HYPERTENSION THE KIDNEY Blood Pressure Classification BP Classification
고혈압과 신장 (HYPERTENSION & THE KIDNEY)
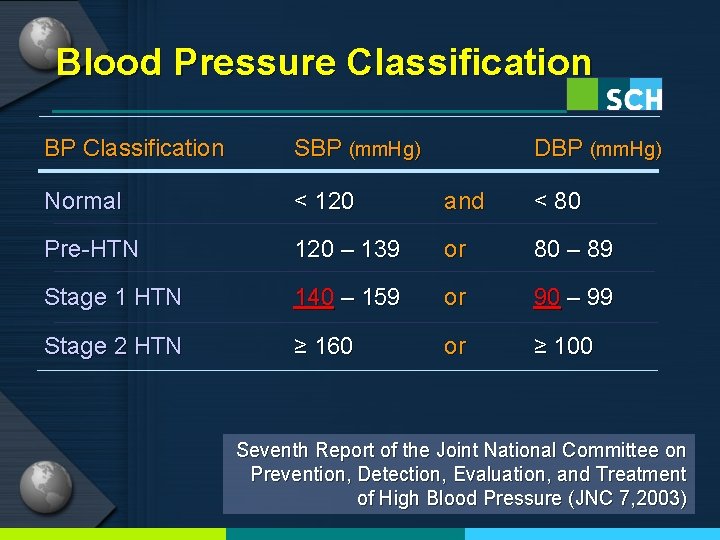
Blood Pressure Classification BP Classification SBP (mm. Hg) DBP (mm. Hg) Normal < 120 and < 80 Pre-HTN 120 – 139 or 80 – 89 Stage 1 HTN 140 – 159 or 90 – 99 Stage 2 HTN ≥ 160 or ≥ 100 Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7, 2003)
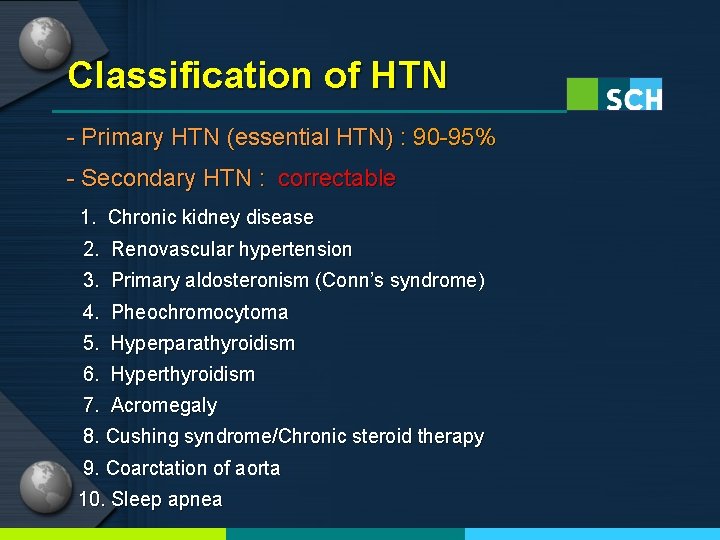
Classification of HTN - Primary HTN (essential HTN) : 90 -95% - Secondary HTN : correctable 1. Chronic kidney disease 2. Renovascular hypertension 3. Primary aldosteronism (Conn’s syndrome) 4. Pheochromocytoma 5. Hyperparathyroidism 6. Hyperthyroidism 7. Acromegaly 8. Cushing syndrome/Chronic steroid therapy 9. Coarctation of aorta 10. Sleep apnea
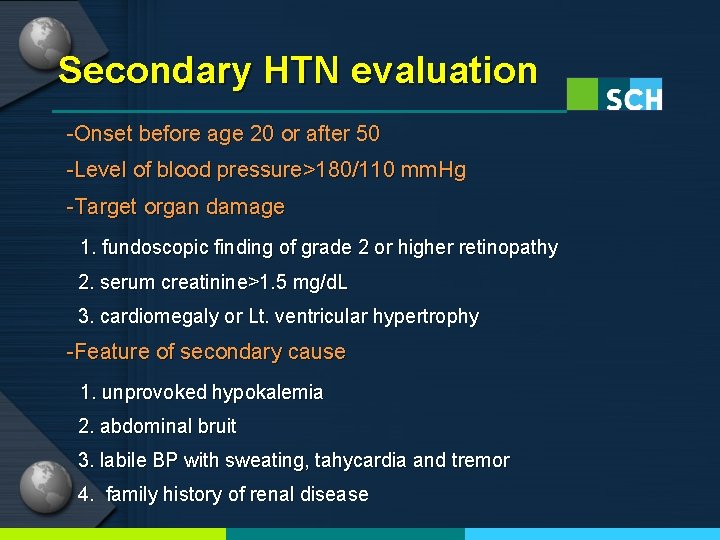
Secondary HTN evaluation -Onset before age 20 or after 50 -Level of blood pressure>180/110 mm. Hg -Target organ damage 1. fundoscopic finding of grade 2 or higher retinopathy 2. serum creatinine>1. 5 mg/d. L 3. cardiomegaly or Lt. ventricular hypertrophy -Feature of secondary cause 1. unprovoked hypokalemia 2. abdominal bruit 3. labile BP with sweating, tahycardia and tremor 4. family history of renal disease
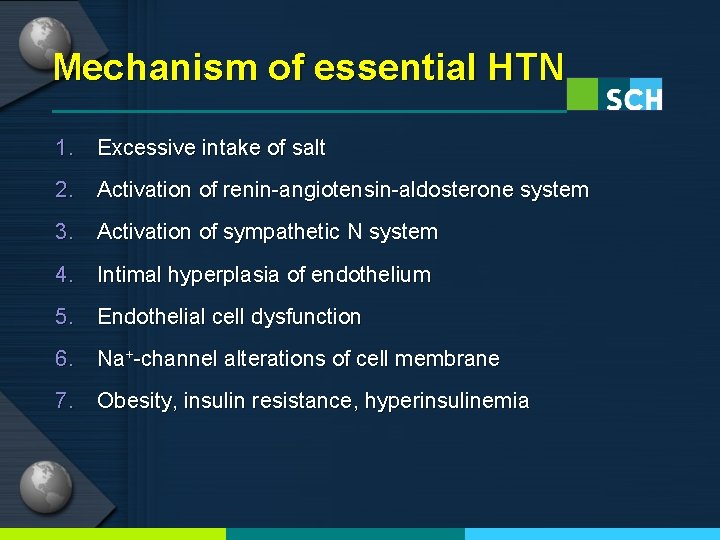
Mechanism of essential HTN 1. Excessive intake of salt 2. Activation of renin-angiotensin-aldosterone system 3. Activation of sympathetic N system 4. Intimal hyperplasia of endothelium 5. Endothelial cell dysfunction 6. Na+-channel alterations of cell membrane 7. Obesity, insulin resistance, hyperinsulinemia
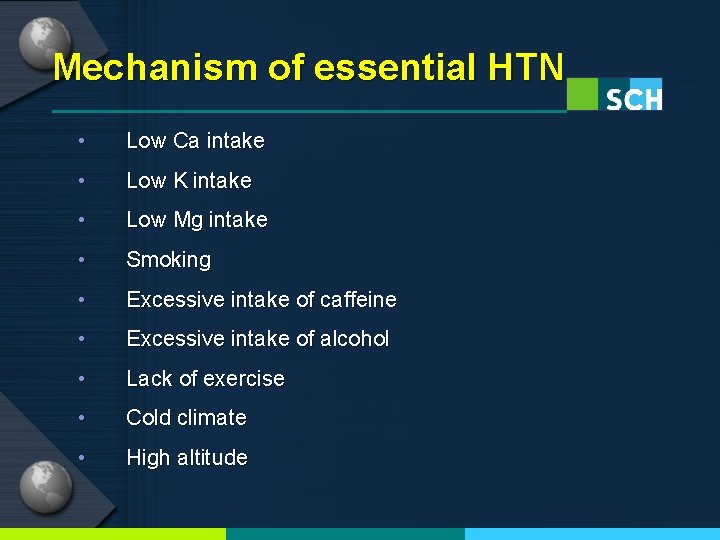
Mechanism of essential HTN • Low Ca intake • Low K intake • Low Mg intake • Smoking • Excessive intake of caffeine • Excessive intake of alcohol • Lack of exercise • Cold climate • High altitude
Effect of HTN on the Kidney
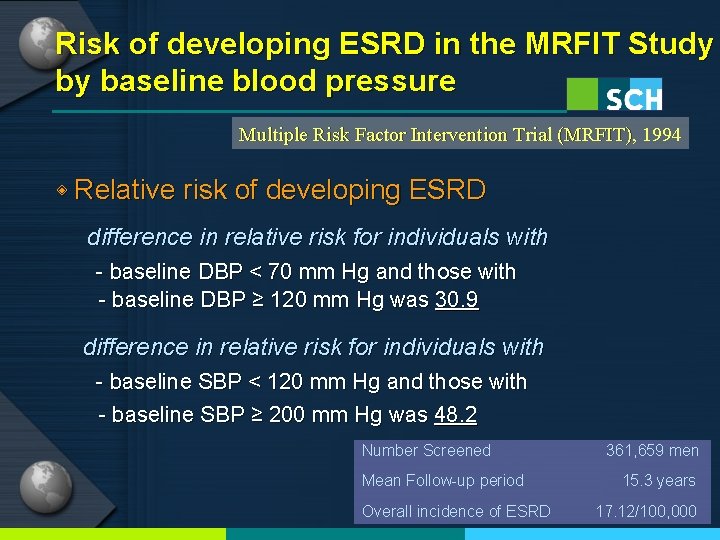
Risk of developing ESRD in the MRFIT Study by baseline blood pressure Multiple Risk Factor Intervention Trial (MRFIT), 1994 ◈ Relative risk of developing ESRD difference in relative risk for individuals with - baseline DBP < 70 mm Hg and those with - baseline DBP ≥ 120 mm Hg was 30. 9 difference in relative risk for individuals with - baseline SBP < 120 mm Hg and those with - baseline SBP ≥ 200 mm Hg was 48. 2 Number Screened Mean Follow-up period Overall incidence of ESRD 361, 659 men 15. 3 years 17. 12/100, 000
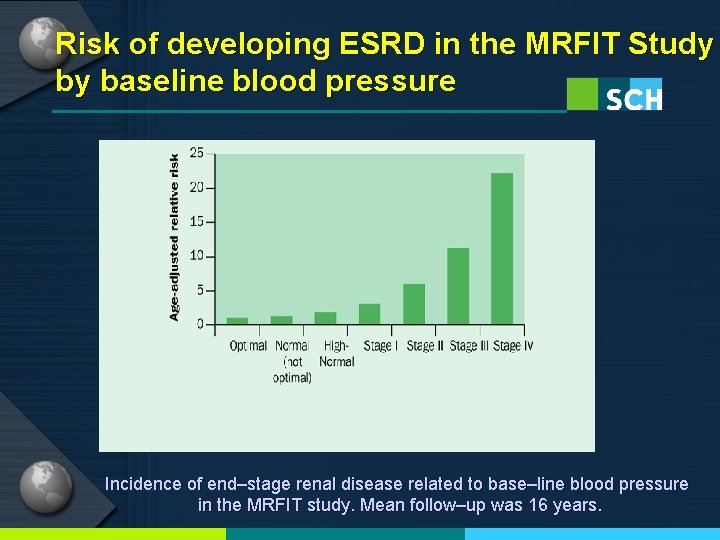
Risk of developing ESRD in the MRFIT Study by baseline blood pressure Incidence of end–stage renal disease related to base–line blood pressure in the MRFIT study. Mean follow–up was 16 years.
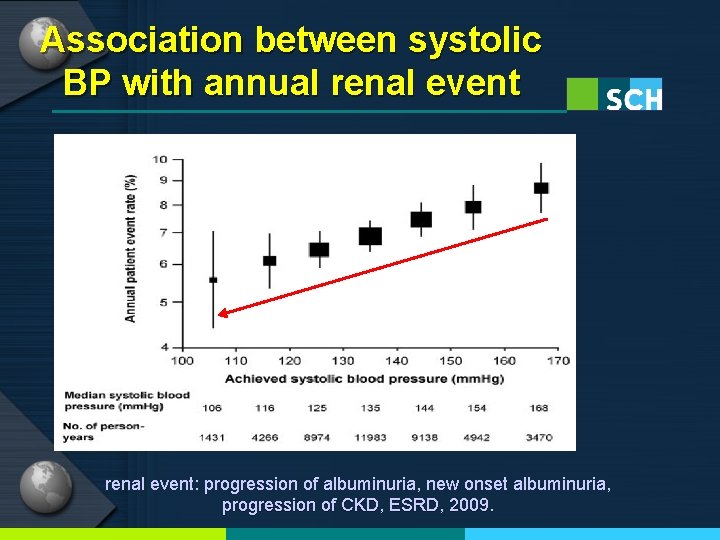
Association between systolic BP with annual renal event: progression of albuminuria, new onset albuminuria, progression of CKD, ESRD, 2009.
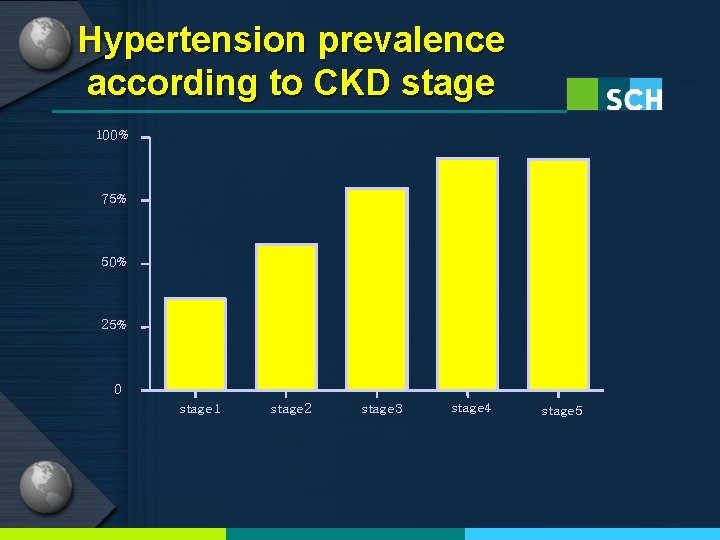
Hypertension prevalence according to CKD stage 100% 75% 50% 25% 0 stage 1 stage 2 stage 3 stage 4 stage 5
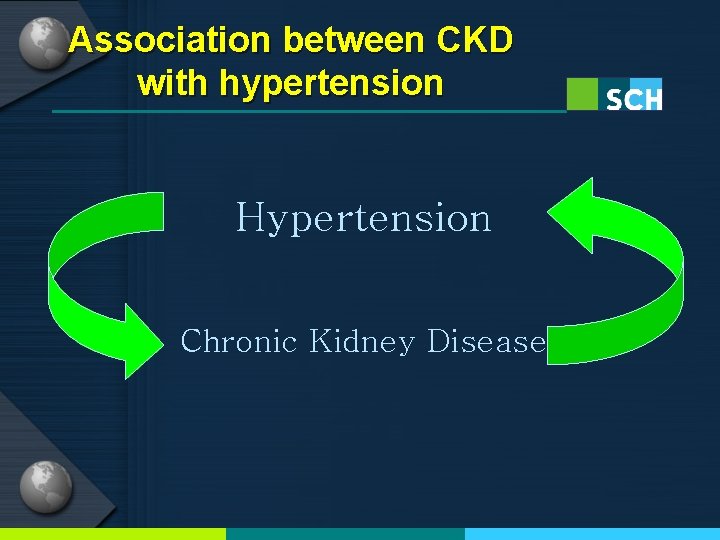
Association between CKD with hypertension Hypertension Chronic Kidney Disease
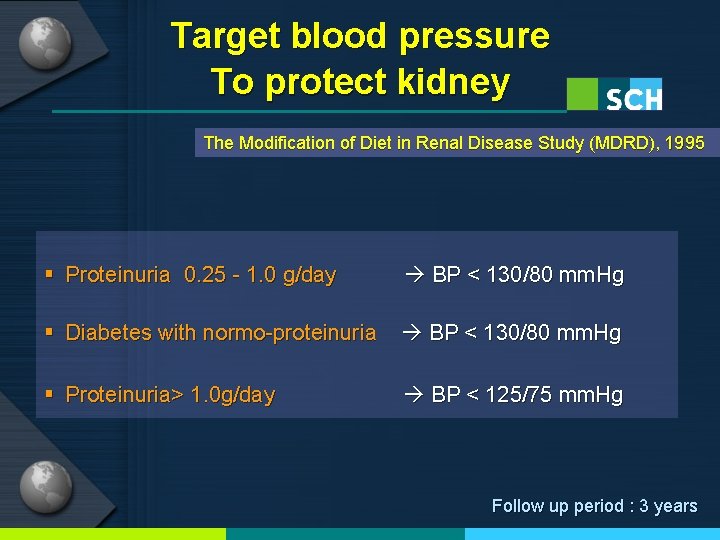
Target blood pressure To protect kidney The Modification of Diet in Renal Disease Study (MDRD), 1995 § Proteinuria 0. 25 - 1. 0 g/day BP < 130/80 mm. Hg § Diabetes with normo-proteinuria BP < 130/80 mm. Hg § Proteinuria> 1. 0 g/day BP < 125/75 mm. Hg Follow up period : 3 years
Effect of the kidney on HTN (Renal hypertension) - Renal parenchymal HTN - Renovascular HTN
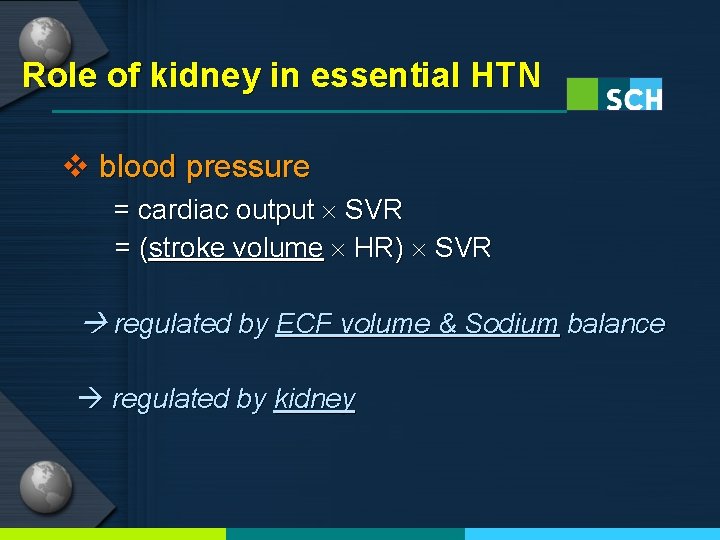
Role of kidney in essential HTN v blood pressure = cardiac output SVR = (stroke volume HR) SVR regulated by ECF volume & Sodium balance regulated by kidney
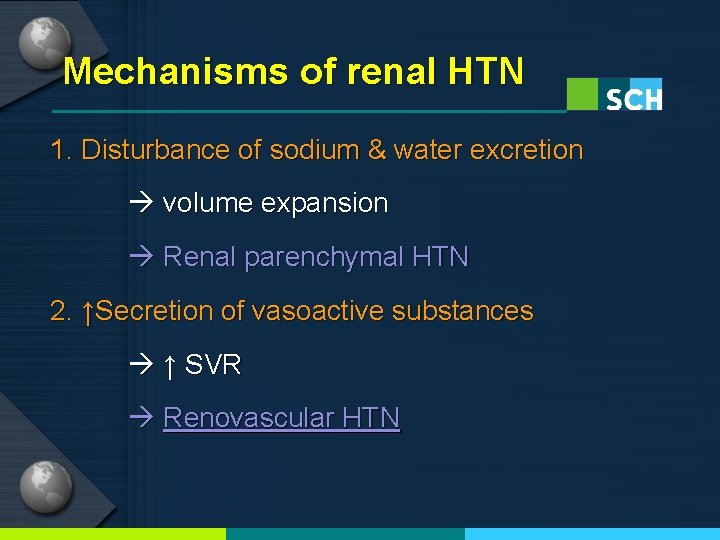
Mechanisms of renal HTN 1. Disturbance of sodium & water excretion volume expansion Renal parenchymal HTN 2. ↑Secretion of vasoactive substances ↑ SVR Renovascular HTN
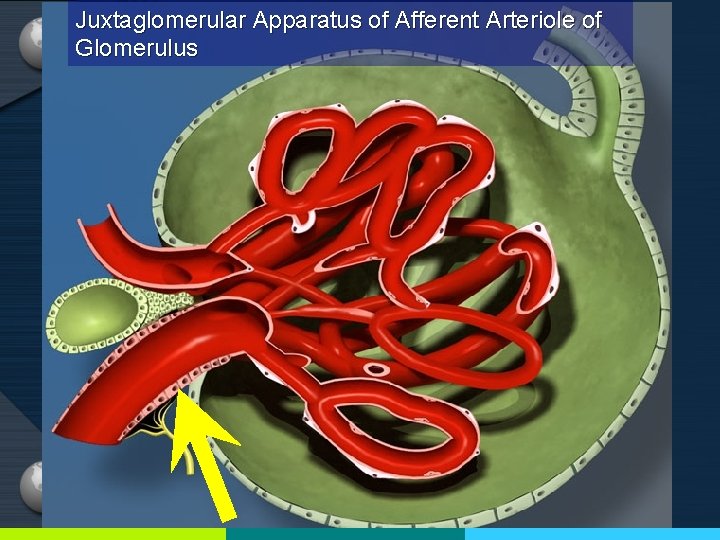
Juxtaglomerular Apparatus of Afferent Arteriole of Glomerulus
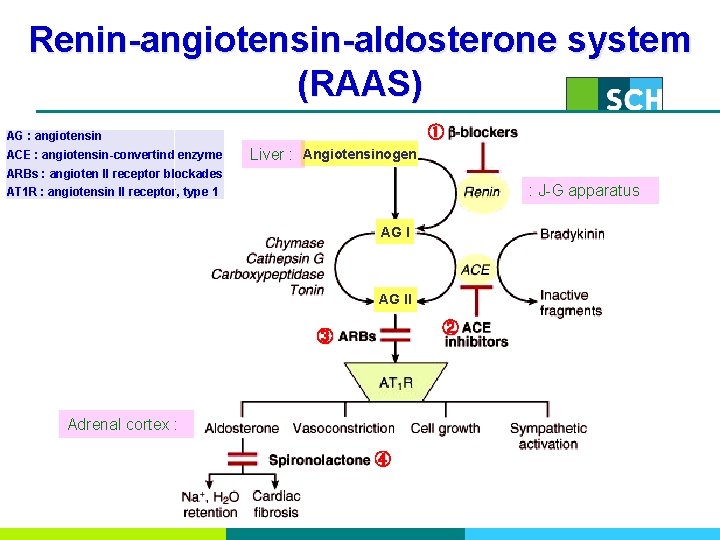
Renin-angiotensin-aldosterone system (RAAS) ① AG : angiotensin ACE : angiotensin-convertind enzyme Liver : Angiotensinogen ARBs : angioten II receptor blockades : J-G apparatus AT 1 R : angiotensin II receptor, type 1 AG II ② ③ Adrenal cortex : ④
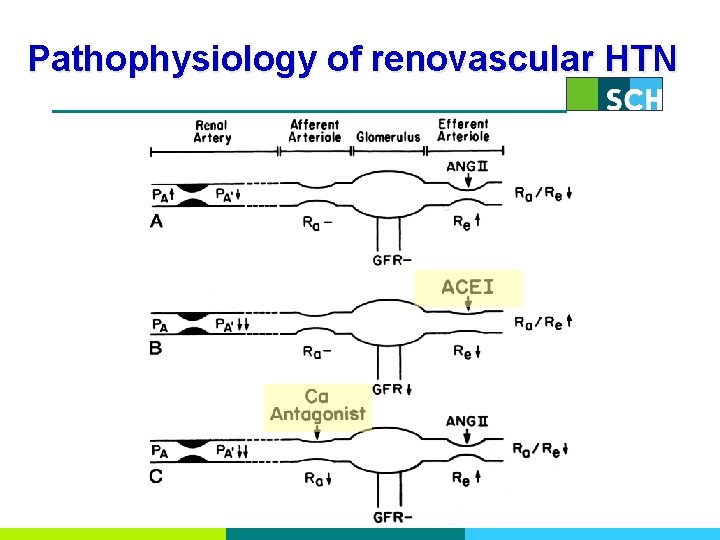
Pathophysiology of renovascular HTN
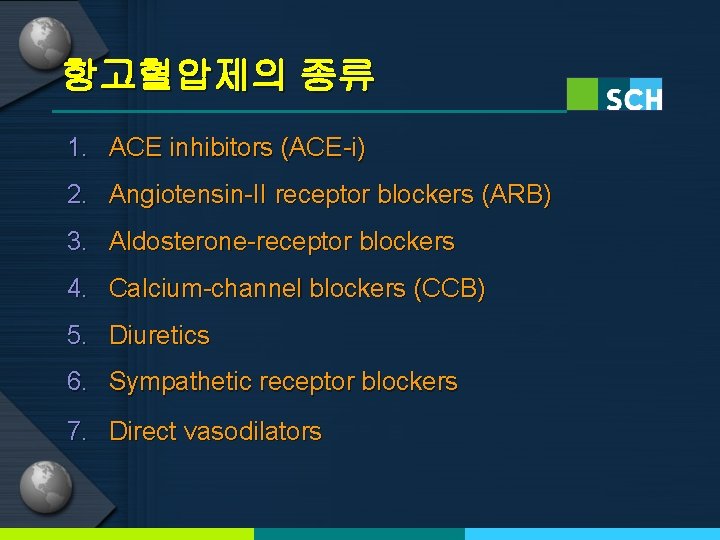
항고혈압제의 종류 1. ACE inhibitors (ACE-i) 2. Angiotensin-II receptor blockers (ARB) 3. Aldosterone-receptor blockers 4. Calcium-channel blockers (CCB) 5. Diuretics 6. Sympathetic receptor blockers 7. Direct vasodilators
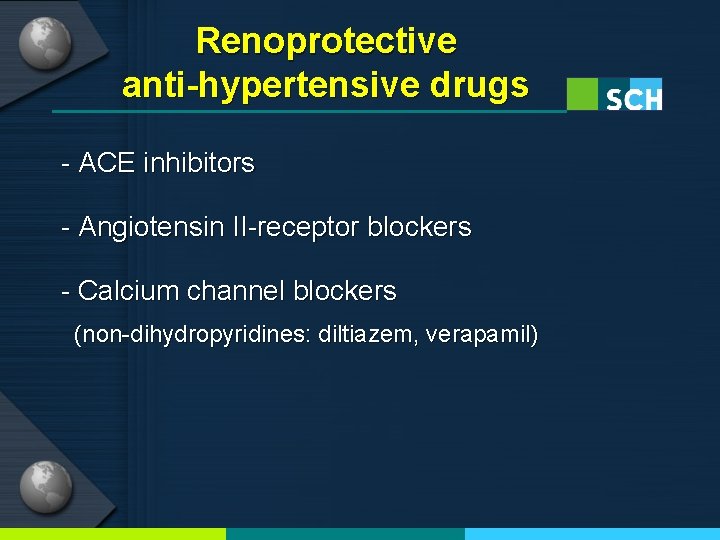
Renoprotective anti-hypertensive drugs - ACE inhibitors - Angiotensin II-receptor blockers - Calcium channel blockers (non-dihydropyridines: diltiazem, verapamil)
신혈관 질환 (VASCULAR INJURY TO THE KIDNEY)
죽상경화증과 신장혈류순환 -미세혈관질환- (Atherosclerosis and kidney circulation -Microvascular disease-)
Microvascular disease 1. Glomerular capillary endothelium: share oxidative stress, pressure injury, inflammation with other vessel 2. Urinary albumin excretion(UAE) rate: - predictor of systemic atherosclerosis - increased UAE develop years before cardiovascular event - pharmaco. Tx with statin can reduce UAE, cardiovascular event 3. Accelerated atherosclerosis and decreased perfusion pressure of large vessel: result renal microvessel functional change and rarefaction
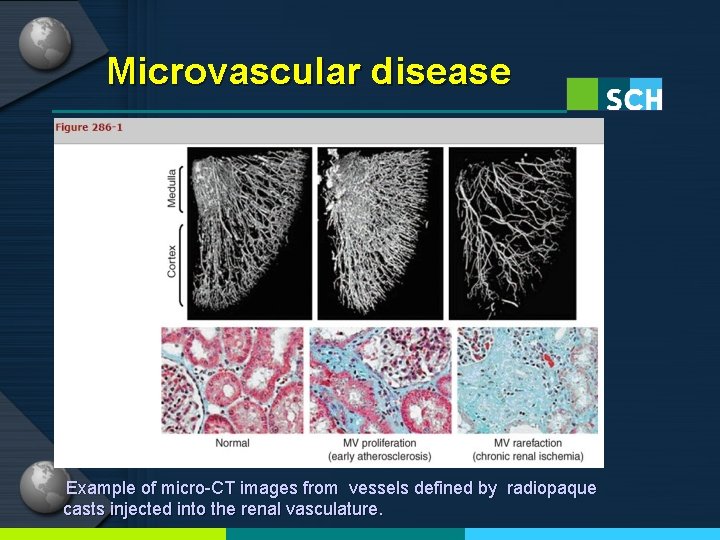
Microvascular disease Example of micro-CT images from vessels defined by radiopaque casts injected into the renal vasculature.
죽상경화증과 신장혈류순환 -대혈관질환- (Atherosclerosis and kidney circulation -Macrovascular disease-)
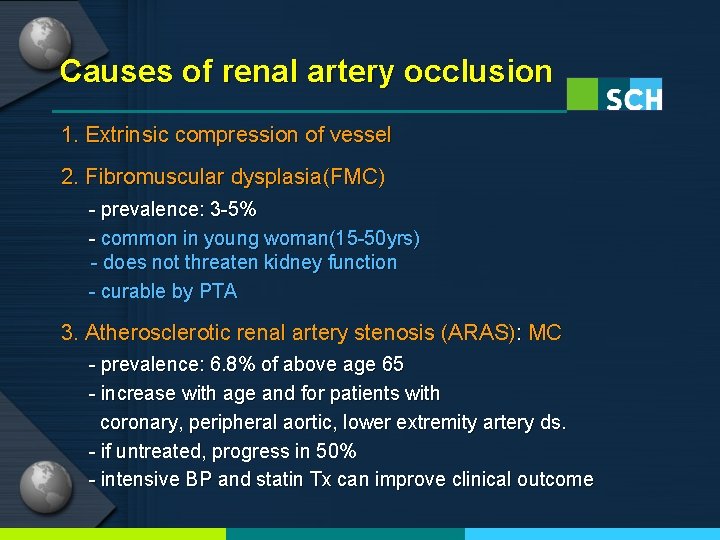
Causes of renal artery occlusion 1. Extrinsic compression of vessel 2. Fibromuscular dysplasia(FMC) - prevalence: 3 -5% - common in young woman(15 -50 yrs) - does not threaten kidney function - curable by PTA 3. Atherosclerotic renal artery stenosis (ARAS): MC - prevalence: 6. 8% of above age 65 - increase with age and for patients with coronary, peripheral aortic, lower extremity artery ds. - if untreated, progress in 50% - intensive BP and statin Tx can improve clinical outcome
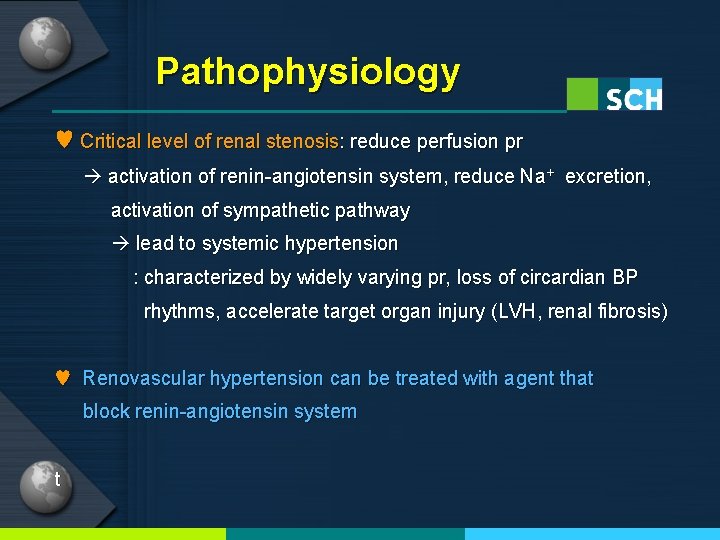
Pathophysiology ♥ Critical level of renal stenosis: reduce perfusion pr activation of renin-angiotensin system, reduce Na+ excretion, activation of sympathetic pathway lead to systemic hypertension : characterized by widely varying pr, loss of circardian BP rhythms, accelerate target organ injury (LVH, renal fibrosis) ♥ Renovascular hypertension can be treated with agent that block renin-angiotensin system t
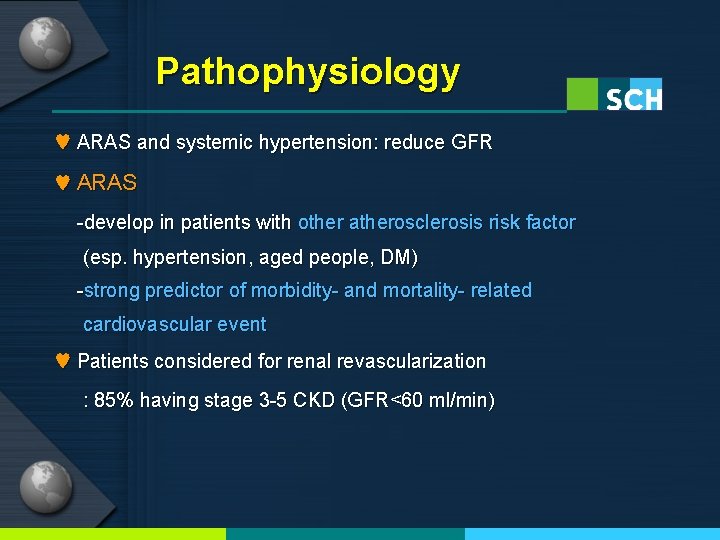
Pathophysiology ♥ ARAS and systemic hypertension: reduce GFR ♥ ARAS -develop in patients with other atherosclerosis risk factor (esp. hypertension, aged people, DM) -strong predictor of morbidity- and mortality- related cardiovascular event ♥ Patients considered for renal revascularization : 85% having stage 3 -5 CKD (GFR<60 ml/min)
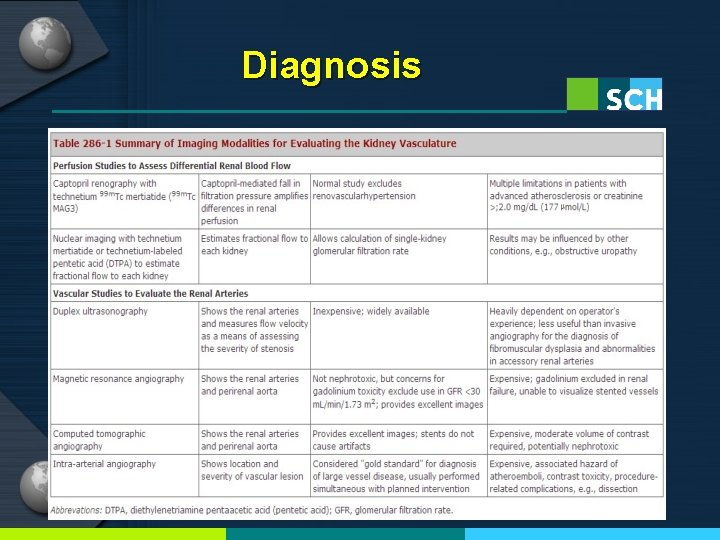
Diagnosis
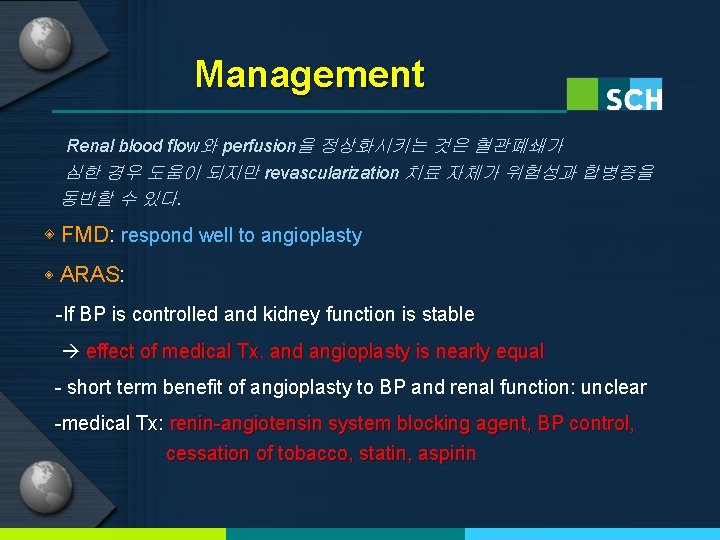
Management Renal blood flow와 perfusion을 정상화시키는 것은 혈관폐쇄가 심한 경우 도움이 되지만 revascularization 치료 자체가 위험성과 합병증을 동반할 수 있다. ◈ FMD: respond well to angioplasty ◈ ARAS: -If BP is controlled and kidney function is stable effect of medical Tx. and angioplasty is nearly equal - short term benefit of angioplasty to BP and renal function: unclear -medical Tx: renin-angiotensin system blocking agent, BP control, cessation of tobacco, statin, aspirin
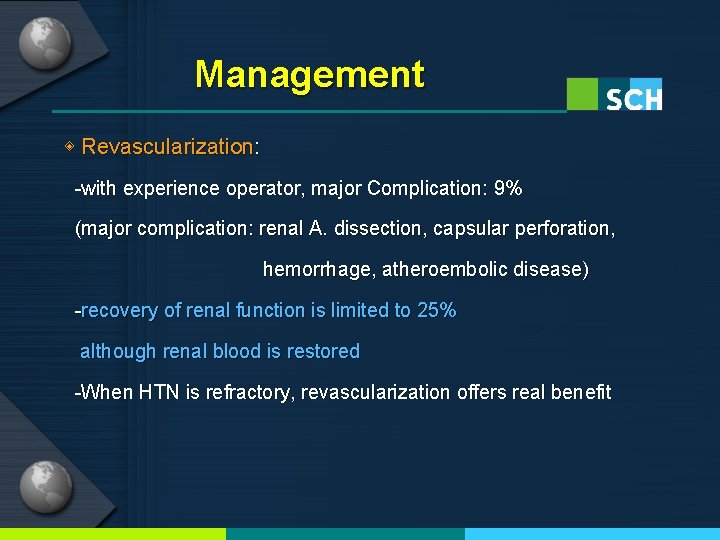
Management ◈ Revascularization: -with experience operator, major Complication: 9% (major complication: renal A. dissection, capsular perforation, hemorrhage, atheroembolic disease) -recovery of renal function is limited to 25% although renal blood is restored -When HTN is refractory, revascularization offers real benefit
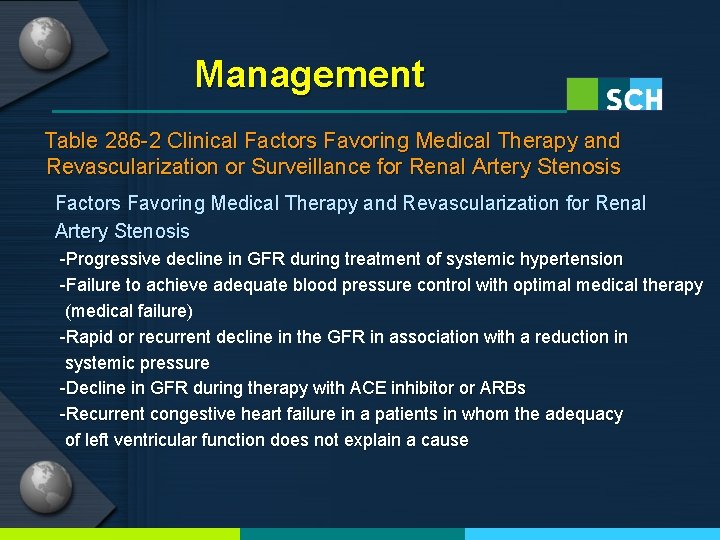
Management Table 286 -2 Clinical Factors Favoring Medical Therapy and Revascularization or Surveillance for Renal Artery Stenosis Factors Favoring Medical Therapy and Revascularization for Renal Artery Stenosis -Progressive decline in GFR during treatment of systemic hypertension -Failure to achieve adequate blood pressure control with optimal medical therapy (medical failure) -Rapid or recurrent decline in the GFR in association with a reduction in systemic pressure -Decline in GFR during therapy with ACE inhibitor or ARBs -Recurrent congestive heart failure in a patients in whom the adequacy of left ventricular function does not explain a cause
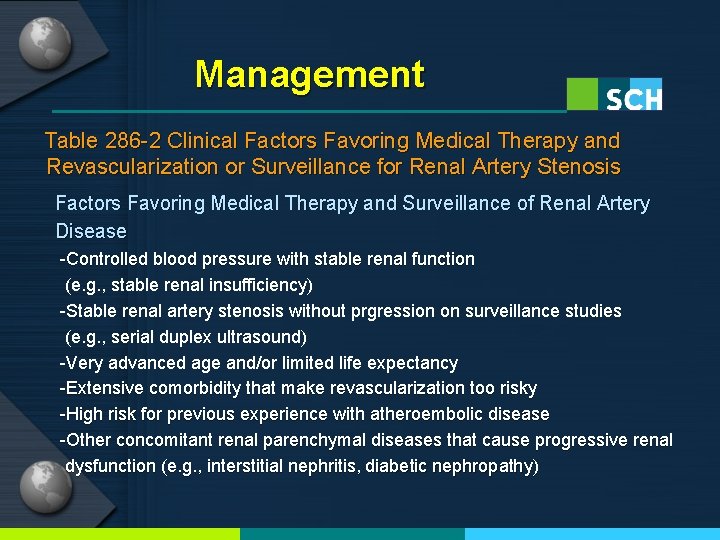
Management Table 286 -2 Clinical Factors Favoring Medical Therapy and Revascularization or Surveillance for Renal Artery Stenosis Factors Favoring Medical Therapy and Surveillance of Renal Artery Disease -Controlled blood pressure with stable renal function (e. g. , stable renal insufficiency) -Stable renal artery stenosis without prgression on surveillance studies (e. g. , serial duplex ultrasound) -Very advanced age and/or limited life expectancy -Extensive comorbidity that make revascularization too risky -High risk for previous experience with atheroembolic disease -Other concomitant renal parenchymal diseases that cause progressive renal dysfunction (e. g. , interstitial nephritis, diabetic nephropathy)
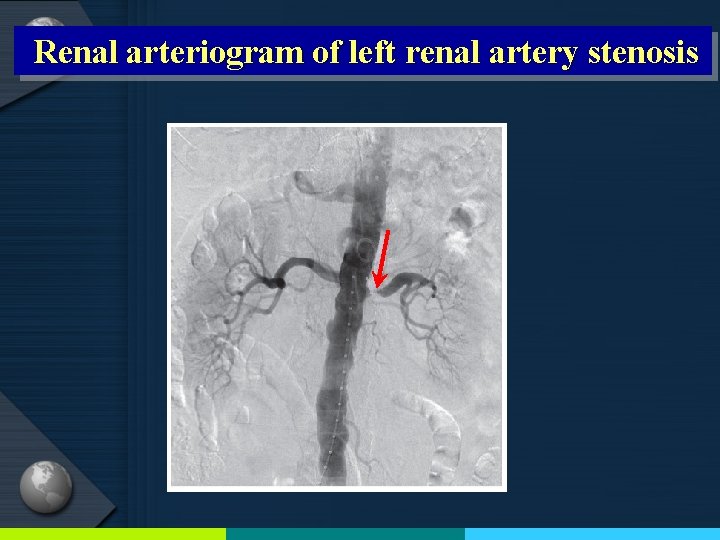
Renal arteriogram of left renal artery stenosis
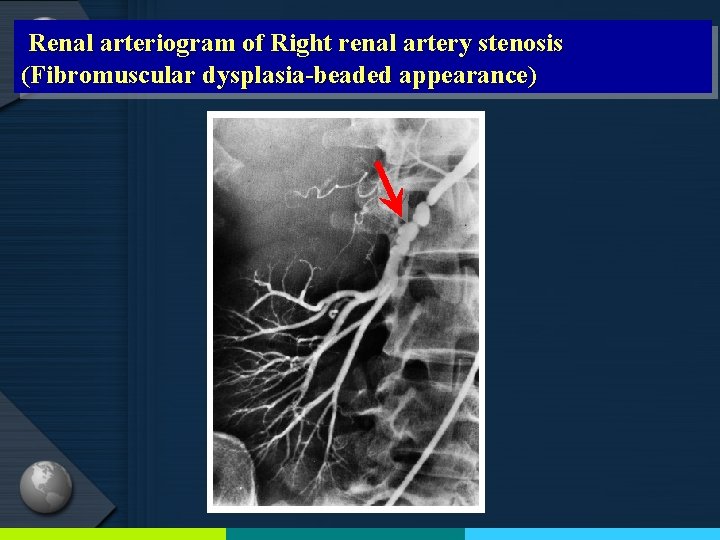
Renal arteriogram of Right renal artery stenosis (Fibromuscular dysplasia-beaded appearance)
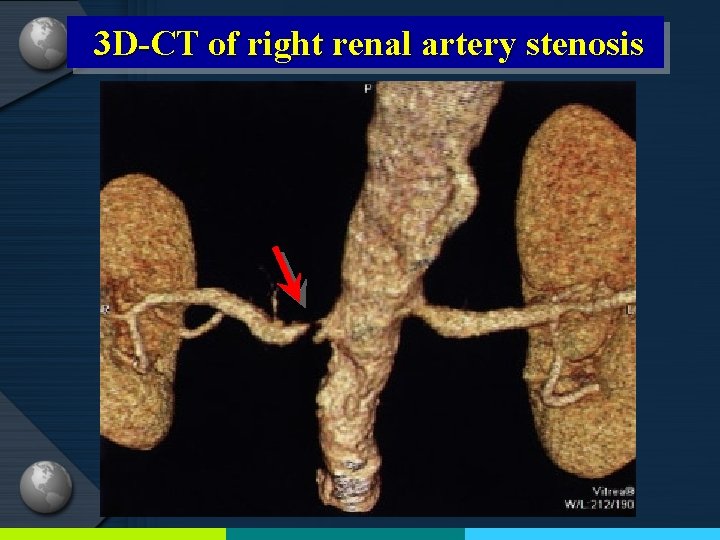
3 D-CT of right renal artery stenosis
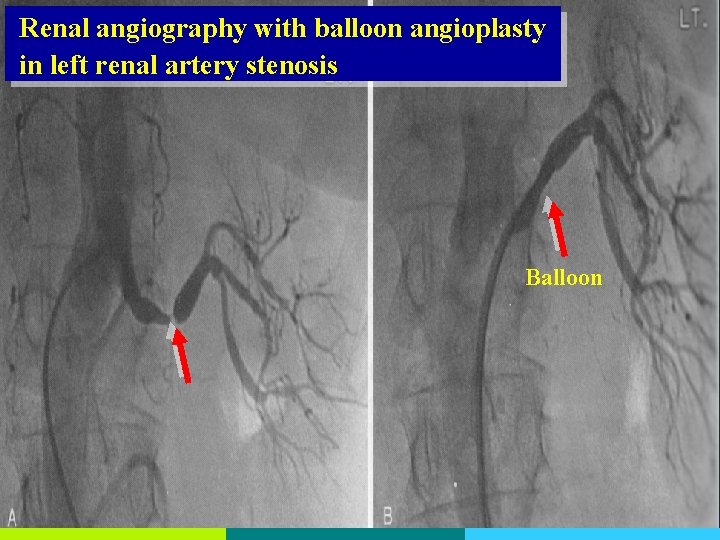
Renal angiography with balloon angioplasty in left renal artery stenosis Balloon
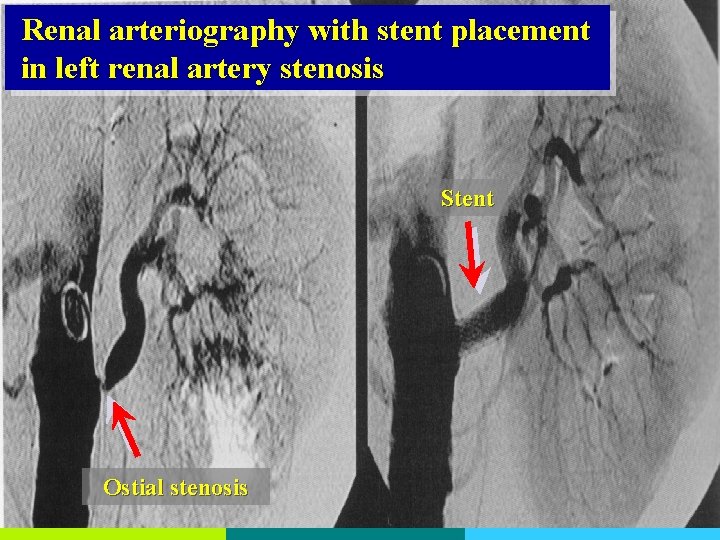
Renal arteriography with stent placement in left renal artery stenosis Stent Ostial stenosis
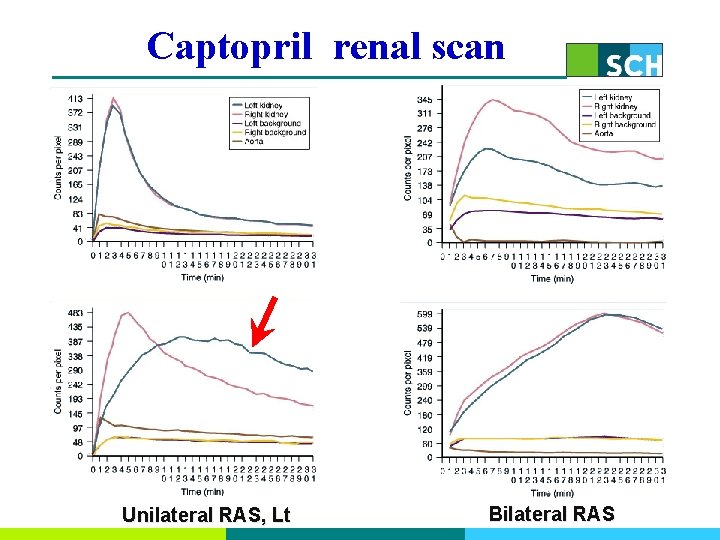
Captopril renal scan Unilateral RAS, Lt Bilateral RAS
죽종색전성 신장 질환 (Atheroembolic renal disease)
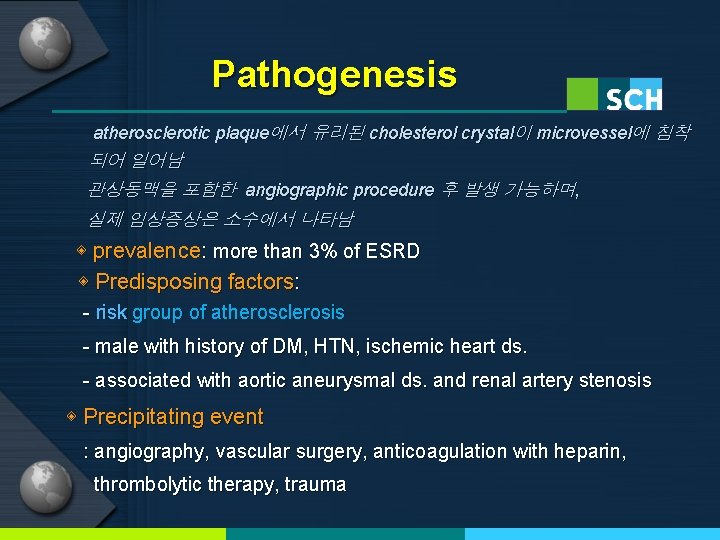
Pathogenesis atherosclerotic plaque에서 유리된 cholesterol crystal이 microvessel에 침착 되어 일어남 관상동맥을 포함한 angiographic procedure 후 발생 가능하며, 실제 임상증상은 소수에서 나타남 ◈ prevalence: more than 3% of ESRD ◈ Predisposing factors: - risk group of atherosclerosis - male with history of DM, HTN, ischemic heart ds. - associated with aortic aneurysmal ds. and renal artery stenosis ◈ Precipitating event : angiography, vascular surgery, anticoagulation with heparin, thrombolytic therapy, trauma
Coronary Angiography
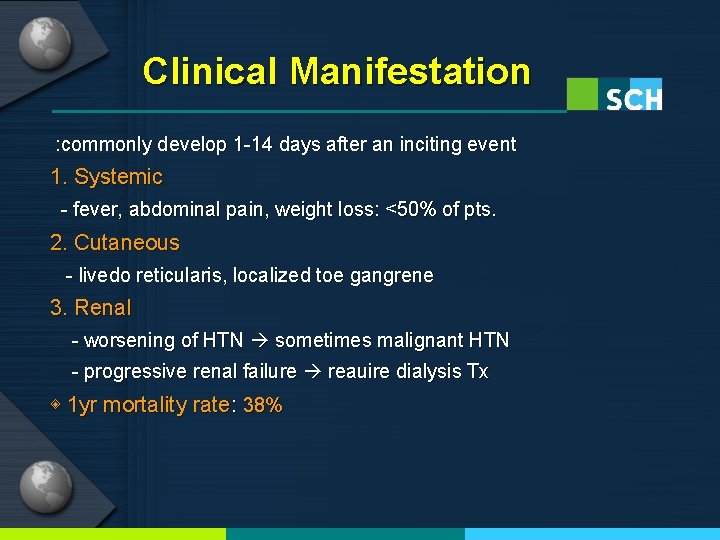
Clinical Manifestation : commonly develop 1 -14 days after an inciting event 1. Systemic - fever, abdominal pain, weight loss: <50% of pts. 2. Cutaneous - livedo reticularis, localized toe gangrene 3. Renal - worsening of HTN sometimes malignant HTN - progressive renal failure reauire dialysis Tx ◈ 1 yr mortality rate: 38%
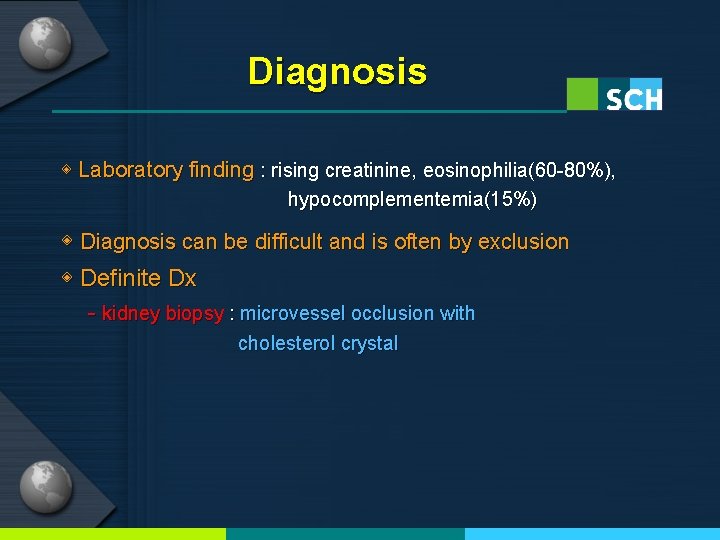
Diagnosis ◈ Laboratory finding : rising creatinine, eosinophilia(60 -80%), hypocomplementemia(15%) ◈ Diagnosis can be difficult and is often by exclusion ◈ Definite Dx - kidney biopsy : microvessel occlusion with cholesterol crystal
Management - No effective treatment - Withdrawal of anticoagulation - Statin Tx may improve outcome - Role of Embolic protection devices is unclear
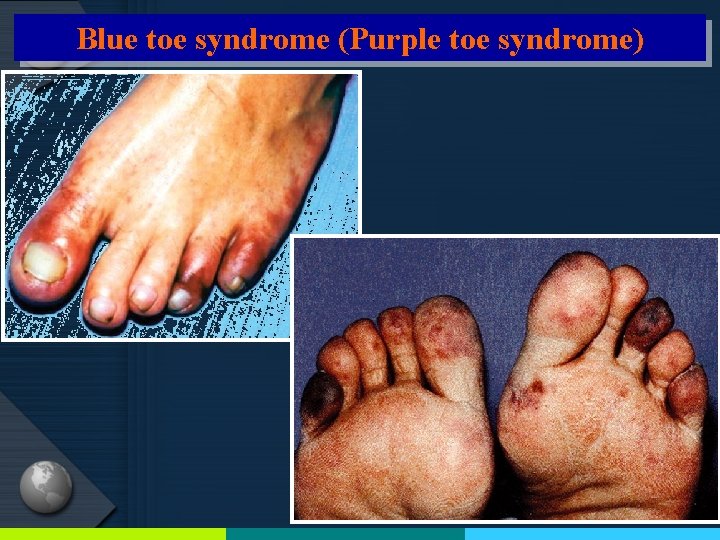
Blue toe syndrome (Purple toe syndrome)

Livedo reticularis
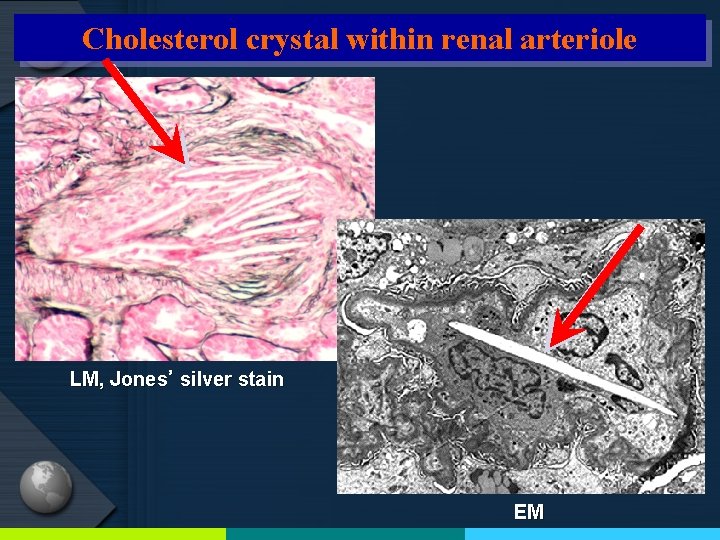
Cholesterol crystal within renal arteriole LM, Jones’ silver stain EM
혈전색전성 신장 질환 (Thromboembolic renal disease)
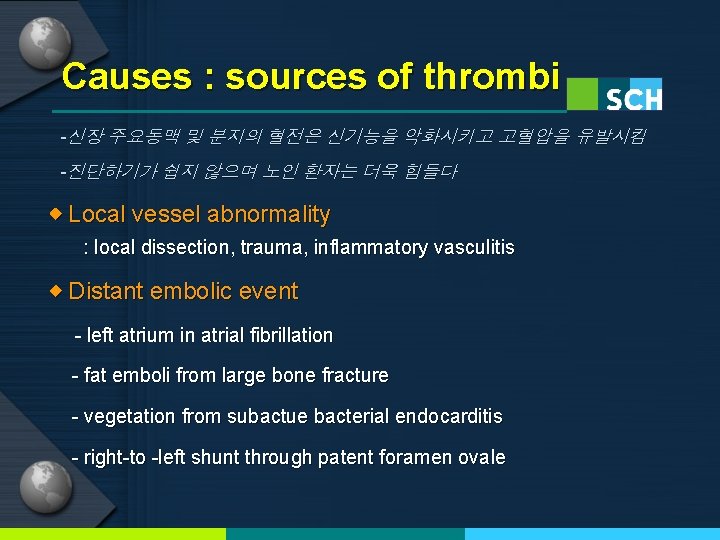
Causes : sources of thrombi -신장 주요동맥 및 분지의 혈전은 신기능을 악화시키고 고혈압을 유발시킴 -진단하기가 쉽지 않으며 노인 환자는 더욱 힘들다 ◈ Local vessel abnormality : local dissection, trauma, inflammatory vasculitis ◈ Distant embolic event - left atrium in atrial fibrillation - fat emboli from large bone fracture - vegetation from subactue bacterial endocarditis - right-to -left shunt through patent foramen ovale
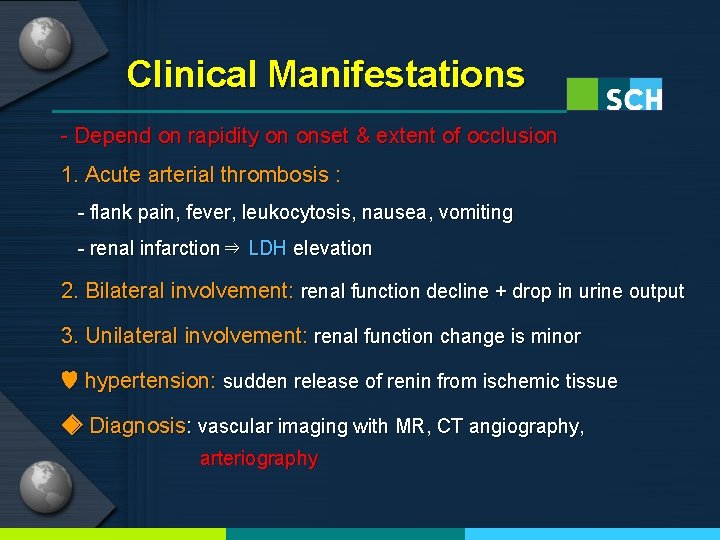
Clinical Manifestations - Depend on rapidity on onset & extent of occlusion 1. Acute arterial thrombosis : - flank pain, fever, leukocytosis, nausea, vomiting - renal infarction⇒ LDH elevation 2. Bilateral involvement: renal function decline + drop in urine output 3. Unilateral involvement: renal function change is minor ♥ hypertension: sudden release of renin from ischemic tissue ◈ Diagnosis: vascular imaging with MR, CT angiography, arteriography
Management ① surgical reconstruction ② anticoagulation ③ thrombolytic TX ④ endovascular procedure ⑤ supportive Tx with antihypertensive medication ◈ Choice of Tx depends on ① patient’s overall condition ② precipitating factor(local trauma or systemic illness) ③ magnitude of renal tissue and function at risk ④ likelihood of recurrent events in the future
Management 1. Unilateral thrombosis: -e. g. arterial dissection with thrombosis - supportive care with anticoagulation Tx 2. Acute bilateral thrombosis - can produce anuric renal failure - depending upon the precipitating event, surgical and thrombolytic therapy can restore kidney viability
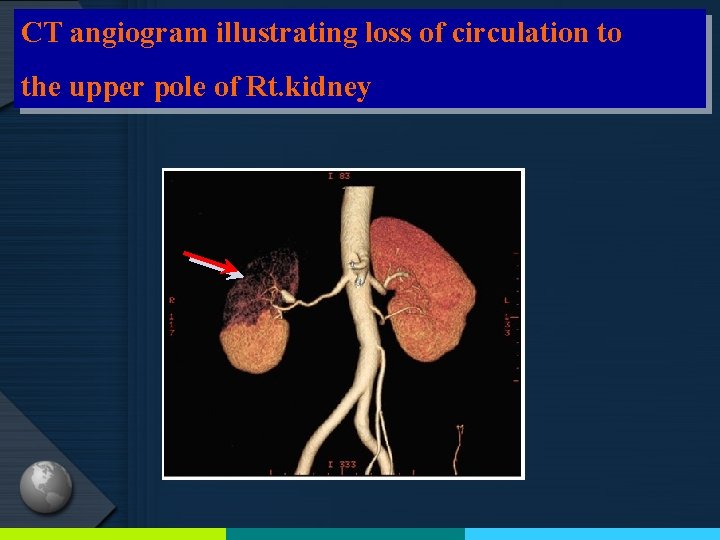
CT angiogram illustrating loss of circulation to the upper pole of Rt. kidney
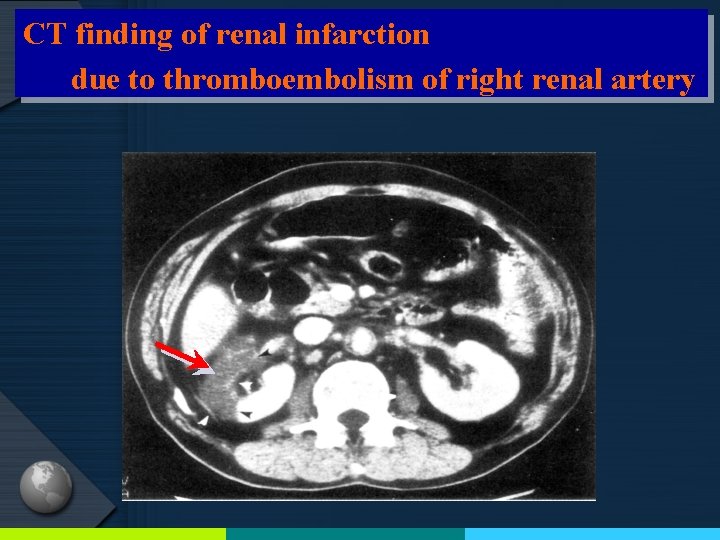
CT finding of renal infarction due to thromboembolism of right renal artery
미세혈관 손상과 고혈압 -동맥신장경화증- (Microvascular injury and Hypertension -Arterionephrosclerosis-)
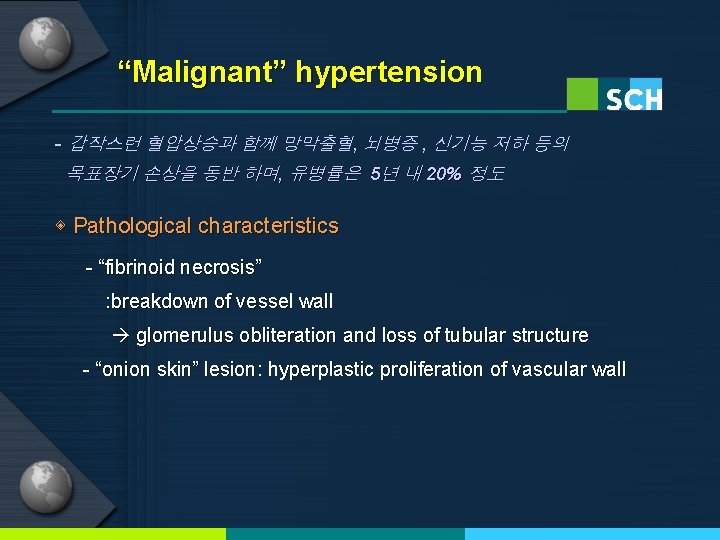
“Malignant” hypertension - 갑작스런 혈압상승과 함께 망막출혈, 뇌병증 , 신기능 저하 등의 목표장기 손상을 동반 하며, 유병률은 5년 내 20% 정도 ◈ Pathological characteristics - “fibrinoid necrosis” : breakdown of vessel wall glomerulus obliteration and loss of tubular structure - “onion skin” lesion: hyperplastic proliferation of vascular wall
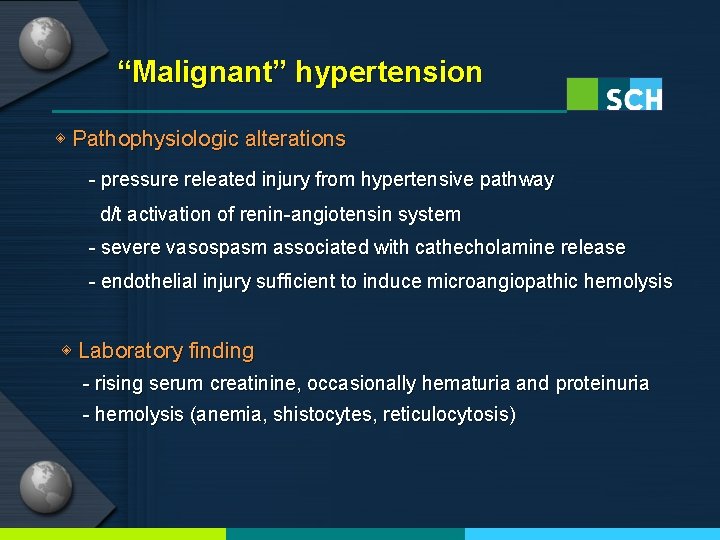
“Malignant” hypertension ◈ Pathophysiologic alterations - pressure releated injury from hypertensive pathway d/t activation of renin-angiotensin system - severe vasospasm associated with cathecholamine release - endothelial injury sufficient to induce microangiopathic hemolysis ◈ Laboratory finding - rising serum creatinine, occasionally hematuria and proteinuria - hemolysis (anemia, shistocytes, reticulocytosis)
“Malignant” hypertension ◈ Treatment - antihypertensive medication is mainstay therapy - effective BP reduction can improve vascular injury including microangiopathic hemolysis and renal dysfuction ◈ Epidemiology - 약물치료 실시 전: 1년 사망률>90% - 현재 5년 사망률: 50% - 의료서비스와 항고혈압 약물 사용이 힘든 지역에 호발 - 주로 혈압 치료 중이던 환자가 약물을 중단한 경우 발생
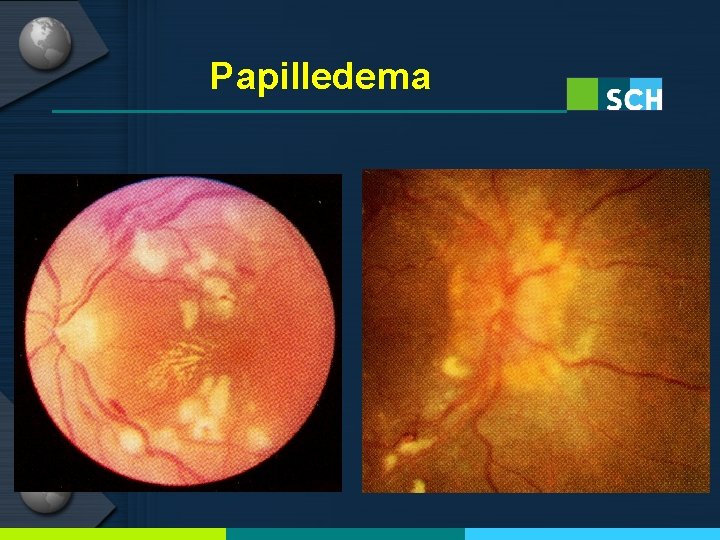
Papilledema
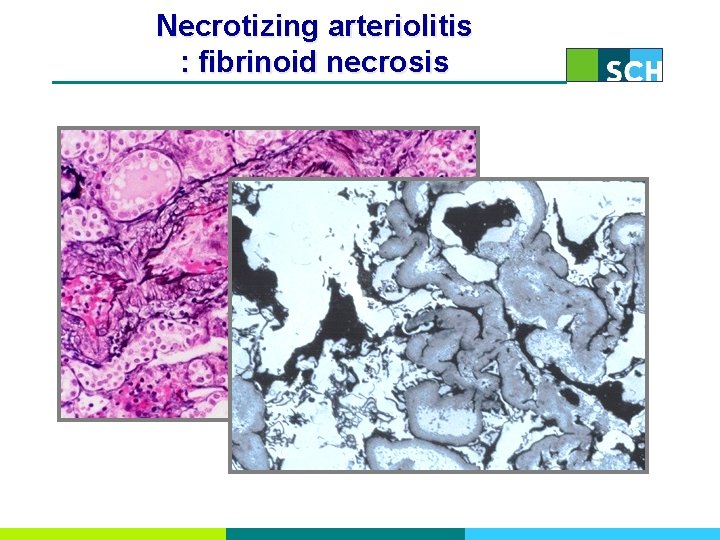
Necrotizing arteriolitis : fibrinoid necrosis
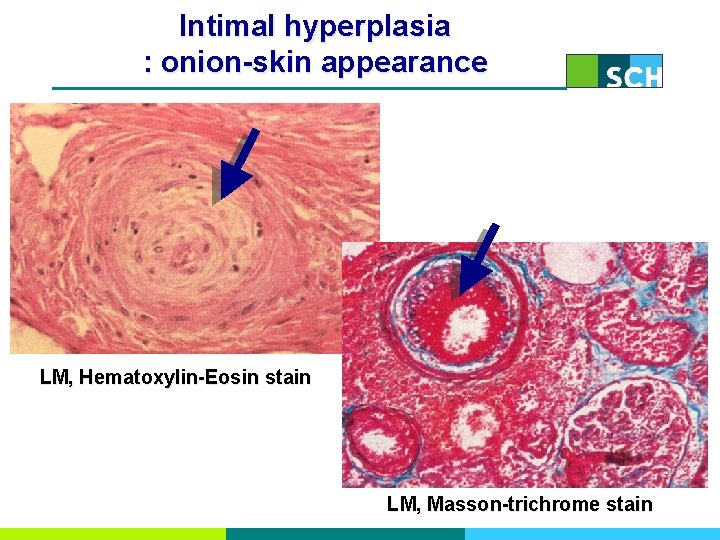
Intimal hyperplasia : onion-skin appearance LM, Hematoxylin-Eosin stain LM, Masson-trichrome stain
“Hypertensive nephrosclerosis” - 고혈압 환자는 혈압이 심하게 높지 않더라도 신장혈관에 작지만 영구적인 손상을 가져와 신기능 소실을 초래할 수 있음 - 특이 질병 없이 만성신부전에 이른 많은 환자가 고혈압이 원인 ◈ Clinical manifestation - retinal vessel change, LVH, BP elevation ◈ Pathologic characteristics - Hyaline arteriolosclerosis (afferent arteriolar thickening with deposition of eosinophilic material) ◈ Treatment - BP reduction does slow progression of proteinuric kidney ds. - does not alter the course of kidney dysfunction
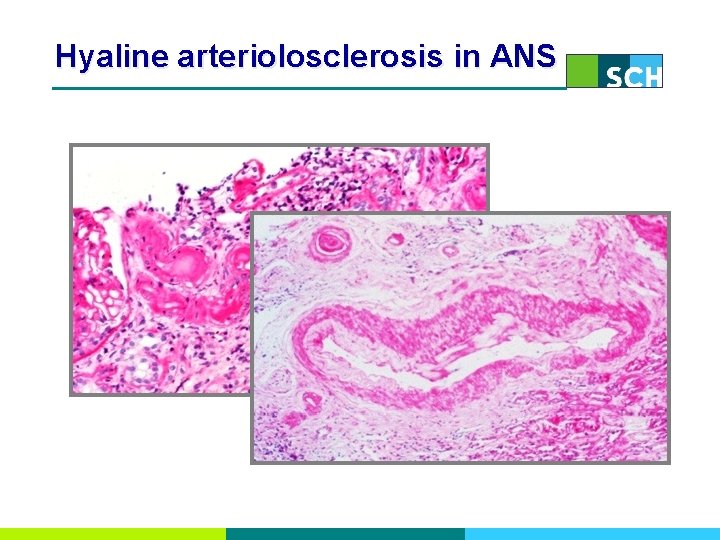
Hyaline arteriolosclerosis in ANS

혈전성 미세혈관병증 (Thrombotic Microangiopathy)
Thrombotic Microangiopathy - refer to injured endothelial cell that are thickened, swollen, detached mainly from arteriole or capillary - histologic result of microangiopathic hemolytic anemia(MAHA) - consume platelet and erythrocytes : characterized by thrombocytopenia and shistocytes
Thrombotic Microangiopathy ◈ disease entities - Thrombotic thrombocytopenic purpura (TTP) - Hemolytic uremic syndrome (HUS) - Malignant hypertension - Scleroderma renal crisis - Antiphospholipid syndrome - Preeclampsia/HELLP syndrome - HIV infection - Radiation nephropathy - Transplantation associated
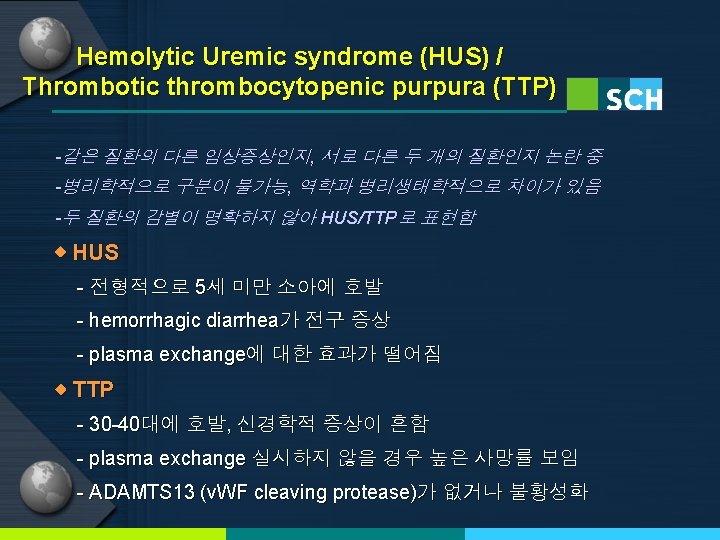
Hemolytic Uremic Syndrome (HUS) ① D+ HUS - MC type, associated with bacterial enteritis - typically affect young children (<5 yr) - preceded within a week by bloody diarrhea (>80%) - clinical manifestation: abdominal pain, vomiting, no fever lethargy, encephalopathy, seizure, cerebral infarct - pathogen: shiga toxin (verotoxin) produced by O 157: H 7 E. coli
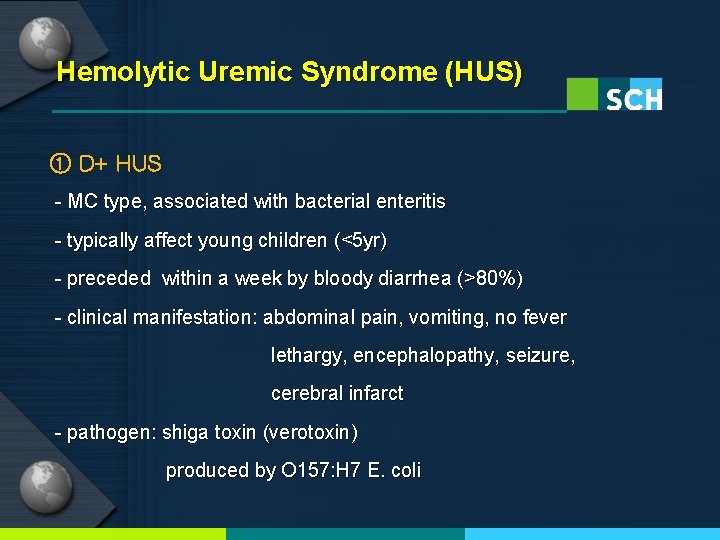
Hemolytic Uremic Syndrome (HUS) ② Atypical HUS - triggered by congenital complement dysregulation - low C 3 level: alternative pathway activation -factor H deficiency : MC cause linked to familial a. HUS ③ Autoimmune variant HUS

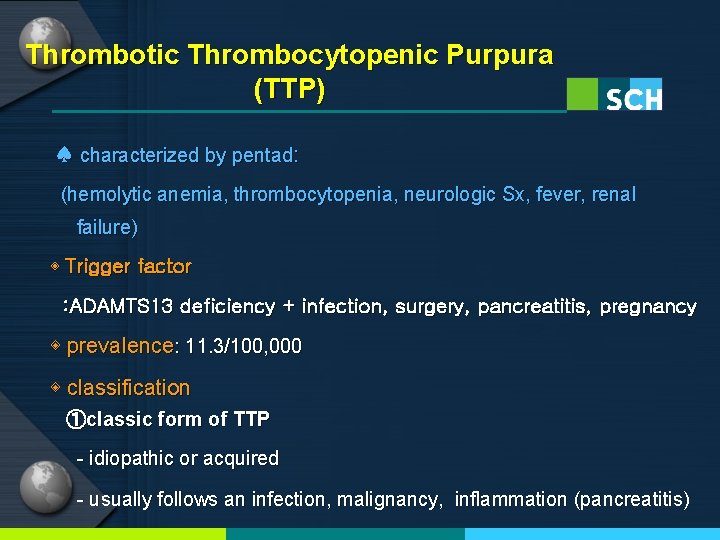
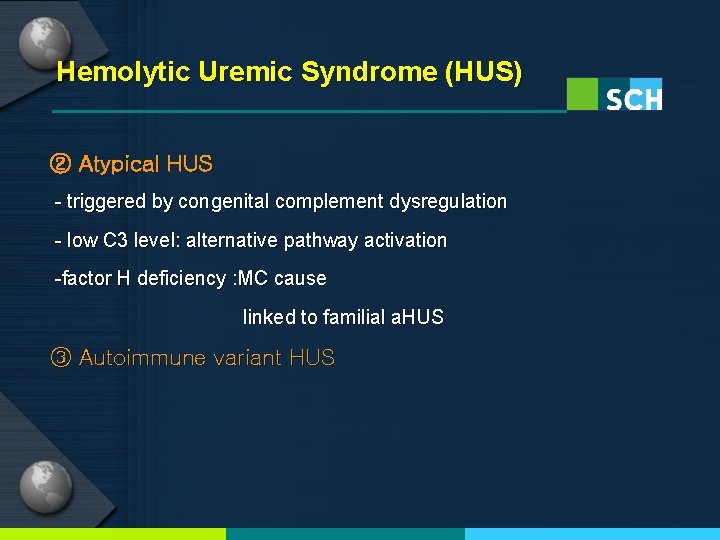
Thrombotic Thrombocytopenic Purpura (TTP) ♠ characterized by pentad: (hemolytic anemia, thrombocytopenia, neurologic Sx, fever, renal failure) ◈ Trigger factor : ADAMTS 13 deficiency + infection, surgery, pancreatitis, pregnancy ◈ prevalence: 11. 3/100, 000 ◈ classification ①classic form of TTP - idiopathic or acquired - usually follows an infection, malignancy, inflammation (pancreatitis)
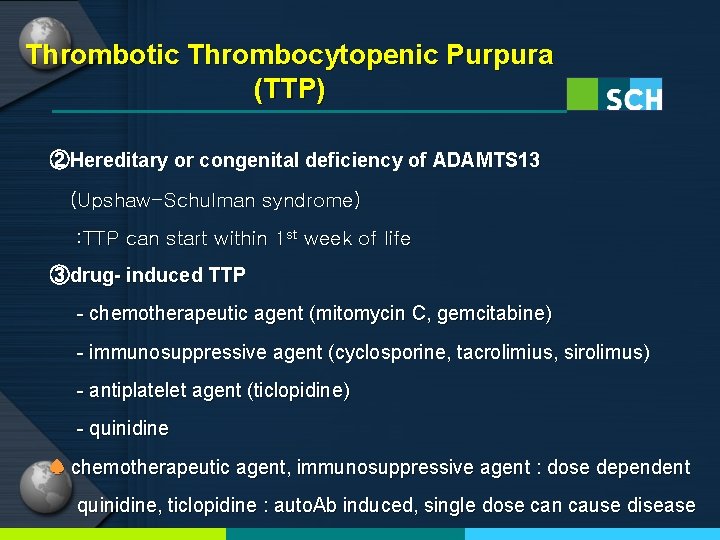
Thrombotic Thrombocytopenic Purpura (TTP) ②Hereditary or congenital deficiency of ADAMTS 13 (Upshaw-Schulman syndrome) : TTP can start within 1 st week of life ③drug- induced TTP - chemotherapeutic agent (mitomycin C, gemcitabine) - immunosuppressive agent (cyclosporine, tacrolimius, sirolimus) - antiplatelet agent (ticlopidine) - quinidine ♠ chemotherapeutic agent, immunosuppressive agent : dose dependent quinidine, ticlopidine : auto. Ab induced, single dose can cause disease
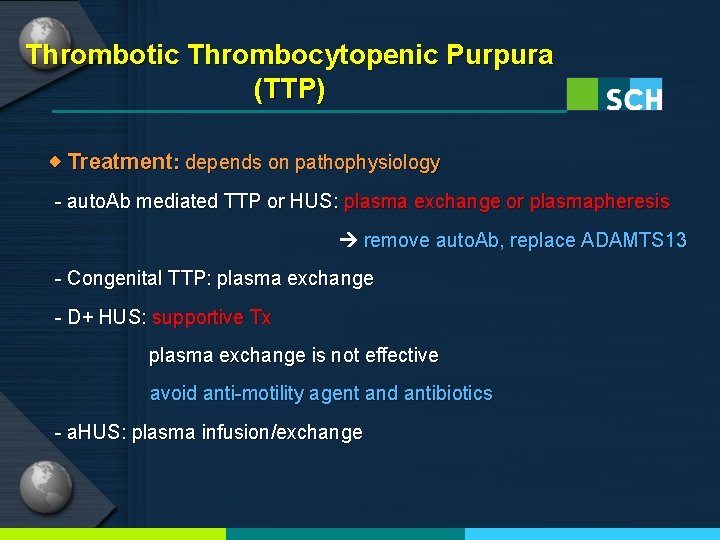
Thrombotic Thrombocytopenic Purpura (TTP) ◈ Treatment: depends on pathophysiology - auto. Ab mediated TTP or HUS: plasma exchange or plasmapheresis remove auto. Ab, replace ADAMTS 13 - Congenital TTP: plasma exchange - D+ HUS: supportive Tx plasma exchange is not effective avoid anti-motility agent and antibiotics - a. HUS: plasma infusion/exchange
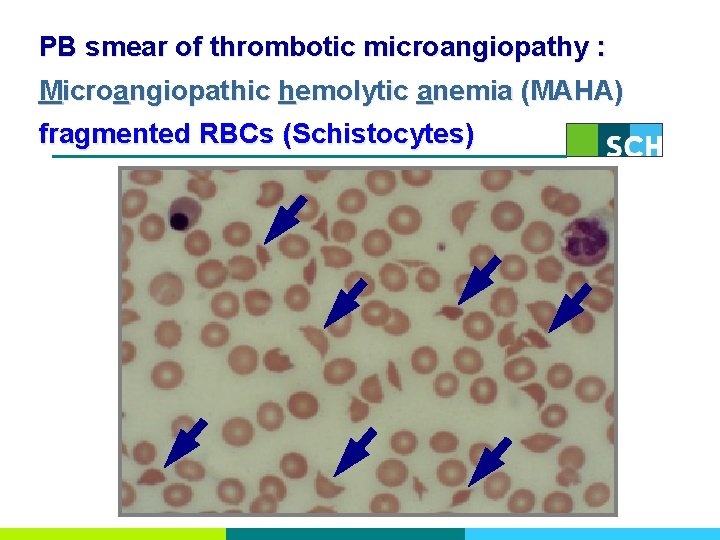
PB smear of thrombotic microangiopathy : Microangiopathic hemolytic anemia (MAHA) fragmented RBCs (Schistocytes)
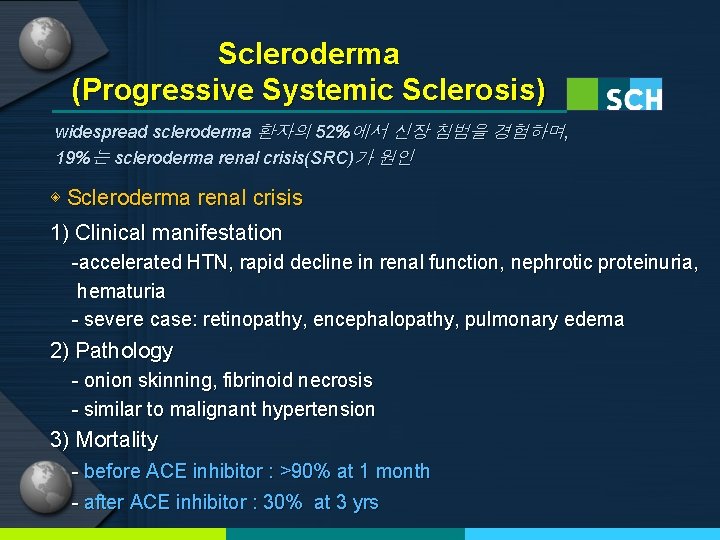
Scleroderma (Progressive Systemic Sclerosis) widespread scleroderma 환자의 52%에서 신장 침범을 경험하며, 19%는 scleroderma renal crisis(SRC)가 원인 ◈ Scleroderma renal crisis 1) Clinical manifestation -accelerated HTN, rapid decline in renal function, nephrotic proteinuria, hematuria - severe case: retinopathy, encephalopathy, pulmonary edema 2) Pathology - onion skinning, fibrinoid necrosis - similar to malignant hypertension 3) Mortality - before ACE inhibitor : >90% at 1 month - after ACE inhibitor : 30% at 3 yrs
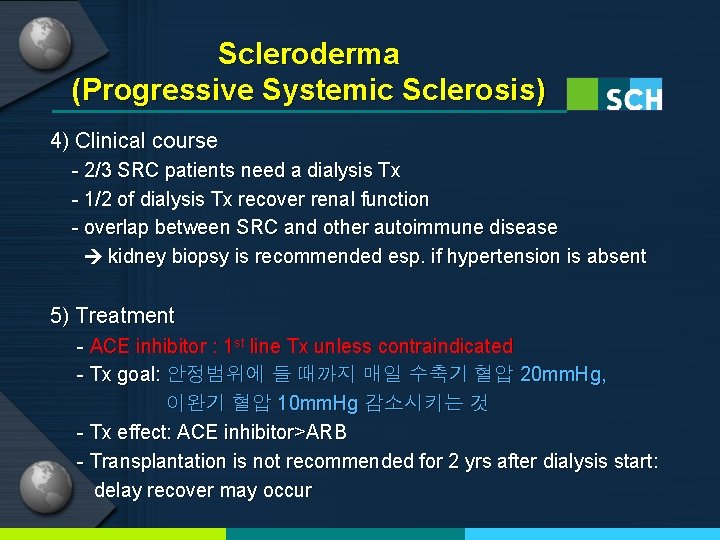
Scleroderma (Progressive Systemic Sclerosis) 4) Clinical course - 2/3 SRC patients need a dialysis Tx - 1/2 of dialysis Tx recover renal function - overlap between SRC and other autoimmune disease kidney biopsy is recommended esp. if hypertension is absent 5) Treatment - ACE inhibitor : 1 st line Tx unless contraindicated - Tx goal: 안정범위에 들 때까지 매일 수축기 혈압 20 mm. Hg, 이완기 혈압 10 mm. Hg 감소시키는 것 - Tx effect: ACE inhibitor>ARB - Transplantation is not recommended for 2 yrs after dialysis start: delay recover may occur
HELLP syndrome
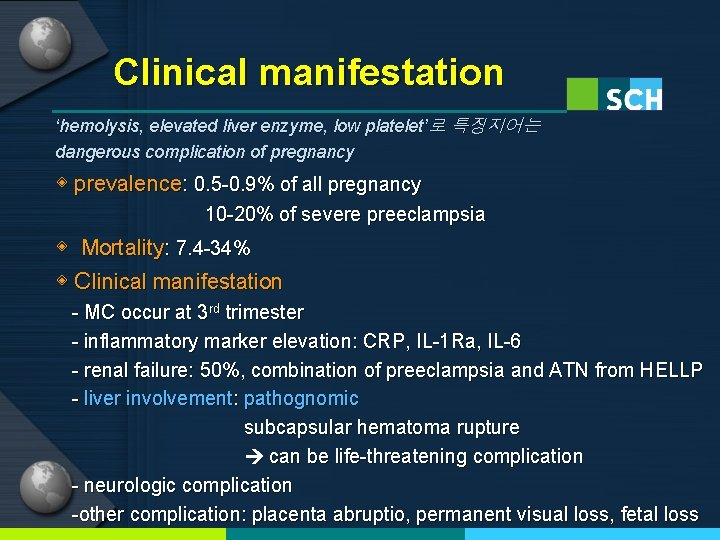
Clinical manifestation ‘hemolysis, elevated liver enzyme, low platelet’로 특징지어는 dangerous complication of pregnancy ◈ prevalence: 0. 5 -0. 9% of all pregnancy 10 -20% of severe preeclampsia ◈ Mortality: 7. 4 -34% ◈ Clinical manifestation - MC occur at 3 rd trimester - inflammatory marker elevation: CRP, IL-1 Ra, IL-6 - renal failure: 50%, combination of preeclampsia and ATN from HELLP - liver involvement: pathognomic subcapsular hematoma rupture can be life-threatening complication - neurologic complication -other complication: placenta abruptio, permanent visual loss, fetal loss
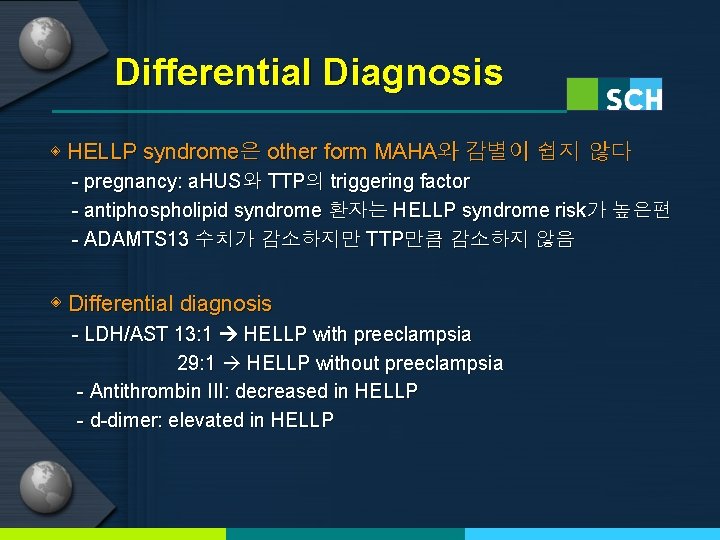
Differential Diagnosis ◈ HELLP syndrome은 other form MAHA와 감별이 쉽지 않다 - pregnancy: a. HUS와 TTP의 triggering factor - antiphospholipid syndrome 환자는 HELLP syndrome risk가 높은편 - ADAMTS 13 수치가 감소하지만 TTP만큼 감소하지 않음 ◈ Differential diagnosis - LDH/AST 13: 1 HELLP with preeclampsia 29: 1 HELLP without preeclampsia - Antithrombin III: decreased in HELLP - d-dimer: elevated in HELLP
Treatment ◈ Treatment - spontaneously recover after delivery - glucocorticoid: may decreased inflammatory marker - plasma exchange: hemolysis is refractory to glucocorticoid/delivery (esp. TTP can not be ruled out)
신정맥 혈전증 (Renal vein thrombosis)
Cause ① endothelial damage : homocystinuria, endovascular intervention, surgery ② venous stasis - dehydration (pediatrics) - renal vein compression or kinking (retroperitoneal fibrosis or abdominal neoplasm) ③ hypercoaglable state - antiphospholipid syndrome - nephrotic syndrome (membranous GN) - protein C, S and anti-thrombin deficiency - disseminated malignancy - oral contraceptive
Clinical manifestation - flank pain and tenderness, hematuria proteinuria may be silent rapid decline in renal function - identified during pulmonary embolism work up - left renal vein is more common, 2/3: bilateral
Diagnosis and Treatment ◈ Diagnosis - screening method: Doppler US> US alone - CT angiography: most sensitive (100% sensitivity) ◈ Treatment - main Tx: anticoagulation with therapy for underlying cause - endovascular thrombolysis: severe case - nephrectomy - vena cava filter: prevention of thrombus migration
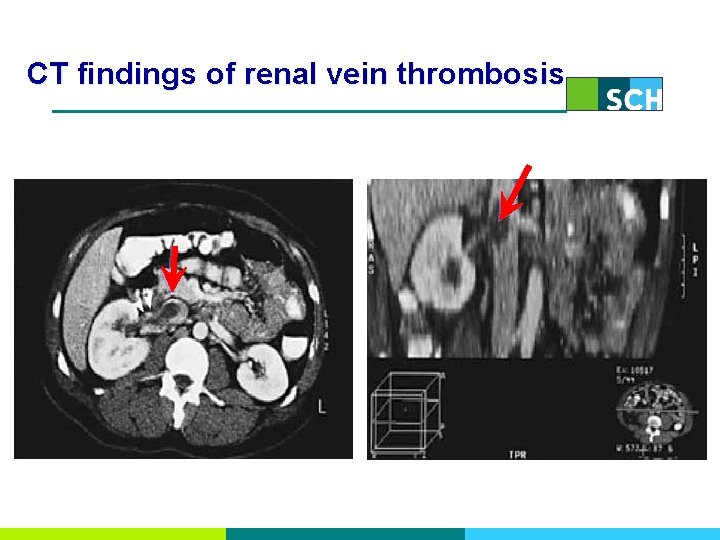
CT findings of renal vein thrombosis
- Slides: 89