HYDROCEPHALUS Hydrocephalus A syndrome or sign resulting from

















- Slides: 59
HYDROCEPHALUS
Hydrocephalus • A syndrome, or sign, resulting from disturbances in the dynamics of cerebrospinal fluid (CSF), which may be caused by several diseases.

Incidence • Occurs in 3 -4 of every 1000 births. • Cause may be congenital or acquired. • Congenital- may be due to maldevelopment or intrauterine infection • Acquired- may be due to infection, neoplasm or hemorrhage.
Pathophysiology • CSF is formed by two mechanisms: – Secretion by the choroid plexus, – Lymphatic-like drainage by the extracellular fluid in brain. CSF circulates thru ventricular system and is absorbed within subarachnoid spaces by unknown mechanism.

Mechanisms of Fluid Imbalance • Hydrocephalus results from: • 1. Impaired absorption of CSF within the subarachnoid space (communicating hydrocephalus), or • 2. Obstruction to the flow of CSF through the ventricular system (noncommunicating hydrocephalus)
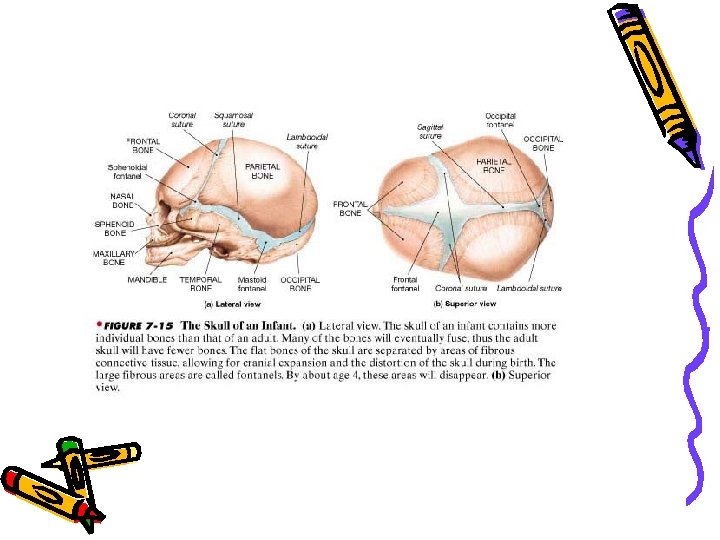
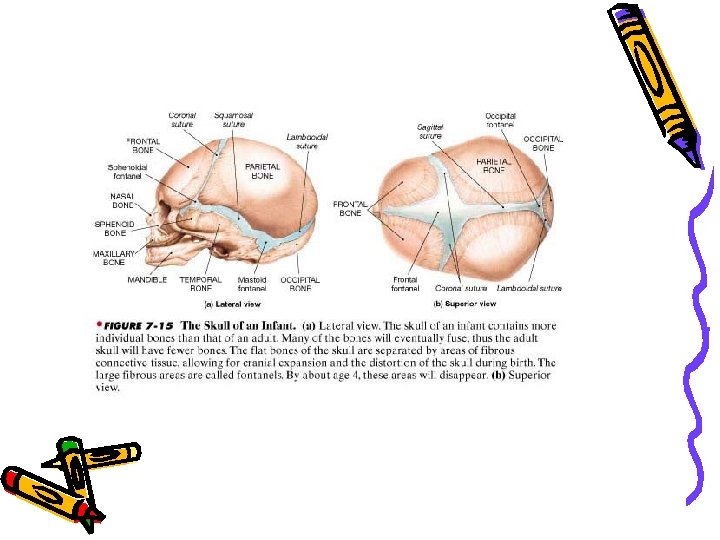
Mechanisms of fluid imbalance • Both lead to increase accumulation of CSF in the ventricles! • Ventricles become dilated and compress the brain. • When this happens before cranial sutures are closed, skull enlarges. • In children <10 -12, previously closed sutures may open.
Hydrocephalus • Most cases of non-communicating (obstructive) hydrocephalus are a result of developmental malformations. • Other causes: neoplasms, intrauterine infections, trauma. • Developmental defects account for most causes of hydrocephalus from birth to 2 years of age.
Common Defects • Arnold-Chiari Malformation (ACM) – Type 2 malformation of brain seen most exclusively with myelomeningocele, is characterized by herniation of a small cerebellum, medulla, pons, and fourth ventricle into the cervical spinal canal through an enlarged foramen magnum.

Clinical manifestations • Clinical picture depends on acuity of onset and presence of preexisting structural lesions.
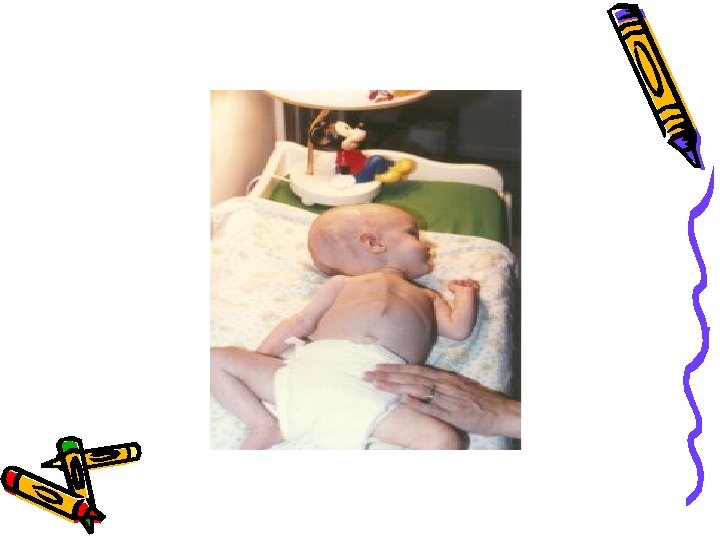
Infancy • Head grows at alarming rate with hydrocephalus. – First signs- bulging of fontanels without head enlargement. – Tense, bulging, non-pulsatile anterior fontanel – Dilated scalp veins, esp. when crying – Thin skull bones with separated sutures (cracked pot sounds on percussion)

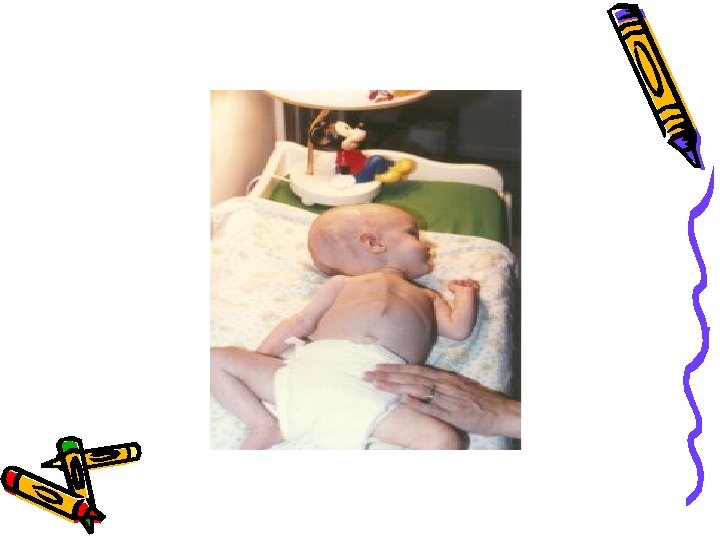
Infancy • Protruding forehead or bossing. • Depressed eyes or setting-sun eyes (eyes rotating or downward with sclera visible above pupil) • Pupils sluggish with unequal response to light • Irritability, lethargy, feeds poorly, changes in LOC, arching of back (opisthotonos), lower extremity spasticity. • May cry when picked up or rocked; quiets when allowed to lay still.
Infancy • Swallowing difficulties, stridor, apnea, aspiration, respiratory difficulties and arm weakness may indicate brain stem compression. • If hydrocephalus progresses, difficulty sucking and feeding, and a high-pitched shrill cry results. (lower brain stem dysfunction)
Infancy • Emesis, somnolence, seizures, and cardiopulmonary distress ensues and hydrocephalus progresses. • Severely affected infants may not survive neonatal period.


Childhood • Signs and symptoms caused by increased ICP. • Manifestations caused by posterior neoplasms and aqueduct stenosis, manifestations associated with space -occupying lesions.
Childhood • Headache on awakening with improvement following emesis or sitting up. • Papilledema (swelling of optic disc DT obstruction), strabismus, and extrapyramidal tract signs such as ataxia • Irritability, lethargy, apathy, confusion, and often incoherent

Childhood • Dandy-Walker syndrome- congenital defect-late onset. – Obstruction of foramen of Lushka and Magendie – Bulging occiput, nystagmus, ataxia, cranial nerve palsies – Female predominance (3: 1) – Absence or occlusion of ventricles
Diagnostic Evaluation • Antenatal- fetal ultrasound as early as 14 weeks • Infancy- based on head circumference crosses one or more grid lines on the infant growth chart within a 4 week period and there are progressive neuro signs. • CT and MRI to localize site of obstruction; reveal large ventricles

Therapeutic management • • Goals: Relieve hydrocephaly Treat complications Manage problem resulting from effects of disorder on psychomotor development • USUALLY SURGICAL!
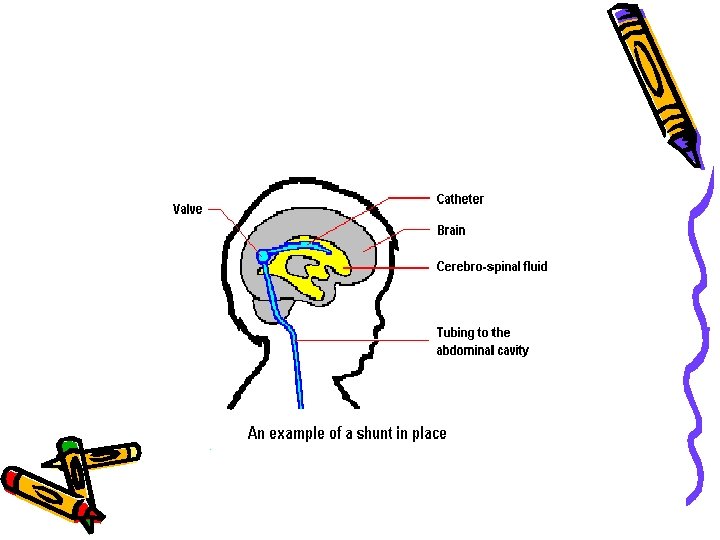
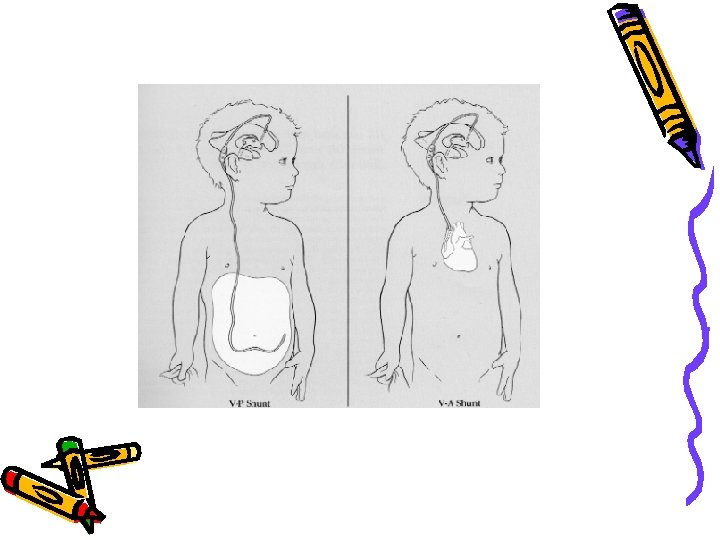
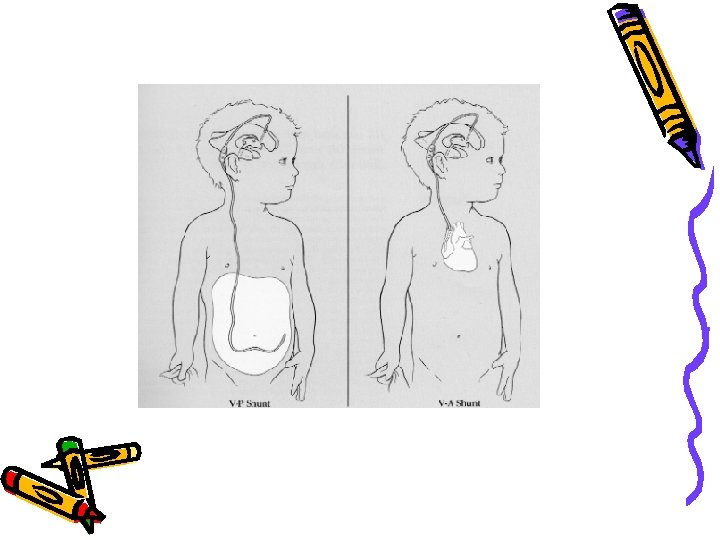
Surgical Treatment • Therapy of choice! • Direct removal of source of obstruction (neoplasm, cyst, or hematoma) • Most require shunt procedure to drain CSF from ventricles to extracranial area; usually peritoneum(VP shunt), or right atrium (VA shunt) for absorption.
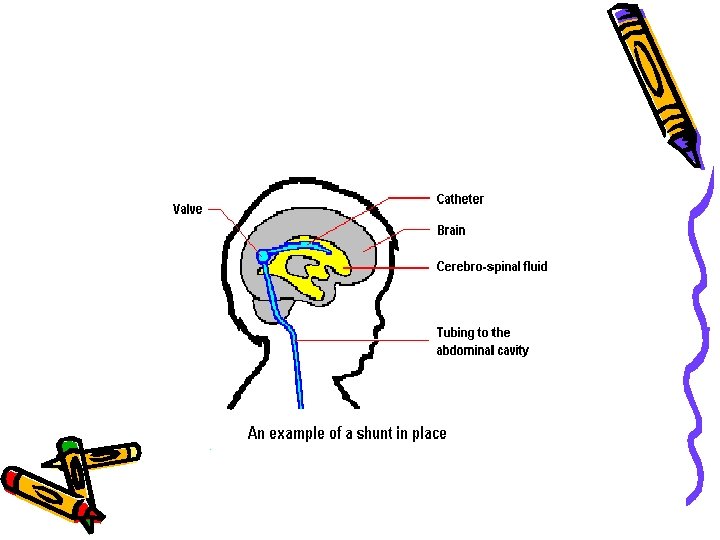

VP shunt • Used in neonates and young infants • Greater allowance for excess tubing; which minimizes number of revisions needed as child grows

VA shunt • Reserved for older children who have attained most of somatic growth, or children with abdominal pathology. • Contraindicated in children with cardiopulmonary disease or with elevated CSF protein.

Major Complications • Shunt infection is most serious complication! • Period of greatest risk is 1 to 2 months following placement. • Staph and strep most common organisms
Complications • Mechanical difficulties kinking, plugging, migration of tubing. • Malfunction is most often by mechanical obstruction! • Look for signs of increased ICP; fever, inflammation and abdominal pain.

Post-op care • In addition to routine post-op care: – 1. Place on unoperated side to prevent pressure on shunt valve – 2. Keep HOB flat; rapid decrease in IC fluid may cause subdural hematoma due to small vein rupture in cerebral cortex. – 3. Do not pump shunt without specific direction from doctor (too many different pump devices)
Post-op care • 4. Observe for signs of Increased ICP! May indicate obstruction of shunt! – Assess pupil size; as pressure on oculomotor nerve may cause dilation on same side as pressure. – Blood pressure may be variable due to hypoxia to brainstem – Abdominal distention- due to CSF peritonitis or post-op ileus due to catheter placement.
Post-op • 5. Monitor I and O- may be on fluid restriction or NPO for 24 hours to prevent fluid overload. • 6. Monitor VS- increased temp may indicate infection. • 7. Give good skin care to prevent tissue damage, etc.
Family support • Fear • Communication of procedures • Prepare for discharge.
SPINA BIFIDA • Neural Tube defects are largest group of congenital anomalies. • Failure of neural tube to close produces defects of either entire neural tube or small areas.
Etiology • Anacephaly and spina bifida occur together very often. • Higher in females than males • 50% occur due to nutritional deficiency (folic acid)
Spina Bifida • Defined as midline defects involving failure of the bony spine to close. • Spina bifida occulta- defect not visible externally. – Occurs most often in lumbosacral area. – Not apparent unless there are gait disturbances, foot deformities, sphincter dysfunction or other neuromuscular manifestations. – Many people with occulta will never have any deficits and may not know they have it.

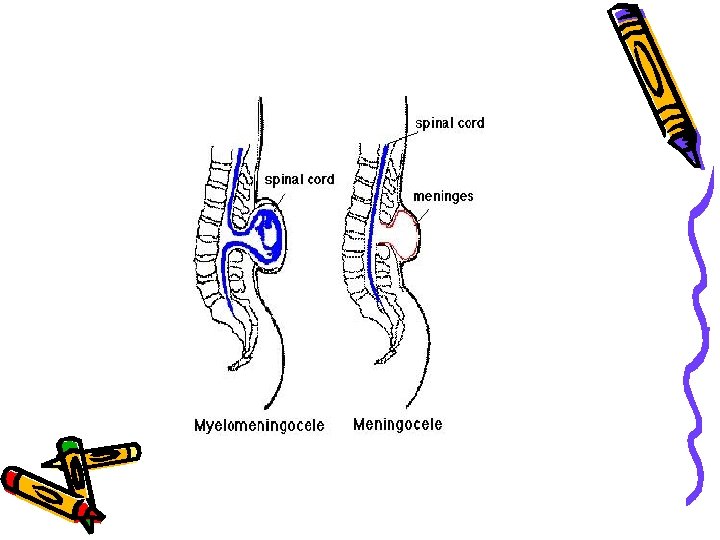
Spina Bifida • Spina Bifida cystica- visible defect with external saclike protrusion. – A. meningocele- encases meninges and spinal fluid, but no neurological deficits. – B. meningomyelocele-contains meninges, spinal fluid, and nerves. Neuromotor deficits depend on anatomic level of protrusion and nerves involved.
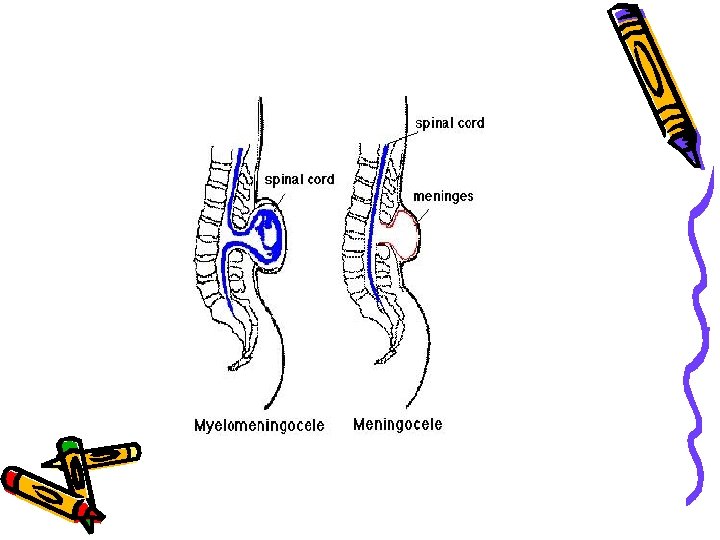


Meningomyelocele • AKA spina bifida • Develops during first 28 days of pregnancy when neural tube fails to close and fuse. • 90% of spinal cord lesions, and may occur at any point along spine. • Sac usually enclosed in fine membrane that is prone to tears.
meningomyelocele • Largest number in lumbar or lumbosacral area • 90 -95% of children have hydrocephalus • Careful monitoring of head size important • Chiari malformation may be present: observe infant for stridor, hoarse cry from vocal cord paralysis; feeding difficulties, deteriorating upper extremity function.
Clinical manifestations • S/S vary according to degree of spinal defect. • Readily apparent on inspection! • Loss of sensation below lesion • Poor urinary and bladder control • Joint deformities in lower extremities • Scoliosis or kyphosis • Hip dislocations
Diagnostic evaluation • Examination of meningeal sac and clinical manifestations • MRI, CT to assess condition of brain and spinal cord. Other defects may be present. • Prenatal- fetal ultrasound or amniotic fluid sample for (alpha-fetal protein (AFP). • Test should be done between 16 and 18 weeks of gestation. Afterwards AFP level drops, making detection of SB difficult. Also, therapeutic abortion not option after this time.


Therapeutic management • Multi-disciplinary approach – Neurology, neuro-surgery, pediatrics, urology, orthopedics, rehabilitation, PT, OT, social services, intensive nursing in many areas.
Goals • 1. prevent infection • 2. early closure of lesion, within 72 hours (prevents infection and trauma to exposed tissues, and prevents further motor impairment). Goal is satisfactory skin coverage of lesion! • 3. PT for specific deformity
Goals • Physical therapy to prevent joint contractures. – Correct deformity, prevent skin breakdown, obtain best ambulatory functioning
Goals • Management of genitourinary function: – Mylemeningocele is a common cause of neurogenic bladder which leads to urinary system distress (frequent UTI’s, ureterohydronephrosis, vesicoureteral reflux, renal insufficiency. – Urinary incontinence is common
Goals • Clean, intermittent catherization as a conservative treatment. • Vesicostomy (anterior wall of bladder brought through abdominal wall to create stoma) may be done for bladder control. • Meticulous skin care is needed!
Post-op • Use touch for stimulation, since can’t hold • Observe for increased ICP, such as bulging fontanels • Assess for infection: – Increased or decreased temperature, irritability, nuchal rigidity,
Home Care • Involve parents in care – Positioning/feeding/skin care/range of motion exercises/ clean catheterization when prescribed, complications. – Help with assistive devices (if child is paraplegic use hands/arms, etc. ) – Long range planning
 Sign shapes meaning
Sign shapes meaning Hypocalcemia chvostek
Hypocalcemia chvostek Same signs
Same signs Positive trousseau's sign
Positive trousseau's sign Hypophosphatemia symptoms
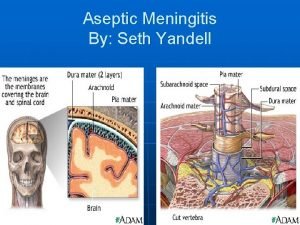
Hypophosphatemia symptoms Aseptic meningitis,
Aseptic meningitis, Communicating hydrocephalus
Communicating hydrocephalus Neck wrapping for low-pressure hydrocephalus
Neck wrapping for low-pressure hydrocephalus Ventricular system
Ventricular system Brain hemorrhage
Brain hemorrhage Acetazolamide dose in hydrocephalus
Acetazolamide dose in hydrocephalus Normal pressure hydrocephalus
Normal pressure hydrocephalus Macrocephaly vs hydrocephalus
Macrocephaly vs hydrocephalus Myelomeningocele with hydrocephalus
Myelomeningocele with hydrocephalus Complications of hydrocephalus
Complications of hydrocephalus Hydrocephalus triad
Hydrocephalus triad Wessex neurological centre
Wessex neurological centre Complications of hydrocephalus
Complications of hydrocephalus Differentials of hydrocephalus
Differentials of hydrocephalus Functions of csf
Functions of csf Stroke precautions nursing
Stroke precautions nursing Complication of hydrocephalus
Complication of hydrocephalus Macewen sign icp
Macewen sign icp N
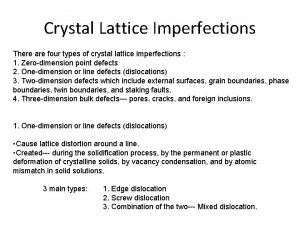
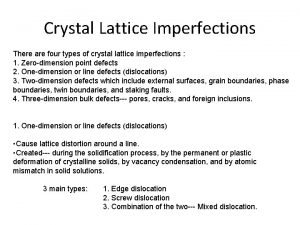
N Lattice imperfections
Lattice imperfections Lattice imperfections
Lattice imperfections Learning is any relatively permanent change
Learning is any relatively permanent change Cylinder cut perpendicular to base
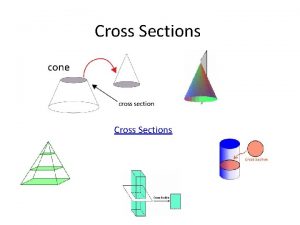
Cylinder cut perpendicular to base Learning is a permanent change in behavior
Learning is a permanent change in behavior A misconception resulting from incorrect reasoning
A misconception resulting from incorrect reasoning Careless neglect often resulting in injury
Careless neglect often resulting in injury Resulting trust
Resulting trust Levator ani syndrome
Levator ani syndrome Syndrome pyramidal de type capsulaire
Syndrome pyramidal de type capsulaire Taiwan earthquake
Taiwan earthquake Alagille syndrome
Alagille syndrome Miller dieker syndrome
Miller dieker syndrome Trisomy male
Trisomy male Billroth 2
Billroth 2 Zion clark anatomie
Zion clark anatomie Dumping syndrome signs
Dumping syndrome signs Digeorge symdrome
Digeorge symdrome Sinus arrest vs sinus block
Sinus arrest vs sinus block Eds
Eds Wolfram syndrome
Wolfram syndrome Bertolotti's syndrome
Bertolotti's syndrome Budd-chiari syndrome triad
Budd-chiari syndrome triad Patau syndrome
Patau syndrome Cryoprecipitate dose
Cryoprecipitate dose Fat malabsorption
Fat malabsorption Tubal ligation side effects
Tubal ligation side effects Acute glomerulonephritis causes
Acute glomerulonephritis causes Hemi neglect
Hemi neglect Crest syndrom
Crest syndrom Stickler syndrome pictures
Stickler syndrome pictures Splinter skills definition
Splinter skills definition Refeeding syndrome
Refeeding syndrome Static posture assessment
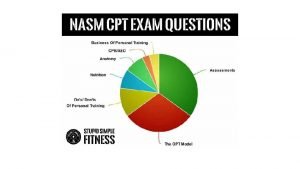
Static posture assessment Trisomy 18
Trisomy 18 Acute radiation syndrome
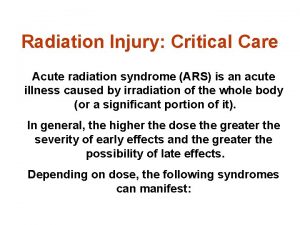
Acute radiation syndrome