http www youtube comwatch v7 TWu 0Gklzofeaturerelated ECG
http: //www. youtube. com/watch? v=7 TWu 0_Gklzo&feature=related

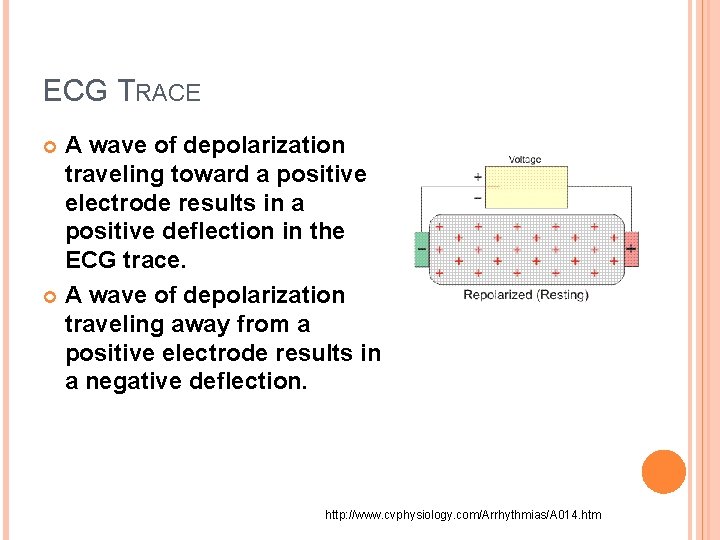
ECG TRACE A wave of depolarization traveling toward a positive electrode results in a positive deflection in the ECG trace. A wave of depolarization traveling away from a positive electrode results in a negative deflection. http: //www. cvphysiology. com/Arrhythmias/A 014. htm
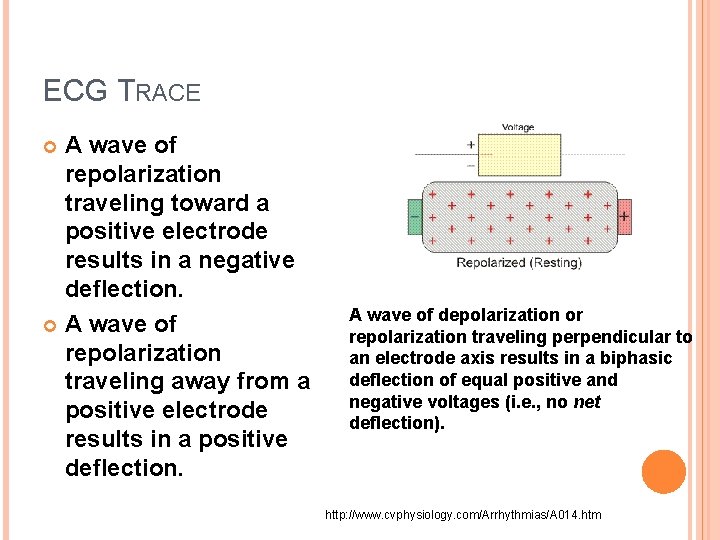
ECG TRACE A wave of repolarization traveling toward a positive electrode results in a negative deflection. A wave of repolarization traveling away from a positive electrode results in a positive deflection. A wave of depolarization or repolarization traveling perpendicular to an electrode axis results in a biphasic deflection of equal positive and negative voltages (i. e. , no net deflection). http: //www. cvphysiology. com/Arrhythmias/A 014. htm

VECTORS The instantaneous amplitude of the measured potentials depends upon the orientation of the positive electrode relative to the mean electrical vector. The voltage amplitude is directly related to the mass of tissue undergoing depolarization or repolarization • Each arrow represents a different individual vector representing depolarization. • The mean electrical vector for all the individual vectors is also shown in the figure (red arrow). • This mean electrical vector represents the sum of all of the individual vectors at a given instant in time.
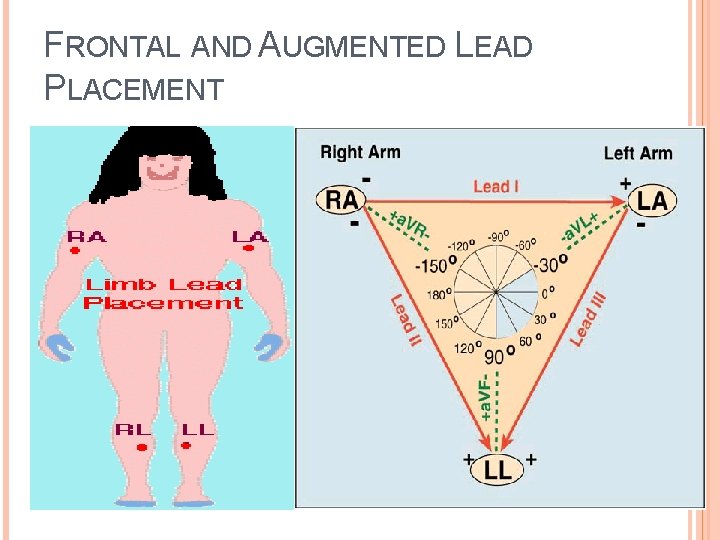
FRONTAL AND AUGMENTED LEAD PLACEMENT
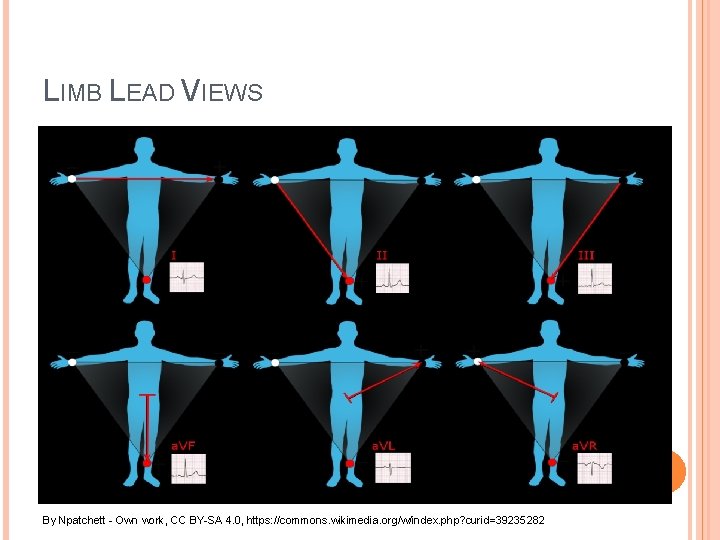
LIMB LEAD VIEWS By Npatchett - Own work, CC BY-SA 4. 0, https: //commons. wikimedia. org/w/index. php? curid=39235282
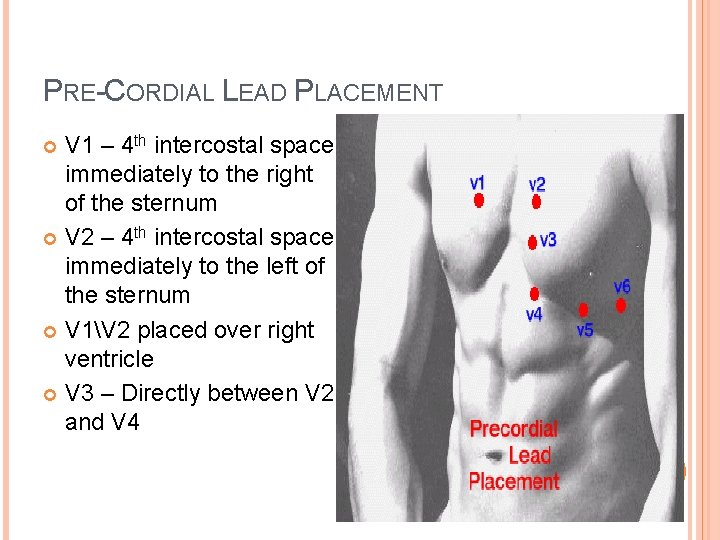
PRE-CORDIAL LEAD PLACEMENT V 1 – 4 th intercostal space immediately to the right of the sternum V 2 – 4 th intercostal space immediately to the left of the sternum V 1V 2 placed over right ventricle V 3 – Directly between V 2 and V 4
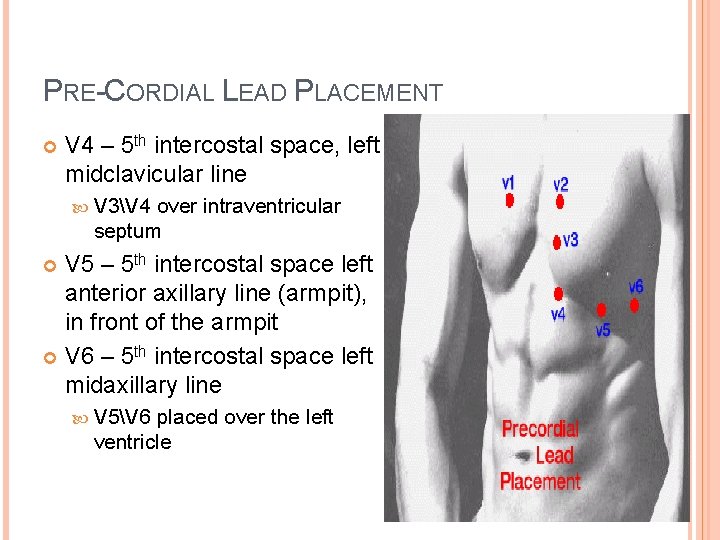
PRE-CORDIAL LEAD PLACEMENT V 4 – 5 th intercostal space, left midclavicular line V 3V 4 over intraventricular septum V 5 – 5 th intercostal space left anterior axillary line (armpit), in front of the armpit V 6 – 5 th intercostal space left midaxillary line V 5V 6 placed over the left ventricle

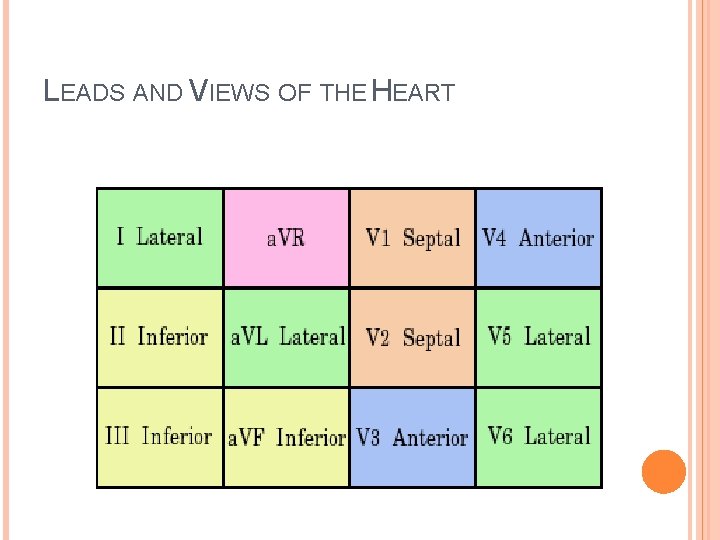
LEADS AND VIEWS OF THE HEART
ECG INTERPRETATION BASICS
OUTLINE OF 12 LEAD INTERPRETATION Rate Rhythm R-R regularity Check Intervals: PR (. 12 -. 20 s), QT depends on HR Check P wave (<. 12 s) and QRS (. 04 -. 11 s) wave duration Determine QRS axis Hypertrophy (both atrial and ventricular) Ischemia, Injury, Infarction Examine ST segment for elevation (Injury) or depression (ischemia) Look for Q waves determine if they are pathologic (sign of resolving infarction) Check the T waves
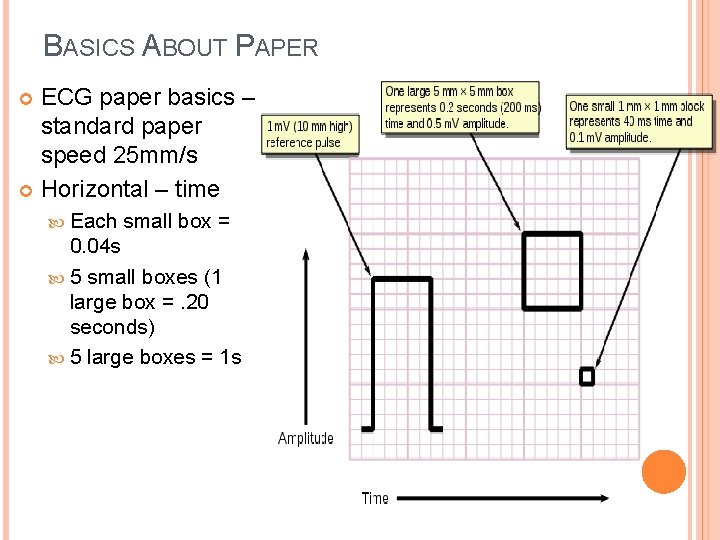
BASICS ABOUT PAPER ECG paper basics – standard paper speed 25 mm/s Horizontal – time Each small box = 0. 04 s 5 small boxes (1 large box =. 20 seconds) 5 large boxes = 1 s
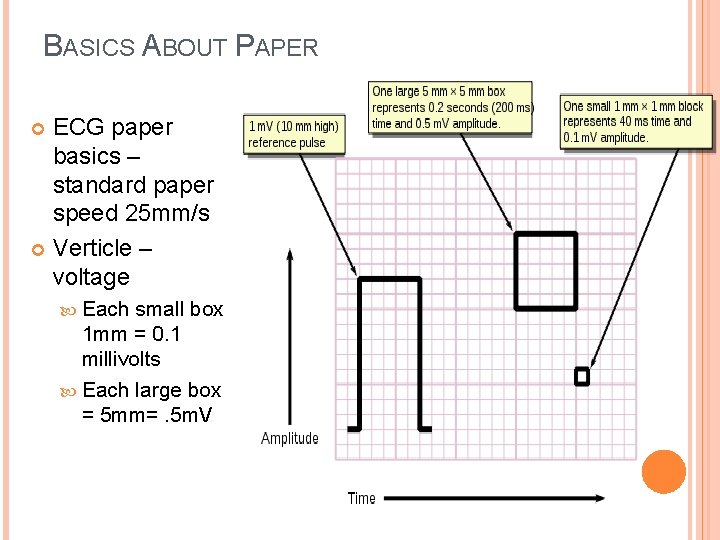
BASICS ABOUT PAPER ECG paper basics – standard paper speed 25 mm/s Verticle – voltage Each small box 1 mm = 0. 1 millivolts Each large box = 5 mm=. 5 m. V
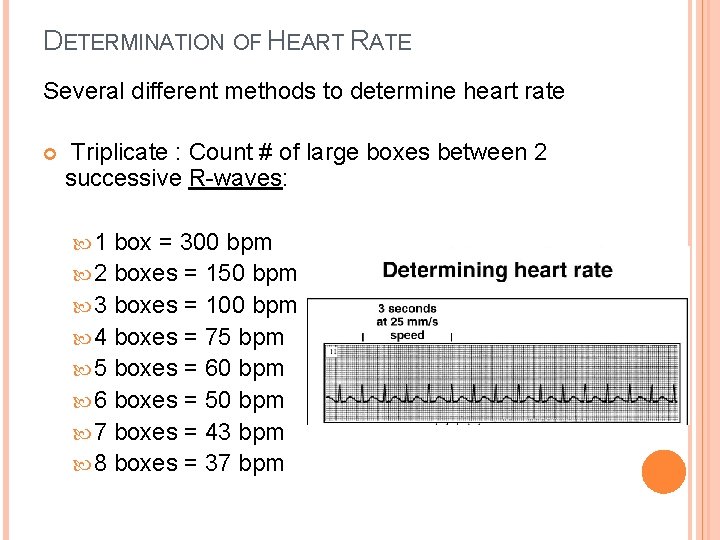
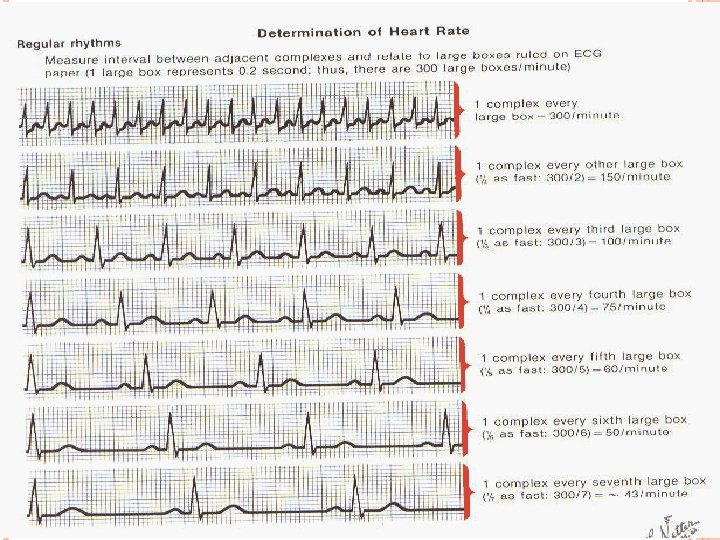
DETERMINATION OF HEART RATE Several different methods to determine heart rate Triplicate : Count # of large boxes between 2 successive R-waves: 1 box = 300 bpm 2 boxes = 150 bpm 3 boxes = 100 bpm 4 boxes = 75 bpm 5 boxes = 60 bpm 6 boxes = 50 bpm 7 boxes = 43 bpm 8 boxes = 37 bpm
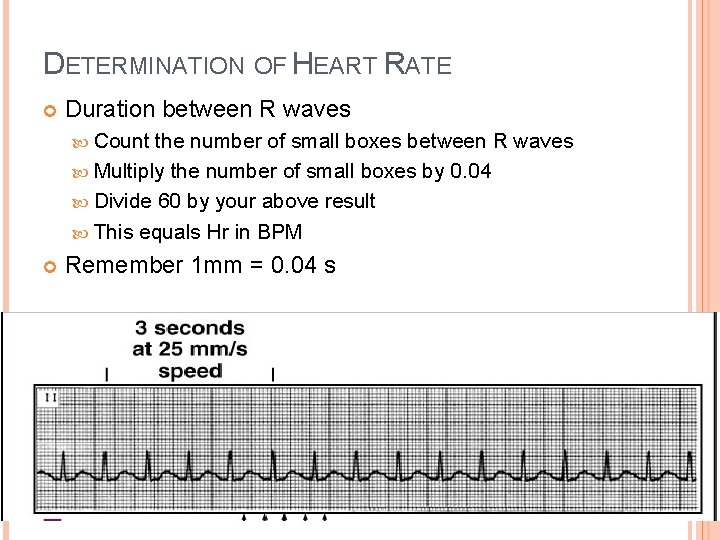
DETERMINATION OF HEART RATE Duration between R waves Count the number of small boxes between R waves Multiply the number of small boxes by 0. 04 Divide 60 by your above result This equals Hr in BPM Remember 1 mm = 0. 04 s
DETERMINATION OF RHYTHM
DETERMINATION OF HEART RHYTHM Rhythm – most difficult in determination and interpretation Arrhythmia – abnormal or inconsistent cardiac rhythms Determined by rhythm strip – measure R-R interval if it is consistent then rhythm is regular, if not then have arrhythmia NSR originates at the SA node
DETERMINING THE RATE FOR IRREGULAR RHYTHMS If the R-R Interval is irregular: Count the number of QRS complexes in a 10 sec span (that is on the entire EKG) and multiply it by 6! {or no. of QRS complexes in a 6 sec span multiplied by 10}

DETERMINATION OF HEART RHYTHM
SINUS RHYTHM…OR NOT! First ALWAYS determine whether the rhythm is Sinus or Non-Sinus. Look at P waves. Every QRS is preceded by a P-waves appear normal, that is they are of sinus node origin: A. Normal Morphology: 1. P-wave duration < 0. 12 sec (< 3 boxes) 2. P-wave height < 2. 5 mm B. Normal Axis – upright P-waves in lead II
DETERMINING THE CARDIAC RHYTHM 2. Determine the Intervals: a. P-wave duration b. PR interval c. QRS interval d. QT interval
EKG INTERVALS P-wave < 0. 110 sec (approximately 3 small boxes) PR interval = beginning of the P-wave to the beginning of QRS. Normal = 0. 120 – 0. 200 sec QRS interval = from the first deflection to return to the baseline. Normal < 0. 120 sec QT interval = beginning of the QRS to the END of the T-wave. Normal < 0. 450 sec
NOT NORMAL ECGS http: //www. emedu. org/ecg_lib/index. htm http: //library. med. utah. edu/kw/ecg/
APPROACH TO EKG INTERPRETATION ALWAYS, ALWAYS: 1. Rate 2. Rhythm (includes analysis of intervals: PR, QRS, QT) 3. Axis 4. Hypertrophy 5. Ischemia, Injury, or Infarct
REMEMBER Depolarization moving to an electrode will record a positive deflection Depolarization moving away from an electrode will record a negative deflection. A wave of depolarization moving at right angles to the electrode will cause either no or a very small deflection.
P WAVES Lead II will always have the tallest P waves - P wave vector is moving directly toward it. a. VR will always have a negative P wave – P wave vector is moving away from it III and a. VL will have the smallest P wave because the mean P wave vector is moving at about a right angle to those leads. The normal P wave should not be wider that . 11 s. or taller than 2. 4 mm
VENTRICULAR DEPOLARIZATION The QRS will be the most negative in a. VR, V 1, V 2 (have a large S wave) The QRS will be the least positive in III and a. VF I, II V 3, a. VL will have positive QRS complexes V 4 -6 will have the most positive QRS The transition from a large S wave to a large R wave should occur in V 3 or V 4
VENTRICULAR REPOLARIZATION – T WAVE Positive in I, II, a. VL, V 2 -6 Variable in III and V 1 Negative in a. VR ST segment should be isoelectric – not more than 1 mm above or below the isoelectric line.
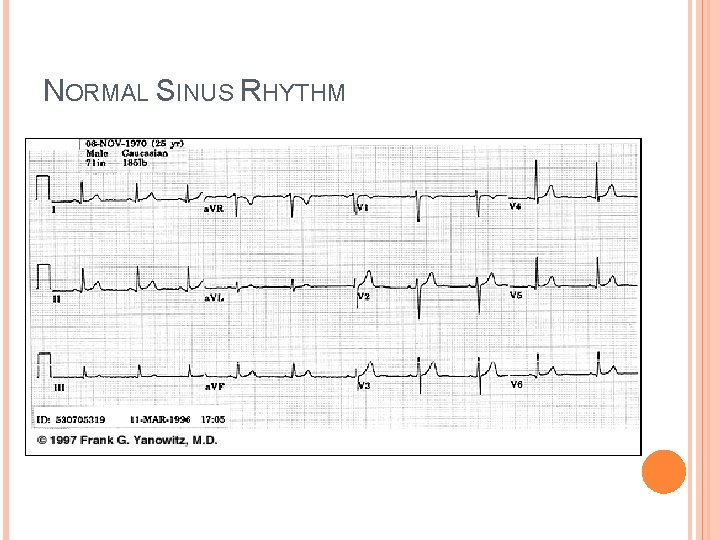
NORMAL SINUS RHYTHM
INTERPRETING RHYTHM

BLOCKS The heart is capable of sustaining its own rhythm through spontaneous depolarization at different areas of the myocardium. The rate of spontaneous depolarization of decreases down the conducting system: SA node (60 -100 bpm) Atria (< 60 bpm) AV node (40 -60 bpm) Ventricles (20 -40 bpm) The SA node rhythm normally overrides the other pacemaker sites. With Blocks this relationship is disrupted http: //lifeinthefastlane. com/ecg-library/ventricular-escape-rhythm/

1 ST DEGREE A-V BLOCK P-R interval consistently greater than. 20 s This may be caused by: Increased vagal tone Athletic training Inferior MI Mitral valve surgery Myocarditis (e. g. Lyme disease) Electrolyte disturbances (e. g. Hyperkaliemia) AV nodal blocking drugs (beta-blockers, calcium channel blockers, digoxin, amiodarone) May be a normal variant http: //lifeinthefastlane. com/ecg-library/basics/first-degree-heart-block/
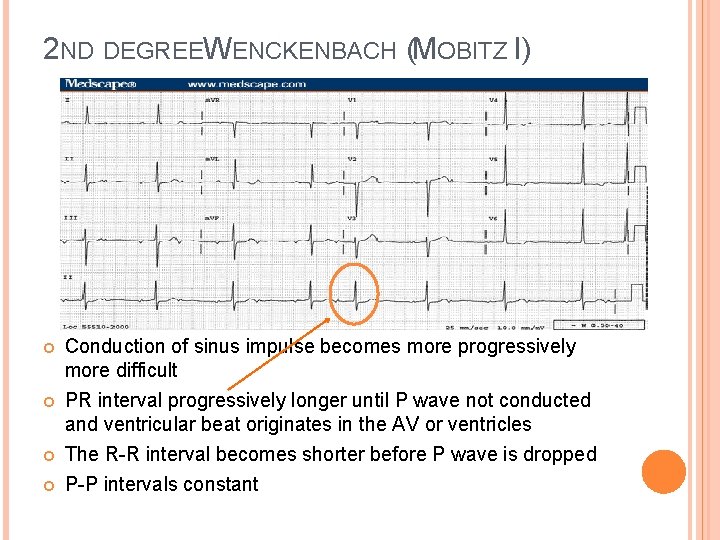
2 ND DEGREEW ENCKENBACH (MOBITZ I) Conduction of sinus impulse becomes more progressively more difficult PR interval progressively longer until P wave not conducted and ventricular beat originates in the AV or ventricles The R-R interval becomes shorter before P wave is dropped P-P intervals constant
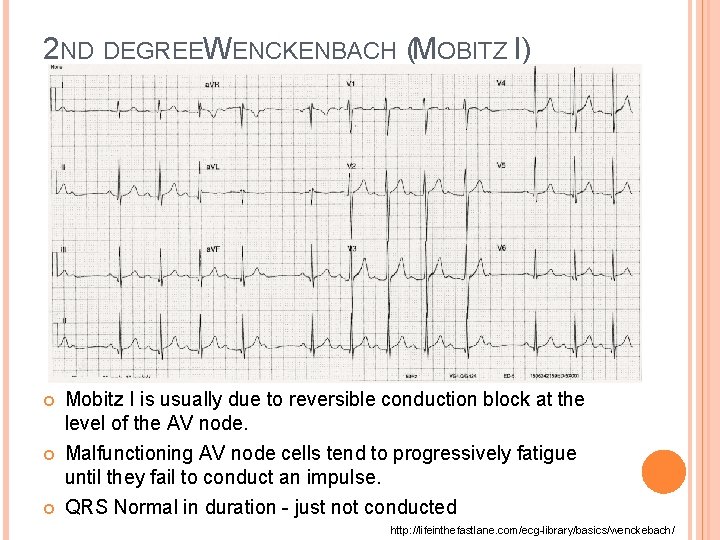
2 ND DEGREEW ENCKENBACH (MOBITZ I) Mobitz I is usually due to reversible conduction block at the level of the AV node. Malfunctioning AV node cells tend to progressively fatigue until they fail to conduct an impulse. QRS Normal in duration - just not conducted http: //lifeinthefastlane. com/ecg-library/basics/wenckebach/
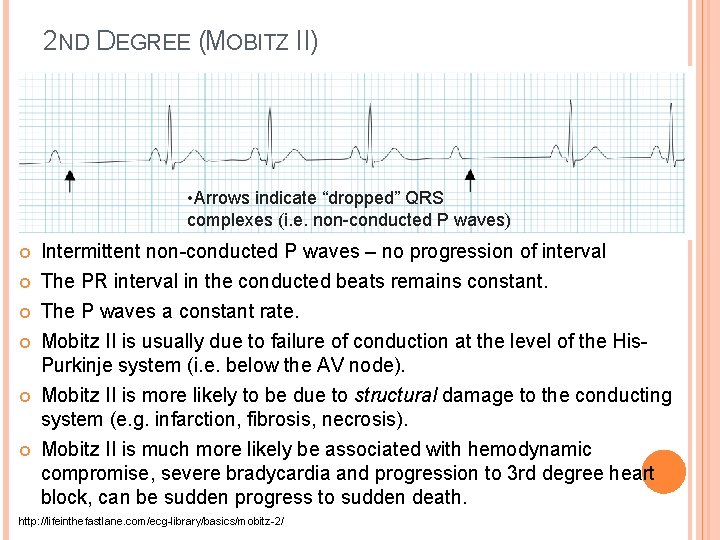
2 ND DEGREE (MOBITZ II) • Arrows indicate “dropped” QRS complexes (i. e. non-conducted P waves) Intermittent non-conducted P waves – no progression of interval The PR interval in the conducted beats remains constant. The P waves a constant rate. Mobitz II is usually due to failure of conduction at the level of the His. Purkinje system (i. e. below the AV node). Mobitz II is more likely to be due to structural damage to the conducting system (e. g. infarction, fibrosis, necrosis). Mobitz II is much more likely be associated with hemodynamic compromise, severe bradycardia and progression to 3 rd degree heart block, can be sudden progress to sudden death. http: //lifeinthefastlane. com/ecg-library/basics/mobitz-2/

3 RD DEGREE A-V BLOCK The atrial rate is approximately 100 bpm. The ventricular rate is approximately 40 bpm PR interval varies, no relationship between P to QRS No conduction between atria and ventricles Atria under control of sinus or supraventricular focus, ventricles are controlled by junctional or ventricular escape beat.

3 RD DEGREE A-V BLOCK Complete heart block is essentially the end point of either Mobitz I or Mobitz II AV block. It may be due to progressive fatigue of AV node cells as per Mobitz I Alternatively, it may be due to sudden onset of complete conduction failure throughout the His-Purkinje system, as per Mobitz II (acute anterior MI). http: //lifeinthefastlane. com/ecg-library/basics/complete-heart-block/
BUNDLE BRANCH BLOCKS Normally the septum is activated from left to right. In RBBB, activation of the right ventricle is delayed as depolarization has to spread across the septum from the left ventricle. The left ventricle is activated normally, meaning that the early part of the QRS complex is unchanged. In LBBB, the normal direction of septal depolarization is reversed (becomes right to left), as the impulse spreads first to the RV via the right bundle branch and then to the LV via the septum. This sequence of activation extends the QRS duration to > 120 ms. http: //lifeinthefastlane. com/ecg-library/basics/
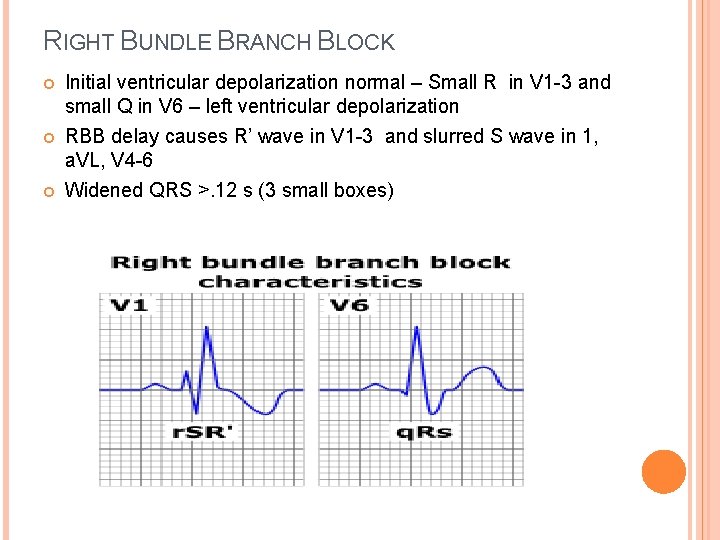
RIGHT BUNDLE BRANCH BLOCK Initial ventricular depolarization normal – Small R in V 1 -3 and small Q in V 6 – left ventricular depolarization RBB delay causes R’ wave in V 1 -3 and slurred S wave in 1, a. VL, V 4 -6 Widened QRS >. 12 s (3 small boxes)
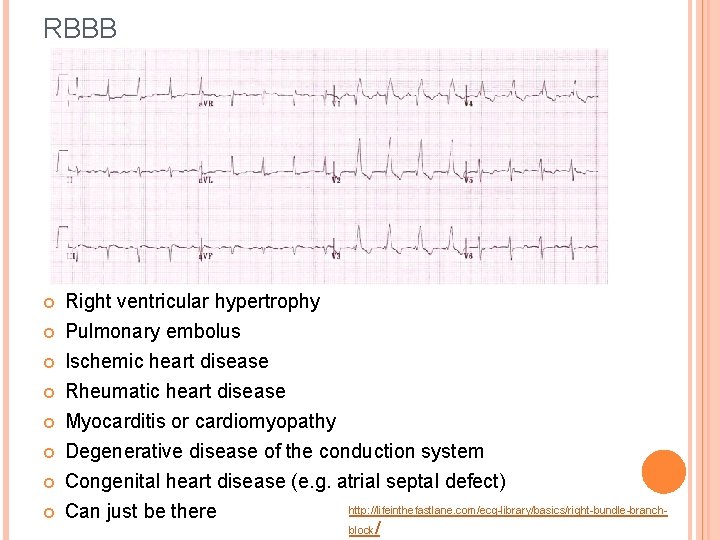
RBBB Right ventricular hypertrophy Pulmonary embolus Ischemic heart disease Rheumatic heart disease Myocarditis or cardiomyopathy Degenerative disease of the conduction system Congenital heart disease (e. g. atrial septal defect) http: //lifeinthefastlane. com/ecg-library/basics/right-bundle-branch. Can just be there block /
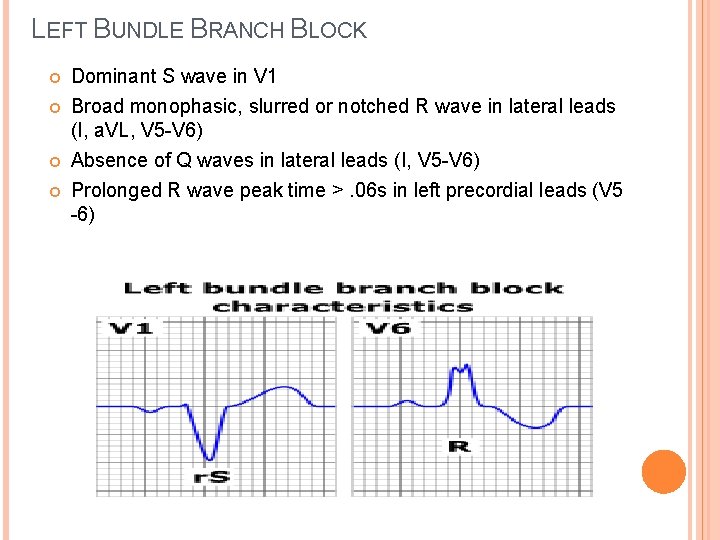
LEFT BUNDLE BRANCH BLOCK Dominant S wave in V 1 Broad monophasic, slurred or notched R wave in lateral leads (I, a. VL, V 5 -V 6) Absence of Q waves in lateral leads (I, V 5 -V 6) Prolonged R wave peak time >. 06 s in left precordial leads (V 5 -6)

LBBB Aortic stenosis Ischemic heart disease Hypertension Dilated cardiomyopathy Anterior MI Primary degenerative disease (fibrosis) of the conducting system Hyperkalaemia Digoxin toxicity
PREMATURE BEATS

ECTOPIC FOCI -AN EXCITABLE GROUP OF CELLS THAT CAUSES A PREMATURE HEART BEAT OUTSIDE THE NORMALLY FUNCTIONING SA NODE Increased local parasympathetic nervous system activity Elevated sympathetic nervous system output Overstimulation from drugs such as caffeine, digitalis and catechola mines Infection SA node dysfunction, (1 st degree block) which can cause the rate of impulse to slow. SA node blockage so that impulses never leave the atria. AV node blockage (3 rd degree block) prevents normal conduction across ventricles. Cardiac Ischemia (particularly ventricular ischemia) - The membranes of apoptotic (dying) cells become "leaky" and cause surrounding tissue to become hyperkalemic or hypercalcemic (high concentration of potassium/calcium), causing random excitation. https: //en. wikipedia. org/wiki/Ectopic_pacemaker

PREMATURE CONTRACTIONS A premature beat arising from an ectopic focus Recall: Groups of pacemaker cells throughout the conducting system are capable of spontaneous depolarization. The rate of depolarization decreases from top to bottom: fastest at the sinoatrial node (60 -100)and slowest within the ventricles (20 -40). Ectopic impulses from subsidiary pacemakers are normally suppressed by more rapid impulses from above. However, if an ectopic focus depolarizes early enough — prior to the arrival of the next sinus impulse — it may “capture” the impulse, producing a premature contraction. Premature contractions are classified by their origin — atrial (PACs), junctional (PJCs) or ventricular (PVCs).
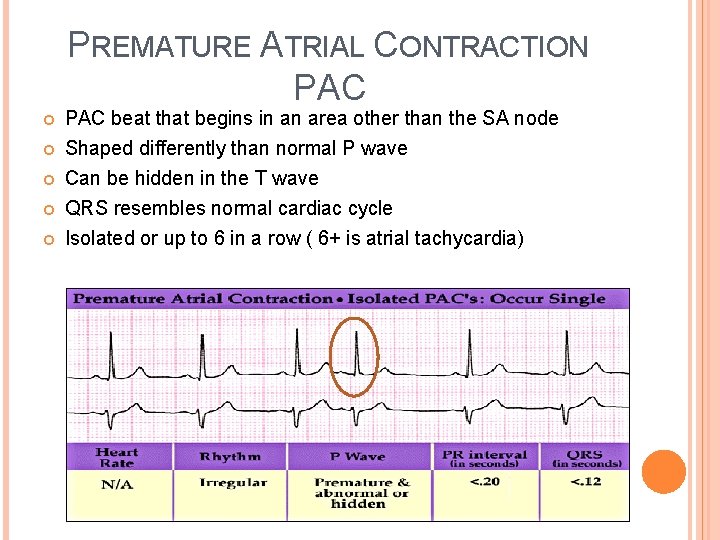
PREMATURE ATRIAL CONTRACTION PAC beat that begins in an area other than the SA node Shaped differently than normal P wave Can be hidden in the T wave QRS resembles normal cardiac cycle Isolated or up to 6 in a row ( 6+ is atrial tachycardia)
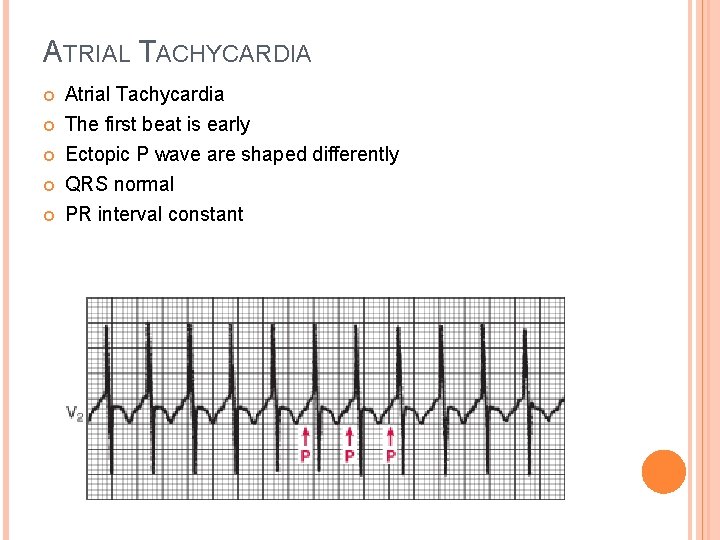
ATRIAL TACHYCARDIA Atrial Tachycardia The first beat is early Ectopic P wave are shaped differently QRS normal PR interval constant
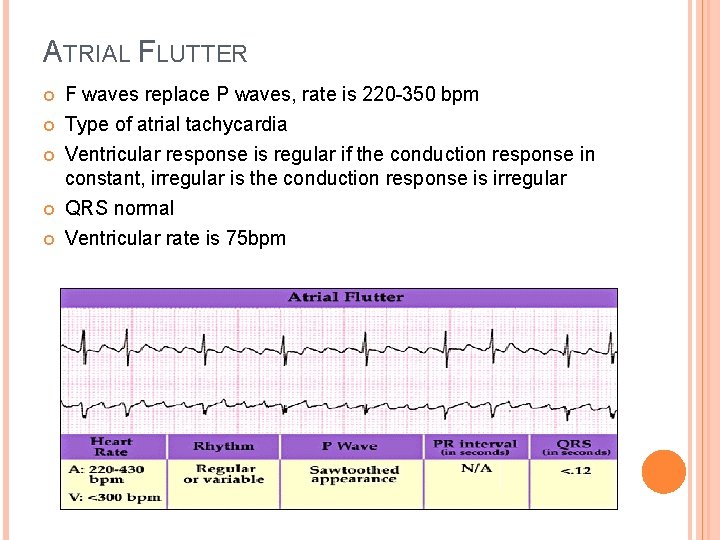
ATRIAL FLUTTER F waves replace P waves, rate is 220 -350 bpm Type of atrial tachycardia Ventricular response is regular if the conduction response in constant, irregular is the conduction response is irregular QRS normal Ventricular rate is 75 bpm
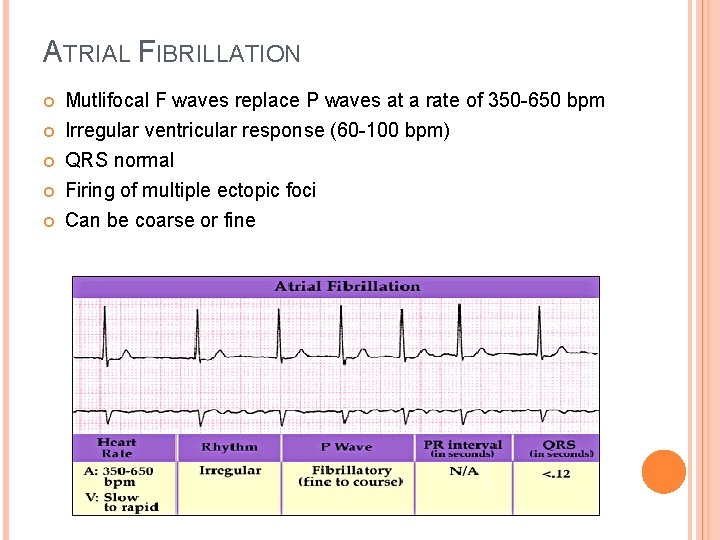
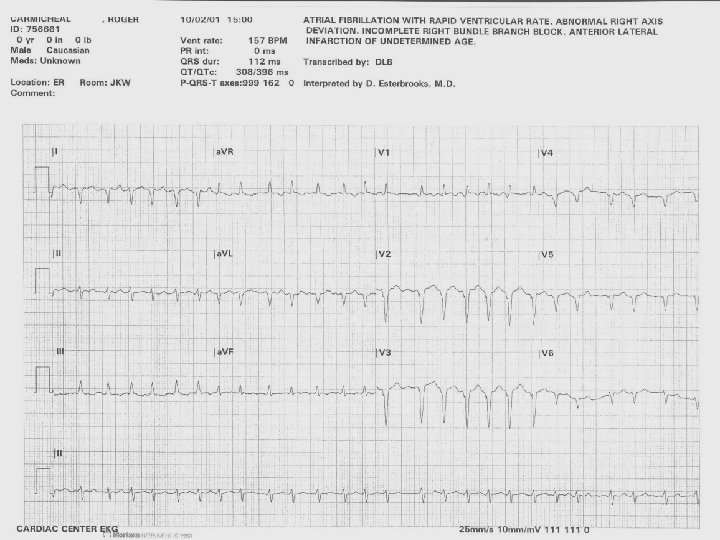
ATRIAL FIBRILLATION Mutlifocal F waves replace P waves at a rate of 350 -650 bpm Irregular ventricular response (60 -100 bpm) QRS normal Firing of multiple ectopic foci Can be coarse or fine
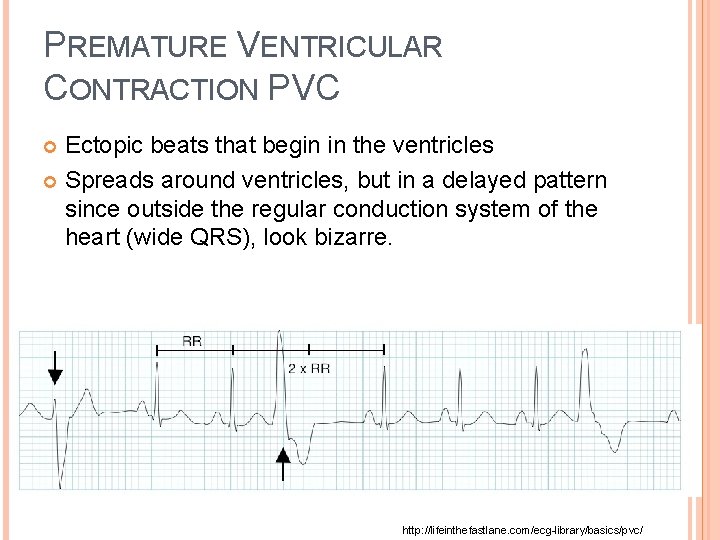
PREMATURE VENTRICULAR CONTRACTION PVC Ectopic beats that begin in the ventricles Spreads around ventricles, but in a delayed pattern since outside the regular conduction system of the heart (wide QRS), look bizarre. http: //lifeinthefastlane. com/ecg-library/basics/pvc/
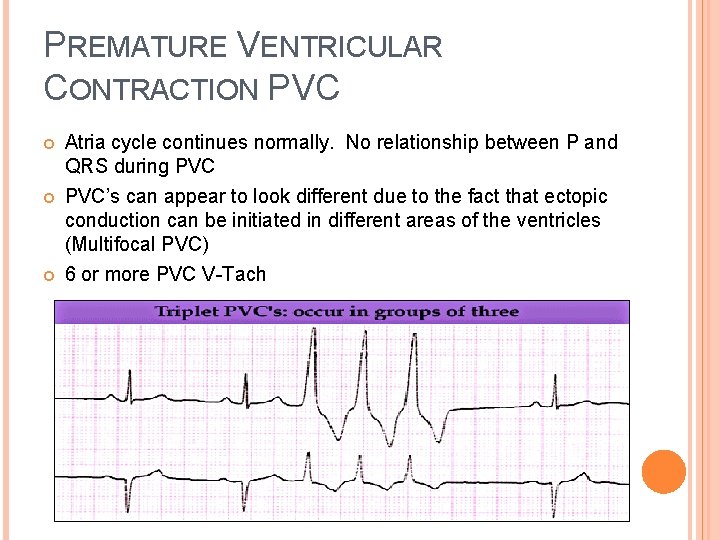
PREMATURE VENTRICULAR CONTRACTION PVC Atria cycle continues normally. No relationship between P and QRS during PVC’s can appear to look different due to the fact that ectopic conduction can be initiated in different areas of the ventricles (Multifocal PVC) 6 or more PVC V-Tach
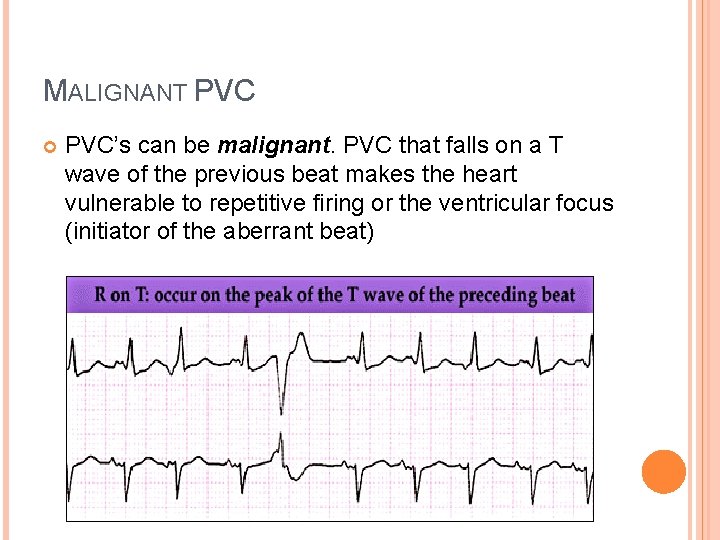
MALIGNANT PVC’s can be malignant. PVC that falls on a T wave of the previous beat makes the heart vulnerable to repetitive firing or the ventricular focus (initiator of the aberrant beat)
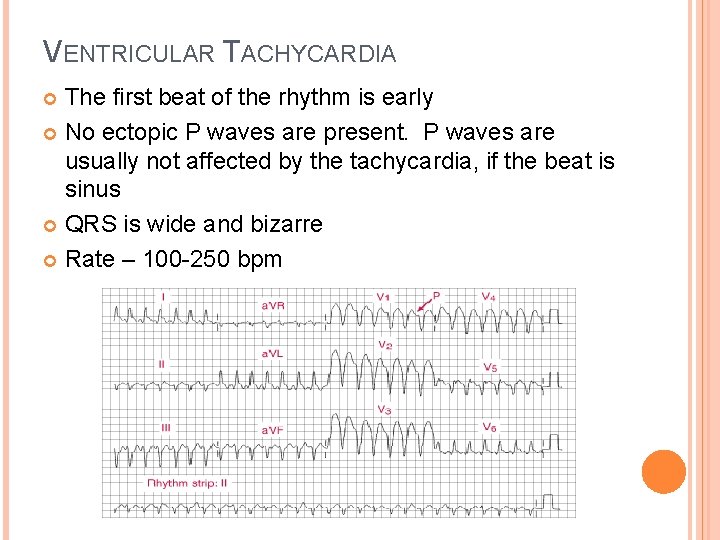
VENTRICULAR TACHYCARDIA The first beat of the rhythm is early No ectopic P waves are present. P waves are usually not affected by the tachycardia, if the beat is sinus QRS is wide and bizarre Rate – 100 -250 bpm
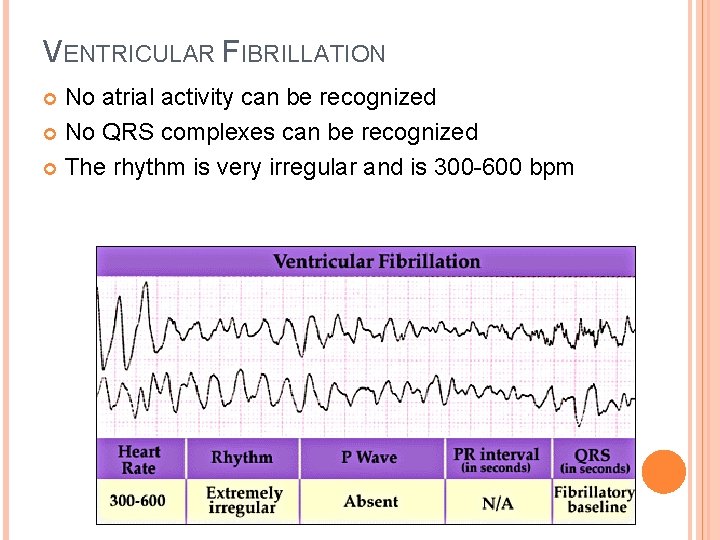
VENTRICULAR FIBRILLATION No atrial activity can be recognized No QRS complexes can be recognized The rhythm is very irregular and is 300 -600 bpm

QT INTERVAL: ECG REPOLARIZATION ABNORMALITIES Q-T interval represents the time for both ventricular depolarization and repolarization to occur Estimates the duration of an average ventricular action potential (VAT). This interval can range from 0. 2 to 0. 4 seconds depending upon heart rate. At high heart rates, ventricular action potentials shorten in duration, which decreases the Q-T interval. Because prolonged Q-T intervals can be diagnostic for susceptibility to certain types of arrhythmias, it is important to determine if a given Q-T interval is excessively long.
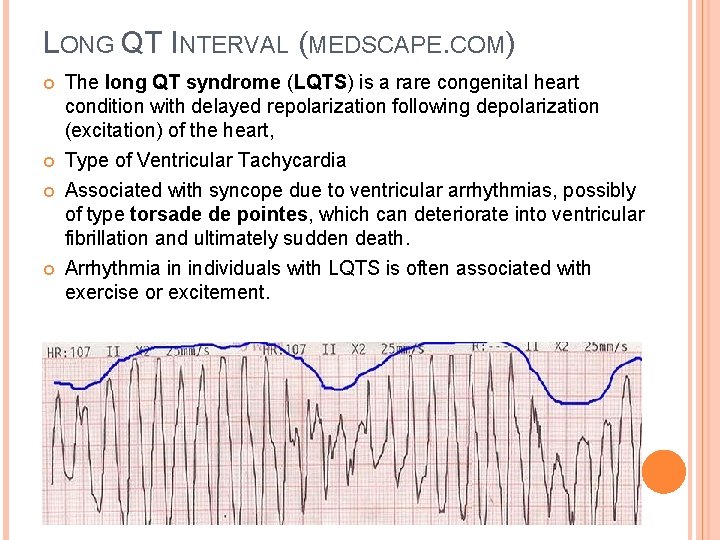
LONG QT INTERVAL (MEDSCAPE. COM) The long QT syndrome (LQTS) is a rare congenital heart condition with delayed repolarization following depolarization (excitation) of the heart, Type of Ventricular Tachycardia Associated with syncope due to ventricular arrhythmias, possibly of type torsade de pointes, which can deteriorate into ventricular fibrillation and ultimately sudden death. Arrhythmia in individuals with LQTS is often associated with exercise or excitement.
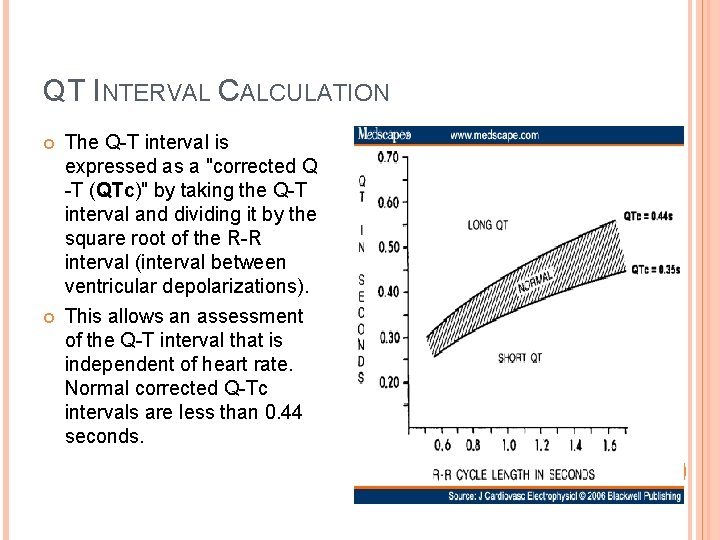
QT INTERVAL CALCULATION The Q-T interval is expressed as a "corrected Q -T (QTc)" by taking the Q-T interval and dividing it by the square root of the R-R interval (interval between ventricular depolarizations). This allows an assessment of the Q-T interval that is independent of heart rate. Normal corrected Q-Tc intervals are less than 0. 44 seconds.
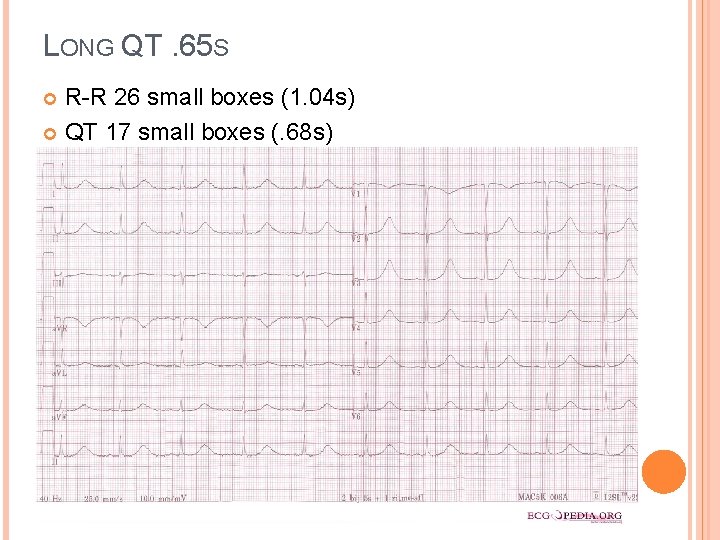
LONG QT. 65 S R-R 26 small boxes (1. 04 s) QT 17 small boxes (. 68 s)
INTERPRETING EKG AXIS
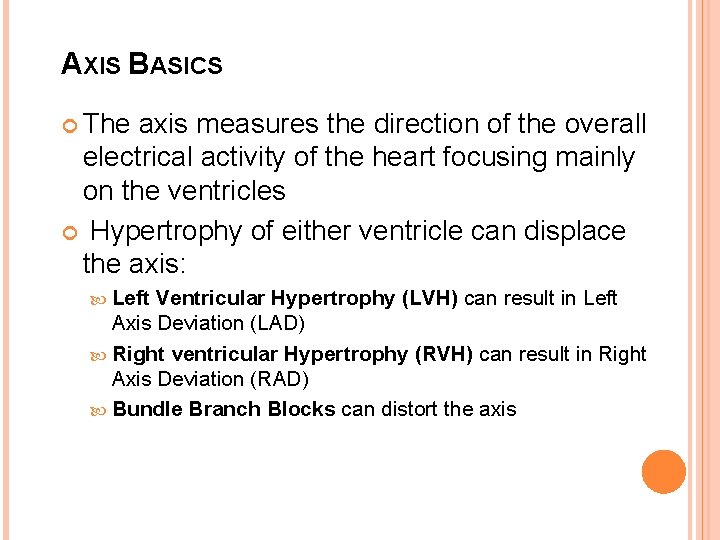
AXIS BASICS The axis measures the direction of the overall electrical activity of the heart focusing mainly on the ventricles Hypertrophy of either ventricle can displace the axis: Left Ventricular Hypertrophy (LVH) can result in Left Axis Deviation (LAD) Right ventricular Hypertrophy (RVH) can result in Right Axis Deviation (RAD) Bundle Branch Blocks can distort the axis
APPROACH TO EKG AXIS The Limb Leads and Augmented Leads are used to determine the axis Lead I and a. VF are the most common Normal axis usually results in a + QRS complex in leads I, III & a. VF Generally, a normal axis falls between 0° & +90°

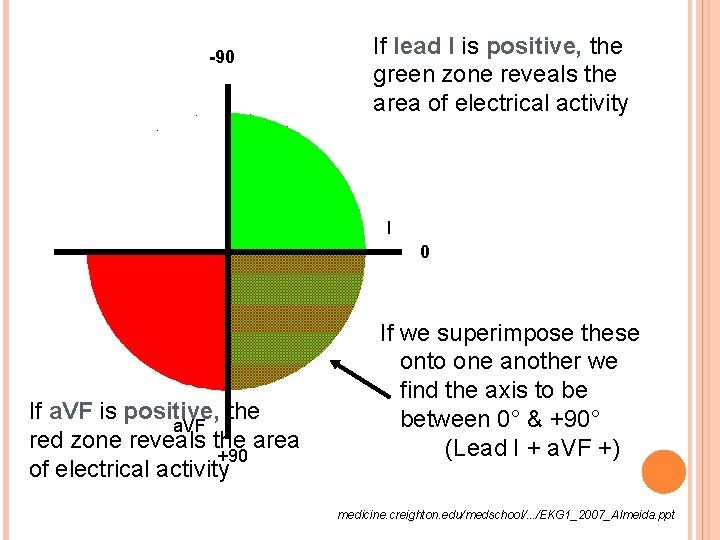
-90 If lead I is positive, the green zone reveals the area of electrical activity I 0 If a. VF is positive, the a. VF red zone reveals the area +90 of electrical activity If we superimpose these onto one another we find the axis to be between 0° & +90° (Lead I + a. VF +) medicine. creighton. edu/medschool/. . . /EKG 1_2007_Almeida. ppt
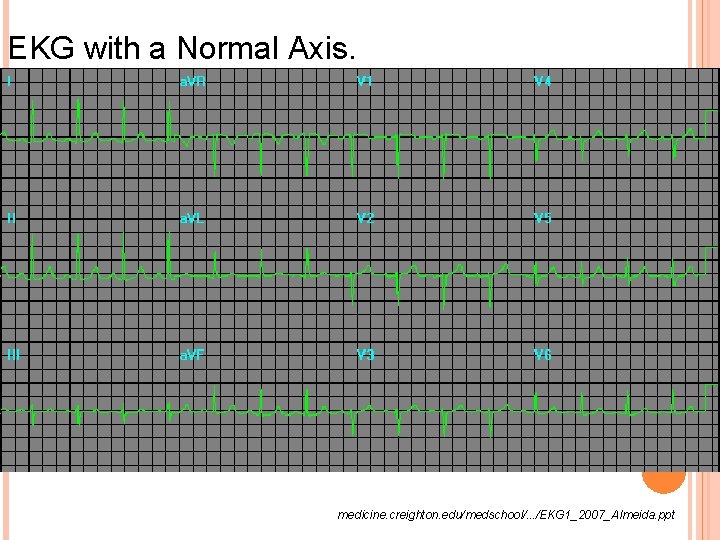
EKG with a Normal Axis. medicine. creighton. edu/medschool/. . . /EKG 1_2007_Almeida. ppt
LEFT AXIS DEVIATION LAD Axis between 0 ° and -90 ° May be caused by: HTN, aortic valve disease & cardiomyopathies Once you have determined that the axis lies between 0° & – 90°, it is clinically useful to decided if it is between – 30° & – 90°, as this is true LAD medicine. creighton. edu/medschool/. . . /EKG 1_2007_Almeida. ppt
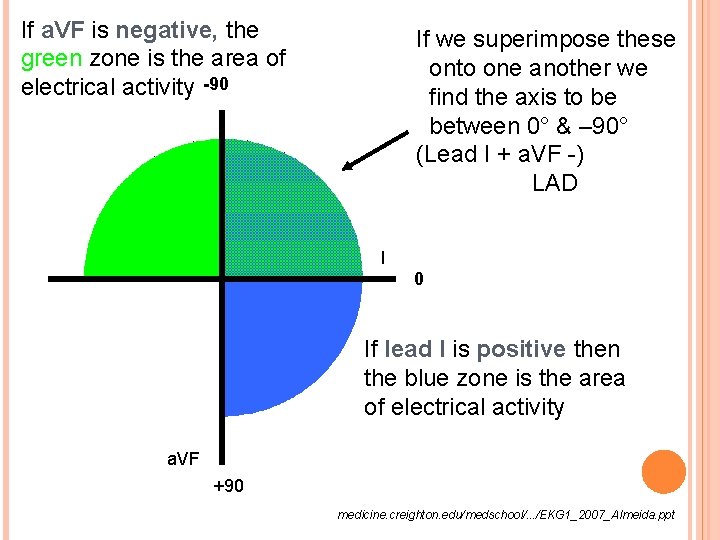
If a. VF is negative, the green zone is the area of electrical activity -90 If we superimpose these onto one another we find the axis to be between 0° & – 90° (Lead I + a. VF -) LAD I 0 If lead I is positive then the blue zone is the area of electrical activity a. VF +90 medicine. creighton. edu/medschool/. . . /EKG 1_2007_Almeida. ppt
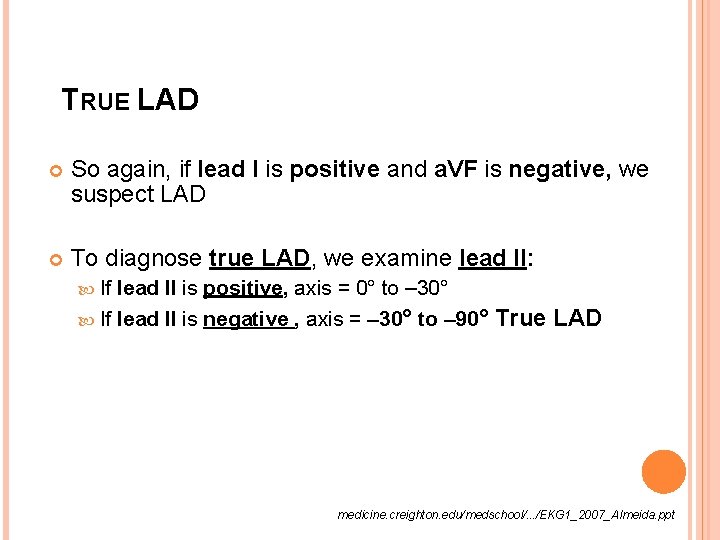
TRUE LAD So again, if lead I is positive and a. VF is negative, we suspect LAD To diagnose true LAD, we examine lead II: If lead II is positive, axis = 0° to – 30° If lead II is negative , axis = – 30° to – 90° True LAD medicine. creighton. edu/medschool/. . . /EKG 1_2007_Almeida. ppt
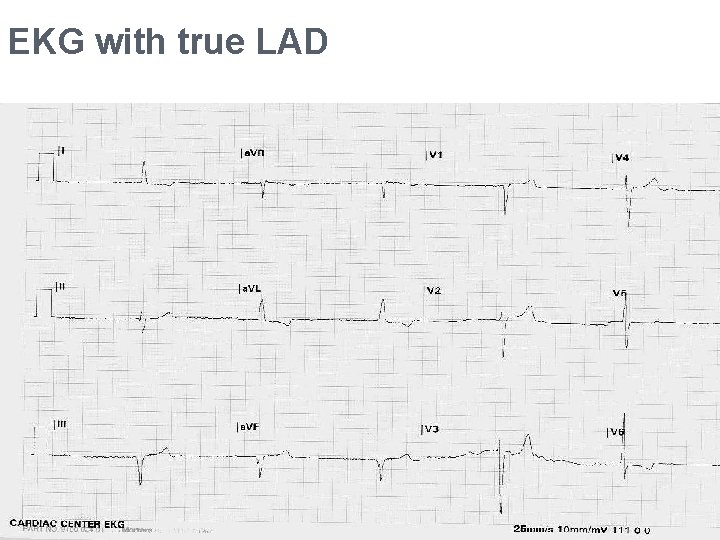
EKG with true LAD
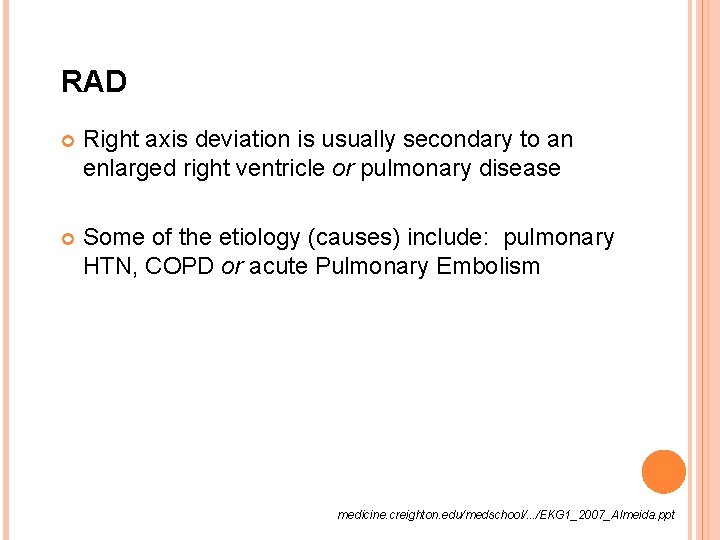
RAD Right axis deviation is usually secondary to an enlarged right ventricle or pulmonary disease Some of the etiology (causes) include: pulmonary HTN, COPD or acute Pulmonary Embolism medicine. creighton. edu/medschool/. . . /EKG 1_2007_Almeida. ppt
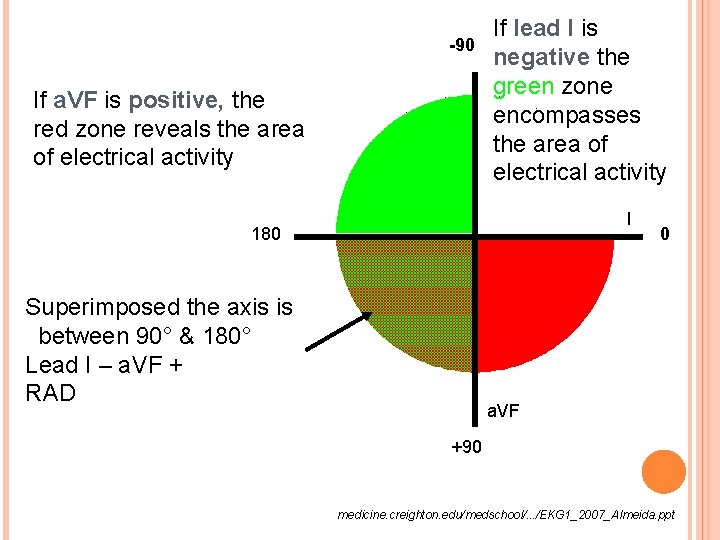
-90 If a. VF is positive, the red zone reveals the area of electrical activity If lead I is negative the green zone encompasses the area of electrical activity I 180 Superimposed the axis is between 90° & 180° Lead I – a. VF + RAD 0 a. VF +90 medicine. creighton. edu/medschool/. . . /EKG 1_2007_Almeida. ppt
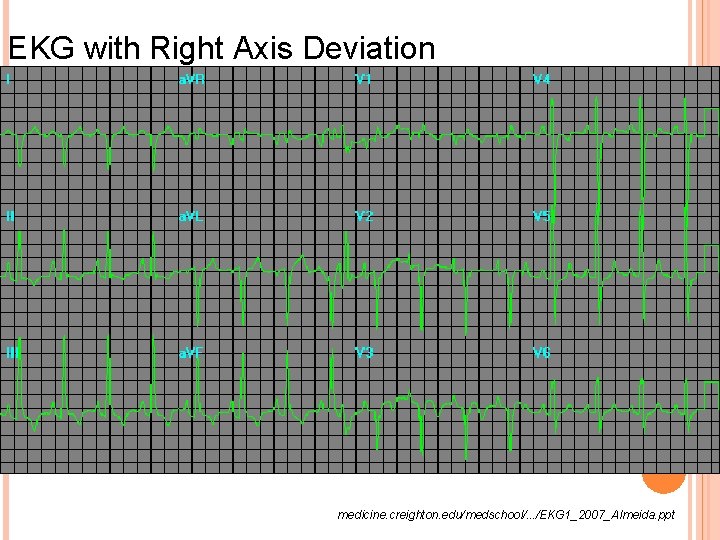
EKG with Right Axis Deviation medicine. creighton. edu/medschool/. . . /EKG 1_2007_Almeida. ppt
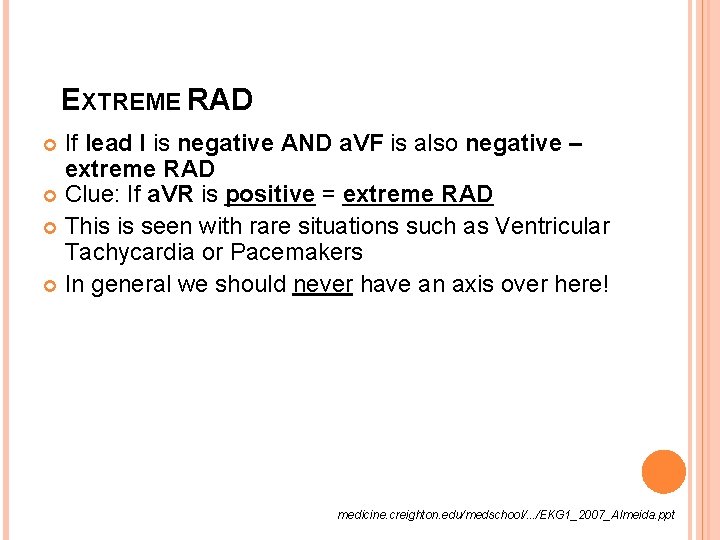
EXTREME RAD If lead I is negative AND a. VF is also negative – extreme RAD Clue: If a. VR is positive = extreme RAD This is seen with rare situations such as Ventricular Tachycardia or Pacemakers In general we should never have an axis over here! medicine. creighton. edu/medschool/. . . /EKG 1_2007_Almeida. ppt
HYPERTROPHIES
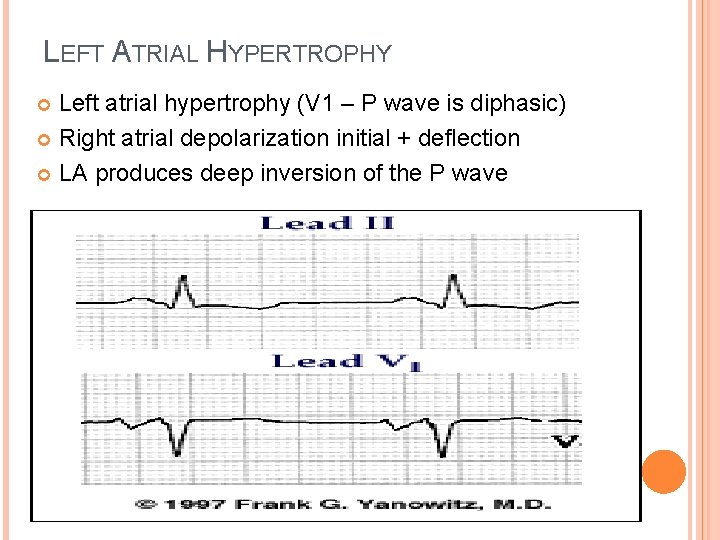
LEFT ATRIAL HYPERTROPHY Left atrial hypertrophy (V 1 – P wave is diphasic) Right atrial depolarization initial + deflection LA produces deep inversion of the P wave

RIGHT ATRIAL HYPERTROPHY Tall, peaked P wave in lead II > 2. 4 mm
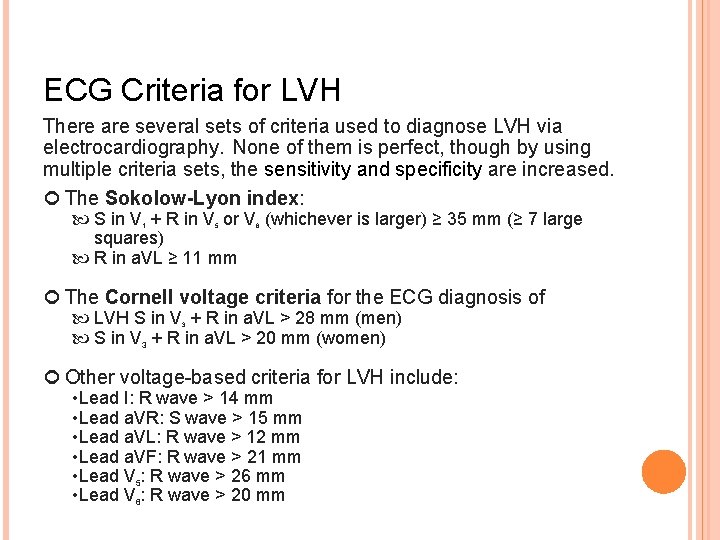
ECG Criteria for LVH There are several sets of criteria used to diagnose LVH via electrocardiography. None of them is perfect, though by using multiple criteria sets, the sensitivity and specificity are increased. The Sokolow-Lyon index: S in V + R in V or V (whichever is larger) ≥ 35 mm (≥ 7 large squares) R in a. VL ≥ 11 mm 1 5 6 The Cornell voltage criteria for the ECG diagnosis of LVH S in V + R in a. VL > 28 mm (men) S in V 3 + R in a. VL > 20 mm (women) 3 Other voltage-based criteria for LVH include: • Lead I: R wave > 14 mm • Lead a. VR: S wave > 15 mm • Lead a. VL: R wave > 12 mm • Lead a. VF: R wave > 21 mm • Lead V 5: R wave > 26 mm • Lead V 6: R wave > 20 mm
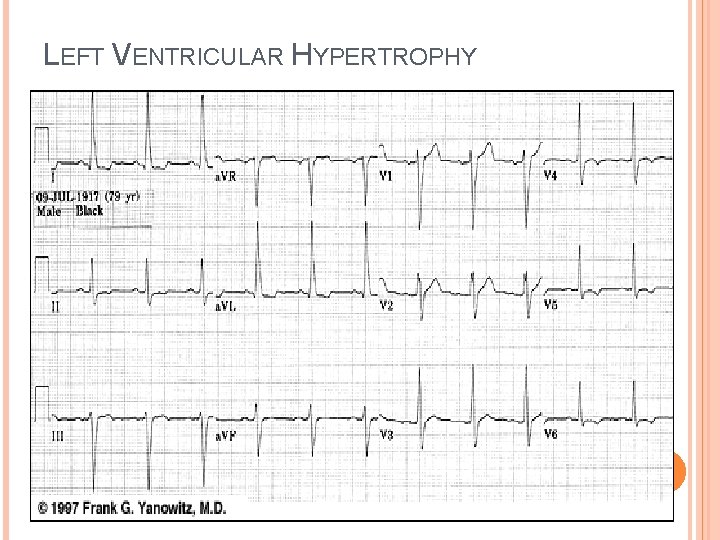
LEFT VENTRICULAR HYPERTROPHY

LVH Hypertension (most common cause) Aortic stenosis Aortic regurgitation Mitral regurgitation Coarctation of the aorta – constricted aortic segment Hypertrophic cardiomyopathy Normal adaptation to training Hard to know which on of these without more information. http: //lifeinthefastlane. com/ecg-library/basics/left-ventricularhypertrophy/
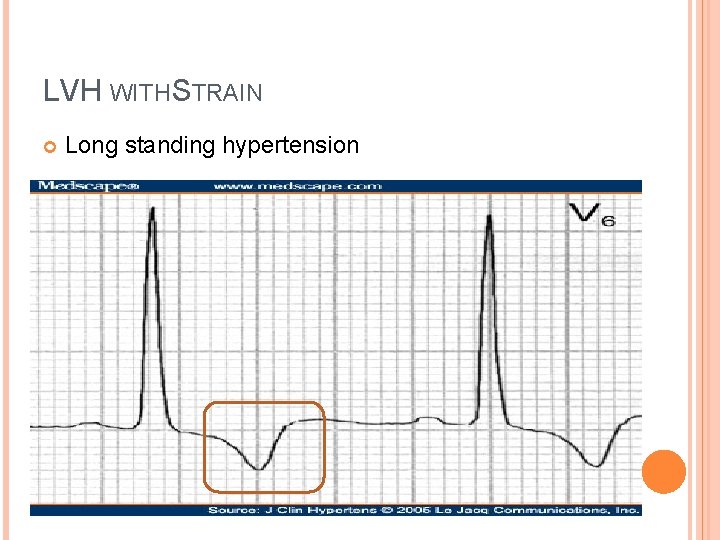
LVH WITH STRAIN Long standing hypertension
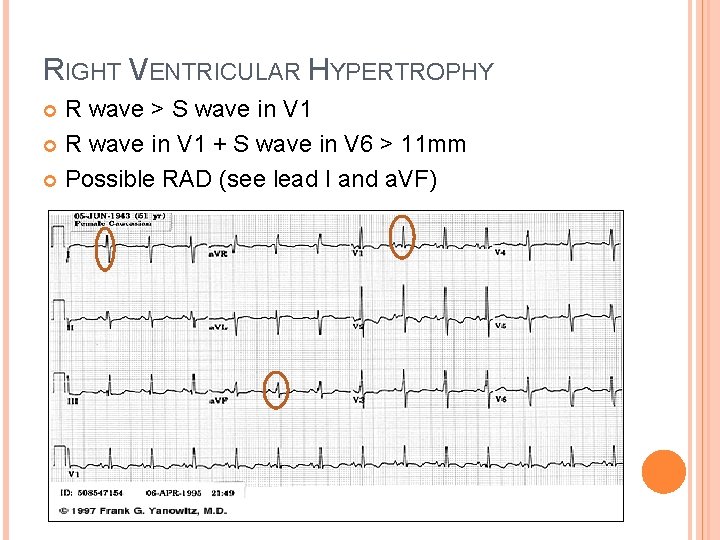
RIGHT VENTRICULAR HYPERTROPHY R wave > S wave in V 1 R wave in V 1 + S wave in V 6 > 11 mm Possible RAD (see lead I and a. VF)
RVH Pulmonary hypertension Mitral stenosis Pulmonary embolism Chronic lung disease (cor pulmonale) Congenital heart disease (e. g. Tetralogy of Fallot, pulmonary stenosis) Arrhythmogenic right ventricular cardiomyopathy Sometimes normal adaptation to exercise http: //lifeinthefastlane. com/ecg-library/basics/right-ventricularhypertrophy/
ISCHEMIA, INJURY INFRACTION

ISCHEMIA Ischemia – lack of oxygenated blood to left ventricle inverted T waves andor ST segment depression T waves always inverted in a. VR and can sometimes be inverted in III and V 1
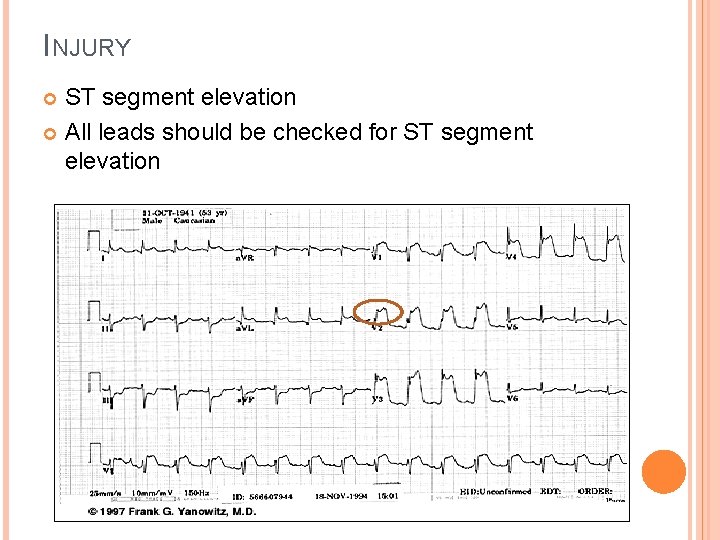
INJURY ST segment elevation All leads should be checked for ST segment elevation
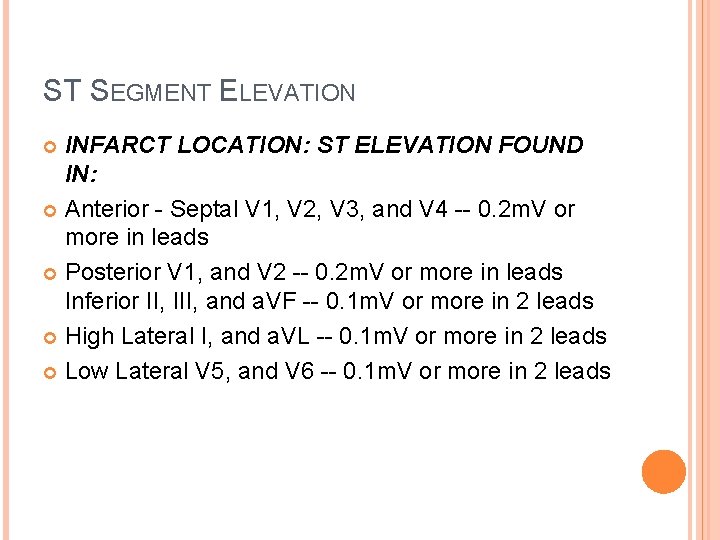
ST SEGMENT ELEVATION INFARCT LOCATION: ST ELEVATION FOUND IN: Anterior - Septal V 1, V 2, V 3, and V 4 -- 0. 2 m. V or more in leads Posterior V 1, and V 2 -- 0. 2 m. V or more in leads Inferior II, III, and a. VF -- 0. 1 m. V or more in 2 leads High Lateral I, and a. VL -- 0. 1 m. V or more in 2 leads Low Lateral V 5, and V 6 -- 0. 1 m. V or more in 2 leads
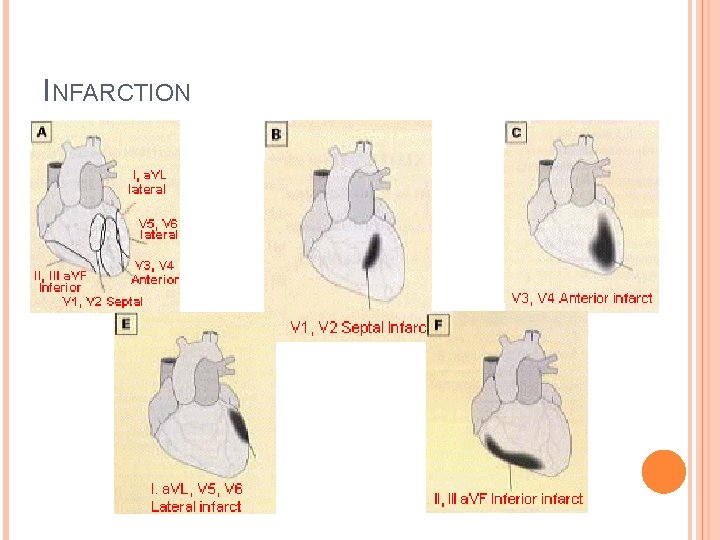
INFARCTION

INFARCTION Significant Q waves. 04 s wide or 1/3 the height of the R waves Q waves develop over the area damaged Septal Q waves (I, a. VL, V 5 -6) are not pathologic T wave inversion in the leads over the damaged area

THE ATHLETE’S HEART Resting Sinus Bradycardia Non specific ST segment and T wave changes ST segment elevation precordial leads T wave flattening or inversion LVH and sometimes RVH Incomplete RBBB seen in V 1 -3, not in V 4 -6 Various arrhythmias (junctional rhythms or wandering atrial pacemaker). 1 st degree or Wenckebach (Mobitz I)AV block.
- Slides: 92