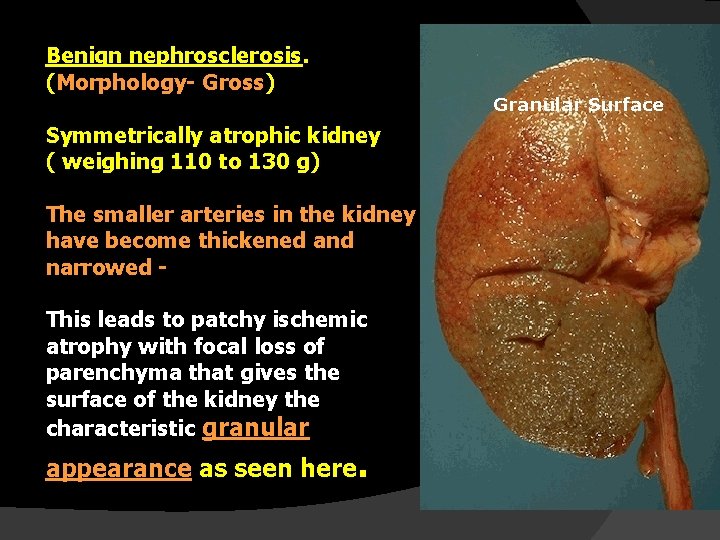
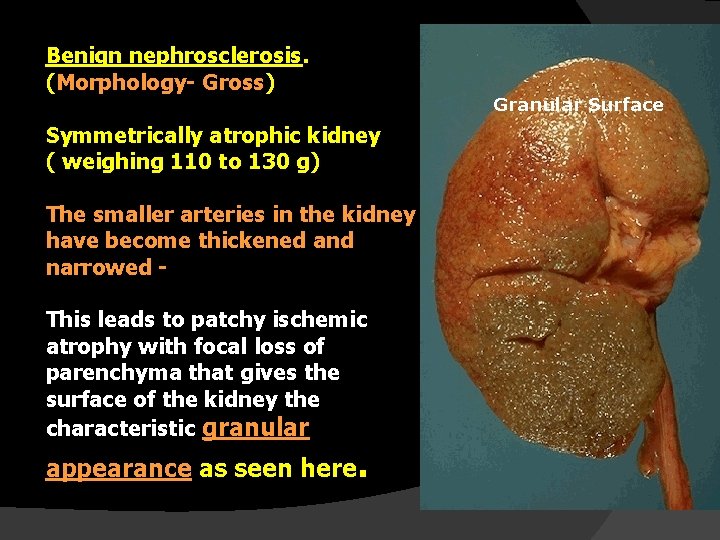
Benign nephrosclerosis. (Morphology- Gross) Symmetrically atrophic kidney ( weighing 110 to 130 g) The smaller arteries in the kidney have become thickened and narrowed - This leads to patchy ischemic atrophy with focal loss of parenchyma that gives the surface of the kidney the characteristic granular appearance as seen here. Granular Surface
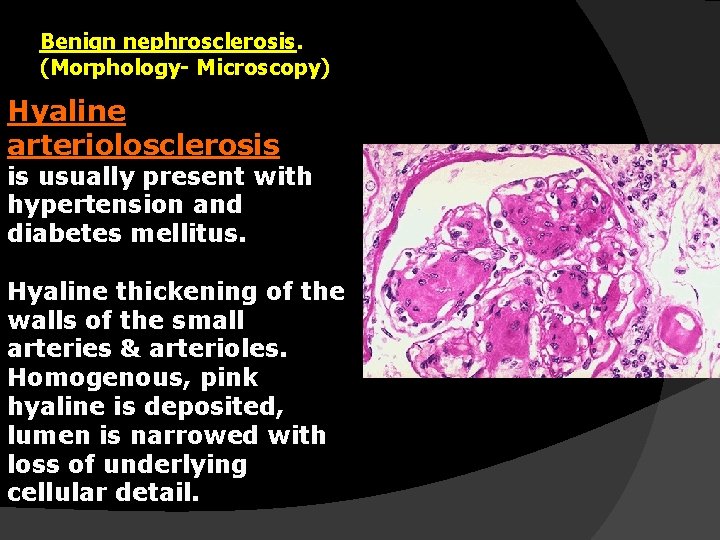
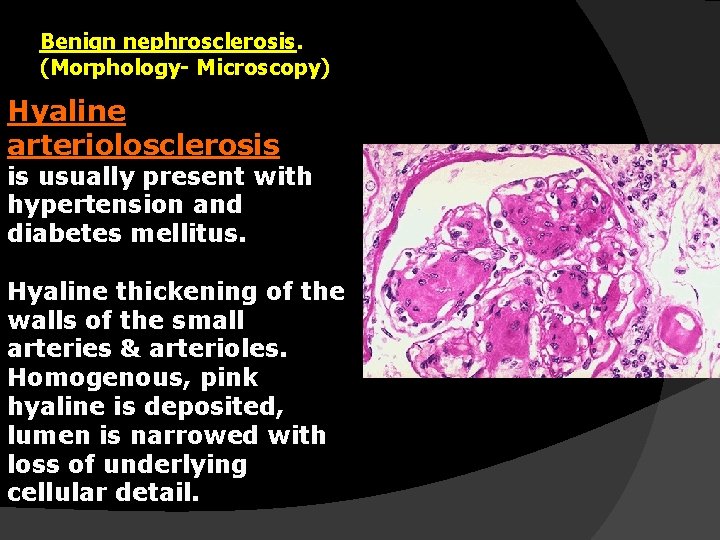
Benign nephrosclerosis. (Morphology- Microscopy) Hyaline arteriolosclerosis is usually present with hypertension and diabetes mellitus. Hyaline thickening of the walls of the small arteries & arterioles. Homogenous, pink hyaline is deposited, lumen is narrowed with loss of underlying cellular detail.
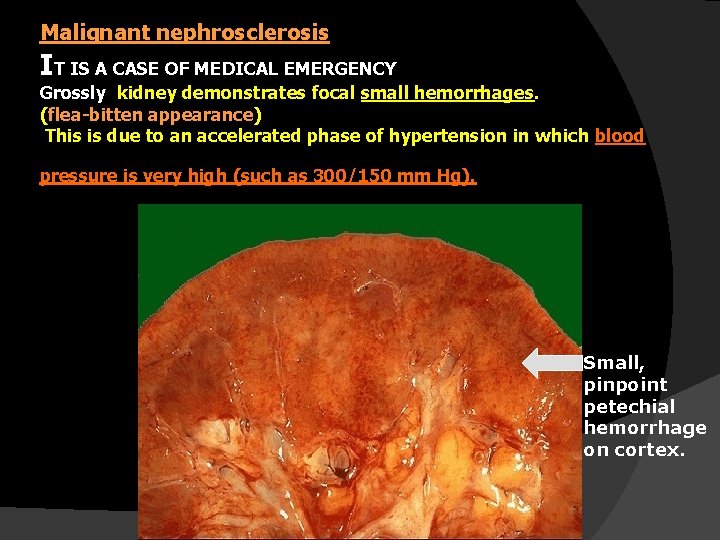
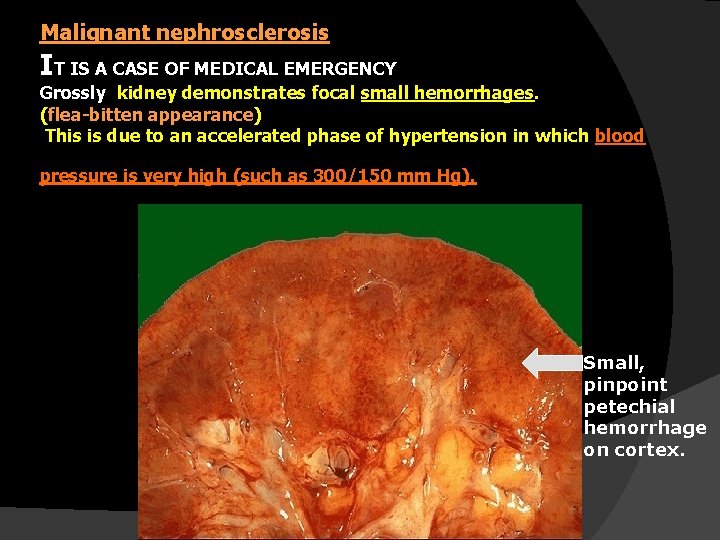
Malignant nephrosclerosis IT IS A CASE OF MEDICAL EMERGENCY Grossly kidney demonstrates focal small hemorrhages. (flea-bitten appearance) This is due to an accelerated phase of hypertension in which blood pressure is very high (such as 300/150 mm Hg). Small, pinpoint petechial hemorrhage on cortex.
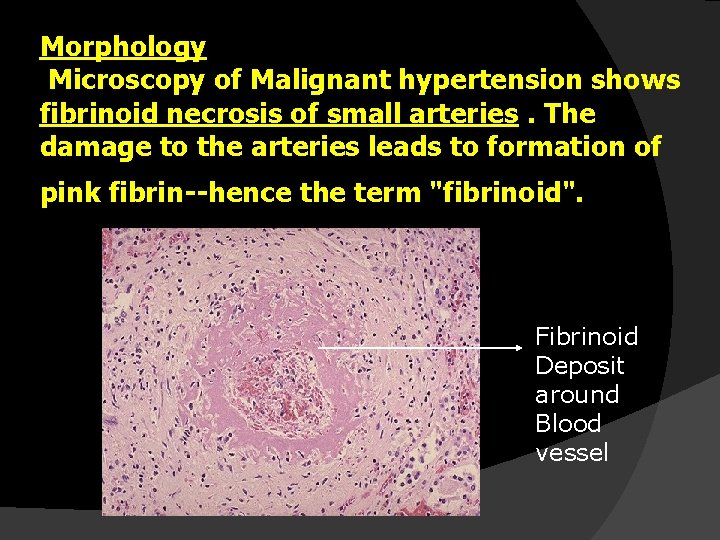
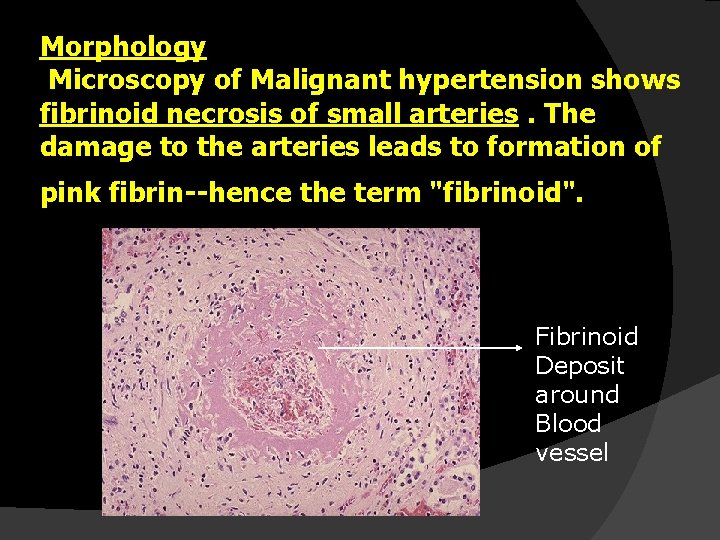
Morphology Microscopy of Malignant hypertension shows fibrinoid necrosis of small arteries. The damage to the arteries leads to formation of pink fibrin--hence the term "fibrinoid". Fibrinoid Deposit around Blood vessel
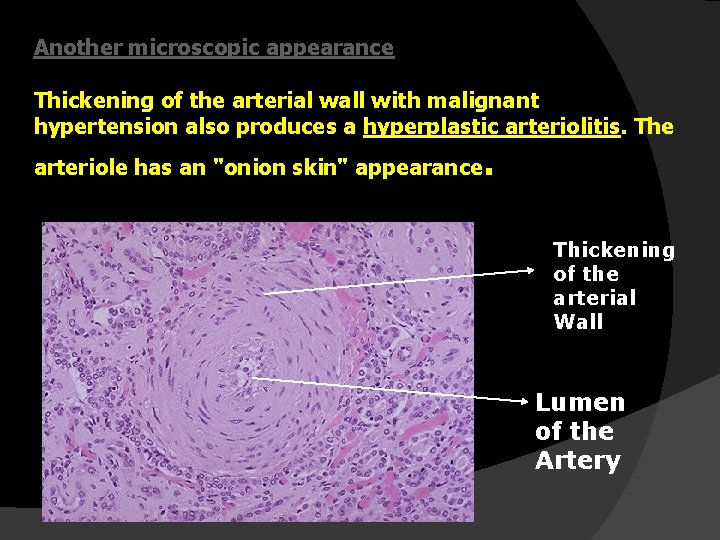
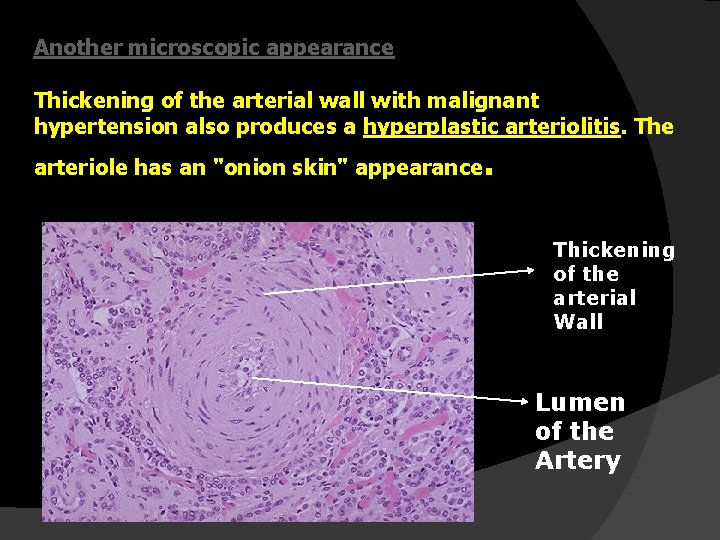
Another microscopic appearance Thickening of the arterial wall with malignant hypertension also produces a hyperplastic arteriolitis. The arteriole has an "onion skin" appearance . Thickening of the arterial Wall Lumen of the Artery
Malignant Nephrosclerosis Clinical Features. � Characterized by Diastolic pressure more than 120 mm Hg. ( Hypertension) � Patient may present with: � 1. Papilledema, encephalopathy, cardiovascular abnormality and � 2. Renal failure.
Malignant Nephrosclerosis clinical Symptoms. � � Nausea, vomiting Marked proteinuria Hematuria. Visual impairment 50% - survive for at least 5 years. 90% - death – caused by Uremia 10%- death – by Cerebral Hemorrhage IT IS CASE OF TRUE MEDICAL EMERGENCY