Hypertension Pathogenesis Morphology of the Kidney DR KSHEERA




- Slides: 63
Hypertension – Pathogenesis & Morphology of the Kidney DR. KSHEERA CARIAPPA ASSISTANT PROFESSOR 7/9/16
HYPERTENSION DEFINITION: Hypertension, or high blood pressure (BP), is defined as a persistent systolic blood pressure (SBP) greater than or equal to 140 mm Hg, diastolic blood pressure (DBP) greater than or equal to 90 mm Hg, or current use of antihypertensive medication.
INTRODUCTION � Prevalence and vulnerability to complications of hypertension increases with age. � Major risk factors for atherosclerosis. � Cause cardiac hypertrophy, heart failure, multi-infarct dementia, aortic dissection and renal failure. � Remains asymptomatic until late in its course. � Even severely elevated pressures can be clinically silent for years.
UNDERSTANDING BLOOD PRESSURE �Clinically, blood pressure measurements mm of mercury (mm. Hg). �Ratio of systolic pressure over diastolic pressure (e. g. 120/80 mm. Hg).
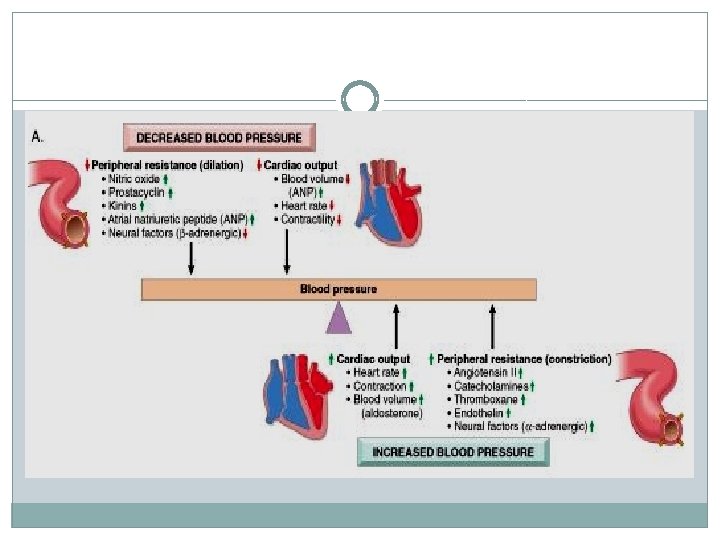

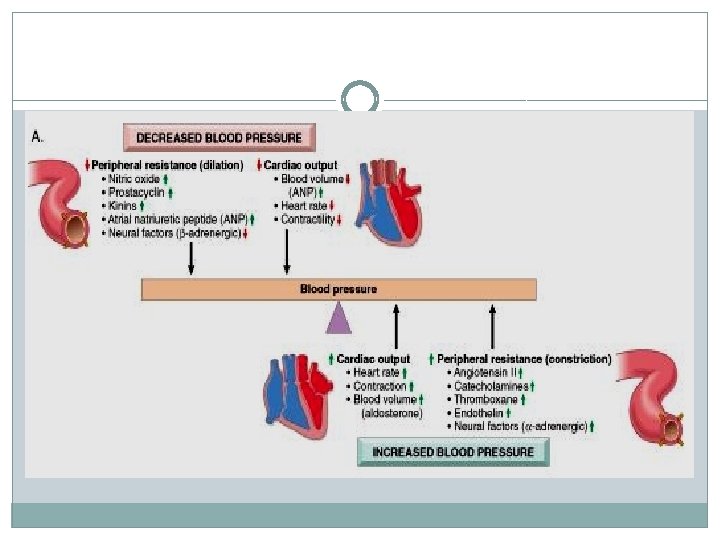
Blood pressure regulation
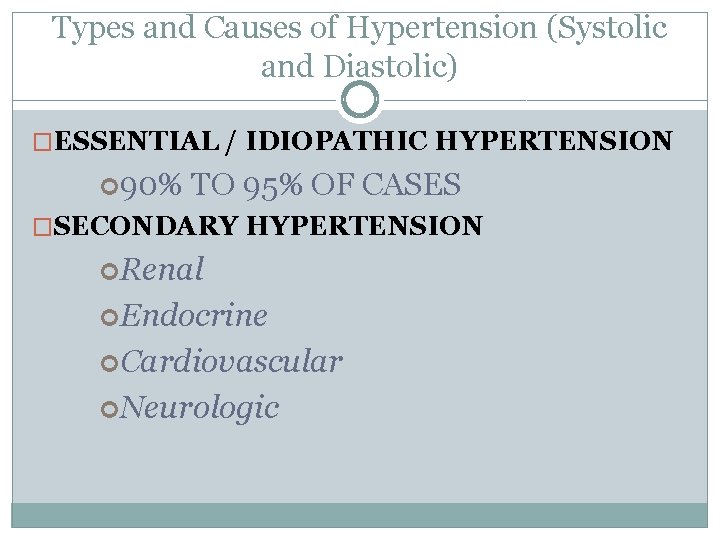
Types and Causes of Hypertension (Systolic and Diastolic) �ESSENTIAL / IDIOPATHIC HYPERTENSION 90% TO 95% OF CASES �SECONDARY HYPERTENSION Renal Endocrine Cardiovascular Neurologic
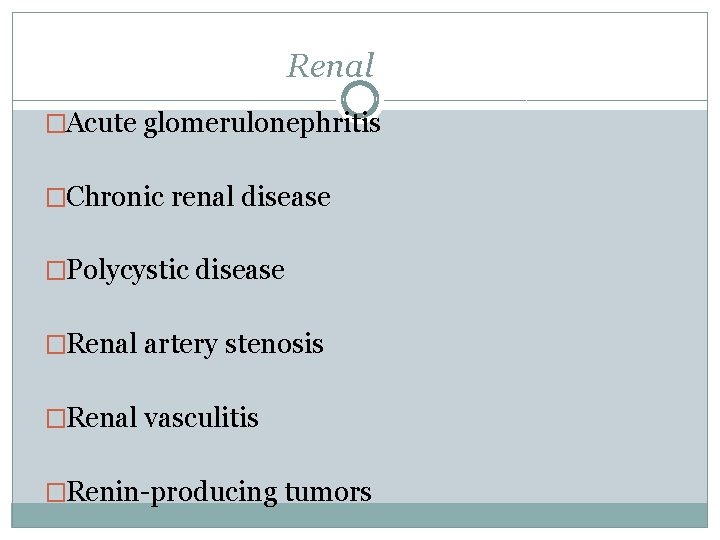
Renal �Acute glomerulonephritis �Chronic renal disease �Polycystic disease �Renal artery stenosis �Renal vasculitis �Renin-producing tumors
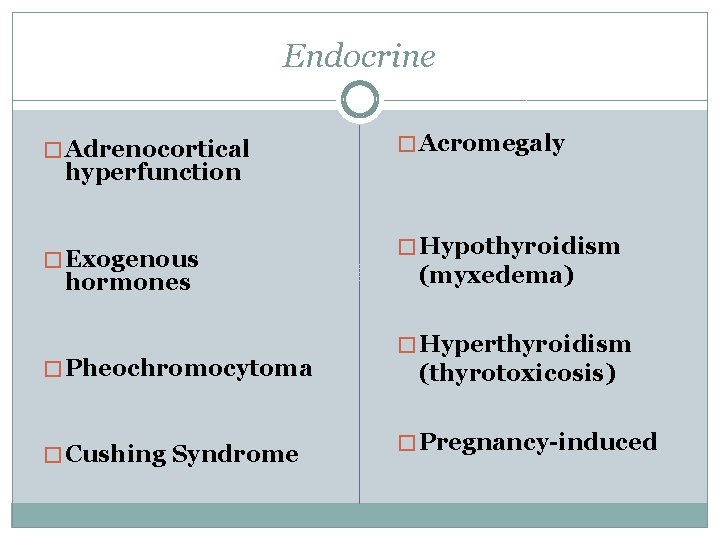
Endocrine � Adrenocortical hyperfunction � Exogenous hormones � Acromegaly � Hypothyroidism (myxedema) � Pheochromocytoma � Hyperthyroidism (thyrotoxicosis) � Cushing Syndrome � Pregnancy-induced
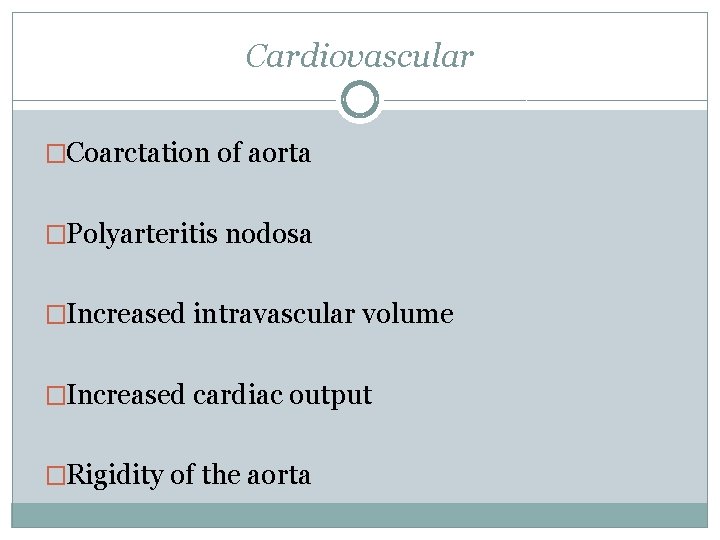
Cardiovascular �Coarctation of aorta �Polyarteritis nodosa �Increased intravascular volume �Increased cardiac output �Rigidity of the aorta
Neurologic �Psychogenic �Increased intracranial pressure �Sleep apnoea �Acute stress, including surgery
Essential hypertension � 95% �Idiopathic �Generally does not cause short-term problems.
Essential hypertension �When controlled Compatible with long life Asymptomatic �Unless �A myocardial infarction, cerebrovascular accident, or other complication supervenes.
Accelerated / Malignant Hypertension � 5% of hypertensives �Rapidly rising blood pressure �If untreated death within a year or two. �May develop in previously normotensives
Accelerated / Malignant Hypertension Systolic pressure >200 mm hg, Diastolic pressure >120 mm hg Renal failure Retinal hemorrhages and exudates With or without papilledema.
Mechanisms of Essential Hypertension
a complex, multifactorial disorder �Genetic factors �Reduced renal sodium excretion �Vasoconstrictive influences �Environmental factors �It is more likely that essential hypertension results from interactions of mutations or polymorphisms at several loci that influence blood pressure, with a variety of environmental factors (e. g. , stress, salt intake), rather than single gene disorders
Genetic factors �play a definite role �several single-gene disorders cause relatively rare forms of hypertension (and hypotension) by altering net sodium reabsorption in the kidney through several mechanisms
Gene defects affecting 1. Enzymes involved in Aldosterone Metabolism (e. g. , aldosterone synthase, 11β-hydroxylase, 17α -hydroxylase). � � increase in secretion of aldosterone increased salt and water reabsorption plasma volume expansion ultimately, hypertension
2. proteins that influence Sodium Reabsorption � Mutations in epithelial Na+ channel protein � increased distal tubular reabsorption of sodium induced by aldosterone � Liddle syndrome
�Inherited variations in BP may also depend on the cumulative effects of polymorphisms in several genes that affect blood pressure. �For example �variations in the genes encoding components of the reninangiotensin system
Reduced renal sodium excretion �may be a key initiating event in essential hypertension �may lead sequentially to an increase in fluid volume cardiac output peripheral vasoconstriction thereby elevating blood pressure.
Vasoconstrictive influences �increase peripheral resistance �chronic or repeated vasoconstrictive influences could cause thickening and rigidity of the involved vessels.

Environmental factors �can modify the impact of genetic determinants. Stress Obesity Smoking physical inactivity heavy consumption of salt
Pathogenesis of Secondary Hypertension
Renovascular Hypertension – 1 of 3 mechanisms 1. Activation of Renin-AT system a) Decreased CO or Renal artery stenosis causes � Decreased glomerular flow and pressure in the afferent arteriole of the glomerulus. (1) induces renin secretion initiating angiotensin II – mediated vasoconstriction increased peripheral resistance (2) increases aldosterone sodium reabsorption increase blood volume b) Primary hyperaldosteronism is one of the most common causes of secondary hypertension
2. Sodium and Water retention: further regulated by a) Release of Aldosterone b) Reduction in GFR - leading to proximal reabsorption of Sodium c) Release of ANF in response to volume expansion, causing increased GFR and inhibition of Sodium reabsorption 3. Release of Vasodepressor material : like Prostaglandins, urinary kallikrein-kinin system and Platelet activating factor.
VASCULAR PATHOLOGY IN HYPERTENSION
VASCULAR PATHOLOGY IN HYPERTENSION �Accelerates atherogenesis �Causes degenerative changes in the walls of large and medium arteries that can lead to • Aortic dissection and • Cerebrovascular hemorrhage.
Morphology �Two forms of small blood vessel disease: Hyaline arteriolosclerosis & Hyperplastic arteriolosclerosis.
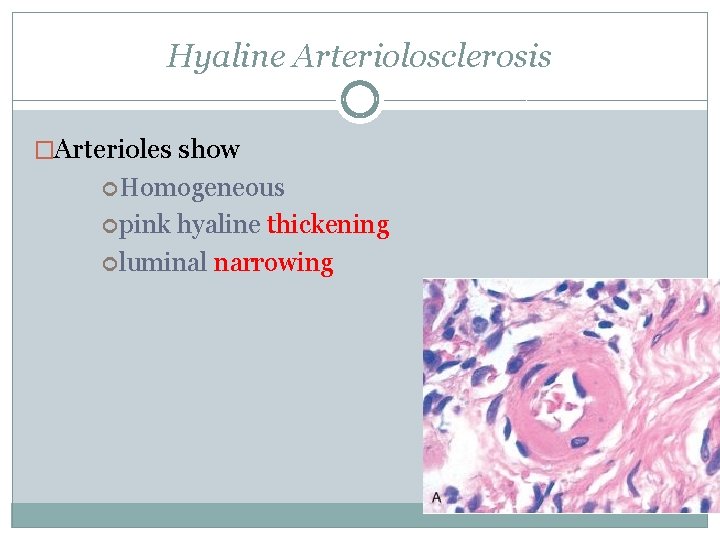
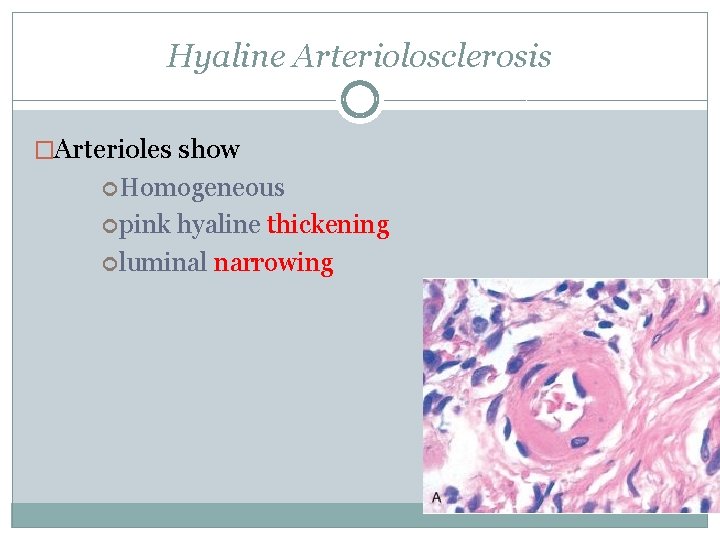
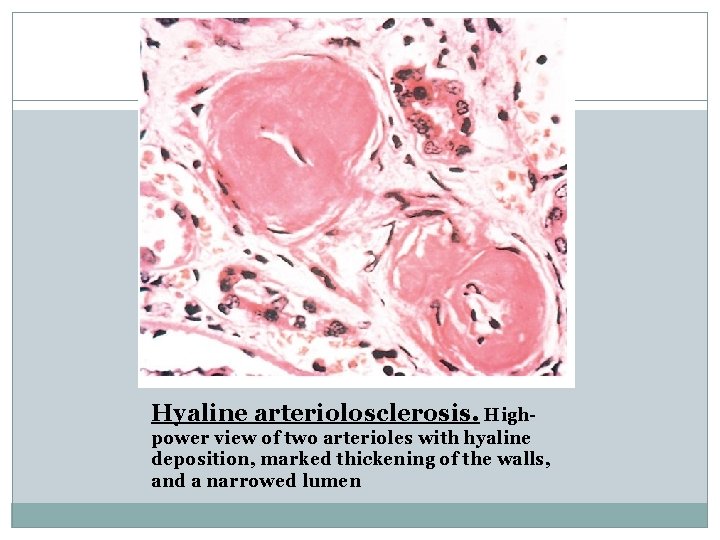
Hyaline Arteriolosclerosis �Arterioles show Homogeneous pink hyaline thickening luminal narrowing
Hyaline Arteriolosclerosis �Plasma protein leakage across injured endothelial cells �Increased smooth muscle cell matrix synthesis in response to chronic hemodynamic stress.
Hyaline Arteriolosclerosis �In Nephrosclerosis due to chronic hypertension, the arteriolar narrowing of hyaline arteriosclerosis causes �diffuse impairment of renal blood supply �glomerular scarring
Hyaline Arteriolosclerosis �Vessels of elderly persons (either normo- or hypertensive) �Diabetic microangiography
Morphology �Two forms of small blood vessel disease: Hyaline arteriolosclerosis & Hyperplastic arteriolosclerosis.

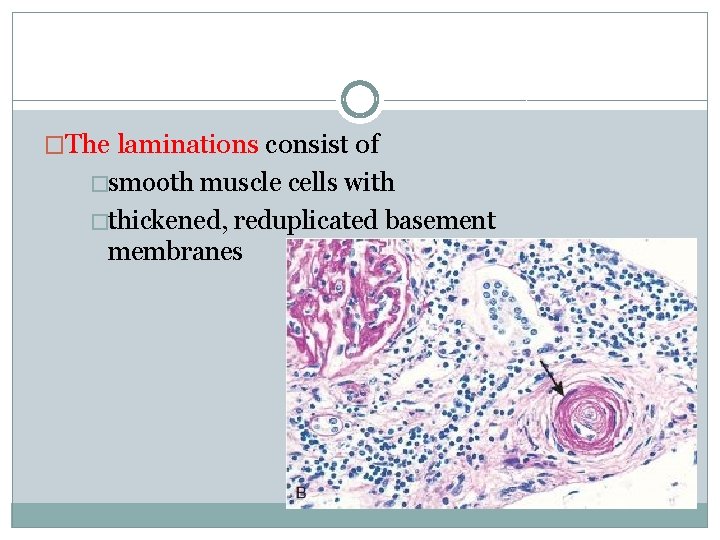
Hyperplastic Arteriolosclerosis. �in severe (malignant) hypertension �vessels exhibit “onion-skin lesions, ” �characterized by �concentric �laminated thickening of the walls and �luminal narrowing
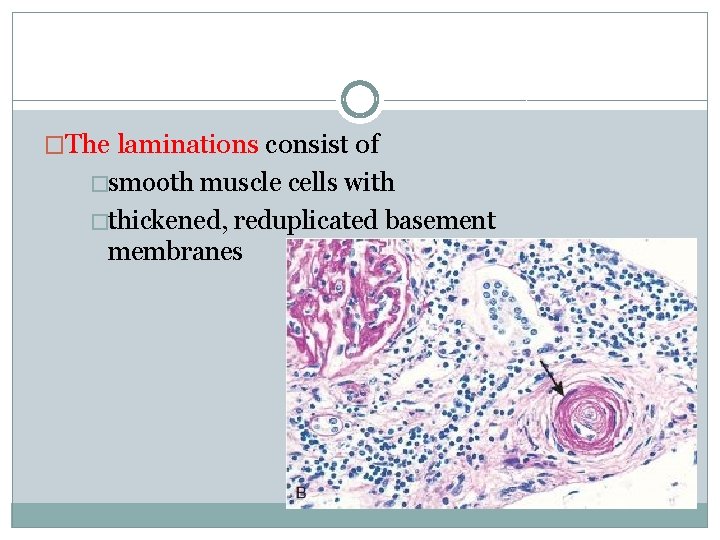
�The laminations consist of �smooth muscle cells with �thickened, reduplicated basement membranes
�In malignant hypertension they are accompanied by �fibrinoid deposits & �vessel wall necrosis (necrotizing arteriolitis), particularly in the kidney.
KIDNEY 1. BENIGN NEPHROSCLEROSIS �Describes Kidney in the benign phase of Hypertension �It is the most common renal disease in persons > 60 years of age �Severity increases in the presence of Diabetes
KIDNEY - BENIGN NEPHROSCLEROSIS � Renal pathology associated with sclerosis of renal arterioles and small arteries. � Focal ischemia of parenchyma supplied by vessels with thickened walls narrowed lumens. 1. Parenchymal effects: ü glomerulosclerosis reduction in functional renal mass ü chronic tubulointersititial injury.
BENIGN NEPHROSCLEROSIS 2. Vascular changes Two processes participate in the arterial lesions: � Medial and intimal thickening: -- due to smooth muscle proliferation in response to hemodynamic changes, aging, genetic defects, or combination of these. � Hyaline deposition in arterioles: -- extravasation of plasma proteins through injured endothelium -- increased deposition of basement membrane matrix.
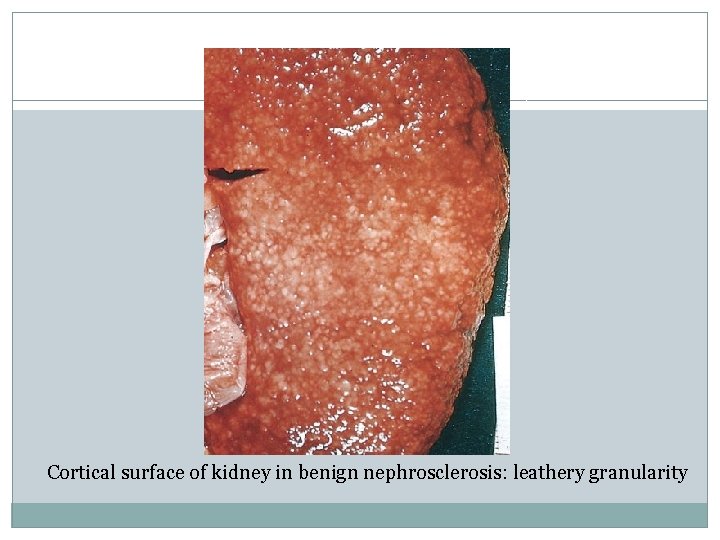
BENIGN NEPHROSCLEROSIS Morphology: Kidneys : �B/L kidneys reduced in size, �Average weight between 110 and 130 gm. �Cortical surfaces fine, even granularity that resembles grain leather. �Loss of mass due to cortical V – shaped scarring and shrinking.
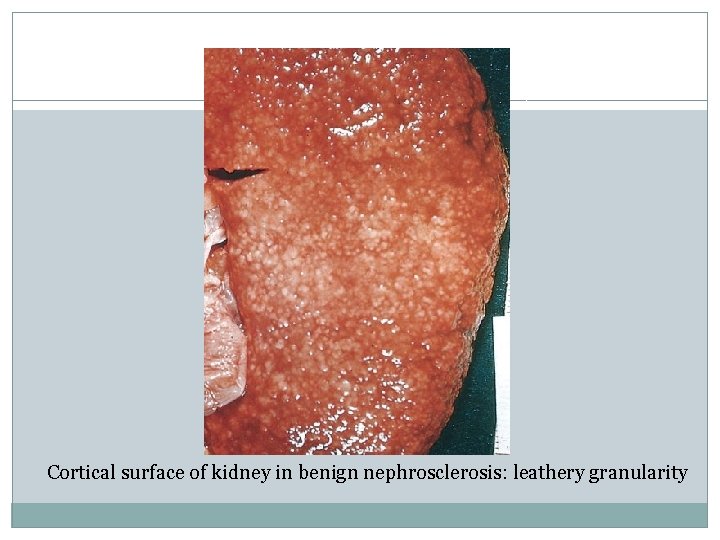
Cortical surface of kidney in benign nephrosclerosis: leathery granularity
DDs for Granular/ Small Contracted Kidney 1. 2. 3. 4. 5. 6. Chronic GN (Granular Glomerular scars) Chronic Pyelonephritis (U shaped Uneven scars) & Benign Nephrosclerosis ( V shaped Vascular scars). Other rare causes are Amyloidosis of kidney Myeloma Kidney and Diabetic Nephropathy
BENIGN NEPHROSCLEROSIS On histologic examination: �Thickening and hyalinization of the walls (hyaline arteriolosclerosis) narrowing of the lumens of arterioles and small arteries. �Corresponding to the fine surface granulations ü microscopic subcapsular scars ü sclerotic glomeruli and tubular dropout ü alternating with better preserved parenchyma.
BENIGN NEPHROSCLEROSIS �Interlobular and arcuate arteries show fibroelastic hyperplasia narrow the lumen ü medial hypertrophy ü reduplication of the elastic lamina ü increased myofibroblastic tissue in the intima. �Vascular narrowing patchy ischemic atrophy consisting of: (1) foci of tubular atrophy and interstitial fibrosis (2) variety of glomerular alterations.
BENIGN NEPHROSCLEROSIS �Glomerular changes: ü collapse of the GBM ü deposition of collagen within the Bowman space ü periglomerular fibrosis ü total sclerosis of glomeruli. �Ischemic changes are pronounced and affect large areas of parenchyma produce regional scars.
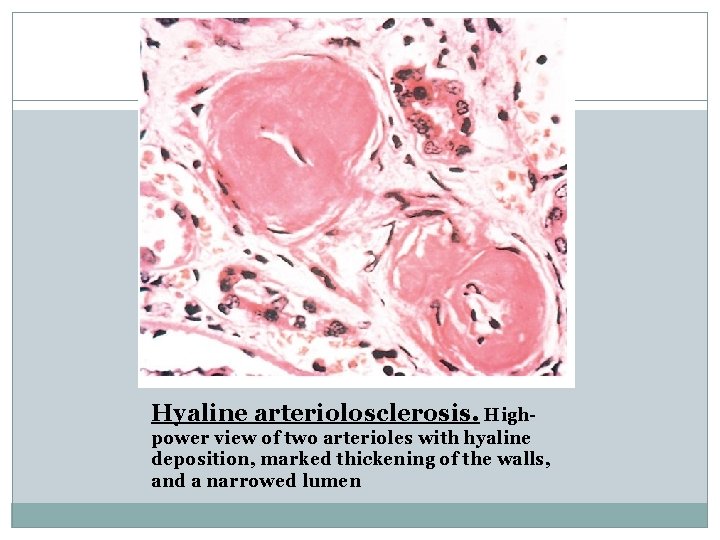
Hyaline arteriolosclerosis. Highpower view of two arterioles with hyaline deposition, marked thickening of the walls, and a narrowed lumen
CLINICAL FEATURES �Elevated BP with Headaches, dizziness, palpitation �Eye ground changes but without papilloedema �RFT and Urine analysis is Normal in early stages �Mild proteinuria with hyaline or granular casts in long standing cases
2. MALIGNANT NEPHROSCLEROSIS �Renal disease in Malignant or accelerated Hypertension �Rare, usually in 5% cases or pre-existing Benign HT Or in those with Secondary HT, with known causes like Chronic Renal diseases. �Pure form also occurs and seen at a younger age with male preponderance
MALIGNANT HYPERTENSION AND ACCELERATED NEPHROSCLEROSIS Pathogenesis: � Basis is unclear, following sequence of events is suggested. � Initial insult vascular damage to the kidneys. � Might result from: ü long-standing benign hypertension, with eventual injury to the arteriolar walls ü de novo from arteritis, a coagulopathy, or some injury causing acute exacerbation of the hypertension.
MALIGNANT HYPERTENSION AND ACCELERATED NEPHROSCLEROSIS � Increased permeability of the small vessels to fibrinogen & other plasma proteins endothelial injury focal death of cells of vascular wall platelet deposition. � Appearance of fibrinoid necrosis of arterioles and small arteries, swelling of the vascular intima & intravascular thrombosis. � Mitogenic factors from platelets (e. g. , PDGF), plasma, and other cells hyperplasia of intimal smooth muscle of vessels hyperplastic arteriolosclerosis further narrowing of the lumens. � Kidneys become markedly ischemic.
MALIGNANT HYPERTENSION AND ACCELERATED NEPHROSCLEROSIS �Severe involvement of the renal afferent arterioles renin-angiotensin system receives a powerful stimulus. �Self-perpetuating cycle angiotensin II intrarenal vasoconstriction renal ischemia renin secretion. �Other vasoconstrictors (e. g. , endothelin) and loss of vasodilators (nitric oxide) may also contribute to vasoconstriction. � Aldosterone levels are also elevated salt retention elevation of blood pressure.
MALIGNANT HYPERTENSION AND ACCELERATED NEPHROSCLEROSIS MORPHOLOGY: Gross: � Size of kidney depends on the duration and severity of hypertensive disease. �Rupture of arterioles or glomerular capillaries small, pinpoint petechial hemorrhages appear on cortical surface “flea-bitten” appearance.
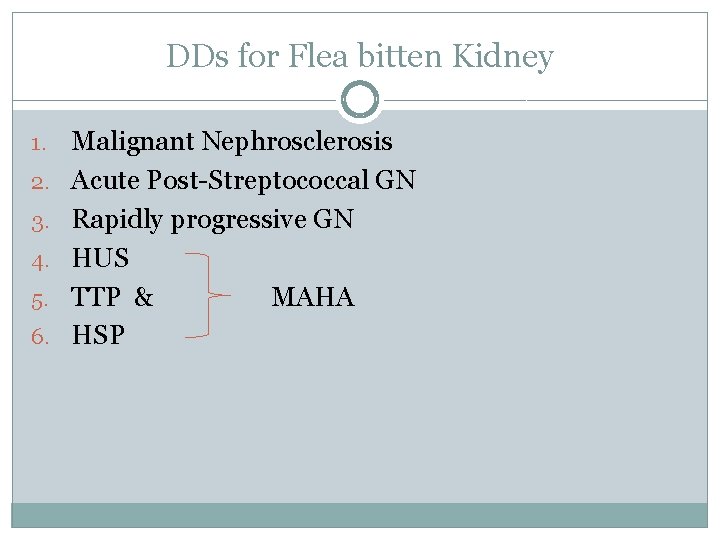
DDs for Flea bitten Kidney 1. 2. 3. 4. 5. 6. Malignant Nephrosclerosis Acute Post-Streptococcal GN Rapidly progressive GN HUS TTP & MAHA HSP
MALIGNANT HYPERTENSION AND ACCELERATED NEPHROSCLEROSIS �Histologic alterations characterize both vascular and parenchymal changes - Parenchymal changes include tubular loss, fine interstitial fibrosis and foci of infarction necrosis. - Vascular changes in malignant hypertension: 1. Fibrinoid necrosis of arterioles 2. Hyperplastic arteriolitis
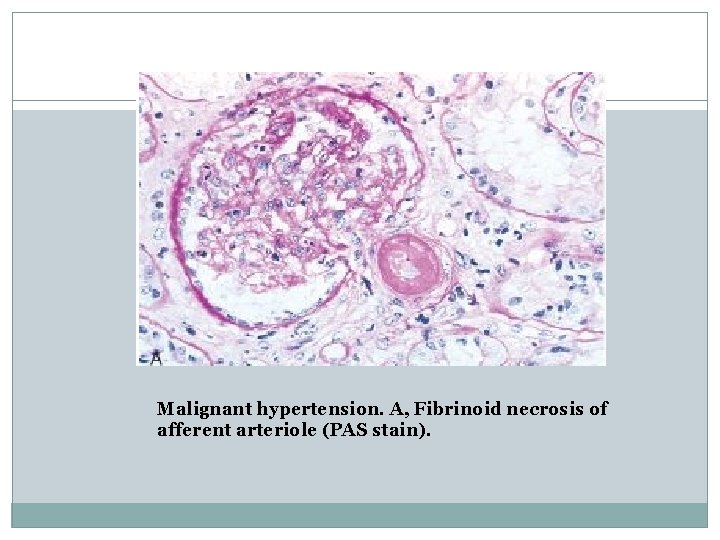
1. FIBRINOID NECROSIS OF ARTERIOLES: � Eosinophilic granular change in blood vessel wall, which stains positively for fibrin by histochemical or immunofluorescence techniques. � Represents an acute event. � Accompanied by limited inflammatory infiltrate within the wall, but prominent inflammation is not seen. � Sometimes glomeruli become necrotic and infiltrated with neutrophils & glomerular capillaries may thrombose.
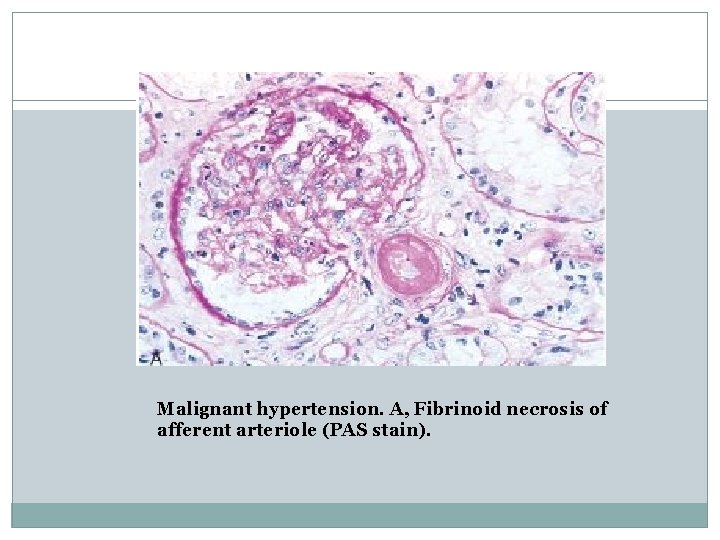
Malignant hypertension. A, Fibrinoid necrosis of afferent arteriole (PAS stain).
2. HYPERPLASTIC ARTERIOLITIS: � Interlobular arteries and arterioles intimal thickening Onion-skinning because of its concentric appearance. � Correlates well with renal failure in malignant hypertension. � Superimposed intraluminal thrombosis. � Arteriolar and arterial lesions narrowing of all vascular lumens ischemic atrophy & infarction distal to the abnormal vessels.

Malignant hypertension. Hyperplastic arteriolitis (onion-skin lesion).
CLINICAL FEATURES �BP 200/140 mm. Hg or higher �Headache, dizziness and vision impairment �Papilloedema is characteristic �U/A shows hematuria & proteinuria �RFT shows deterioration �Azotemia and uraemia develop if untreated �Approx 90% pts die within 1 yr from Uremia, CHF and CVAs.
REFERENCES: �Robbins and Cotran: Pathologic basis of disease-8 th edition. �Harrison’s: Principles of internal medicine 17 th edition. �Internet sources
THANK YOU