HUMAN HERPES VIRUSES 1 Dr D Kalita Associate
















- Slides: 68
HUMAN HERPES VIRUSES -1 Dr. D Kalita, Associate professor, Department of Microbiology, AIIMS Rishikesh Date of Class: 26/4/2017 (4 PM to 5 PM, LT-4)
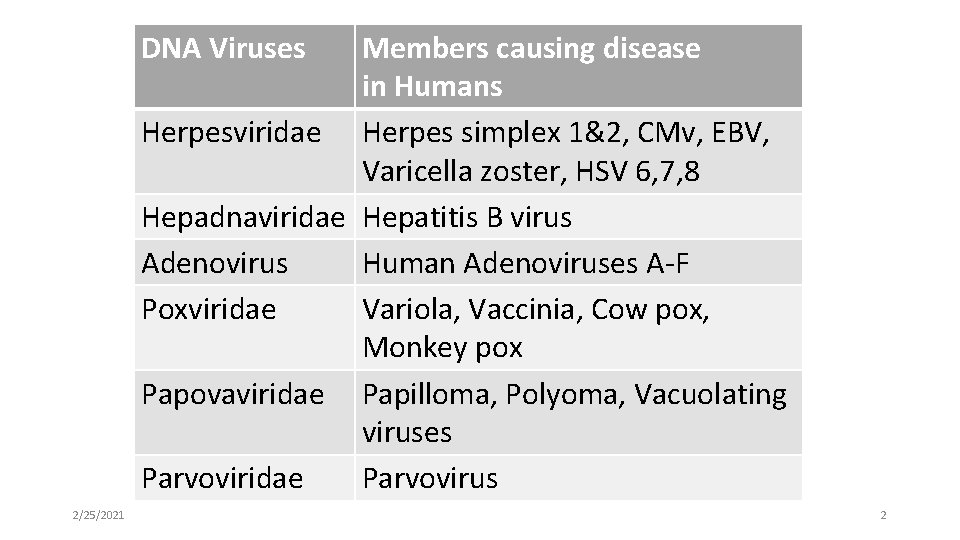
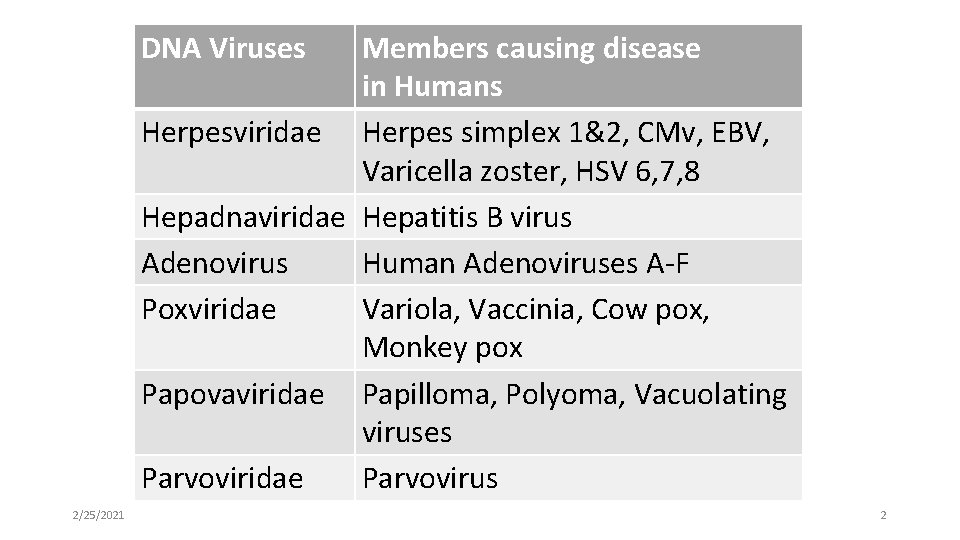
DNA Viruses Members causing disease in Humans Herpesviridae Herpes simplex 1&2, CMv, EBV, Varicella zoster, HSV 6, 7, 8 Hepadnaviridae Hepatitis B virus Adenovirus Human Adenoviruses A-F Poxviridae Variola, Vaccinia, Cow pox, Monkey pox Papovaviridae Papilloma, Polyoma, Vacuolating viruses Parvoviridae Parvovirus 2/25/2021 2
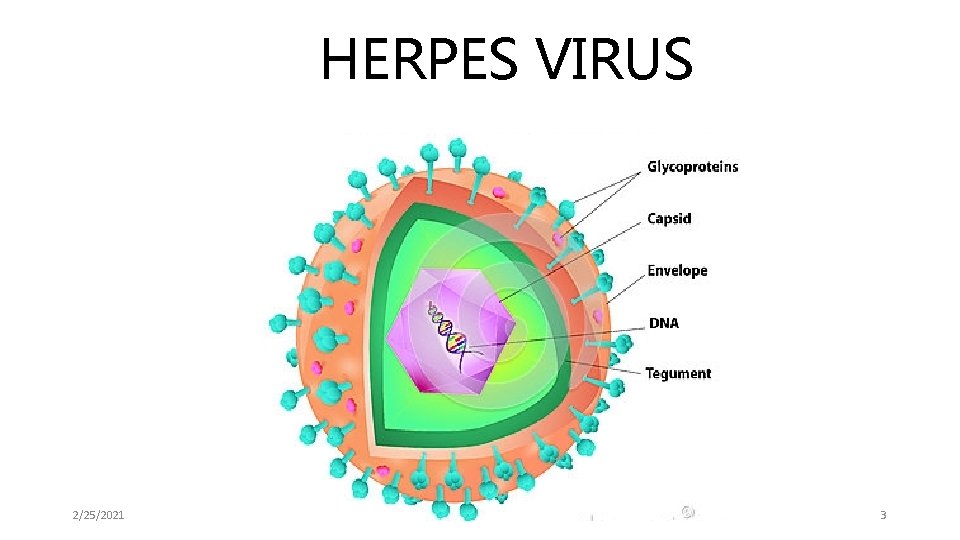
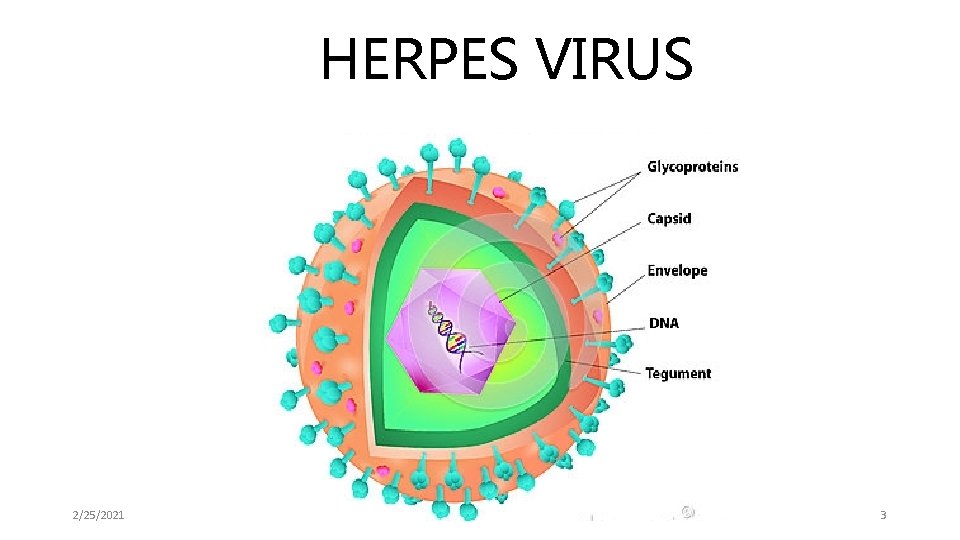
HERPES VIRUS 2/25/2021 3

Introduction to HERPES VIRUS • About 100 Enveloped DNA viruses affecting Humans and animals • Can cause Latent infections – enabling virus to persist within infected hosts and to undergo periodic reactivation. 2/25/2021 4
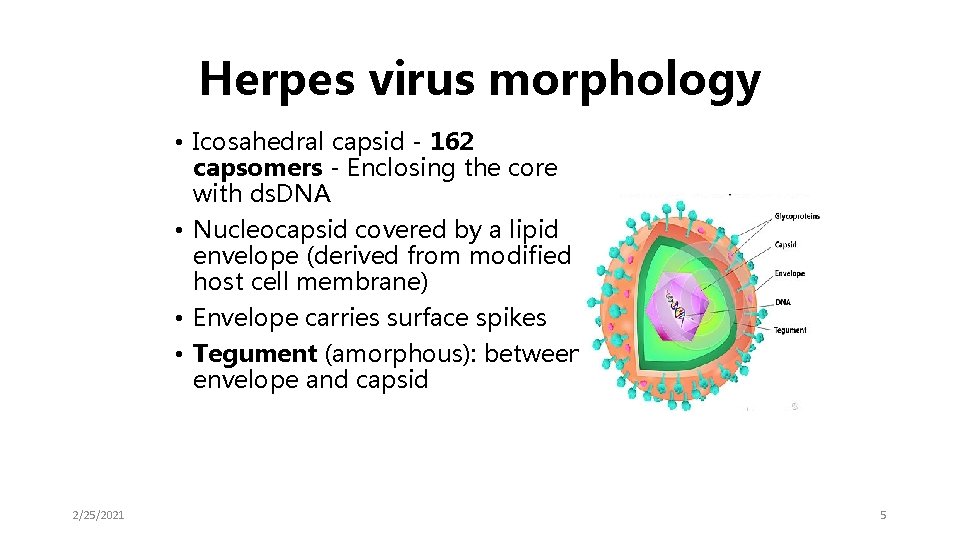
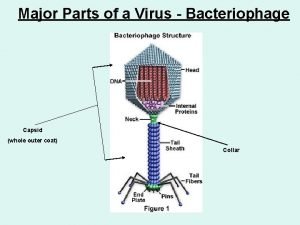
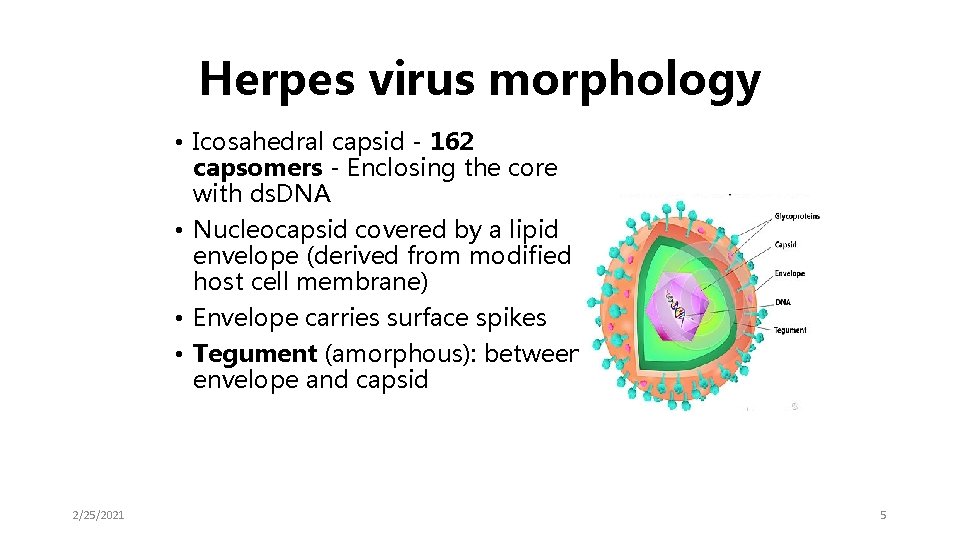
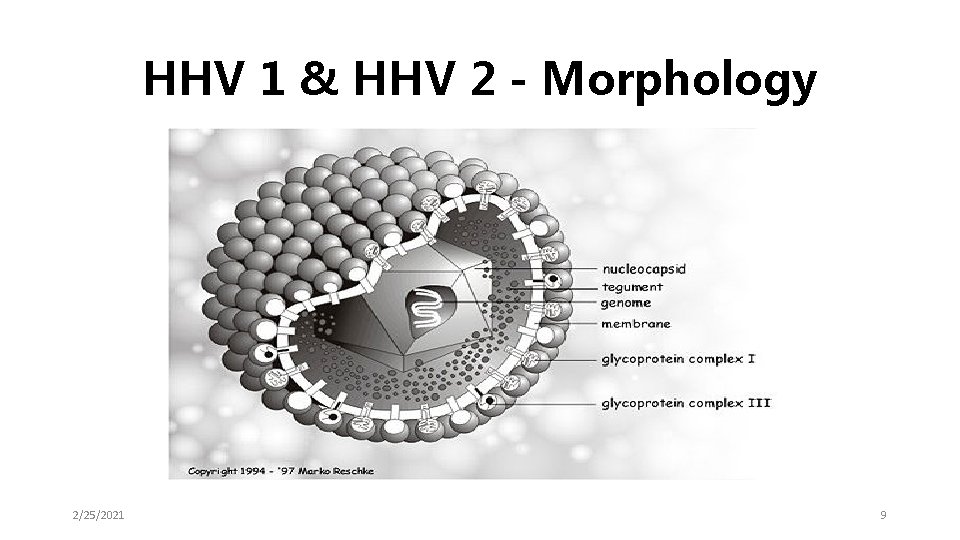
Herpes virus morphology • Icosahedral capsid - 162 capsomers - Enclosing the core with ds. DNA • Nucleocapsid covered by a lipid envelope (derived from modified host cell membrane) • Envelope carries surface spikes • Tegument (amorphous): between envelope and capsid 2/25/2021 5
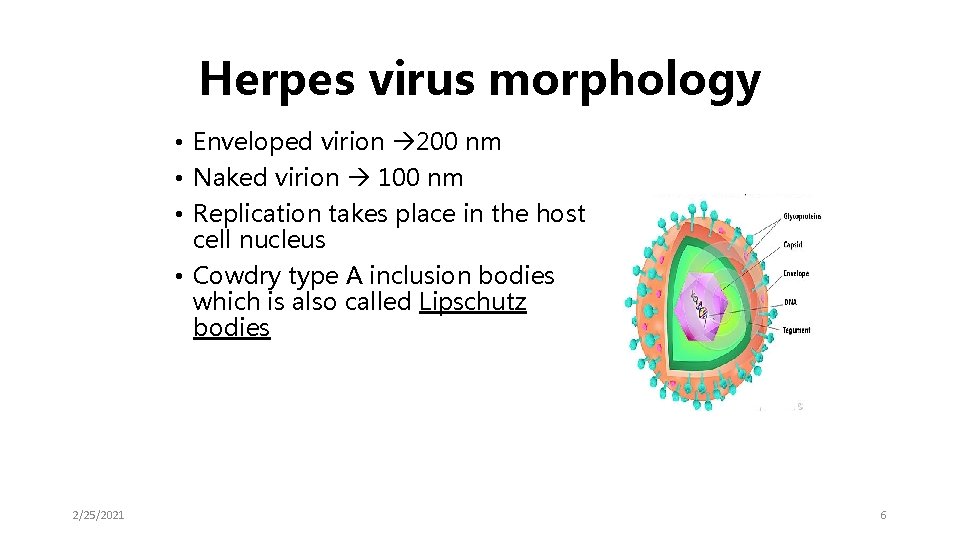
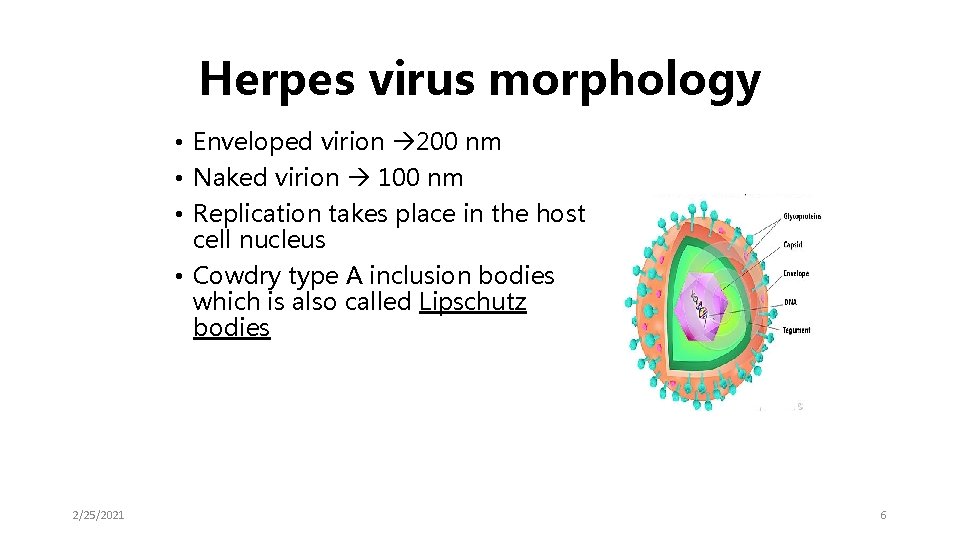
Herpes virus morphology • Enveloped virion 200 nm • Naked virion 100 nm • Replication takes place in the host cell nucleus • Cowdry type A inclusion bodies which is also called Lipschutz bodies 2/25/2021 6

CLASSIFICATION 2/25/2021 7
Herpes simplex
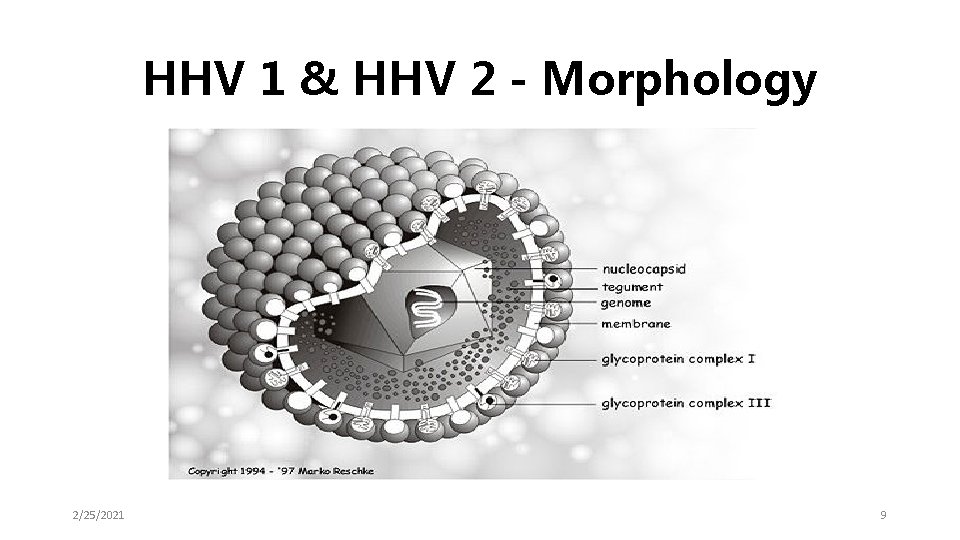
HHV 1 & HHV 2 - Morphology 2/25/2021 9
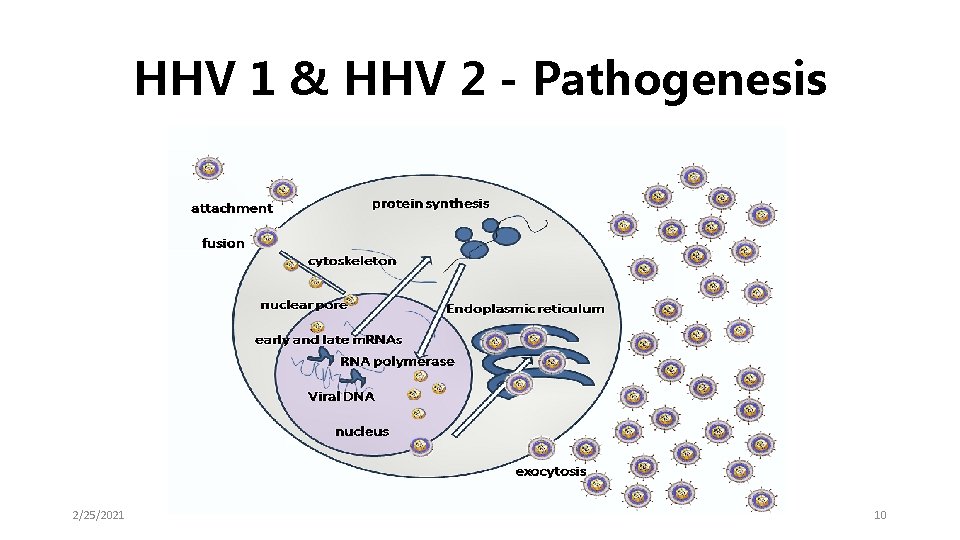
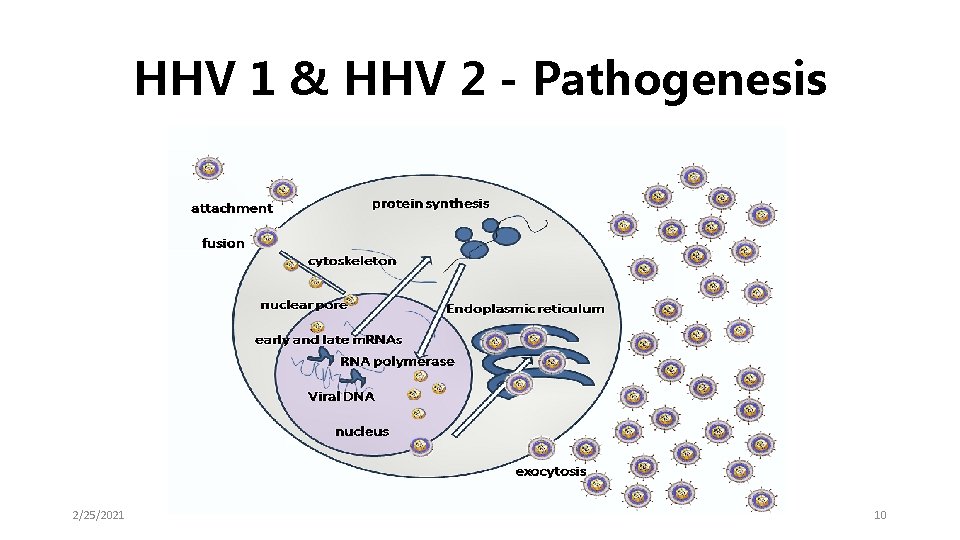
HHV 1 & HHV 2 - Pathogenesis 2/25/2021 10

Differentiation of HSV 1 and HSV 2 • • • Monoclonal antibodies Pocks in CAM (HSV 2 > HSV 1) HSV 2 more neurovirulent in lab animals HSV 2 is more resistant in vitro to antivirals (e. g. Cytarabine & IUDR) DNA RE studies differentiates (upto strain level) Etc. ……………. Ref to a textbook 2/25/2021 11
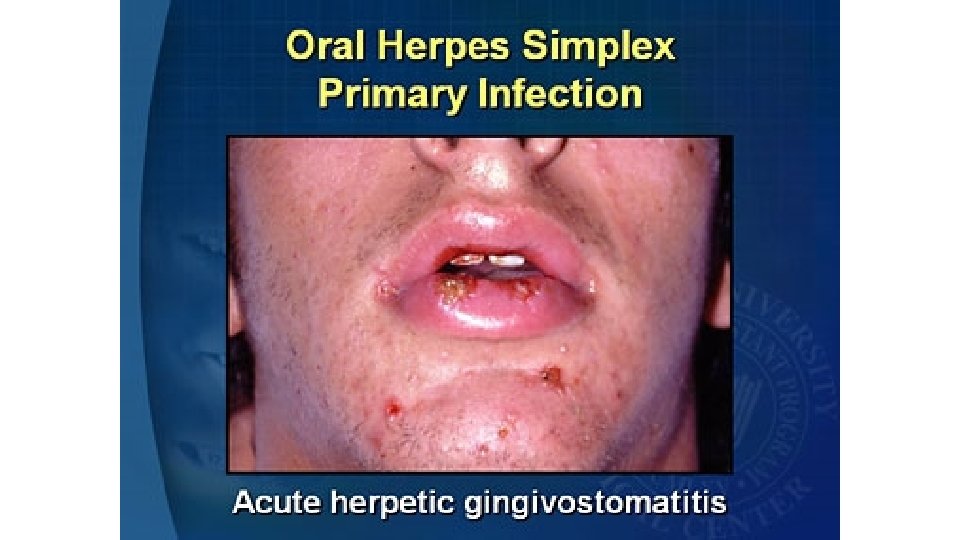
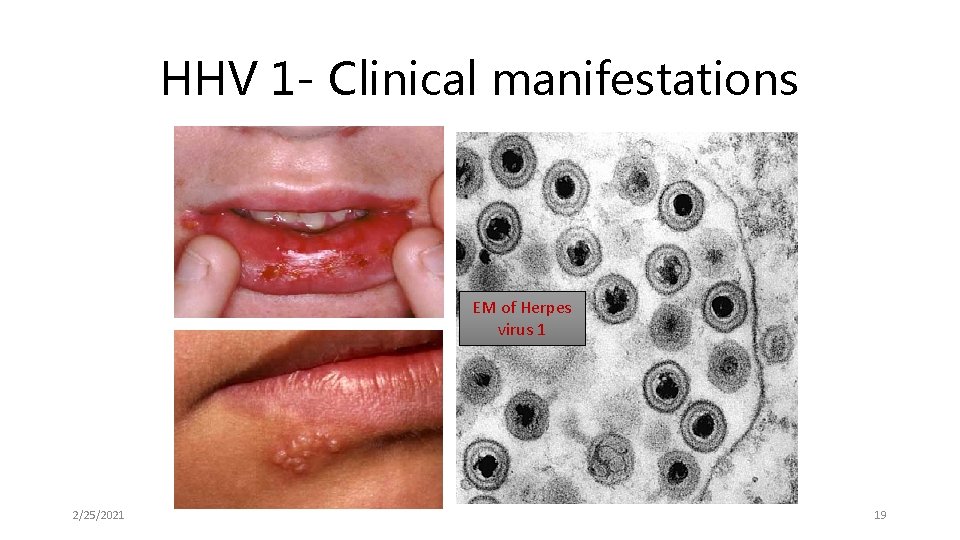
Infections • HSV 1 • • • Acute gingivostomatitis Herpes labialis (cold sore) Keratoconjunctivitis Eczema herpericum Encephalitis Dendritic keratitis (above waist…………………but…) 2/25/2021 12
• HSV 2 • Genital herpes (Penile, Urethral, Cervix, Vulval, Vaginal) • Neonatal herpes • Aseptic meningitis (Below waist…. . but…………. ) 2/25/2021 13
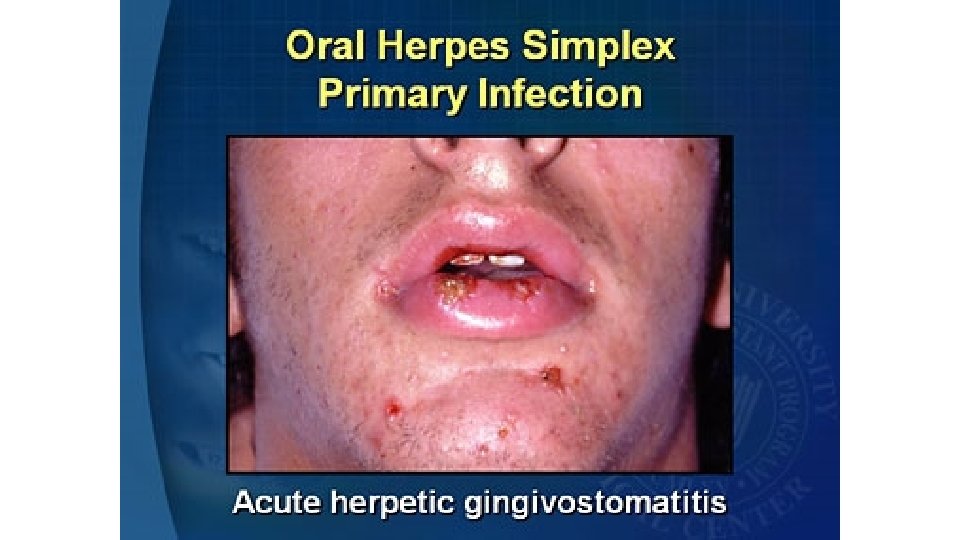
ACUTE GINGIVOSTOMATITIS • Acute gingivostomatitis is the commonest manifestation of primary herpetic infection. • Pain and bleeding of the gums • Ulcers with necrotic bases • Neck glands are commonly enlarged accompanied by fever. • Usually a self limiting disease lasting around 13 days.
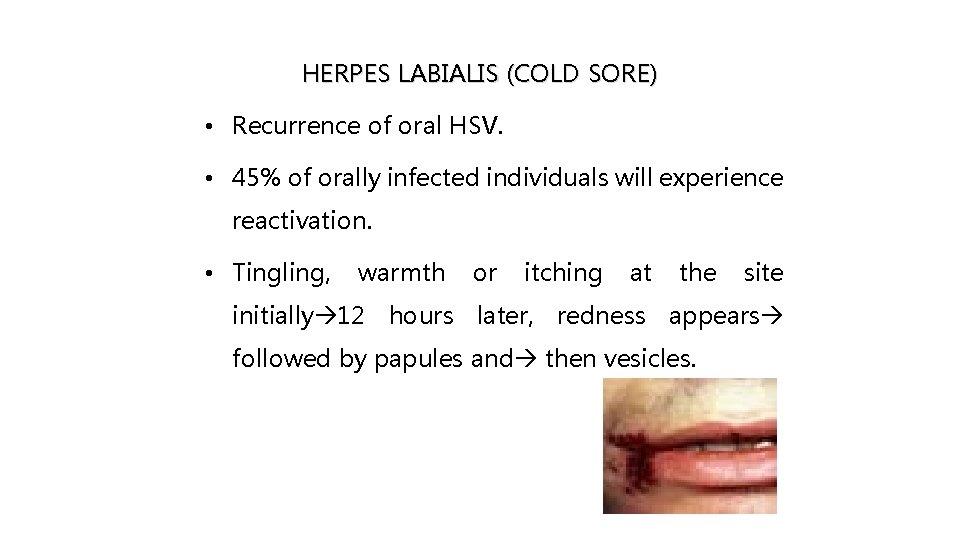
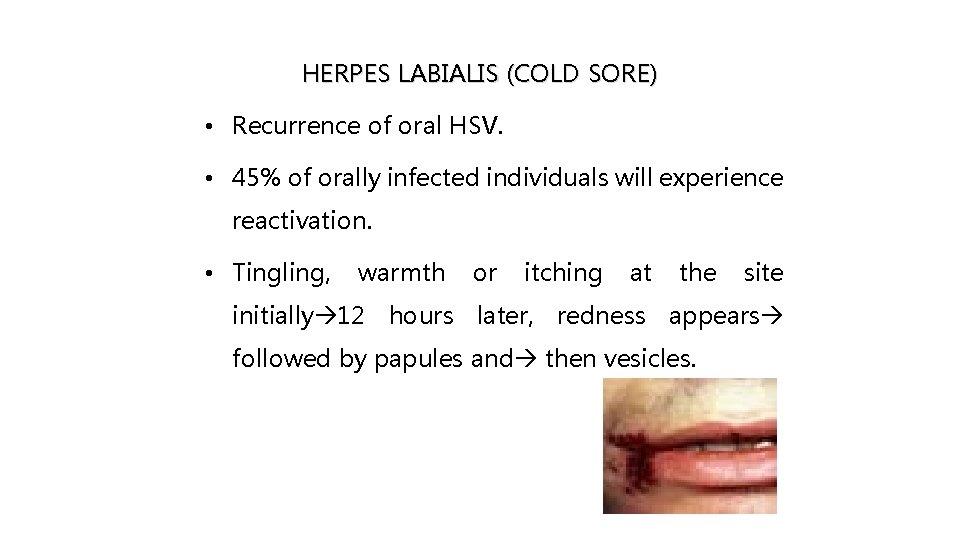
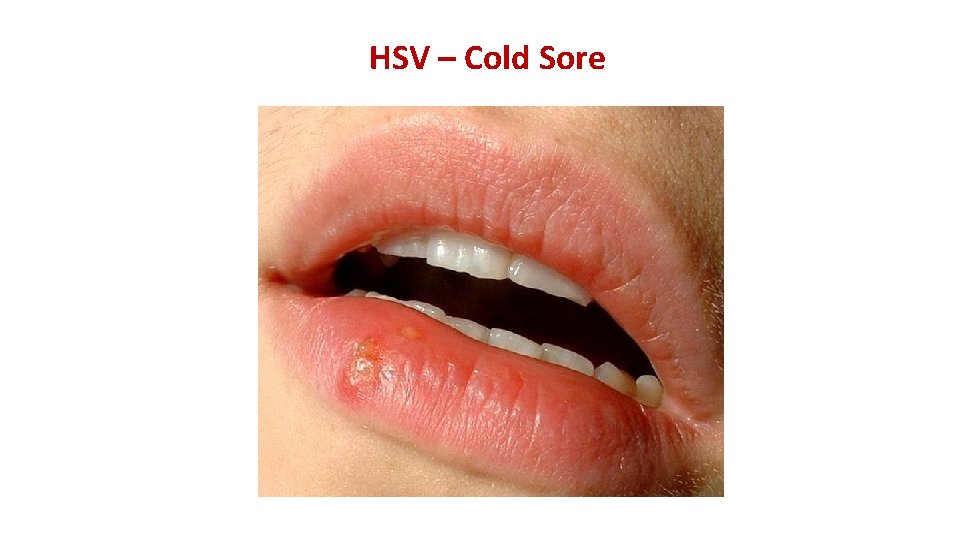
HERPES LABIALIS (COLD SORE) • Recurrence of oral HSV. • 45% of orally infected individuals will experience reactivation. • Tingling, warmth or itching at the site initially 12 hours later, redness appears followed by papules and then vesicles.
SYMPTOMS Mild or severe and may include: • Sores on the inside of the cheeks or gums • Fever • General discomfort, uneasiness, or ill feeling • Very sore mouth with no desire to eat • Halitosis
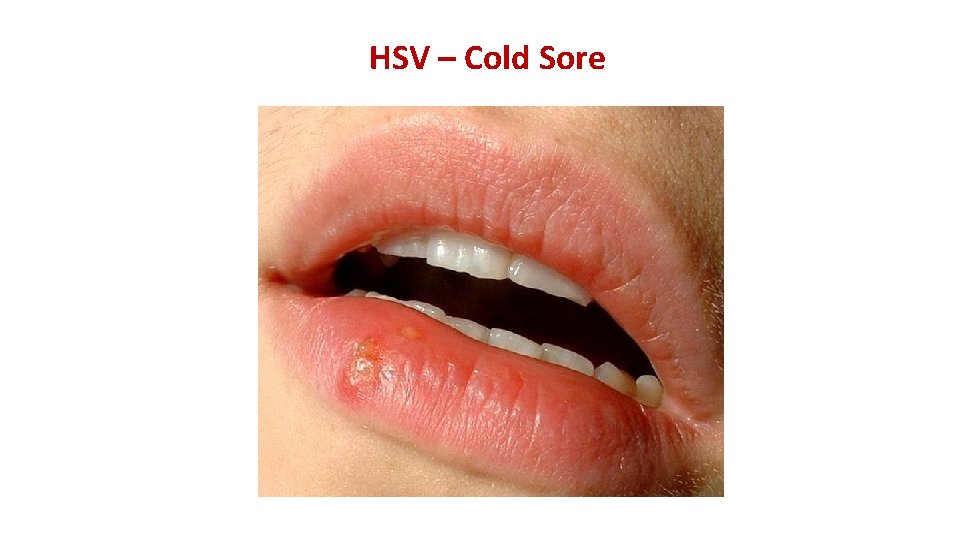
HSV – Cold Sore
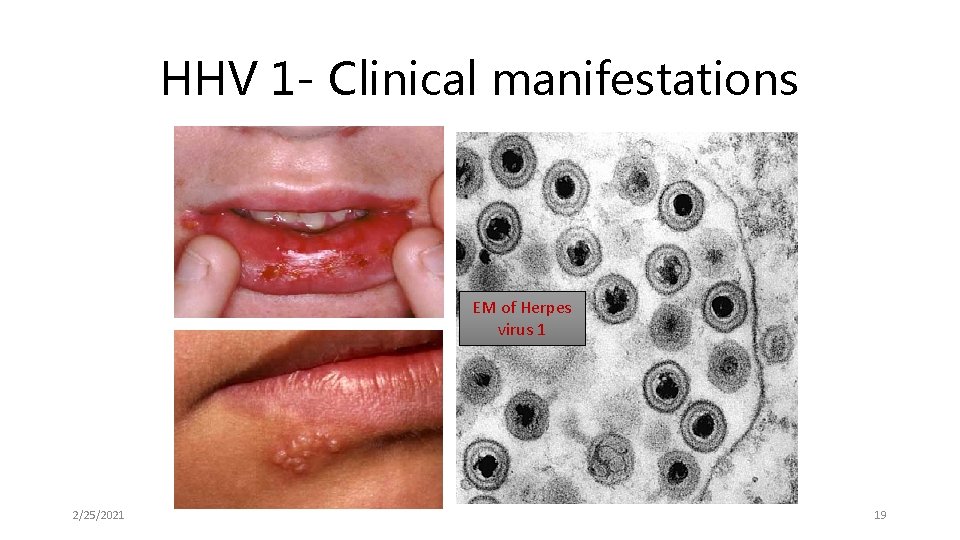
HHV 1 - Clinical manifestations EM of Herpes virus 1 2/25/2021 19
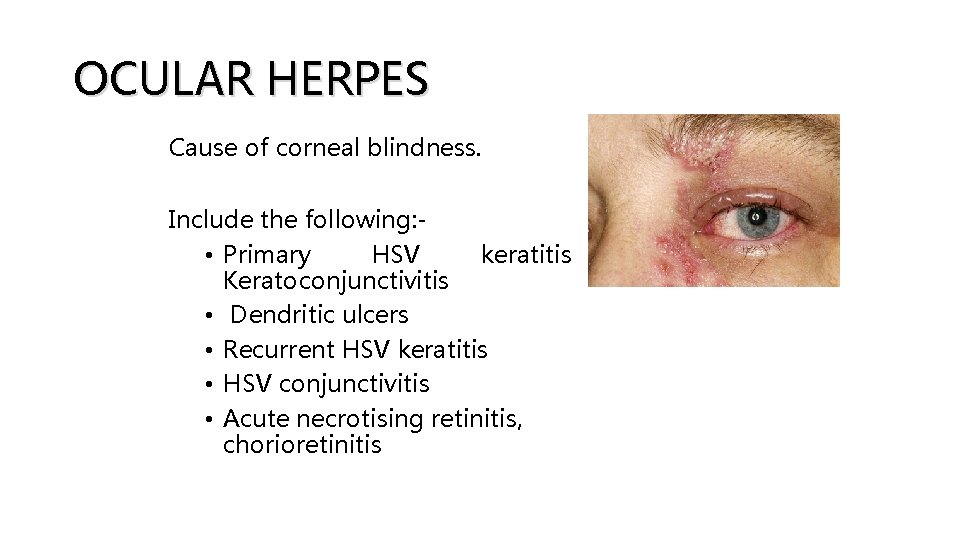
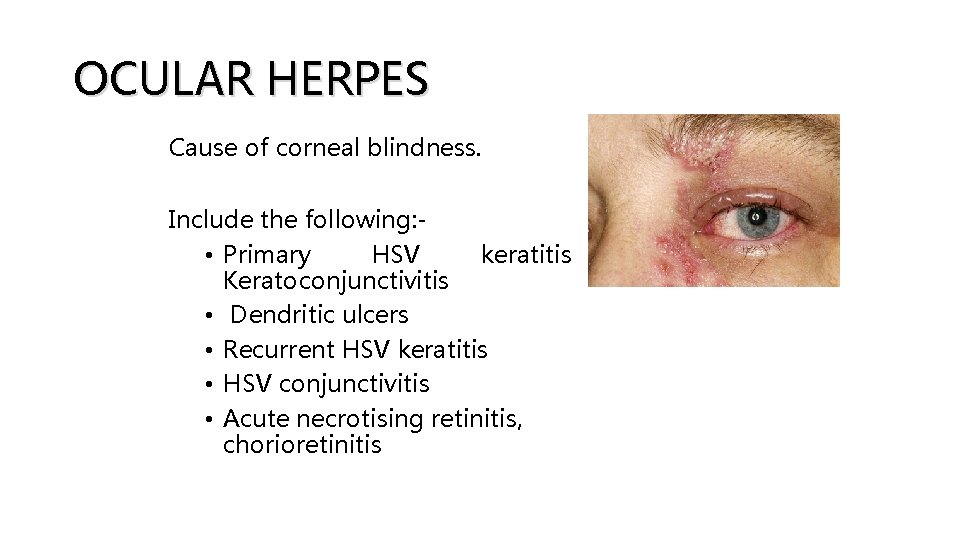
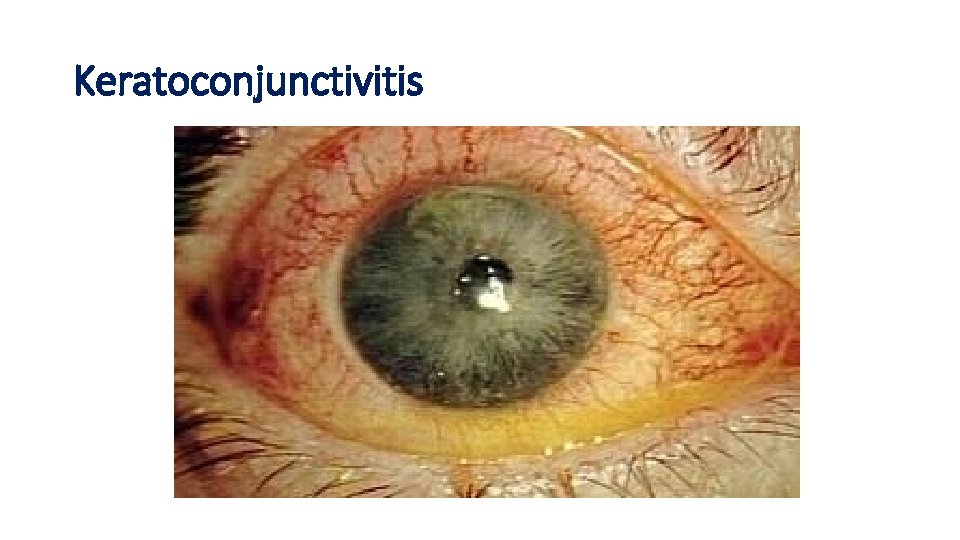
OCULAR HERPES Cause of corneal blindness. Include the following: • Primary HSV keratitis Keratoconjunctivitis • Dendritic ulcers • Recurrent HSV keratitis • HSV conjunctivitis • Acute necrotising retinitis, chorioretinitis –
KERATOCONJUNCTIVITIS • Inflammation of the cornea and conjunctiva. • Minor damage to the epithelium (superficial punctate keratitis) to formation of dendritic ulcers.
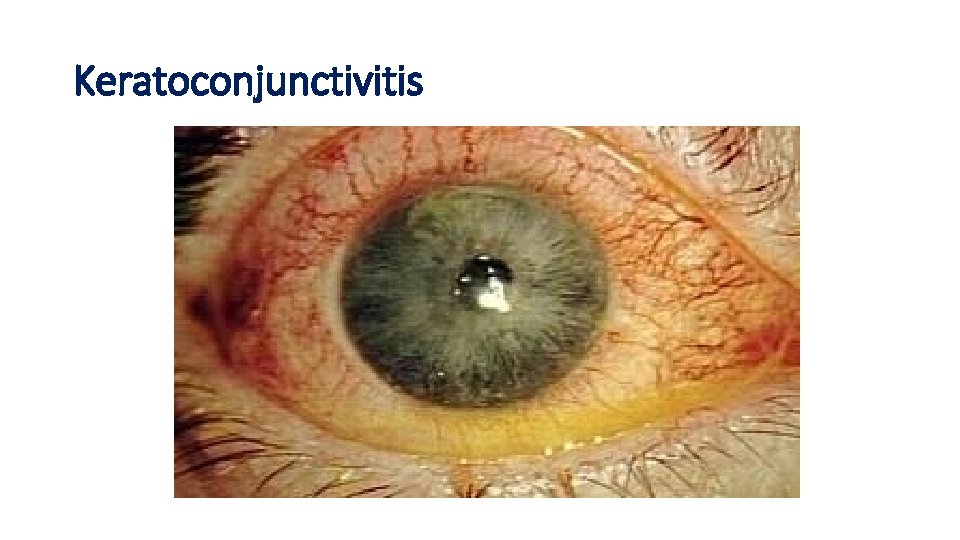
Keratoconjunctivitis
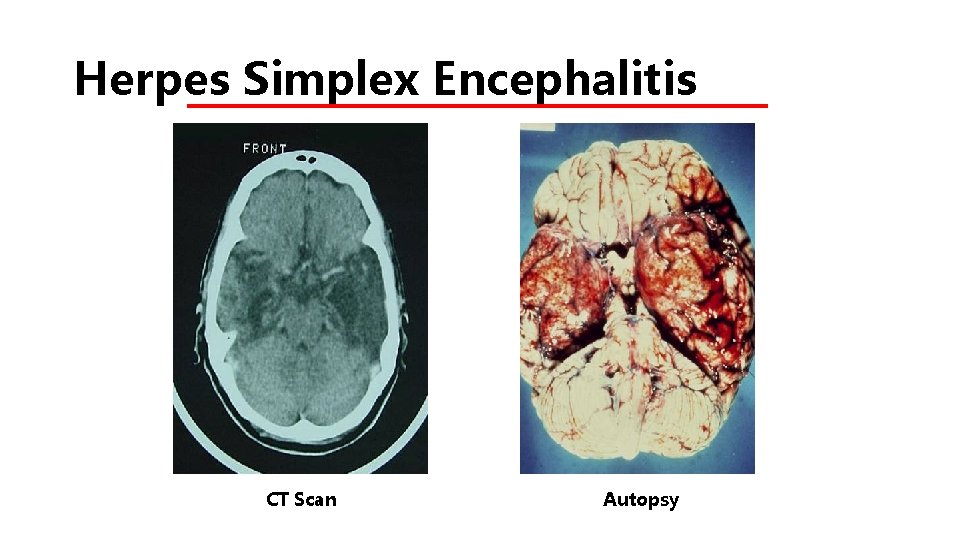
HERPES SIMPLEX ENCEPHALITIS • One of the most serious complications of herpes simplex disease. • There are two forms:
1. Neonatal – global involvement and the brain is almost liquefied mortality rate approaches 100%. 2. Focal disease – • Temporal lobe is most commonly affected. • In children and adults • Many arise from reactivation of virus. • Mortality rate is high (70%) in untreated
• Early diagnosis and treatment of HSE is very essential. • IV acyclovir is recommended in all cases of suspected HSE before laboratory results are available. 2/25/2021 25
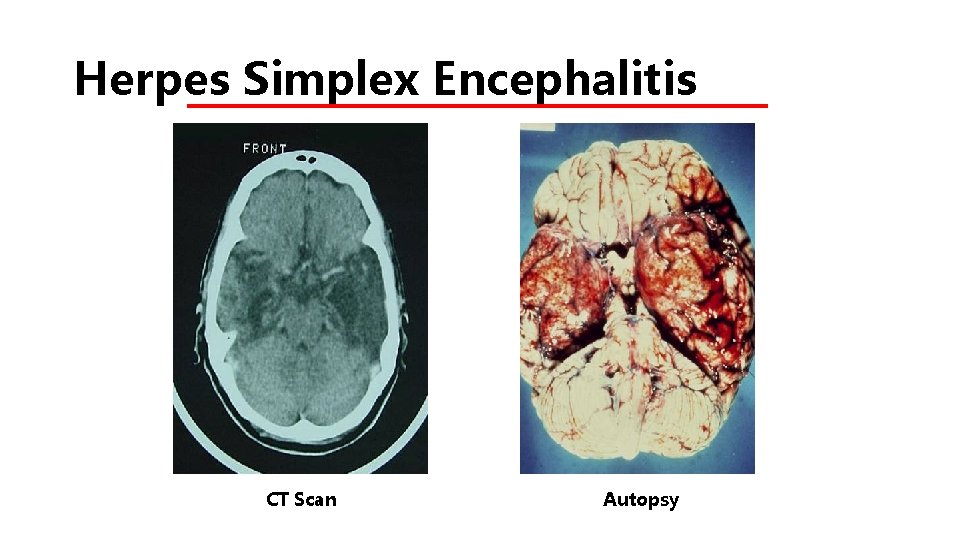
Herpes Simplex Encephalitis CT Scan Autopsy
MENINGITIS • Most commonly with primary HSV-2 infection; less likely with recurrences of genital herpes • Benign, self-limited (contrast with encephalitis) • Usually affects sexually active young adults • No neurologic sequelae
GENITAL HERPES • Genital lesions may be primary, recurrent • Sites: penis, vagina, cervix, anus, vulva, bladder, the sacral nerve routes, the spinal and the meninges. • Prone to secondary infection eg. Staphylococcus aureus, Streptococcus group, Trichomonas and Candida albicans.
GENITAL HERPES • Dysuria is a common complaint, • Recurrences in 60%. • Recurrent lesions in the perianal area more numerous and persists longer.

HSV – CONGENITAL/PERINATAL • Perinatal infection: • ¾ th are due to HSV 2 acquired during delivery • Post natal infection • HSV-1 acquired from maternal genital, oral or breast lesions or nosocomial infection from other infected babies

HERPETIC WHITLOW • A lesion (whitlow) on a finger or thumb caused by the herpes simplex virus. • HSV-1 or HSV-2. • HSV-1 whitlow is often contracted by health care workers dental workers and medical workers exposed to oral secretions.

Laboratory Diagnosis • Direct Detection § Electron microscopy of vesicle fluid - rapid result § Immunofluorescence of skin scrappings distinguish between HSV and VZV

HHV 1& 2 Diagnosis • Multinucleate Giant cells – Tzanck’s smear 2/25/2021 35

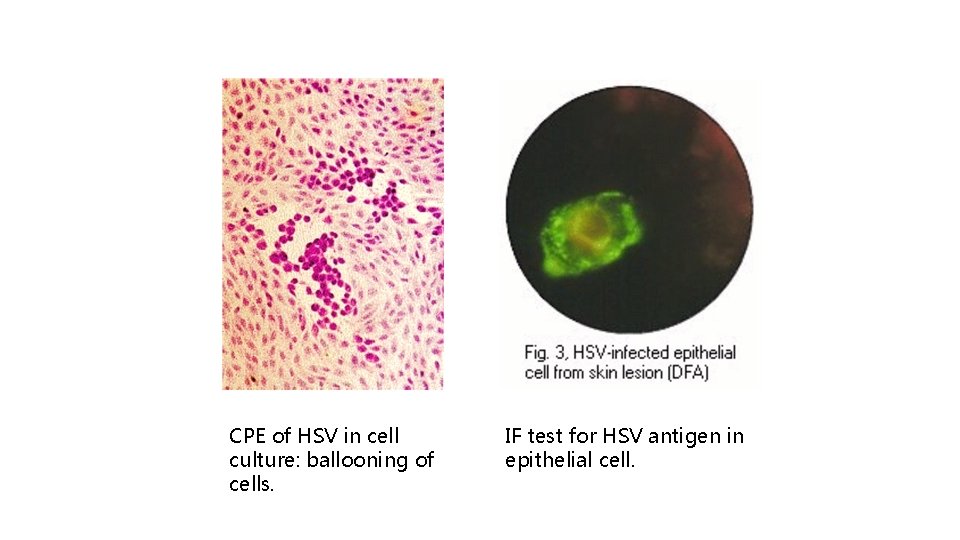
Laboratory Diagnosis • Viral culture (gold standard) • Preferred test in genital ulcers or mucocutaneous lesions Highly specific (>99%) • Sensitivity declines rapidly as lesions begin to heal • Positive more in primary infection (80%– 90%) than with recurrences (30%)
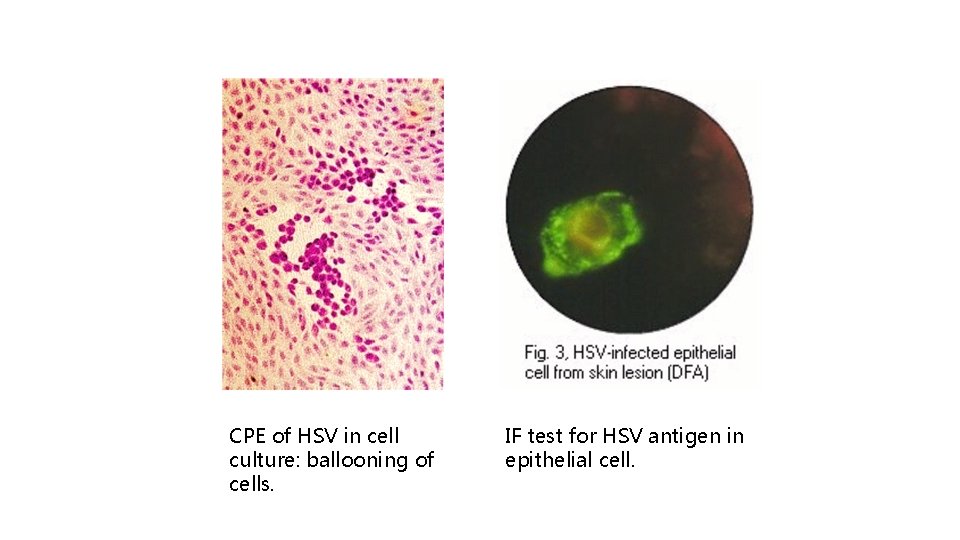
CPE of HSV in cell culture: ballooning of cells. IF test for HSV antigen in epithelial cell.

Laboratory Diagnosis…cntd Polymerase Chain Reaction (PCR) • More sensitive than viral culture; has been used instead of culture in some settings not widely available • Preferred test for detecting HSV in spinal fluid (Routinely used in HSE)
Serology • Type-specific and nonspecific antibodies • Anti HSV-2 antibody indicates anogenital infection • Anti HSV-1 antibody does not distinguish anogenital from orolabial infection • Ig. G, Ig. M - ELISA 39
ANTIVIRAL Several antivirals available for treatment of the conditions: • Aciclovir (acyclovir), • Valaciclovir (valacyclovir), • Famciclovir, • Penciclovir.

Varicella zoster
VARICELLA • Primary infection results in varicella (chickenpox) • Incubation period : 14 -21 days • Presents fever, lymphadadenopathy. a widespread vesicular rash. • Diagnosis can be made on clinical grounds alone.
• Complications are rare occurs more frequently and with greater severity in • Adults • Immunocompromised persons • MC complication is secondary bacterial infection. • Life threatening complications Viral pneumonia, Encephalititis, Haemorrhagic chickenpox.

NEONATAL VARICELLA • VZV can cross the placenta in the late stages of pregnancy to infect the fetus congenitally. • Mild disease to fatal disseminated infection. • If rash in mother occurs more than 1 week before delivery sufficient immunity is transferred to the fetus.
LABORATORY DIAGNOSIS • C/Fs of varicella or Herpes zoster are characteristic laboratory confirmation is rarely required. • Laboratory diagnosis for atypical presentations (as seen in immunocompromised patients)
LABORATORY DIAGNOSIS…. cntd • Direct detection - electron microscopy (no d/d between HSV and VZV). • IF on skin scrapings can distinguish the 2 • VZV Ig. G is indicative of past infection and immunity. Ig. M is indicative of recent primary infection. • Virus Isolation - rarely carried requires 2 -3 weeks for a results.
HERPES ZOSTER (Shingles) • Manifestation of recurrent infection following a primary attack of chicken pox. • Caused by varicella zoster • Unlike herpes labialis repeated recurrences of zoster are uncommon. • Infection typically affect adult of middle aged group
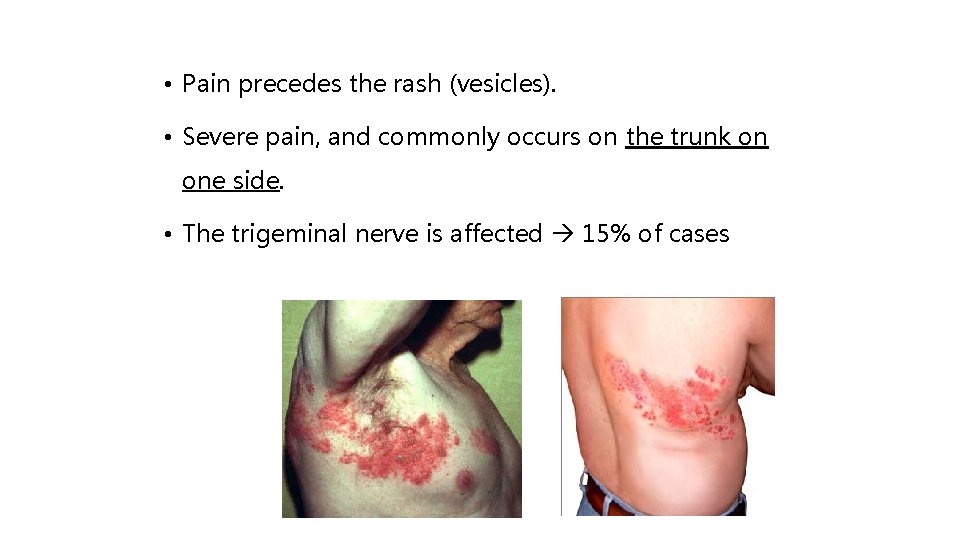
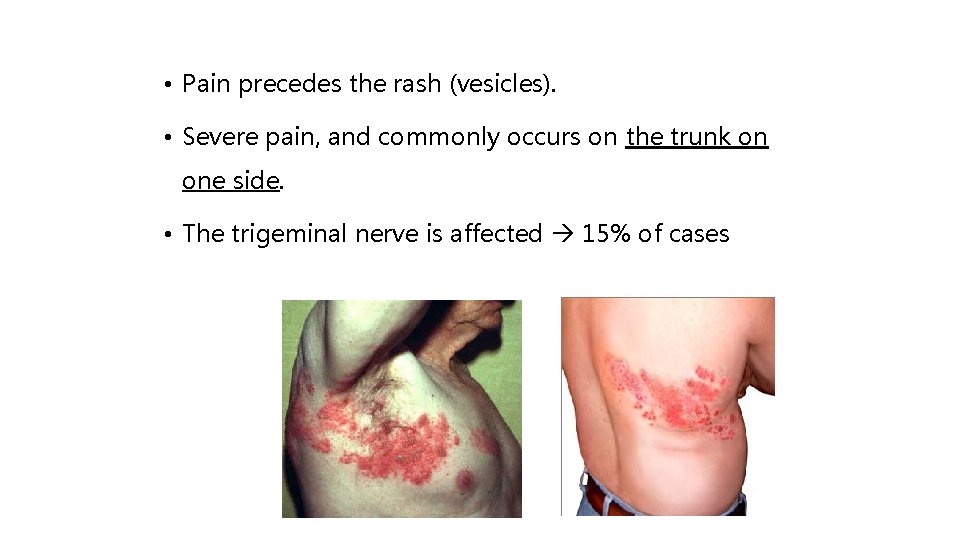
• Pain precedes the rash (vesicles). • Severe pain, and commonly occurs on the trunk on one side. • The trigeminal nerve is affected 15% of cases
• Lesions localized to one side, along distribution of nerve (e. g. any divisions of the trigeminal nerve up to the midline) • Malaise can be severe. • Regional lymph node are enlarged and can be lifethreatening in HIV disease.
TREATMENT Only in severe cases : • Oral acyclovir 800 mg five times daily for 7 -10 + analgesic.
RAMSAY HUNT SYNDROME Involvement of facial nerve with VZV • Facial nerve palsy • Vesicles in external auditory meatus • Vesicles on palate • Symptoms : dizziness, loss of taste. • Usually self limiting condition rarely permanent facial weakness may remain.

Clinical case scenario A 21 years old female presented with a complaint of malaise and loss of appetite X 1 month and sore throat and fever (especially in afternoon) since 5 days. O/E: Cervical hepatosplenomegaly+. Mononuclear lymphadenopathy+, CBC lymphocytosis showed (mostly Mild Absolute atypical lymphocytes). Her serum was tested by Monospot where Ig. M was positive. 2/25/2021 Diagnosis? 53
Diagnosis • Human Herpes Virus 4 (HHV-4) / Epstein Barr virus infection • Infectious mononucleosis / Glandular fever/ Kissing’s disease 2/25/2021 54

HHV 4 Ebstein Barr virus - EBV 2/25/2021 55

EBV or HHV-4 • 1964 – Epstein, Barr and Achong – identified a new type of herpes virus EB virus affecting B lymphocyte lineage. • CD 21 receptors necessary for acquiring EBV infection 2/25/2021 56
EBV EPIDEMIOLOGY • Source of infection: Saliva of infected persons – • Not highly contagious, droplets and aerosols not effective in disease transmission • Intimate oral contact (as in kissing) – predominant mode of transmission – hence the name ‘Kissing disease’ 2/25/2021 57
EBV – Clinical spectrum • Infectious mononucleosis • EBV associated malignancies: • Burkitt’s lymphoma • Lymphomas in immunodeficient persons e. g. AIDS & transplant recipients • Nasopharyngeal carcinoma in East Asia/China 2/25/2021 58
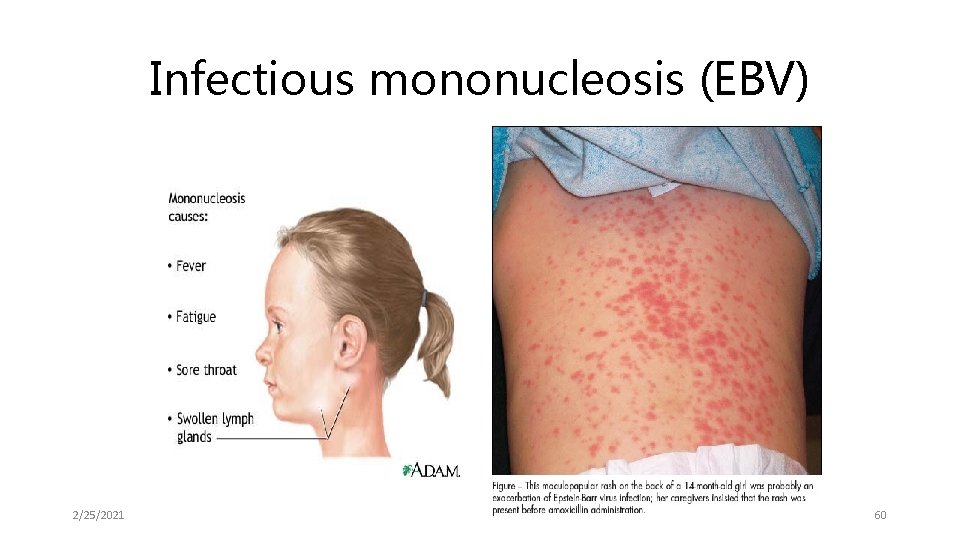
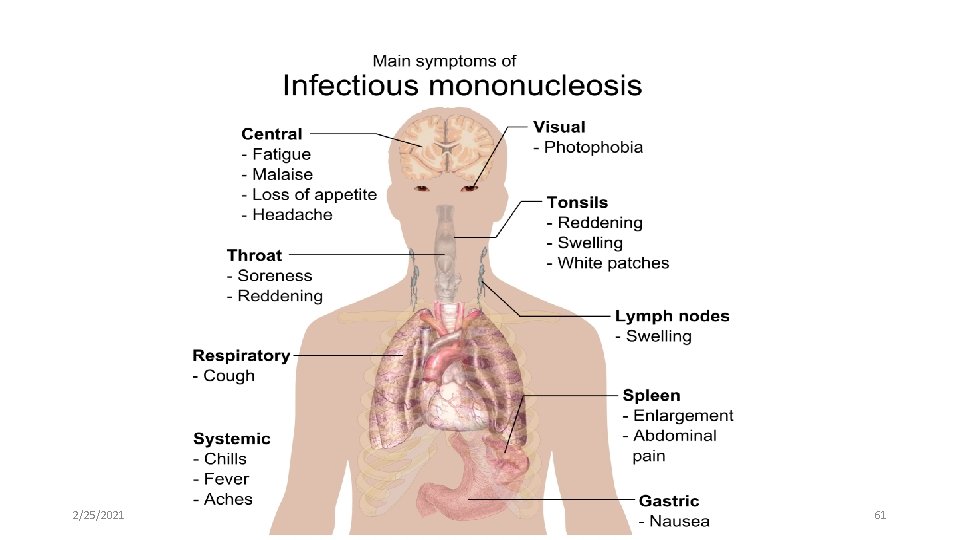
Infectious mononucleosis • Glandular fever • Acute self-limited illness • Usually seen in non-immune young adults following primary infection with EBV • Incubation period: 4 -8 weeks. 2/25/2021 59
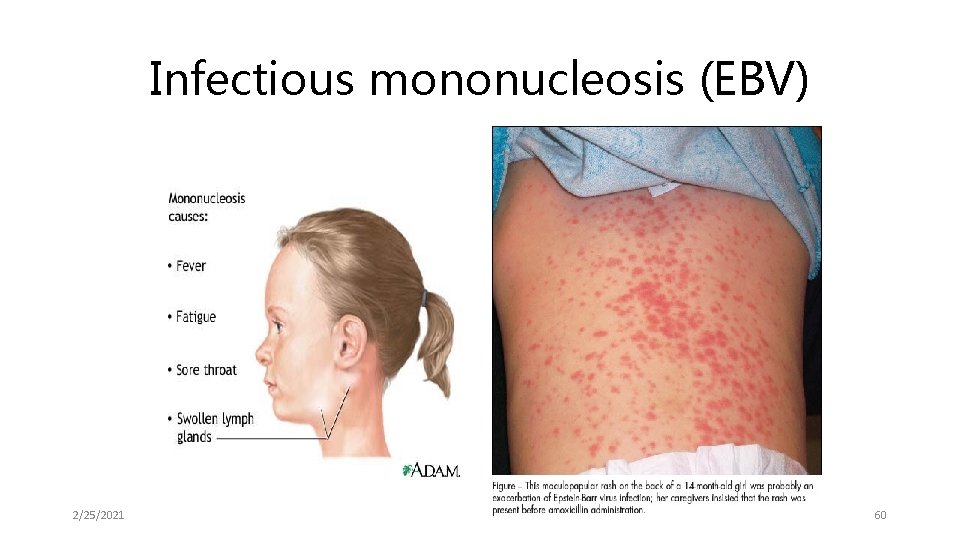
Infectious mononucleosis (EBV) 2/25/2021 60
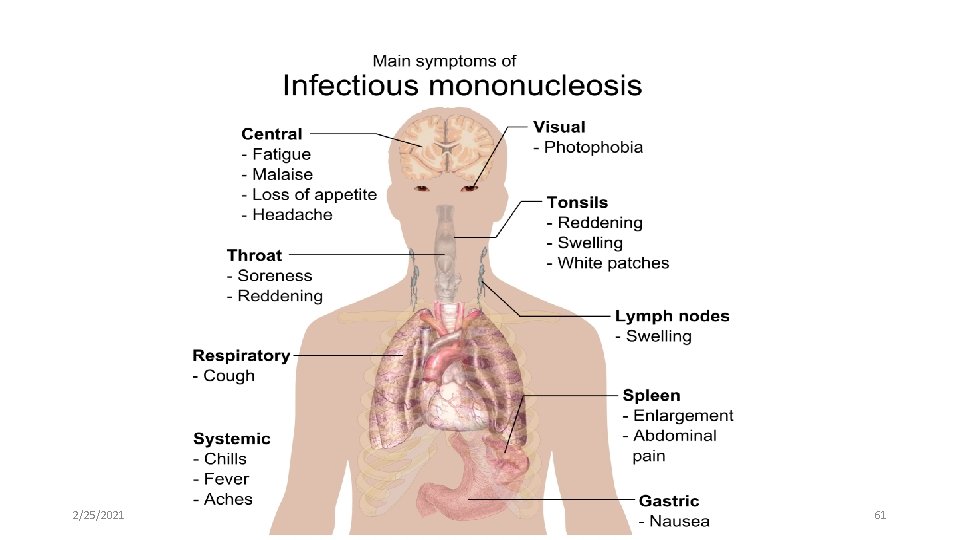
2/25/2021 61
Infectious mononucleosis • Ampicillin Rx may lead to develop maculopapular rash • May associate sub-clinical Hepatitis • Complications: Hematological, Neurological, Cardiac & Pulmonary conditions and Splenic rupture • Spontaneous resolution occurs in 2 -4 weeks 2/25/2021 62
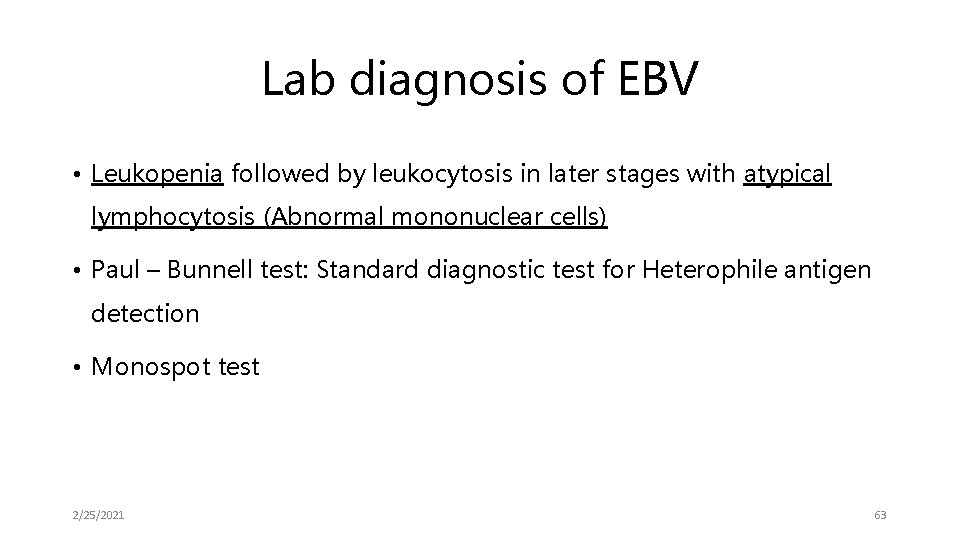
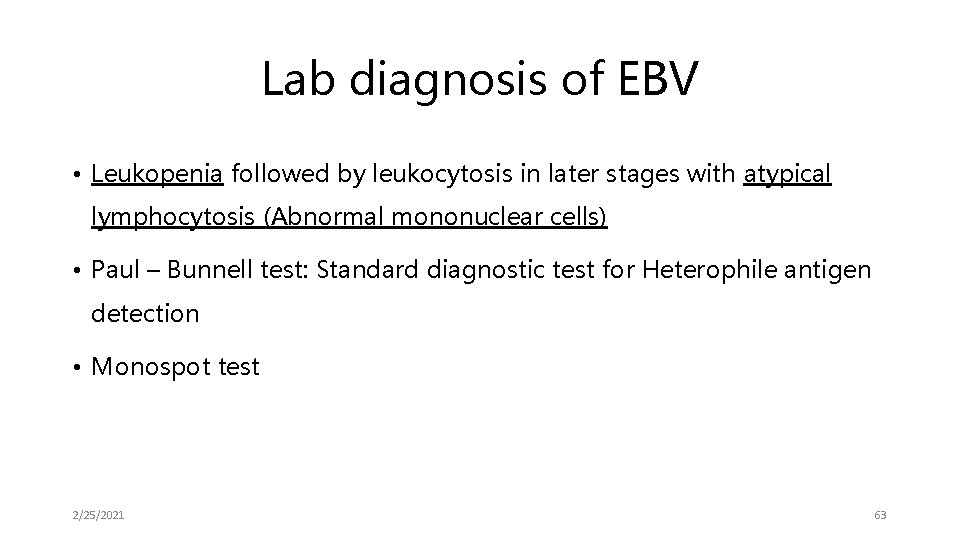
Lab diagnosis of EBV • Leukopenia followed by leukocytosis in later stages with atypical lymphocytosis (Abnormal mononuclear cells) • Paul – Bunnell test: Standard diagnostic test for Heterophile antigen detection • Monospot test 2/25/2021 63
Lab diagnosis of EBV cont. . • Differential agglutination test: Differential absorption of Agglutinins with Ox red cells and Guinea pig kidney cells • Immunofluorescence • ELISA 2/25/2021 64
Lab diagnosis of EBV cont… • Ig. M antibody to VCA (Viral Capsid Antigen) indication of primary infection • EB Nuclear Antigen (EBNA) is also a useful marker of primary infection • Ab to Early antigens (EA) high in EB-associated lymphomas 2/25/2021 65
Case scenario A 27 years old male a K/C/O HIV/AIDS presented to Ophthalmology OPD with Progressive diminution of vision X 3 months. CD 4 counts<100 cells/mm 3. Fundus examination: Fluffy retinal infiltrates+ Multiple hemorrhages+ Serological tests positive for Ig. G antibodies and PCR were positive for DNA (Herpes group). Diagnosis? Rx 2/25/2021 66

DIAGNOSIS • CMV retinitis made • Patient was started on Ganciclovir. • Note: Patient did not take Anti-HIV medications regularly. …to be initiated urgently 2/25/2021 67

Thanks …. . to be continued to next class 2/25/2021 68
 Lytic cycle animation
Lytic cycle animation Youtube . com / watch v = roxnvcaezjs
Youtube . com / watch v = roxnvcaezjs Dr deepjyoti kalita
Dr deepjyoti kalita Herpes simplex virus
Herpes simplex virus Herpes hsv2
Herpes hsv2 Herpes simpleksserotipe 2
Herpes simpleksserotipe 2 Herpes genital
Herpes genital Mulluscum
Mulluscum Genial herpes
Genial herpes Herpes latency
Herpes latency Herpes zoster
Herpes zoster Historia natural de herpes genital
Historia natural de herpes genital Varicela la adulti etape
Varicela la adulti etape Glosita micotica
Glosita micotica Herpes zoster infection
Herpes zoster infection Tuba fallopi berfungsi
Tuba fallopi berfungsi Indurerat
Indurerat Papilomavírus humano
Papilomavírus humano Rhinopneumonitis definition
Rhinopneumonitis definition Herpes rugbiorum
Herpes rugbiorum Herpes zoster clasificacion
Herpes zoster clasificacion Aciclovir varicela copii
Aciclovir varicela copii Zostavax reconstitution
Zostavax reconstitution Arterias helicinas mujer
Arterias helicinas mujer Corrimento líquido como água
Corrimento líquido como água Herpes genital agente causal
Herpes genital agente causal Herpes simplex virus 2
Herpes simplex virus 2 Ectima
Ectima Herpes genital glande
Herpes genital glande Herpes simpleksserotipe 2
Herpes simpleksserotipe 2 Hsv encephalitis
Hsv encephalitis Iridocyctitis
Iridocyctitis Simplex
Simplex Herpes simplex
Herpes simplex Bryonia 5ch posologia
Bryonia 5ch posologia Human herpesvirus 2
Human herpesvirus 2 Herpes genitalis gravid
Herpes genitalis gravid Glositis intersticial
Glositis intersticial Basic properties of viruses
Basic properties of viruses Parts of a virus
Parts of a virus Best viruses
Best viruses Hepatotropic viruses
Hepatotropic viruses Virus taxonomy
Virus taxonomy Are viruses alive yes or no
Are viruses alive yes or no Viruses are the smallest infectious agents
Viruses are the smallest infectious agents General characteristics of viruses
General characteristics of viruses General properties of viruses
General properties of viruses Importance of viruses
Importance of viruses Helical virus
Helical virus Cultivation of viruses
Cultivation of viruses Chapter 20 viruses and prokaryotes
Chapter 20 viruses and prokaryotes Tcid
Tcid Viruses video
Viruses video Milad haddad
Milad haddad Study guide chapter 18 section 1 bacteria
Study guide chapter 18 section 1 bacteria Importance of viruses
Importance of viruses Viruses
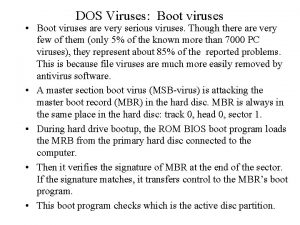
Viruses Computer viruses presentation
Computer viruses presentation Virus
Virus Baltimore classification of virus
Baltimore classification of virus What kingdom do viruses belong to
What kingdom do viruses belong to Hepatotropic viruses
Hepatotropic viruses Blood borne viruses
Blood borne viruses Section 1 studying viruses and prokaryotes
Section 1 studying viruses and prokaryotes Why are viruses considered nonliving?
Why are viruses considered nonliving? Properties of viruses
Properties of viruses Chapter 20 viruses and prokaryotes
Chapter 20 viruses and prokaryotes Replication of viruses
Replication of viruses Lytic infection
Lytic infection