HYPERLIPIDAEMIAS Dr D Rispa Assistant Professor Pharmacy Practice






- Slides: 32

HYPERLIPIDAEMIAS Dr. D. Rispa Assistant Professor Pharmacy Practice Department

Definition § Hyperlipidemia, hyperlipoproteinemia, or hyperlipidaemia involves abnormally elevated levels of any or all lipids and/or lipoproteins in the blood. § It is the most common form of dyslipidemia (which also includes any decreased lipid levels).
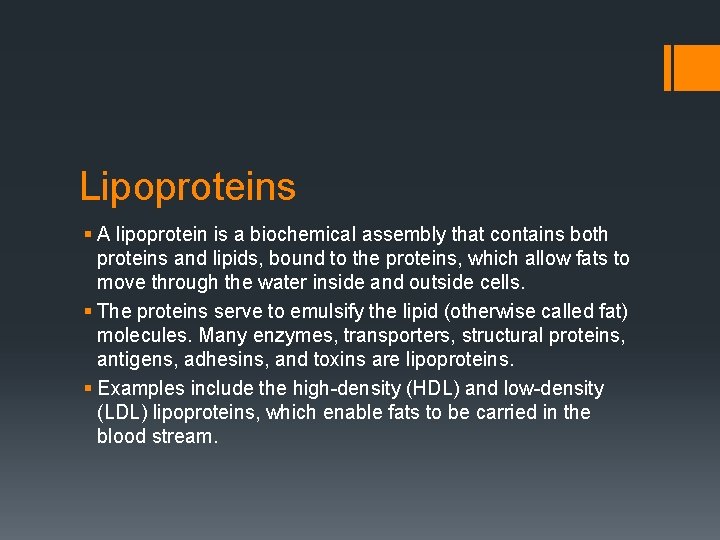
Lipoproteins § A lipoprotein is a biochemical assembly that contains both proteins and lipids, bound to the proteins, which allow fats to move through the water inside and outside cells. § The proteins serve to emulsify the lipid (otherwise called fat) molecules. Many enzymes, transporters, structural proteins, antigens, adhesins, and toxins are lipoproteins. § Examples include the high-density (HDL) and low-density (LDL) lipoproteins, which enable fats to be carried in the blood stream.
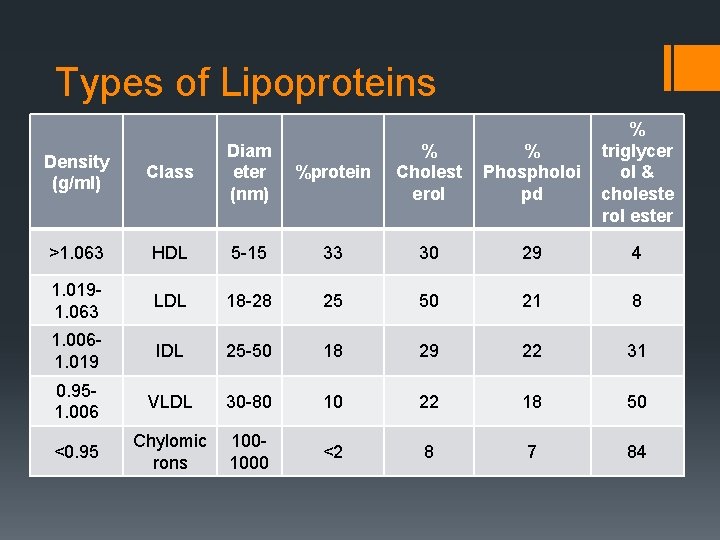
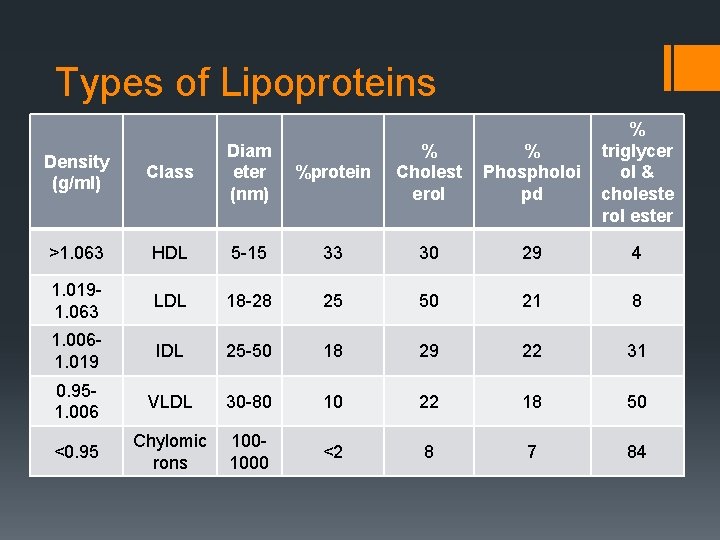
Types of Lipoproteins %protein % Cholest erol % Phospholoi pd % triglycer ol & choleste rol ester 5 -15 33 30 29 4 LDL 18 -28 25 50 21 8 1. 0061. 019 IDL 25 -50 18 29 22 31 0. 951. 006 VLDL 30 -80 10 22 18 50 <0. 95 Chylomic rons 1001000 <2 8 7 84 Class Diam eter (nm) >1. 063 HDL 1. 0191. 063 Density (g/ml)
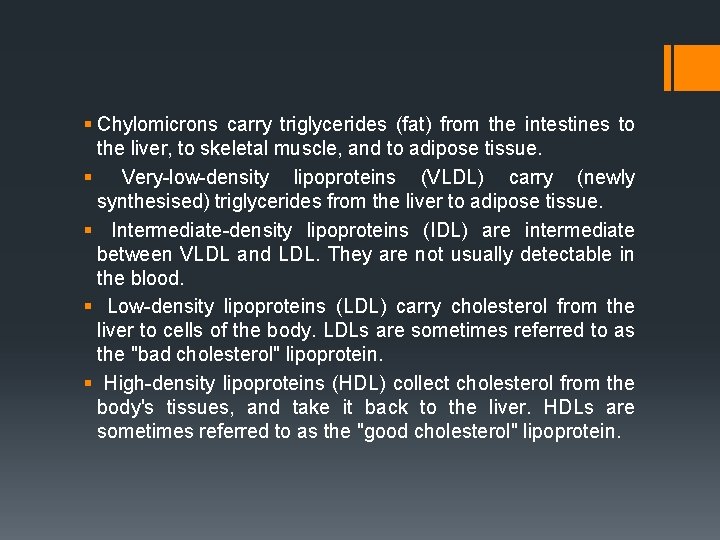
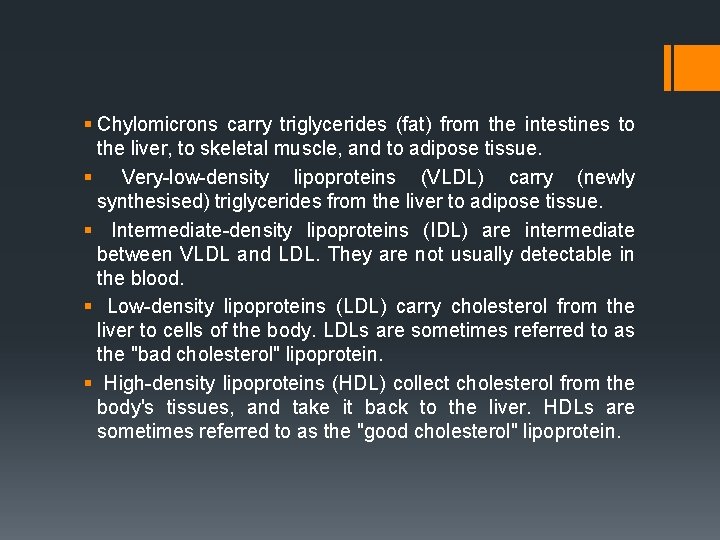
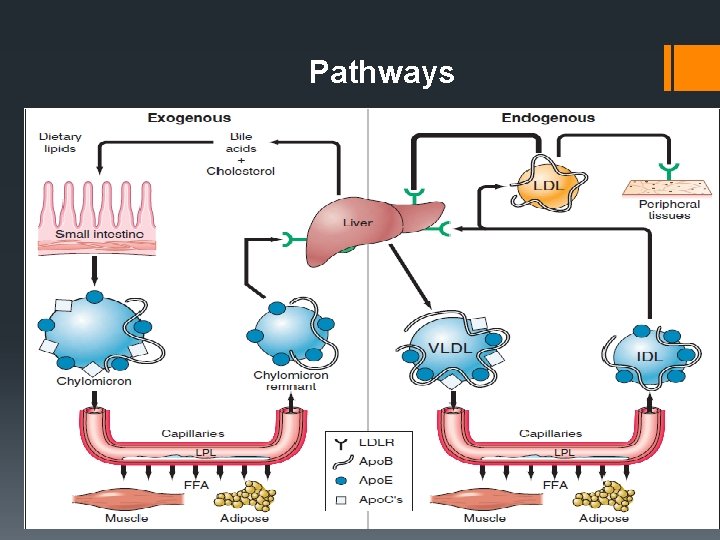
§ Chylomicrons carry triglycerides (fat) from the intestines to the liver, to skeletal muscle, and to adipose tissue. § Very-low-density lipoproteins (VLDL) carry (newly synthesised) triglycerides from the liver to adipose tissue. § Intermediate-density lipoproteins (IDL) are intermediate between VLDL and LDL. They are not usually detectable in the blood. § Low-density lipoproteins (LDL) carry cholesterol from the liver to cells of the body. LDLs are sometimes referred to as the "bad cholesterol" lipoprotein. § High-density lipoproteins (HDL) collect cholesterol from the body's tissues, and take it back to the liver. HDLs are sometimes referred to as the "good cholesterol" lipoprotein.
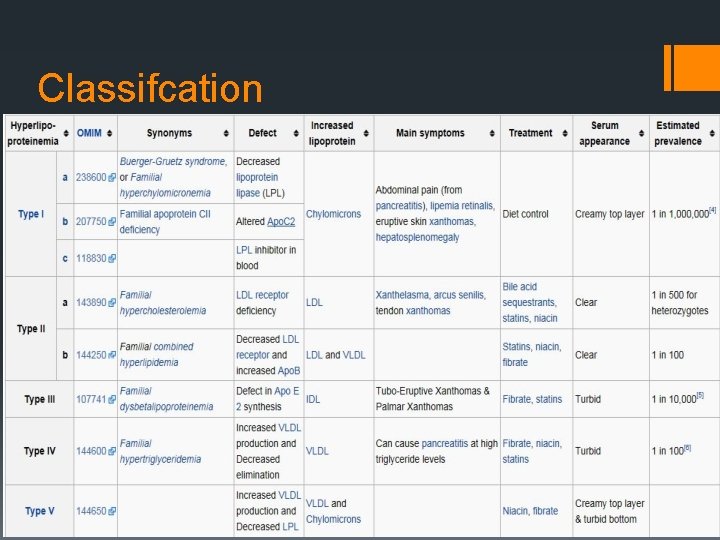
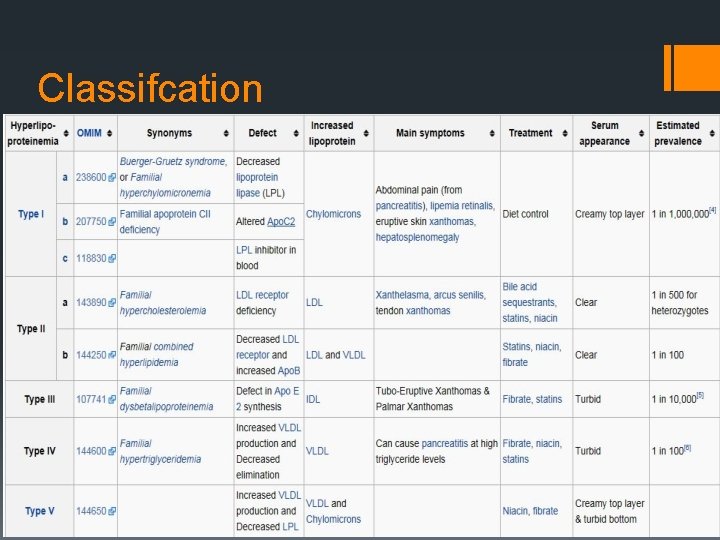
Classifcation
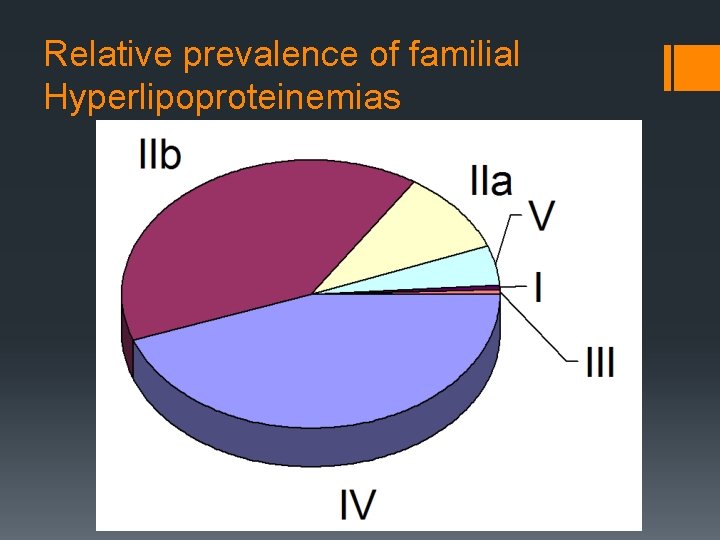
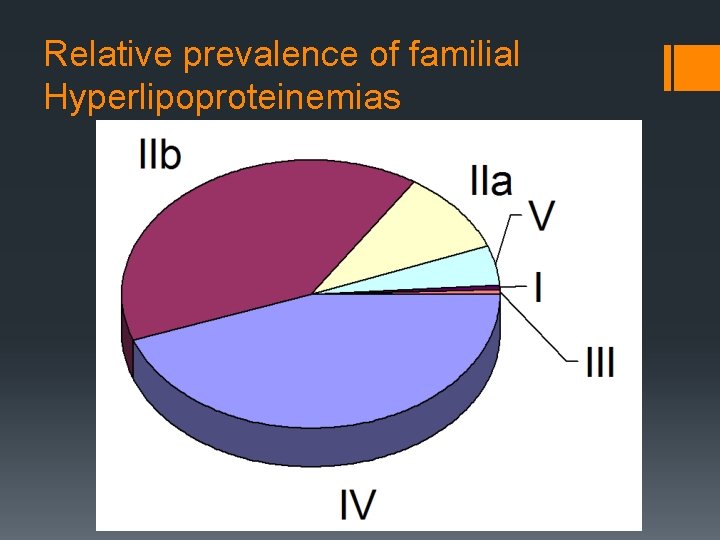
Relative prevalence of familial Hyperlipoproteinemias
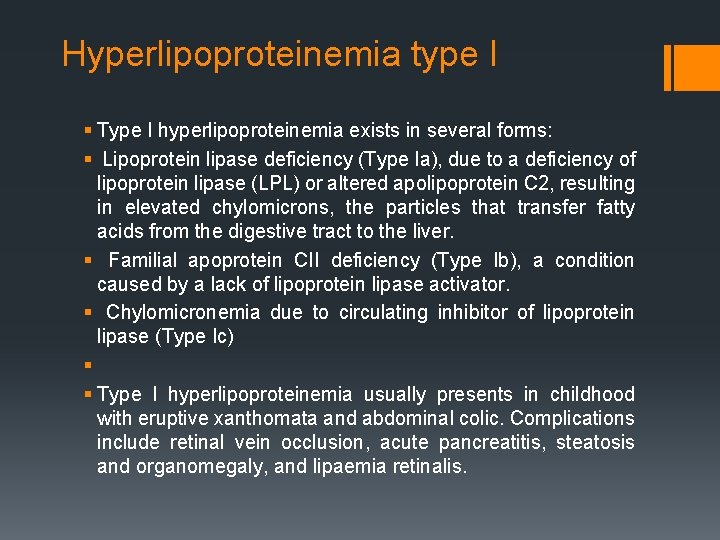
Hyperlipoproteinemia type I § Type I hyperlipoproteinemia exists in several forms: § Lipoprotein lipase deficiency (Type Ia), due to a deficiency of lipoprotein lipase (LPL) or altered apolipoprotein C 2, resulting in elevated chylomicrons, the particles that transfer fatty acids from the digestive tract to the liver. § Familial apoprotein CII deficiency (Type Ib), a condition caused by a lack of lipoprotein lipase activator. § Chylomicronemia due to circulating inhibitor of lipoprotein lipase (Type Ic) § § Type I hyperlipoproteinemia usually presents in childhood with eruptive xanthomata and abdominal colic. Complications include retinal vein occlusion, acute pancreatitis, steatosis and organomegaly, and lipaemia retinalis.
Hyperlipoproteinemia type II § Hyperlipoproteinemia type II, by far the most common form, is further classified into type IIa and type IIb, depending mainly on whethere is elevation in the triglyceride level in addition to LDL cholesterol. § Type II (a) § This may be sporadic (due to dietary factors), polygenic, or truly familial as a result of a mutation either in the LDL receptor gene on chromosome 19 (0. 2% of the population) or the Apo. B gene (0. 2%). The familial form is characterized by tendon xanthoma, xanthelasma and premature cardiovascular disease. The incidence of this disease is about 1 in 500 for heterozygotes, and 1 in 1, 000 for homozygotes. § Type II (b) § The high VLDL levels are due to overproduction of substrates, including triglycerides, acetyl Co. A, and an increase in B-100 synthesis. They may also be caused by the decreased clearance of LDL. Prevalence in the population is 10%. § Familial combined hyperlipoproteinemia (FCH) § Lysosomal acid lipase deficiency, often called (Cholesteryl ester storage disease) § Secondary combined hyperlipoproteinemia (usually in the context of metabolic syndrome, for which it is a diagnostic criterion)
Hyperlipoproteinemia type III § This form is due to high chylomicrons and IDL (intermediate density lipoprotein). Also known as broad beta disease or dysbetalipoproteinemia, the most common cause for this form is the presence of Apo. E E 2/E 2 genotype. § It is due to cholesterol-rich VLDL (β-VLDL). Its prevalence has been estimated to be approximately 1 in 10, 000. Hyperlipoproteinemia type IV § Familial hypertriglyceridemia is an autosomal recessive condition occurring in approximately 1% of the population. Hyperlipoproteinemia type V § Hyperlipoproteinemia type V is very similar to type I, but with high VLDL in addition to chylomicrons. § It is also associated with glucose intolerance and hyperuricemia.
Acquired (secondary) § Acquired hyperlipidemias (also called secondary dyslipoproteinemias) often mimic primary forms of hyperlipidemia and can have similar consequences. § They may result in increased risk of premature atherosclerosis or, when associated with marked hypertriglyceridemia, may lead to pancreatitis and other complications of the chylomicronemia syndrome. § The most common causes of acquired hyperlipidemia are: ü diabetes mellitus ü Use of drugs such as diuretics, beta blockers, and estrogens § Other conditions leading to acquired hyperlipidemia include: ü Hypothyroidism ü ü renal failure nephrotic syndrome alcohol usage Some rare endocrine disorders and metabolic disorders.
Epidemiology § Lipid and lipoprotein concentrations vary among different populations with countries consuming a western type of diet having higher TC and LDL levels than those where regular consumption of saturated fat is low. § Despite a 50% reduction in the death rate from CVD over the past 25 years, It remains the leading cause of premature death and morbidity in the UK. § The higher levels of TC in an individual the greater the chance of developing CVD. § TC levels tend to increase with age such that 80% of British men aged 45 -64 years have a level that exceeds 5 mmol/lit and the population average is 5. 6 mmol/lit, in contrast in rural China and Japan the average is 4 mmol/lit.
Etiology § The etiology can be classified into primary and secondary causes. § Primary causes are due to single or multiple gene mutations resulting in a disturbance of LDL and triglyceride production or clearance. § They vary in location of genetic defect, inheritance pattern, prevalence, clinical features, and treatment. § At least 18 separate entities have been described. The suspicion for a primary lipid disorder should be especially high in patients with premature atherosclerotic disease, a family history of early atherosclerotic disease, a significantly elevated serum cholesterol level (>240 mg/d. L), and physical signs of hyperlipidemia. § Primary dyslipidemias are most commonly seen in children and young adults and cause only a small percentage of cases in adults.
§ Most adult cases of dyslipidemia are secondary in nature. § In Western civilizations, sedentary lifestyle and excessive consumption of saturated fats, trans-fatty acids, and cholesterol are the most important secondary causes. § Certain medical conditions are commonly associated with dyslipidemia, including chronic renal insufficiency, renal failure, diabetes mellitus, hypothyroidism, cholestatic liver disease, and alcohol dependency. § Certain drugs, including high-dose thiazide diuretics, oral estrogens, glucocorticoids, anabolic steroids, and atypical antipsychotics such as olanzapine and clozapine have also been implicated in causing mild-to-moderate degrees of dyslipidemia. § Use of atypical antipsychotics, such as olanzapine and clozapine, and of beta-blockers without intrinsic sympathomimetic or alphablocking activities are associated with reduced HDL-cholesterol levels.
Pathophysiology § Hypercholesterolemia develops as a consequence of abnormal lipoprotein metabolism, mainly reduction of LDL receptor expression or activity, and consequently diminishing hepatic LDL clearance from the plasma. § It is a major predisposing risk factor for the development of atherosclerosis. § This mechanism is classically seen in familial hypercholesterolemia and when excess saturated fat or cholesterol is ingested. § In addition, excessive production of VLDL by the liver, as seen in familial combined hyperlipidemia and insulin resistance states such as abdominal obesity and type 2 diabetes, can also induce hypercholesterolemia or mixed dyslipidemia.
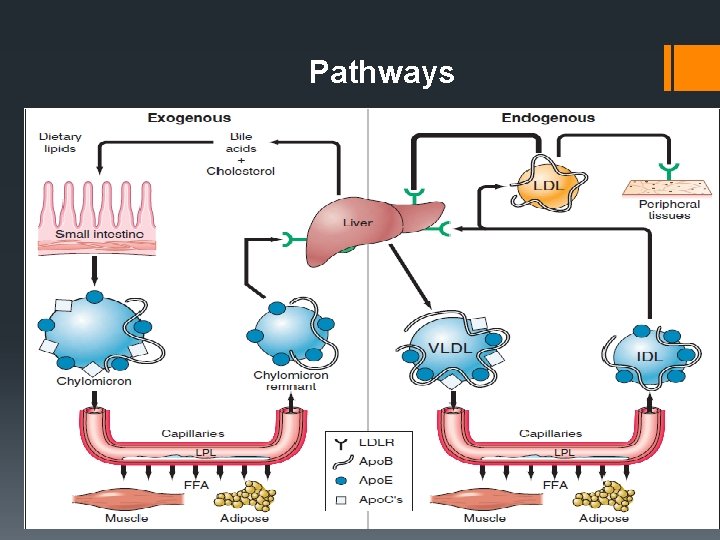
Pathways
§ A current theory for the initiating event in atherogenesis is that apoprotein B-100 -containing lipoproteins are retained in the subendothelial space, by means of a charge-mediated interaction with extracellular matrix and proteoglycans. § This allows reactive oxygen species to modify the surface phospholipids and unesterified cholesterol of the small LDL particles. § Circulating LDL can also be taken up into macrophages through unregulated scavenger receptors. § As a result of LDL oxidation, isoprostanes are formed. Isoprostanes are chemically stable, free radical-catalyzed products of arachidonic acid, and are structural isomers of conventional prostaglandins. § Isoprostane levels are increased in atherosclerotic lesions, but they may also be found as F 2 isoprostanes in the urine of asymptomatic patients with hypercholesterolemia.
§ A strong association exists between elevated plasma concentrations of oxidized LDL and CHD. § The mechanisms through which oxidized LDL promotes atherosclerosis are multiple and include damage to the endothelium, induction of growth factors, and recruitment of macrophages and monocytes. § Vasoconstriction in the setting of high levels of oxidized LDL seem to be related to a reduced release of the vasodilator nitric oxide from the damaged endothelial wall as well as increased platelet aggregation and thromboxane release. § Smooth muscle proliferation has been linked to the release of cytokines from activated platelets. § The state of hypercholesterolemia leads invariably to an excess accumulation of oxidized LDL within the macrophages, thereby transforming them into "foam" cells. The rupture of these cells can lead to further damage of the vessel wall due to the release of oxygen free radicals, oxidized LDL, and intracellular enzymes.
Symptoms § Hyperlipidemia usually does not cause symptoms. § Very high levels of lipids or triglycerides can cause: üFat deposits in the skin or tendons ( Xanthelasma and Xanthoma ) ü Pain, enlargement, or swelling of organs such as the liver, spleen, or pancreas ( Pancreatitis ) üObstruction of blood vessels in heart and brain § If not treated, high lipids can cause: üHeart Attack üStroke üAtherosclerosis (hardening of the arteries)

Diagnosis § This condition is diagnosed with blood tests. ü These tests measure the levels of lipids in the blood. ü The National Cholesterol Education Program advises that you have your lipids checked at least once every five years, starting at age 20. ü Also, the American Academy of Pediatrics recommends lipid screening for children at risk (eg, a family history of hyperlipidemia). § Testing may consist of a fasting blood test for: ü Total cholesterol ü LDL (bad cholesterol) ü HDL (good cholesterol) ü Triglycerides § Your doctor may recommend more frequent or earlier testing if you have: ü Family history of hyperlipidemia. ü Risk factor or disease that may cause hyperlipidemia. ü Complication that may result from hyperlipidemia.

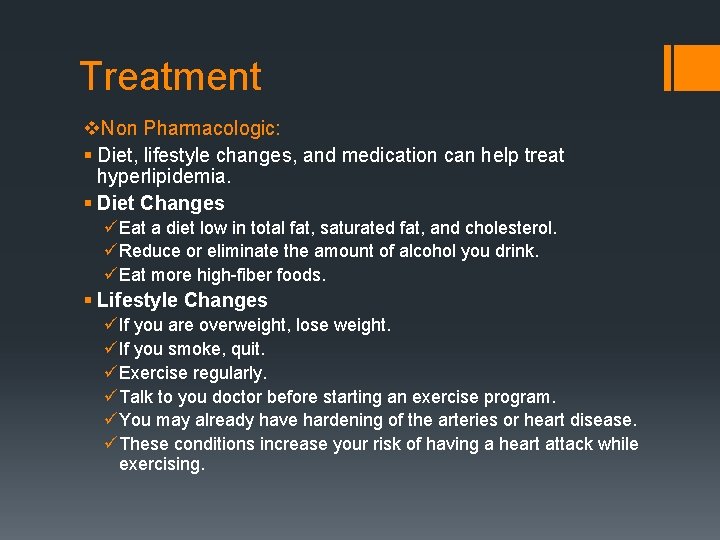
Treatment v. Non Pharmacologic: § Diet, lifestyle changes, and medication can help treat hyperlipidemia. § Diet Changes üEat a diet low in total fat, saturated fat, and cholesterol. üReduce or eliminate the amount of alcohol you drink. üEat more high-fiber foods. § Lifestyle Changes üIf you are overweight, lose weight. üIf you smoke, quit. üExercise regularly. üTalk to you doctor before starting an exercise program. üYou may already have hardening of the arteries or heart disease. üThese conditions increase your risk of having a heart attack while exercising.
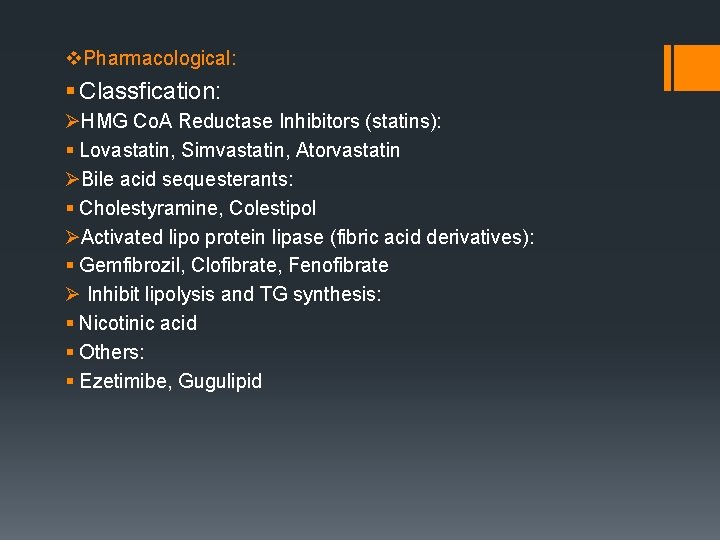
v. Pharmacological: § Classfication: ØHMG Co. A Reductase Inhibitors (statins): § Lovastatin, Simvastatin, Atorvastatin ØBile acid sequesterants: § Cholestyramine, Colestipol ØActivated lipo protein lipase (fibric acid derivatives): § Gemfibrozil, Clofibrate, Fenofibrate Ø Inhibit lipolysis and TG synthesis: § Nicotinic acid § Others: § Ezetimibe, Gugulipid

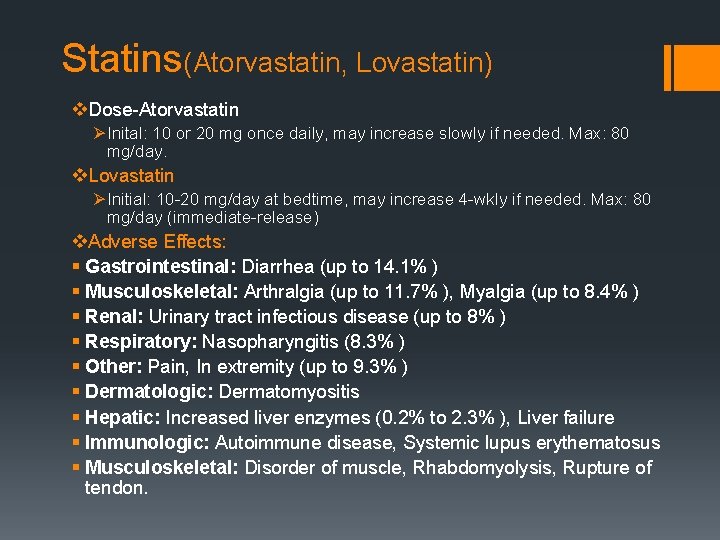
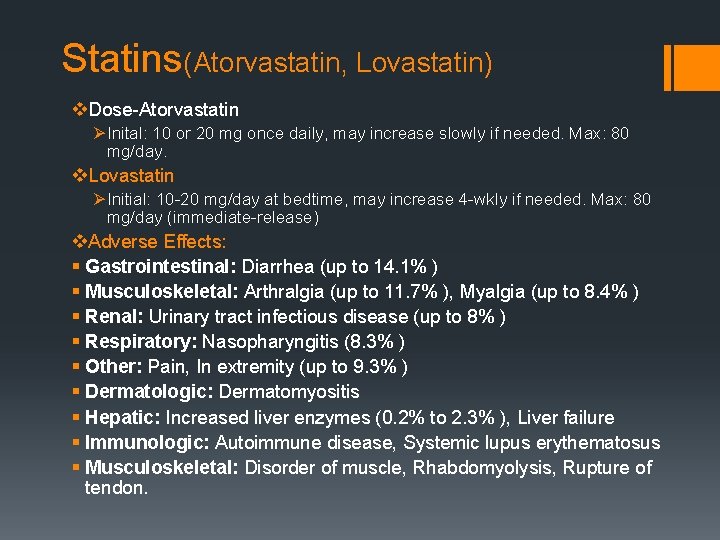
Statins(Atorvastatin, Lovastatin) v. Dose-Atorvastatin ØInital: 10 or 20 mg once daily, may increase slowly if needed. Max: 80 mg/day. v. Lovastatin ØInitial: 10 -20 mg/day at bedtime, may increase 4 -wkly if needed. Max: 80 mg/day (immediate-release) v. Adverse Effects: § Gastrointestinal: Diarrhea (up to 14. 1% ) § Musculoskeletal: Arthralgia (up to 11. 7% ), Myalgia (up to 8. 4% ) § Renal: Urinary tract infectious disease (up to 8% ) § Respiratory: Nasopharyngitis (8. 3% ) § Other: Pain, In extremity (up to 9. 3% ) § Dermatologic: Dermatomyositis § Hepatic: Increased liver enzymes (0. 2% to 2. 3% ), Liver failure § Immunologic: Autoimmune disease, Systemic lupus erythematosus § Musculoskeletal: Disorder of muscle, Rhabdomyolysis, Rupture of tendon.
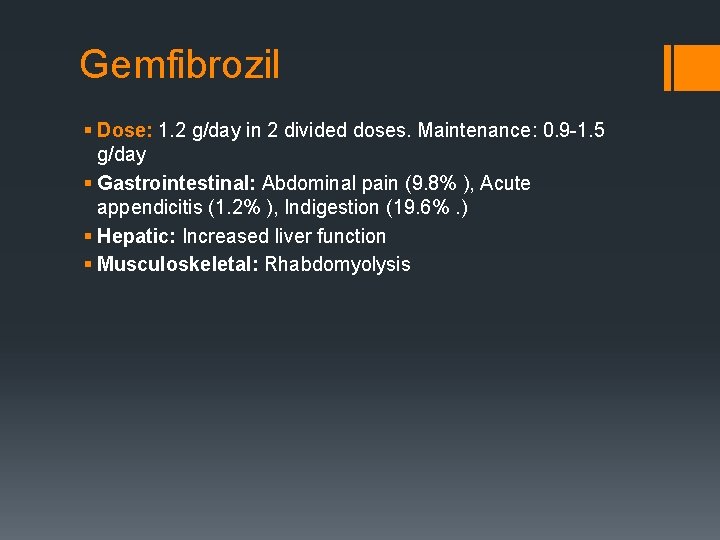
Gemfibrozil § Dose: 1. 2 g/day in 2 divided doses. Maintenance: 0. 9 -1. 5 g/day § Gastrointestinal: Abdominal pain (9. 8% ), Acute appendicitis (1. 2% ), Indigestion (19. 6%. ) § Hepatic: Increased liver function § Musculoskeletal: Rhabdomyolysis
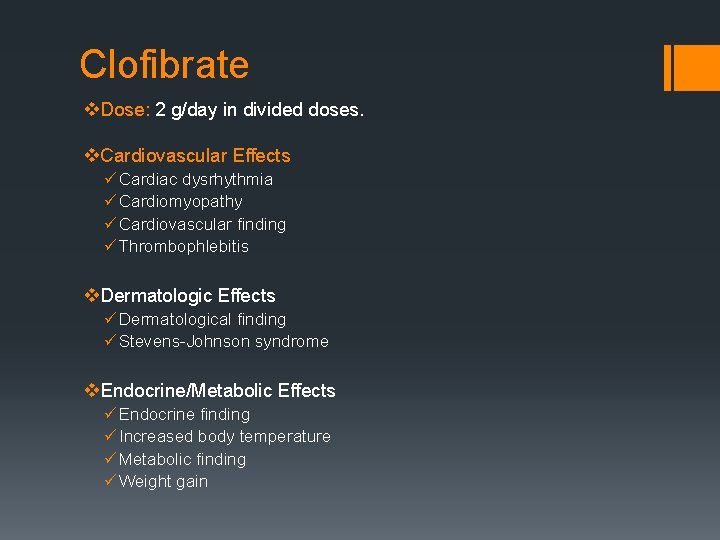
Clofibrate v. Dose: 2 g/day in divided doses. v. Cardiovascular Effects ü Cardiac dysrhythmia ü Cardiomyopathy ü Cardiovascular finding ü Thrombophlebitis v. Dermatologic Effects ü Dermatological finding ü Stevens-Johnson syndrome v. Endocrine/Metabolic Effects ü Endocrine finding ü Increased body temperature ü Metabolic finding ü Weight gain
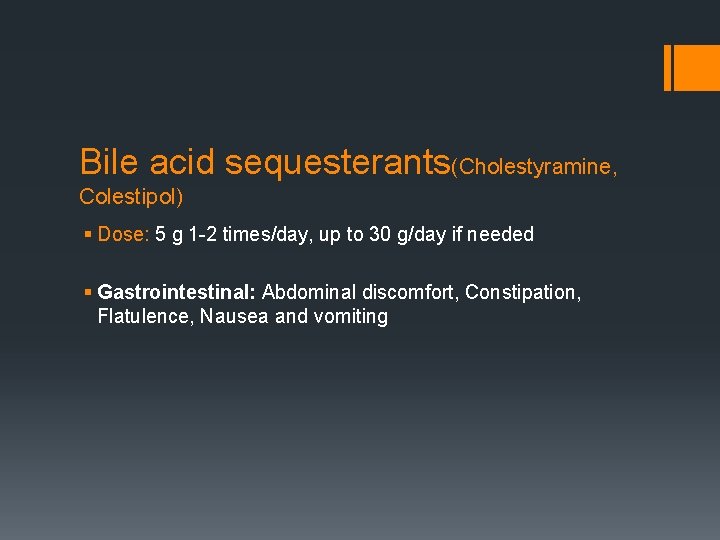
Bile acid sequesterants(Cholestyramine, Colestipol) § Dose: 5 g 1 -2 times/day, up to 30 g/day if needed § Gastrointestinal: Abdominal discomfort, Constipation, Flatulence, Nausea and vomiting
Niacin § Dermatologic: Flushing (88% ) § Gastrointestinal: Nausea (4% to 9% ), Vomiting (2% to 9% ) § Hepatic: Hepatic necrosis, Hepatotoxicity § Musculoskeletal: Rhabdomyolysis
Gugulipid § diarrhea § nausea § hiccup § abdominal discomfort § headache § restlessness § hypersensitivity rash

THANK YOU