Hypersensitivity Disorders Allergic Emergencies Jim Holliman M D

- Slides: 41
Hypersensitivity Disorders Allergic Emergencies Jim Holliman, M. D. , F. A. C. E. P. Professor of Military and Emergency Medicine Uniformed Services University of the Health Sciences Clinical Professor of Emergency Medicine George Washington University Bethesda, Maryland, U. S. A.
Hypersensitivity Disorders & Allergic Emergencies : Lecture Objectives ƒ Describe & compare : –Anaphylaxis & anaphylactoid reactions –Angioneurotic edema –Drug allergies ƒ Describe emergent Rx & followup outpatient Rx for anaphylactic & other allergic reactions
Allergic Reactions Definitions of Terms ƒ Anaphylaxis (Greek = "backward protection") –Rapid generalized immunologic reaction after exposure to antigens in a sensitized person, with at least 2 of : ƒ resp. or airway compromise from swelling or wheezing ƒ hypotension or cardiovascular collapse ƒ diffuse cutaneous findings (urticaria, angioedema, +/- erythroderma)
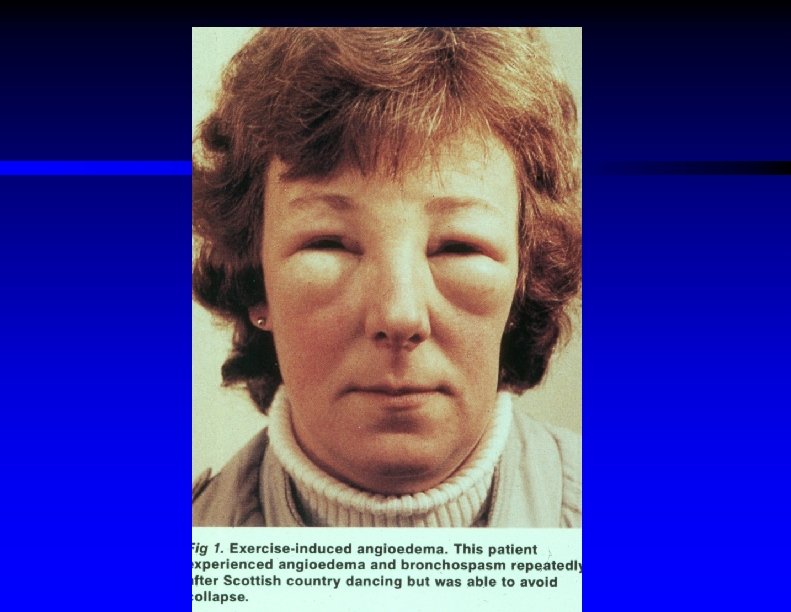
Allergic Reactions Definitions of Terms (cont. ) ƒ Anaphylactoid reaction : –Syndrome presenting similar to anaphylaxis, expressed by similar mediators, but not triggered by Ig. E & not necessarily due to prior exposure to the inciting agent ƒ Urticaria : –Diffuse patchy erythematous pruritic rash with raised borders ƒ Angioedema : –Non-pitting subcutaneous tissue swelling –Often of the face, mouth, or peri-airway tissue
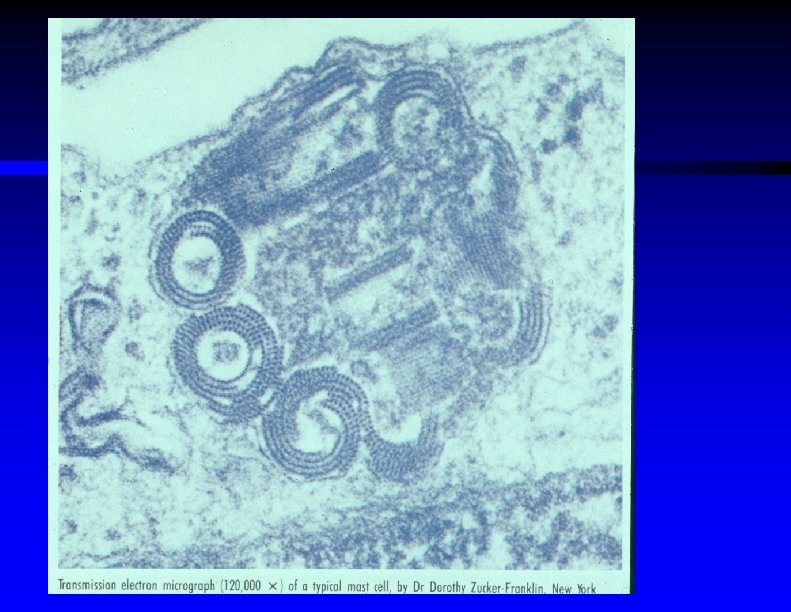
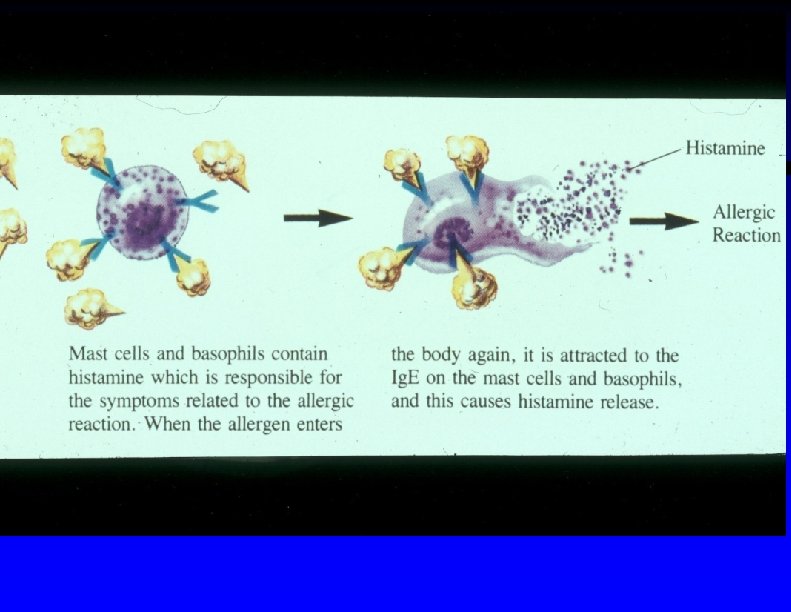
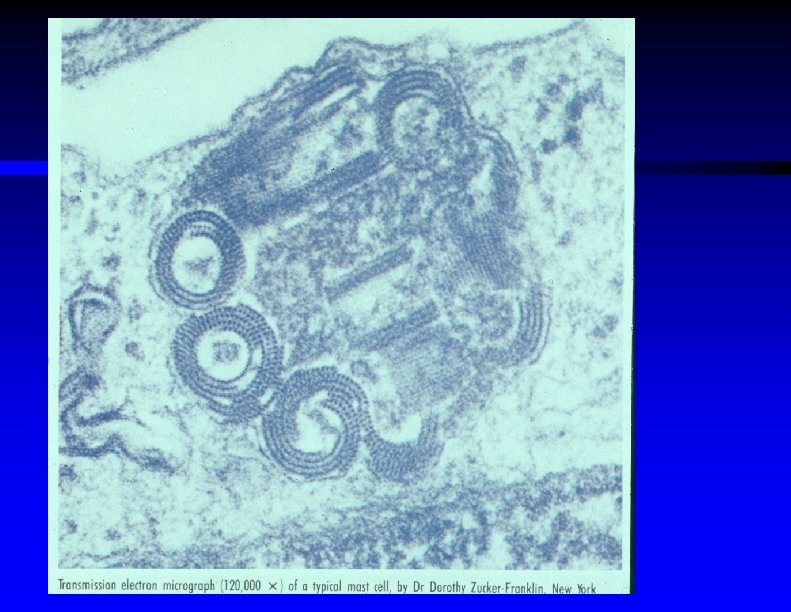
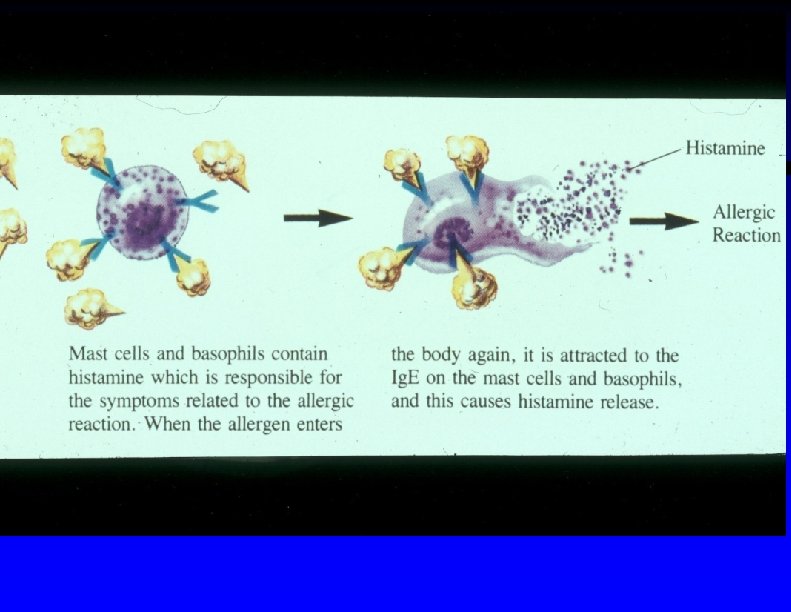
Pathophysiology of Allergic Reactions ƒ Mast cell –Final common pathway of allergic reactions –Present in most tissues –When activated, release (from cell granules) : ƒ Histamine ƒ Bradykinins ƒ Prostaglandins ƒ Leukotrienes –Clinical effects are due to these above mediators
Four Mechanisms that Lead to Mast Cell Degranulation (Release of Mediators) ƒ Immunoglobulin E (Ig. E) mediated hypersensitivity ƒ Complement cascade activation ƒ Direct stimulation of mast cell by anaphylactoid substances ƒ Inhibition of arachidonic acid pathway
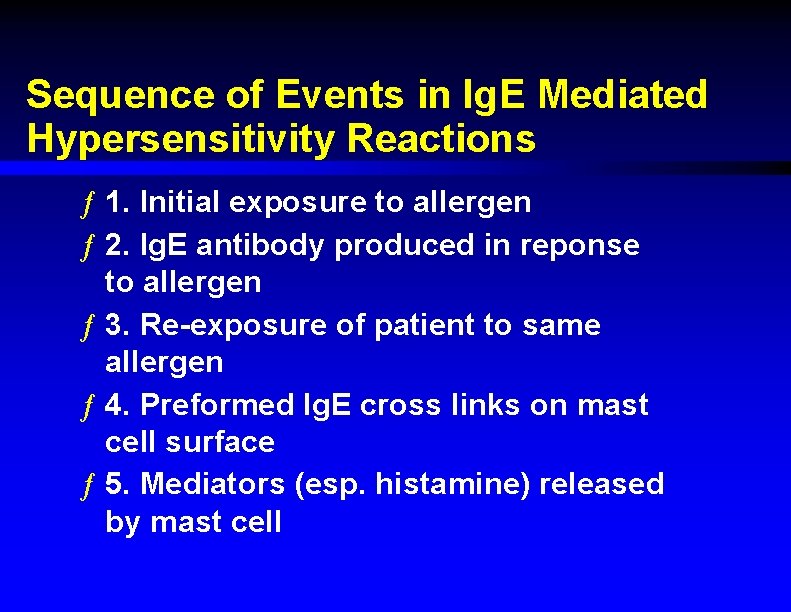
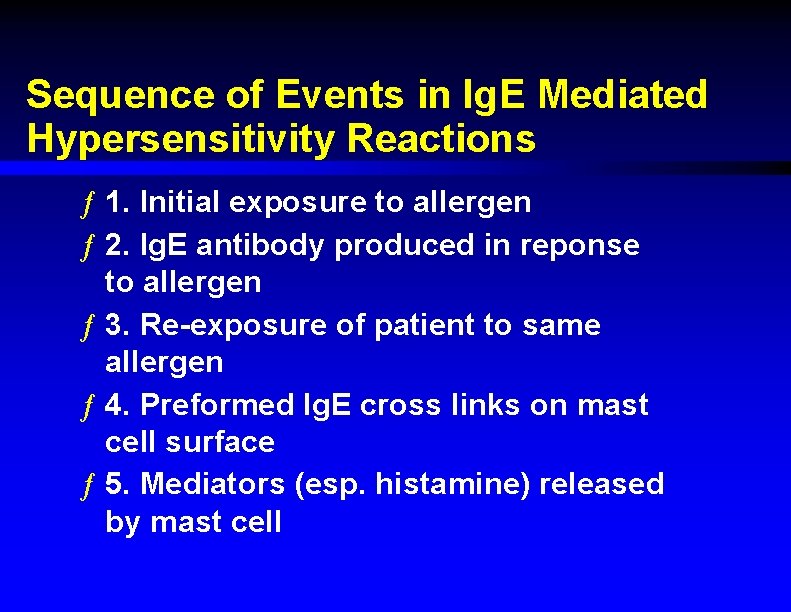
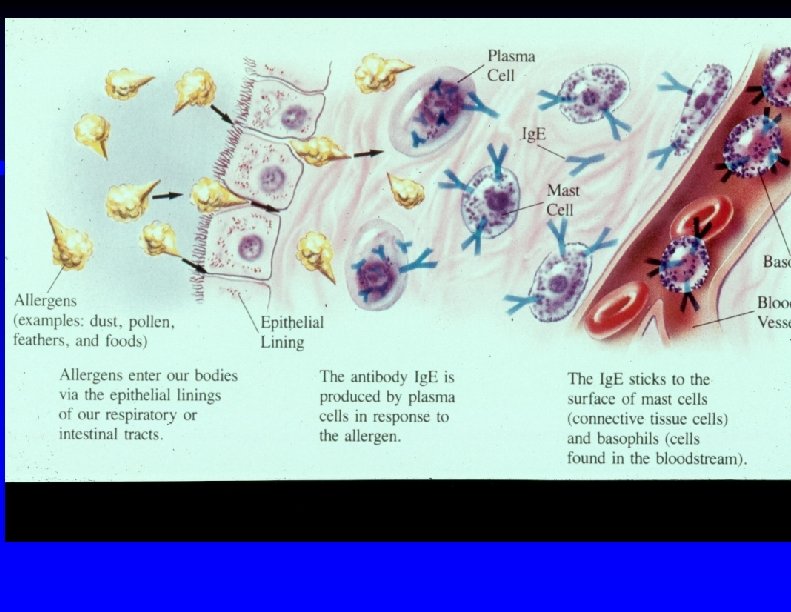
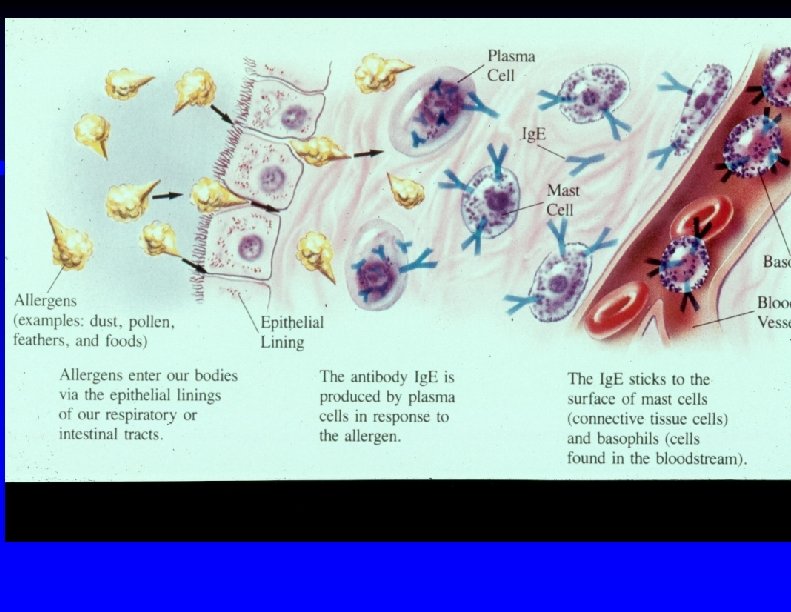
Sequence of Events in Ig. E Mediated Hypersensitivity Reactions ƒ 1. Initial exposure to allergen ƒ 2. Ig. E antibody produced in reponse to allergen ƒ 3. Re-exposure of patient to same allergen ƒ 4. Preformed Ig. E cross links on mast cell surface ƒ 5. Mediators (esp. histamine) released by mast cell
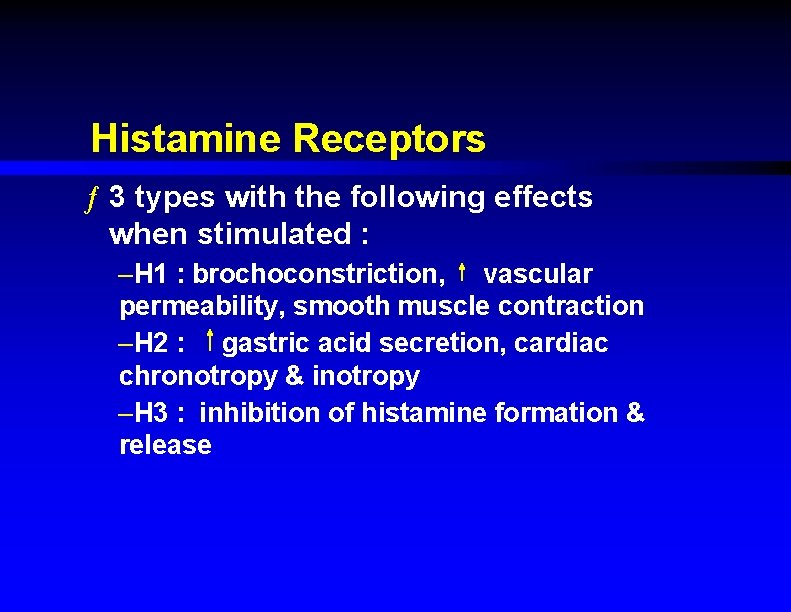
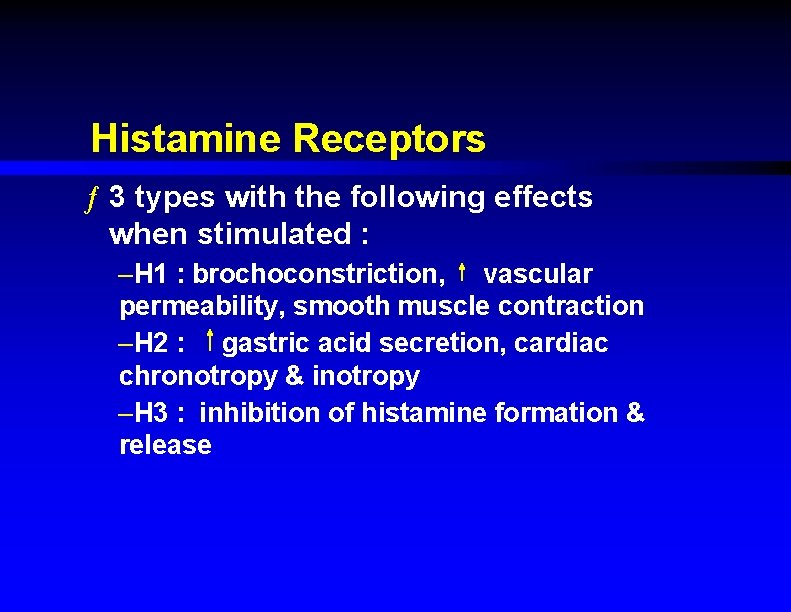
Histamine Receptors ƒ 3 types with the following effects when stimulated : –H 1 : brochoconstriction, vascular permeability, smooth muscle contraction –H 2 : gastric acid secretion, cardiac chronotropy & inotropy –H 3 : inhibition of histamine formation & release
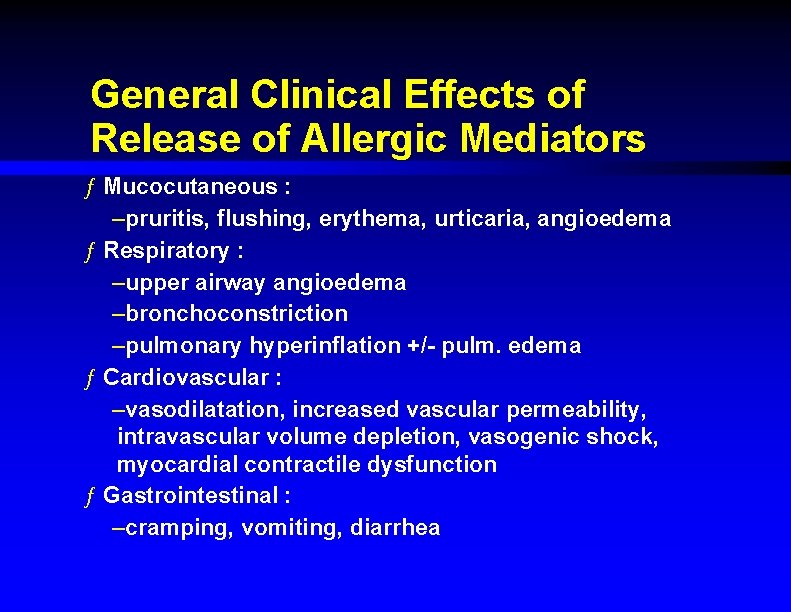
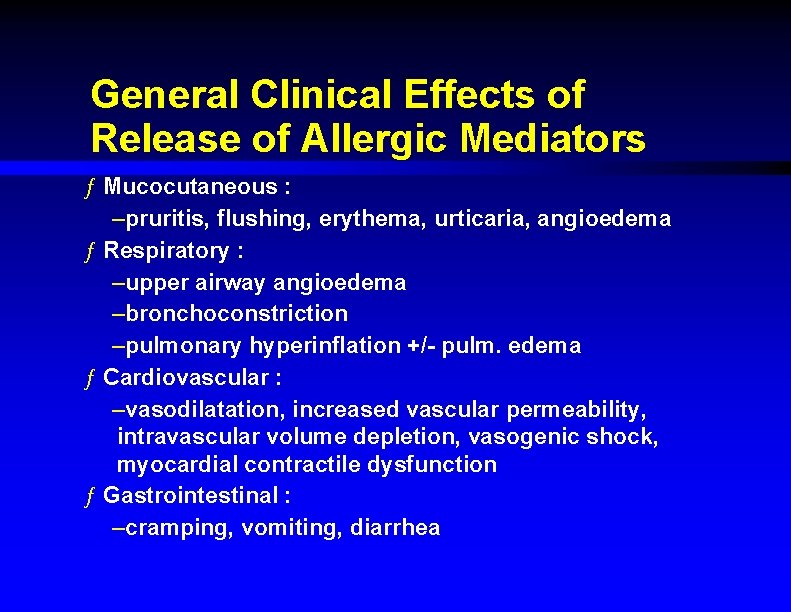
General Clinical Effects of Release of Allergic Mediators ƒ Mucocutaneous : –pruritis, flushing, erythema, urticaria, angioedema ƒ Respiratory : –upper airway angioedema –bronchoconstriction –pulmonary hyperinflation +/- pulm. edema ƒ Cardiovascular : –vasodilatation, increased vascular permeability, intravascular volume depletion, vasogenic shock, myocardial contractile dysfunction ƒ Gastrointestinal : –cramping, vomiting, diarrhea
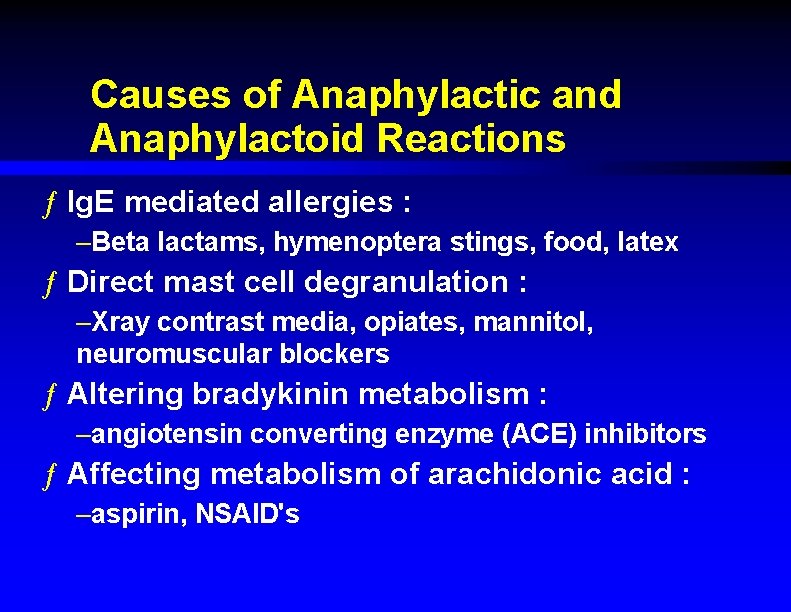
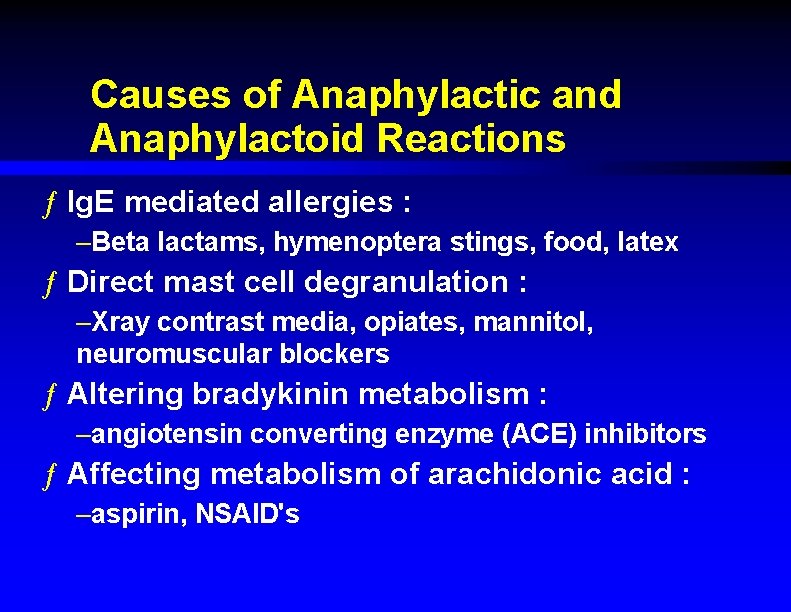
Causes of Anaphylactic and Anaphylactoid Reactions ƒ Ig. E mediated allergies : –Beta lactams, hymenoptera stings, food, latex ƒ Direct mast cell degranulation : –Xray contrast media, opiates, mannitol, neuromuscular blockers ƒ Altering bradykinin metabolism : –angiotensin converting enzyme (ACE) inhibitors ƒ Affecting metabolism of arachidonic acid : –aspirin, NSAID's
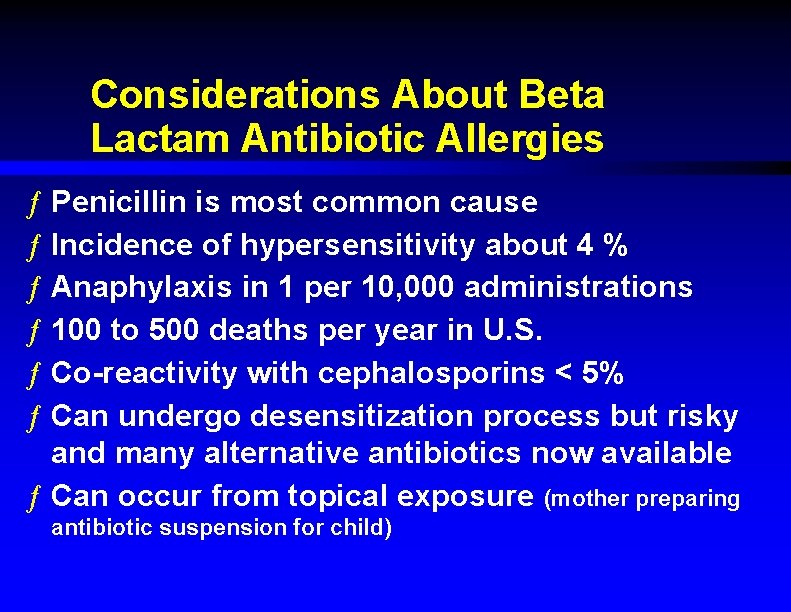
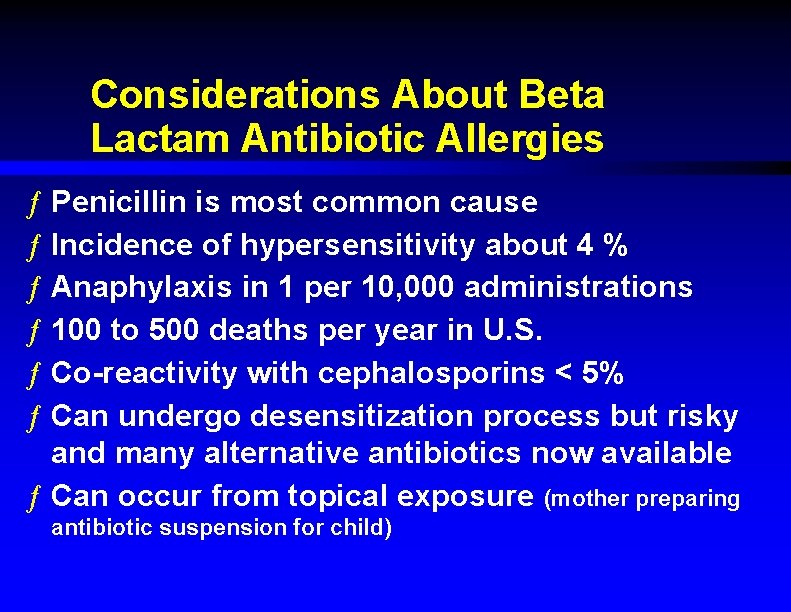
Considerations About Beta Lactam Antibiotic Allergies ƒ Penicillin is most common cause ƒ Incidence of hypersensitivity about 4 % ƒ Anaphylaxis in 1 per 10, 000 administrations ƒ 100 to 500 deaths per year in U. S. ƒ Co-reactivity with cephalosporins < 5% ƒ Can undergo desensitization process but risky and many alternative antibiotics now available ƒ Can occur from topical exposure (mother preparing antibiotic suspension for child)
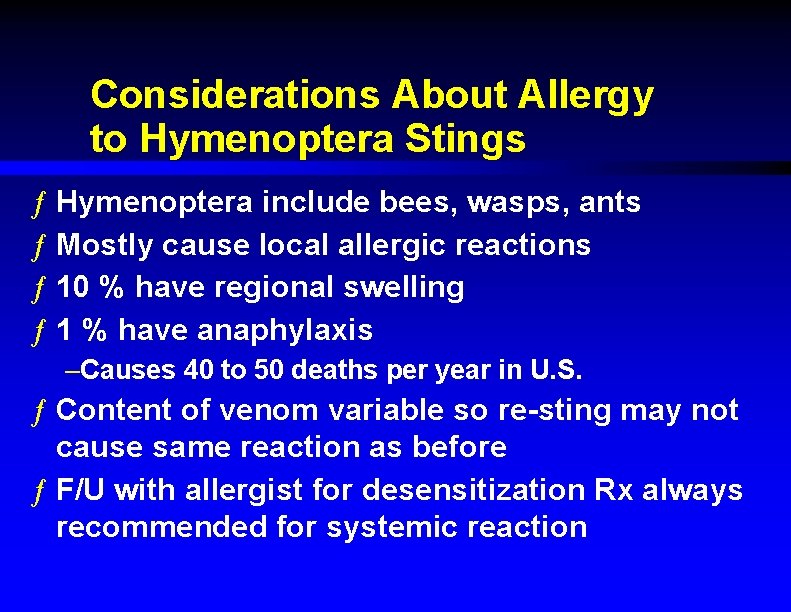
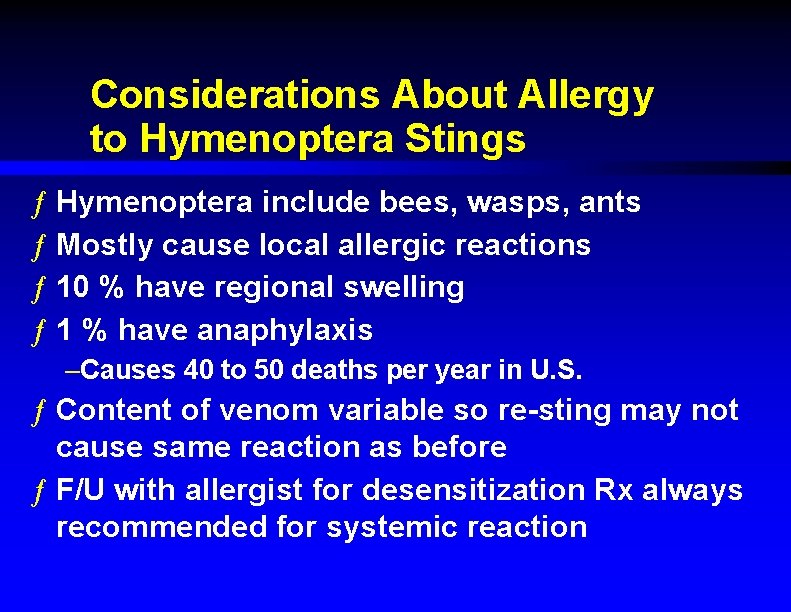
Considerations About Allergy to Hymenoptera Stings ƒ Hymenoptera include bees, wasps, ants ƒ Mostly cause local allergic reactions ƒ 10 % have regional swelling ƒ 1 % have anaphylaxis –Causes 40 to 50 deaths per year in U. S. ƒ Content of venom variable so re-sting may not cause same reaction as before ƒ F/U with allergist for desensitization Rx always recommended for systemic reaction
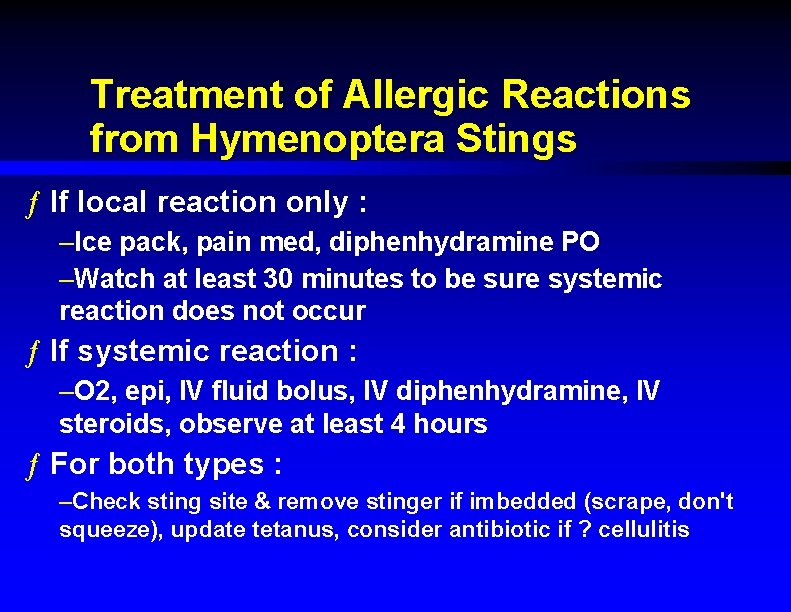
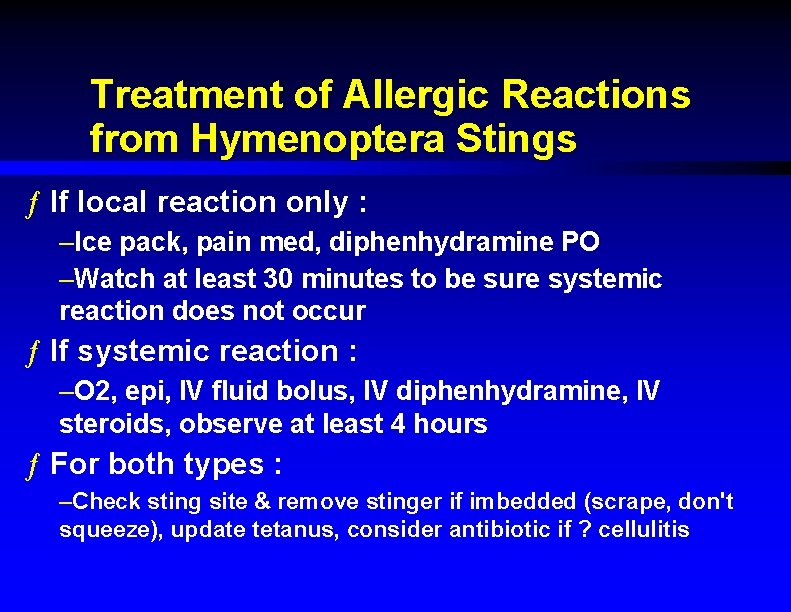
Treatment of Allergic Reactions from Hymenoptera Stings ƒ If local reaction only : –Ice pack, pain med, diphenhydramine PO –Watch at least 30 minutes to be sure systemic reaction does not occur ƒ If systemic reaction : –O 2, epi, IV fluid bolus, IV diphenhydramine, IV steroids, observe at least 4 hours ƒ For both types : –Check sting site & remove stinger if imbedded (scrape, don't squeeze), update tetanus, consider antibiotic if ? cellulitis
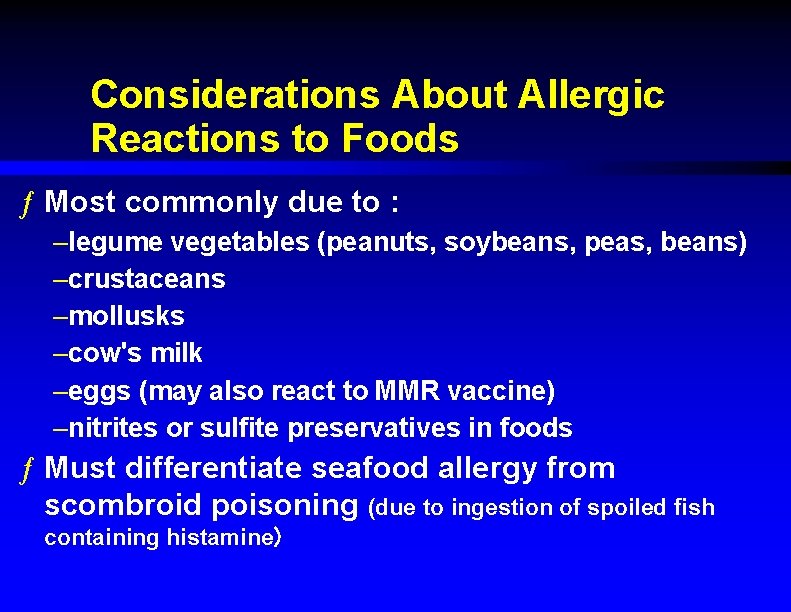
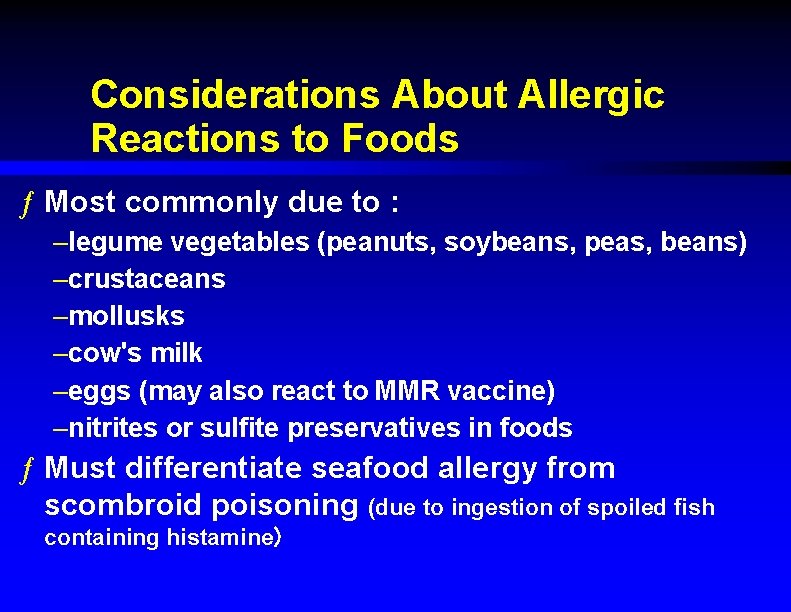
Considerations About Allergic Reactions to Foods ƒ Most commonly due to : –legume vegetables (peanuts, soybeans, peas, beans) –crustaceans –mollusks –cow's milk –eggs (may also react to MMR vaccine) –nitrites or sulfite preservatives in foods ƒ Must differentiate seafood allergy from scombroid poisoning (due to ingestion of spoiled fish containing histamine)
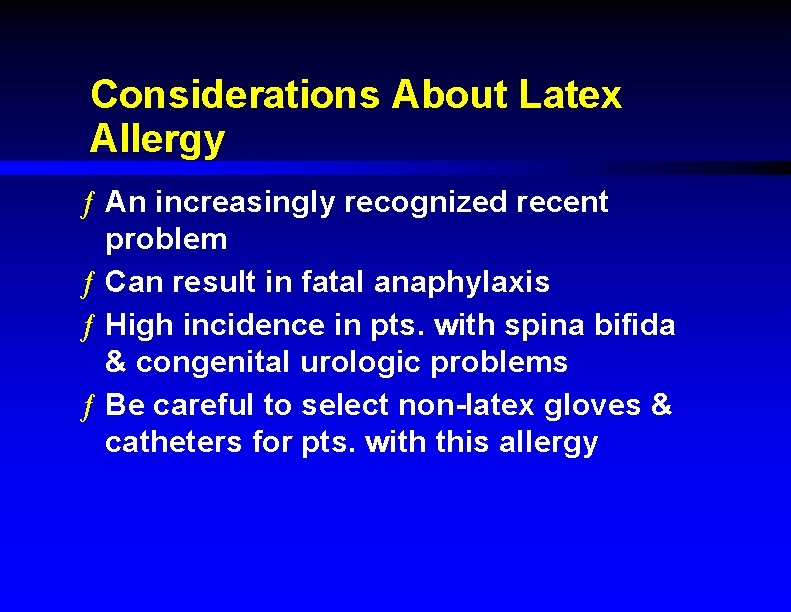
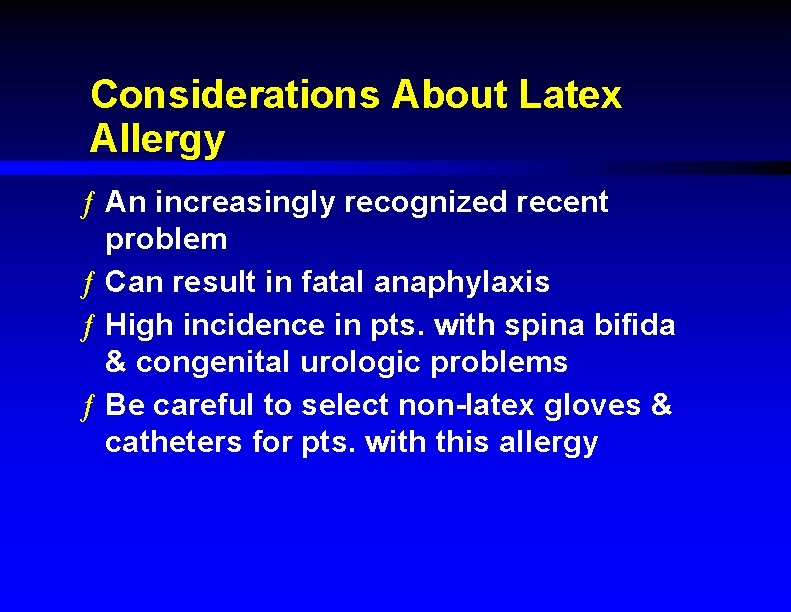
Considerations About Latex Allergy ƒ An increasingly recognized recent problem ƒ Can result in fatal anaphylaxis ƒ High incidence in pts. with spina bifida & congenital urologic problems ƒ Be careful to select non-latex gloves & catheters for pts. with this allergy
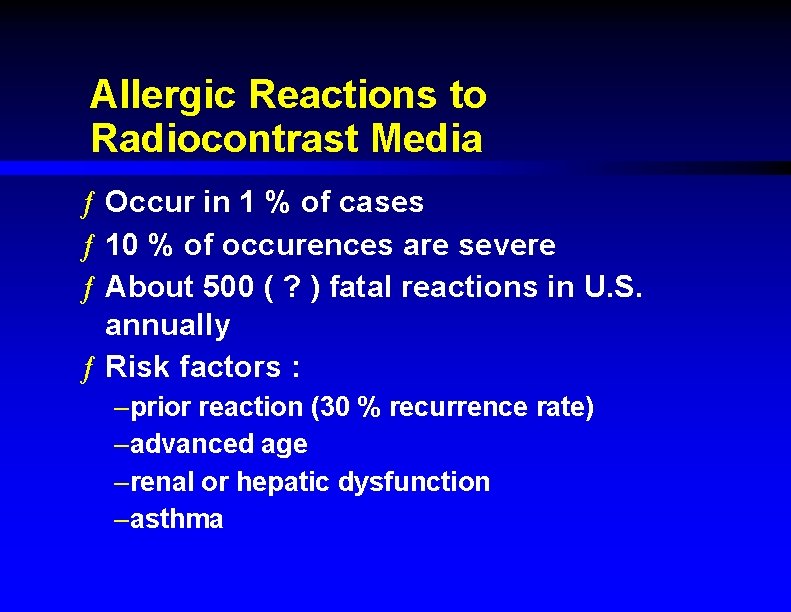
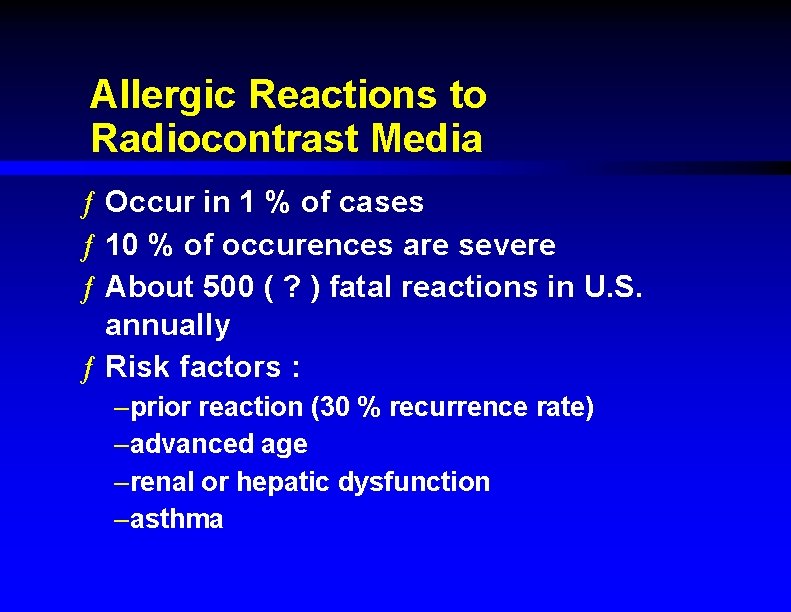
Allergic Reactions to Radiocontrast Media ƒ Occur in 1 % of cases ƒ 10 % of occurences are severe ƒ About 500 ( ? ) fatal reactions in U. S. annually ƒ Risk factors : –prior reaction (30 % recurrence rate) –advanced age –renal or hepatic dysfunction –asthma
Allergic Reactions to Radiocontrast Agents (cont. ) ƒ High osmolarity agents (Hypaque, Renografin, Conray) –Tri-iodinated, ionic ƒ Low osmolarity agents : –non-ionic dimers –produce less histamine release & less vascular endothelial irritation –Much more expensive (5 X) –Recent reports show reduction in complications of contrast studies using these agents, but reactions still occur in 30%
Allergic Reaction Prophylaxis for Radiocontrast Agent Use ƒ Pretreatment reduces recurrent allergic reaction rate to 1% ƒ One suggested regimen : –Hydrocortisone 200 mg IV just prior to & 4 hours after contrast, & cimetidine 300 mg IV & diphenhydramine 50 mg IV just prior to contrast –Should have epi & resus. equipment available ƒ Pre-Rx indicated for pt. requiring a contrast study with prior Hx of reaction or renal dysfunction
Angioedema Due to ACE Inhibitors ƒ Occurs in 0. 2 % of pts. on ACE inhibitors ƒ Can occur even after prolonged use of ACE inhibitors without a prior reaction ƒ Predeliction for head & neck angioedema so airway compromise possible ƒ Rx by stopping the ACE inhibitor, epi, steroids, diphenhydramine, +/- airway management

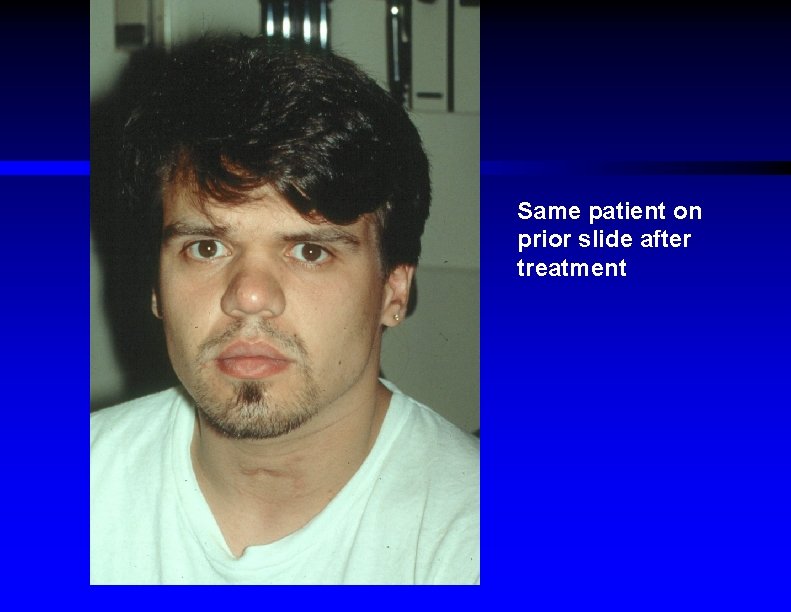
Severe angioedema
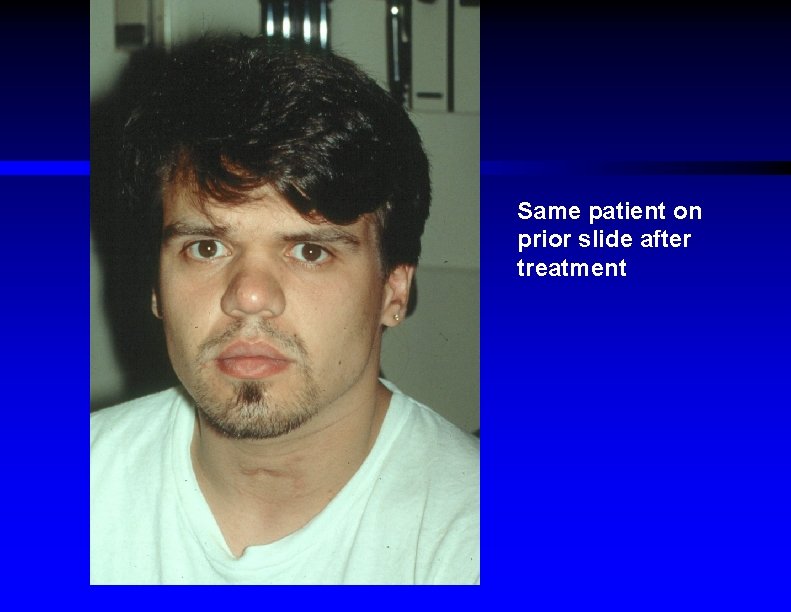
Same patient on prior slide after treatment
Spectrum of Presentations of Allergic Reactions ƒ Time to onset, intensity, & duration of reaction vary, depending on : –degree of sensitivity of pt. –route of exposure –amount ("dose") of antigen ƒ Rarely pts. may have "biphasic" reaction with reexacerbation of Sx 4 to 8 hours after the initial reaction
Clinical Manifestations of Systemic Allergic Reactions ƒ Diffuse pruritis, urticaria, angioedema, erythroderma ƒ Anxiety, dizziness, sense of doom, altered mental status ƒ Dyspnea, stridor, wheezing ƒ Dysphagia, dysarthria, drooling ƒ Vomiting, diarrhea, abd. cramps ƒ Urinary incontinence ƒ Hypotension +/- bradycardia
Differential Dx of Severe Allergic Reaction ƒ Sudden loss of consciousness : –vasovagal syncope, seizures, dysrhythmias, CVA ƒ Acute respiratory distress : –status asthmaticus, upper airway infection, foreign body aspiration, pulm. embolus ƒ Cardiovascular collapse : –intraabdominal bleed, acute MI ƒ Systemic disorders : –mastocytosis, hereditary angioedema (C 1 esterase deficiency syndrome) , carcinoid syndrome, scromboid poisoning, MSG syndrome
E. D. Management of Systemic Allergic Reactions ƒ Since may progress rapidly & unpredictably, all pts. with possible systemic reaction should be rapidly triaged to acute care room & continuously monitored ƒ Suggested initial sequence : –O 2 / airway management –SQ or IM epi (0. 01 mg/kg or max. 0. 3 mg in adults) –IV placement ; IV fluid bolus (NS) if hypotensive –IV diphenhydramine & IV steroids –Beta 2 aerosol if wheezing –Secondary meds ; consider repeat epi doses –Remove source of reaction if possible – Give IV fresh frozen plasma if hereditary angioedema from C 1 esterase deficiency
Airway Management Considerations for Severe Allergic Reactions ƒ Swelling impinging the airway may progress rapidly so earlier intubation more likely successful than later ƒ Consider sedation without paralysis if anticipated difficulty ƒ Start with ETT size one size smaller than usual ƒ Have surgical airway equipment at bedside ƒ Place nasal airway early even if ETT not initially required ƒ Consider use of inhaled racemic epi
The Key Med in Rx of Allergic Reactions : Epinephrine (epi) ƒ Is the most important & effective Rx med ƒ Alpha agonist effects : –Vasoconstriction, decreased vascular permeability, resolution of angioedema ƒ Beta agonist effects : –Bronchodilatation, cardiac inotropy, mast cell membrane stabilization
Potential Complications of Use of Epi for Allergic Reactions ƒ Hypertension (may cause CNS bleed) ƒ Increased myocardial O 2 consumption ƒ Coronary vasoconstriction ƒ Tachycardia / dysrhythmias In pts. who have HBP, CAD, CVA, or pregnancy, should consider need for epi carefully & may need to decrease dose; should still be given though to these pts. if reaction is severe
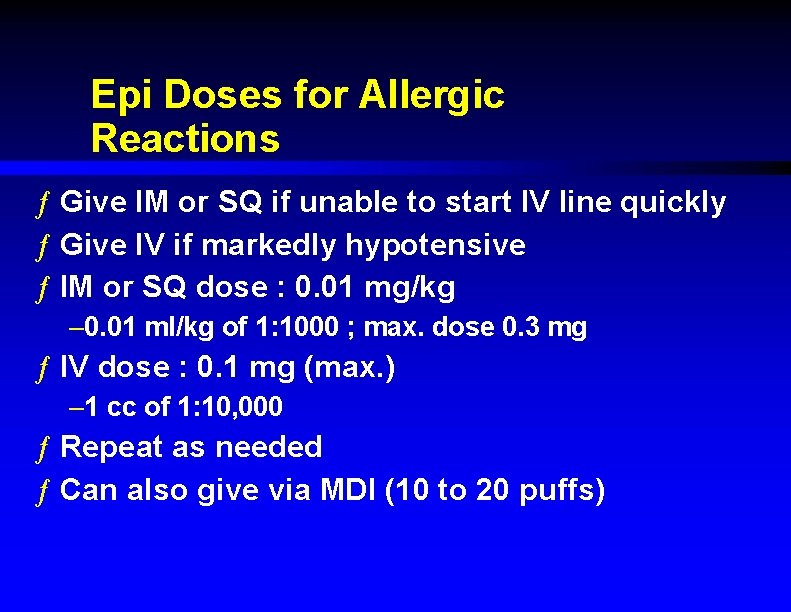
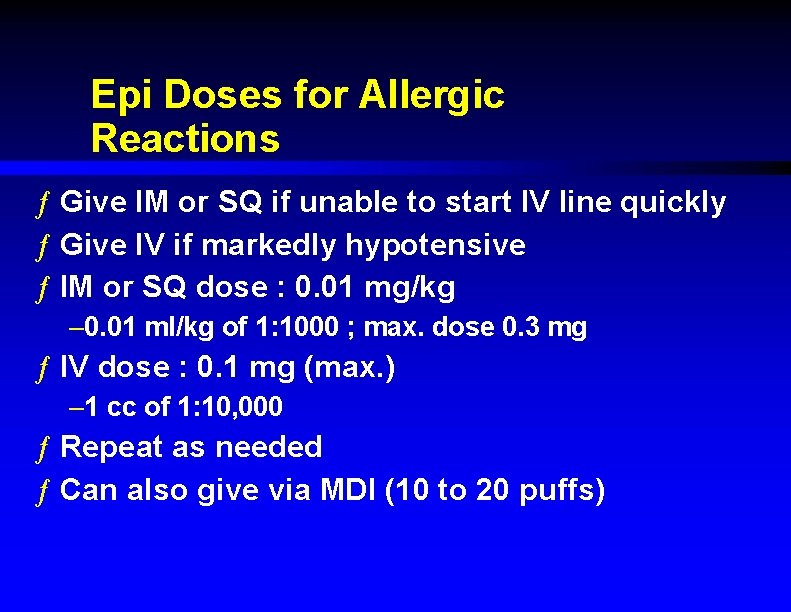
Epi Doses for Allergic Reactions ƒ Give IM or SQ if unable to start IV line quickly ƒ Give IV if markedly hypotensive ƒ IM or SQ dose : 0. 01 mg/kg – 0. 01 ml/kg of 1: 1000 ; max. dose 0. 3 mg ƒ IV dose : 0. 1 mg (max. ) – 1 cc of 1: 10, 000 ƒ Repeat as needed ƒ Can also give via MDI (10 to 20 puffs)
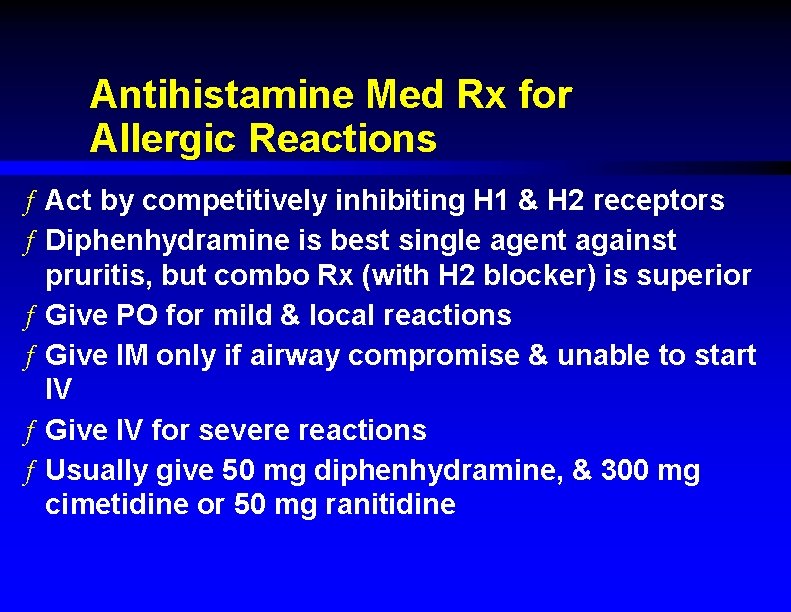
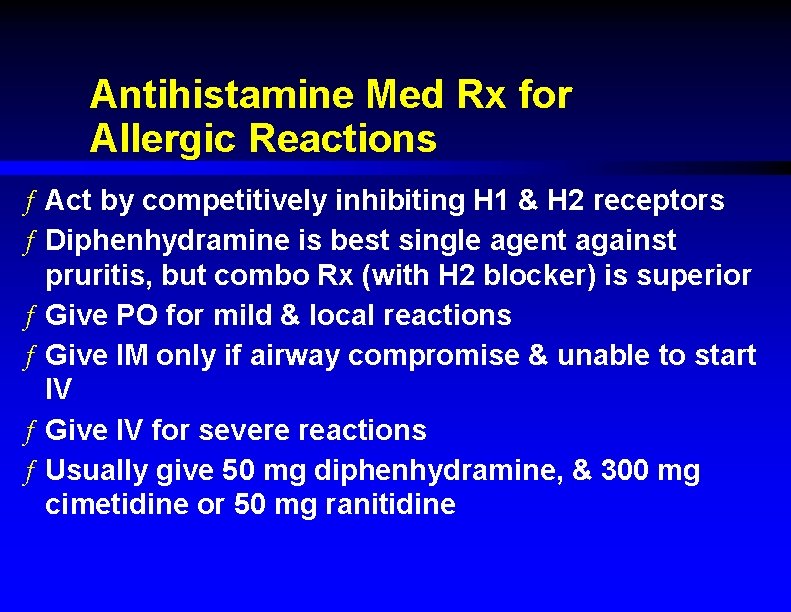
Antihistamine Med Rx for Allergic Reactions ƒ Act by competitively inhibiting H 1 & H 2 receptors ƒ Diphenhydramine is best single agent against pruritis, but combo Rx (with H 2 blocker) is superior ƒ Give PO for mild & local reactions ƒ Give IM only if airway compromise & unable to start IV ƒ Give IV for severe reactions ƒ Usually give 50 mg diphenhydramine, & 300 mg cimetidine or 50 mg ranitidine
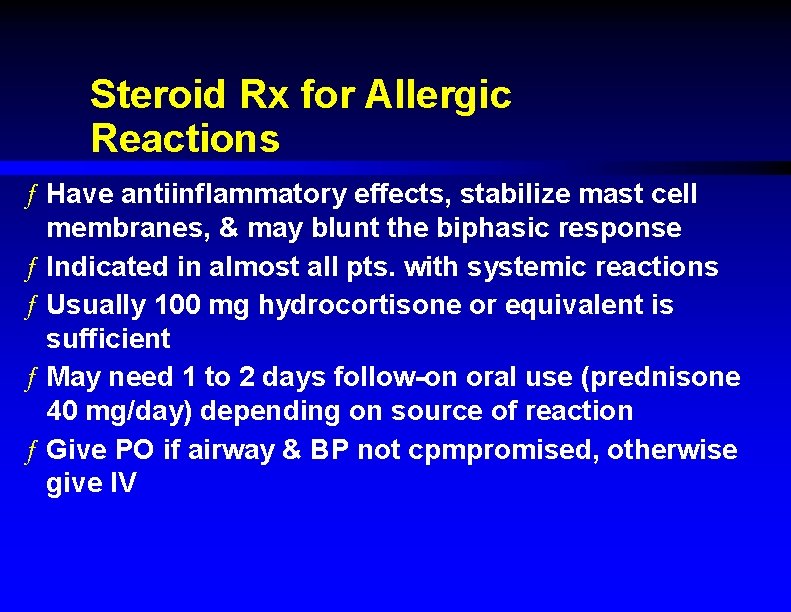
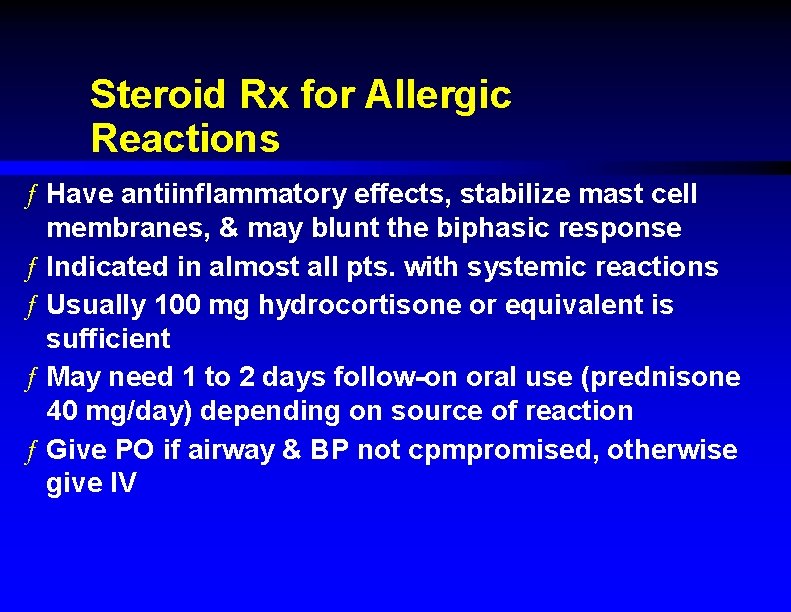
Steroid Rx for Allergic Reactions ƒ Have antiinflammatory effects, stabilize mast cell membranes, & may blunt the biphasic response ƒ Indicated in almost all pts. with systemic reactions ƒ Usually 100 mg hydrocortisone or equivalent is sufficient ƒ May need 1 to 2 days follow-on oral use (prednisone 40 mg/day) depending on source of reaction ƒ Give PO if airway & BP not cpmpromised, otherwise give IV
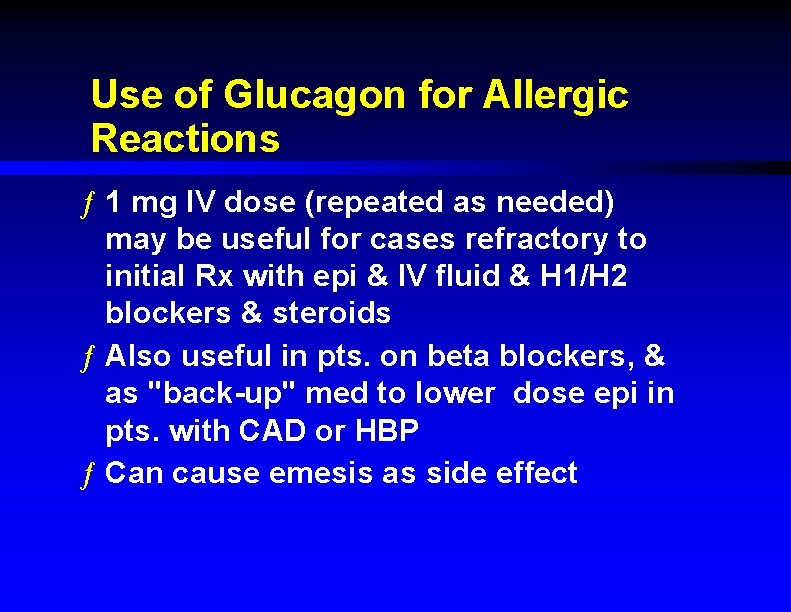
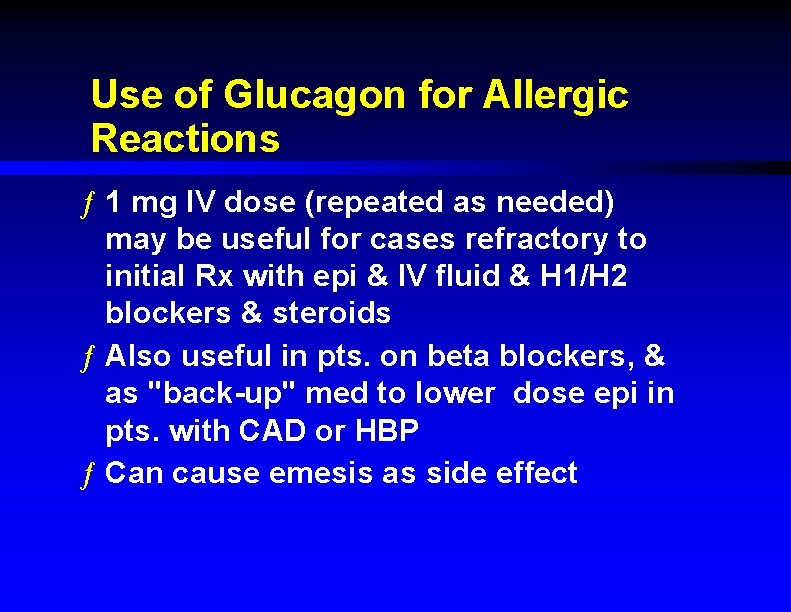
Use of Glucagon for Allergic Reactions ƒ 1 mg IV dose (repeated as needed) may be useful for cases refractory to initial Rx with epi & IV fluid & H 1/H 2 blockers & steroids ƒ Also useful in pts. on beta blockers, & as "back-up" med to lower dose epi in pts. with CAD or HBP ƒ Can cause emesis as side effect
Disposition Decisions for Patients with Allergic Reactions ƒ Mild local reactions should be observed for 30 minutes ; then sent home on PO diphenhydramine if no Sx progression ƒ Systemic reactions that respond to initial Rx should be observed 2 to 4 hours for recurrence ƒ Those manifesting airway compromise or hypotension (even if they respond to Rx) probably should be admitted overnight ƒ Pts. on beta blockers, elderly, asthmatics, or with other comorbid diseases should often be admitted
Discharge Medications for Patients with Allergic Reactions ƒ Most should receive : –Diphenhydramine 25 to 50 mg PO QID X 2 days –Cimetidine 300 mg PO QID X 2 days –Prednisone 40 to 50 mg PO (1 to 2 mg/kg) QD X 2 days –Consider susphrine (epi tannate in oil) 0. 005 cc/kg (max. 0. 3 cc) SQ prior to D/C –Consider epi self-injection kit (Epi-Pen or Ana-Kit) –Consider standby albuterol MDI –Consider non-sedating antihistamine
Other Discharge Considerations for Patients with Systemic Allergic Reactions ƒ Education about preventive or avoidance measures ƒ Get Medic-Alert bracelet or necklace ƒ Consider epi self-injection kit ƒ Standby oral diphenhydramine ƒ Discontinue beta blockers if possible ƒ Referral to allergist for desensitization
Hypersensitivity Disorders & Allergic Reactions : Summary ƒ Evaluate all pts. with allergic reactions emergently ƒ Assess airway & hemodynamics first ƒ Epi is mainstay of Rx ƒ Consider use of adjunctive meds ƒ Observe to determine if relapse or need for admission ƒ Discharged pts. should be instructed carefully about F/U & prevention