Hypertension Definition Hypertension is defined as a systolic




- Slides: 19
Hypertension
Definition • Hypertension is defined as a systolic blood pressure greater than 140 mm Hg and a diastolic pressure greater than 90 mm Hg, based on two or more measurements. Blood pressure can be classified as follows: • Normal: systolic less than 120 mm Hg; diastolic less than 80 mm Hg • Prehypertension: systolic 120 to 139 mm Hg; diastolic 80 to 89 mm Hg • Stage 1: systolic 140 to 159 mm Hg; diastolic 90 to 99 mm Hg • Stage 2: systolic 160 mm Hg; diastolic 100 mm Hg
Key points • Hypertension is a major risk factor for: • Atherosclerotic cardiovascular disease, • HF, • CVA, and • RF. • Hypertension carries the risk for premature morbidity or mortality, which increases as systolic and diastolic pressures rise. • Prolonged HTN damages blood vessels in target organs (heart, kidneys, brain, and eyes).
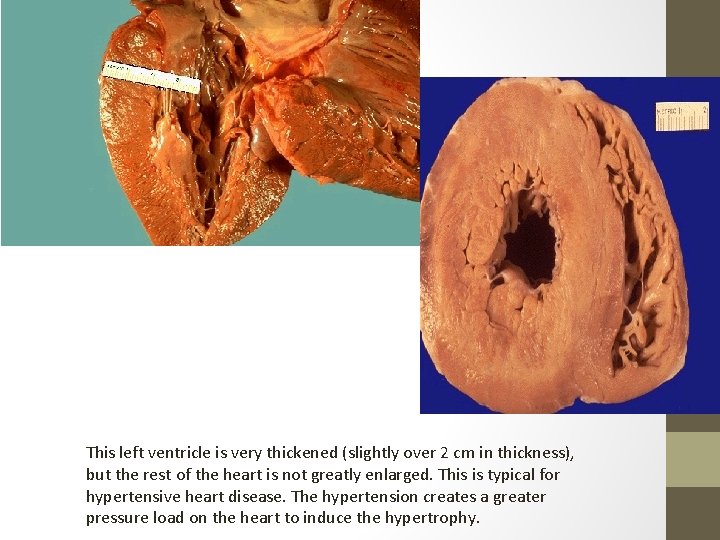
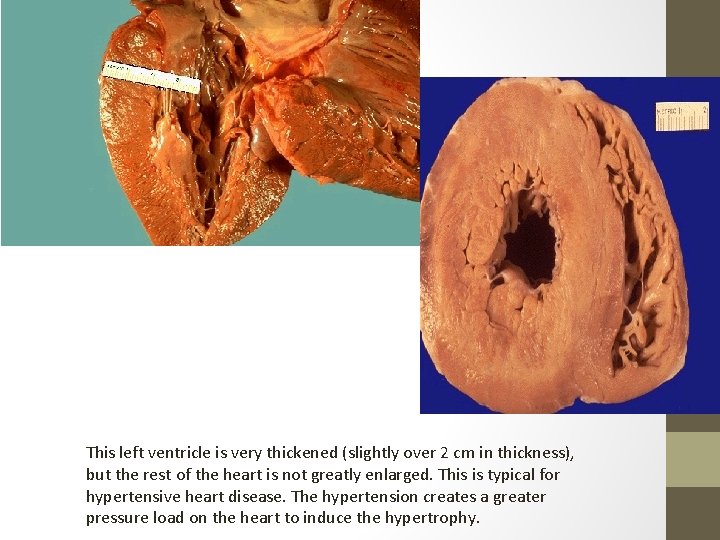
This left ventricle is very thickened (slightly over 2 cm in thickness), but the rest of the heart is not greatly enlarged. This is typical for hypertensive heart disease. The hypertension creates a greater pressure load on the heart to induce the hypertrophy.
Hypertension and Diabetes • Hypertension co-exists with type II in about 40% at age 45 rising to 60% at age 75. • 70% of type II patients die from cardio-vascular disease. • At least 60% of patients will require 2 or 3 antihypertensive agents to achieve tight control.
Key points • Bp is regulated by four bodily mechanisms: • Arterial baroreceptors. • Baroreceptors are located in the carotid sinus, aorta, and left ventricle. • They control BP by altering the heart rate and/or causing • • • vasoconstriction or vasodilation. Regulation of body-fluid volume. Kidneys either retain fluid when the client is hypotensive or excrete fluid when the client is hypertensive. Renin-angiotensin system. Angiotensin II vasoconstricts and controls aldosterone release, which causes the kidneys to reabsorb sodium and inhibit fluid loss. Vascular autoregulation. • This maintains consistent levels of tissue perfusion.
Types of HTN 1. Essential HTN (primary hypertension), there is no known cause. 2. Secondary HTN may be caused by certain disease states such as renal disease, , hyperaldosteronism and coarctation of the aorta 3. Iatrogenic HTN, as a side effect of some medications
Essential (Primary) Hypertension • 90% - 95% of HTN is essential (primary) hypertension, which has no identifiable medical cause. • 1 ry HTN appears to be a multifactorial, polygenic condition. • An increase in peripheral resistance and/or cardiac output must occur secondary to increased sympathetic stimulation before occurrence of HTN
Risk Factors for Essential Hypertension • Positive family history • Excessive sodium intake • Sedentary life • Obesity • High alcohol consumption • Smoking • Hyperlipidemia • Stress

Risk Factors for Secondary Hypertension • Renal disease • Cushing’s disease (excessive glucocorticoid secretion) • Primary aldosteronism (causes hypertension and hypokalemia) • Pheochromocytoma (a tumor of the sympathetic nervous system or adrenal medulla, that produces excess norepinephrine and causes hypertension, headaches, nausea, etc) • Brain tumors, encephalitis
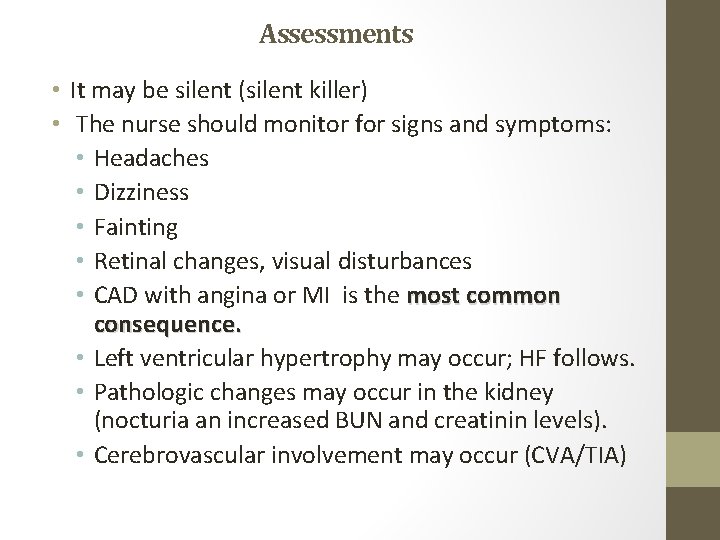
Assessments • It may be silent (silent killer) • The nurse should monitor for signs and symptoms: • Headaches • Dizziness • Fainting • Retinal changes, visual disturbances • CAD with angina or MI is the most common consequence. • Left ventricular hypertrophy may occur; HF follows. • Pathologic changes may occur in the kidney (nocturia an increased BUN and creatinin levels). • Cerebrovascular involvement may occur (CVA/TIA)
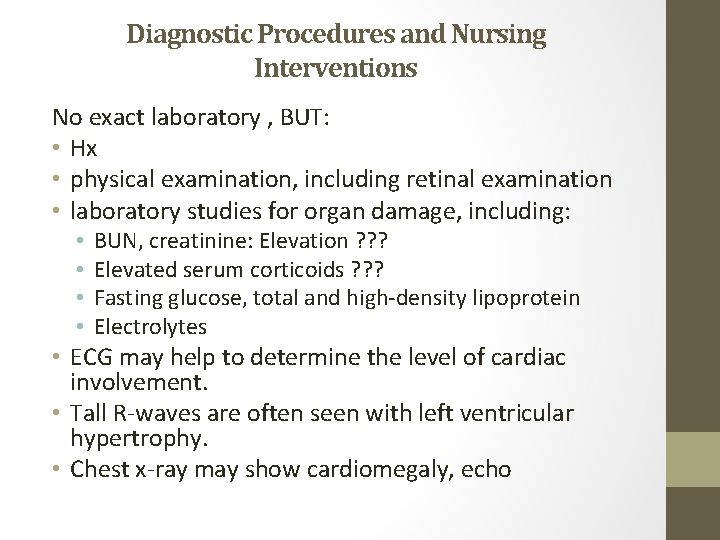
Diagnostic Procedures and Nursing Interventions No exact laboratory , BUT: • Hx • physical examination, including retinal examination • laboratory studies for organ damage, including: • • BUN, creatinine: Elevation ? ? ? Elevated serum corticoids ? ? ? Fasting glucose, total and high-density lipoprotein Electrolytes • ECG may help to determine the level of cardiac involvement. • Tall R-waves are often seen with left ventricular hypertrophy. • Chest x-ray may show cardiomegaly, echo

Assess/Monitor • Blood pressure • Factors that increase the risk of HTN (age, dietary intake, exercise habits, current medications) • General appearance (temperature, skin color) • Laboratory findings (BUN, creatinine)
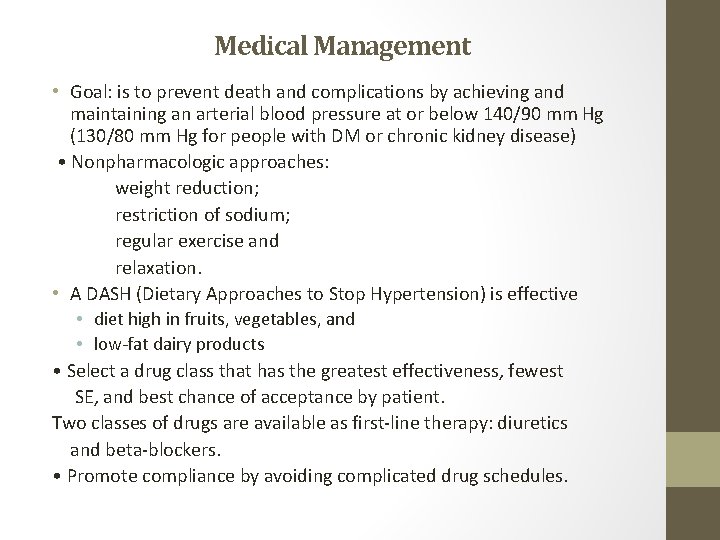
Medical Management • Goal: is to prevent death and complications by achieving and maintaining an arterial blood pressure at or below 140/90 mm Hg (130/80 mm Hg for people with DM or chronic kidney disease) • Nonpharmacologic approaches: weight reduction; restriction of sodium; regular exercise and relaxation. • A DASH (Dietary Approaches to Stop Hypertension) is effective • diet high in fruits, vegetables, and • low-fat dairy products • Select a drug class that has the greatest effectiveness, fewest SE, and best chance of acceptance by patient. Two classes of drugs are available as first-line therapy: diuretics and beta-blockers. • Promote compliance by avoiding complicated drug schedules.

NANDA Nursing Diagnoses • Deficient knowledge • Ineffective therapeutic regimen management • Ineffective tissue perfusion • Sexual dysfunction
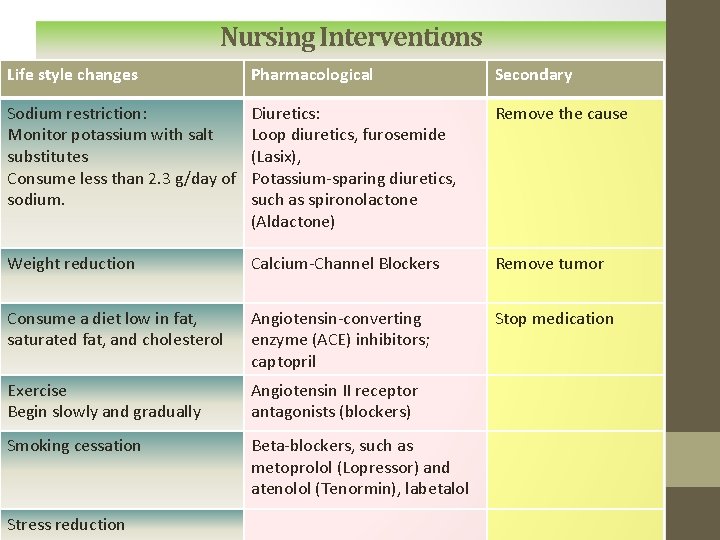
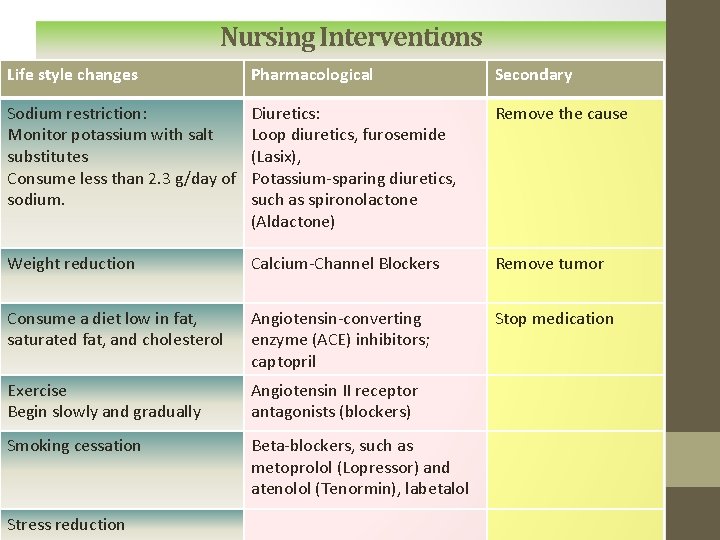
Nursing Interventions Life style changes Pharmacological Secondary Sodium restriction: Monitor potassium with salt substitutes Consume less than 2. 3 g/day of sodium. Diuretics: Loop diuretics, furosemide (Lasix), Potassium-sparing diuretics, such as spironolactone (Aldactone) Remove the cause Weight reduction Calcium-Channel Blockers Remove tumor Consume a diet low in fat, saturated fat, and cholesterol Angiotensin-converting enzyme (ACE) inhibitors; captopril Stop medication Exercise Begin slowly and gradually Angiotensin II receptor antagonists (blockers) Smoking cessation Beta-blockers, such as metoprolol (Lopressor) and atenolol (Tenormin), labetalol Stress reduction
Nursing Interventions • Encourage the client and family to participate in the lifestyle changes • Express to the client and family the importance of adhering to the medication regimen, even if the client is asymptomatic. • Arrange a consultation with a dietitian to help develop a plan for improving nutrient intake or for weight loss. • Advise client to avoid use of tobacco. • Recommend support groups for weight control, smoking cessation, and stress reduction, if necessary.

Nursing Interventions • Assist the client to develop and adhere to an appropriate exercise regimen. . • Provide verbal and written education regarding medications and their side effects. • Encourage the client to have regular provider appointments to monitor HTN and cardiovascular status. • Encourage the client to report symptoms or side effects as they may be indicative of additional problems. Medications can often be changed to alleviate side effects.
Complications and Nursing Implications • Hypertensive Crisis (malignant hypertension) • Often occurs when clients do not follow the medication therapy regimen. • Signs and symptoms include: • Severe headache. • Extremely high blood pressure (systolic blood pressure greater than 240 mm Hg, diastolic greater than 120 mm Hg). • Blurred vision, dizziness, and disorientation. • Administer IV antihypertensive therapies, such as nitroprusside (Nipride), nicardipine (Cardene IV), and labetalol (Normodyne).
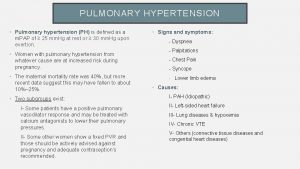
 Isolated systolic hypertension
Isolated systolic hypertension Well-defined set example
Well-defined set example Diastolic pressure definition
Diastolic pressure definition What is stroke volume
What is stroke volume End diastolic volume meaning
End diastolic volume meaning Sam systolic anterior motion
Sam systolic anterior motion Location of heart sounds
Location of heart sounds Machinary murmur
Machinary murmur Rvsp
Rvsp Tapping sounds
Tapping sounds Systolic mm hg
Systolic mm hg Added heart sounds
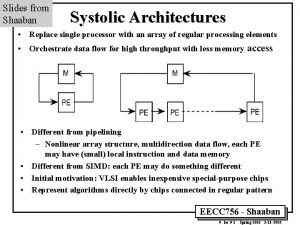
Added heart sounds Systolic array vs simd
Systolic array vs simd Trunctus
Trunctus Systolic array
Systolic array Arteriol
Arteriol What is systolic and diastolic pressure
What is systolic and diastolic pressure Why systolic architectures
Why systolic architectures Systemic vascular resistance
Systemic vascular resistance Definition of hypertension
Definition of hypertension