Humana Gold Plus Integrated A Commonwealth Coordinated Care

- Slides: 13

Humana Gold Plus Integrated, A Commonwealth Coordinated Care Plan Orientation Training 996 VA 0315
Who we are: Humana and its various businesses serve more than 13 million members across the country. Humana delivers primary care and occupational health care services through a network of more than 300 wholly owned medical centers and clinics. • Founded in 1961. • Long-term commitment to seniors and chronically ill. • 5 million Medicare Advantage and Part D members. • 550, 000 dual-eligible Medicare-Medicaid members. • 18 years Medicaid experience. Humana’s Values • Thrive Together • Cultivate Uniqueness • Pioneer Simplicity • Inspire Health • Rethink Routine 2
Humana for Virginia Our eight years of experience in Virginia prepare us well to meet the specific needs of our members. Our Virginia Footprint: • 120, 000 Medicare Advantage and 98, 000 Medicare Prescription Drug Plan members • Only Dual-eligible Special Needs Plan (D-SNP) within the Commonwealth Coordinated Care (CCC) demonstration area • Unique collaborations with Virginia provider groups and clinic arrangements (e. g. , Jen. Care®) aimed at promoting quality, delivering high standards of care and providing access to coverage in areas historically underserved • Highly rated Medicare Advantage HMO plan across Virginia (achieving a CMS rating of 3. 5 of 5 stars) 3
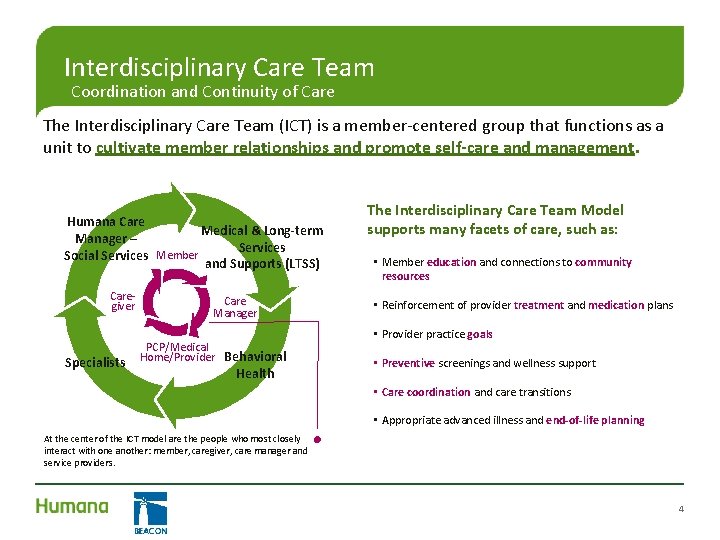
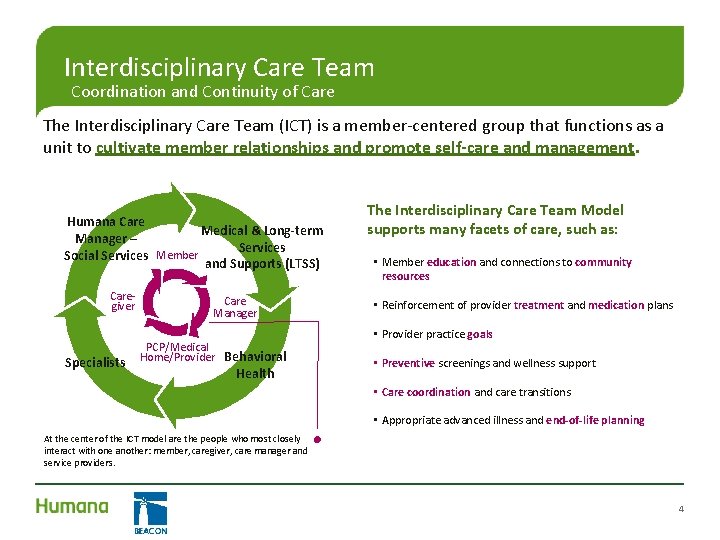
Interdisciplinary Care Team Coordination and Continuity of Care The Interdisciplinary Care Team (ICT) is a member-centered group that functions as a unit to cultivate member relationships and promote self-care and management. Humana Care Medical & Long-term Manager – Services Social Services Member and Supports (LTSS) Caregiver Specialists Care Manager PCP/Medical Home/Provider Behavioral Health The Interdisciplinary Care Team Model supports many facets of care, such as: • Member education and connections to community resources • Reinforcement of provider treatment and medication plans • Provider practice goals • Preventive screenings and wellness support • Care coordination and care transitions • Appropriate advanced illness and end-of-life planning At the center of the ICT model are the people who most closely interact with one another: member, caregiver, care manager and service providers. 4
Tele-Psychiatry Services • Telemedicine is the real-time two-way transfer of medical data and information using an interactive audio/video connection for the purposes of medical diagnosis and treatment. • The Medicaid recipient is located with a provider at the “originating” site, while the “remote” provider renders services via the audio/video connection. • Equipment utilized for telemedicine must be of sufficient audio quality and visual clarity as to be functionally equivalent to a face-to-face encounter for professional medical services. 5
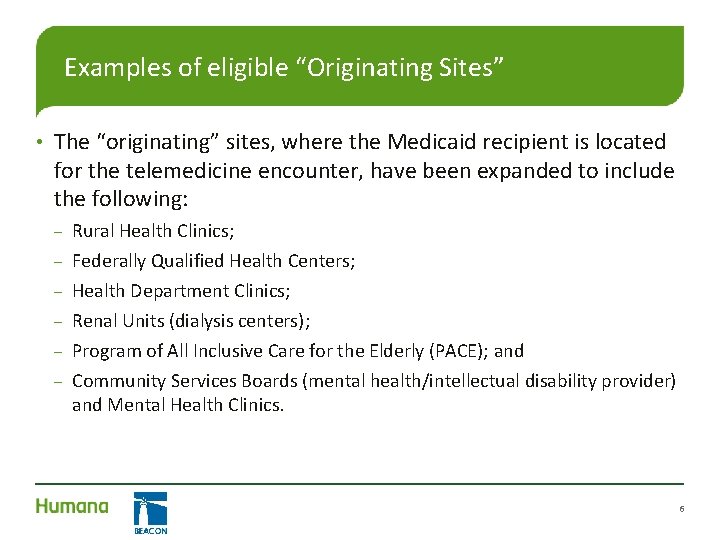
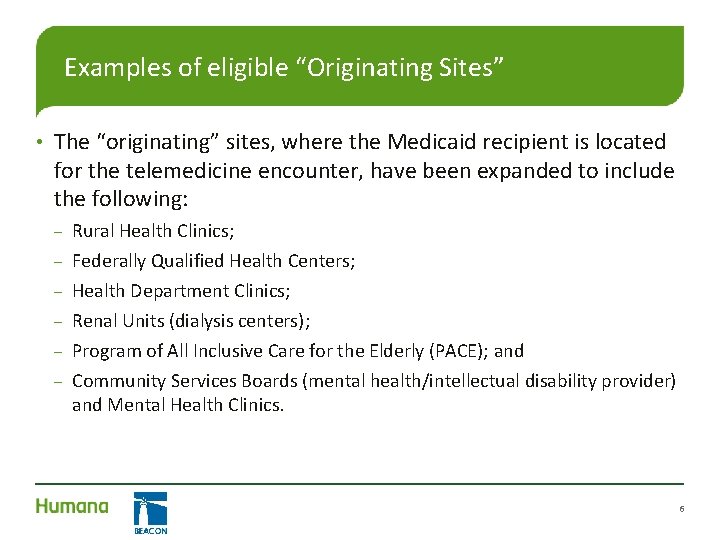
Examples of eligible “Originating Sites” • The “originating” sites, where the Medicaid recipient is located for the telemedicine encounter, have been expanded to include the following: – – – Rural Health Clinics; Federally Qualified Health Centers; Health Department Clinics; Renal Units (dialysis centers); Program of All Inclusive Care for the Elderly (PACE); and Community Services Boards (mental health/intellectual disability provider) and Mental Health Clinics. 6
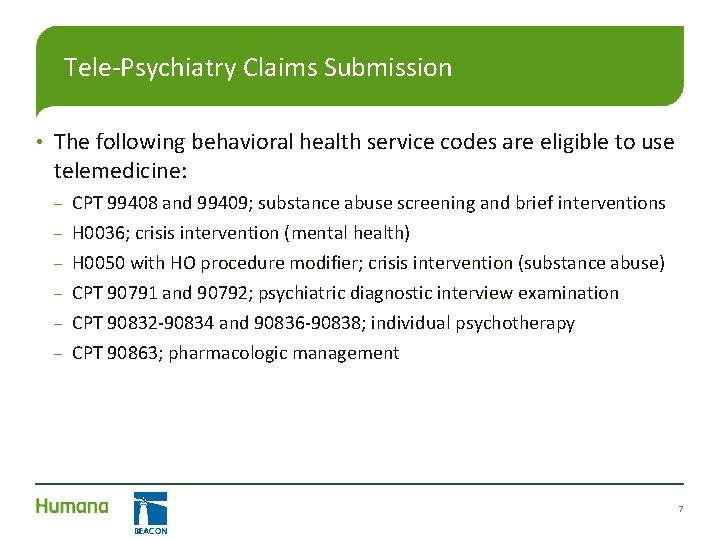
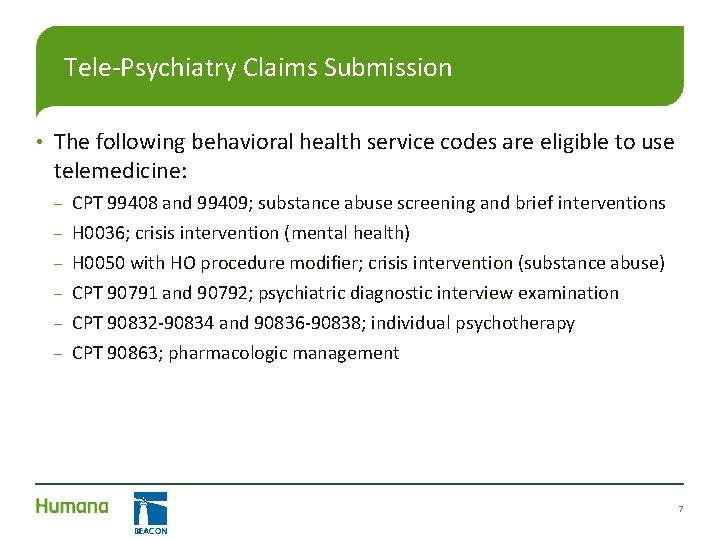
Tele-Psychiatry Claims Submission • The following behavioral health service codes are eligible to use telemedicine: – – – CPT 99408 and 99409; substance abuse screening and brief interventions H 0036; crisis intervention (mental health) H 0050 with HO procedure modifier; crisis intervention (substance abuse) CPT 90791 and 90792; psychiatric diagnostic interview examination CPT 90832 -90834 and 90836 -90838; individual psychotherapy CPT 90863; pharmacologic management 7
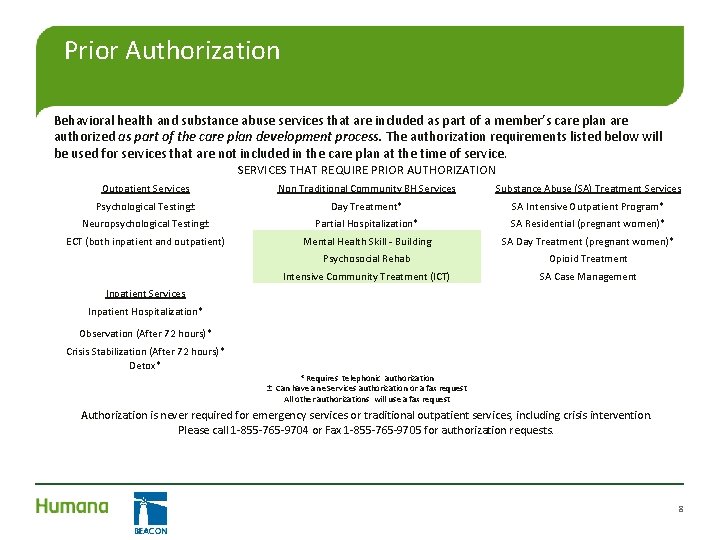
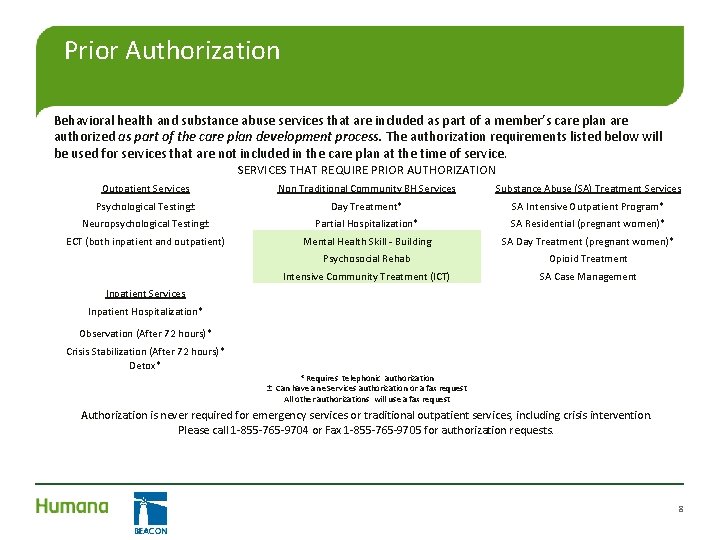
Prior Authorization Behavioral health and substance abuse services that are included as part of a member’s care plan are authorized as part of the care plan development process. The authorization requirements listed below will be used for services that are not included in the care plan at the time of service. SERVICES THAT REQUIRE PRIOR AUTHORIZATION Outpatient Services Non Traditional Community BH Services Substance Abuse (SA) Treatment Services Psychological Testing± Day Treatment* SA Intensive Outpatient Program* Neuropsychological Testing± Partial Hospitalization* SA Residential (pregnant women)* ECT (both inpatient and outpatient) Mental Health Skill - Building SA Day Treatment (pregnant women)* Psychosocial Rehab Opioid Treatment Intensive Community Treatment (ICT) SA Case Management Inpatient Services Inpatient Hospitalization* Observation (After 72 hours)* Crisis Stabilization (After 72 hours)* Detox* * Requires telephonic authorization ± Can have an e. Services authorization or a fax request All other authorizations will use a fax request Authorization is never required for emergency services or traditional outpatient services, including crisis intervention. Please call 1 -855 -765 -9704 or Fax 1 -855 -765 -9705 for authorization requests. 8
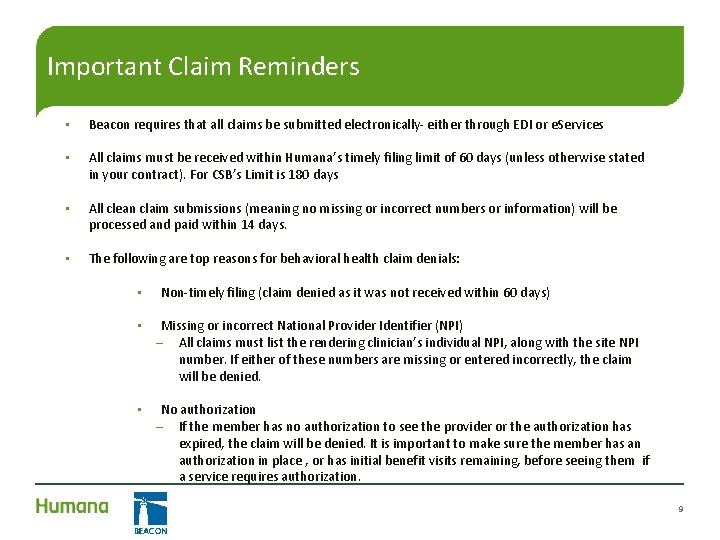
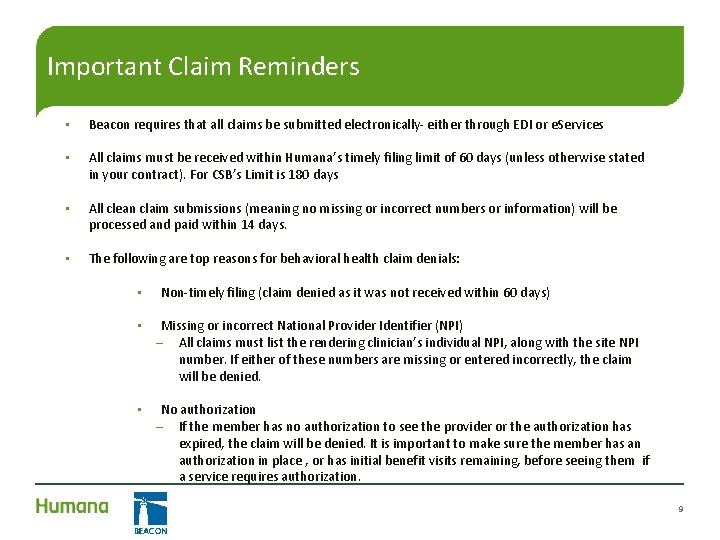
Important Claim Reminders • Beacon requires that all claims be submitted electronically- either through EDI or e. Services • All claims must be received within Humana’s timely filing limit of 60 days (unless otherwise stated in your contract). For CSB’s Limit is 180 days • All clean claim submissions (meaning no missing or incorrect numbers or information) will be processed and paid within 14 days. • The following are top reasons for behavioral health claim denials: • Non-timely filing (claim denied as it was not received within 60 days) • Missing or incorrect National Provider Identifier (NPI) – All claims must list the rendering clinician’s individual NPI, along with the site NPI number. If either of these numbers are missing or entered incorrectly, the claim will be denied. • No authorization – If the member has no authorization to see the provider or the authorization has expired, the claim will be denied. It is important to make sure the member has an authorization in place , or has initial benefit visits remaining, before seeing them if a service requires authorization. 9
e. Services is a free services for all contracted and in-network providers. The goal of e. Services is to make clinical, administrative and claims transactions easy to do. By using e. Services, health care providers will be able to: • Submit requests for authorization • Submit claims • Verify member eligibility for Humana • Confirm authorization status • Access assessments and care plan (feature under development) • Check claim status • View claims performance information • Access provider manuals, forms, bulletins and mailings • View or print frequently asked questions (FAQs) • Access Electronic Health Records (feature under development) • e. Services can be accessed at: https: //provider. beaconhs. com 10
Claims Submission – Electronic Data Interchange (EDI) Direct Electronic Claim Submission to Beacon: • Providers and/or their billing agents can submit electronic claims to Beacon using the standard HIPAA 837 transactions • Beacon Companion Guides and EDI Registration forms (Trading Partner Setup and Billing Intermediary Forms) are available on Beacon’s website at www. beaconhs. com/providers. html under Tools. • EDI Registration forms must be submitted to the EDI Operations team. They will work directly with you to complete the testing and setup process. They can be reached at 855 -765 -9704, or via email at ediops. miami@beaconhs. com. • Beacon provides 835 transactions via Pay. Span Health. Electronic Claim Submission through Emdeon: • Beacon allows EDI claims to be submitted through Emdeon • Emdeon Payer ID for Beacon is 43324 11
Resources • Beacon’s Provider website • Includes: • – Forms – LOCC – Provider manual (link) – eservices manual, and more • Humana’s Provider Manual For Physicians, Hospitals and Other Healthcare Providers • – Virginia Demonstration Appendix – February 2014 http: //apps. humana. com/marketing/ documents. asp? file=2308072 How to access: 1. Navigate to www. Beaconhs. com/providers. htm l 2. Click on tools. 3. Enter “Humana” in the search bar. 4. Select “Virginia” from the drop down menu. 12
Contact Information Humana’s Member Services Hotline: CCC Customer Service – 1 -855 -280 -4002 Beacon’s Provider Hotline: 855 -765 -9704 Provider Fax line 855 -765 -9705 Beacon’s TTY Number (for hearing impaired): 1 -855 -371 -3939 IVR: 1 -888 -210 -2018 Grievances and Clinical Appeals: Administrative/Claims Appeals: Humana Inc. CT Beacon Health Strategies LLC, Attn: Grievance and Appeals Attn: Claims Department PO Box 14546 10200 Sunset Drive Lexington, KY 40512 -4546 Miami, FL 33173 _________________________________ Beacon Network Contact Information Telephone: 855 -765 -9704 Email: Provider. Partnerships@beaconhs. com Scott Parker Beacon Program Director Telephone: 804 -793 -0463 Email: Scott. Parker@beaconhs. com John Strube Beacon Network Manager 804 -793 -0464 John. Strube@beaconhs. com Tim Pace Manager, Provider Partnerships 804 -793 -0476 Timothy. Pace@beaconhs. com 13