Hyperglycemic crises DKA NKHHC Acute complications of DM


- Slides: 38
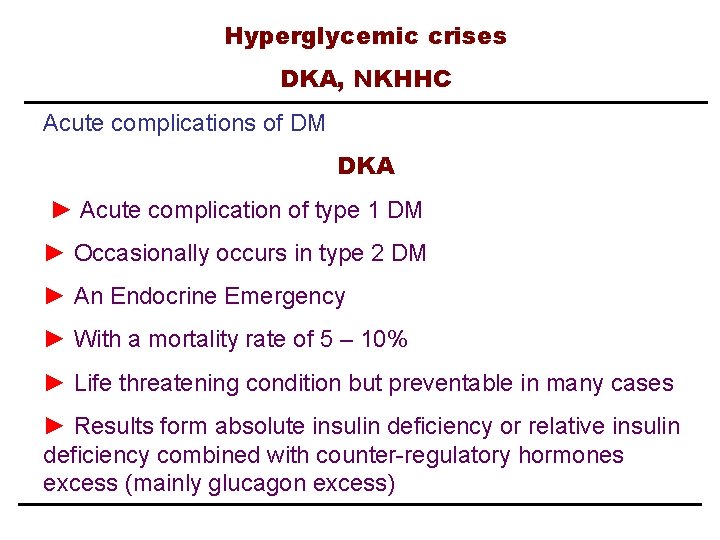
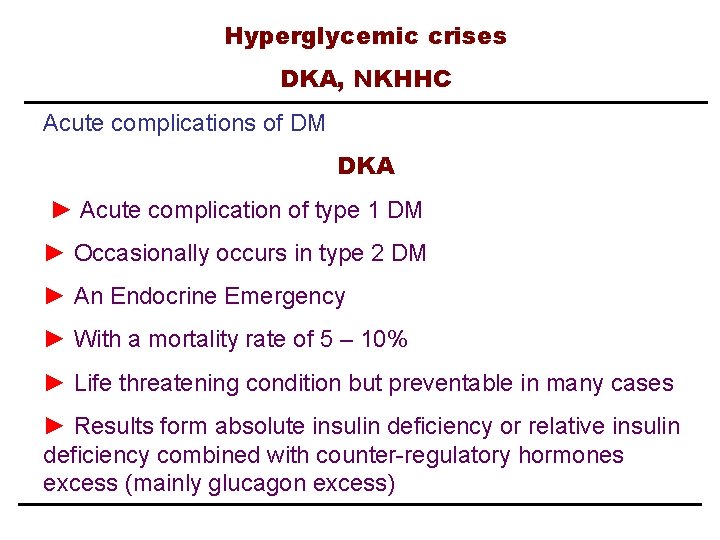
Hyperglycemic crises DKA, NKHHC Acute complications of DM DKA ► Acute complication of type 1 DM ► Occasionally occurs in type 2 DM ► An Endocrine Emergency ► With a mortality rate of 5 – 10% ► Life threatening condition but preventable in many cases ► Results form absolute insulin deficiency or relative insulin deficiency combined with counter-regulatory hormones excess (mainly glucagon excess)
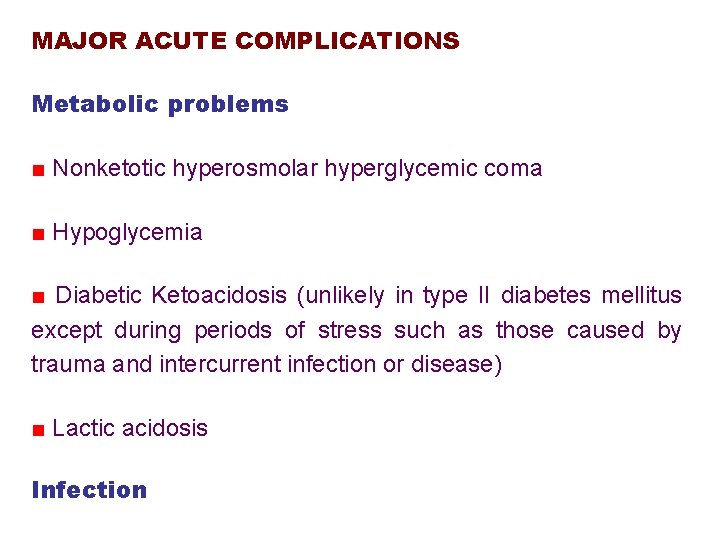
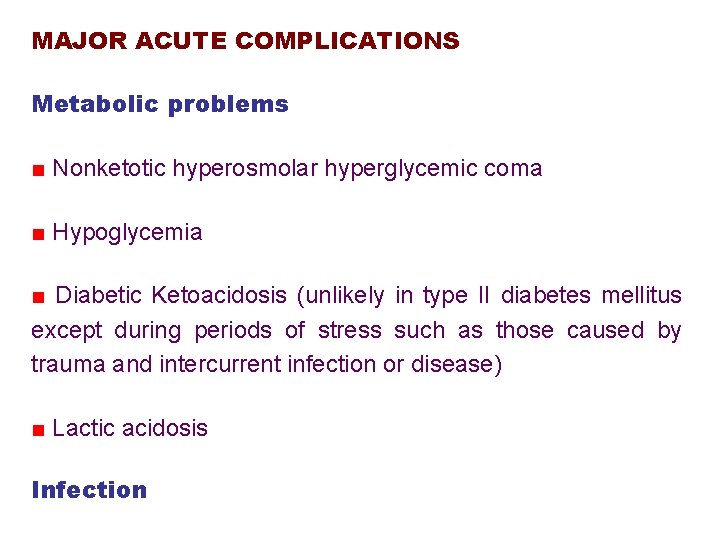
MAJOR ACUTE COMPLICATIONS Metabolic problems ■ Nonketotic hyperosmolar hyperglycemic coma ■ Hypoglycemia ■ Diabetic Ketoacidosis (unlikely in type II diabetes mellitus except during periods of stress such as those caused by trauma and intercurrent infection or disease) ■ Lactic acidosis Infection
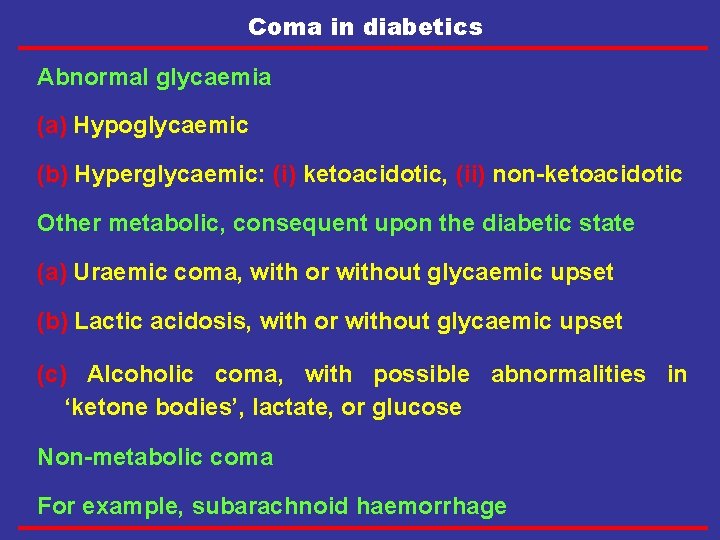
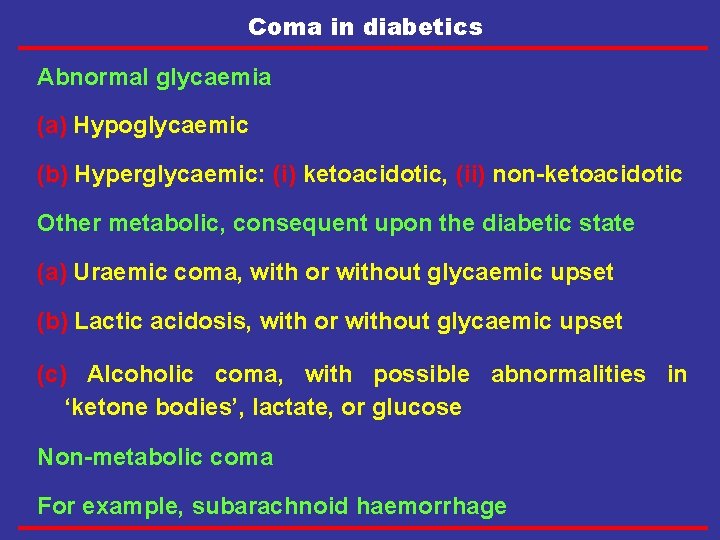
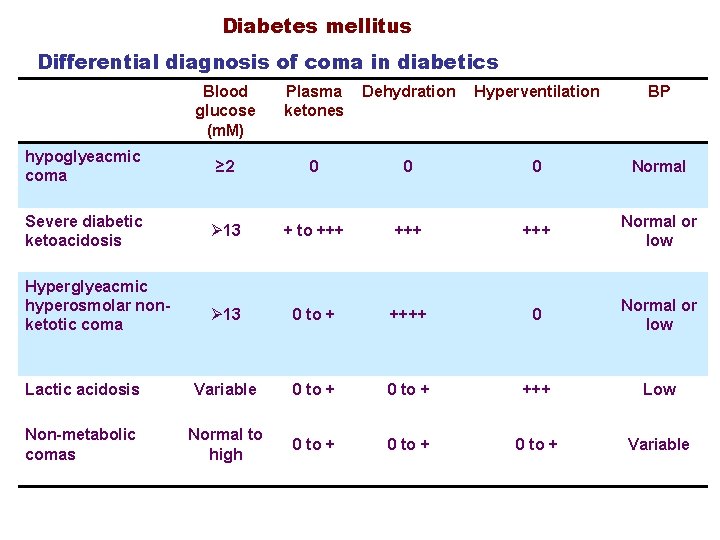
Coma in diabetics Abnormal glycaemia (a) Hypoglycaemic (b) Hyperglycaemic: (i) ketoacidotic, (ii) non-ketoacidotic Other metabolic, consequent upon the diabetic state (a) Uraemic coma, with or without glycaemic upset (b) Lactic acidosis, with or without glycaemic upset (c) Alcoholic coma, with possible abnormalities in ‘ketone bodies’, lactate, or glucose Non-metabolic coma For example, subarachnoid haemorrhage
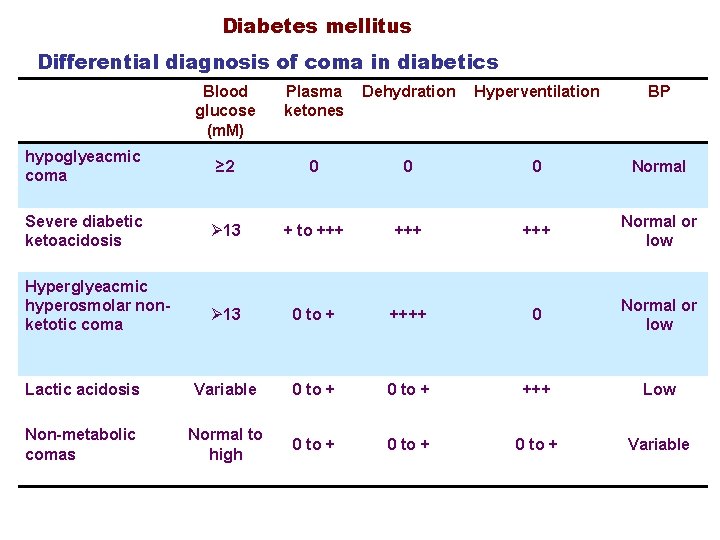
Diabetes mellitus Differential diagnosis of coma in diabetics Blood glucose (m. M) Plasma ketones Dehydration Hyperventilation BP hypoglyeacmic coma ≥ 2 0 0 0 Normal Severe diabetic ketoacidosis Ø 13 + to +++ +++ Normal or low Ø 13 0 to + ++++ 0 Normal or low Lactic acidosis Variable 0 to + +++ Low Non-metabolic comas Normal to high 0 to + Variable Hyperglyeacmic hyperosmolar nonketotic coma
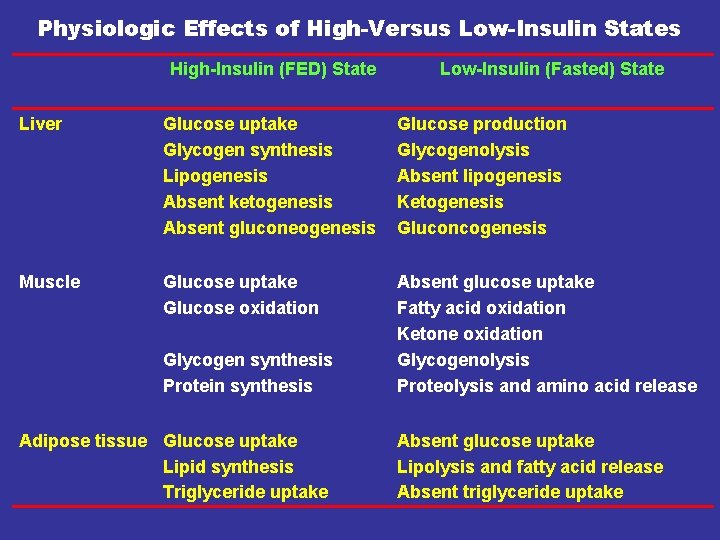
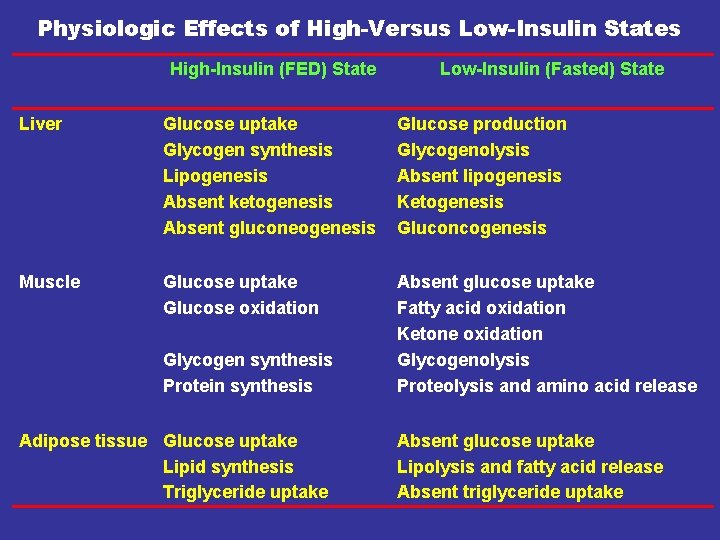
Physiologic Effects of High-Versus Low-Insulin States High-Insulin (FED) State Low-Insulin (Fasted) State Liver Glucose uptake Glycogen synthesis Lipogenesis Absent ketogenesis Absent gluconeogenesis Glucose production Glycogenolysis Absent lipogenesis Ketogenesis Gluconcogenesis Muscle Glucose uptake Glucose oxidation Absent glucose uptake Fatty acid oxidation Ketone oxidation Glycogenolysis Proteolysis and amino acid release Glycogen synthesis Protein synthesis Adipose tissue Glucose uptake Lipid synthesis Triglyceride uptake Absent glucose uptake Lipolysis and fatty acid release Absent triglyceride uptake
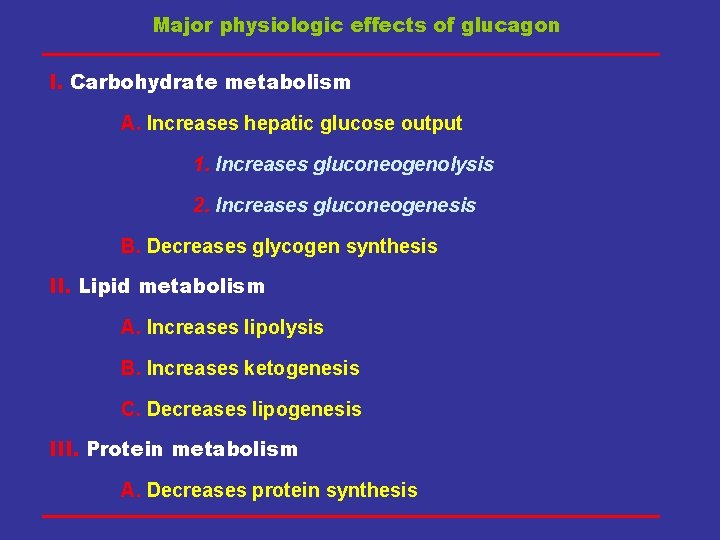
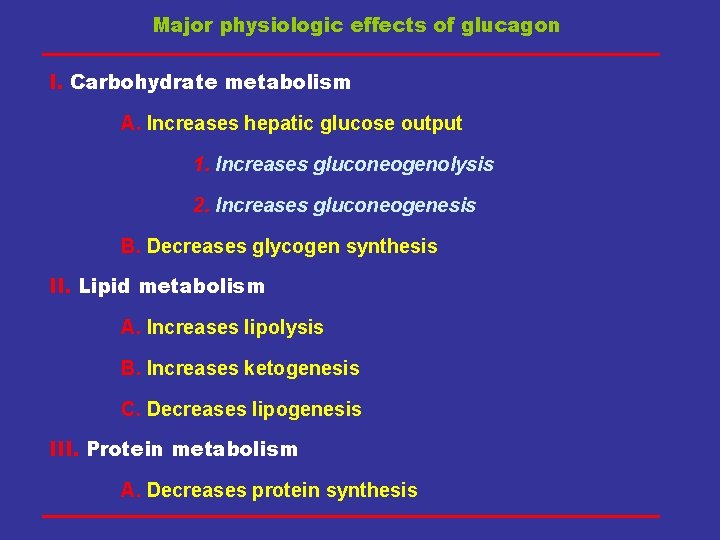
Major physiologic effects of glucagon I. Carbohydrate metabolism A. Increases hepatic glucose output 1. Increases gluconeogenolysis 2. Increases gluconeogenesis B. Decreases glycogen synthesis II. Lipid metabolism A. Increases lipolysis B. Increases ketogenesis C. Decreases lipogenesis III. Protein metabolism A. Decreases protein synthesis
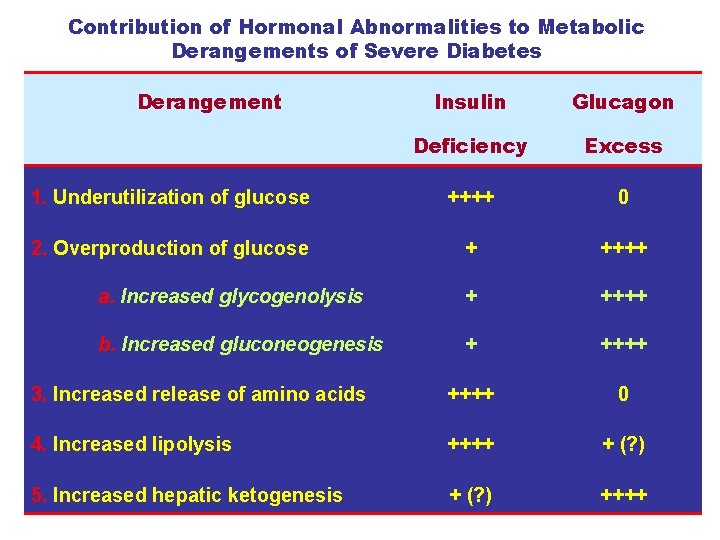
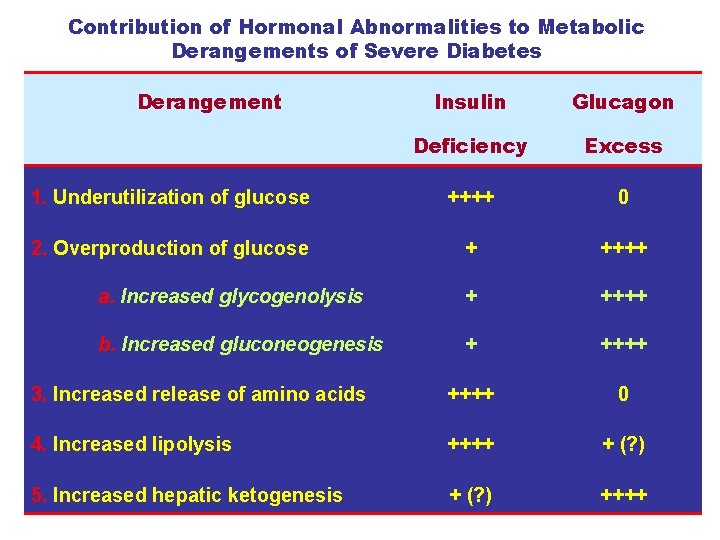
Contribution of Hormonal Abnormalities to Metabolic Derangements of Severe Diabetes Derangement Insulin Glucagon Deficiency Excess 1. Underutilization of glucose ++++ 0 2. Overproduction of glucose + ++++ a. Increased glycogenolysis + ++++ b. Increased gluconeogenesis + ++++ 3. Increased release of amino acids ++++ 0 4. Increased lipolysis ++++ + (? ) 5. Increased hepatic ketogenesis + (? ) ++++
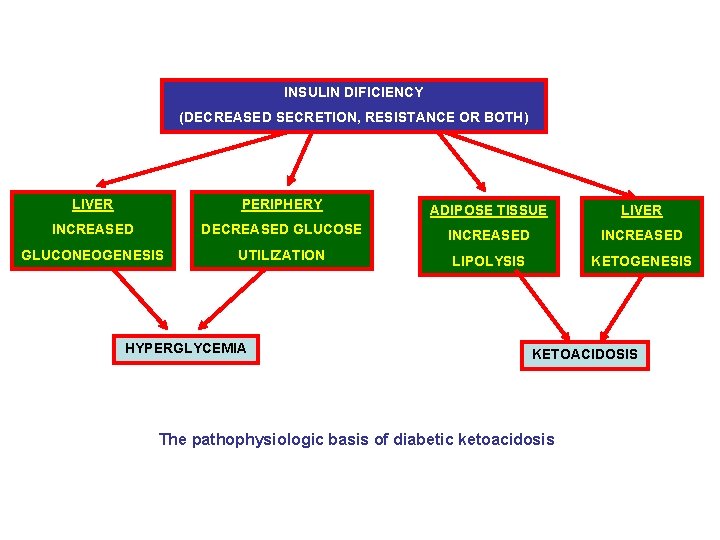
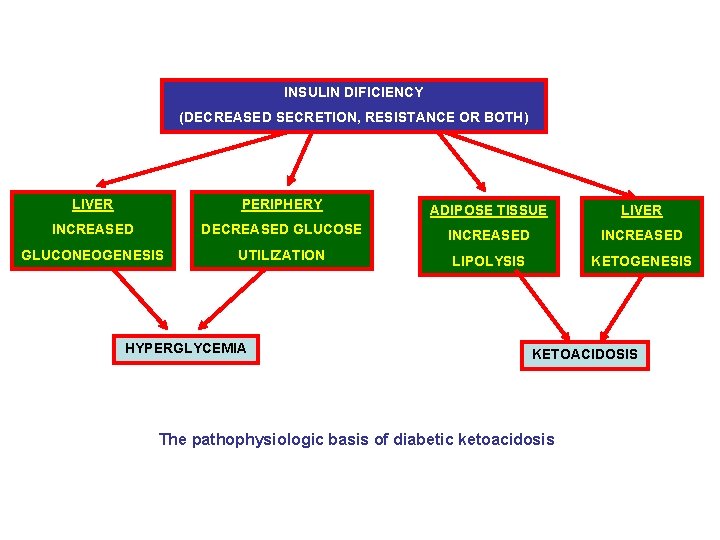
INSULIN DIFICIENCY (DECREASED SECRETION, RESISTANCE OR BOTH) LIVER PERIPHERY ADIPOSE TISSUE LIVER INCREASED DECREASED GLUCOSE INCREASED GLUCONEOGENESIS UTILIZATION LIPOLYSIS KETOGENESIS HYPERGLYCEMIA KETOACIDOSIS The pathophysiologic basis of diabetic ketoacidosis
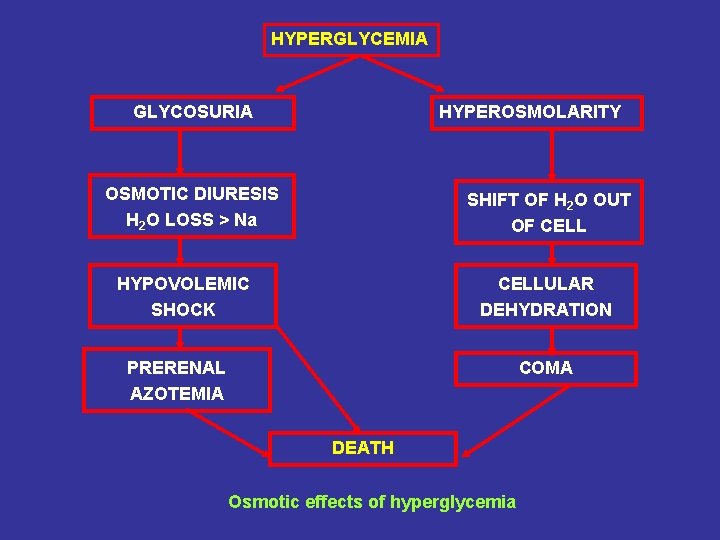
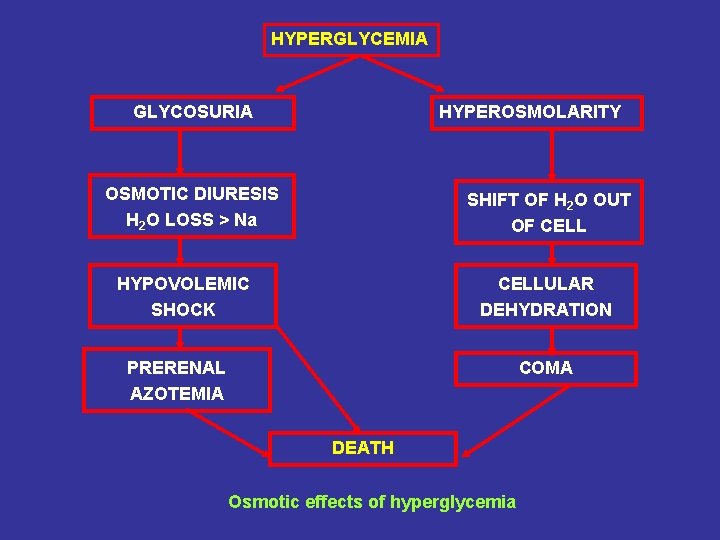
HYPERGLYCEMIA GLYCOSURIA HYPEROSMOLARITY OSMOTIC DIURESIS H 2 O LOSS > Na SHIFT OF H 2 O OUT OF CELL HYPOVOLEMIC SHOCK CELLULAR DEHYDRATION PRERENAL AZOTEMIA COMA DEATH Osmotic effects of hyperglycemia
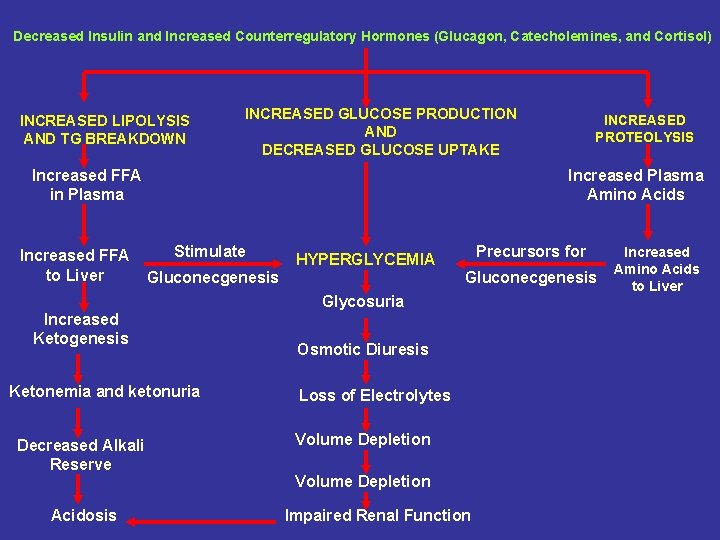
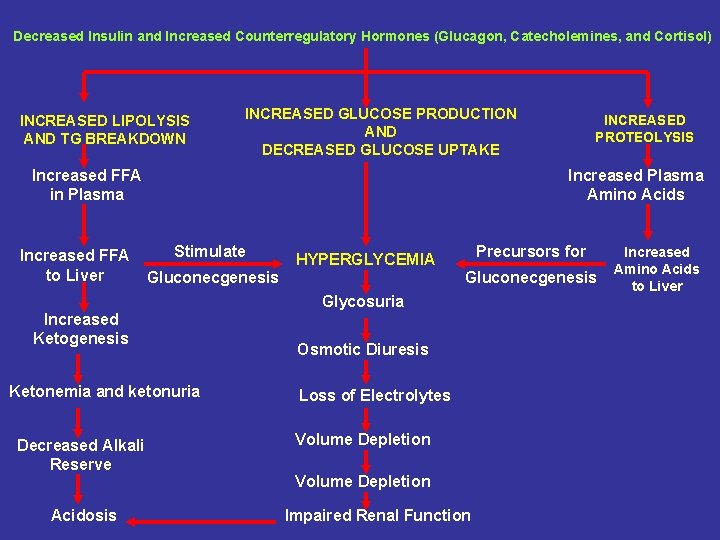
Decreased Insulin and Increased Counterregulatory Hormones (Glucagon, Catecholemines, and Cortisol) INCREASED LIPOLYSIS AND TG BREAKDOWN INCREASED GLUCOSE PRODUCTION AND DECREASED GLUCOSE UPTAKE Increased FFA in Plasma Increased FFA to Liver Increased Plasma Amino Acids Stimulate Precursors for HYPERGLYCEMIA Gluconecgenesis Glycosuria Increased Ketogenesis Ketonemia and ketonuria Decreased Alkali Reserve Acidosis INCREASED PROTEOLYSIS Osmotic Diuresis Loss of Electrolytes Volume Depletion Impaired Renal Function Increased Amino Acids to Liver
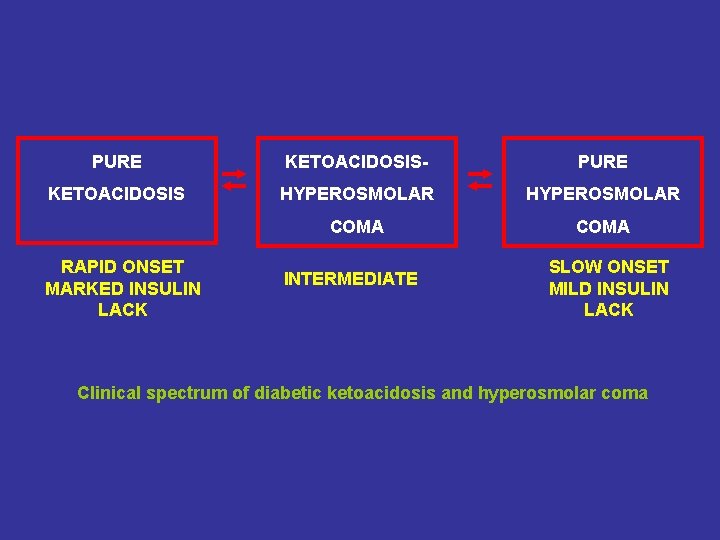
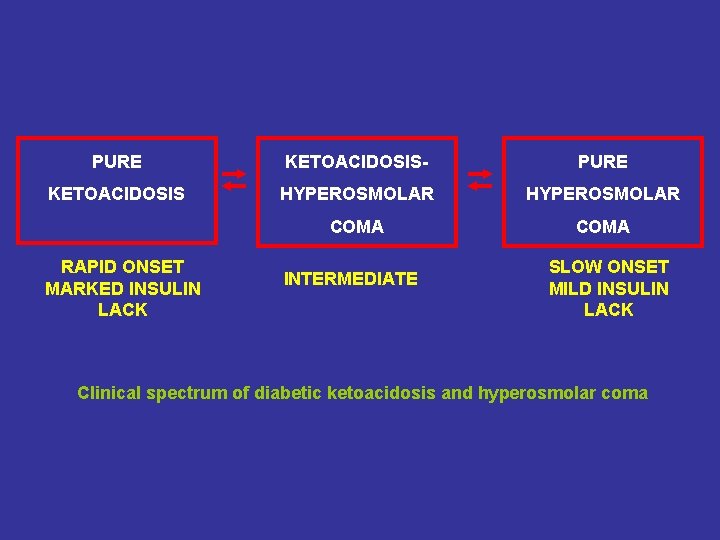
PURE KETOACIDOSIS- PURE KETOACIDOSIS HYPEROSMOLAR COMA RAPID ONSET MARKED INSULIN LACK INTERMEDIATE SLOW ONSET MILD INSULIN LACK Clinical spectrum of diabetic ketoacidosis and hyperosmolar coma
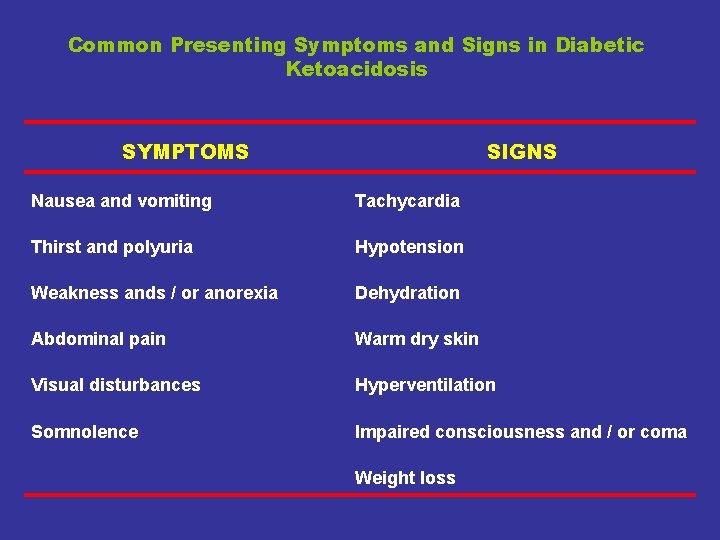
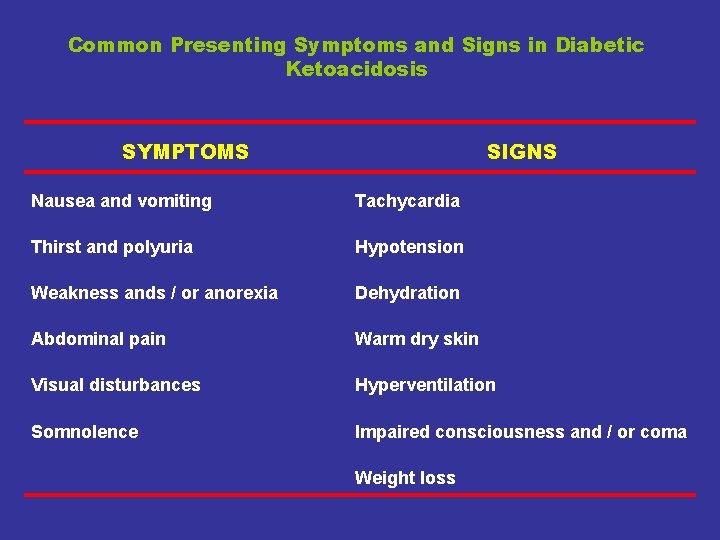
Common Presenting Symptoms and Signs in Diabetic Ketoacidosis SYMPTOMS SIGNS Nausea and vomiting Tachycardia Thirst and polyuria Hypotension Weakness ands / or anorexia Dehydration Abdominal pain Warm dry skin Visual disturbances Hyperventilation Somnolence Impaired consciousness and / or coma Weight loss
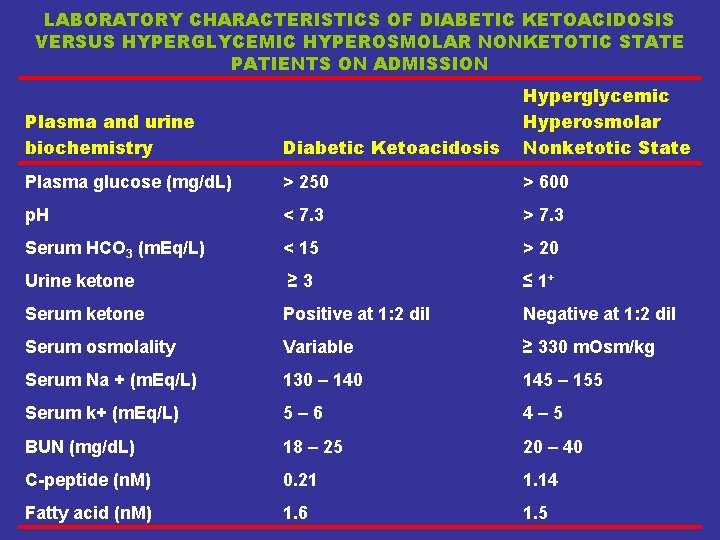
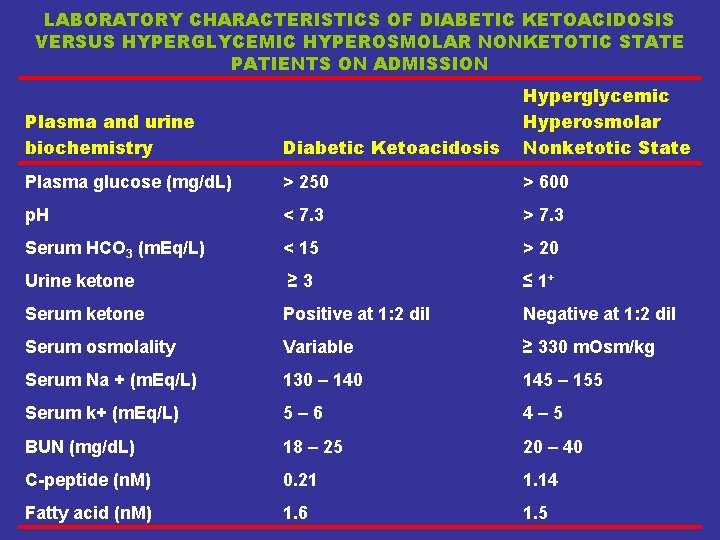
LABORATORY CHARACTERISTICS OF DIABETIC KETOACIDOSIS VERSUS HYPERGLYCEMIC HYPEROSMOLAR NONKETOTIC STATE PATIENTS ON ADMISSION Plasma and urine biochemistry Diabetic Ketoacidosis Hyperglycemic Hyperosmolar Nonketotic State Plasma glucose (mg/d. L) > 250 > 600 p. H < 7. 3 > 7. 3 Serum HCO 3 (m. Eq/L) < 15 > 20 Urine ketone ≥ 3 ≤ 1+ Serum ketone Positive at 1: 2 dil Negative at 1: 2 dil Serum osmolality Variable ≥ 330 m. Osm/kg Serum Na + (m. Eq/L) 130 – 140 145 – 155 Serum k+ (m. Eq/L) 5– 6 4– 5 BUN (mg/d. L) 18 – 25 20 – 40 C-peptide (n. M) 0. 21 1. 14 Fatty acid (n. M) 1. 6 1. 5
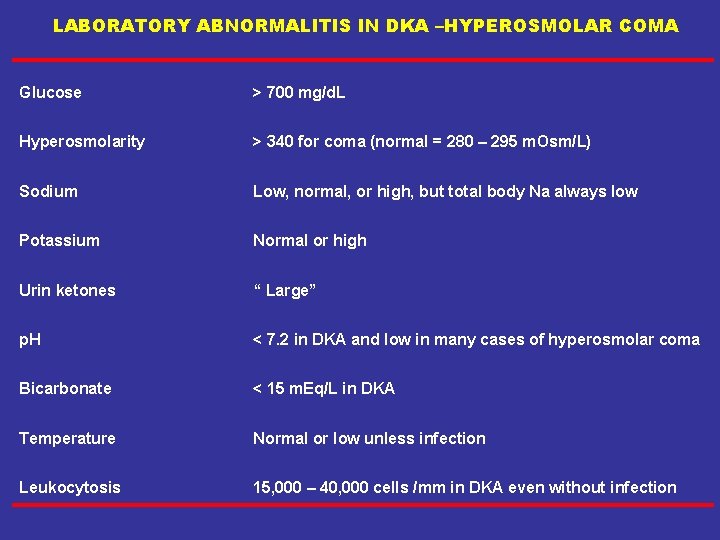
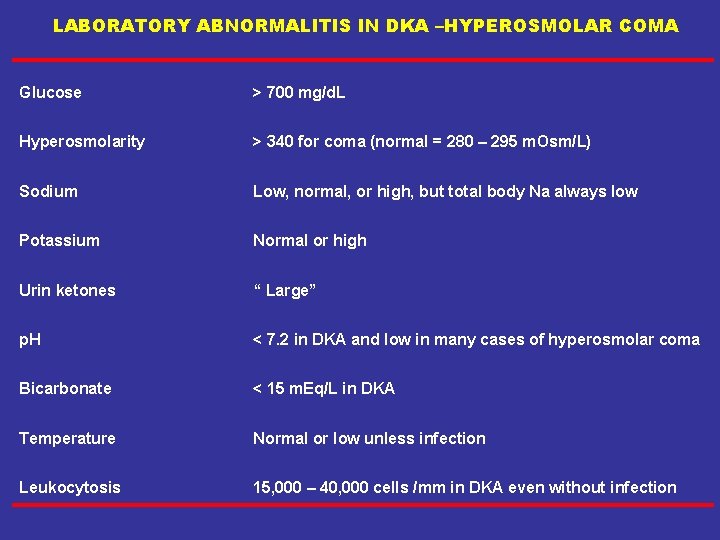
LABORATORY ABNORMALITIS IN DKA –HYPEROSMOLAR COMA Glucose > 700 mg/d. L Hyperosmolarity > 340 for coma (normal = 280 – 295 m. Osm/L) Sodium Low, normal, or high, but total body Na always low Potassium Normal or high Urin ketones “ Large” p. H < 7. 2 in DKA and low in many cases of hyperosmolar coma Bicarbonate < 15 m. Eq/L in DKA Temperature Normal or low unless infection Leukocytosis 15, 000 – 40, 000 cells /mm in DKA even without infection
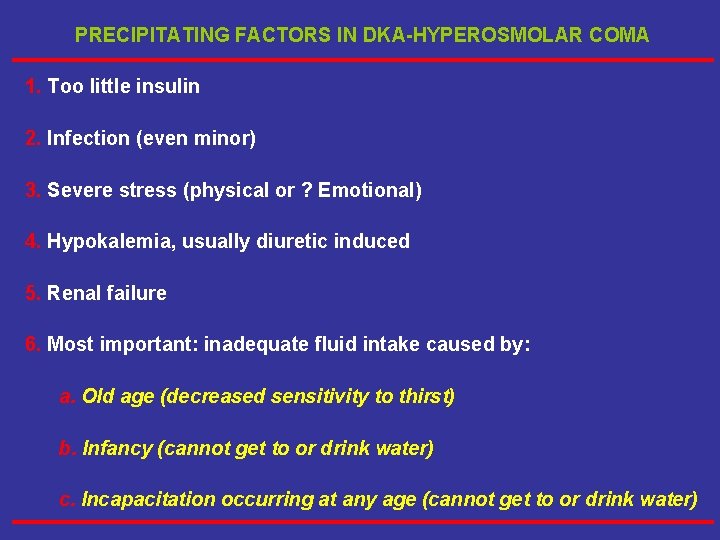
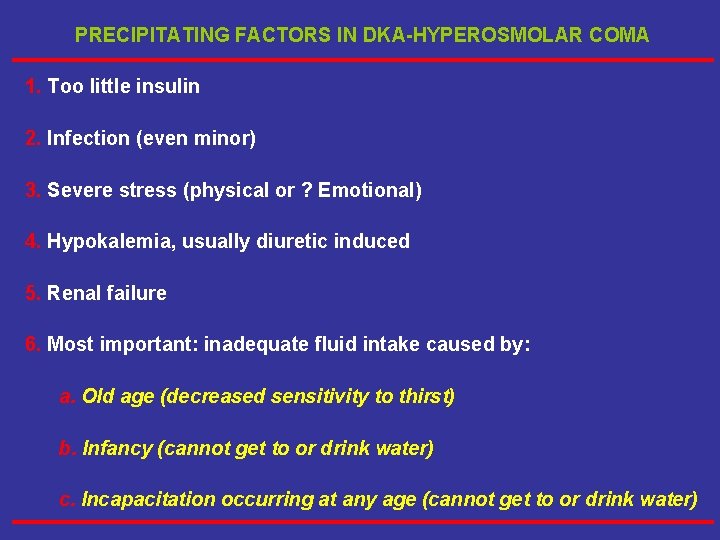
PRECIPITATING FACTORS IN DKA-HYPEROSMOLAR COMA 1. Too little insulin 2. Infection (even minor) 3. Severe stress (physical or ? Emotional) 4. Hypokalemia, usually diuretic induced 5. Renal failure 6. Most important: inadequate fluid intake caused by: a. Old age (decreased sensitivity to thirst) b. Infancy (cannot get to or drink water) c. Incapacitation occurring at any age (cannot get to or drink water)
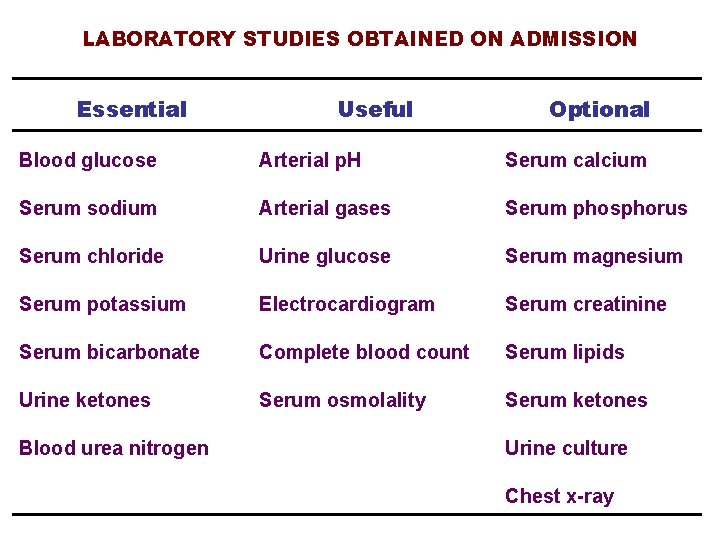
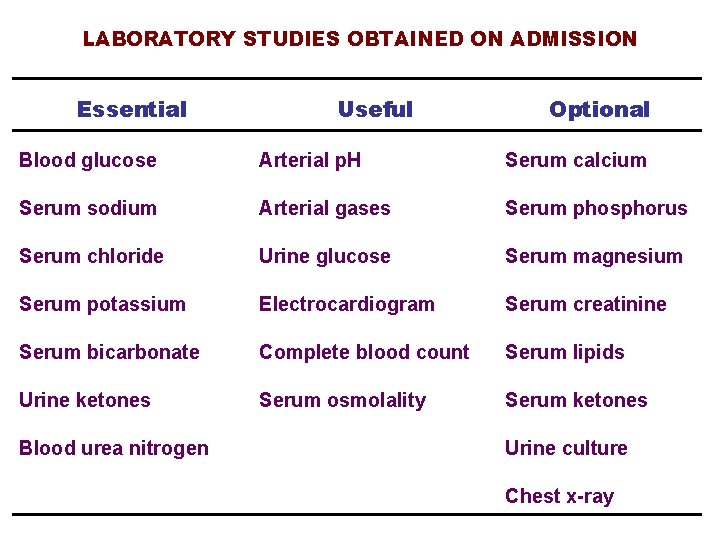
LABORATORY STUDIES OBTAINED ON ADMISSION Essential Useful Optional Blood glucose Arterial p. H Serum calcium Serum sodium Arterial gases Serum phosphorus Serum chloride Urine glucose Serum magnesium Serum potassium Electrocardiogram Serum creatinine Serum bicarbonate Complete blood count Serum lipids Urine ketones Serum osmolality Serum ketones Blood urea nitrogen Urine culture Chest x-ray
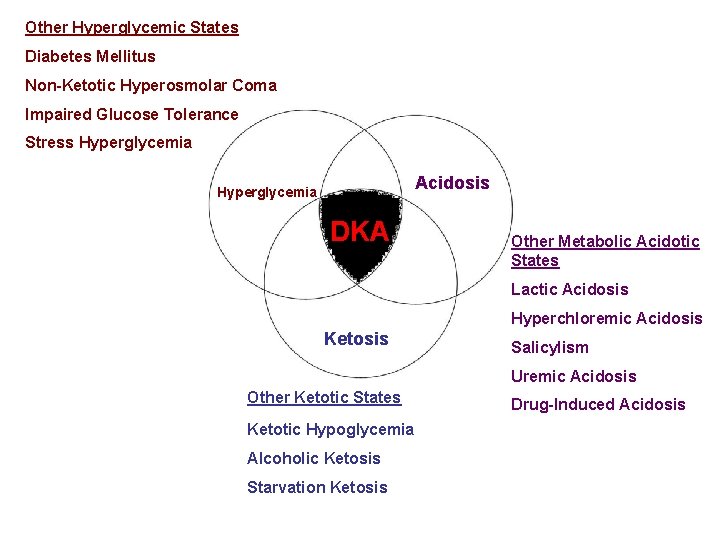
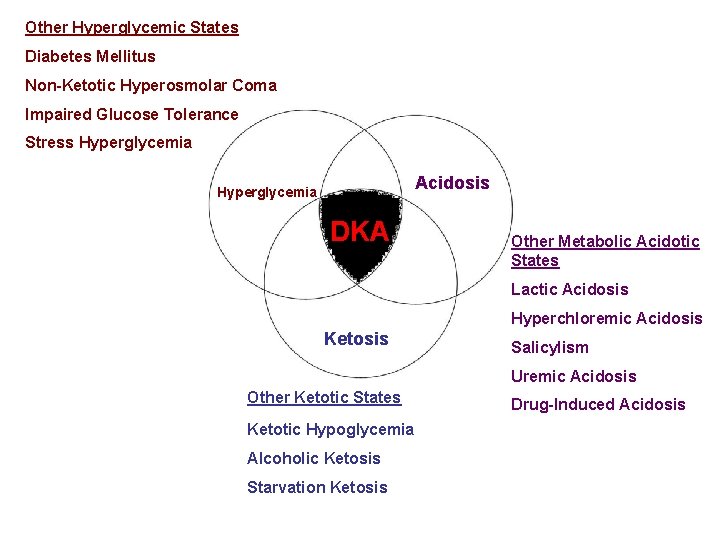
Other Hyperglycemic States Diabetes Mellitus Non-Ketotic Hyperosmolar Coma Impaired Glucose Tolerance Stress Hyperglycemia Acidosis Hyperglycemia DKA Other Metabolic Acidotic States Lactic Acidosis Hyperchloremic Acidosis Ketosis Salicylism Uremic Acidosis Other Ketotic States Ketotic Hypoglycemia Alcoholic Ketosis Starvation Ketosis Drug-Induced Acidosis
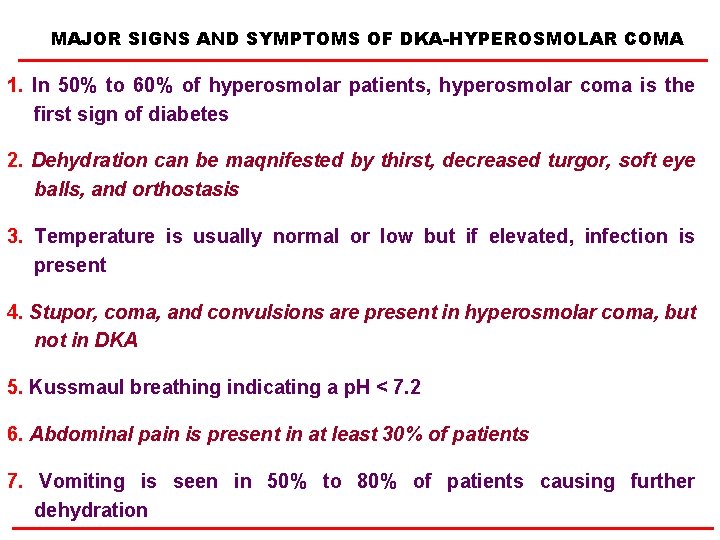
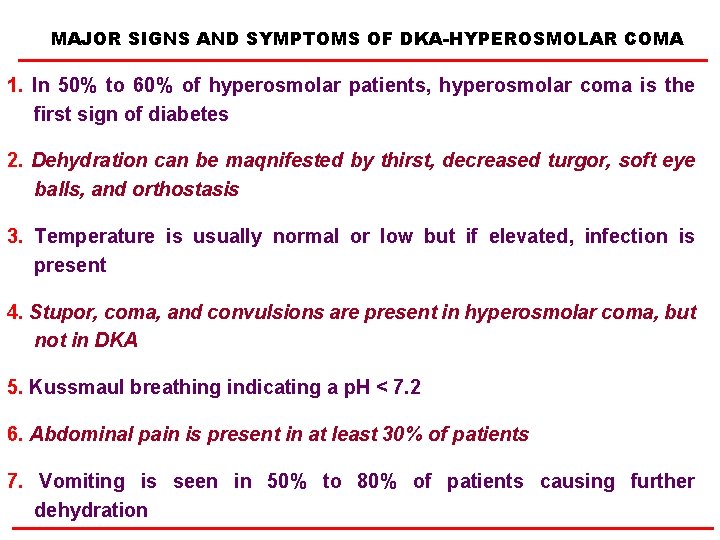
MAJOR SIGNS AND SYMPTOMS OF DKA-HYPEROSMOLAR COMA 1. In 50% to 60% of hyperosmolar patients, hyperosmolar coma is the first sign of diabetes 2. Dehydration can be maqnifested by thirst, decreased turgor, soft eye balls, and orthostasis 3. Temperature is usually normal or low but if elevated, infection is present 4. Stupor, coma, and convulsions are present in hyperosmolar coma, but not in DKA 5. Kussmaul breathing indicating a p. H < 7. 2 6. Abdominal pain is present in at least 30% of patients 7. Vomiting is seen in 50% to 80% of patients causing further dehydration
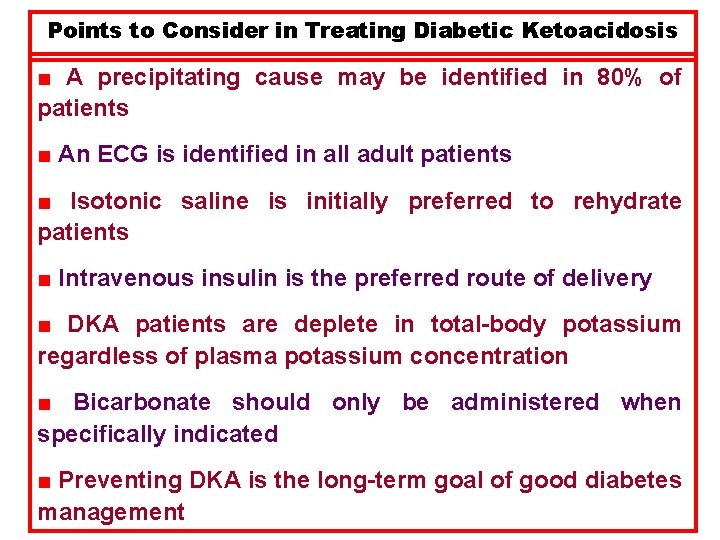
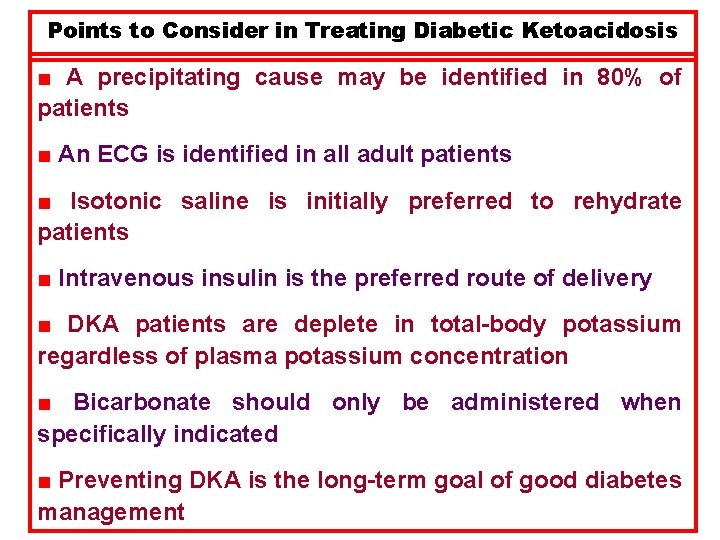
Points to Consider in Treating Diabetic Ketoacidosis ■ A precipitating cause may be identified in 80% of patients ■ An ECG is identified in all adult patients ■ Isotonic saline is initially preferred to rehydrate patients ■ Intravenous insulin is the preferred route of delivery ■ DKA patients are deplete in total-body potassium regardless of plasma potassium concentration ■ Bicarbonate should only be administered when specifically indicated ■ Preventing DKA is the long-term goal of good diabetes management
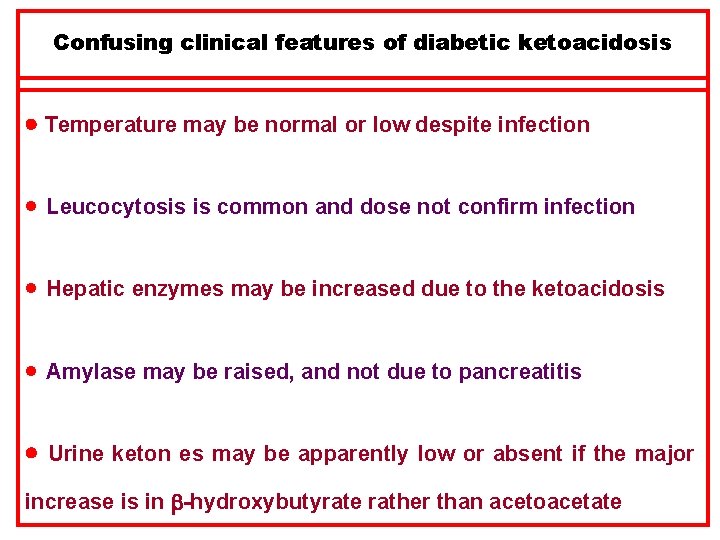
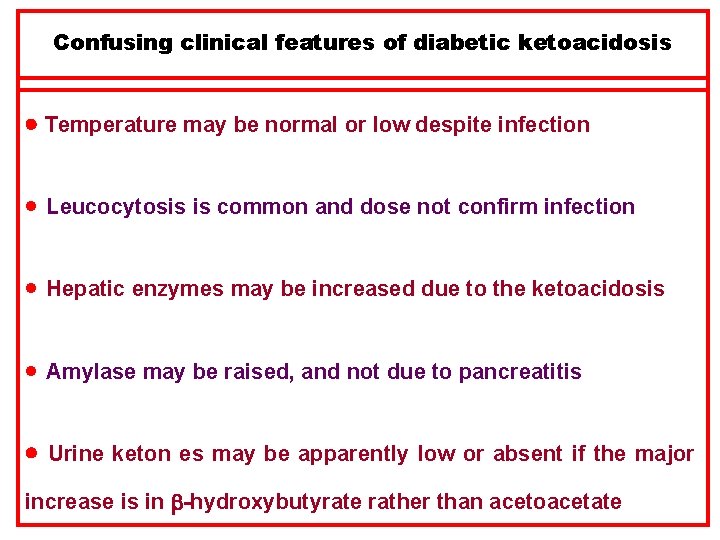
Confusing clinical features of diabetic ketoacidosis Temperature may be normal or low despite infection · Leucocytosis is common and dose not confirm infection · Hepatic enzymes may be increased due to the ketoacidosis · Amylase may be raised, and not due to pancreatitis Urine keton es may be apparently low or absent if the major increase is in -hydroxybutyrate rather than acetoacetate
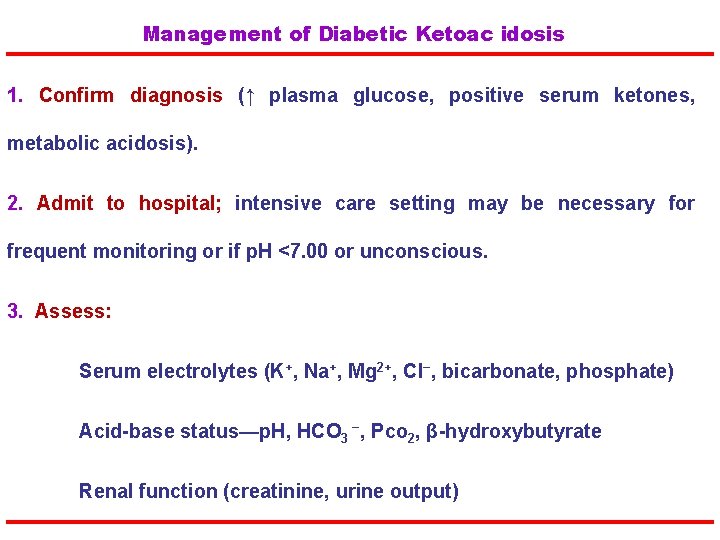
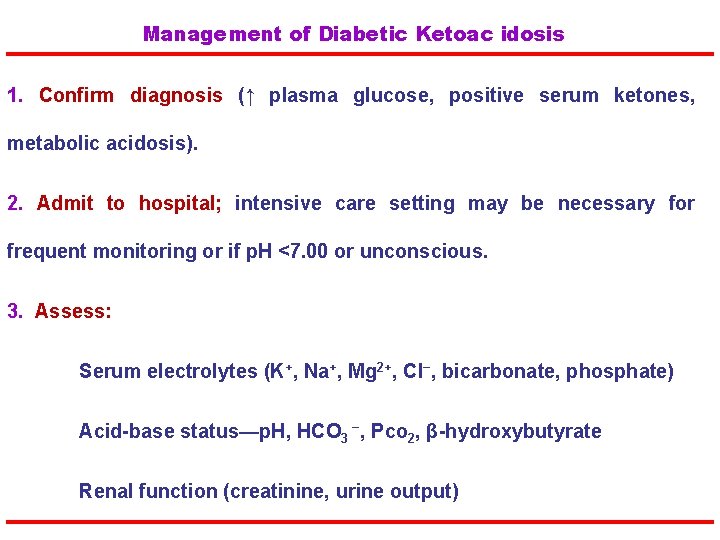
Management of Diabetic Ketoac idosis 1. Confirm diagnosis (↑ plasma glucose, positive serum ketones, metabolic acidosis). 2. Admit to hospital; intensive care setting may be necessary for frequent monitoring or if p. H <7. 00 or unconscious. 3. Assess: Serum electrolytes (K+, Na+, Mg 2+, Cl−, bicarbonate, phosphate) Acid-base status—p. H, HCO 3 −, Pco 2, β-hydroxybutyrate Renal function (creatinine, urine output)
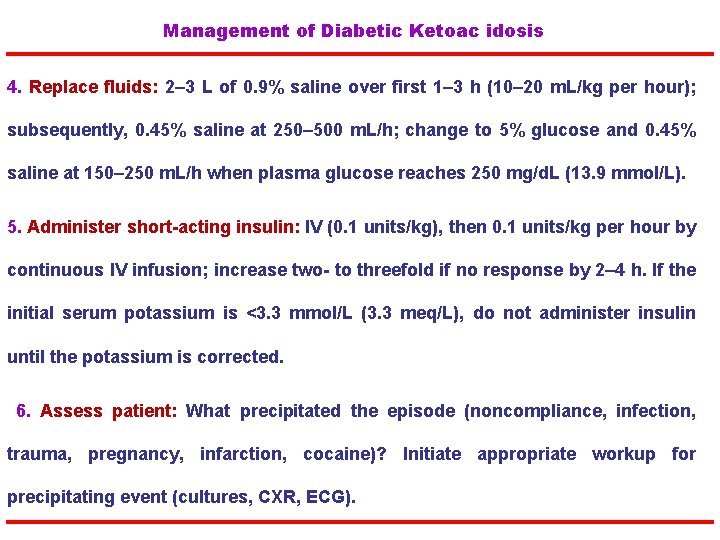
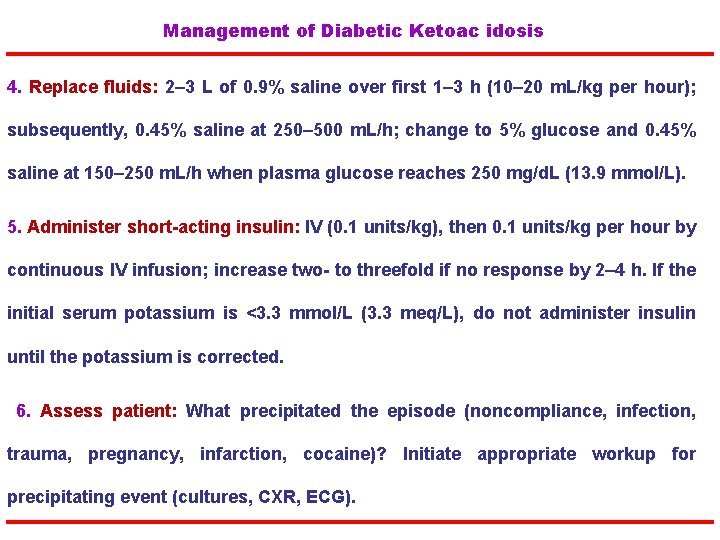
Management of Diabetic Ketoac idosis 4. Replace fluids: 2– 3 L of 0. 9% saline over first 1– 3 h (10– 20 m. L/kg per hour); subsequently, 0. 45% saline at 250– 500 m. L/h; change to 5% glucose and 0. 45% saline at 150– 250 m. L/h when plasma glucose reaches 250 mg/d. L (13. 9 mmol/L). 5. Administer short-acting insulin: IV (0. 1 units/kg), then 0. 1 units/kg per hour by continuous IV infusion; increase two- to threefold if no response by 2– 4 h. If the initial serum potassium is <3. 3 mmol/L (3. 3 meq/L), do not administer insulin until the potassium is corrected. 6. Assess patient: What precipitated the episode (noncompliance, infection, trauma, pregnancy, infarction, cocaine)? Initiate appropriate workup for precipitating event (cultures, CXR, ECG).
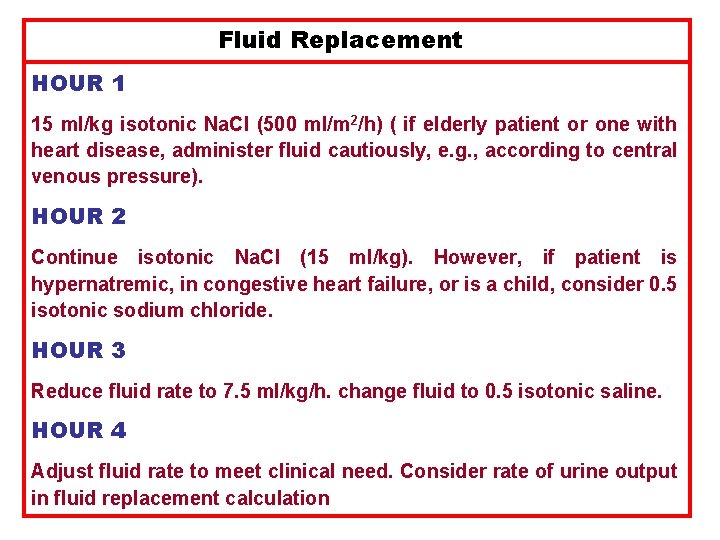
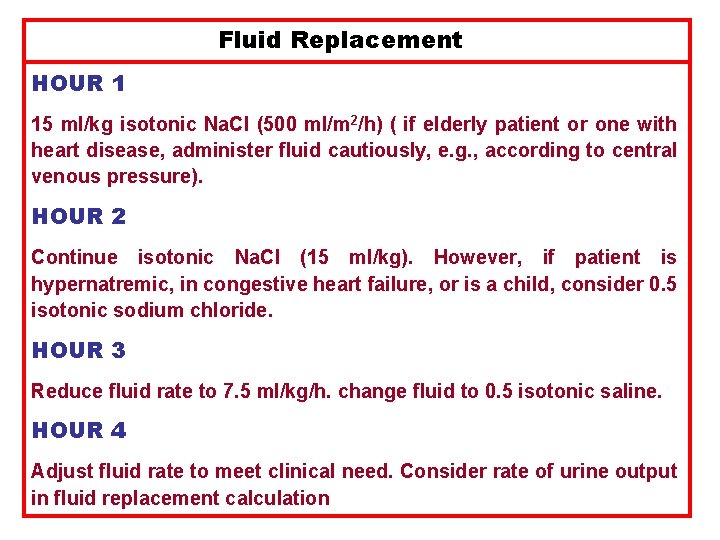
Fluid Replacement HOUR 1 15 ml/kg isotonic Na. Cl (500 ml/m 2/h) ( if elderly patient or one with heart disease, administer fluid cautiously, e. g. , according to central venous pressure). HOUR 2 Continue isotonic Na. Cl (15 ml/kg). However, if patient is hypernatremic, in congestive heart failure, or is a child, consider 0. 5 isotonic sodium chloride. HOUR 3 Reduce fluid rate to 7. 5 ml/kg/h. change fluid to 0. 5 isotonic saline. HOUR 4 Adjust fluid rate to meet clinical need. Consider rate of urine output in fluid replacement calculation
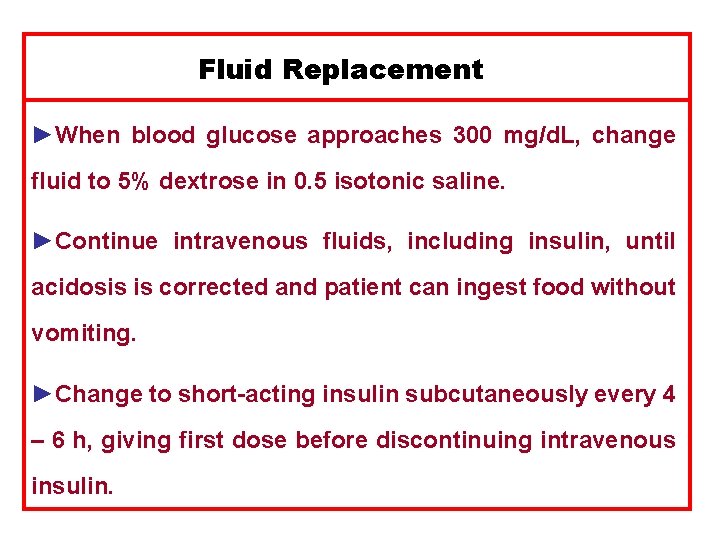
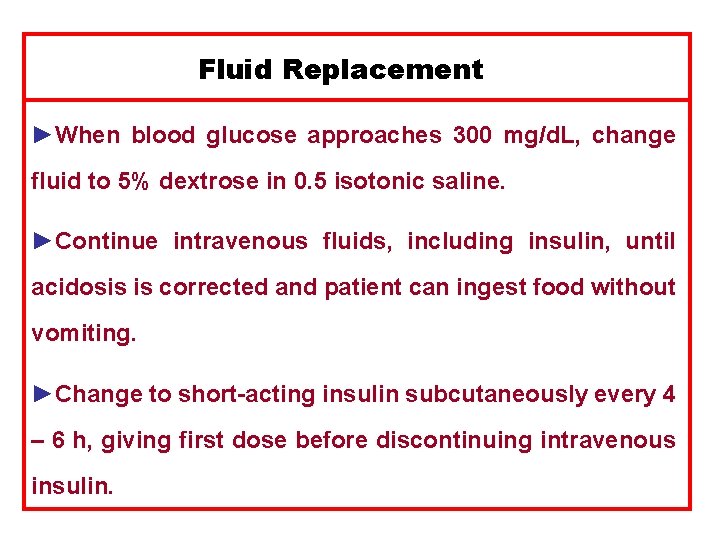
Fluid Replacement ►When blood glucose approaches 300 mg/d. L, change fluid to 5% dextrose in 0. 5 isotonic saline. ►Continue intravenous fluids, including insulin, until acidosis is corrected and patient can ingest food without vomiting. ►Change to short-acting insulin subcutaneously every 4 – 6 h, giving first dose before discontinuing intravenous insulin.
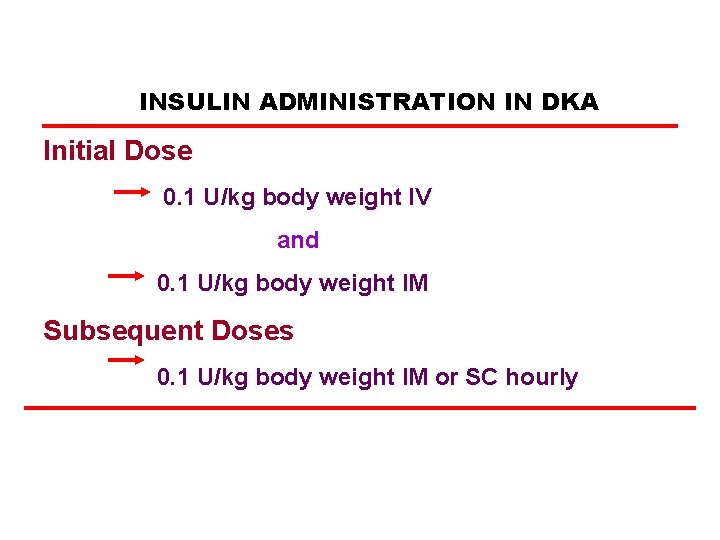
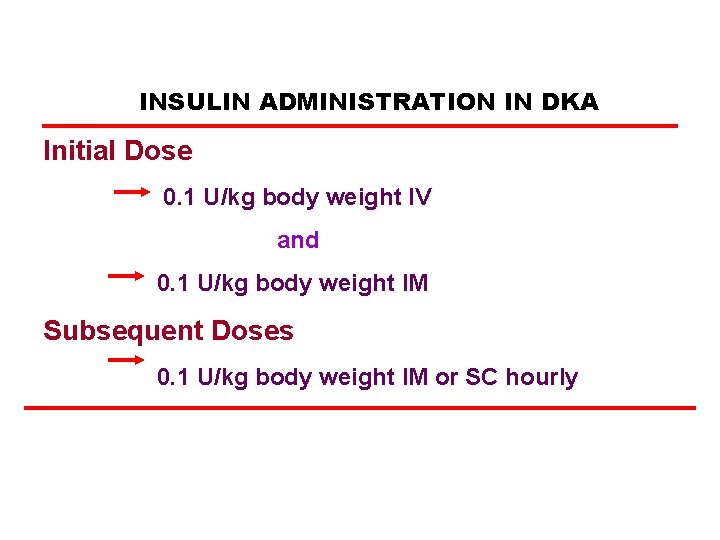
INSULIN ADMINISTRATION IN DKA Initial Dose 0. 1 U/kg body weight IV and 0. 1 U/kg body weight IM Subsequent Doses 0. 1 U/kg body weight IM or SC hourly
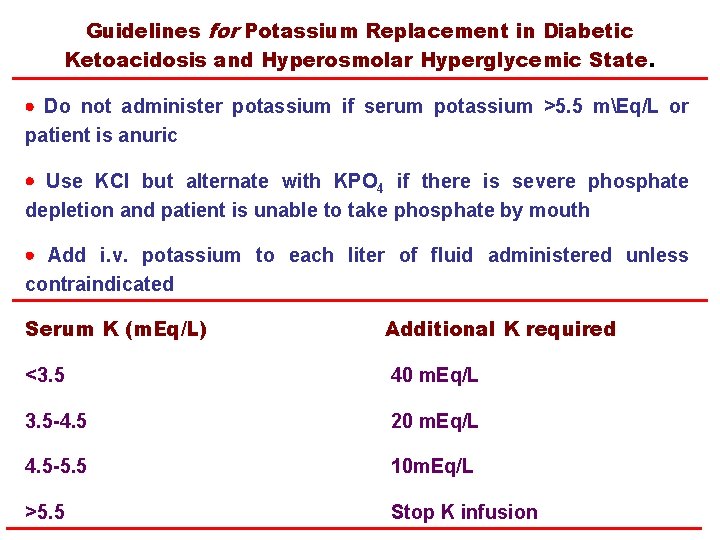
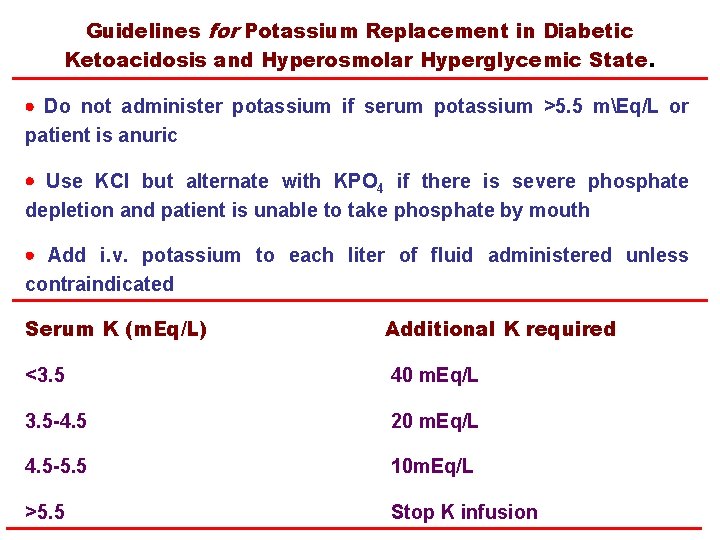
Guidelines for Potassium Replacement in Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State. Do not administer potassium if serum potassium >5. 5 mEq/L or patient is anuric Use KCI but alternate with KPO 4 if there is severe phosphate depletion and patient is unable to take phosphate by mouth Add i. v. potassium to each liter of fluid administered unless contraindicated Serum K (m. Eq/L) Additional K required <3. 5 40 m. Eq/L 3. 5 -4. 5 20 m. Eq/L 4. 5 -5. 5 10 m. Eq/L >5. 5 Stop K infusion
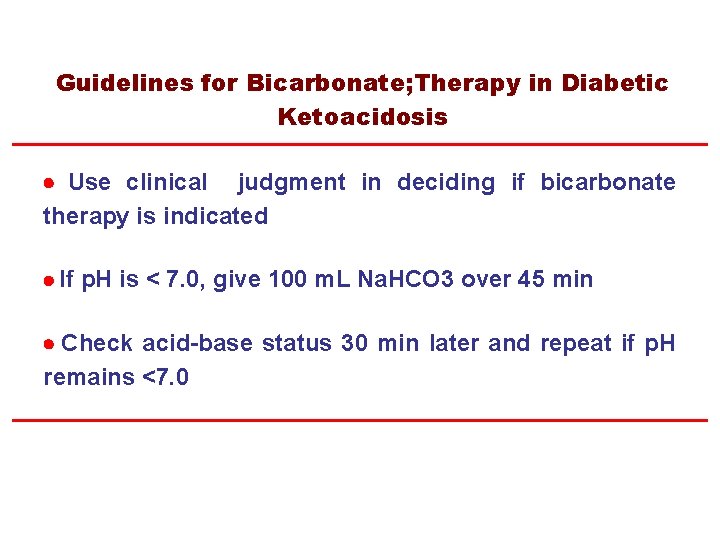
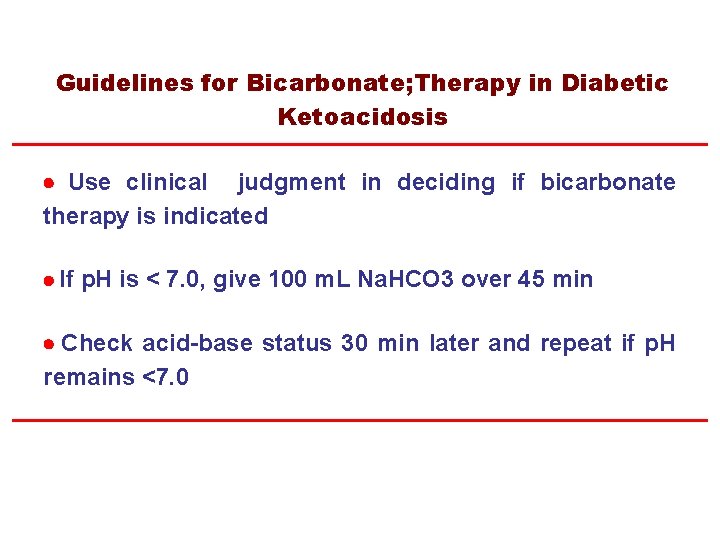
Guidelines for Bicarbonate; Therapy in Diabetic Ketoacidosis Use clinical judgment in deciding if bicarbonate therapy is indicated If p. H is < 7. 0, give 100 m. L Na. HCO 3 over 45 min Check acid-base status 30 min later and repeat if p. H remains <7. 0
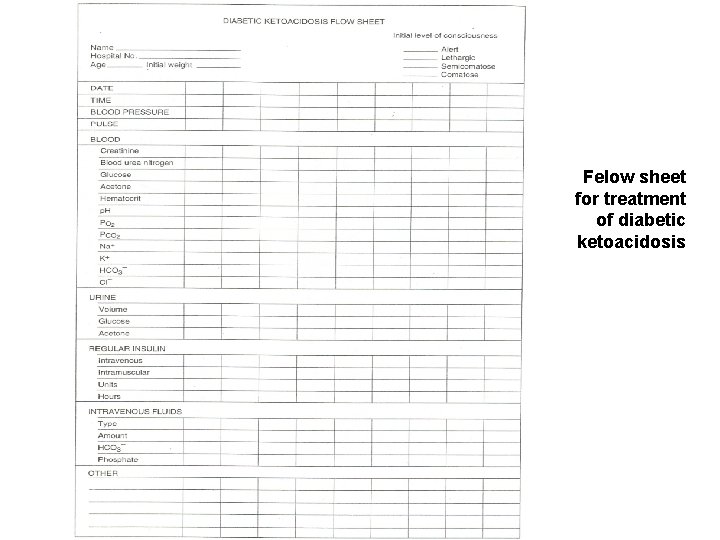
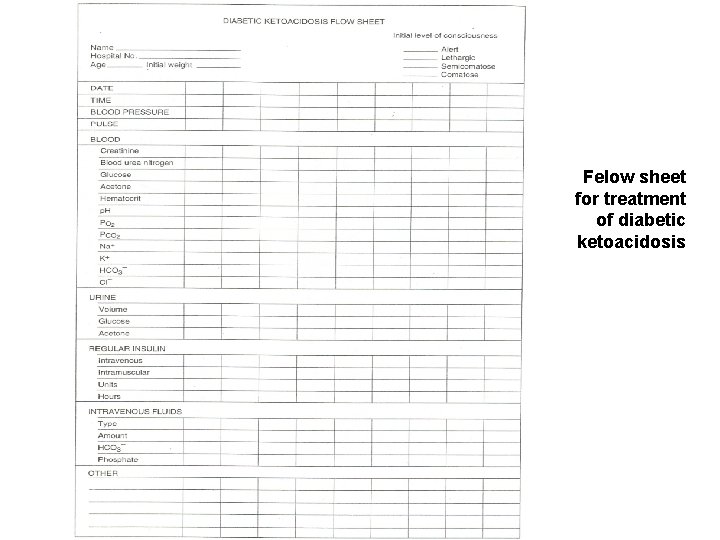
Felow sheet for treatment of diabetic ketoacidosis

Prevention of DKA and HHC
Prevention of DKA and HHC are preventable disorders. These conditions may be the first presentation of diabetes The most common precipitating causes of DKA include: Infection, Intercurrent illness Psychological stress Noncompliance with therapy.
Prevention of DKA and HHC Outpatient management is more cost- effective and can minimize missed days of school and work for patients with diabetes Patient education and 24 - hour access to advice and care, remain the cornerstone of preventative therapy. With improved outpatient treatment programs and better adherence to self-care, nearly 50% to 75% of DKA admission may be preventable.
Prevention of DKA and HHC The frequency of hospitalizations for DKA has been reduced following: Diabetes education programs Improved follow-up care Access to medical advice. Many patients with recurrent DKA are unaware of sick- day management or the consequences of skipping or discontinuing insulin therapy.
Prevention of DKA and HHC An important feature of patient education is how to deal with illness. This includes: 1) Initiating early contact with health care providers 2) Emphasizing the importance of insulin therapy during illness and that insulin should never be discontinued 3) Initiating early management of fevers and infections 4) Ensuring adequate fluid intake.
Prevention of DKA and HHC Patients should be taught how to manage their diabetes during periods of stress or intercurrent infection (sick –day rules) Should understand the importance of frequent monitoring of: Blood glucose Urine ketones Temperature
Prevention of DKA and HHC Diabetes education and sick-day management should be reviewed periodically in patients with type 1 diabetes and should include: Specific information on when to contact the health care provider The use of supplemental short-or rapid-acting insulin during illness Most imperative, the importance of never discontinuing insulin.
Prevention of DKA and HHC The elderly patient living in a nursing home, who is unable to keep up with fluid losses or is unaware of fluid losses during intercurrent illness, is particularly at risk for the development of HHC. Education of caregivers who should learn to recognize signs and symptoms of increasing hyperglycemia will reduce the incidence of severe HHC.

Thank you