http uia fnplzen cz Immune system J Ochotn












- Slides: 70
http: //uia. fnplzen. cz/
Immune system J. Ochotná
The main functions of the immune system Immune system belongs to the basic homeostatic mechanisms Defense - identification and protection against pathogenic microorganisms and their toxins Autotolerance – recognition of own tissues and keeping tolerance to them Immune surveillance - identifying and removing the old , damaged and otherwise changed cells
Antigen (immunogen) * substance that can induce a humoral and/or cell-mediated immune response * predominantly proteins or polysaccharides * molecules >5 k. Da * optimal size of antigen is about 40 k. Da
* autoantigen - antigen derived from his own body exoantigen - alien substance from the external environment * * allergen - exoantigen that in susceptible individuals may cause pathological (allergic) immune response
Haptens * small molecules, that are able to induce specific immune response only after the establishment to the macromolecular carrier (separate haptens are not immunogenic) * typically drugs (eg penicillin antibiotics, hydralazin)

Interaction antigen – antibody Binding site of antibody (paratop) form non-covalent complexes with the corresponding part on antigen molecule (epitope) * participation: the hydrogen bonds, electrostatic and hydrophobic interactions, van der Waals forces * antigen-antibody complex is reversible
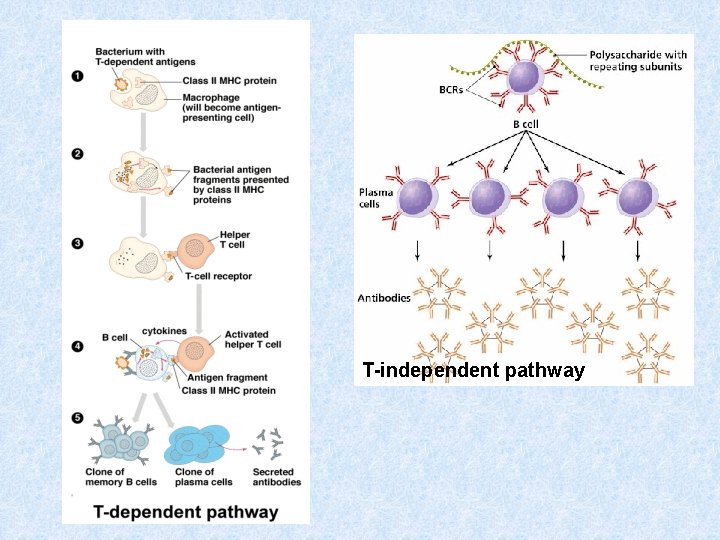
Types of antigens according to antigen presentation 1) thymus dependent antigens * more frequent, especially protein Ag * for induction of humoral immune response is necessary cooperation with TH lymphocytes (or response isn´t enough effective) * assistance implemented in the form of cytokines produced by TH lymphocytes
Types of antigens according to antigen presentation 2) thymus independent antigens * can induce antibodies production directly without the participation of T lymphocytes * mainly bacterial polysaccharides, lipopolysaccharides and polymer forms of proteins (e. g. Haemophilus, Str. pneumoniae)
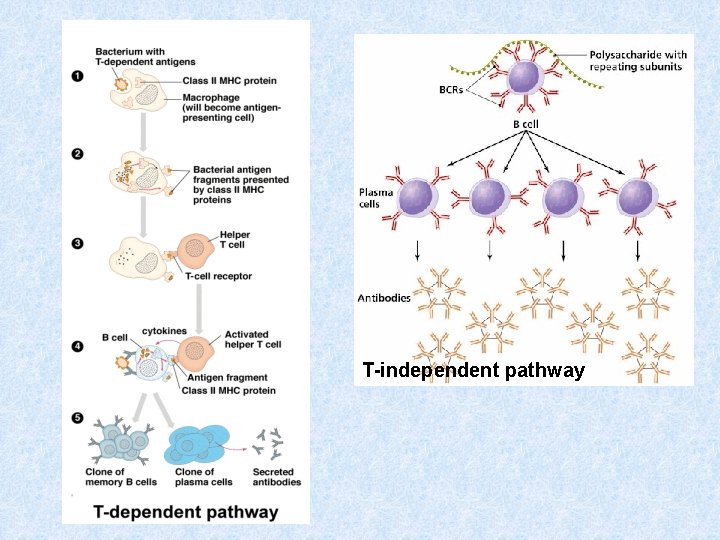
T-independent pathway
Superantigens * stimulate lymphocytes polyclonaly and massively (5 -25%) * massive activation of T lymphocytes can cause shock * e. g. bacterial toxins (Staph. aureus, Str. pyogenes, Pseud. aeruginosa)

Sequestered antigens * autoantigens that are normally hidden from the immune system and therefore unknow (e. g. the lens of the eye , testes, brain) * if they are "uncovered" by demage, can induce the immune response (one of theories of autoimmune processes)
Components of the immune system
Components of the immune system * Lymphoid tissues and organs * Cells of the immune system * Molecules of the immune system
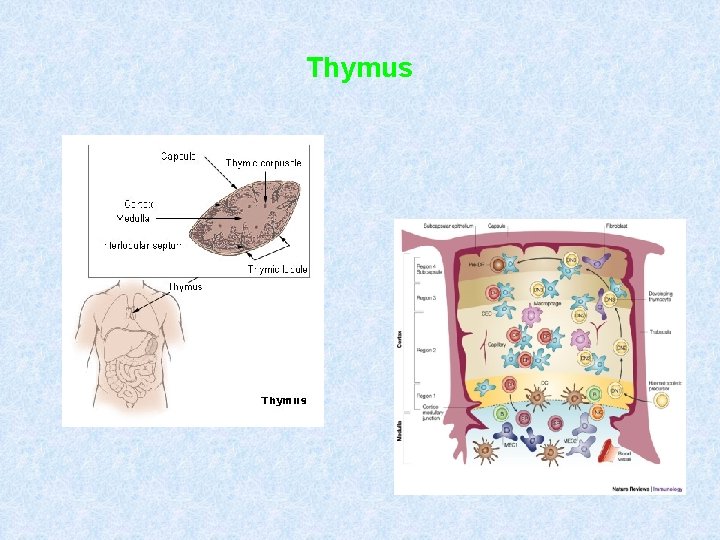
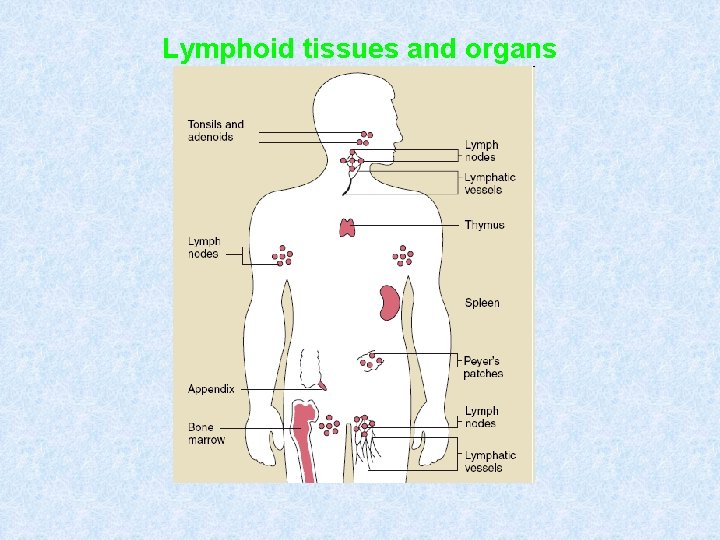
Lymphoid tissues and organs * are linked with the other organs and tissues by network of lymphatic and blood vessels Primary lymphoid tissues and organs * bone marrow, thymus * maturation and differentiation of immunocompetent cells * immature lymphocytes acquire here their antigenic specificity
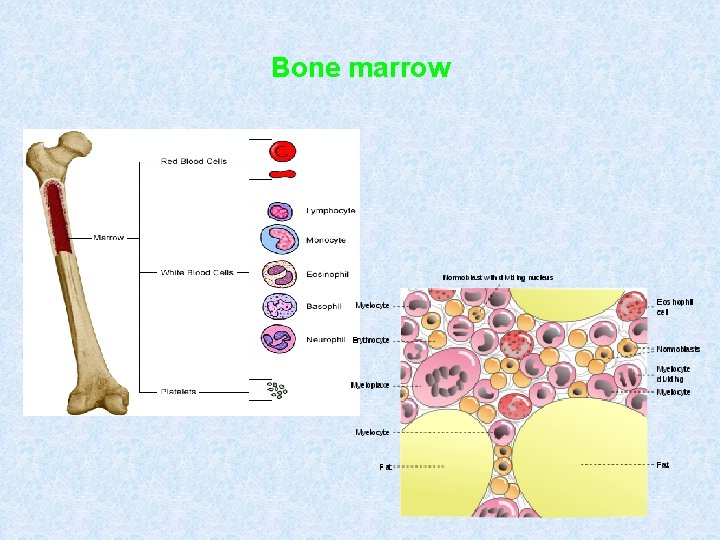
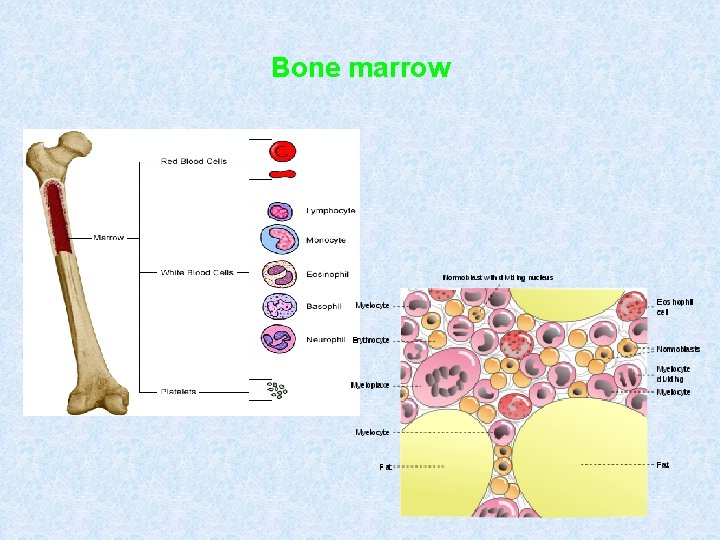
Bone marrow
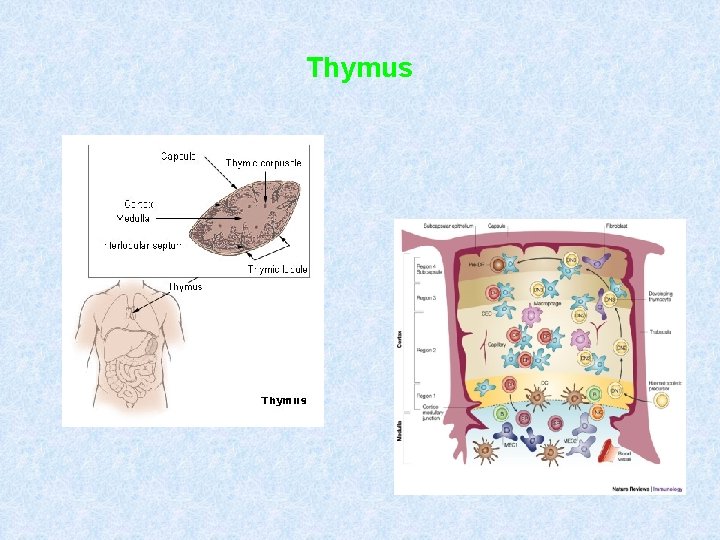
Thymus
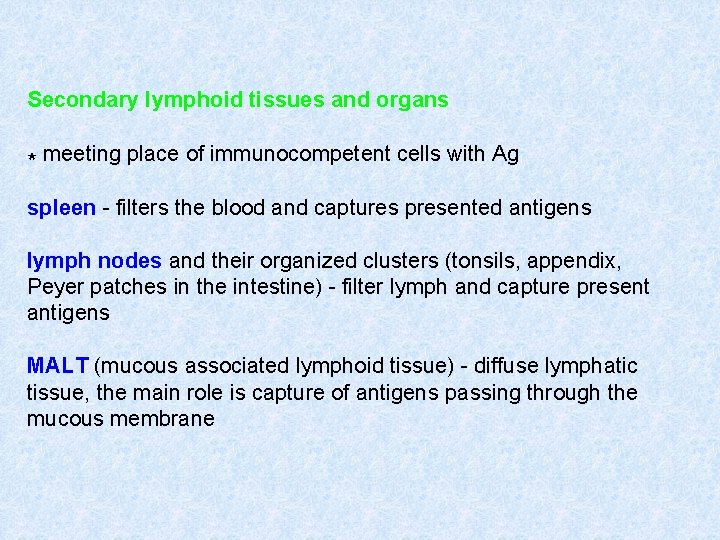
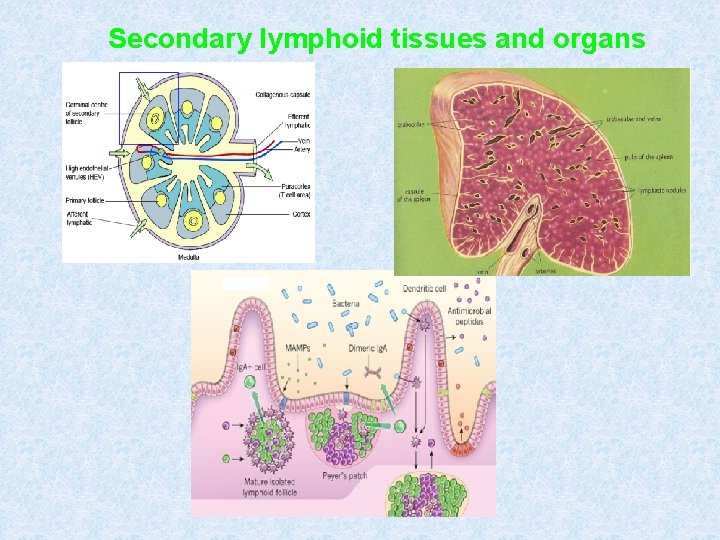
Secondary lymphoid tissues and organs * meeting place of immunocompetent cells with Ag spleen - filters the blood and captures presented antigens lymph nodes and their organized clusters (tonsils, appendix, Peyer patches in the intestine) - filter lymph and capture present antigens MALT (mucous associated lymphoid tissue) - diffuse lymphatic tissue, the main role is capture of antigens passing through the mucous membrane
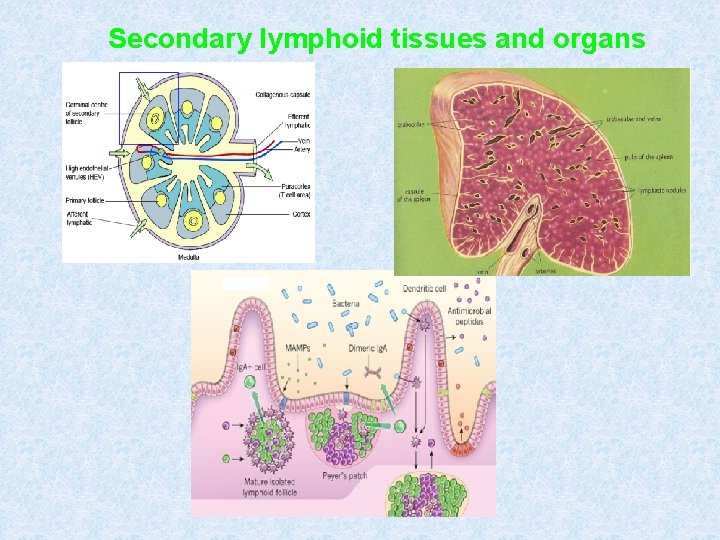
Secondary lymphoid tissues and organs
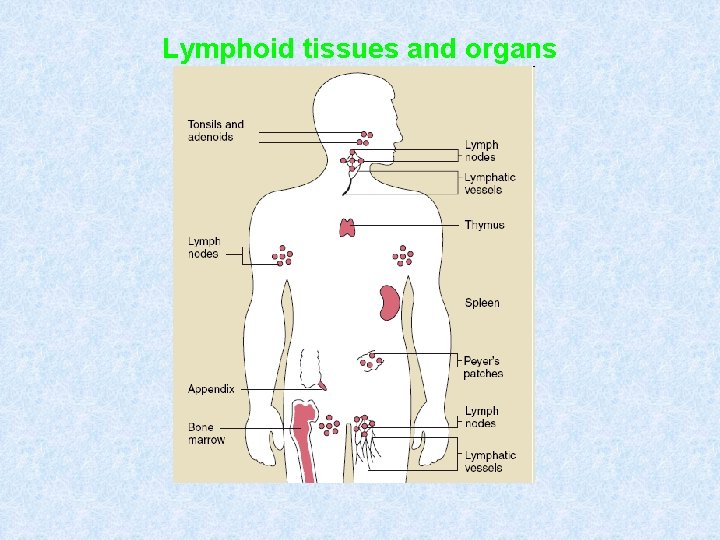
Lymphoid tissues and organs
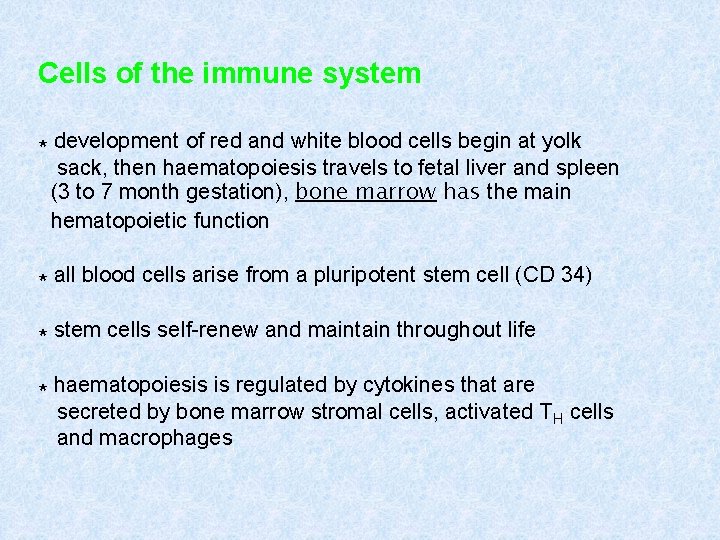
Cells of the immune system * development of red and white blood cells begin at yolk sack, then haematopoiesis travels to fetal liver and spleen (3 to 7 month gestation), bone marrow has the main hematopoietic function * all blood cells arise from a pluripotent stem cell (CD 34) * stem cells self-renew and maintain throughout life * haematopoiesis is regulated by cytokines that are secreted by bone marrow stromal cells, activated TH cells and macrophages


Immune mechanisms
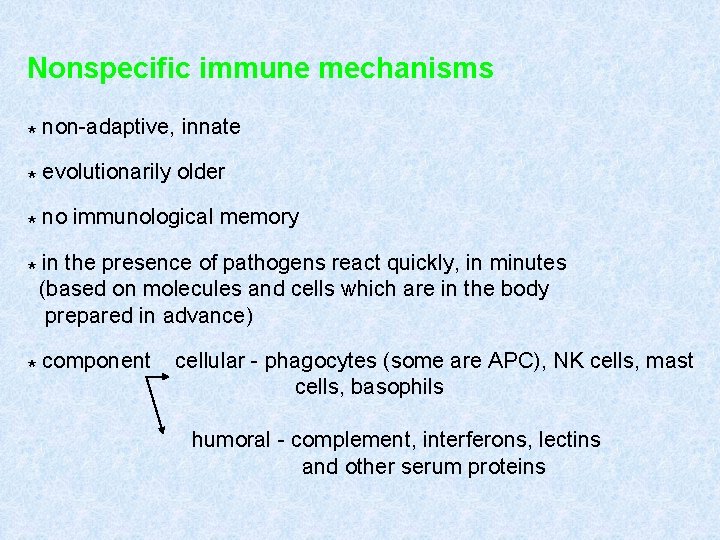
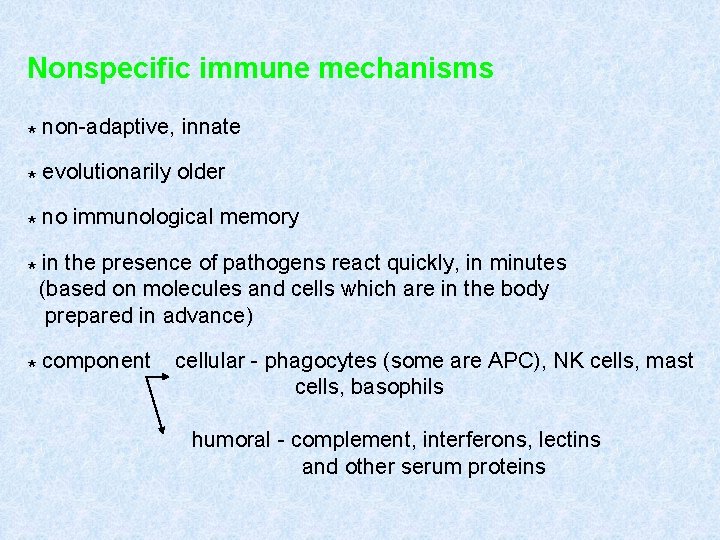
Nonspecific immune mechanisms * non-adaptive, innate * evolutionarily older * no immunological memory * in the presence of pathogens react quickly, in minutes (based on molecules and cells which are in the body prepared in advance) * component cellular - phagocytes (some are APC), NK cells, mast cells, basophils humoral - complement, interferons, lectins and other serum proteins
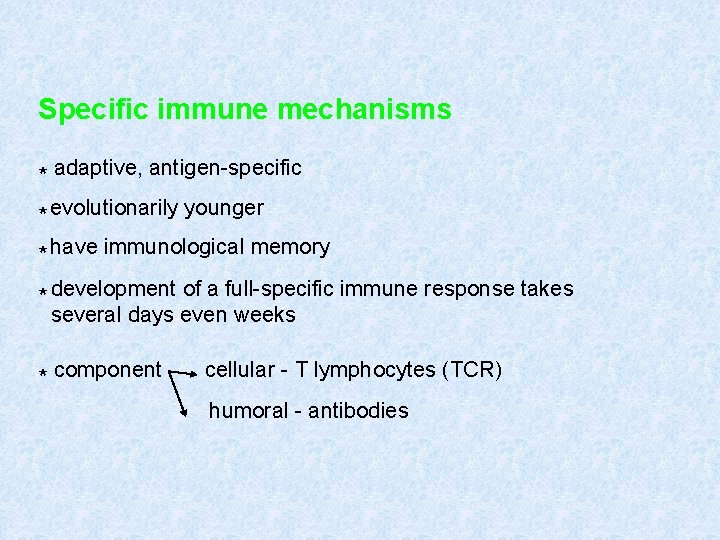
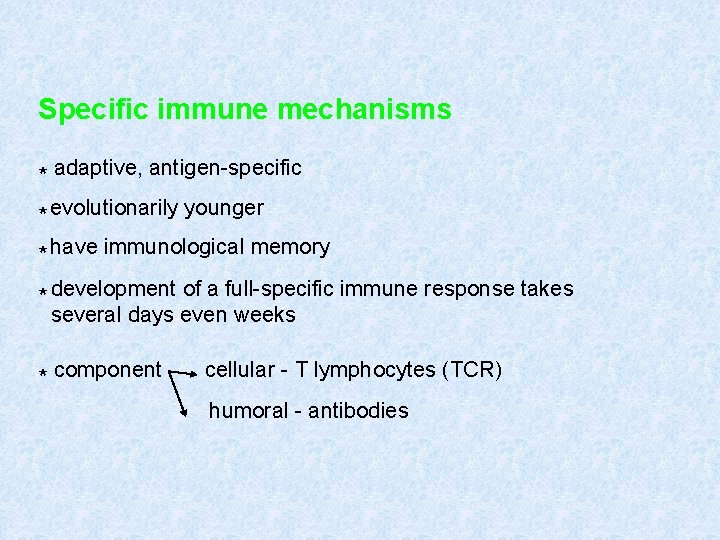
Specific immune mechanisms * adaptive, antigen-specific * evolutionarily younger * have immunological memory * development of a full-specific immune response takes several days even weeks * component cellular - T lymphocytes (TCR) humoral - antibodies
Phagocytosis
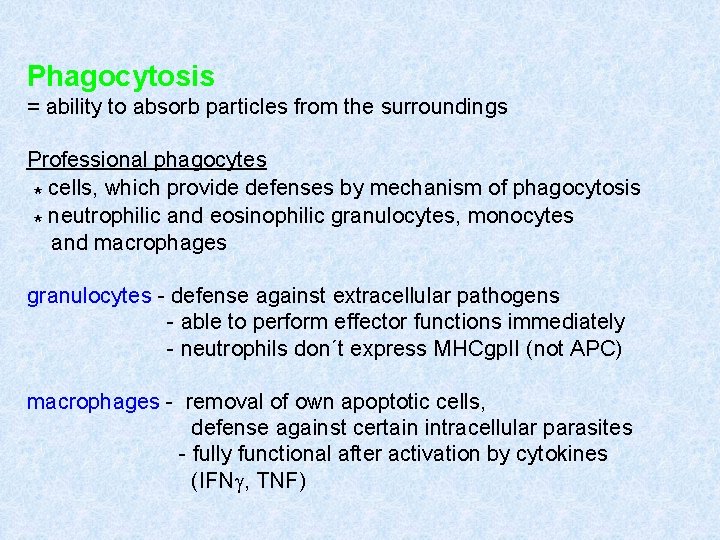
Phagocytosis = ability to absorb particles from the surroundings Professional phagocytes * cells, which provide defenses by mechanism of phagocytosis * neutrophilic and eosinophilic granulocytes, monocytes and macrophages granulocytes - defense against extracellular pathogens - able to perform effector functions immediately - neutrophils don´t express MHCgp. II (not APC) macrophages - removal of own apoptotic cells, defense against certain intracellular parasites - fully functional after activation by cytokines (IFNg, TNF)
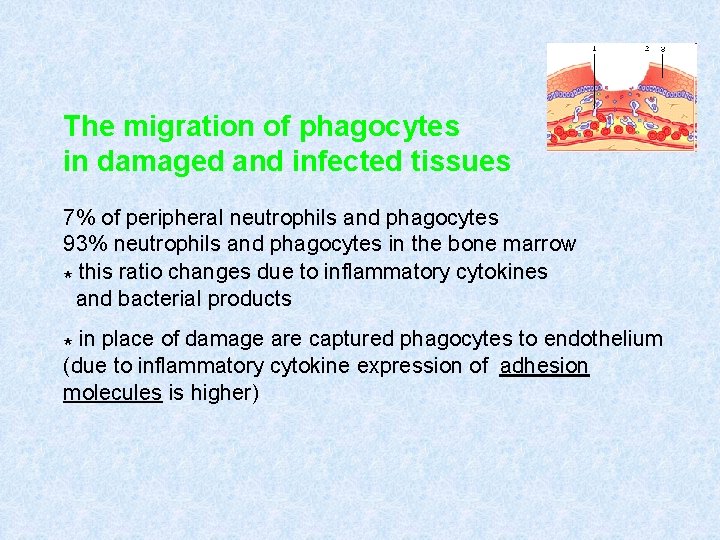
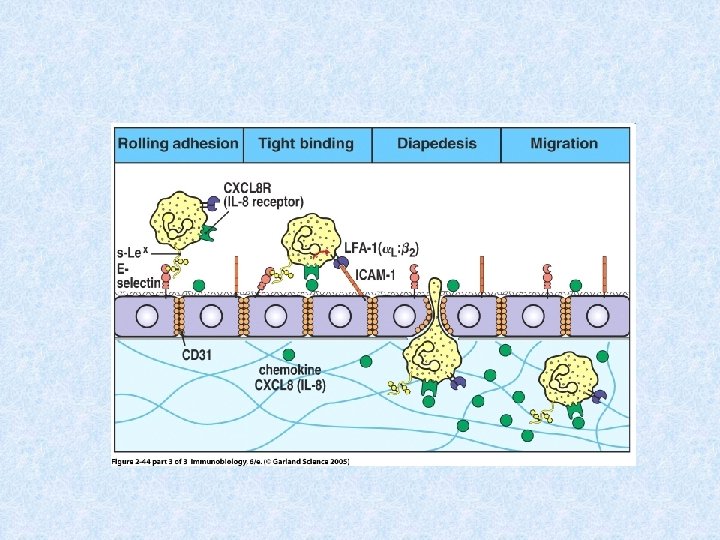
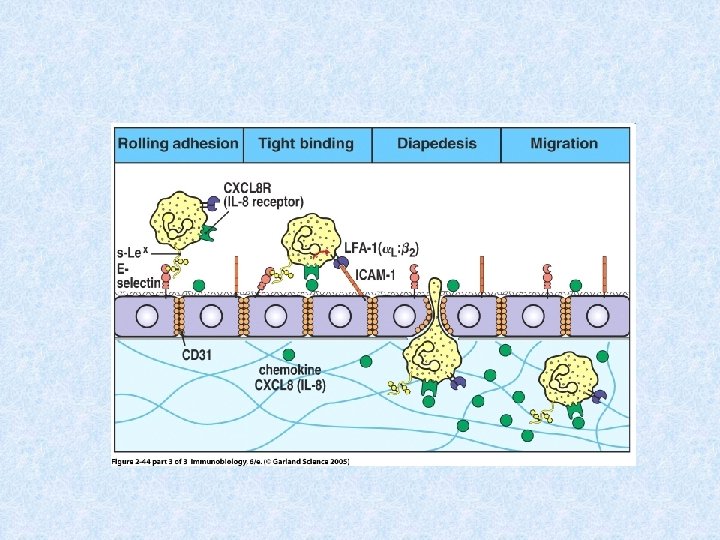
The migration of phagocytes in damaged and infected tissues 7% of peripheral neutrophils and phagocytes 93% neutrophils and phagocytes in the bone marrow * this ratio changes due to inflammatory cytokines and bacterial products * in place of damage are captured phagocytes to endothelium (due to inflammatory cytokine expression of adhesion molecules is higher)
* the first is interactions slows the movement of neutrophils - called roling * then there is a stronger link between endothelial cells and leukocytes and subsequent penetration between endothelial cells to the tissue - diapedesis , extravasation * phagocytes are directed to the site of inflammation by chemokines (IL-8, MIP-1 a and , MCP-1, RANTES, C 3 a, C 5 a, bacterial products. . . )

Receptors on phagocytes PAMPs - "pathogen associated molecular patterns„ - structures that are located on the surface of microorganisms, but not on their own intact cells * mannose receptor * galactose receptor * CD 14 (binds bacterial LPS) * TLR receptors (binds bacterial lipoproteins, lipopolysaccharides, bacterial DNA) * scavenger receptors (bind phospholipids on the surface of apoptotic cells)
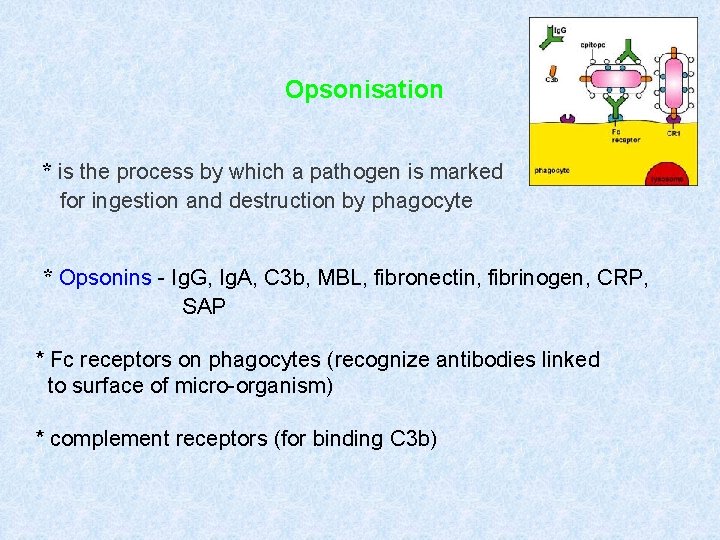
Opsonisation * is the process by which a pathogen is marked for ingestion and destruction by phagocyte * Opsonins - Ig. G, Ig. A, C 3 b, MBL, fibronectin, fibrinogen, CRP, SAP * Fc receptors on phagocytes (recognize antibodies linked to surface of micro-organism) * complement receptors (for binding C 3 b)

Phagocytosis
Degradation of ingested material * fagosome fusion with lysosomes * activation of membrane NADPH oxidase * production of nitric oxide (NO)
Fagosome fusion with lysosomes * bactericidal substances (defensins) * hydrolytic enzymes (cathepsin, lysozyme) * liquid with a p. H of 4 -5
activation of membrane NADPH oxidase * activation of Fc receptors and complement receptors leads to respiratory (oxidative) flash * oxygen intermediates (superoxid radical O 2 -, singlet oxygen, hydrogen peroxide, hydroxyl radical) → damage of the pathogen
production of nitric oxide (NO) * macrophages produce NO after activation with cytokines (IFNg, TNF) that are produced by TH 1 lymphocytes * NO liquidate intracellular parasites of macrophages
Secretory products of phagocytes * IL-1, 6, TNF (systemic response to inflammation) * IL-8 (chemokine) * IL-3, GM-CSF (control haematopoiesis) * TGFa, TGF (tissue regeneration) * metabolic products of arachidonic acid (prostaglandins, prostacyclin, leukotrienes and thromboxanes)
Complement
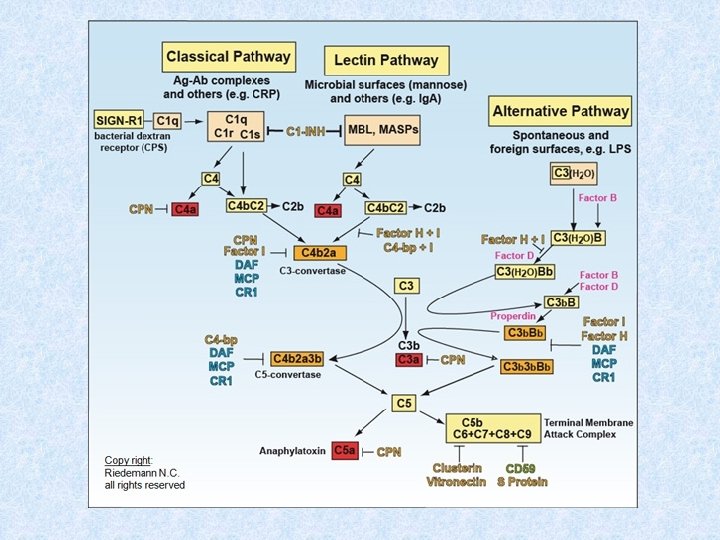
Complement * system of about 30 serum and membrane proteins (humoral component of nonspecific immunity) * complement components in serum are present in inactive form * complement activation has cascade character * complement proteins are synthesized in the liver, less by tissue macrophages and fibroblasts * the main complement components: C 1 -C 9 (C 3 is the central component) * other complement components: factor B, factor D, factor P * regulatory proteins: C 1 - inhibitor, factor I, factor H, DAF, MCP, CR 1, CD 59 (protektin) inactivator of anafylatoxin

Complement functions * Opsonization (C 3 b) * Chemotaxis (C 3 a, C 5 a) * Osmotic lysis (MAC C 5 b-C 9) * Anafylatoxins (C 3 a, C 4 a, C 5 a)
Complement activation * Alternative pathway * Clasial pathway * Lektin pathway
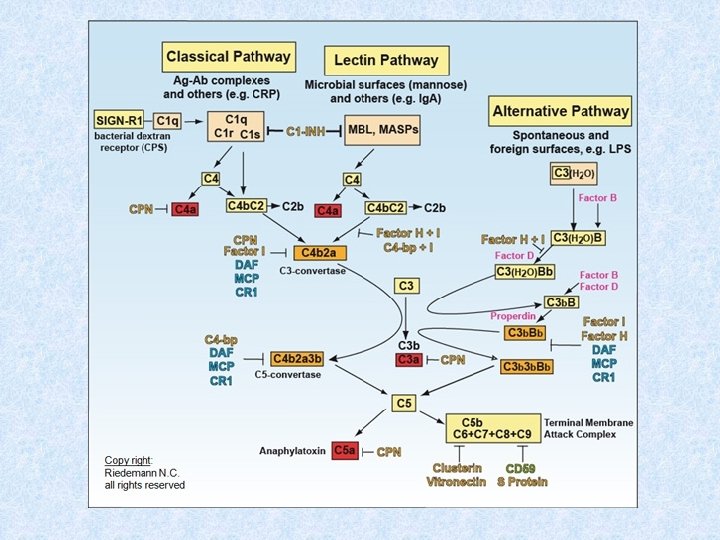
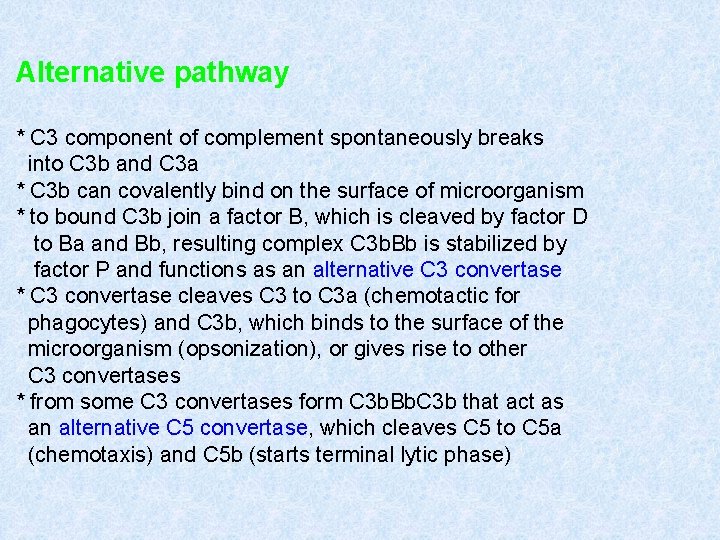
Alternative pathway * C 3 component of complement spontaneously breaks into C 3 b and C 3 a * C 3 b can covalently bind on the surface of microorganism * to bound C 3 b join a factor B, which is cleaved by factor D to Ba and Bb, resulting complex C 3 b. Bb is stabilized by factor P and functions as an alternative C 3 convertase * C 3 convertase cleaves C 3 to C 3 a (chemotactic for phagocytes) and C 3 b, which binds to the surface of the microorganism (opsonization), or gives rise to other C 3 convertases * from some C 3 convertases form C 3 b. Bb. C 3 b that act as an alternative C 5 convertase, which cleaves C 5 to C 5 a (chemotaxis) and C 5 b (starts terminal lytic phase)
Classical pathway * Can be initiated by antibodies (Ig. G, not by Ig. G 4; Ig. M) or so-called pentraxins (CRP, SAP - acute phase proteins) * after binding of antibodies to the bacteria surface, there is a change in its conformation and C 1 protein can bind * C 1 have to bind to the 2 molecules of antibodies, change their conformation and get proteolytic activity - will cleave proteins C 4 and C 2 * fragments C 4 b and C 2 a bind to the surface of organism and create the classic C 3 convertase (C 4 b. C 2 a), which cleaves C 3 to C 3 a and C 3 b * then creates a classic C 5 convertase (C 4 b. C 2 a. C 3 b) that cleaves C 5 to C 5 a and C 5 b
Lectin pathway * is initiated by serum mannose binding lectin (MBL) * MBL binds to manose, glucose or other sugars on the surface of some microbes, after the bindins starts cleave C 4 and C 2 * this way is similar to the classical pathway
Terminal (lytic) phase of the complement cascade C 5 b fragments creates a complex with C 6, C 7 and C 8, the complex dive into the lipid membrane of the cell and attached to it into a circle 13 -18 molecules of C 9, thus create pores in the membrane and cell can lysis (G-bacteria, protozoans, some viruses). Most microorganisms is resistant to this lytic effect of complement (protection by cell wall).
Complement regulation and protection of own cells Activation of complement cascade is controlled by serum and membrane inhibitors. * C 1 inhibitor * DAF (decay-accelerating protein)-degradation of C 3 convertase * factor I, MCP (membrane cofactor protein), CR 1, factor H – C 3 b cleavage * CD 59 (protectin) - prevents the polymerization of C 9 * anafylatoxin inactivator - inactivates anafylatoxins (C 3 a, C 4 a, C 5 a)

Complement receptors * Bind fragments of complement components CR 1 - on various cells - removing of immunecomplexes CR 2 - on B lymphocytes and FDC - activation of B cells CR 3, CR 4 - on phagocytes - participation in opsonization, adhesion
NK CELLS INTERFERONS

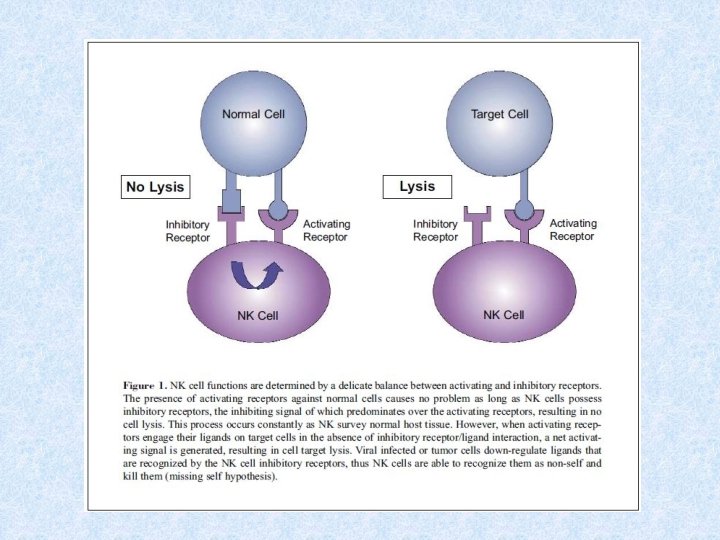
NK CELLS § lymphoid cells which belon to innate immune mechanisms § kill cells which have abnormally low MHCgp. I expression (some tumor and virus infected cells) § have similar cytotoxic mechanisms as Tc § NK cells activators - IFNa, IFN
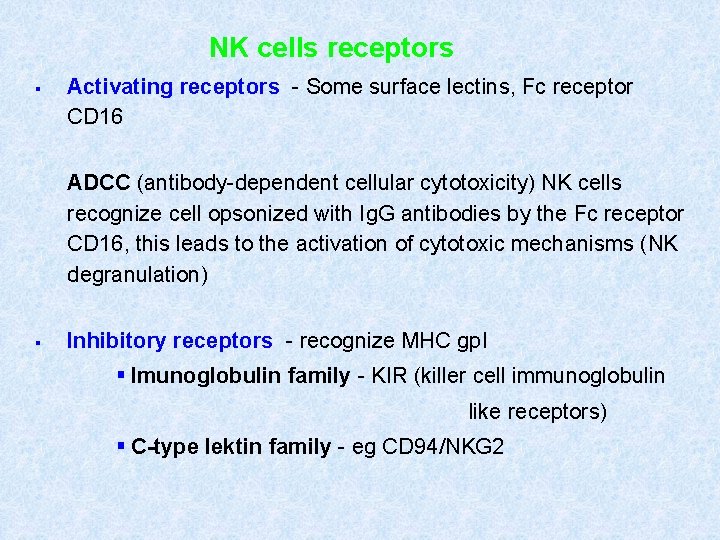
NK cells receptors § Activating receptors - Some surface lectins, Fc receptor CD 16 ADCC (antibody-dependent cellular cytotoxicity) NK cells recognize cell opsonized with Ig. G antibodies by the Fc receptor CD 16, this leads to the activation of cytotoxic mechanisms (NK degranulation) § Inhibitory receptors - recognize MHC gp. I § Imunoglobulin family - KIR (killer cell immunoglobulin like receptors) § C-type lektin family - eg CD 94/NKG 2
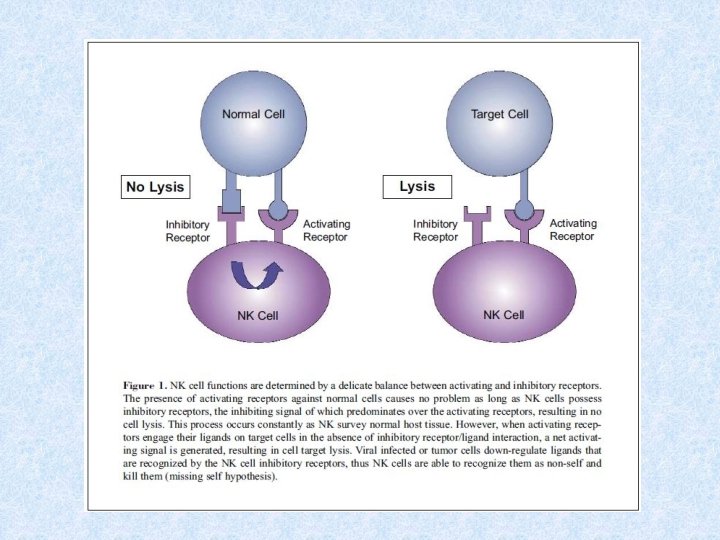
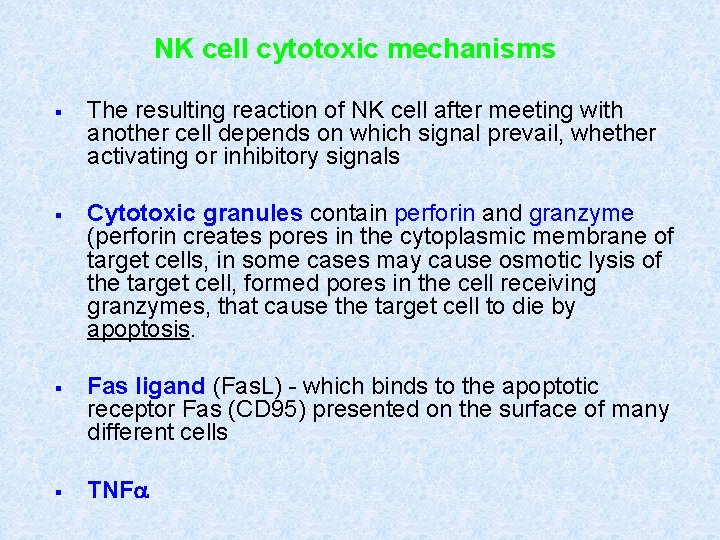
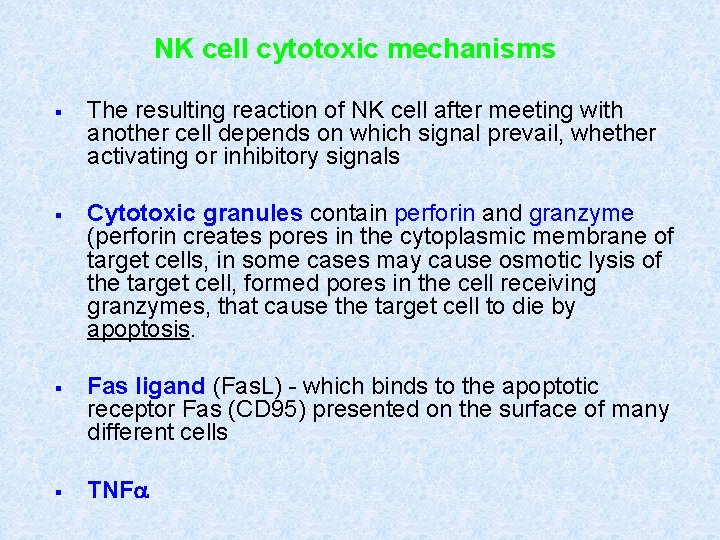
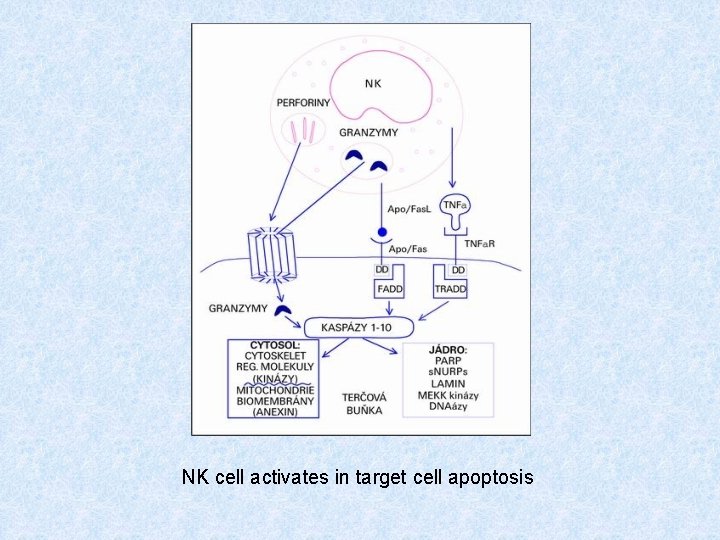
NK cell cytotoxic mechanisms § The resulting reaction of NK cell after meeting with another cell depends on which signal prevail, whether activating or inhibitory signals § Cytotoxic granules contain perforin and granzyme (perforin creates pores in the cytoplasmic membrane of target cells, in some cases may cause osmotic lysis of the target cell, formed pores in the cell receiving granzymes, that cause the target cell to die by apoptosis. § Fas ligand (Fas. L) - which binds to the apoptotic receptor Fas (CD 95) presented on the surface of many different cells § TNFa
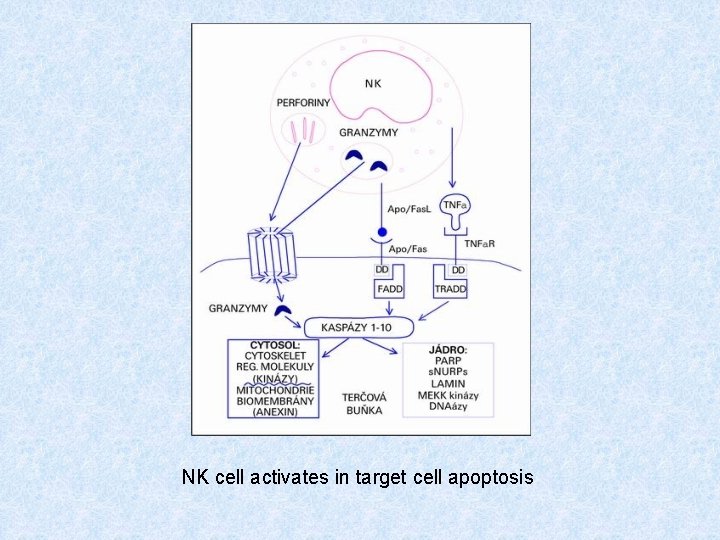
NK cell activates in target cell apoptosis

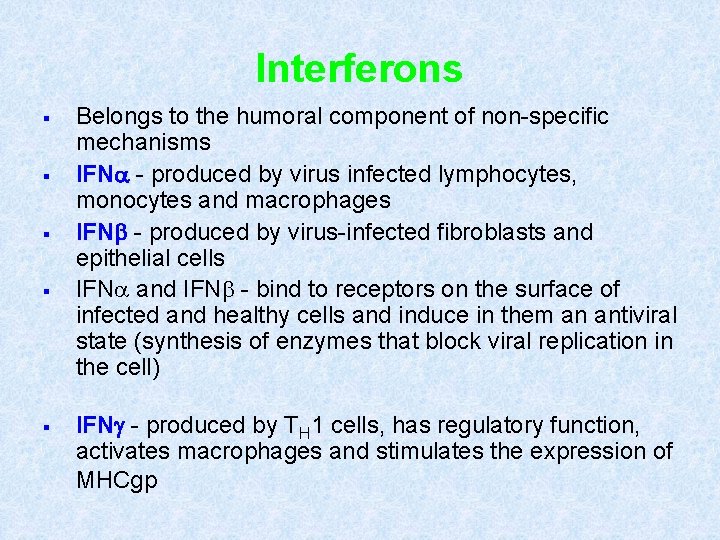
Interferons § § § Belongs to the humoral component of non-specific mechanisms IFNa - produced by virus infected lymphocytes, monocytes and macrophages IFNb - produced by virus-infected fibroblasts and epithelial cells IFNa and IFN - bind to receptors on the surface of infected and healthy cells and induce in them an antiviral state (synthesis of enzymes that block viral replication in the cell) IFNg - produced by TH 1 cells, has regulatory function, activates macrophages and stimulates the expression of MHCgp

Interferons
Basophils and mast cells and their importance in immune responses
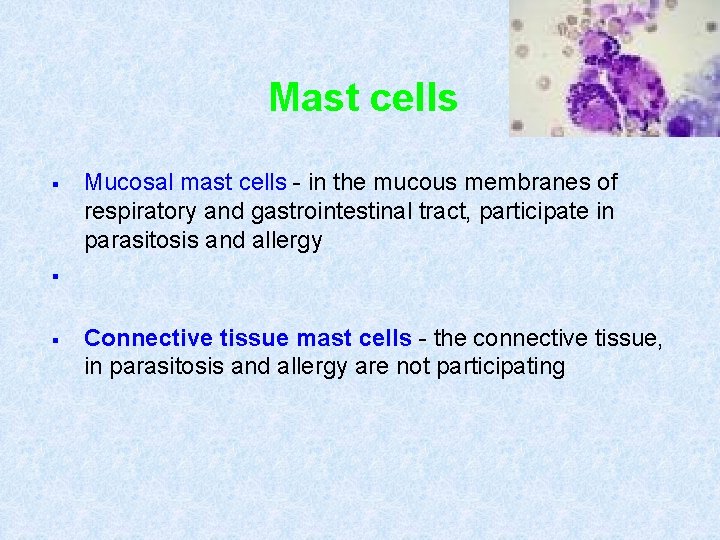
Mast cells § Mucosal mast cells - in the mucous membranes of respiratory and gastrointestinal tract, participate in parasitosis and allergy § § Connective tissue mast cells - the connective tissue, in parasitosis and allergy are not participating
Mast cell functions § Defense against parasitic infections § In pathological circumstances, responsible for the early type of hypersensitivity (immunopathological reaction type. I) § Apply during inflammation, in angiogenesis, in tissue remodeling § Regulation of immune response
Mast cell activation Mast cells degranulation can be stimulated by: § cross-linking of Ig. E Fc receptors § anafylatoxins (C 3 a, C 4 a, C 5 a) § TLR
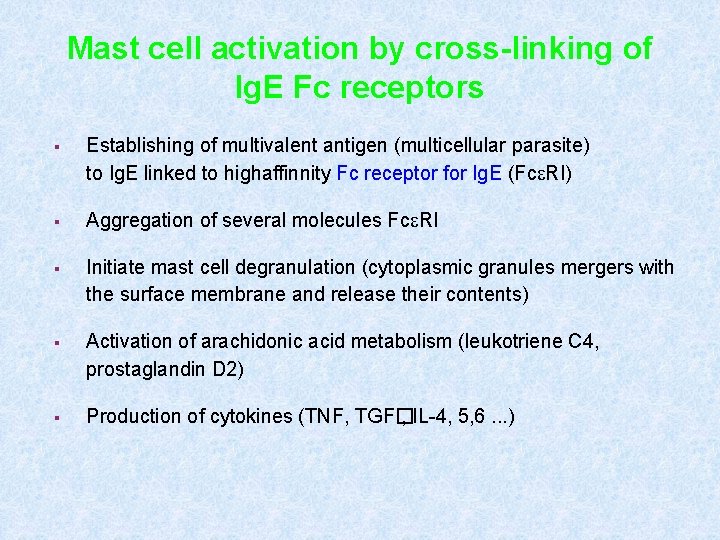
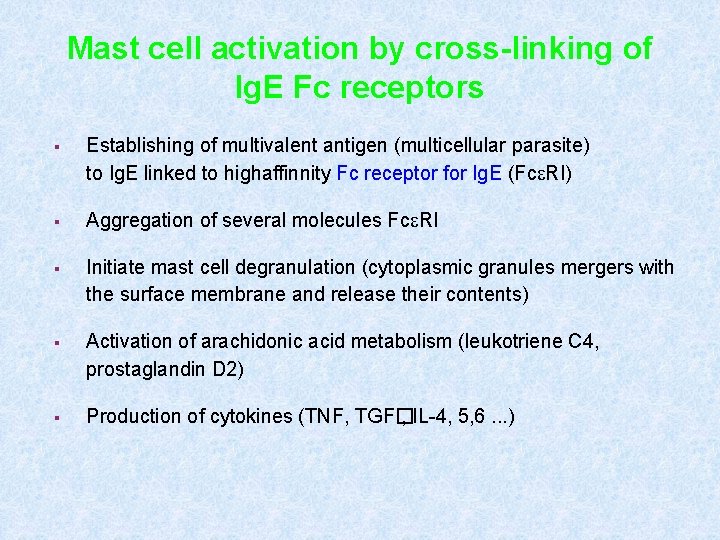
Mast cell activation by cross-linking of Ig. E Fc receptors § Establishing of multivalent antigen (multicellular parasite) to Ig. E linked to highaffinnity Fc receptor for Ig. E (Fc RI) § Aggregation of several molecules Fc RI § Initiate mast cell degranulation (cytoplasmic granules mergers with the surface membrane and release their contents) § Activation of arachidonic acid metabolism (leukotriene C 4, prostaglandin D 2) § Production of cytokines (TNF, TGF� , IL-4, 5, 6. . . )
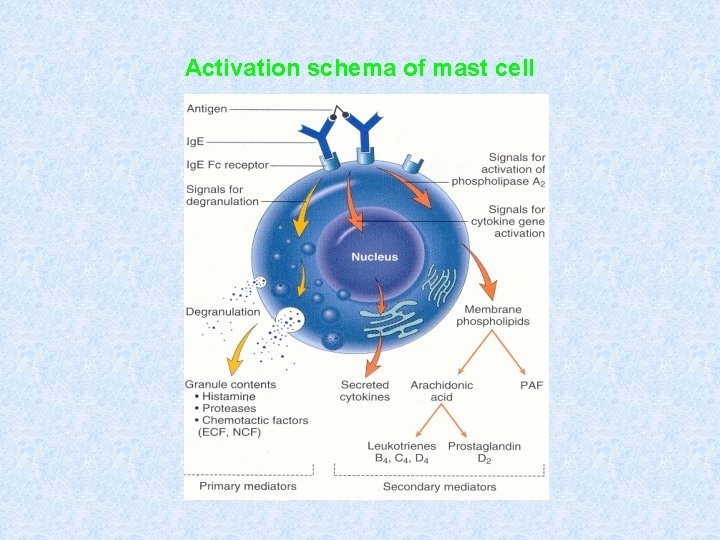
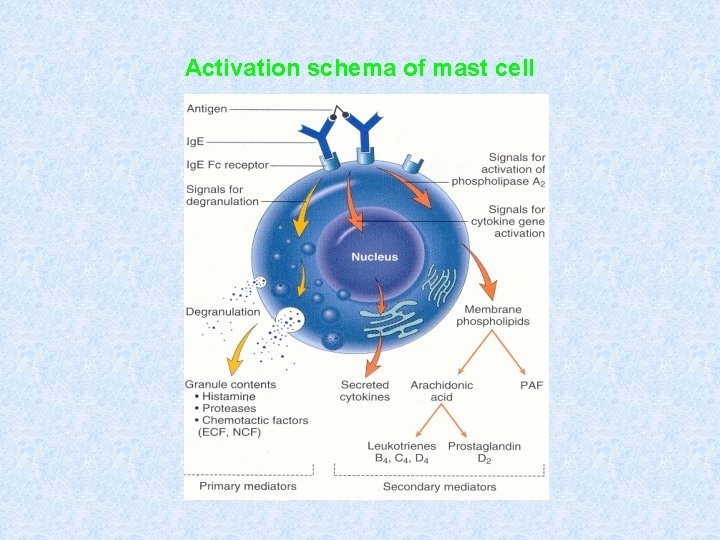
Activation schema of mast cell
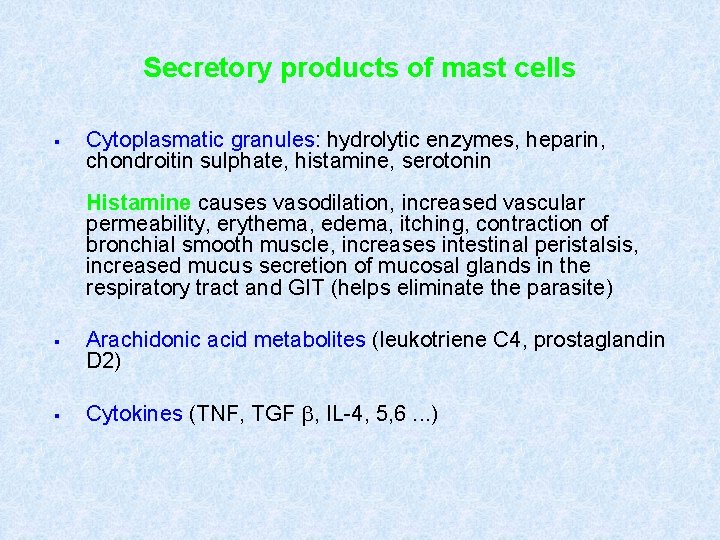
Secretory products of mast cells § Cytoplasmatic granules: hydrolytic enzymes, heparin, chondroitin sulphate, histamine, serotonin Histamine causes vasodilation, increased vascular permeability, erythema, edema, itching, contraction of bronchial smooth muscle, increases intestinal peristalsis, increased mucus secretion of mucosal glands in the respiratory tract and GIT (helps eliminate the parasite) § § Arachidonic acid metabolites (leukotriene C 4, prostaglandin D 2) Cytokines (TNF, TGF , IL-4, 5, 6. . . )
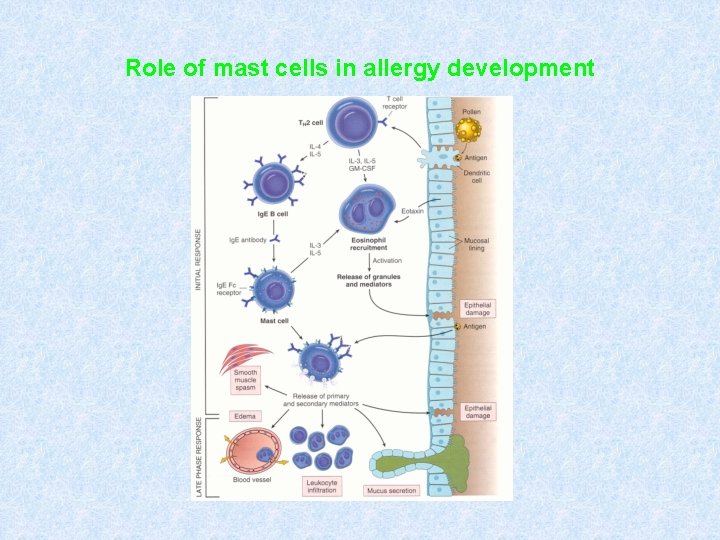
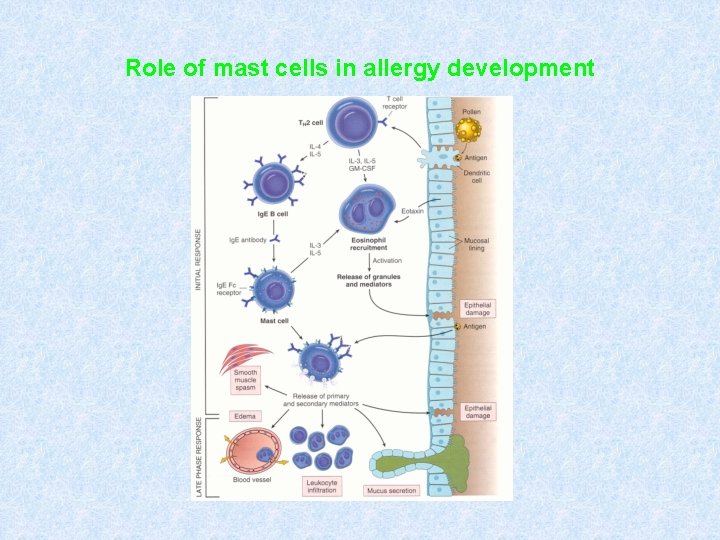
Role of mast cells in allergy development
Basophils § Differentiate from myeloid precursor § They are considered to be the circulating form of mast cells § Receptor equipment, containing granules, the mechanisms of stimulation and functions are very similar to mast cells § They are responsible for the emergence of anaphylactic shock

Complement – clasical pathway https: //www. youtube. com/watch? v=vb. WYz 9 XDt Lw Complement – clasical and alternative pathway https: //www. youtube. com/watch? v=a. Nh 5 A 0 gtu LE NK cells https: //www. youtube. com/watch? v=y. Rnuw. TDR 1 og Immune response https: //www. youtube. com/watch? v=G 7 r. Qu. FZx. V QQ