HYPERCALCEMIA APPROACH TO THE DIAGNOSIS Palak Choksi MD











- Slides: 52

HYPERCALCEMIA: APPROACH TO THE DIAGNOSIS Palak Choksi, MD Assistant Professor of Medicine Metabolism, Endocrinology and Diabetes

Disclosures NONE
Intended Learning Outcomes –Review calcium metabolism –Describe symptoms of hypercalcemia –Review the etiology of hypercalcemia –Discuss the treatments for hypercalcemia –Conclusions
Intended Learning Outcomes –Review calcium metabolism –Describe symptoms of hypercalcemia –Review the etiology of hypercalcemia –Discuss the treatments for hypercalcemia –Conclusions
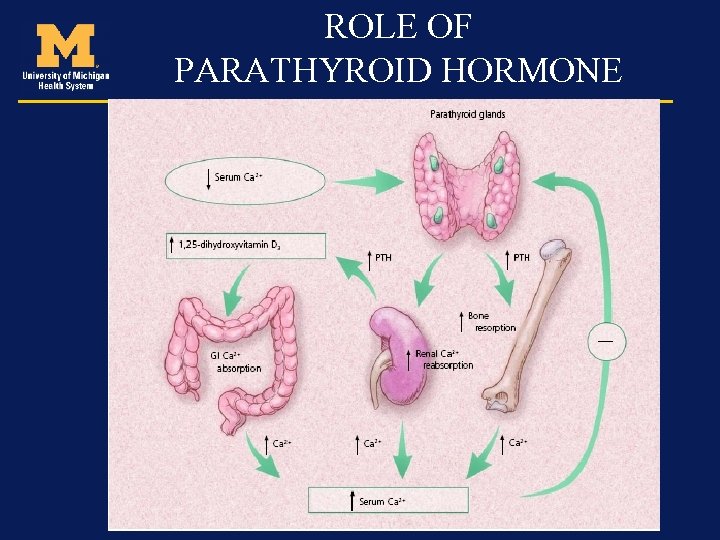
Calcium metabolism • Absorption from GI tract is by passive diffusion and active transport • Most of the calcium is reabsorbed by the kidney – net loss is about 2% • Calcium is controlled by both PTH and calcitonin
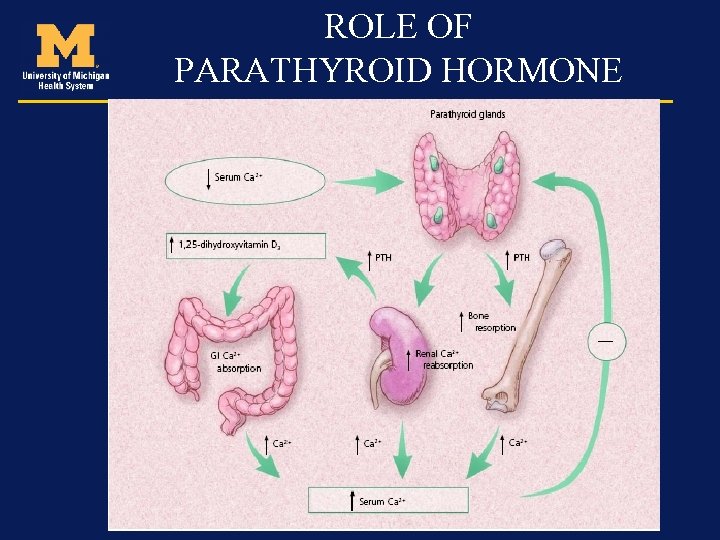
ROLE OF PARATHYROID HORMONE
Calcium • Total calcium - Free (ionized) calcium (50%) - Protein bound calcium (40%) - Calcium complexed with organic and inorganic molecules (10%)
Role of albumin High albumin states (volume depletion or multiple myeloma) may lead to pseudohypercalcemia. Low albumin states like malnutrition, total serum calcium may appear low while ionized calcium is again not very affected. Ca 2+= serum Ca 2+ + 0. 8 x [normal alb-patient alb]
Intended Learning Outcomes –Review calcium metabolism –Describe symptoms of hypercalcemia –Review the etiology of hypercalcemia –Discuss the treatments for hypercalcemia –Conclusions
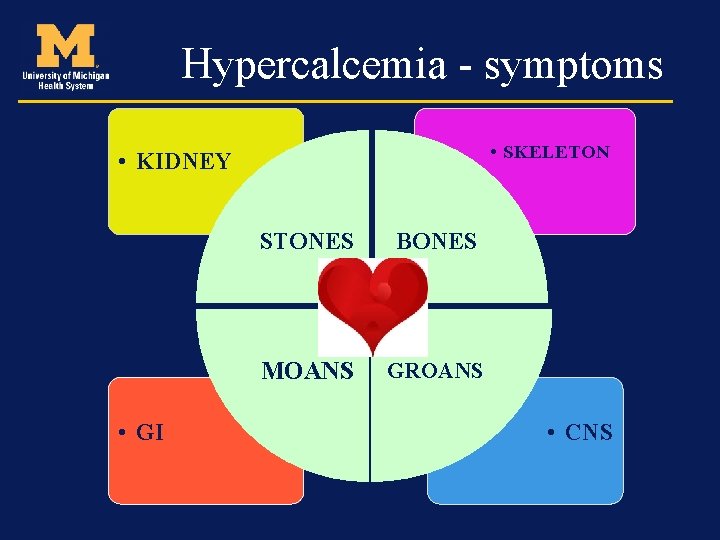
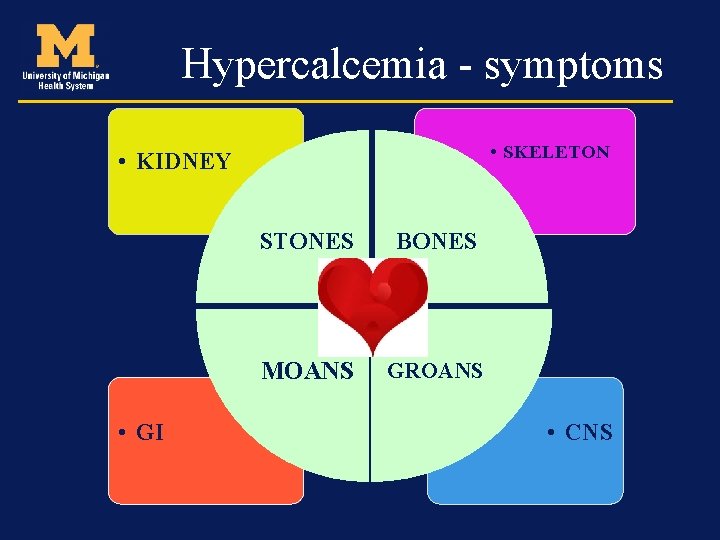
Hypercalcemia - symptoms • SKELETON • KIDNEY • GI STONES BONES MOANS GROANS • CNS
Renal (stones) • Polyuria • Renal insufficiency (rarely seen in mild disease, although in severe cases may cause a reversible drop in GFR) • Nephrolithiasis • Nephrogenic DI
Skeleton (Bones) • Bone pains • Arthritis • Osteoporosis • Osteitis fibrosa cystica
Neuro-psychiatric (Groans) • Depression • Anxiety • Cognitive dysfunction • Lethargy, confusion, stupor, and coma may occur in patients with severe hypercalcemia • More likely to occur in the elderly and in those with rapidly rising calcium concentrations

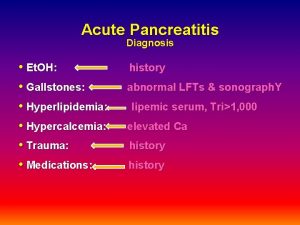
Gastro-intestinal (Moans) • Constipation • Anorexia • Nausea • Pancreatitis • Peptic Ulcers

Cardiovascular • Increases myocardial contractility and irritability • Shortened QT interval • Prolonged PR • Wide QRS complexes • Calcium deposition in coronary arteries and myocardial fibers • Hypertension
Intended Learning Outcomes –Review calcium metabolism –Describe symptoms of hypercalcemia –Review the etiology of hypercalcemia –Discuss the treatments for hypercalcemia –Conclusions
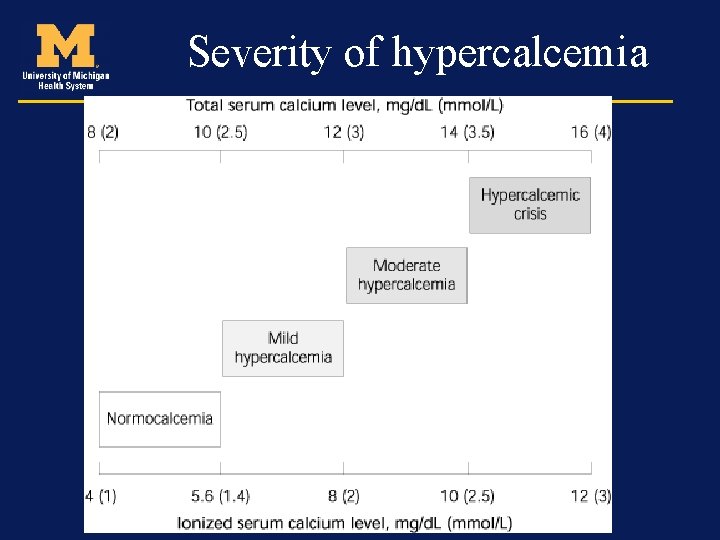
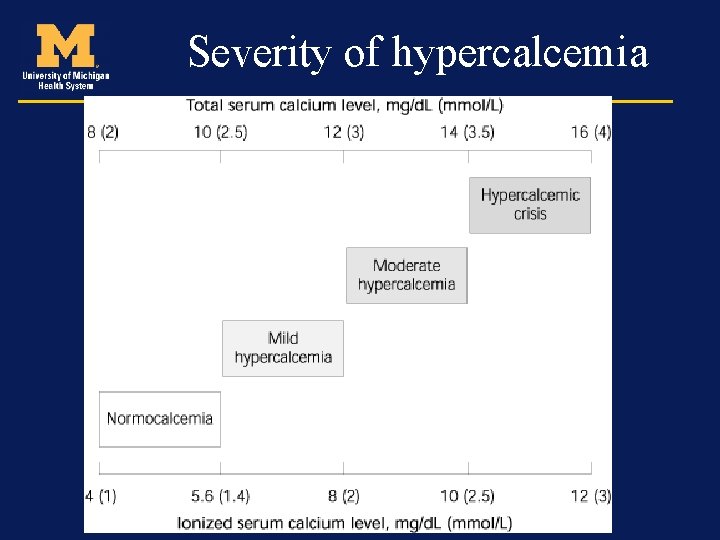
Severity of hypercalcemia
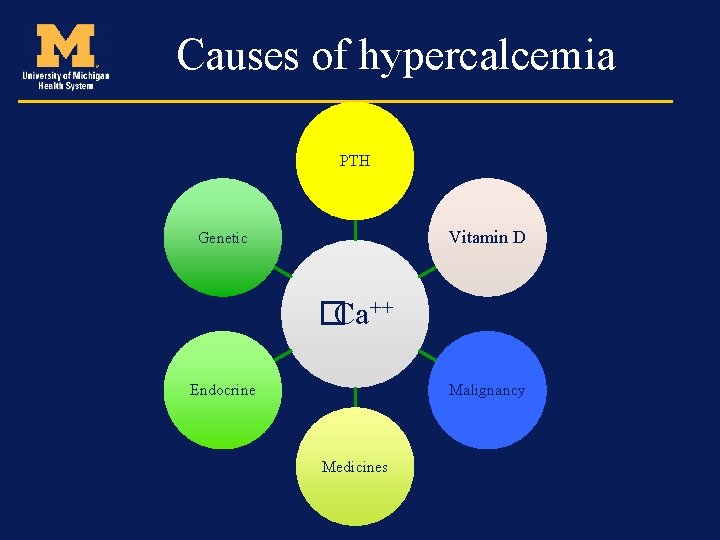
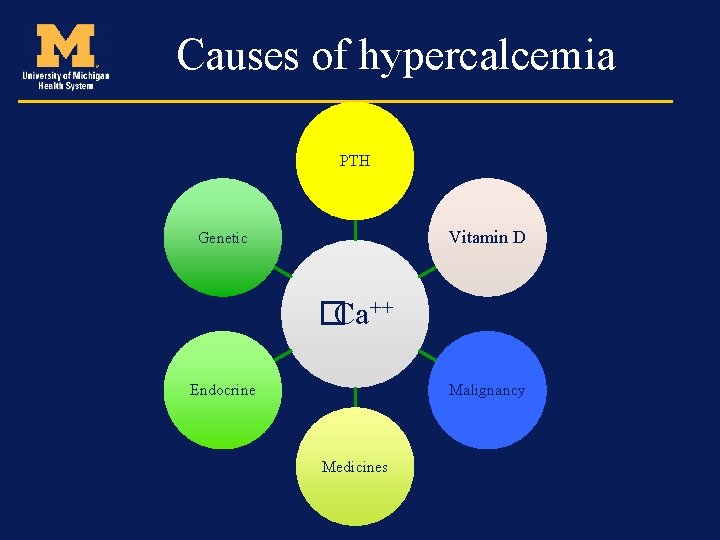
Causes of hypercalcemia PTH Vitamin D Genetic �Ca++ Endocrine Malignancy Medicines
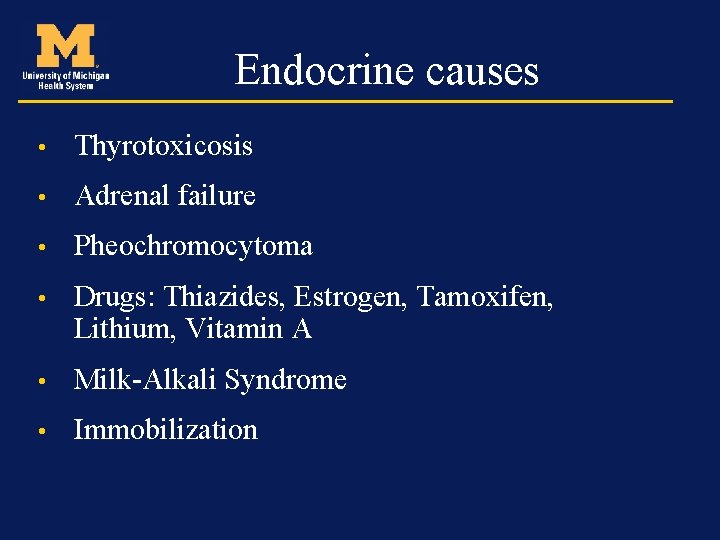
Endocrine causes • Thyrotoxicosis • Adrenal failure • Pheochromocytoma • Drugs: Thiazides, Estrogen, Tamoxifen, Lithium, Vitamin A • Milk-Alkali Syndrome • Immobilization
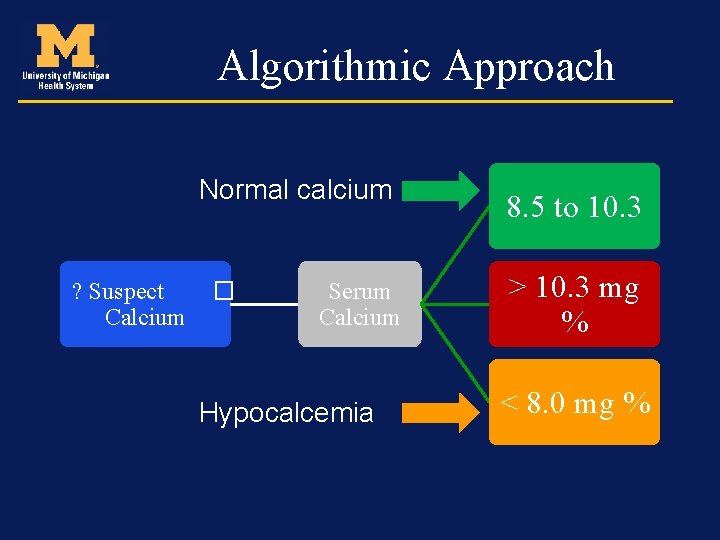
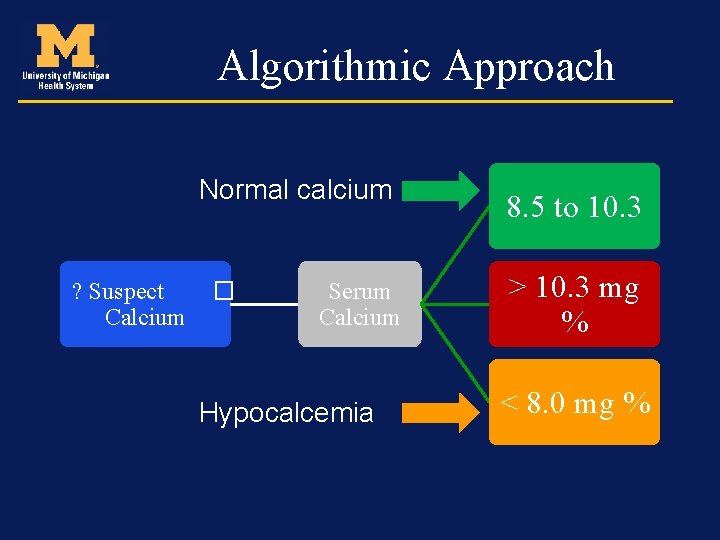
Algorithmic Approach Normal calcium ? Suspect Calcium � Serum Calcium Hypocalcemia 8. 5 to 10. 3 > 10. 3 mg % < 8. 0 mg %
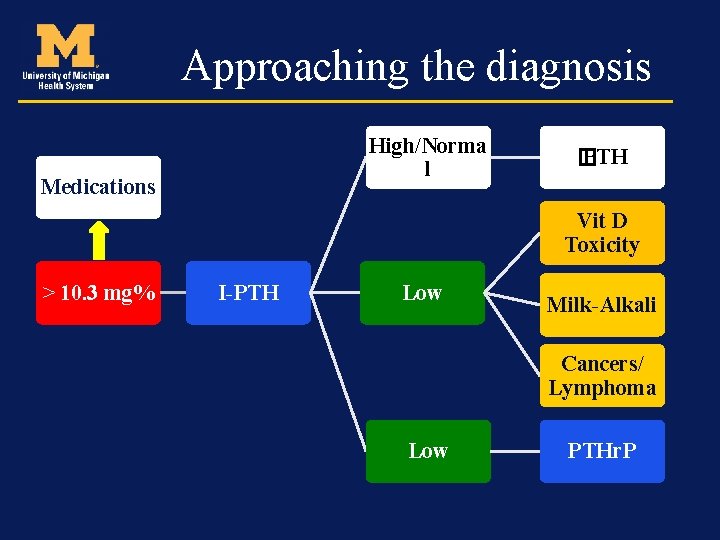
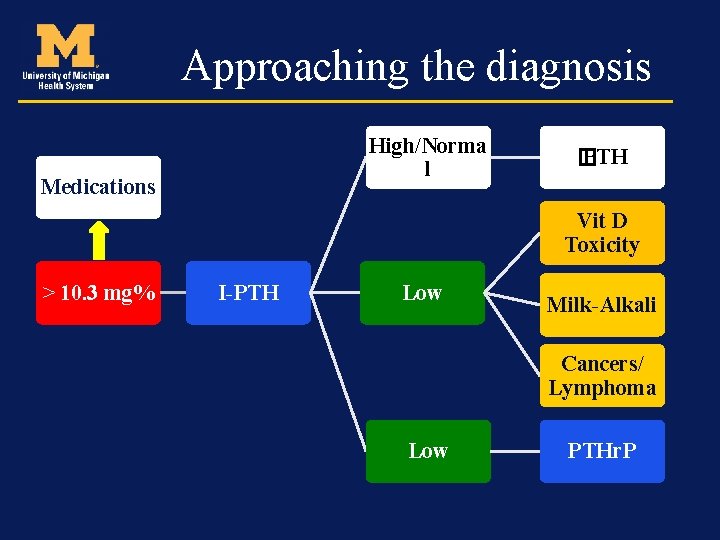
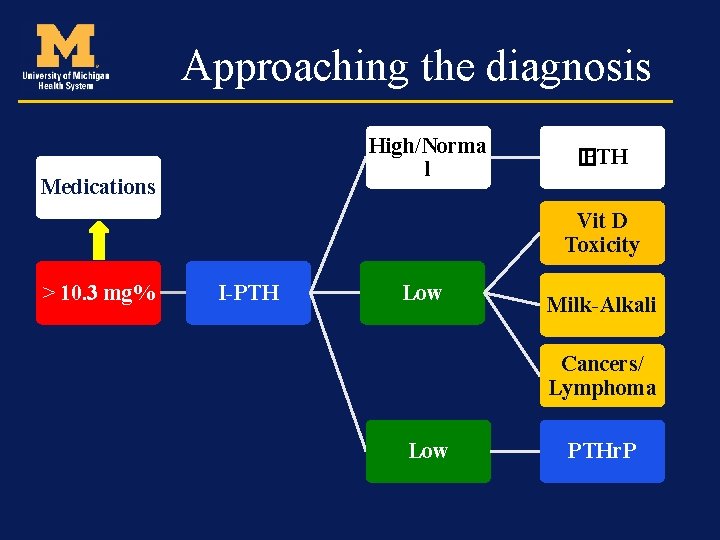
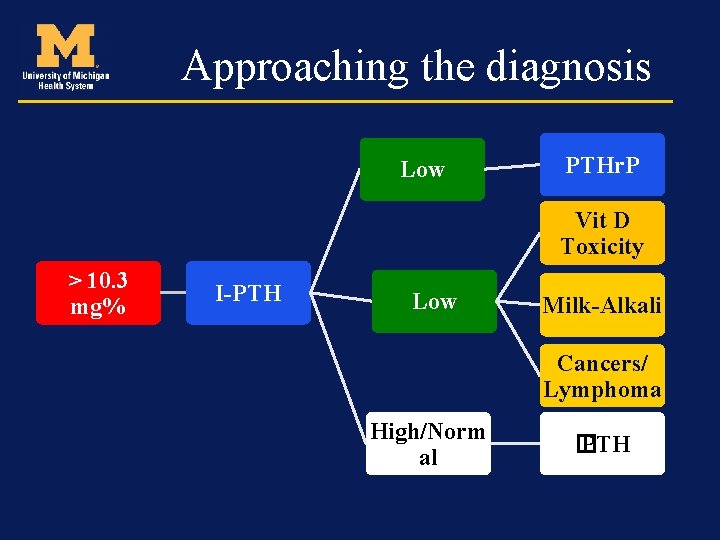
Approaching the diagnosis High/Norma l Medications � PTH Vit D Toxicity > 10. 3 mg% I-PTH Low Milk-Alkali Cancers/ Lymphoma Low PTHr. P

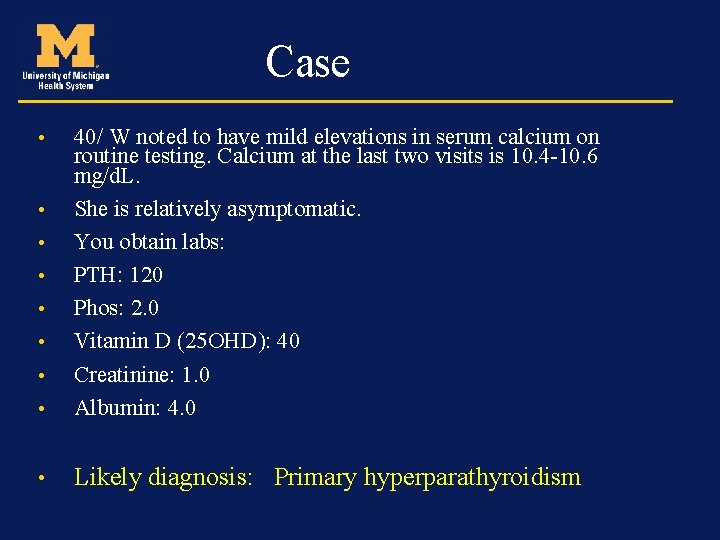
Case • 40/ W noted to have mild elevations in serum calcium on routine testing. Calcium at the last two visits is 10. 410. 6 mg/d. L. • She is relatively asymptomatic. • You obtain labs: • PTH: • 120

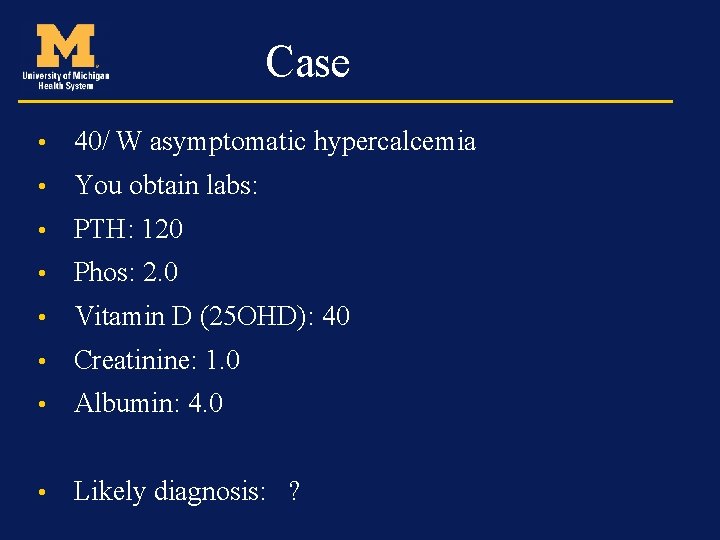
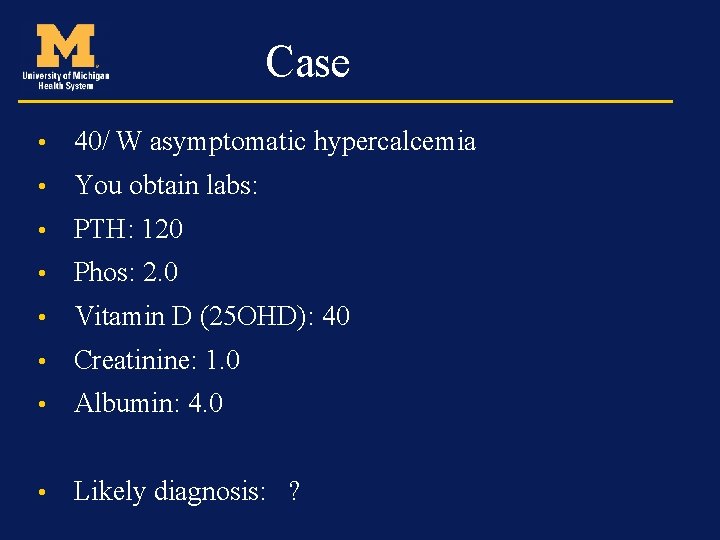
Case • 40/ W asymptomatic hypercalcemia • You obtain labs: • PTH: 120 • Phos: 2. 0 • Vitamin D (25 OHD): 40 • Creatinine: 1. 0 • Albumin: 4. 0 • Likely diagnosis: ?
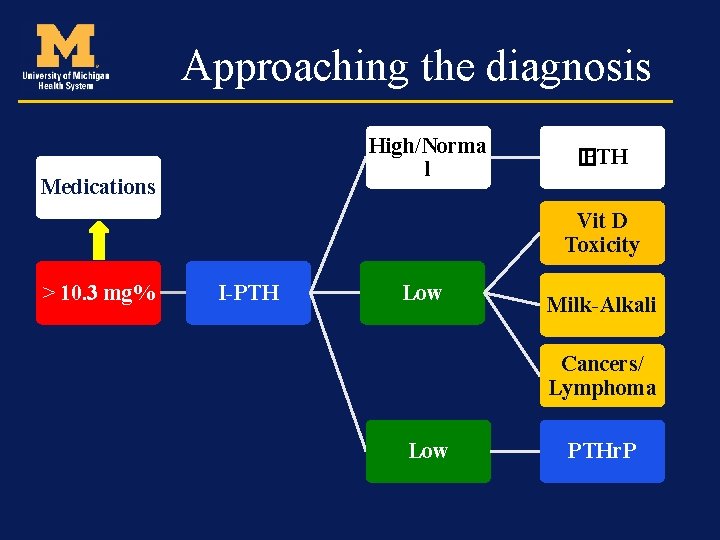
Approaching the diagnosis High/Norma l Medications � PTH Vit D Toxicity > 10. 3 mg% I-PTH Low Milk-Alkali Cancers/ Lymphoma Low PTHr. P
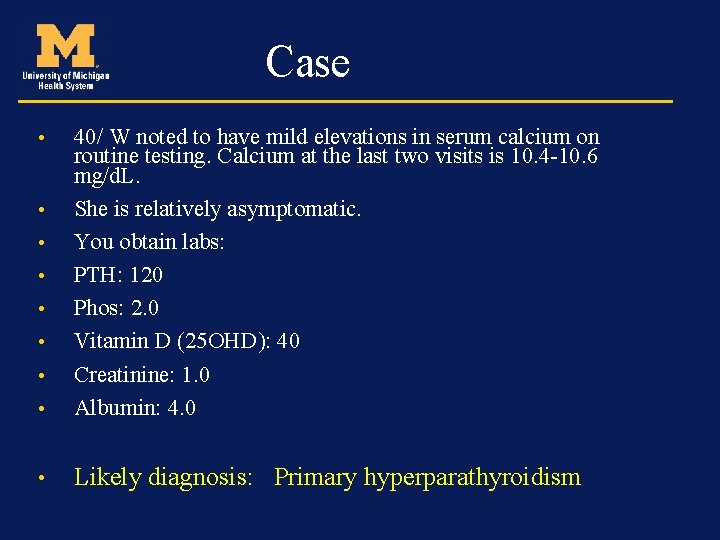
Case • 40/ W noted to have mild elevations in serum calcium on routine testing. Calcium at the last two visits is 10. 4 -10. 6 mg/d. L. She is relatively asymptomatic. You obtain labs: PTH: 120 Phos: 2. 0 Vitamin D (25 OHD): 40 Creatinine: 1. 0 Albumin: 4. 0 • Likely diagnosis: Primary hyperparathyroidism • •
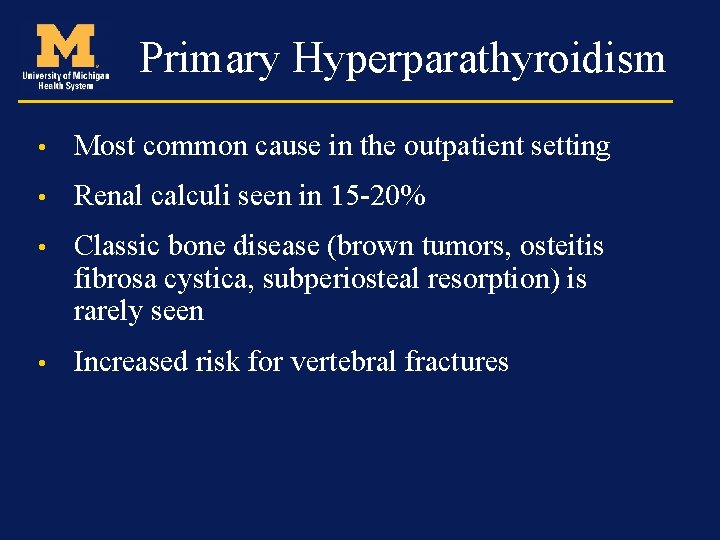
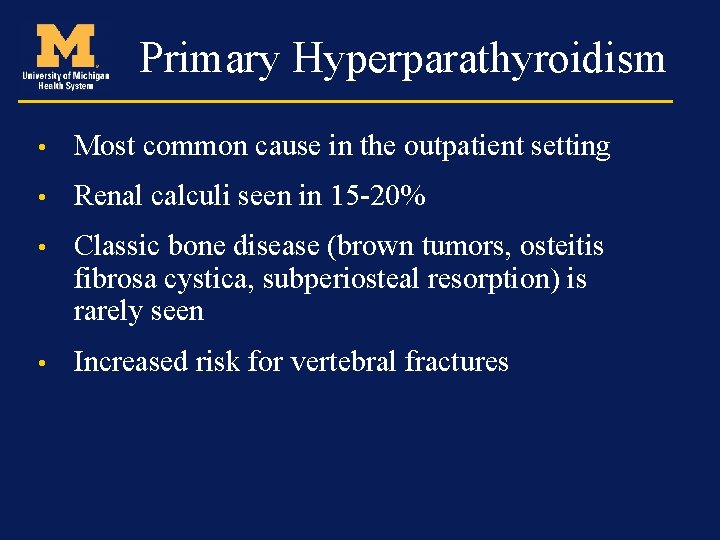
Primary Hyperparathyroidism • Most common cause in the outpatient setting • Renal calculi seen in 15 -20% • Classic bone disease (brown tumors, osteitis fibrosa cystica, subperiosteal resorption) is rarely seen • Increased risk for vertebral fractures
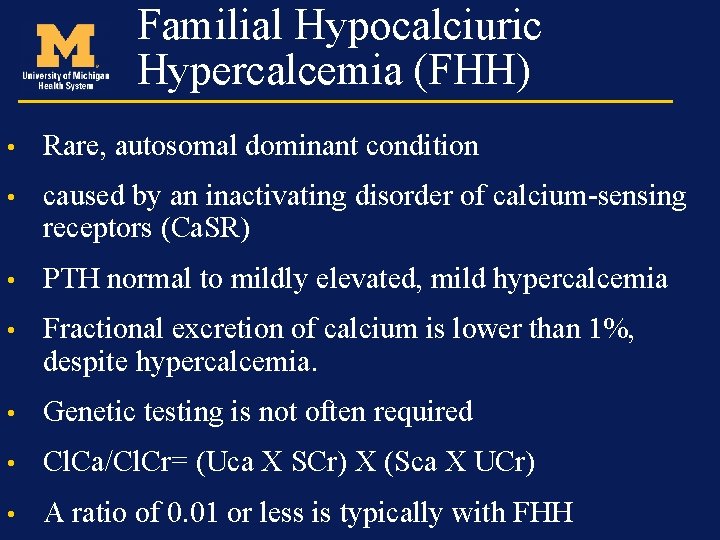
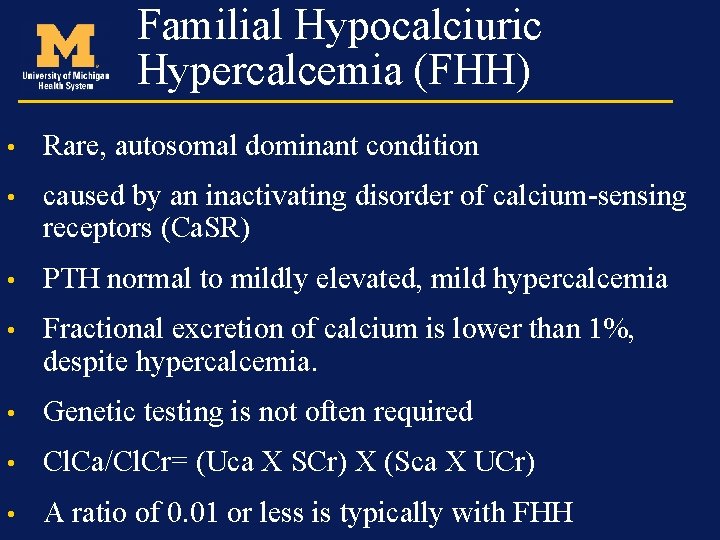
Familial Hypocalciuric Hypercalcemia (FHH) • Rare, autosomal dominant condition • caused by an inactivating disorder of calcium-sensing receptors (Ca. SR) • PTH normal to mildly elevated, mild hypercalcemia • Fractional excretion of calcium is lower than 1%, despite hypercalcemia. • Genetic testing is not often required • Cl. Ca/Cl. Cr= (Uca X SCr) X (Sca X UCr) • A ratio of 0. 01 or less is typically with FHH
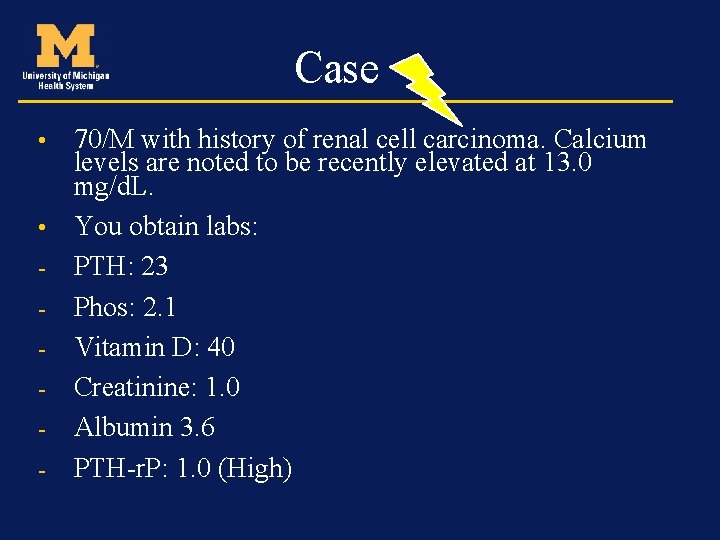
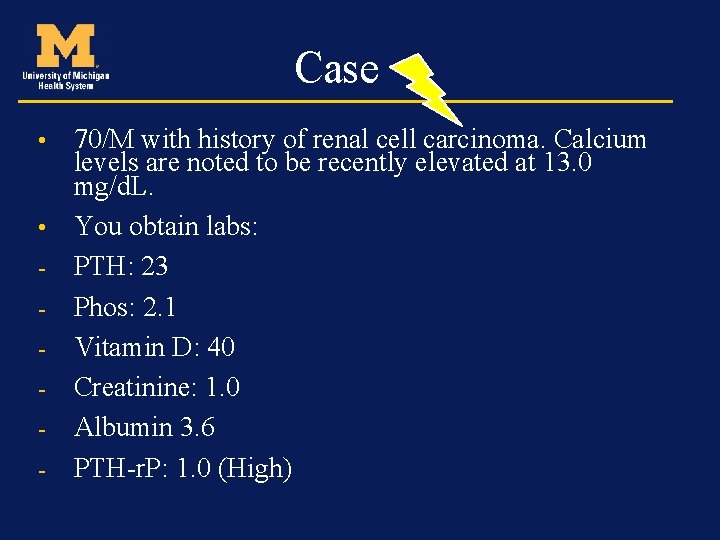
Case 70/M with history of renal cell carcinoma. Calcium levels are noted to be recently elevated at 13. 0 mg/d. L. • You obtain labs: - PTH: 23 - Phos: 2. 1 - Vitamin D: 40 - Creatinine: 1. 0 - Albumin 3. 6 - PTH-r. P: 1. 0 (High) •
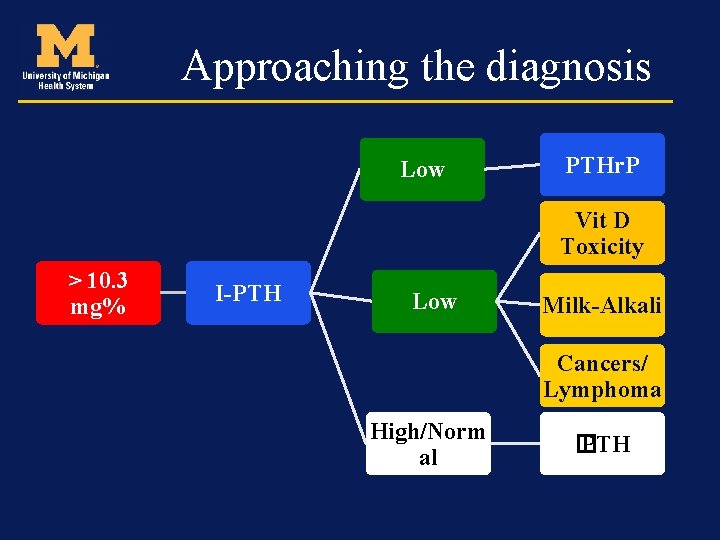
Approaching the diagnosis Low PTHr. P Vit D Toxicity > 10. 3 mg% I-PTH Low Milk-Alkali Cancers/ Lymphoma High/Norm al � PTH

Case • 70/M with history of renal cell carcinoma. Calcium levels are noted to be recently elevated at 13. 0 mg/d. L. • You obtain labs: - PTH: 23 - Phos: 2. 1 - Vitamin D: 40 - Creatinine: 1. 0 - Albumin 3. 6 - PTH-rp: 1. 0 (High) - Likely diagnosis: Hypercalcemia of malignancy
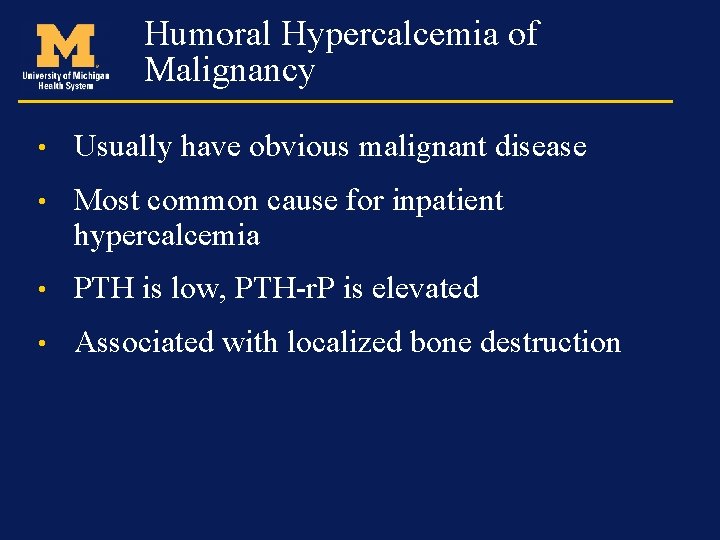
Humoral Hypercalcemia of Malignancy • Usually have obvious malignant disease • Most common cause for inpatient hypercalcemia • PTH is low, PTH-r. P is elevated • Associated with localized bone destruction
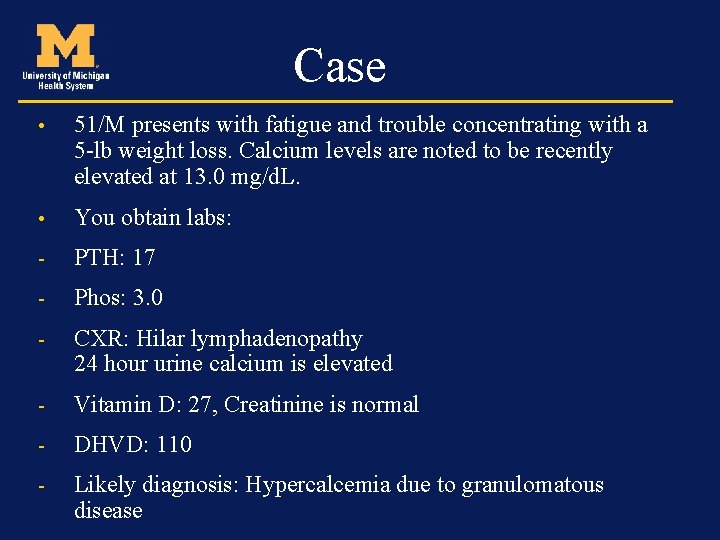
Case • 51/M presents with fatigue and trouble concentrating with a 5 -lb weight loss. Calcium levels are noted to be recently elevated at 13. 0 mg/d. L. • You obtain labs: - PTH: 17 - Phos: 3. 0 - CXR: Hilar lymphadenopathy 24 hour urine calcium is elevated - Vitamin D: 27, Creatinine is normal - DHVD: 110 - Likely diagnosis: Hypercalcemia due to granulomatous disease
Hypercalcemia associated with granulomatous diseases • Sarcoidosis is most commonly associated although can occur in any granulomatous disease • Increased activation of 1α hydroxylase that converts 25 OHD to 1, 25(OH)2 D
Intended Learning Outcomes –Review calcium metabolism –Describe symptoms of hypercalcemia –Review the etiology of hypercalcemia –Discuss the treatments for hypercalcemia –Conclusions
Treatment • Asymptomatic or mildly symptomatic patients do not require immediate treatment • Chronic hypercalcemia with no symptoms 12 -14 mg/dl can be monitored as well • > 14 mg/dl needs treatment even if asymptomatic
Treatment • Correction of dehydration/volume depletion • Correction of any electrolyte abnormalities • Discontinuation of medications that may cause calcium elevation • Reduction of dietary calcium in states of intestinal hyperabsorption (vitamin D intoxication and milk alkali) • Weight bearing or mobilization

The Four Rx Modalities I. V. Saline Hydration & Diuresis Gluco. Corticoids Antiresorptives Calcitonin I. M/S. C.
Treatment • Agents that decrease the release of calcium from bone or increase the uptake of calcium into bone • Agents that increased urinary excretion of calcium • Agents that reduce intestinal absorption of calcium
Treatment • IV fluids Depending on clinical status 200 -300 ml/hour to maintain UO of 100 -150 ml/hour Dehydration can make hypercalcemia worse by impairing the renal excretion of calcium
Salmon Calcitonin • IM or SQ injections at dose of 4 IU/kg • At 6 -12 hour intervals • Modest reductions and low toxicity profile • Vitamin D intoxication and immobilization • Acts quickly • Escape phenomenon may develop in 48 hours
Bisphonates • Inhibit release of calcium by interfering with osteoclast mediated bone resorption • More potent than saline and calcitonin • Can be used for hypercalcemia of any cause • Max effect seen in 2 -4 days • Also used to prevent hypercalcemia and skeletal events in malignancy
Bisphonates • Pamidronate 60 or 90 mg IV over 2 -4 hours • Zoledronic acid (ZA) 4 mg over 15 minutes • ZA preferred due to quicker infusion time • Side effects (low grade fever, myalgias, osteonecrosis of the jaw, atypical fractures)
NEWER THERAPIES • DENOSUMAB monoclonal antibody • RANKL inhibitor • Humoral hypercalcemia of malignancy • Bisphonate refractory hypercalcemia
Treatment • Agents that decrease the release of calcium from bone or increase the uptake of calcium into bone • Agents that increased urinary excretion of calcium • Agents that reduce intestinal absorption of calcium
Loop diuretics • WITH SALINE • Correct volume depletion first! • 80 -120 mg every 2 -6 hours • Monitor lytes, large losses of K and Mg • Fallen out of favor: 1) Better drugs 2) Frequent monitoring of lytes
Dialysis • Renal insufficiency • Congestive heart failure • Life threatening hypercalcemia

Treatment • Agents that decrease the release of calcium from bone or increase the uptake of calcium into bone • Agents that increased urinary excretion of calcium • Agents that reduce intestinal absorption of calcium
Glucocorticoids • Vitamin D intoxication or endogenous production of calcitriol (sarcoidosis, TB) • Prednisone 20 -40 mg • Lowers calcium in 2 -5 days
Intended Learning Outcomes –Review calcium metabolism –Describe symptoms of hypercalcemia –Review the etiology of hypercalcemia –Discuss the treatments for hypercalcemia –Conclusions

Conclusion • Most common cause of hypercalcemia in the outpatient setting is primary hyperparathyroidism • Most common cause of hypercalcemia in the inpatient setting is malignancy • Establishing the cause is important for treatment decisions

palak@med. umich. edu
 Palak choksi
Palak choksi Anne evered
Anne evered Mds
Mds Palak desai md
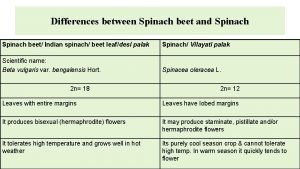
Palak desai md Spinach and palak difference
Spinach and palak difference Hypercalcemia
Hypercalcemia Hypercalcemia ecg
Hypercalcemia ecg Familial hypocalciuric hypercalcemia
Familial hypocalciuric hypercalcemia Sevelamer hypercalcemia
Sevelamer hypercalcemia Simple cardiac cycle flow chart
Simple cardiac cycle flow chart Familial hypocalciuric hypercalcemia
Familial hypocalciuric hypercalcemia Hypercalcemia ecg
Hypercalcemia ecg Hypercalcemia nephrogenic di
Hypercalcemia nephrogenic di Hypercalcemia
Hypercalcemia Hypercalcemia workup
Hypercalcemia workup Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference The nursing process
The nursing process Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Nursing diagnosis three parts
Nursing diagnosis three parts Theoretical models of counseling
Theoretical models of counseling What is research approach definition
What is research approach definition Waterfall approach in international marketing
Waterfall approach in international marketing Traditional approach to systems implementation
Traditional approach to systems implementation Multiple approach avoidance conflict
Multiple approach avoidance conflict Deep learning approach and surface learning approach
Deep learning approach and surface learning approach Virtual circuit network and datagram network
Virtual circuit network and datagram network Cognitive approach vs behavioral approach
Cognitive approach vs behavioral approach Công thức tính thế năng
Công thức tính thế năng Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Phản ứng thế ankan
Phản ứng thế ankan Môn thể thao bắt đầu bằng từ chạy
Môn thể thao bắt đầu bằng từ chạy Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu điện thế nghỉ
điện thế nghỉ Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Gấu đi như thế nào
Gấu đi như thế nào Ng-html
Ng-html Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Phối cảnh
Phối cảnh Một số thể thơ truyền thống
Một số thể thơ truyền thống Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Sơ đồ cơ thể người
Sơ đồ cơ thể người Các số nguyên tố là gì
Các số nguyên tố là gì Tư thế ngồi viết
Tư thế ngồi viết đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ