Human Tissue Authority Code of Practice F Revised





- Slides: 24
Human Tissue Authority Code of Practice F
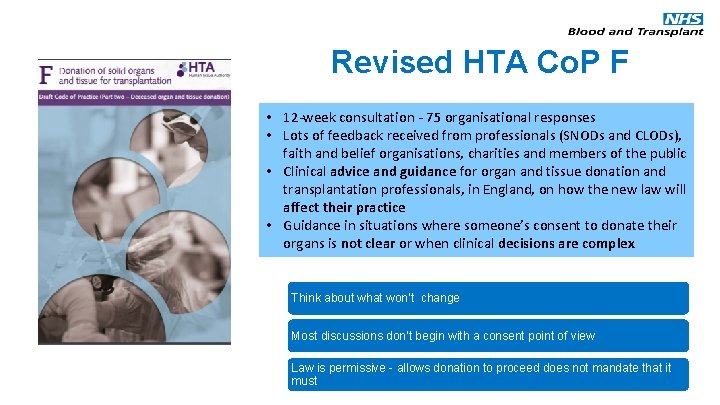
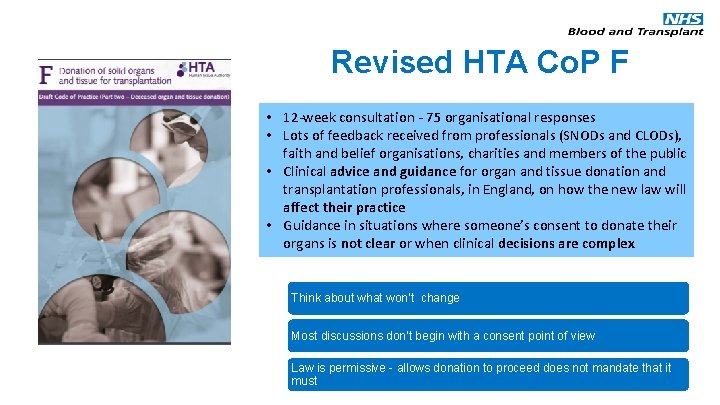
Revised HTA Co. P F • 12 -week consultation - 75 organisational responses • Lots of feedback received from professionals (SNODs and CLODs), faith and belief organisations, charities and members of the public • Clinical advice and guidance for organ and tissue donation and transplantation professionals, in England, on how the new law will affect their practice • Guidance in situations where someone’s consent to donate their organs is not clear or when clinical decisions are complex Think about what won’t change Most discussions don’t begin with a consent point of view Law is permissive - allows donation to proceed does not mandate that it must
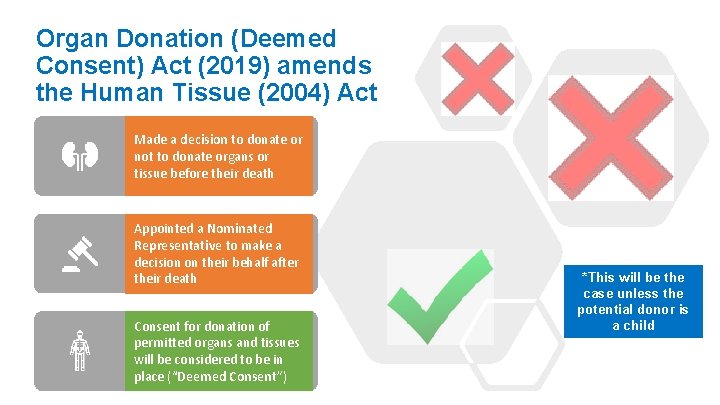
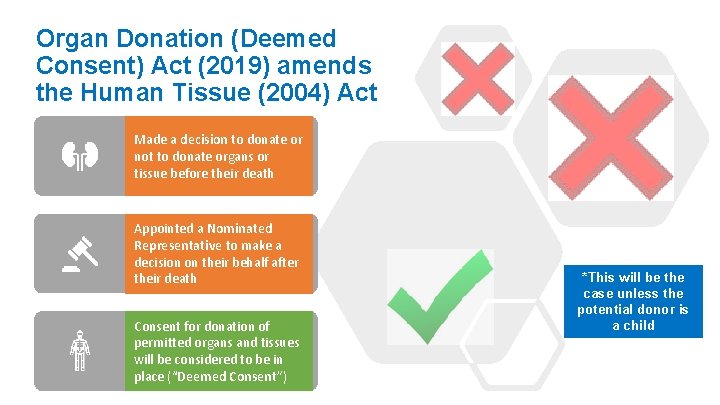
Organ Donation (Deemed Consent) Act (2019) amends the Human Tissue (2004) Act Made a decision to donate or not to donate organs or tissue before their death Appointed a Nominated Representative to make a decision on their behalf after their death Consent for donation of permitted organs and tissues will be considered to be in place (“Deemed Consent”) *This will be the case unless the potential donor is a child
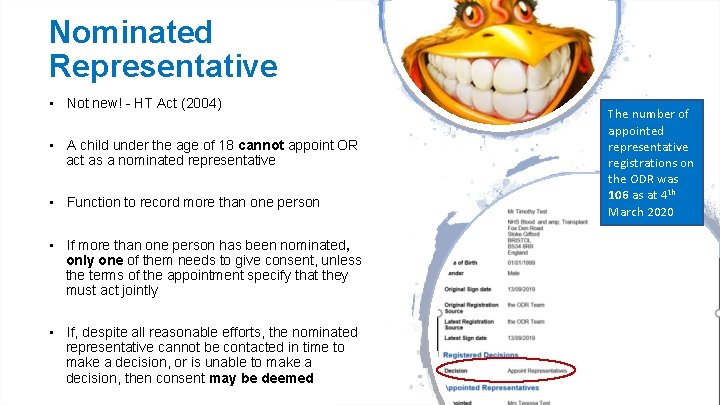
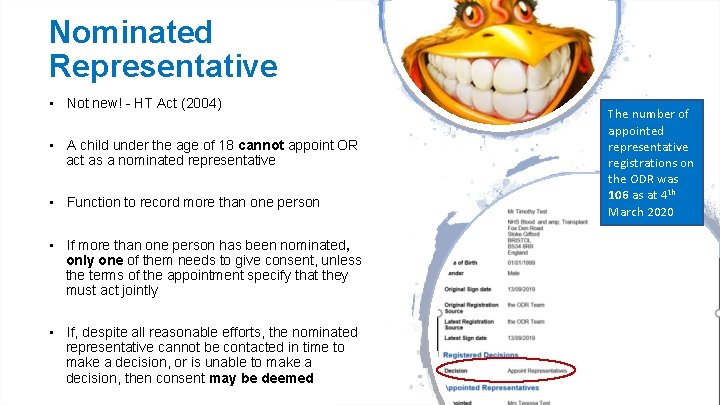
Nominated Representative • Not new! - HT Act (2004) • A child under the age of 18 cannot appoint OR act as a nominated representative • Function to record more than one person • If more than one person has been nominated, only one of them needs to give consent, unless the terms of the appointment specify that they must act jointly • If, despite all reasonable efforts, the nominated representative cannot be contacted in time to make a decision, or is unable to make a decision, then consent may be deemed The number of appointed representative registrations on the ODR was 106 as at 4 th March 2020
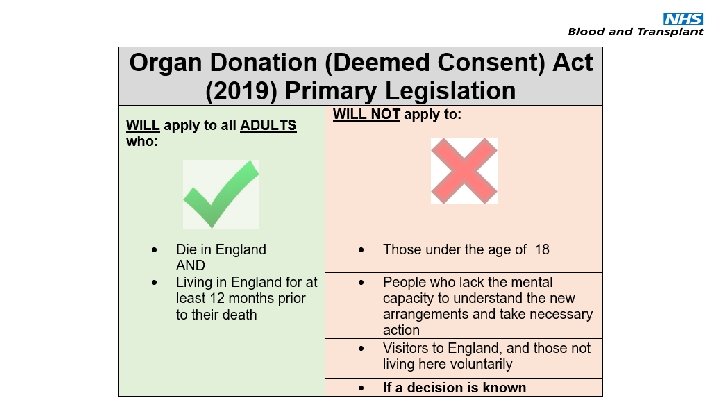
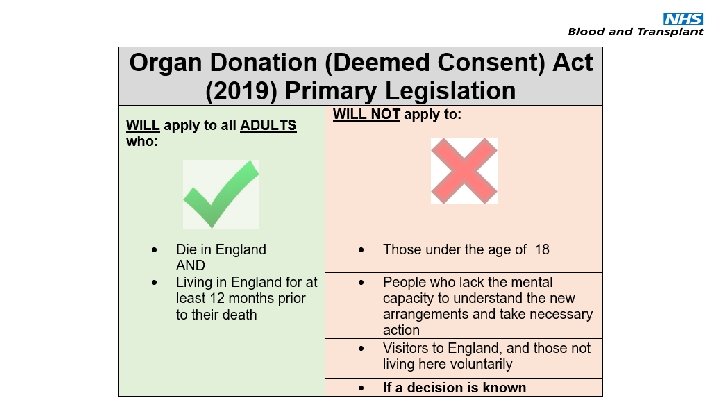
Safeguards: Excepted Adult • An adult who had not been ordinarily resident in England for a period of at least 12 months immediately before dying; • An adult who lacked the capacity to understand the notion of deemed consent for a significant period before their death.

Ordinarily Resident • Ordinarily resident refers to people living in England on a lawful, voluntary and properly settled basis • Ordinary residence can be of long or short duration • E. g. Overseas workers, students, overseas Armed Forces personnel • *Deemed consent will not apply unless someone has been ordinarily resident in England for at least 12 months immediately before dying
Students • Education can have the quality of a settled purpose • Students could be considered ordinarily resident as soon as they begin studying • Consent could only be deemed if they are 18 years old and have been ordinarily resident for 12 months in England immediately before dying
Armed Forces • Ordinarily resident refers to people living in England on a lawful, voluntary and properly settled basis • This may, or may not, apply to armed forces personnel depending on where they regarded as home • Armed forces personnel are therefore not automatically excepted on voluntarily grounds in England • Spouses or family members of armed forces personnel are generally considered ordinarily resident in England if they choose to join them *In practice, it would be for the Specialist Nurse to establish whether the person was ordinarily resident on a case-by-case basis
Those Seeking Asylum • Consent cannot be deemed for those seeking asylum.

People in prison cannot have their consent to organ and tissue donation deemed A person who is in prison cannot be considered to be residing in England voluntarily and Cannot therefore be considered ordinarily resident in England during their time in prison Prisoners

Safeguard • If in doubt whether ordinarily resident status applies - do not deem consent
Mental Capacity • The potential donor will be an excepted adult only if they lacked capacity to understand that consent could be deemed for a significant period prior to their death. • HT Act defines significant period’ as a sufficiently long period as to lead a reasonable person to conclude that it would be inappropriate for consent to be deemed. • In practice, a ‘significant period’ should mean that the potential donor did not have capacity to understand that consent could be deemed for a period of twelve months immediately before their death. • The lack of capacity to understand that consent can be deemed for a significant period only negates deemed consent. If the potential donor had made an expressed decision to consent, or not to consent, while they had capacity to make that decision then that decision remains valid regardless of a subsequent loss of capacity.
Independent Mental Capacity Advocates (IMCA) Not lawfully entitled to give or refuse consent for organ and tissue donation • Act as safeguards for people who lack capacity- where it is not possible for them to be represented by family or friends • May be involved in decisions up to the point of death-but not beyond it • Can only act for individuals aged 16 and over • If IMCA appointed (and in place prior to death) this is likely to indicate that they were an excepted person who lacked the capacity to understand the notion of deemed consent for a significant period before their death.
Lasting Power of Attorney • A Lasting Power of Attorney only remains valid during the lifetime of the person who made it. • After the person dies, the Lasting Power of Attorney will end.
Learning Disability • Assume capacity-unless evidence to the contrary • Discussion with family-seek the facts • Ascertain level of understanding • Mental capacity exclusion is there to ensure those who would not be able to understand the new legislation (regardless of a simple explanation) could not have their consent deemed
Safeguard • If in doubt whether the patient has mental capacity - do not deem consent

Operational Considerations This Photo by Unknown Author is licensed under CC BY-NC
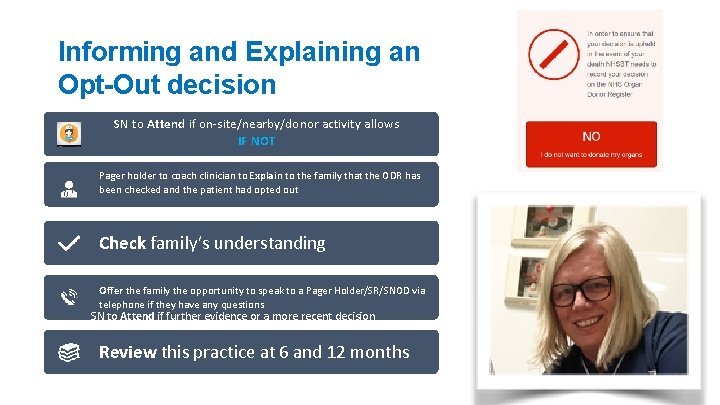
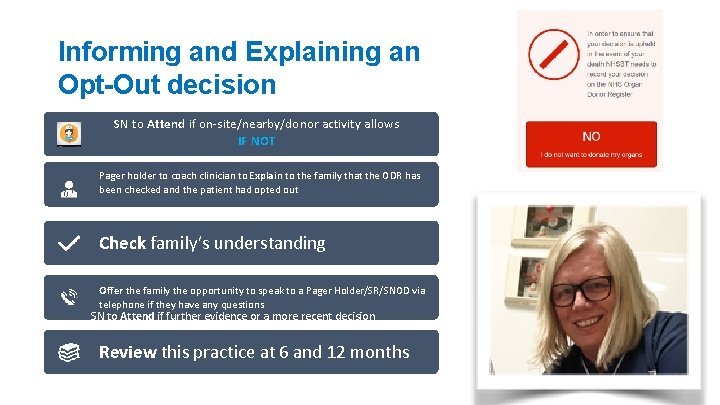
Informing and Explaining an Opt-Out decision SN to Attend if on-site/nearby/donor activity allows IF NOT Pager holder to coach clinician to Explain to the family that the ODR has been checked and the patient had opted out Check family’s understanding Offer the family the opportunity to speak to a Pager Holder/SR/SNOD via telephone if they have any questions SN to Attend if further evidence or a more recent decision Review this practice at 6 and 12 months
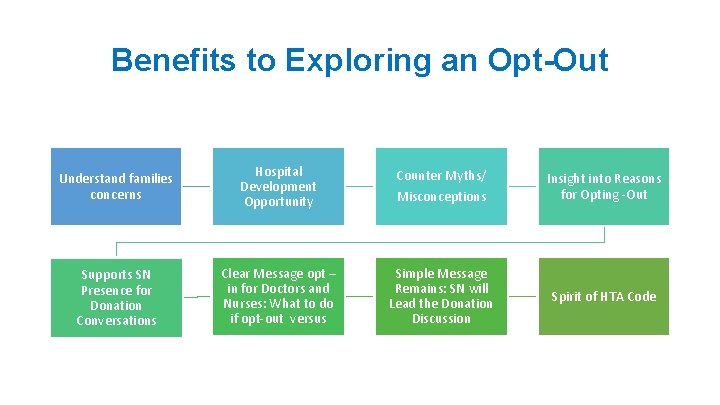
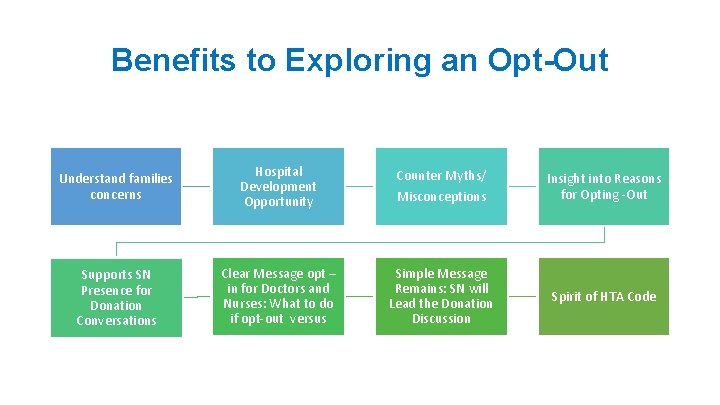
Benefits to Exploring an Opt-Out Understand families concerns Hospital Development Opportunity Counter Myths/ Misconceptions Insight into Reasons for Opting -Out Supports SN Presence for Donation Conversations Clear Message opt – in for Doctors and Nurses: What to do if opt-out versus Simple Message Remains: SN will Lead the Donation Discussion Spirit of HTA Code

Blood Samples Blood samples can only be taken in cases where expressed consent for donation has been given either by the: • Individual • Nominated/Appointed representative • Someone in a Qualifying Relationship (QR) OR Where consent has been deemed*: *Following discussion with someone in the QR
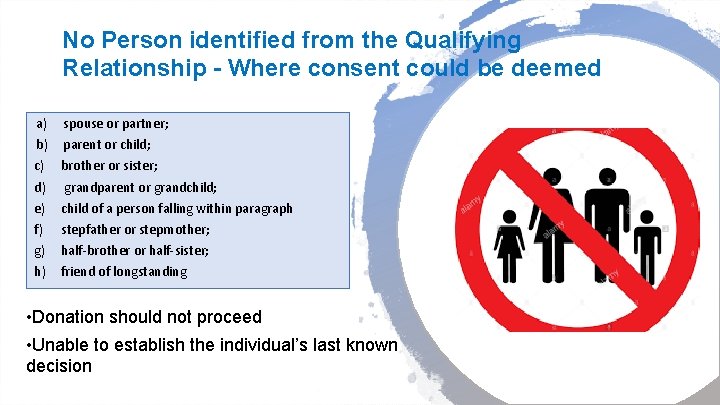
No Person identified from the Qualifying Relationship - Where consent could be deemed a) b) c) d) e) f) g) h) spouse or partner; parent or child; brother or sister; grandparent or grandchild; child of a person falling within paragraph stepfather or stepmother; half-brother or half-sister; friend of longstanding • Donation should not proceed • Unable to establish the individual’s last known decision
Faith and Beliefs • Declaration introduced in December 2018 • Providing reassurance about our processes • Humble approach – make no assumptions • Supported by revised faith pages on the website and faith specific organ donation cards “I would like NHS staff to speak to my family and anyone else appropriate about how Organ Donation can go ahead in line with my faith or beliefs”.
Thank You What Questions Do You Have?