Human Reproduction Structures Functions and Hormones Human reproduction

- Slides: 24
Human Reproduction: Structures, Functions, and Hormones Human reproduction differs from the mechanisms in lower vertebrates and many invertebrates. We depend on internal fertilization – sperm are deposited inside the female anatomy by copulation. Some invertebrates do the same thing, e. g. the queen bee in a hive receives sperm and stores it in a spermotheca, then uses it throughout the remainder of her life. Many lower vertebrates (fish, amphibians, …) have external fertilization – the female sheds eggs in to the environment and the male spews sperm over them.
Many simple invertebrates reproduce asexually, by budding off small pieces that grow into complete individuals, or by fission, in which the individual splits into two, and each half grows. Starfish regenerate lost arms, and if there is the tiniest piece of the central ring attached to the lost arm, it will regenerate a complete ‘new’ individual. Some animals (Daphnia, rotifers) shift between asexual and sexual reproduction, reproducing asexually during summer, but when conditions begin to deteriorate in fall, they produce a single, sexual generation (ephippia in Daphnia) that is resistant, dormant, and overwinters.
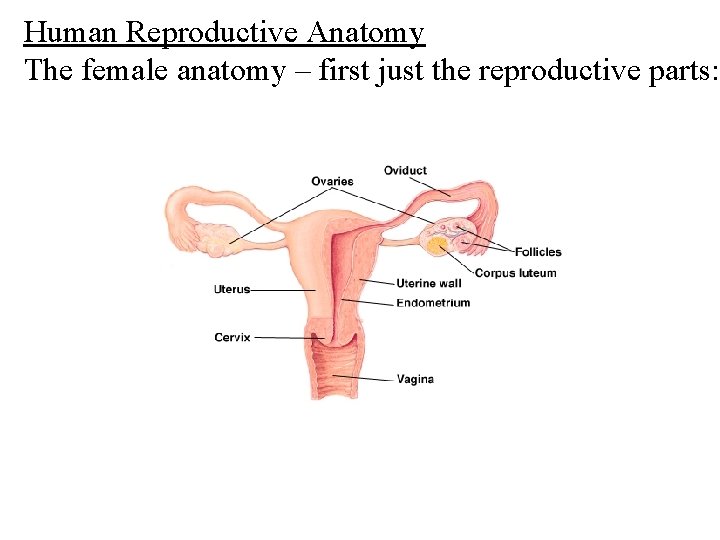
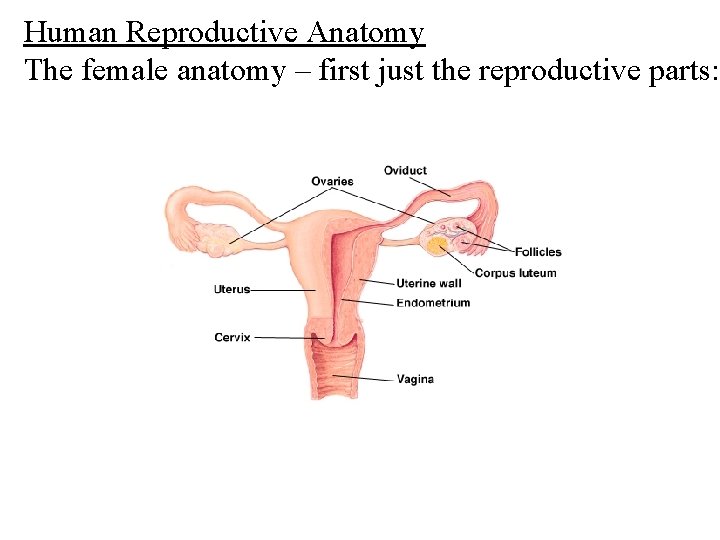
Human Reproductive Anatomy The female anatomy – first just the reproductive parts:
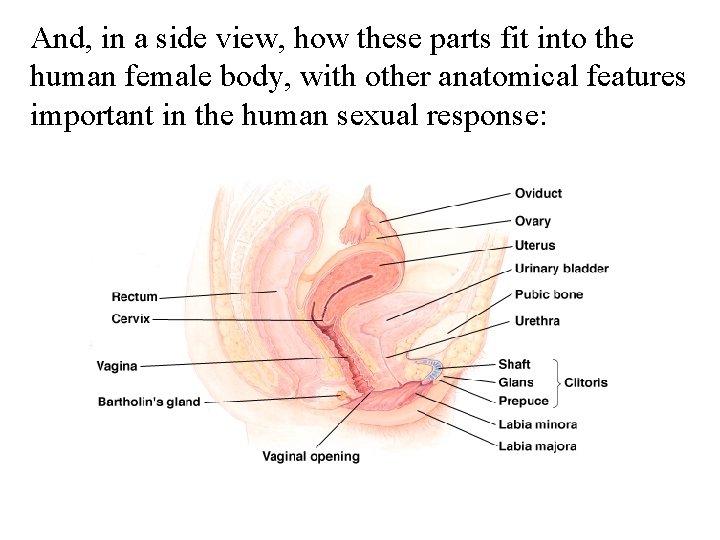
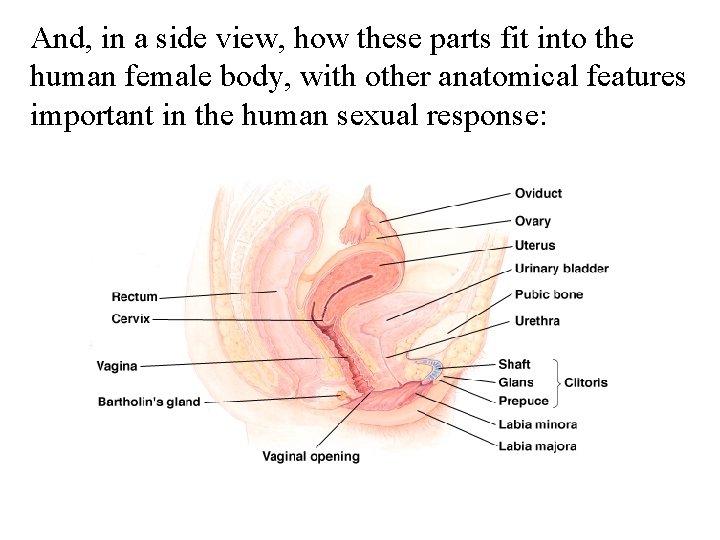
And, in a side view, how these parts fit into the human female body, with other anatomical features important in the human sexual response:
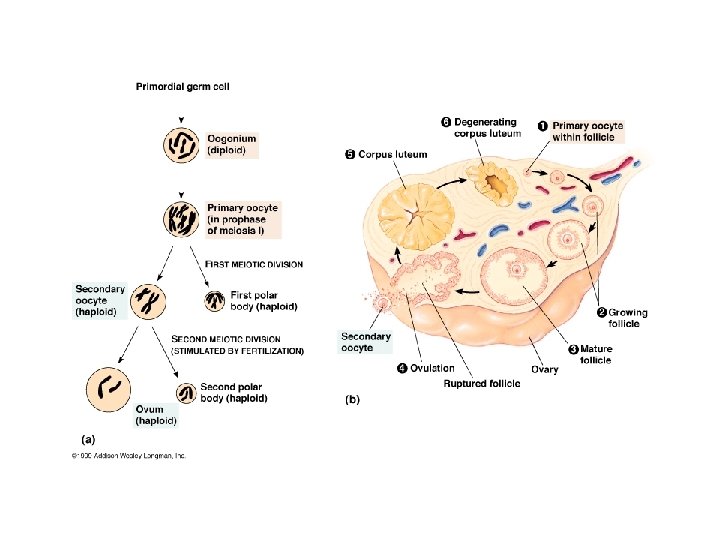
The ovary is the female gonad. In it oogonia (cells that will undergo meiosis) are randomly chosen (usually 1 per month) to undergo meiosis and develop into mature eggs. The ovary (about the size of an almond) has a bumpy surface. Each bump is a follicle, with one oocyte (a cell undergoing meiosis to become an egg) and a large number of nurse (follicle) cells. It is the follicle cells that are stimulated by FSH to produce estrogen. At ovulation (occurring with the stimulus of LH) the mature egg bursts from the follicle, and is drawn into the oviduct (Fallopian tube) by the beating of cilia in the fringed end of the tube.
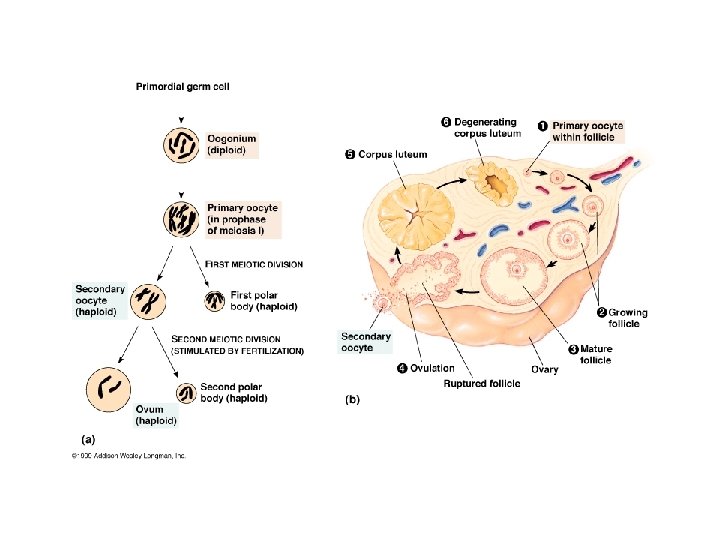
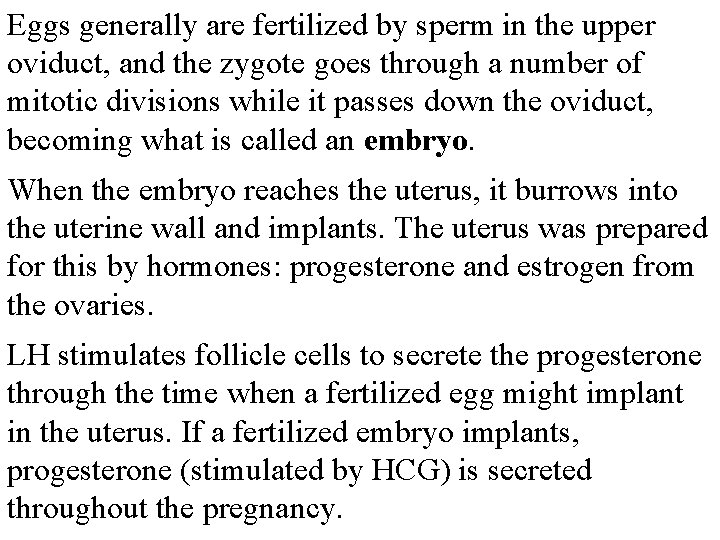
Eggs generally are fertilized by sperm in the upper oviduct, and the zygote goes through a number of mitotic divisions while it passes down the oviduct, becoming what is called an embryo. When the embryo reaches the uterus, it burrows into the uterine wall and implants. The uterus was prepared for this by hormones: progesterone and estrogen from the ovaries. LH stimulates follicle cells to secrete the progesterone through the time when a fertilized egg might implant in the uterus. If a fertilized embryo implants, progesterone (stimulated by HCG) is secreted throughout the pregnancy.
Since the ovary and fallopian tube are not joined, things can go wrong. The egg may not enter the oviduct. If so, it is broken down by phagocytes. A fertilized egg may not be drawn properly into or down the oviduct. If so, it will implant in the oviduct, or even in the body wall. This is called an ectopic pregnancy, and has to be fixed by surgery. Delay in passage and decrease in ovarian hormones, leading to change in the uterine wall, can lead to failure to implant or weak implantation. This is one possible reason for later miscarriage.
I seriously doubt the need to explain the female anatomy. If you don’t know where the labia majora and labia minora, the clitoris (and particularly the glans and prepuce), the vagina, and the cervix are, the diagram will help you learn about them. There are two things you may not know about: both the walls of the vagina and Bartholin’s gland secrete lubricants during sexual arousal. Without them, intercourse would not be the same: enjoyment would decrease and pain increase.
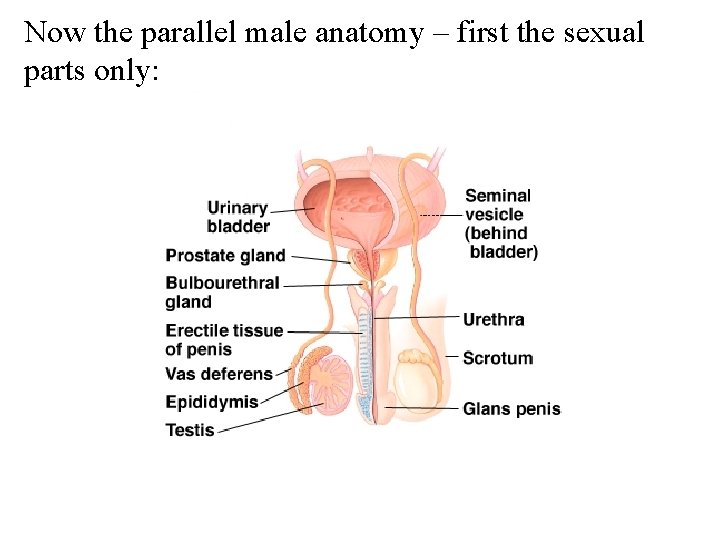
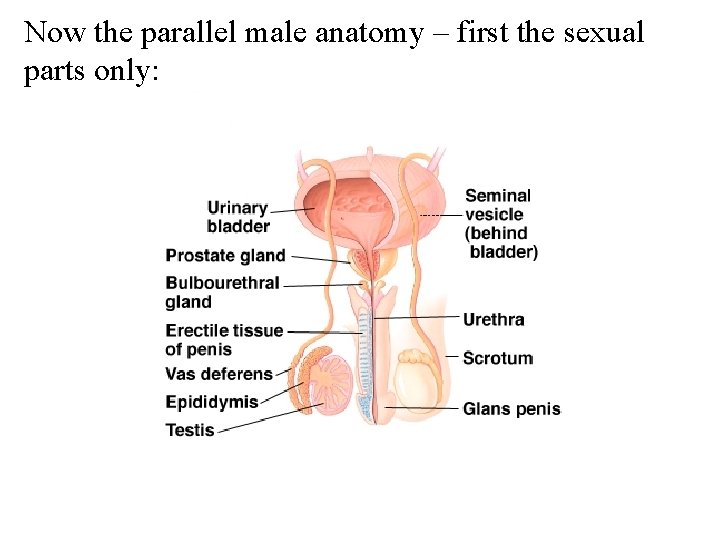
Now the parallel male anatomy – first the sexual parts only:
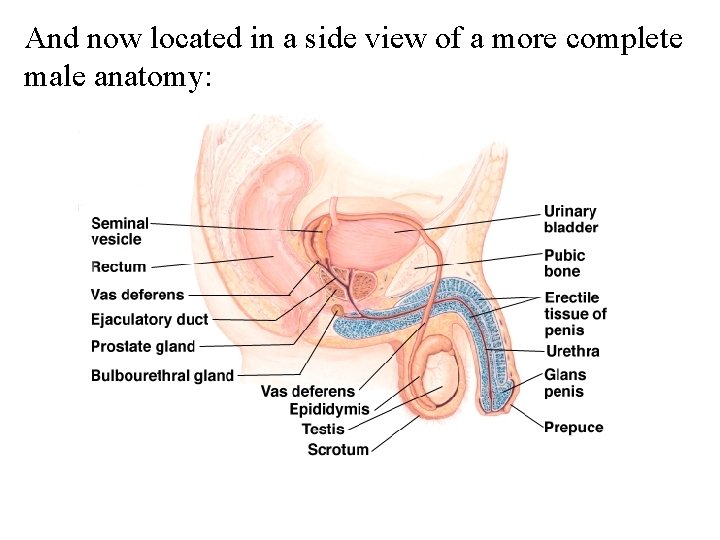
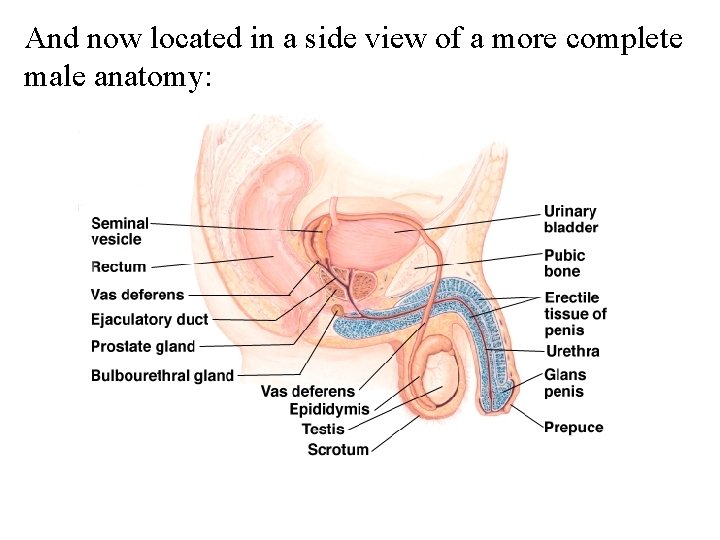
And now located in a side view of a more complete male anatomy:
Once more the basics of the male anatomy should be familiar. The testes, within the scrotum, both respond to and manufacture hormones. FSH from the anterior pituitary stimulates spermatocytes in the seminiferous tubules to undergo meiosis and maturation to become active sperm. LH from the anterior pituitary stimulates interstitial cells, clusters of cells wedged in among the seminiferous tubules, to produce and secrete androgens (male hormones), particularly testosterone.

Sperm that are nearly mature at the center (the lumen) of seminiferous tubules. They are collected from individual tubules into the epididymus, where they complete maturation. Passage takes about 20 days. They are pushed from the epididymus into the vas deferens, which is the duct carrying them to the rear end of the penis, at the time of ejaculation. Before entering the penis to be ejaculated, three other sets of glands contribute fluids to what will be semen.
The seminal vesicles secrete a fluid that contains vitamins and fructose to nourish sperm. The fluid also contains prostaglandins, hormones that are believed to cause contractions in the female reproductive tract to help get sperm to their ‘target’. The bulbourethral glands (sometimes called Cowper’s gland) secrete a lubricant. The prostate gland makes a neutralizing fluid that helps protect sperm from any residual urine in the male tract and potential problems with p. H in the female tract.
Ejaculation is a carefully controlled event. It occurs in at least two steps: 1) as sexual arousal peaks, muscles in the epididymus, seminal vesicles, vas deferens, and prostate all contract. As well, two sphincters associated with the prostate contract. One blocks passage of urine into the urethra. The other, further ‘downstream’, blocks flow off semen. 2) In phase 2 the second sphincter relaxes, and muscular contractions in the base of the penis moves the semen through the urethra and ejects it. Packing semen tightly between the sphincters then propelling it makes forceful ejaculation.
The male penis is erectile (as if this is a necessary bit of information), and so are the female labia (majora and minora), clitoris, and, in case you aren’t aware, also the lips and parts of the nose in both sexes. The most densely innervated and sensitive parts in both males and females are their respective glans and prepuces. In males, the prepuce is frequently surgically removed (called circumcision).
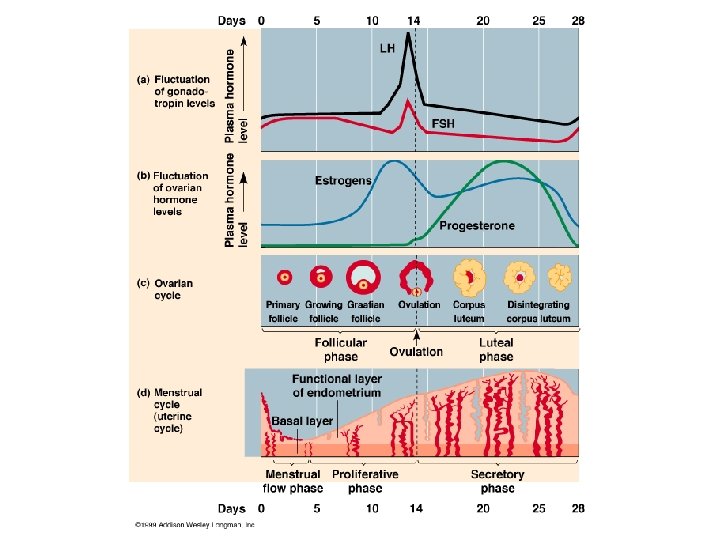
Sex hormones in males are regulated, but do not go through monthly cycles. Sex hormones and tissues in females go through monthly cycles. Those cycles affect the ovaries, the uterus, and also the mammary glands. The repeated cycles of cell division in the female breast milk gland tissue is the probable reason why female breast cancer is much more common than cancer of the male breast. Female sex hormone and tissue cycles are usually thought by students to be complicated, so here is the diagram from your text:
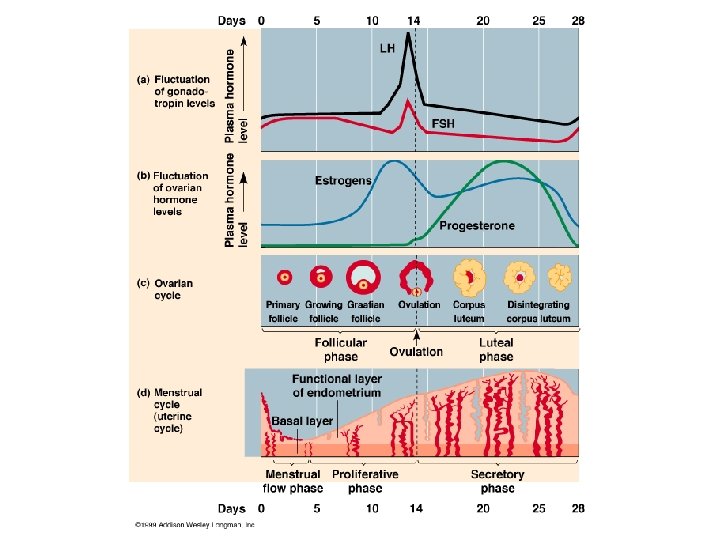
There a number of stimuli and responses evident in the previous diagram: 1) Anterior pituitary hormones FSH and LH are involved in a feedback relationship with estrogen and progesterone. FSH stimulates the initiation of the monthly cycle; the burst of FSH and LH at ovulation is stimulated by high levels of estrogen (while progesterone is low). 2) In the ovary, the cycle begins with FSH stimulation. As the follicle matures, follicle cells make more and more estrogen. After ovulation, the follicle cells become the corpus luteum, which produces progesterone.
3) The corpus luteum continues progesterone production for ~ 2 weeks, after which, without other stimulus, it degenerates. 4) In the uterus, the cycle begins at a phase when estrogen and progesterone titres are low. That leads to a cut-off of blood flow to the endometrium, and the sloughing of the previously thickened tissue – menstrual flow. After menstruation, the estrogen from the ovary stimulates proliferation of endometrial tissue – thickening once more occurs. Progesterone causes the thickened endometrium to enter the secretory phase
5) The high levels of estrogen and progesterone during the post-ovulatory phase, through negative feedback, cause the hypothalamus and anterior pituitary to basically shut down FSH and LH production. Development of a new follicle does not occur until degeneration of the corpus luteum (and a stop to production of estrogen and progesterone) leads to a renewed production of FSH. 6) If an embryo implants in the uterine wall, it begins rapidly making HCG (human chorionic gonadotropin), which replaces progesterone in maintaining the corpus luteum.
It’s HCG, detected in human urine, that is the evidence of pregnancy. Test kits are now very sensitive, using monoclonal antibodies to respond to and indicate the presence of HCG.
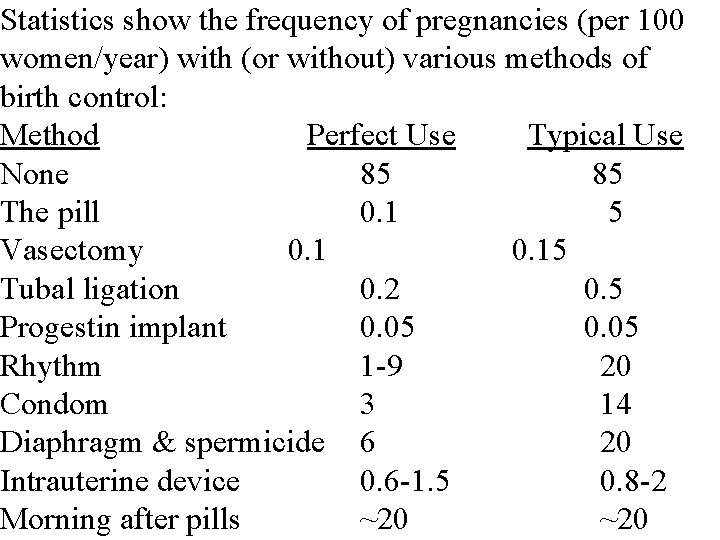
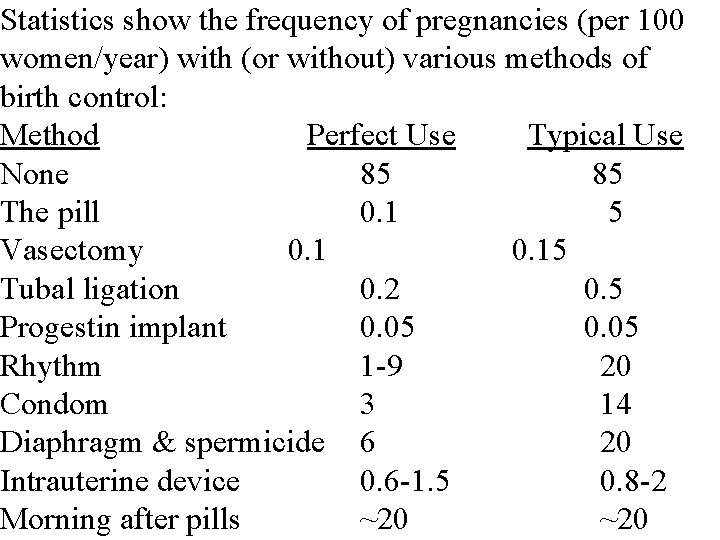
Statistics show the frequency of pregnancies (per 100 women/year) with (or without) various methods of birth control: Method Perfect Use Typical Use None 85 85 The pill 0. 1 5 Vasectomy 0. 15 Tubal ligation 0. 2 0. 5 Progestin implant 0. 05 Rhythm 1 -9 20 Condom 3 14 Diaphragm & spermicide 6 20 Intrauterine device 0. 6 -1. 5 0. 8 -2 Morning after pills ~20