HYPERLIPIDEMIA MANAGEMENT OF PATIENTS IN THE PRIMARY CARE


- Slides: 32
HYPERLIPIDEMIA: MANAGEMENT OF PATIENTS IN THE PRIMARY CARE SETTING Lauren A. Winkler, DNP, RN, FNP-BC
STATISTICS Dyslipidemia is one of the key risk factors for development of CHD 31. 7% of Americans have elevated serum cholesterol levels 1 in 3 Americans have elevated LDL levels 31 million Americans have total cholesterol valuesof 240 mg/dl or greater and are considered at high risk of CHD 39. 8% of adult Indiana state residents have elevated cholesterol levels
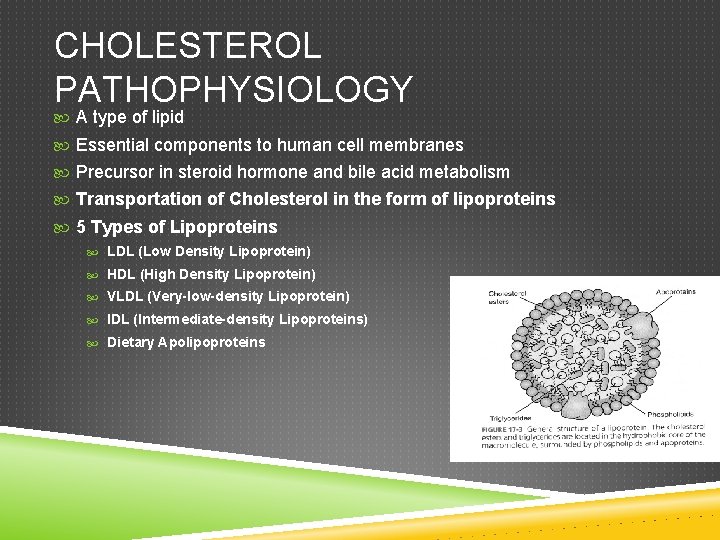
CHOLESTEROL PATHOPHYSIOLOGY A type of lipid Essential components to human cell membranes Precursor in steroid hormone and bile acid metabolism Transportation of Cholesterol in the form of lipoproteins 5 Types of Lipoproteins LDL (Low Density Lipoprotein) HDL (High Density Lipoprotein) VLDL (Very-low-density Lipoprotein) IDL (Intermediate-density Lipoproteins) Dietary Apolipoproteins
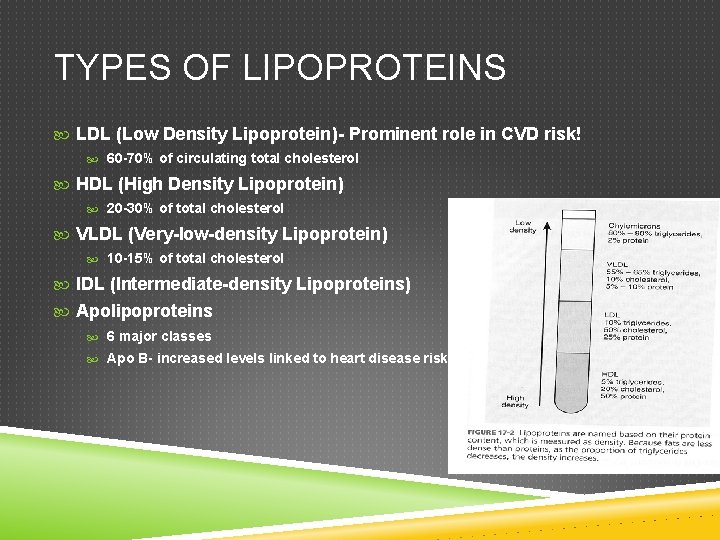
TYPES OF LIPOPROTEINS LDL (Low Density Lipoprotein)- Prominent role in CVD risk! 60 -70% of circulating total cholesterol HDL (High Density Lipoprotein) 20 -30% of total cholesterol VLDL (Very-low-density Lipoprotein) 10 -15% of total cholesterol IDL (Intermediate-density Lipoproteins) Apolipoproteins 6 major classes Apo B- increased levels linked to heart disease risk
TRIGLYCERIDES Type of Lipid Store unused calories Provide energy to body Circulate body via transportation by lipoproteins Biomarker for cardiovascular risk
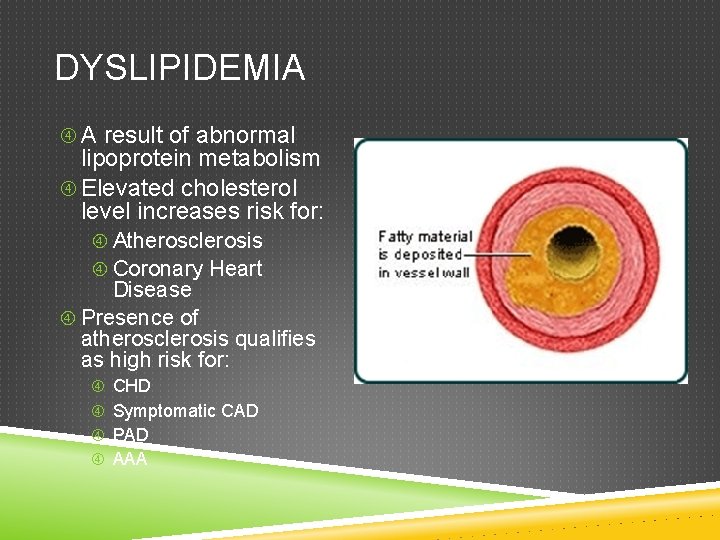
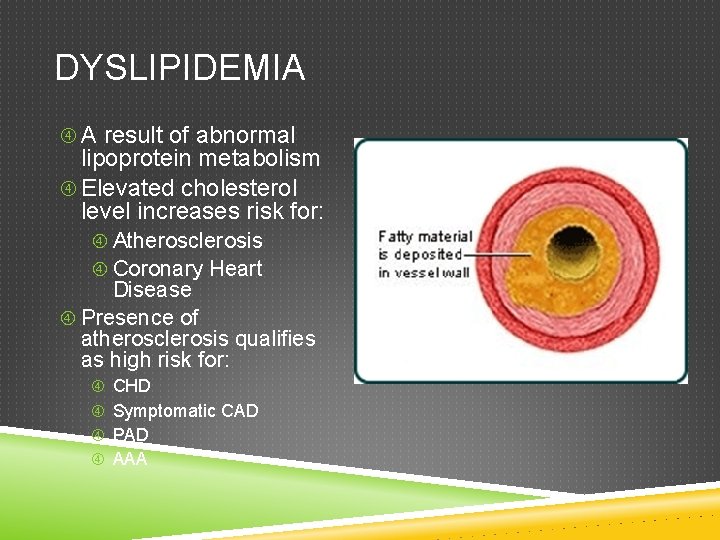
DYSLIPIDEMIA A result of abnormal lipoprotein metabolism Elevated cholesterol level increases risk for: Atherosclerosis Coronary Heart Disease Presence of atherosclerosis qualifies as high risk for: CHD Symptomatic CAD PAD AAA
PRIMARY ETIOLOGY OF DYSLIPIDEMIA Genetics Single gene mutations result in faulty apolipoproteins, receptor, or enzyme resulting in disturbance of production and clearance in LDL, HDL, and triglycerides. Suspect in patients with premature CHD or with family hx of ASD and total cholesterol >240

FAMILIAL HYPERCHOLESTEROLEMIA Two types: Heterozygous Common (1: 250) Homozygous Rare (1: 160, 000 - 1 million) LDL >600 Untreated die in 20’s Treated, CAD in 30’s
SECONDARY ETIOLOGY OF DYSLIPIDEMIA Diet and exercise play a role in the cause and treatment of lipid disorders; Sedentary lifestyle. Diet: saturated fats and trans-fatty acids, caloric excess, alcohol. Obesity: associated with elevated triglycerides, physical inactivity with low HDL. Endocrine disorders Renal disorders Hepatic disorders Immunologic disorders Medications
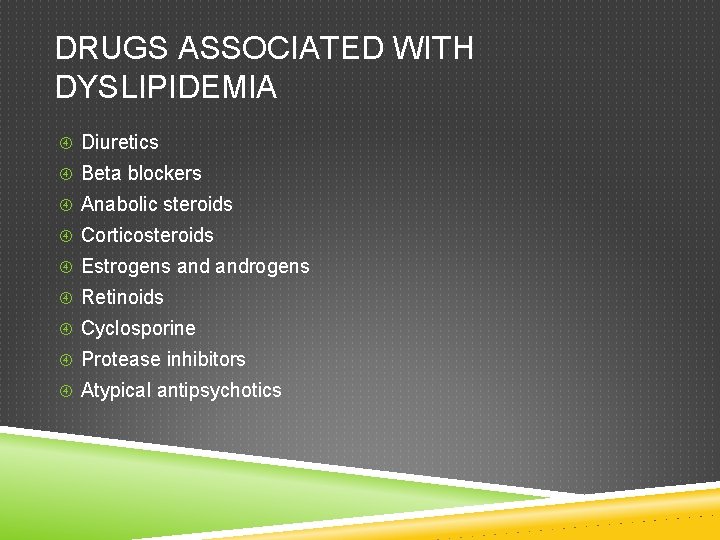
DRUGS ASSOCIATED WITH DYSLIPIDEMIA Diuretics Beta blockers Anabolic steroids Corticosteroids Estrogens androgens Retinoids Cyclosporine Protease inhibitors Atypical antipsychotics
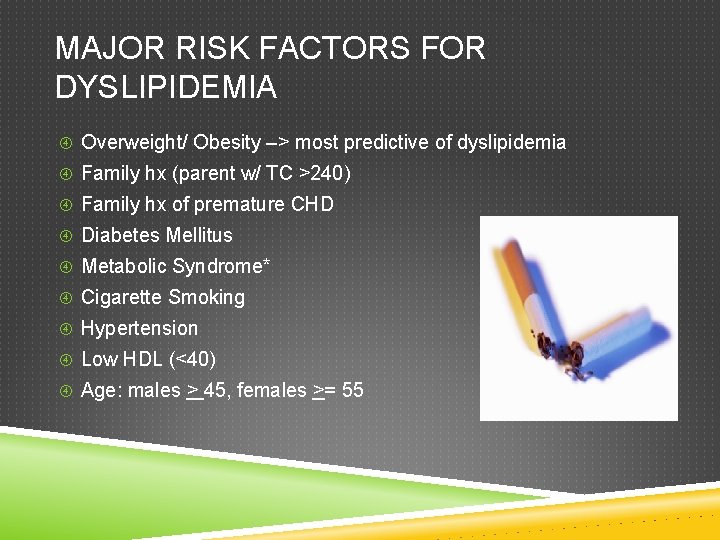
MAJOR RISK FACTORS FOR DYSLIPIDEMIA Overweight/ Obesity –> most predictive of dyslipidemia Family hx (parent w/ TC >240) Family hx of premature CHD Diabetes Mellitus Metabolic Syndrome* Cigarette Smoking Hypertension Low HDL (<40) Age: males > 45, females >= 55
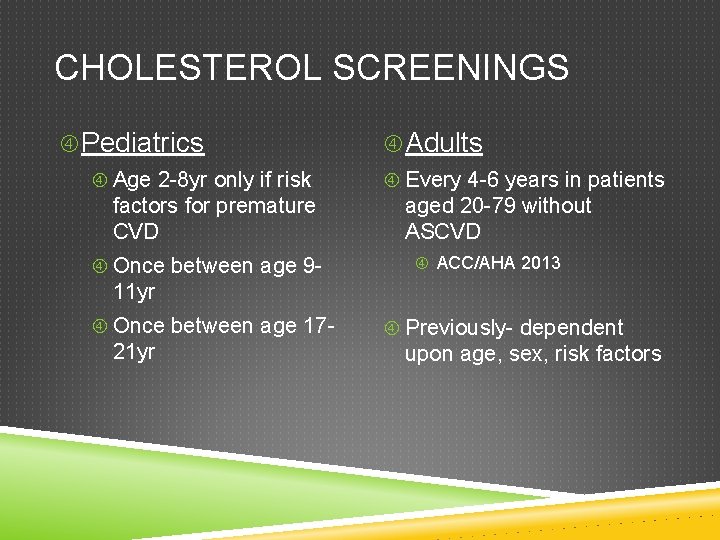
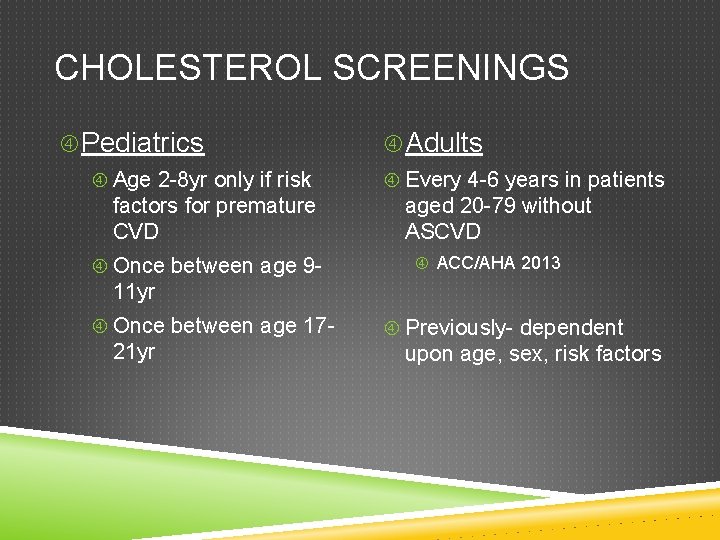
CHOLESTEROL SCREENINGS Pediatrics Age 2 -8 yr only if risk factors for premature CVD Once between age 9 - Adults Every 4 -6 years in patients aged 20 -79 without ASCVD ACC/AHA 2013 11 yr Once between age 17 - 21 yr Previously- dependent upon age, sex, risk factors
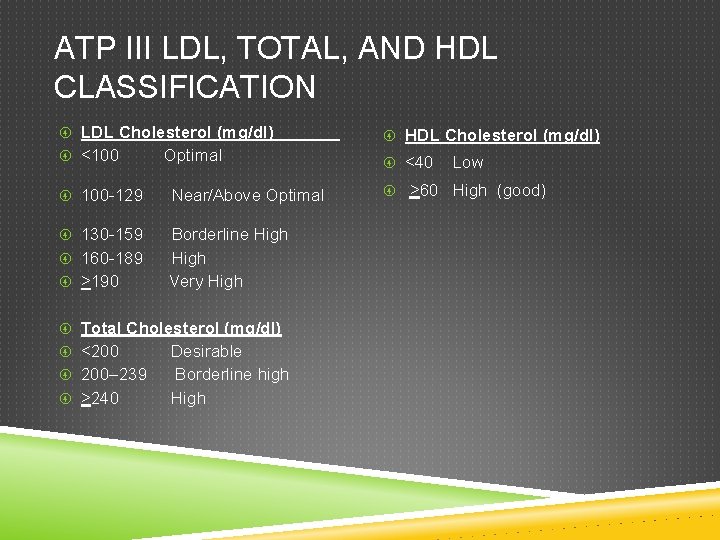
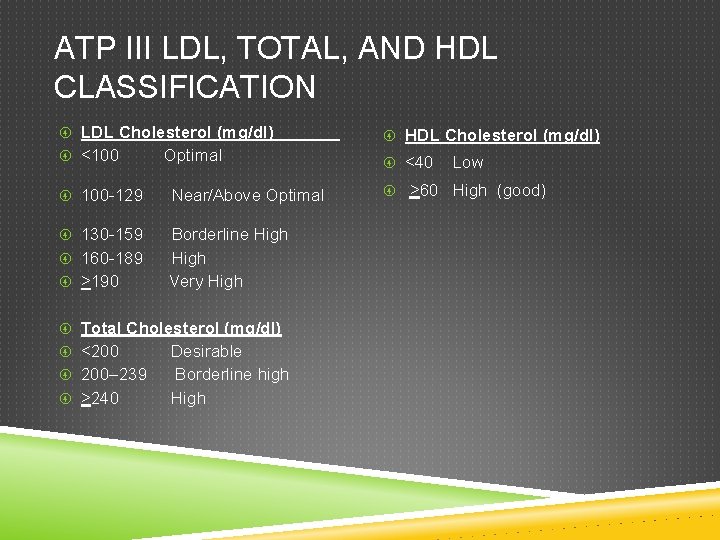
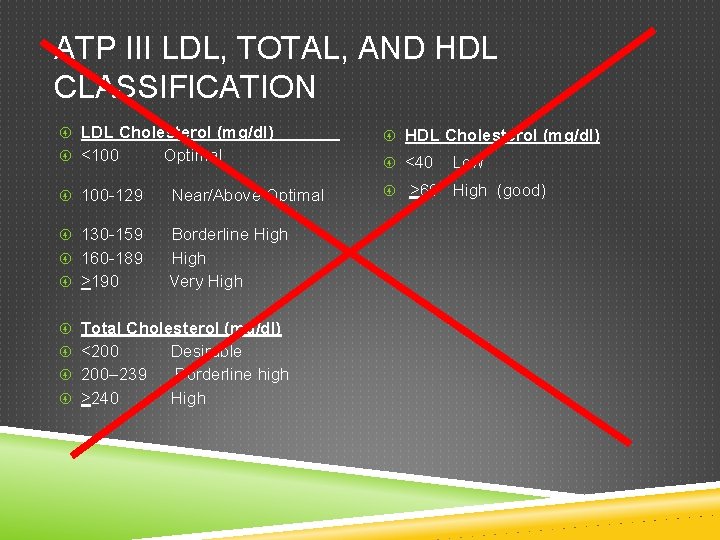
ATP III LDL, TOTAL, AND HDL CLASSIFICATION LDL Cholesterol (mg/dl) HDL Cholesterol (mg/dl) <100 <40 Optimal 100 -129 Near/Above Optimal 130 -159 Borderline High Very High 160 -189 >190 Total Cholesterol (mg/dl) <200 200– 239 >240 Desirable Borderline high High Low >60 High (good)
ATP III LDL, TOTAL, AND HDL CLASSIFICATION LDL Cholesterol (mg/dl) HDL Cholesterol (mg/dl) <100 <40 Optimal 100 -129 Near/Above Optimal 130 -159 Borderline High Very High 160 -189 >190 Total Cholesterol (mg/dl) <200 200– 239 >240 Desirable Borderline high High Low >60 High (good)
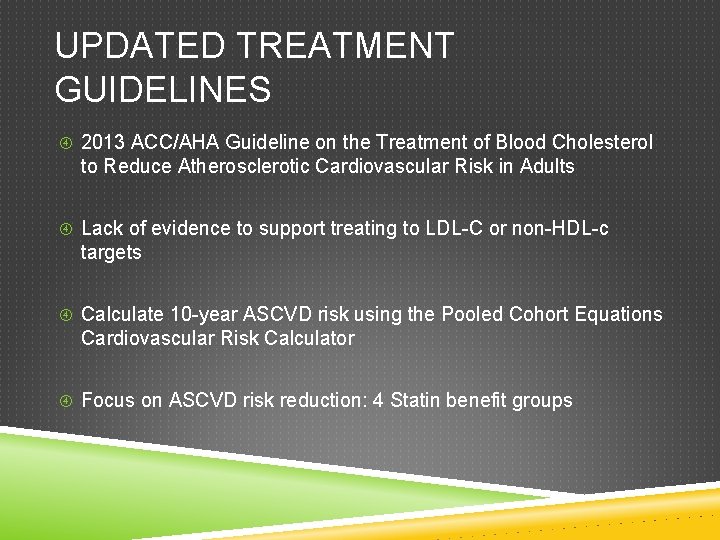
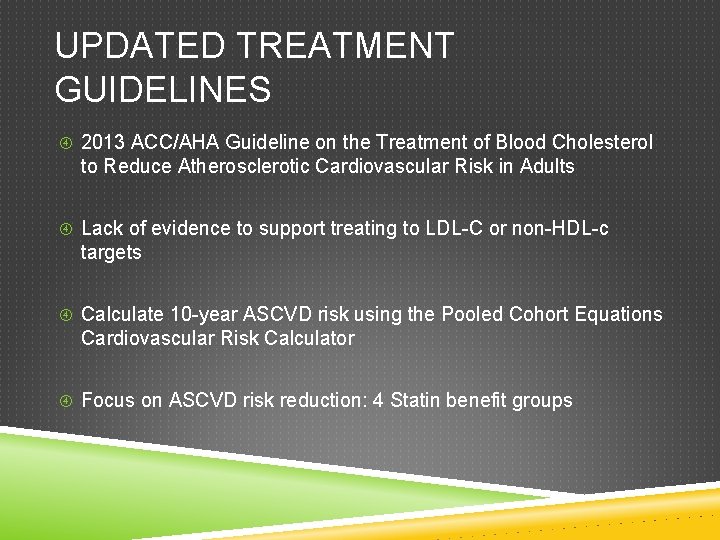
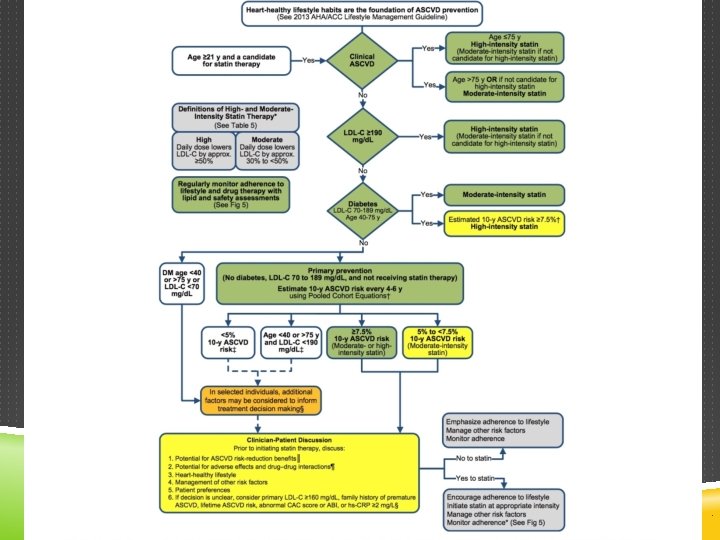
UPDATED TREATMENT GUIDELINES 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults Lack of evidence to support treating to LDL-C or non-HDL-c targets Calculate 10 -year ASCVD risk using the Pooled Cohort Equations Cardiovascular Risk Calculator Focus on ASCVD risk reduction: 4 Statin benefit groups
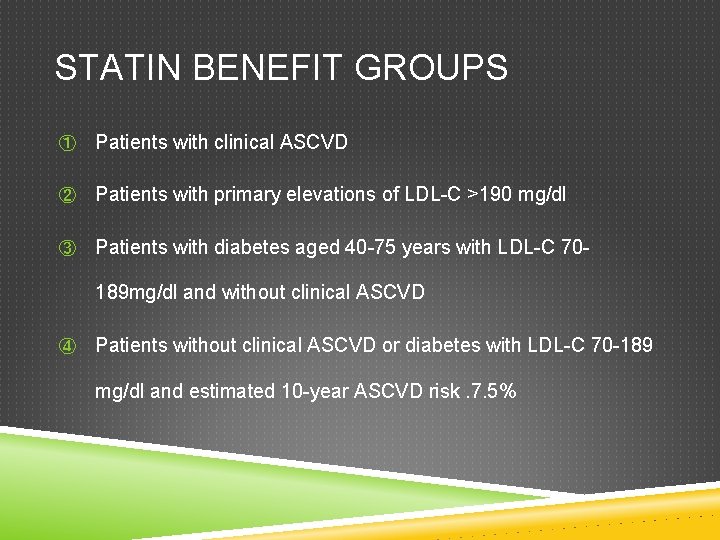
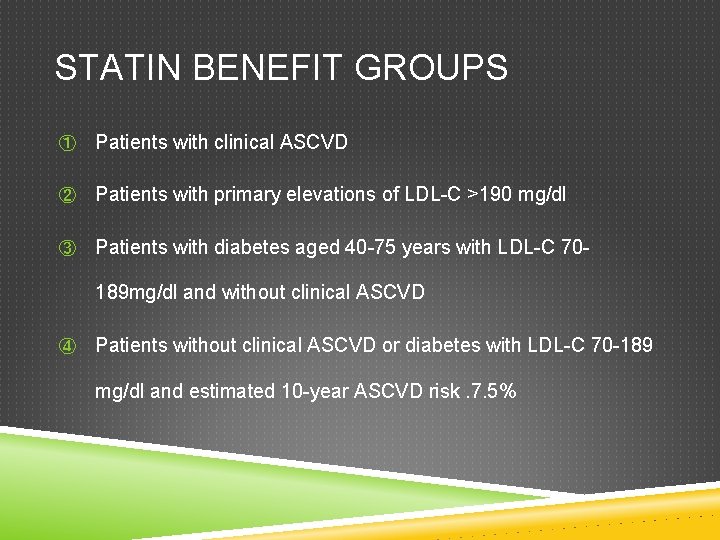
STATIN BENEFIT GROUPS ① Patients with clinical ASCVD ② Patients with primary elevations of LDL-C >190 mg/dl ③ Patients with diabetes aged 40 -75 years with LDL-C 70189 mg/dl and without clinical ASCVD ④ Patients without clinical ASCVD or diabetes with LDL-C 70 -189 mg/dl and estimated 10 -year ASCVD risk. 7. 5%
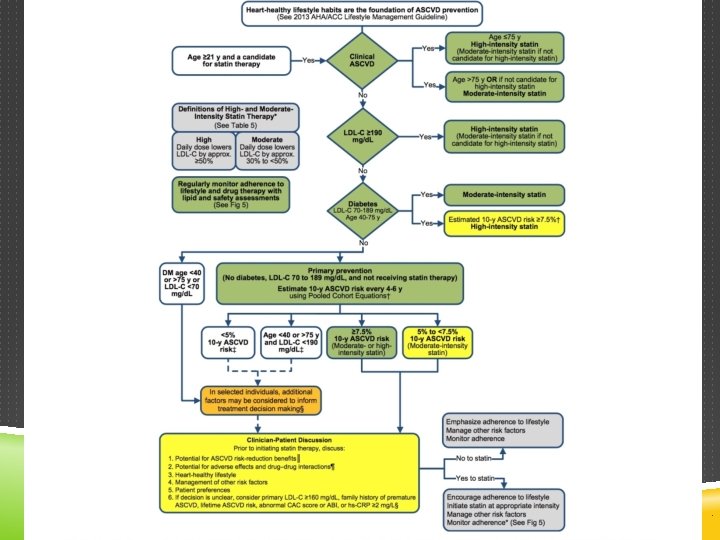
CV RISK ASSESSMENT CALCULATION ACC/AHA 2013 ASCVD Risk Calculator
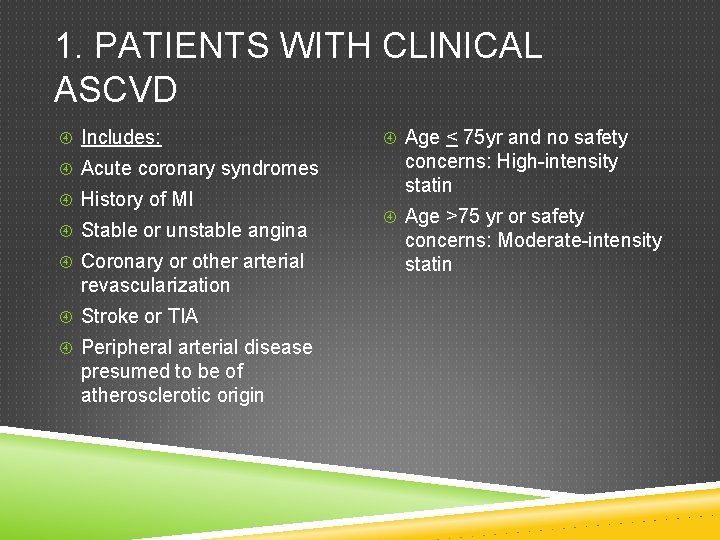
1. PATIENTS WITH CLINICAL ASCVD Includes: Acute coronary syndromes History of MI Stable or unstable angina Coronary or other arterial revascularization Stroke or TIA Peripheral arterial disease presumed to be of atherosclerotic origin Age < 75 yr and no safety concerns: High-intensity statin Age >75 yr or safety concerns: Moderate-intensity statin
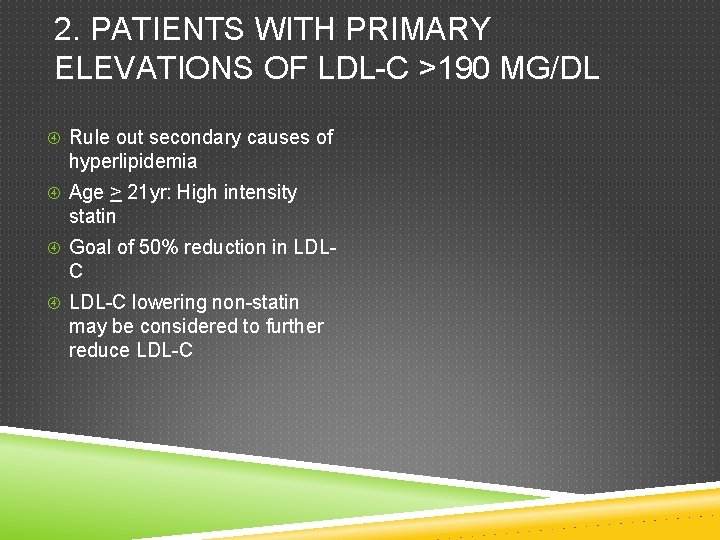
2. PATIENTS WITH PRIMARY ELEVATIONS OF LDL-C >190 MG/DL Rule out secondary causes of hyperlipidemia Age > 21 yr: High intensity statin Goal of 50% reduction in LDL- C LDL-C lowering non-statin may be considered to further reduce LDL-C
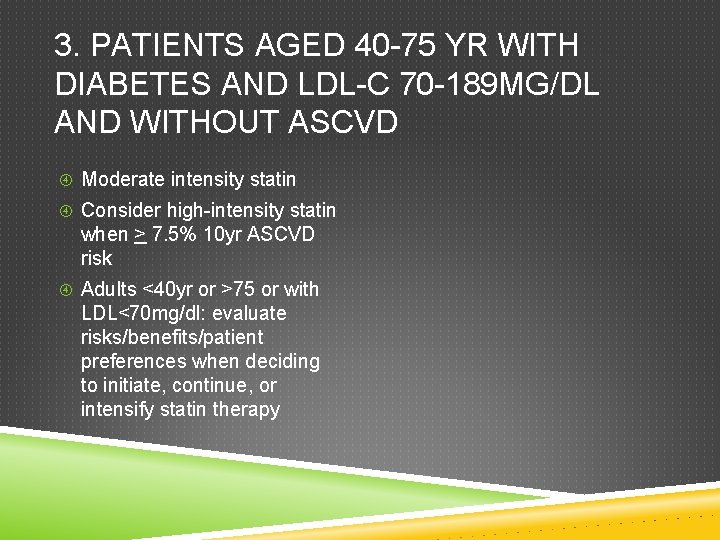
3. PATIENTS AGED 40 -75 YR WITH DIABETES AND LDL-C 70 -189 MG/DL AND WITHOUT ASCVD Moderate intensity statin Consider high-intensity statin when > 7. 5% 10 yr ASCVD risk Adults <40 yr or >75 or with LDL<70 mg/dl: evaluate risks/benefits/patient preferences when deciding to initiate, continue, or intensify statin therapy
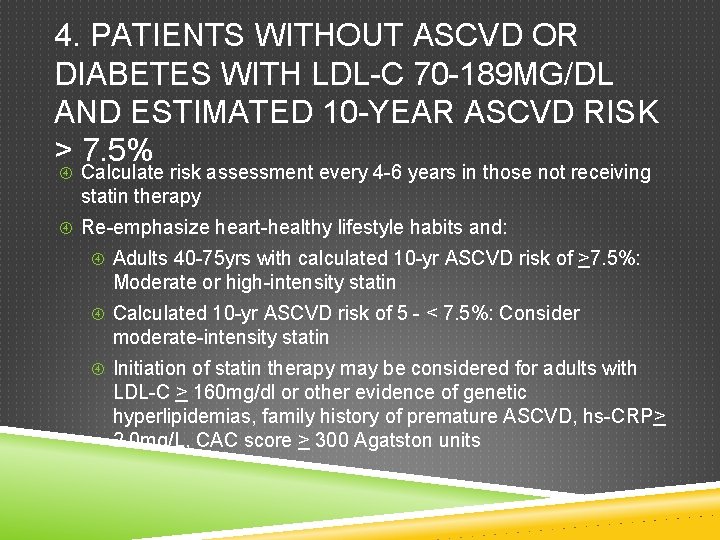
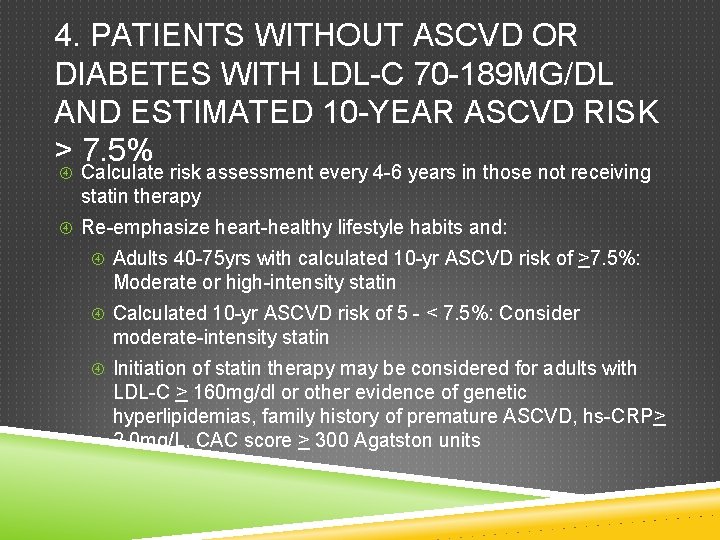
4. PATIENTS WITHOUT ASCVD OR DIABETES WITH LDL-C 70 -189 MG/DL AND ESTIMATED 10 -YEAR ASCVD RISK > 7. 5% Calculate risk assessment every 4 -6 years in those not receiving statin therapy Re-emphasize heart-healthy lifestyle habits and: Adults 40 -75 yrs with calculated 10 -yr ASCVD risk of >7. 5%: Moderate or high-intensity statin Calculated 10 -yr ASCVD risk of 5 - < 7. 5%: Consider moderate-intensity statin Initiation of statin therapy may be considered for adults with LDL-C > 160 mg/dl or other evidence of genetic hyperlipidemias, family history of premature ASCVD, hs-CRP> 2. 0 mg/L, CAC score > 300 Agatston units
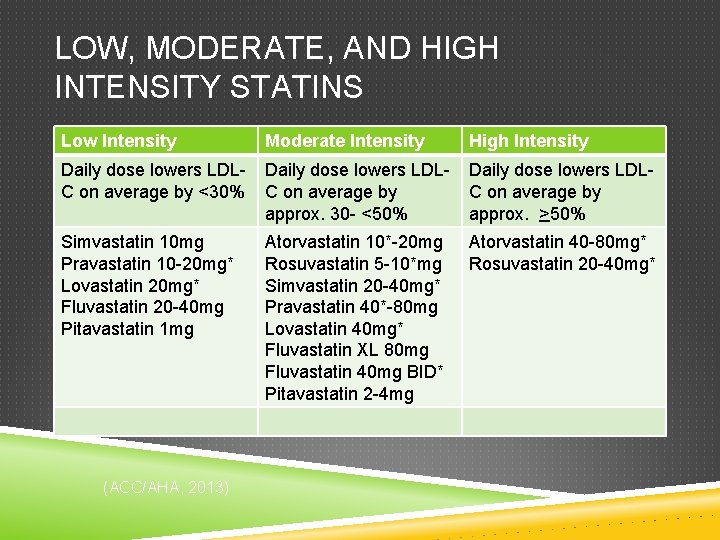
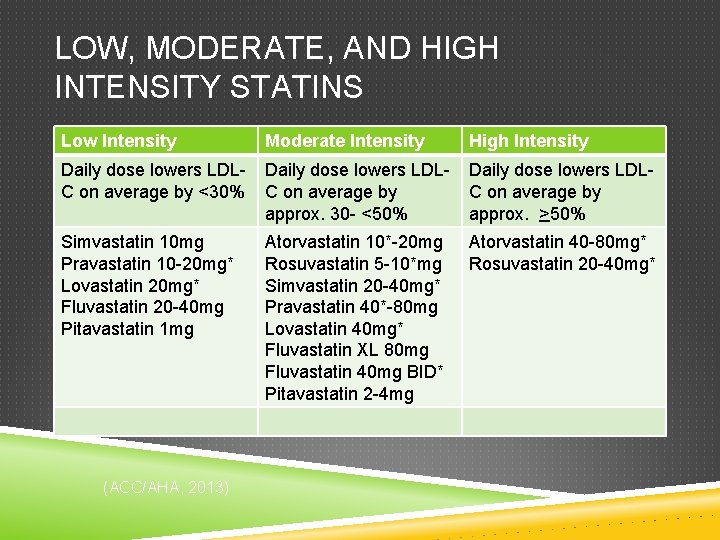
LOW, MODERATE, AND HIGH INTENSITY STATINS Low Intensity Moderate Intensity High Intensity Daily dose lowers LDLC on average by <30% Daily dose lowers LDLC on average by approx. 30 - <50% Daily dose lowers LDLC on average by approx. >50% Simvastatin 10 mg Pravastatin 10 -20 mg* Lovastatin 20 mg* Fluvastatin 20 -40 mg Pitavastatin 1 mg Atorvastatin 10*-20 mg Rosuvastatin 5 -10*mg Simvastatin 20 -40 mg* Pravastatin 40*-80 mg Lovastatin 40 mg* Fluvastatin XL 80 mg Fluvastatin 40 mg BID* Pitavastatin 2 -4 mg Atorvastatin 40 -80 mg* Rosuvastatin 20 -40 mg* (ACC/AHA, 2013)

STATINS: LDL LOWERING RATES Lovastatin Mevacor 20 mg=29% 40 mg=31% 80 mg=48% Pravastatin Pravachor 10 mg=19% 20 mg=29% 40 mg=34% 80 mg=48% Simvastatin Zocor 10 mg=28% 20 mg=35% 40 mg=40% 80 mg=48% 20 mg=17% 40 mg=23% 80 mg=33% Fluvastatin Lescol Atorvastatin Lipitor 10 mg=38% 20 mg=46% 40 mg=51% 80 mg=54% Rosuvastatin Crestor 5 mg=43% 10 mg=50% 20 mg=53% 40 mg=62% 1 mg=30% 2 mg=36% 4 mg=45% Pitavastatin Livalo • Contraindications: Active or chronic liver disease, pregnancy (Cat. X), lactation • Use with caution: Age >75 yr, concomitant use of cyclosporine, erythromycin, itraconazole, ketoconazole, fibric acid, diltiazem, verapamil, fluoxetine, nefazodone, gemfibrozil, niacin, antifungal
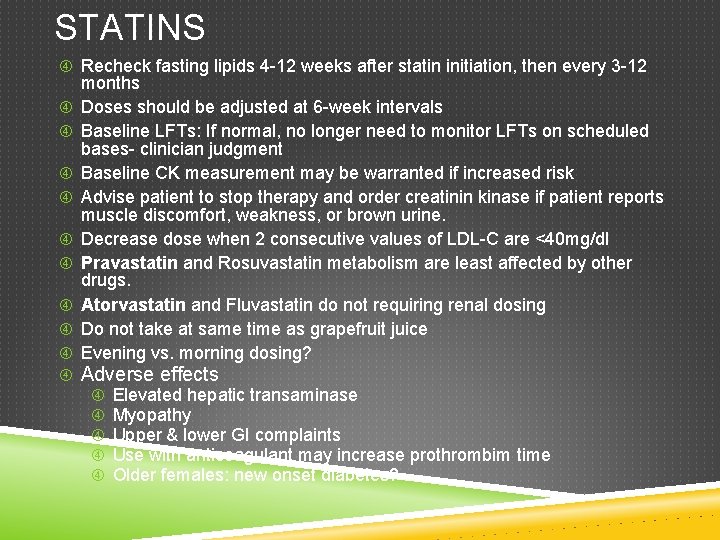
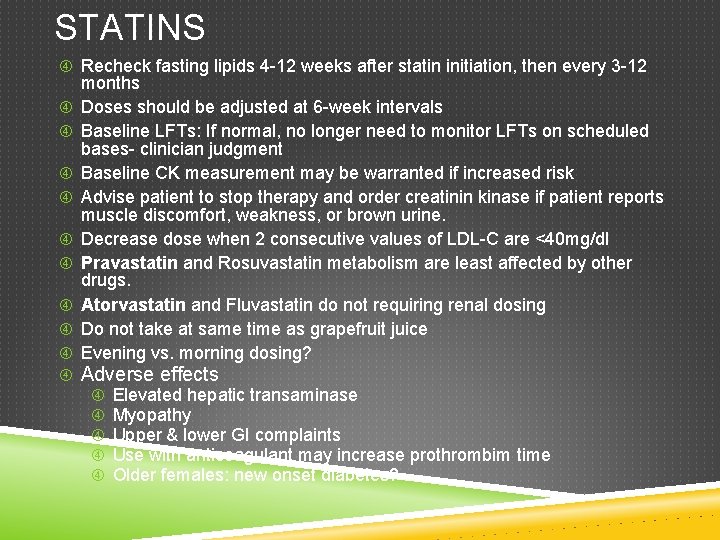
STATINS Recheck fasting lipids 4 -12 weeks after statin initiation, then every 3 -12 months Doses should be adjusted at 6 -week intervals Baseline LFTs: If normal, no longer need to monitor LFTs on scheduled bases- clinician judgment Baseline CK measurement may be warranted if increased risk Advise patient to stop therapy and order creatinin kinase if patient reports muscle discomfort, weakness, or brown urine. Decrease dose when 2 consecutive values of LDL-C are <40 mg/dl Pravastatin and Rosuvastatin metabolism are least affected by other drugs. Atorvastatin and Fluvastatin do not requiring renal dosing Do not take at same time as grapefruit juice Evening vs. morning dosing? Adverse effects Elevated hepatic transaminase Myopathy Upper & lower GI complaints Use with anticoagulant may increase prothrombim time Older females: new onset diabetes?
MANAGEMENT OF HYPERLIPIDEMIA Heart Healthy Lifestyle Habits Emphasize reduction in saturated fat & cholesterol Encourage moderate physical activity Consider referral to a dietitian Healthy food changes Weight reduction Physical activity Smoking cessation Limit alcohol
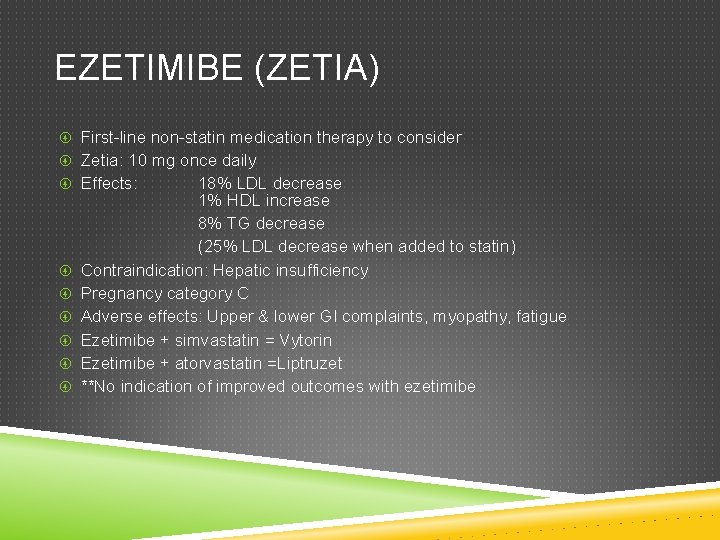
EZETIMIBE (ZETIA) First-line non-statin medication therapy to consider Zetia: 10 mg once daily Effects: 18% LDL decrease 1% HDL increase 8% TG decrease (25% LDL decrease when added to statin) Contraindication: Hepatic insufficiency Pregnancy category C Adverse effects: Upper & lower GI complaints, myopathy, fatigue Ezetimibe + simvastatin = Vytorin Ezetimibe + atorvastatin =Liptruzet **No indication of improved outcomes with ezetimibe
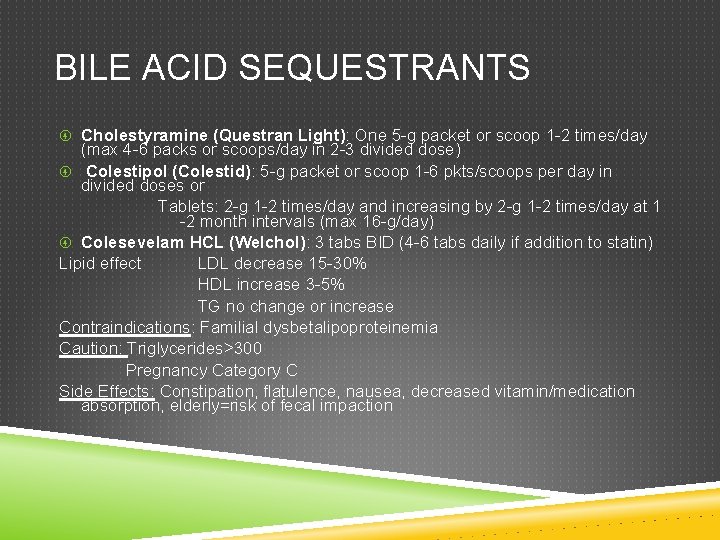
BILE ACID SEQUESTRANTS Cholestyramine (Questran Light): One 5 -g packet or scoop 1 -2 times/day (max 4 -6 packs or scoops/day in 2 -3 divided dose) Colestipol (Colestid): 5 -g packet or scoop 1 -6 pkts/scoops per day in divided doses or Tablets: 2 -g 1 -2 times/day and increasing by 2 -g 1 -2 times/day at 1 -2 month intervals (max 16 -g/day) Colesevelam HCL (Welchol): 3 tabs BID (4 -6 tabs daily if addition to statin) Lipid effect LDL decrease 15 -30% HDL increase 3 -5% TG no change or increase Contraindications: Familial dysbetalipoproteinemia Caution: Triglycerides>300 Pregnancy Category C Side Effects: Constipation, flatulence, nausea, decreased vitamin/medication absorption, elderly=risk of fecal impaction
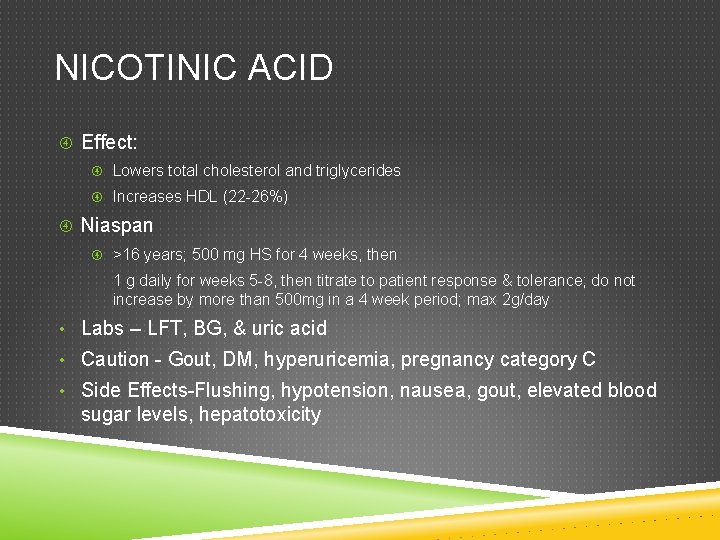
NICOTINIC ACID Effect: Lowers total cholesterol and triglycerides Increases HDL (22 -26%) Niaspan >16 years; 500 mg HS for 4 weeks, then 1 g daily for weeks 5 -8, then titrate to patient response & tolerance; do not increase by more than 500 mg in a 4 week period; max 2 g/day • Labs – LFT, BG, & uric acid • Caution - Gout, DM, hyperuricemia, pregnancy category C • Side Effects-Flushing, hypotension, nausea, gout, elevated blood sugar levels, hepatotoxicity
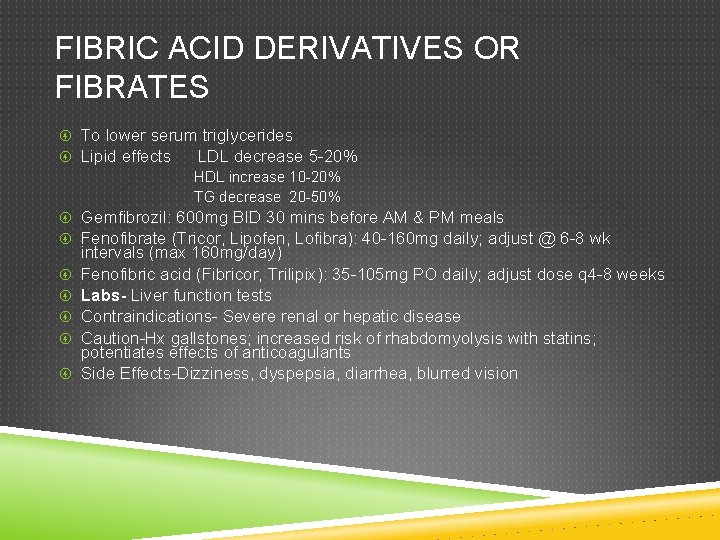
FIBRIC ACID DERIVATIVES OR FIBRATES To lower serum triglycerides Lipid effects LDL decrease 5 -20% HDL increase 10 -20% TG decrease 20 -50% Gemfibrozil: 600 mg BID 30 mins before AM & PM meals Fenofibrate (Tricor, Lipofen, Lofibra): 40 -160 mg daily; adjust @ 6 -8 wk intervals (max 160 mg/day) Fenofibric acid (Fibricor, Trilipix): 35 -105 mg PO daily; adjust dose q 4 -8 weeks Labs- Liver function tests Contraindications- Severe renal or hepatic disease Caution-Hx gallstones; increased risk of rhabdomyolysis with statins; potentiates effects of anticoagulants Side Effects-Dizziness, dyspepsia, diarrhea, blurred vision
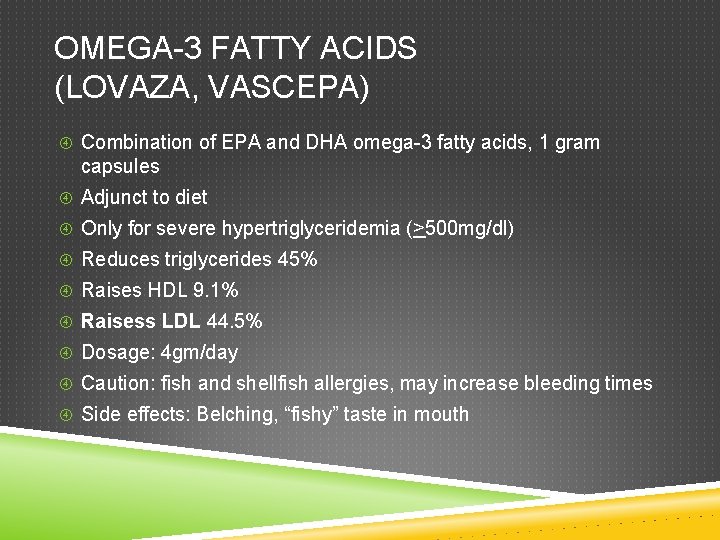
OMEGA-3 FATTY ACIDS (LOVAZA, VASCEPA) Combination of EPA and DHA omega-3 fatty acids, 1 gram capsules Adjunct to diet Only for severe hypertriglyceridemia (>500 mg/dl) Reduces triglycerides 45% Raises HDL 9. 1% Raisess LDL 44. 5% Dosage: 4 gm/day Caution: fish and shellfish allergies, may increase bleeding times Side effects: Belching, “fishy” taste in mouth
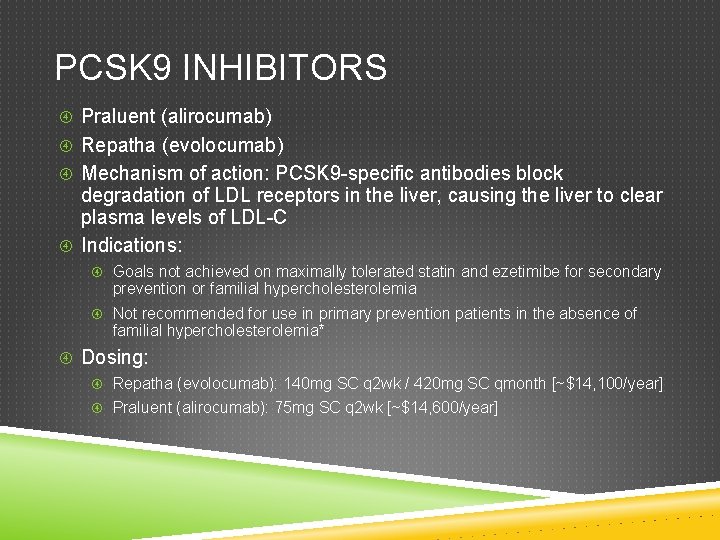
PCSK 9 INHIBITORS Praluent (alirocumab) Repatha (evolocumab) Mechanism of action: PCSK 9 -specific antibodies block degradation of LDL receptors in the liver, causing the liver to clear plasma levels of LDL-C Indications: Goals not achieved on maximally tolerated statin and ezetimibe for secondary prevention or familial hypercholesterolemia Not recommended for use in primary prevention patients in the absence of familial hypercholesterolemia* Dosing: Repatha (evolocumab): 140 mg SC q 2 wk / 420 mg SC qmonth [~$14, 100/year] Praluent (alirocumab): 75 mg SC q 2 wk [~$14, 600/year]