HUMAN IMMUNODEFICIENCY VIRUS DISEASE BY Dr Shabani AIDS
HUMAN IMMUNODEFICIENCY VIRUS DISEASE BY: Dr. Sha`bani
�AIDS first recognized in the United States in 1981 �CDC reported PCP in 5 previously healthy MSMs in Los Angeles and KS in 26 previously healthy MSMs in New York.

DEFINITION �CDC classification : on basis of clinical condition and CD 4 ( a matrix of 9 categories) �Any HIV with CD 4 < 200 has AIDS regardless of the presence of symptoms or opportunistic diseases
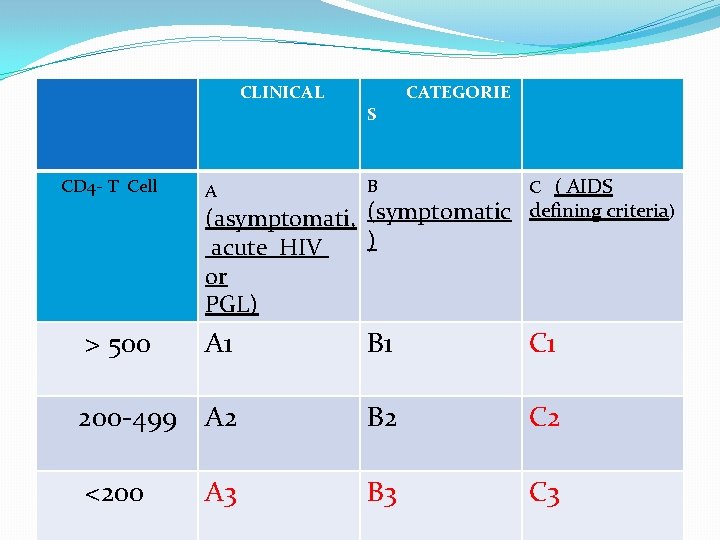
CLINICAL S CATEGORIE CD 4 - T Cell A B C ( AIDS > 500 A 1 B 1 C 1 200 -499 A 2 B 2 C 2 <200 B 3 C 3 (asymptomati, (symptomatic defining criteria) acute HIV ) or PGL) A 3
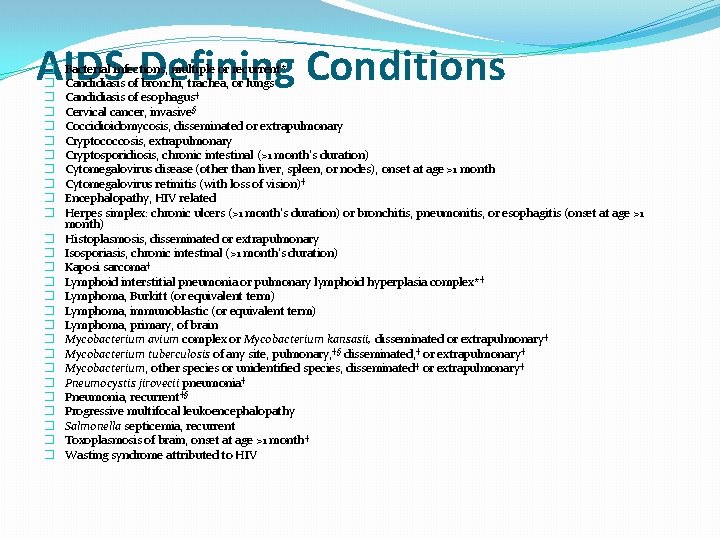
AIDS-Defining Conditions � � � � � � � Bacterial infections, multiple or recurrent* Candidiasis of bronchi, trachea, or lungs Candidiasis of esophagus† Cervical cancer, invasive§ Coccidioidomycosis, disseminated or extrapulmonary Cryptococcosis, extrapulmonary Cryptosporidiosis, chronic intestinal (>1 month's duration) Cytomegalovirus disease (other than liver, spleen, or nodes), onset at age >1 month Cytomegalovirus retinitis (with loss of vision)† Encephalopathy, HIV related Herpes simplex: chronic ulcers (>1 month's duration) or bronchitis, pneumonitis, or esophagitis (onset at age >1 month) Histoplasmosis, disseminated or extrapulmonary Isosporiasis, chronic intestinal (>1 month's duration) Kaposi sarcoma† Lymphoid interstitial pneumonia or pulmonary lymphoid hyperplasia complex* † Lymphoma, Burkitt (or equivalent term) Lymphoma, immunoblastic (or equivalent term) Lymphoma, primary, of brain Mycobacterium avium complex or Mycobacterium kansasii, disseminated or extrapulmonary† Mycobacterium tuberculosis of any site, pulmonary, †§ disseminated, † or extrapulmonary† Mycobacterium, other species or unidentified species, disseminated† or extrapulmonary† Pneumocystis jirovecii pneumonia† Pneumonia, recurrent†§ Progressive multifocal leukoencephalopathy Salmonella septicemia, recurrent Toxoplasmosis of brain, onset at age >1 month † Wasting syndrome attributed to HIV
ETIOLOGIC AGENT �Family : Retroviridae �Subfamily : lentiviruse ( Retroviruses: HIV-1, HIV-2, HTLV-1, HTLV-2) -defined groups of HIV-1 : M, N, O, P -an icosahedral structure with 2 major envelope proteins, gp 120 and gp 41

• HIV-1 and HIV-2 are : 1 -Transmitted through the same routes 2 - Associated with similar opportunistic infections • HIV-1 is more common worldwide • HIV-2 is found in West Africa, Mozambique, and Angola
Basic Components of the Immune System �Lymphocytes (2 major types which protect host): (1) B cells: formed in bone marrow and produce antibodies after exposure to an antigen. (2) T cells: processed in the thymus (two subtypes) Subtype 1: Regulator cells also known as helper or CD 4 cells (“generals” in army of immune system which recognize “invaders” and summon armies of cells to mount a direct attack) - cd 4 is also expressed on surface of monocytes/macrophages and dendritic /langerhans Subtype 2: Fighter or effector cells also known as cytotoxic or CD 8 cells (bind directly to antigen and kill it)
![zax. SCDVFBGNM, . Qaswdefrgthyjulo; p’[ ] � 2 types of CD 4 cells: (1) zax. SCDVFBGNM, . Qaswdefrgthyjulo; p’[ ] � 2 types of CD 4 cells: (1)](http://slidetodoc.com/presentation_image_h/e7a273e15cc0818b7cf79eac898390be/image-9.jpg)
zax. SCDVFBGNM, . Qaswdefrgthyjulo; p’[ ] � 2 types of CD 4 cells: (1) Memory cells: those programmed to recognize a specific antigen after it has been previously seen (2) Naïve cells: non-specific responders �CD 4 cells replicate 100 million times a day. �CD 4 cells are the target cells of HIV.
HIV Viral Dynamics �HIV is classified as a retrovirus -Once HIV enters the host (CD 4) cell, it converts its RNA (ribonucleic acid) to DNA (deoxyribonucleic acid) via its enzyme reverse transcriptase. The replication cycle begins with high-affinity binding of the gp 120 to its receptor on the host cell �Gp 120 binds to CD 4 , then changes that facilitats binding to co-receptors ( CCR 5 and CXCR 4) �Use of at least one of receptors by the virus for entry is an important determinant of cellular tropism of the virus
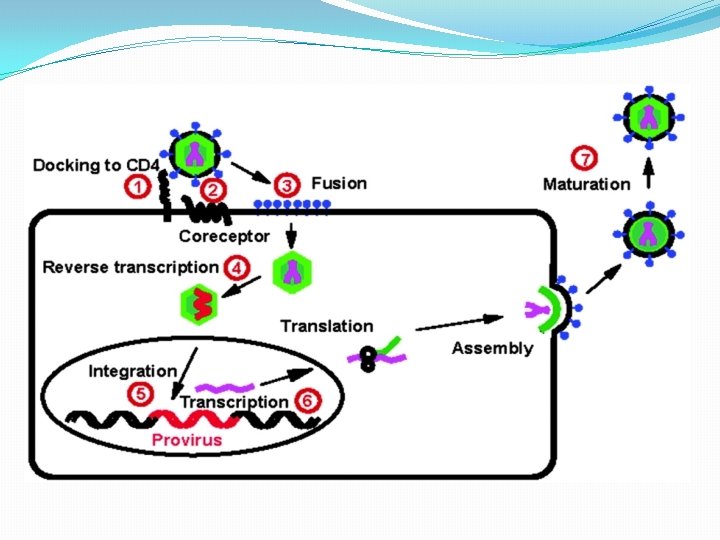
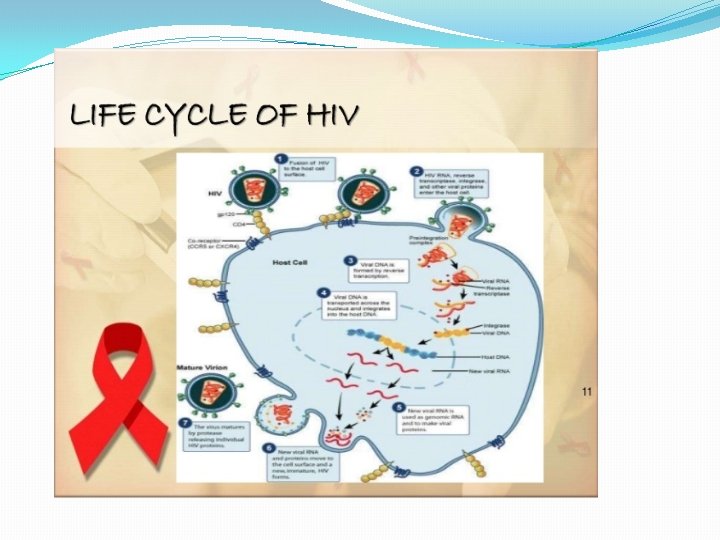
HIV gains entry into the CD 4 cell by binding onto receptors on the outside of the CD 4 cell and fusing with the lipid outer layer of the cell. Once inside the cell, HIV removes its outer coating, exposing its RNA, and releases reverse transcriptase enzyme to convert the HIV RNA to DNA. HIV DNA then enters the nucleus of the CD 4 cell and is integrated into the host (CD 4) DNA
�Once the cellular DNA has been altered in this way, it is known as proviral DNA Long viral protein chains are produced which are then cut into the necessary pieces to produce more HIV. This process is activated by the viral protease enzyme. Each step in this process is a target for antiretroviral therapy (to date, reverse transcriptase, protease inhibitors and fusion inhibitors have been approved)
TRANSMISSION � 1 -Sexual: By far the most common mode of infection –esp. in developing countries- is heterosexual. �Factors that may enhance the efficiency of heterosexual transmissionof HIV: � 1 - higher viremia � 2 -acute primary infection � 3 - receptive anal intercourse � 4 - sex during menses � 5 - lack of male circumcision � 6 - the presence of other STDs.
�Hiv quantity : a predominant factor( highest risk in acute hiv and endstage of disease) �ART reduces risk �Circumcision �OCP �Oral sex �Alcohol and illicit drugs

� 2 -Mother-to-child transmission � 1 -pregnancy(23 - 30%) � 2 - delivery( 50 -65%) � 3 - breast-feeding(12 - 20%) (These numbers based upon 2 studies in congo) � the risk of not breast-feeding varies greatly between and within developing countries (individual)
�Transfusion with HIV-contaminated blood, as a result of � 1 -the absence of implementation of national policies for transfusion � 2 - the recruitment of voluntary and unpaid donors � 3 - proper screening of collected blood � 4 - strategy for its rational use
�Nosocomial transmission: � 1 -percutan. (0. 3%) � 2 -mucous(0. 09%) � 3 -nonintact skin( rare)
�Low titer in saliva but no convincing evidence �Human bite( case report) �Other fluids ( semen , sweat, . . ) if visible bloody
pathophysiology * Hallmark of HIV is profound quantitative and qualitative deficiency of T-helper cells * debate regarding which cells are infected first. * Mucosal transmission as model- fig. 1 and 2� 1 -Cross the barrier by transport on langerhans cells � 2 - seeks susceptible targets ( CD 4) �Spatial dispersion of CD 4 in mucosa ( that is an obstacle for establishment and low efficient sex. Transmission) � 3 -replication in lymphoid cells
�A few to several days the virus can not be detected in plasma ( eclipse phase) �rapid migration to regional lymph nodes is followed by dissemination via the bloodstream to various lymphoid tissues �Viremia : 5 -30 days afterintravaginal exposure
�Initail infection vary somewhat with route entry e. g. �Bloodstream inf( IDUs, . . , traumatized sex): virus is cleared to spleen where primary focal infection occurs then we have a wider dissemination.
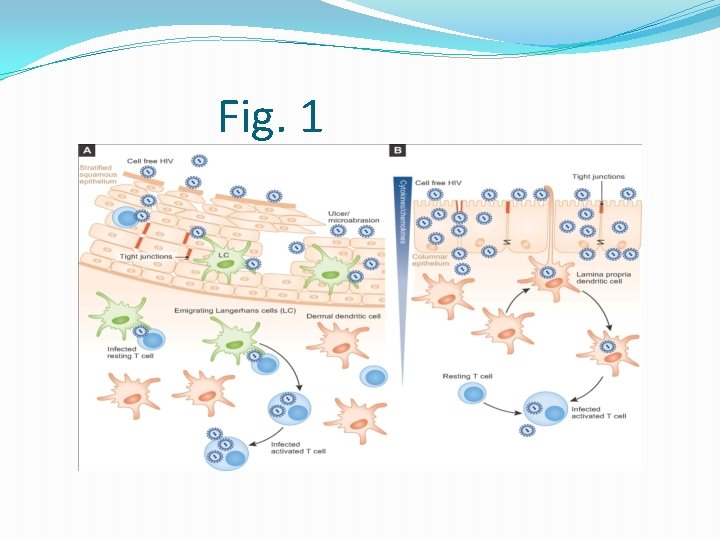
Fig. 1
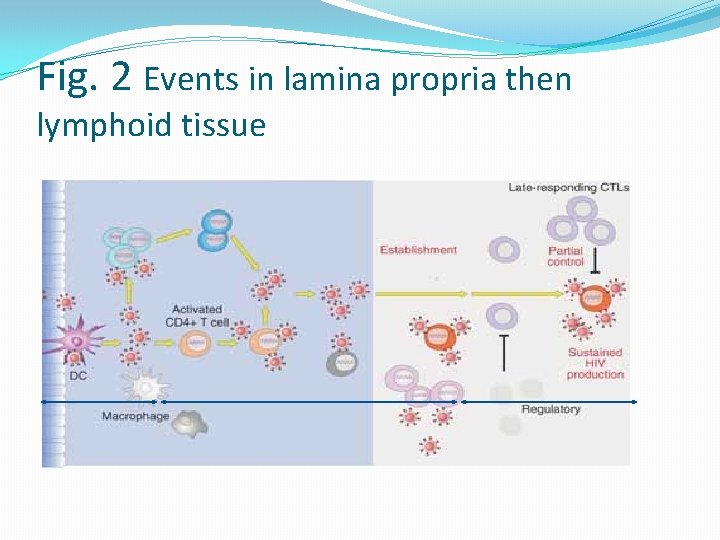
Fig. 2 Events in lamina propria then lymphoid tissue
HUMAN IMMUNODEFICIENCY VIRUS–SPECIFIC IMMUNE RESPONSES �HUMORAL IMMUNE RESPONSES: �Antibodies appear usually during 3 -6 weeks( but neutralizing Abs within the 6 months) �HIV is unique. �Despite the robust cellular and humoral response the virus succeds in escaping. �The virus evades adequate control by both arms of adaptive immune system( because of 1 - mutations produced during the reverse transcription process, combined with high levels of replication over a prolonged period) 2 - no relationship was found between the breadth of the response and levels of plasma HIV viremia
�high levels of antibodies with neutralizing potential appear several weeks later, although their breadth is limited and their ability is inadequate. �genetic diversity and difficulty in neutralizing the virus
Cellular Immune Responses �Cytotoxic T Lymphocytes: �CD 8+ T-lymphocyte in the peripheral blood within the first few months of HIV infection and during the chronic phases of infection in most HIV-infected individuals
�CD 4+ T-Cell Responses: �Unlike most other infections of humans, HIV infection is characterized by the absence or extremely low level of HIV-specific CD 4+ T-cell proliferative responses in the vast majority of untreated patients. �Because HIV infects CD 4+ T cells, it was believed that the early loss of HIV-specific proliferative responses may be the result of infection and deletion of HIV specific CD 4+ T cells in the lymphoid tissues.
�HIV-specific CD 4+ T cells persist at the expected frequencies during the chronic phase of infection in patients with progressive disease, although there is some controversy over whether disruptions of function persist
�In the absence of treatment, survival is short after the diagnosis of clinically defined AIDS �In a trial the mean survival time after a CD 4+ count of 200/mm 3 was 38 to 40 months �More rapid progression of HIV in : � 1 - older � 2 - more severe or long-lasting symptoms during the acute retroviral syndrome �Lab data including TLC< 1000/mm 3, WBC <4000/mm 3, Hct< 40 m. L/d. L, and a low percentage of CD 4+ lymphocytes (CD 4+ percentage has a narrower range of variation than the absolute CD 4+. )
Diagnosis �Diagnosis proceeds from history, physical examination, and laboratory studies. Laboratory detection of HIV is a two-step sequential process using a highly sensitive screening test followed by a highly specific confirmatory assay �Rapid tests are now FDA-approved for screening and confirmation
�Standard screening test: ELISA (or EIA) with sensitivity >99. 5% � 4 th gen. of EIA detects Abs to HIV and P 24 Ag �False positive with technical artifacts, chronic medical conditions, multiparity �medical conditions such as chronic alcohol use, rheumatic disease, congenital bleeding disorders, syphilis, recent vaccination with hepatitis B, recent infections with dengue, malaria, and hepatitis B
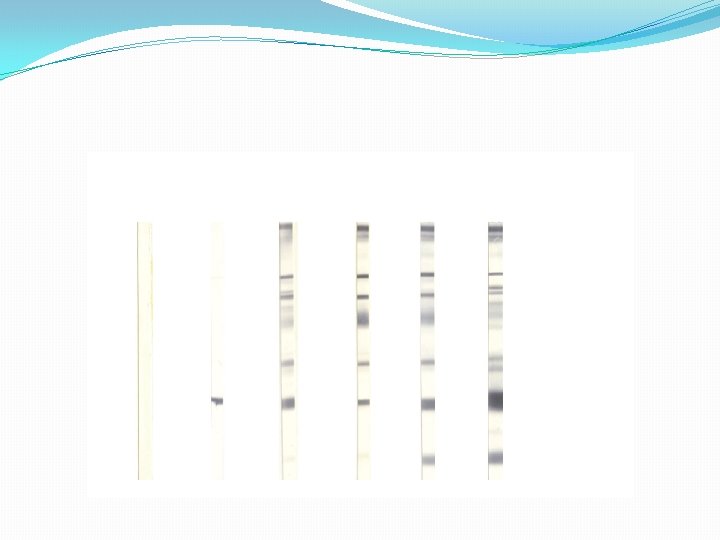
�Then, should be confirmed with a test such as WB (western blot) �Multiple HIV Ags be separated on the basis of different Wt. and Abs to each component can be detected as discrete band.
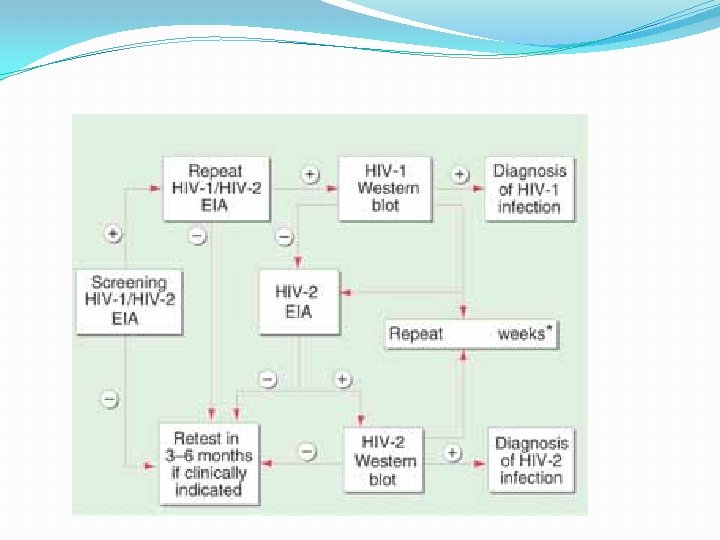
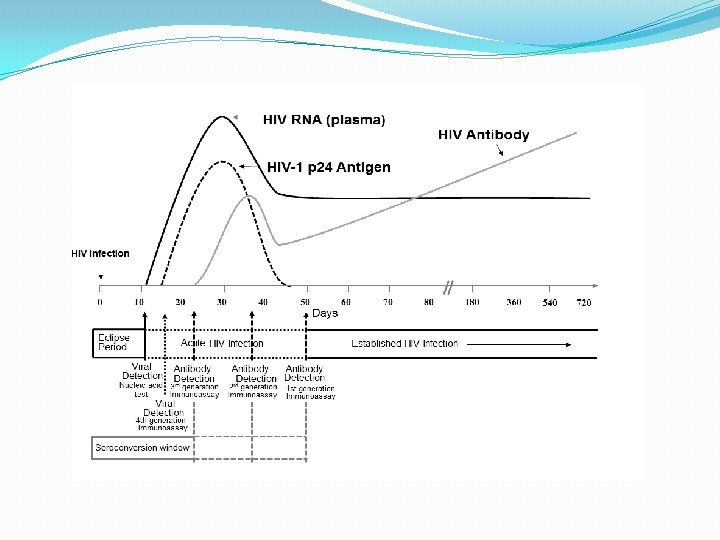
�If there is a significant risk of acute HIV infection, then use of some rapid test is not advised because they are less sensitive in this setting. �Recent advances have developed rapid testing modalities that combine p 24 antigen and HIV-1 antibody detection and were FDA approved in mid 2013.
�All screening ELISA tests with reactive results are repeated in duplicate; repeatedly reactive samples are referred for confirmation �qualitative NAT represents an appropriate modality to resolve indeterminate WBs, especially if acute infection is a possibility.
Clinical Manifestations �three principal types: (1) an acute viral dis. (in the initial weeks) of infection , associated with a high viral load an intense host immune response (2) immunologically mediated processes related to host responses to chronic viral infection, including inflammation (e. g. , lymphadenopathy, thrombocytopenia, HIV-related dementia, an cardiovascular disease (3) opportunistic diseases
�Spectrum and Progression of HIV Infection: �asymptomatic state to severe immunodeficiency and associated serious secondary infections, neoplasms, and other conditions. �Approximately 5% to 8% of HIVinfected individuals remain clinically asymptomatic, with normal CD 4+ Tlymphocyte counts for more than 8 years after infection. These individuals are called “long-term nonprogressors. ”

�Initial or primary infection: acute mononucleosis-like illness associated with seroconversion include fever, lymphadenopathy, sweats, myalgia, arthralgia, rash, malaise, lethargy, sore throat, anorexia, nausea, vomiting, diarrhea, headache, photophobia, and mucocutaneous ulcers �One half to two thirds of patients present with an acute “mononucleosis-like” illness often with a truncal exanthem(may be maculopapular, roseola-like, or �Urticarial) � Symptoms generally resolve within 10 to 15 days.
�The signs and symptoms of acute HIV infection days to weeks( 1 -6 wks) after exposure �The dignosis in this status can not be done with routine serology( 3 rd gen. immunoassay) Because they detect antibodies ( which become positive 3 wks later. �should be made by requesting a plasma HIV-RNA assay, (sensitivity of 100% and specificity of 97. 4%. ) � The test for the presence of detectable p 24 antigen is less sensitive (88. 7%) but more specific (100%) than the plasma HIV-RNA assay for the diagnosis of primary infection �the detection of p 24 antigen was used routinely in the screening of blood donors which is supplanted by NAT(nucleic acis test)
�Laboratory evaluation : �Reduced TLC , elevated ESR, negative heterophil antibody test, and elevated aminotransferase and alkaline phosphatase �TLC including both CD 4+ and CD 8+ T lymphocytes, decreases, with a normal ratio of CD 4+ to CD 8+ cells. � Within several weeks, both increases. The rise in CD 8+ is relatively greater than CD 4/CD 8 ratio is inverted. � In the weeks that follow, the CD 8+ increases rather markedly because of HIV-specific CD 8+ T lymphocytes.
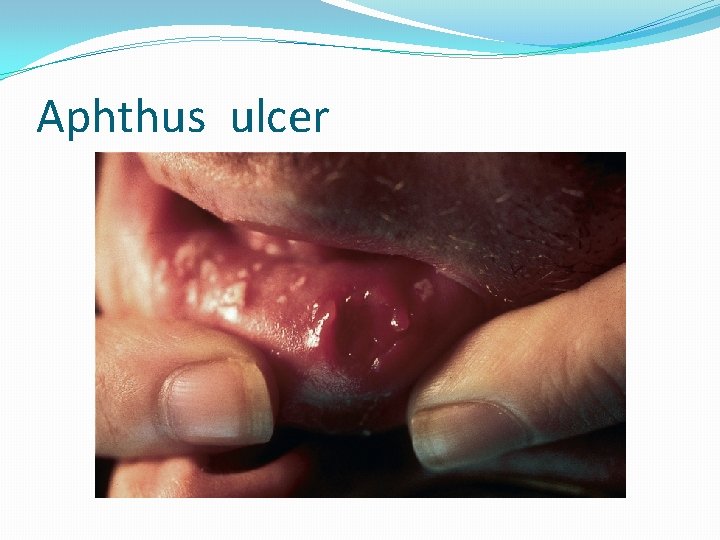
Aphthus ulcer
DDX �infectious mononucleosis and other viral infections such as influenza, viral hepatitis, measles, rubella, primary herpes simplex virus (HSV) infection, cytomegalovirus, and secondary syphilis.
Metabolic and Endocrine Abnormalities �Hypogonadism, particularly depression of testosterone or dihydrotestosterone levels �wasting with decreased caloric intake, elevated catabolism caused by opportunistic infections, or chronic diarrhea
Oral Disease �In Primary HIV : severe aphthous stomatitis and with oropharyngeal and esophageal candidiasis. �Because oral candidiasis itself is an opportunistic infection, it is predictive of the disease progression �The most common form is thrush (pseudomembranous candidiasis). Characteristic cottage cheese plaques that can be removed with a tongue blade are seen on the soft palate, tonsils, and buccal mucosa
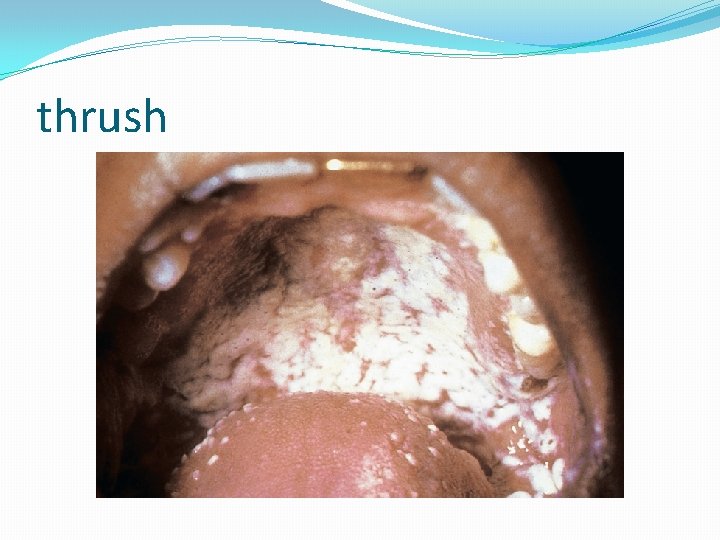
thrush
Pulmonary Manifestations �The differential diagnosis is influenced by the stage of immunosuppression, ART, prophylaxis for opportunistic infections, and the local epidemiology of conditions such as tuberculosis and endemic fungal infections. �Findings on chest radiography can also help
Pneumocystis jirovecii Pneumonia �Most cases of PCP occur at CD 4 <200 cell in patients not receiving ART. � Patients with PCP typically report cough and fever of at least several weeks’ duration. � Radiographic findings include diffuse interstitial infiltrates most commonly, but cavities, pneumothoraces, pleural effusions, and normal radiographs can occur. � Diagnosis relies on identification of the organism in respiratory secretions, often through induced sputum or bronchoalveolar lavage, which is more sensitive
�Bacterial Pneumonia: �Streptococcus pneumoniae and Haemophilus influenzae are the most commonly isolated pathogens. � With worsening immunosuppression, pneumonias due to Staphylococcus aureus, Pseudomonas aeruginosa (especially in the setting of neutropenia), Nocardia spp. , and Rhodococcus equi can occur
�Mycobacterial Pneumonia: �The features vary based on the degree of immunosuppression. � HIV-infected patients with respiratory symptoms who are from tuberculosis-endemic areas or have other risk factors for tuberculosis, who have a positive test for latent tuberculosis without a history of prophylactic therapy, or who have a personal history of tuberculosis without documentation of appropriate treatment should be placed in negative air pressure rooms until the diagnosis of pulmonary tuberculosis is excluded. � Sputum nucleic acid amplification tests can �hasten diagnosis, particularly in smear negative patients
Gastrointestinal Manifestations �Disorders of the Esophagus: �dysphagia or odynophagia and affect up to one third of patients With AIDS � Infectious causes include Candida, cytomegalovirus (CMV), herpes simplex virus, varicella-zoster virus, mycobacteria, Histoplasma, and Pneumocystis jirovecii. � Noninfectious causes include reflux esophagitis and pill esophagitis. � Malignant causes include esophageal carcinoma, lymphoma, and Kaposi sarcoma. . � Upper endoscopy with biopsy of lesions is highly sensitive in many cases
�Disorders of the Liver � Because of shared modes of transmission, hepatitis caused by acute or chronic infection with hepatitis B and C viruses is common �Disorders of the Biliary Tree, Gallbladder, and Pancreas � Acalculous cholecystitis and cholangitis in advanced AIDS � CMV, Cryptosporidium, and microsporidia are most commonly implicated �Endoscopic retrograde cholangiopancreatography can be used for both diagnosis and treatment
�Clostridium difficile is the most common cause of diarrhea in HIV-infected patients �HIV-associated enteropathy causes culture negative diarrhea and may improve with ART.
Neurologic Diseases �Ten percent of HIV-positive patients initially present with neurologic �Cognitive Manifestations: � HIV-associated neurocognitive disorder occurs in 15% of patients with AIDS and can be the first manifestation in 3% to 10%
Central Nervous System (CNS) Mass Lesions �Toxoplasmosis is the most frequent cerebral mass lesion �Empiric treatment with pyrimethamine and sulfadiazine is useful when clinical and radiologic findings are consistent with the diagnosis.
�Primary CNS lymphoma is the most common HIVassociated brain malignancy and is associated with Epstein-Barr virus infection �Progressive multifocal leukoencephalopathy is caused by JC polyomavirus, which induces lytic infection of oligodendrocytes causing multifocal CNS demyelination
Antiretroviral Therapy �Antiretroviral therapy targets and inhibits HIVspecific enzymes. 1 - Nucleoside and nucleotid revers transcriptase inhibitors 2 -Non-nucleoside reverse-transcriptase inhibitors 3 - Protease inhibitors 4 - Integrase inhibitor 5 -CCR 5 antagonists 6 - Entry inhibitors
When to Initiate Antiretroviral Therapy � Recommend Initiation of Therapy � All HIV-infected patients, regardless of CD 4 count � Conditions Favoring Early Initiation of Therapy � Acute or recent HIV infection, or � AIDS-defining conditions, including HIV-associated dementia, or � Pregnancy, or � HIV-associated nephropathy, or � Lower CD 4 counts (<200 cells/mm 3), or � Acute opportunistic infections, or � HIV RNA >100, 000 copies/m. L, or � CD 4 decline >100 cells/mm 3/yr, or � Hepatitis B coinfection, or � Hepatitis C coinfection
� � THANKS A LOT �ANY Q?





- Slides: 111