Human Reproduction 1 The Male Reproductive System The
![The female reproductive organs: [internal] • 1. vagina – Birth canal – Made up The female reproductive organs: [internal] • 1. vagina – Birth canal – Made up](https://slidetodoc.com/presentation_image_h/24cd1a67c6a001468e717cafa9e7447a/image-28.jpg)
![The female reproductive organs: [external] • • • 1. mons pubis 2. labia major The female reproductive organs: [external] • • • 1. mons pubis 2. labia major](https://slidetodoc.com/presentation_image_h/24cd1a67c6a001468e717cafa9e7447a/image-35.jpg)
![• The 2 main hormones folliclestimulating hormone[FSH] and luteinizing hormone[LH] are secreted from • The 2 main hormones folliclestimulating hormone[FSH] and luteinizing hormone[LH] are secreted from](https://slidetodoc.com/presentation_image_h/24cd1a67c6a001468e717cafa9e7447a/image-38.jpg)
![What is PMS? • Premenstrual syndrome[PMS] refers to a variety of symptoms that women What is PMS? • Premenstrual syndrome[PMS] refers to a variety of symptoms that women](https://slidetodoc.com/presentation_image_h/24cd1a67c6a001468e717cafa9e7447a/image-57.jpg)
- Slides: 63
Human Reproduction 1
The Male Reproductive System • The male reproductive system has 2 main functions: – 1. Produces the male gametes[sperm] – 2. secretes the sex hormone testosterone 2
• The formation of sperm cells is called spermatogenesis • Sperm cells are highly specialized cells that are able to move 3
• the formation of sperm requires a temperature that is 2 to 4 degrees cooler than the body 4
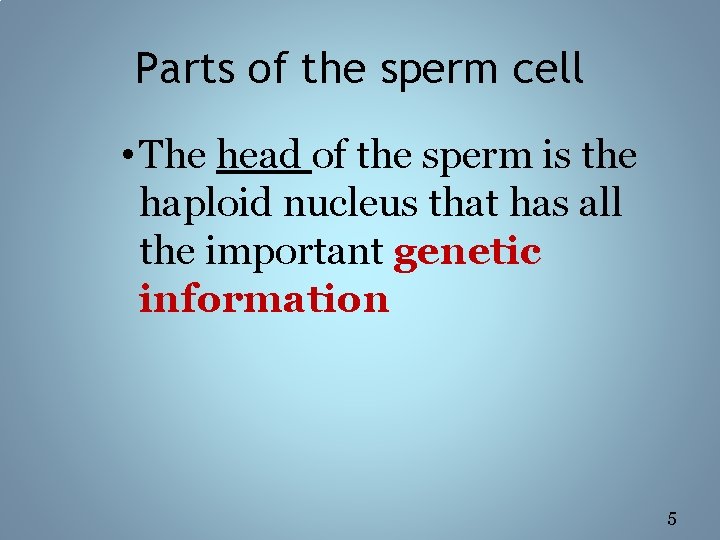
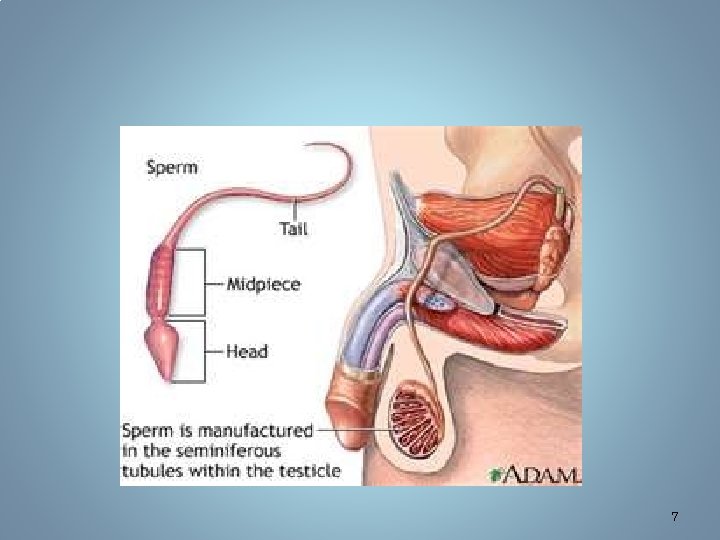
Parts of the sperm cell • The head of the sperm is the haploid nucleus that has all the important genetic information 5
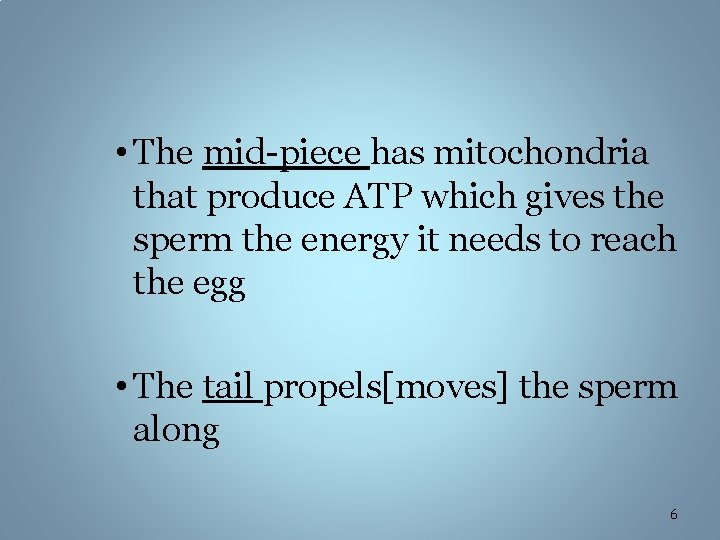
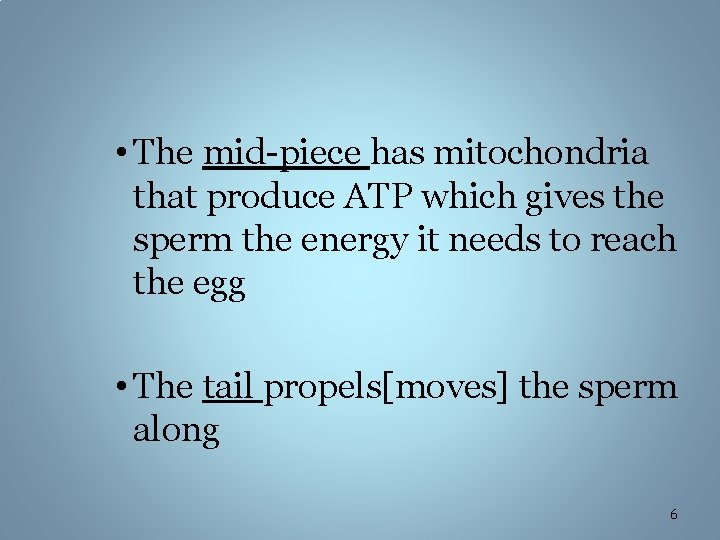
• The mid-piece has mitochondria that produce ATP which gives the sperm the energy it needs to reach the egg • The tail propels[moves] the sperm along 6
7
8
9
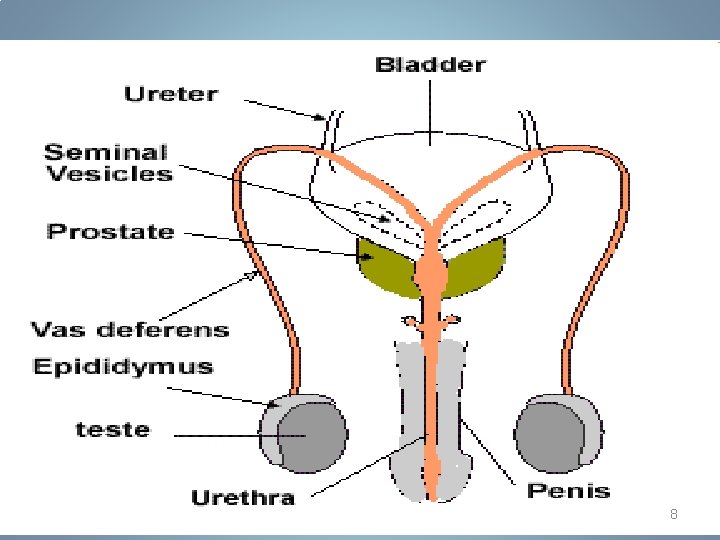
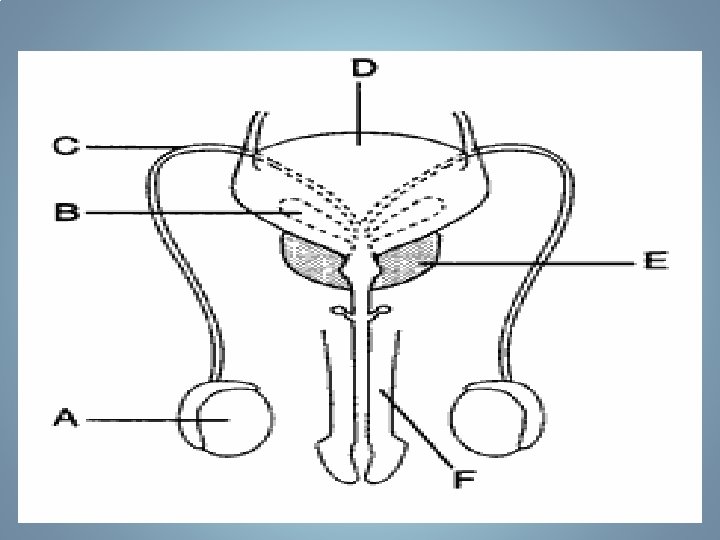
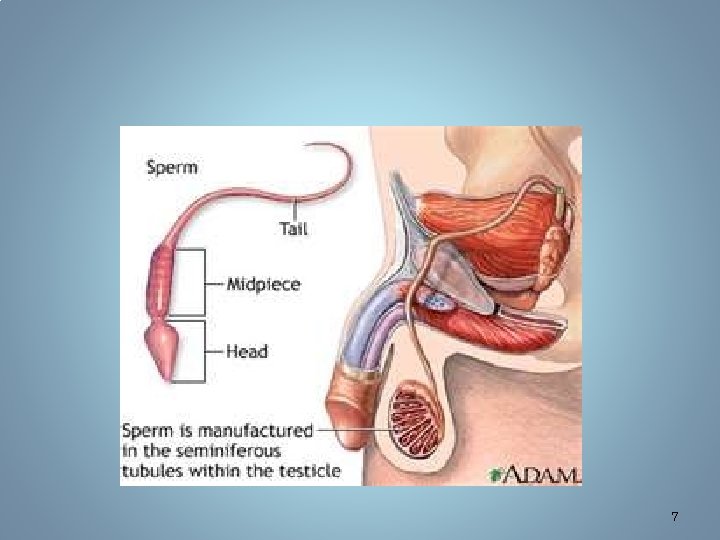
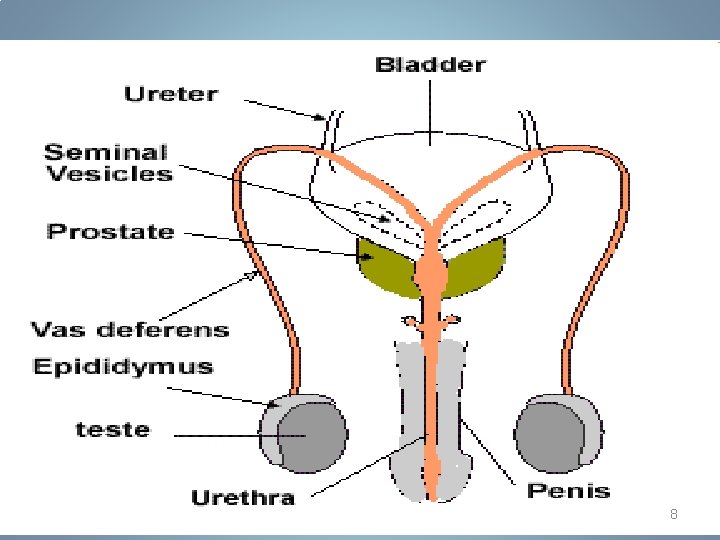
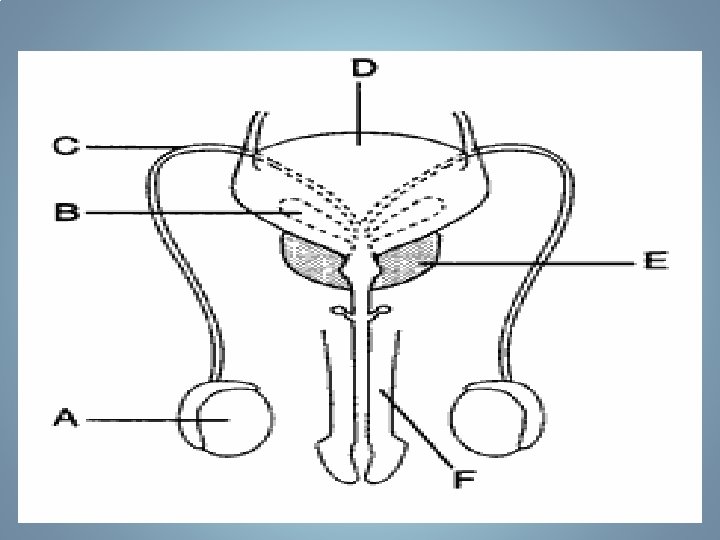
Parts of the male reproductive tract 1. Testes: • -located in the scrotum • -it’s where the production of sperm occurs 10
• -inside the testes are many tiny tubes called seminiferous tubules • - normal diploid cells move through these tubes while they undergo meiotic cell division 11
• 2. scrotum: – the sac that holds the testes – An adaptation of the male reproductive system that provides a lower temperature for the development of sperm cells is the scrotum 12
• 3. Epididymis: – this is where the sperms “live” and complete their development into mature sperm cells 13
4. vas deferens • -this is the beginning of the pathway for the sperm to exit out • - as the sperm moves through the vas deferens, it stops at 3 accessory sex glands to add fluids: 14
The 3 accessory sex glands • 1. Seminal vesicle – A pouch-like gland that secretes fluid that’s rich in fructose – Helps provide a source of energy for the sperm 15
• secretes prostaglandins[these are chemicals that cause contractions to help move the sperm toward the egg] 16
• 2. Prostate gland: • Secretes an anticoagulant enzyme called Prostate Specific Antigen (PSA) • PSA aids in the success of sperm by liquefying semen that has thickened after ejaculation. • This thinning action allows sperm to swim more freely 17
• 3. Cowper’s glands: – secretes alkaline PH; this neutralizes the acid in the male’s urethra and in the female reproductive system that might damage the sperm 18
• -sperm + fluids from the _______, ______ and the _____ is what makes up the semen 19
5. urethra • - tube that passes through the penis • - it’s a passage way for sperm and urine 20
6. penis • -a structure that has evolved to deposit sperm safely within the FEMALE’S body 21
• What causes an erection? • nerves in the brain send chemical messages to nerves in the penis telling the penile blood vessels to relax so that blood can flow freely into the penis. • This causes the penis to expand sustain an erection. 22
• Define ejaculation: the excretion of semen out of the penis 23
The female reproductive system • The female reproductive system has 3 important functions: – 1. oogenesis the production of ova – 2. provides a temporary “home” for the developing embryo – 3. produces estrogen and progesterone 24
• How do females produce their egg cells and at what age does this occur? 25
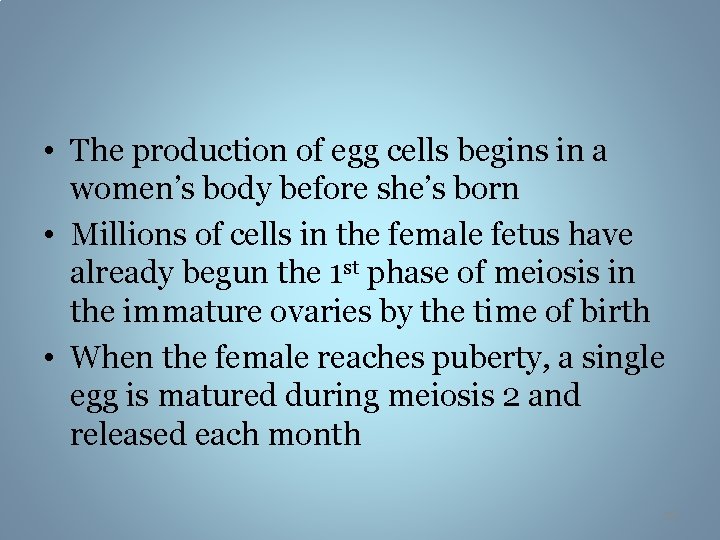
• The production of egg cells begins in a women’s body before she’s born • Millions of cells in the female fetus have already begun the 1 st phase of meiosis in the immature ovaries by the time of birth • When the female reaches puberty, a single egg is matured during meiosis 2 and released each month 26
27
![The female reproductive organs internal 1 vagina Birth canal Made up The female reproductive organs: [internal] • 1. vagina – Birth canal – Made up](https://slidetodoc.com/presentation_image_h/24cd1a67c6a001468e717cafa9e7447a/image-28.jpg)
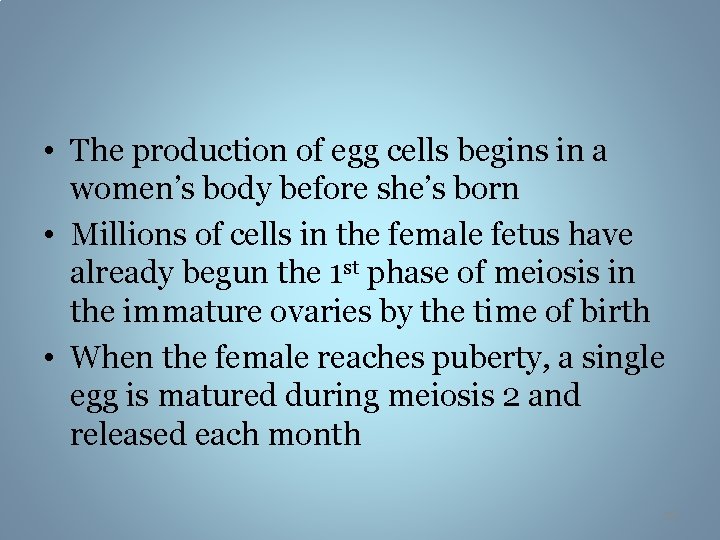
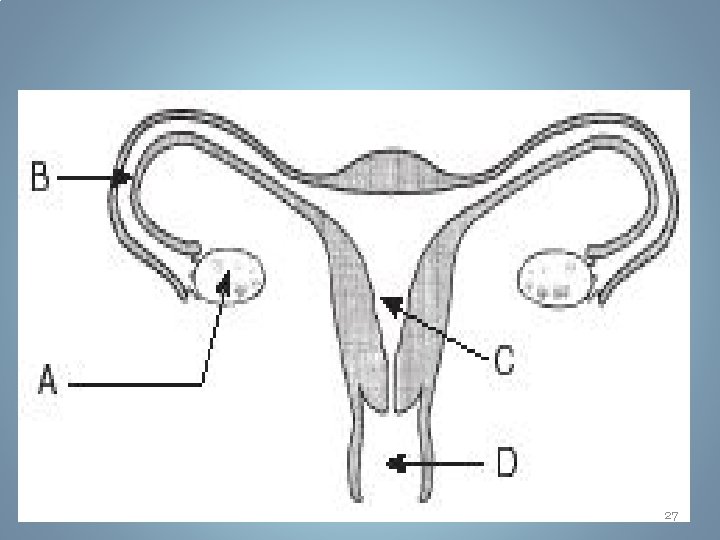
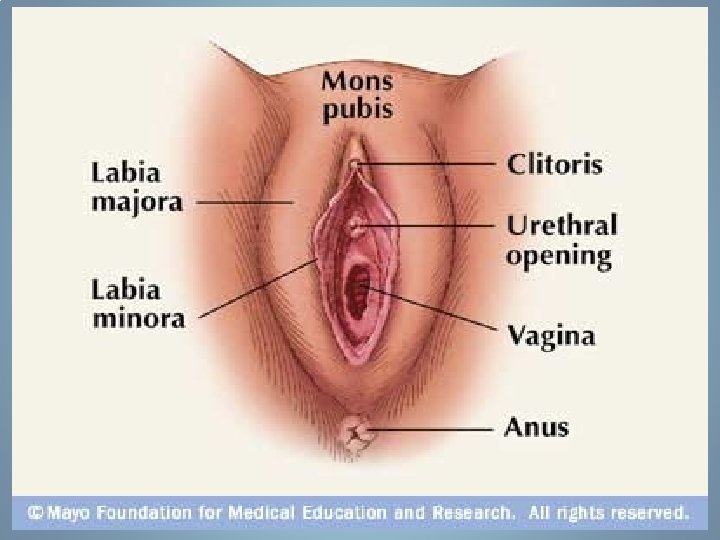
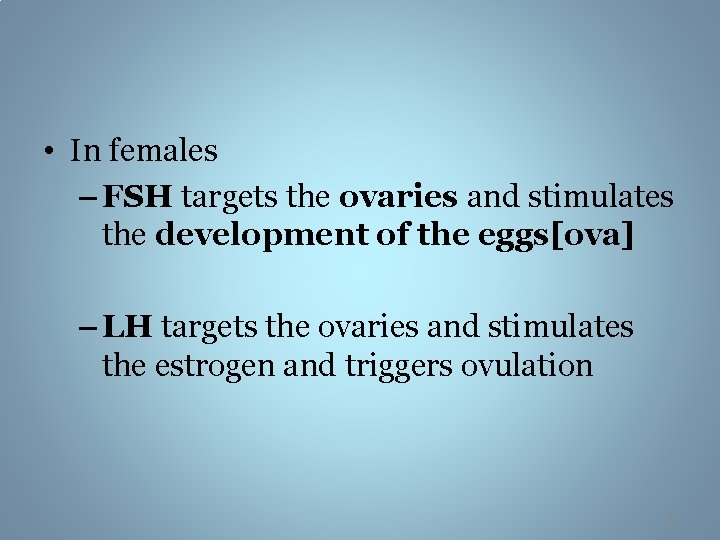
The female reproductive organs: [internal] • 1. vagina – Birth canal – Made up of muscular tissue – Has elasticity – About 10 centimeters long 28
• 2. cervix – A narrow opening at the lower end of the uterus 29
• 3. uterus – a pear-shaped organ with thick muscular walls –Houses a developing fetus for 40 weeks 30
• Contracts during labor and childbirth –Where menstruation occurs 31
• 4. fallopian tubes 2 pair – Also called the oviducts or uterine tubes – A long tubular structure found next to each ovary – Egg travels through here during ovulation 32
–Fertilization occurs here –At the end of each tube are finger-like structures called fimbriae 33
• 5. ovary 2 pair –Houses the developing ova –Produces the female sex hormones 34
![The female reproductive organs external 1 mons pubis 2 labia major The female reproductive organs: [external] • • • 1. mons pubis 2. labia major](https://slidetodoc.com/presentation_image_h/24cd1a67c6a001468e717cafa9e7447a/image-35.jpg)
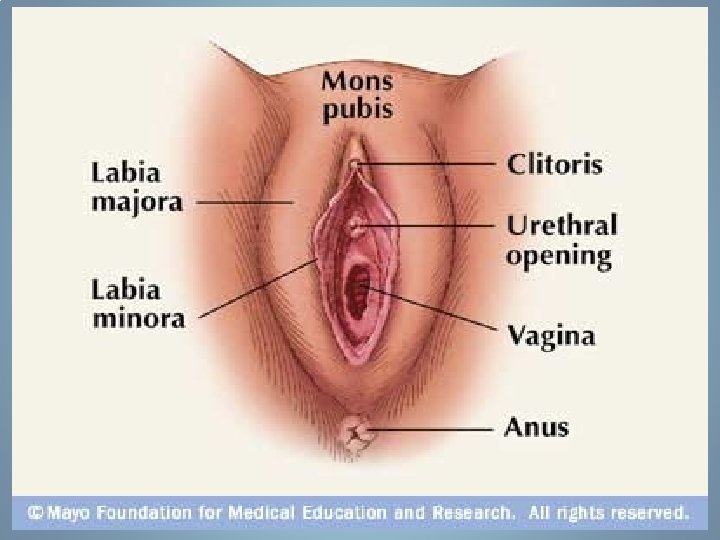
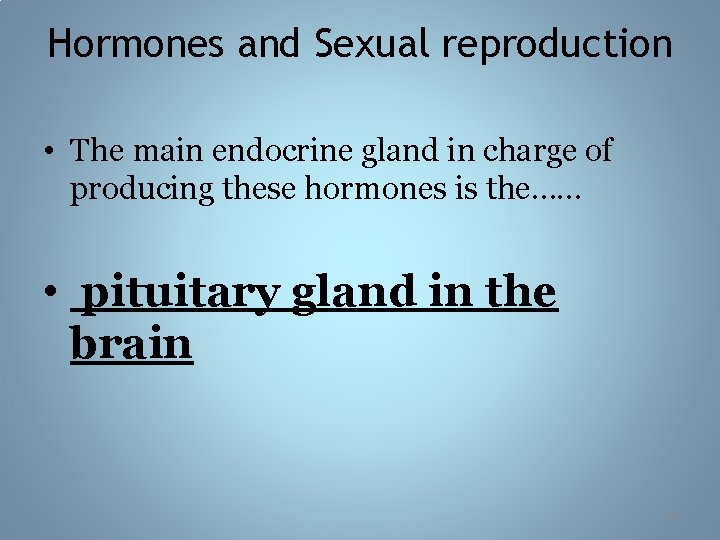
The female reproductive organs: [external] • • • 1. mons pubis 2. labia major 3. labia minor 4. clitoris 5. breast 35
36
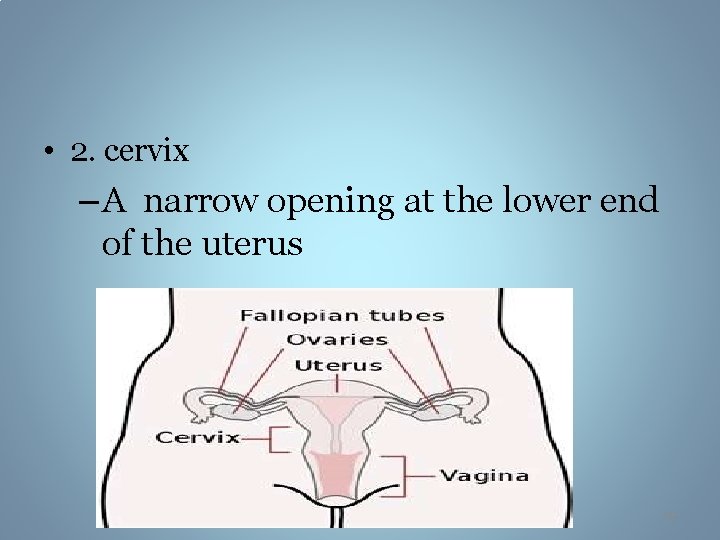
Hormones and Sexual reproduction • The main endocrine gland in charge of producing these hormones is the…… • pituitary gland in the brain 37
![The 2 main hormones folliclestimulating hormoneFSH and luteinizing hormoneLH are secreted from • The 2 main hormones folliclestimulating hormone[FSH] and luteinizing hormone[LH] are secreted from](https://slidetodoc.com/presentation_image_h/24cd1a67c6a001468e717cafa9e7447a/image-38.jpg)
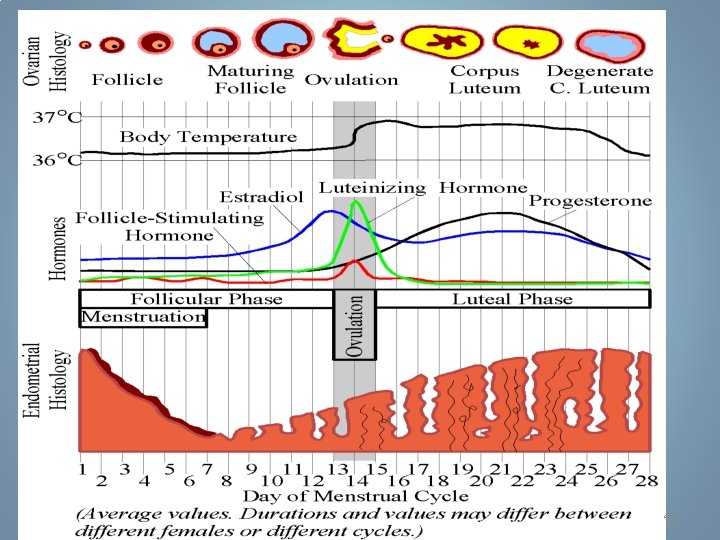
• The 2 main hormones folliclestimulating hormone[FSH] and luteinizing hormone[LH] are secreted from the anterior pituitary 38
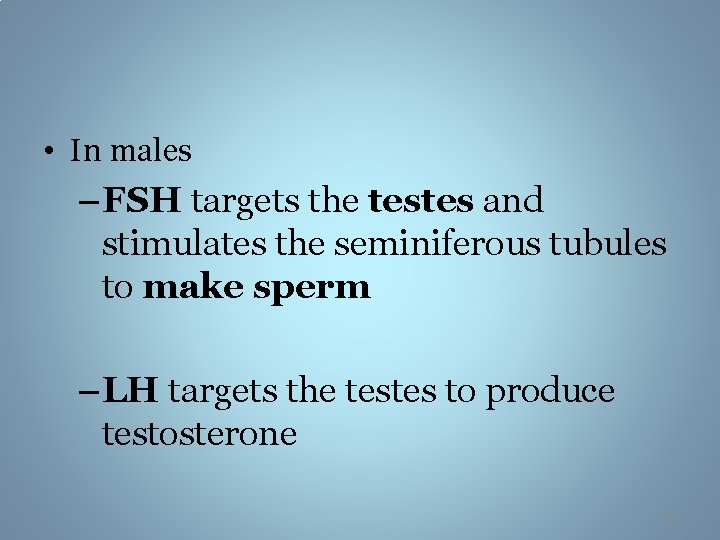
• In males – FSH targets the testes and stimulates the seminiferous tubules to make sperm – LH targets the testes to produce testosterone 39
• What is the function of testosterone? • It plays a role in determining the gender of developing fetuses • Secondary Sex Characteristics • It contributes to an active sexual drive in both men and women • increases the metabolic functions in men • It is necessary for sperm to mature 40
• In females – FSH targets the ovaries and stimulates the development of the eggs[ova] – LH targets the ovaries and stimulates the estrogen and triggers ovulation 41
What is the function of estrogen and progesterone? • secondary sex characteristics • Responsible for ovulation • Responsible for the menstrual cycle 42
43
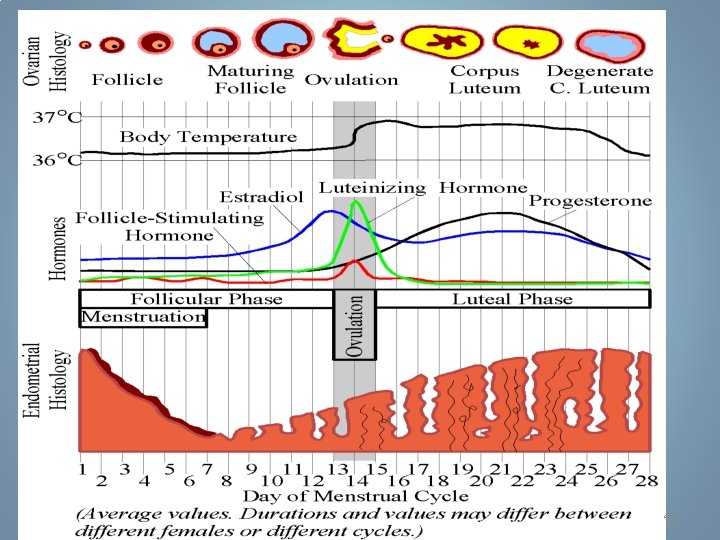
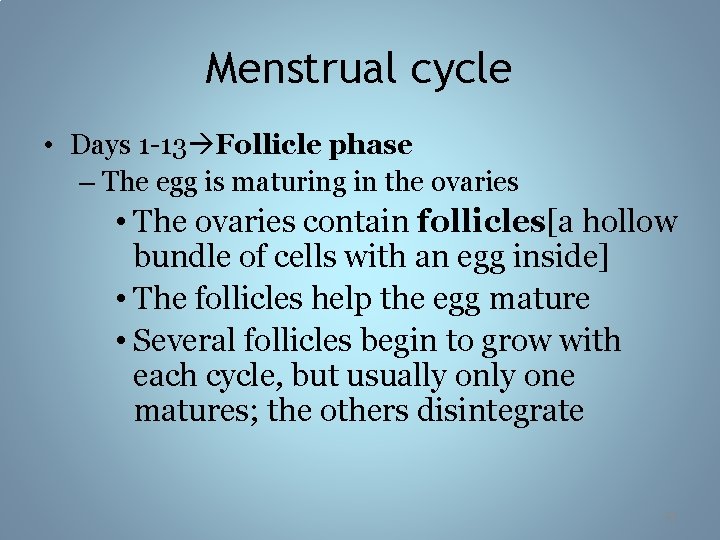
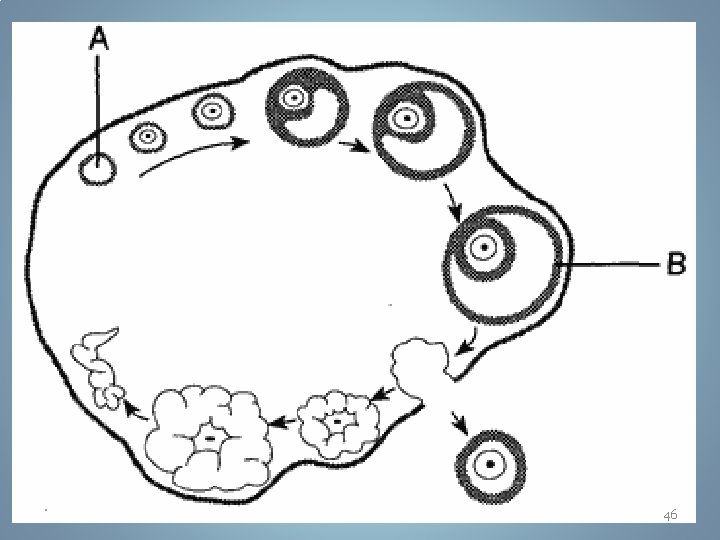
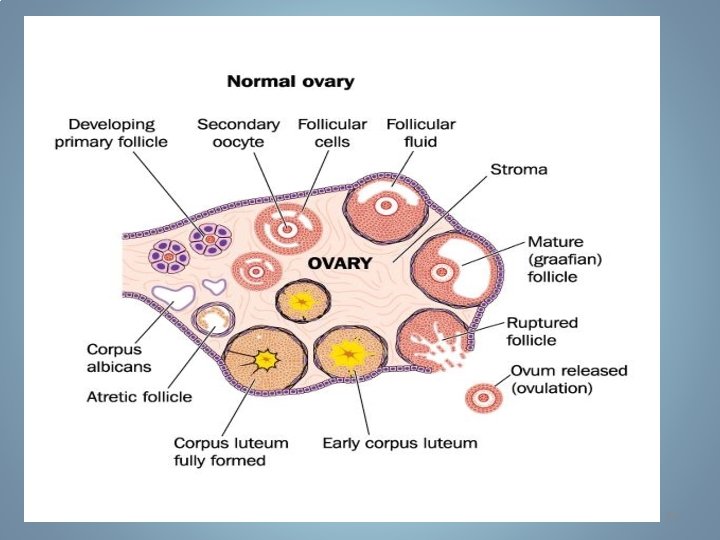
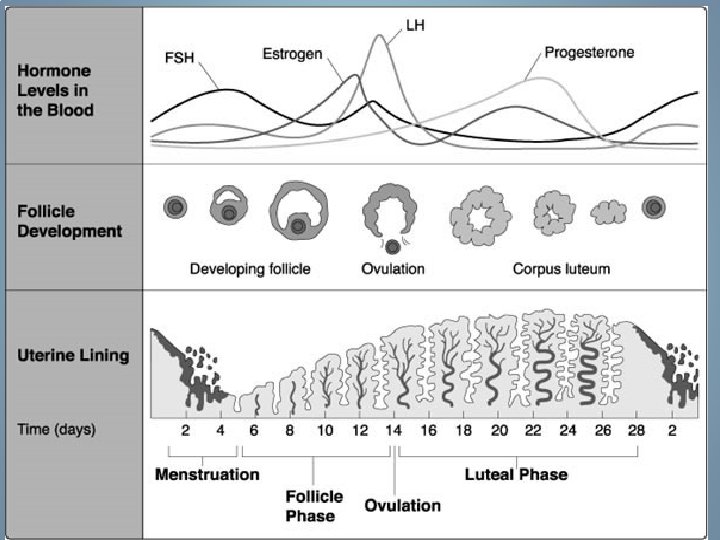
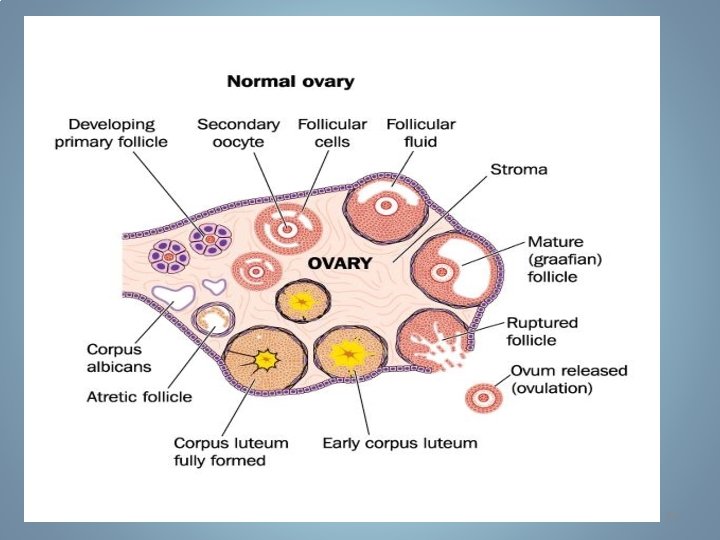
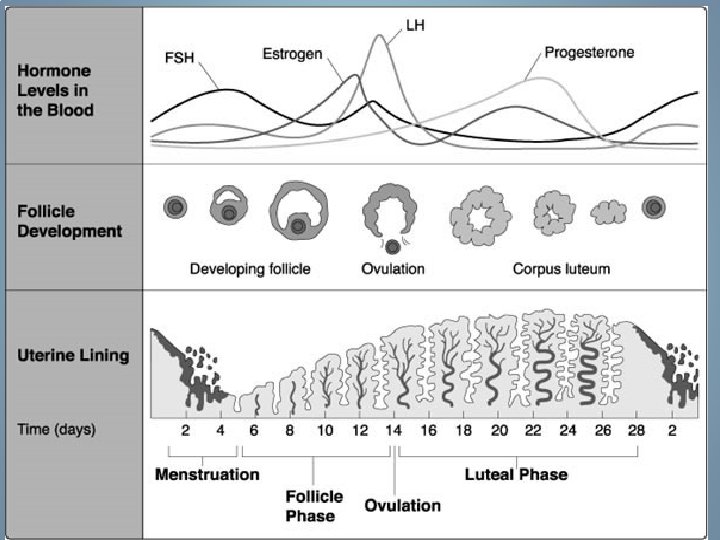
Menstrual cycle • Days 1 -13 Follicle phase – The egg is maturing in the ovaries • The ovaries contain follicles[a hollow bundle of cells with an egg inside] • The follicles help the egg mature • Several follicles begin to grow with each cycle, but usually one matures; the others disintegrate 44
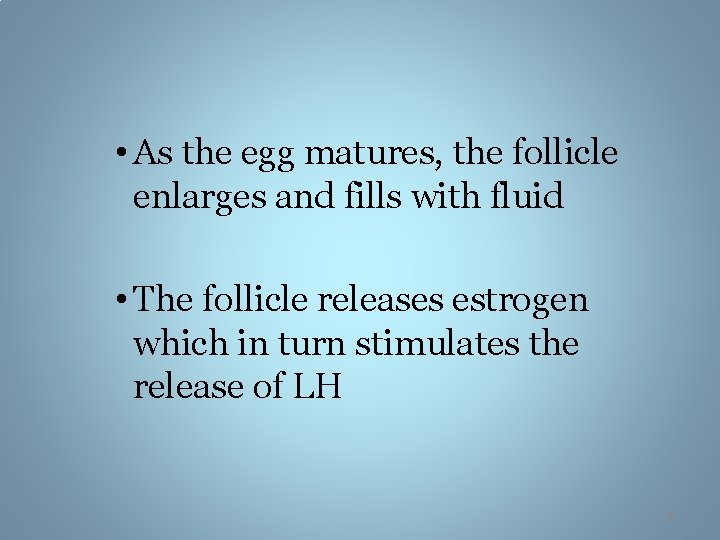
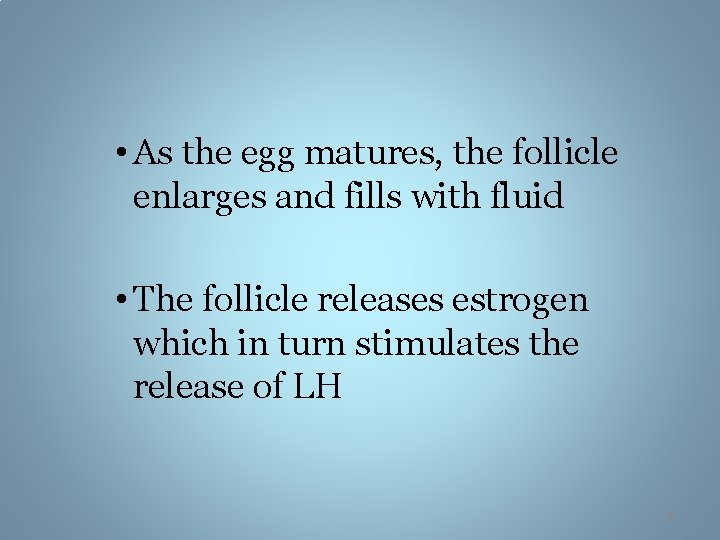
• As the egg matures, the follicle enlarges and fills with fluid • The follicle releases estrogen which in turn stimulates the release of LH 45
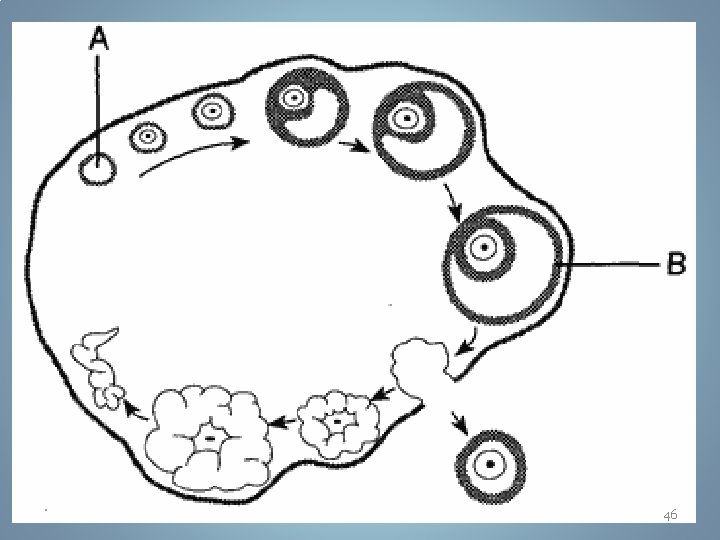
46
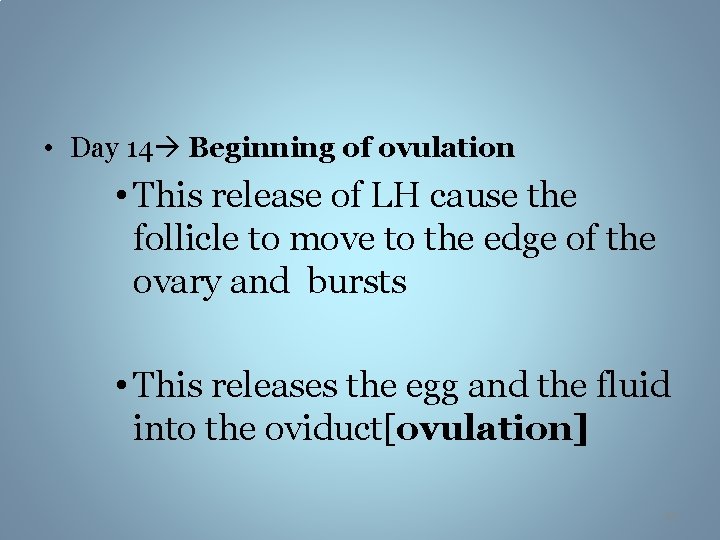
• Day 14 Beginning of ovulation • This release of LH cause the follicle to move to the edge of the ovary and bursts • This releases the egg and the fluid into the oviduct[ovulation] 47
• in addition, estrogen causes the lining of the uterus to thicken and there’s an increase in the amount of blood that flows to this area 48
• days 15 -20 corpus luteum phase • ovulation still occurring • after ovulation has occurred the follicle[now without an egg cell] develops into a yellow-colored body[corpus luteum] 49
• the corpus luteum begins to secrete progesterone and further thickens the lining of the uterus including enlargement of arteries and growth of endometrial glands • These glands secrete a nutrient fluid that can sustain an early embryo even before it implants in the uterine lining 50
51
• days 21 -28 menstruation • the level of LH decreases • the corpus luteum breaks down 52
• level of progesterone decreases • The uterine lining disintegrates, releasing blood that is shed along with endometrial tissue and fluid 53
54
55
56
![What is PMS Premenstrual syndromePMS refers to a variety of symptoms that women What is PMS? • Premenstrual syndrome[PMS] refers to a variety of symptoms that women](https://slidetodoc.com/presentation_image_h/24cd1a67c6a001468e717cafa9e7447a/image-57.jpg)
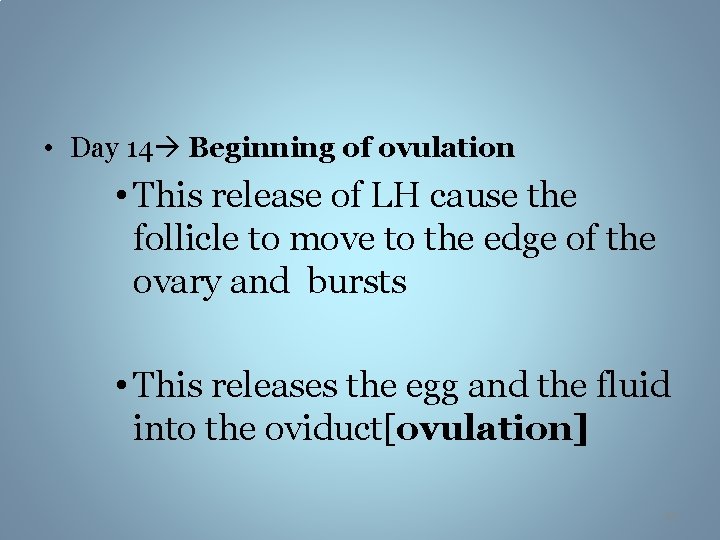
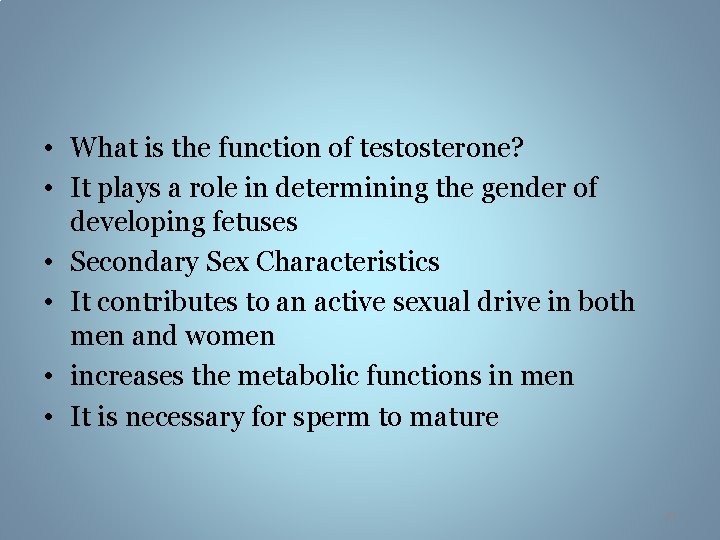
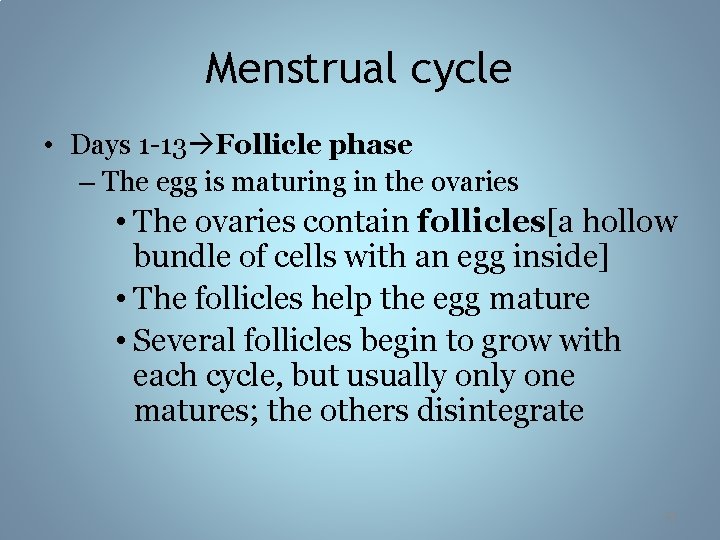
What is PMS? • Premenstrual syndrome[PMS] refers to a variety of symptoms that women can experience 1 -10 days BEFORE her period 57
What are the symptoms of PMS? 58
What causes PMS? • Changes in hormone levels • Poor diet • Stress • Lack of exercise 59
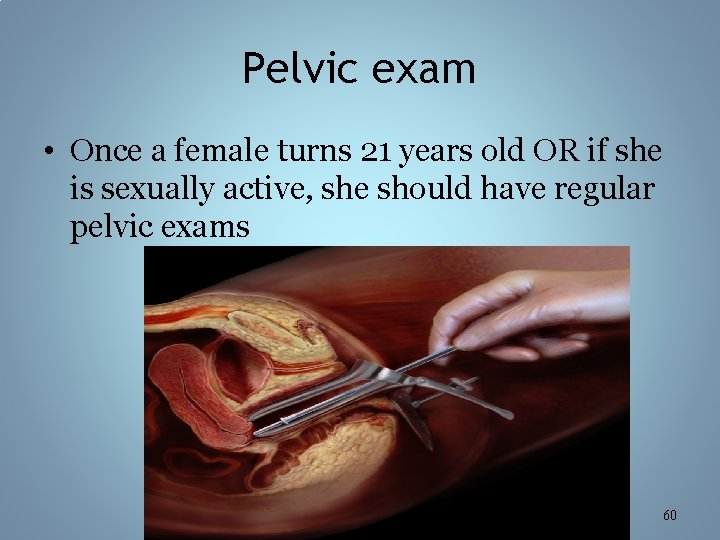
Pelvic exam • Once a female turns 21 years old OR if she is sexually active, she should have regular pelvic exams 60
• After about 500 cycles, human females undergo menopause, the permanent end of ovulation and menstruation 61
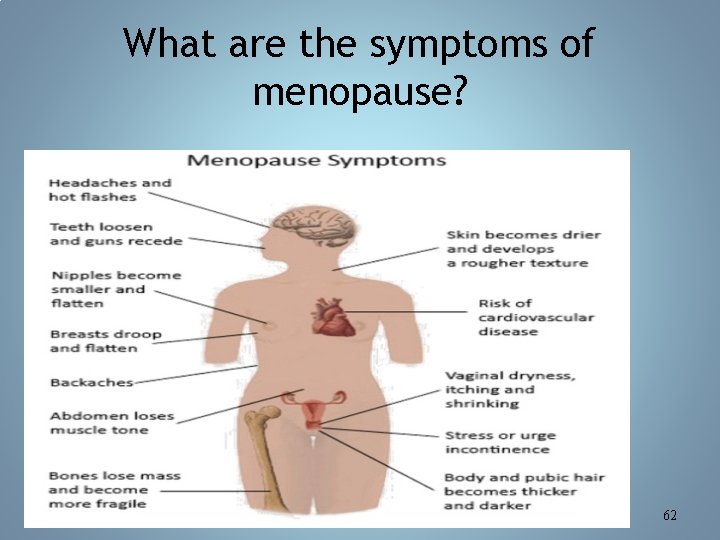
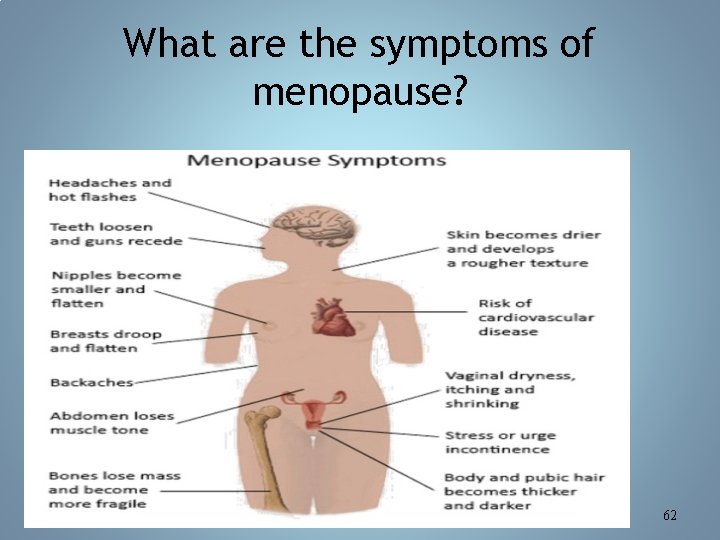
What are the symptoms of menopause? 62
63