HPV PAP SCREENING 2013 MCH Alameda Health System




- Slides: 53
HPV & PAP SCREENING 2013 MCH Alameda Health System Michele Bunker-Alberts, FNP-BC, DNP (s)
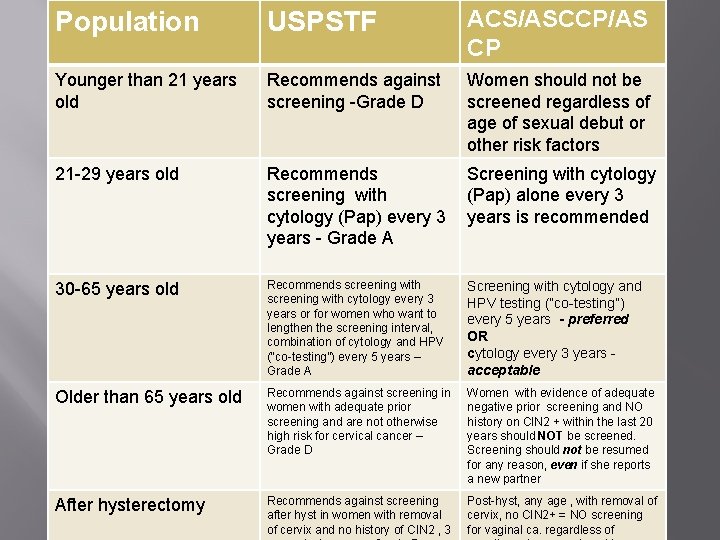
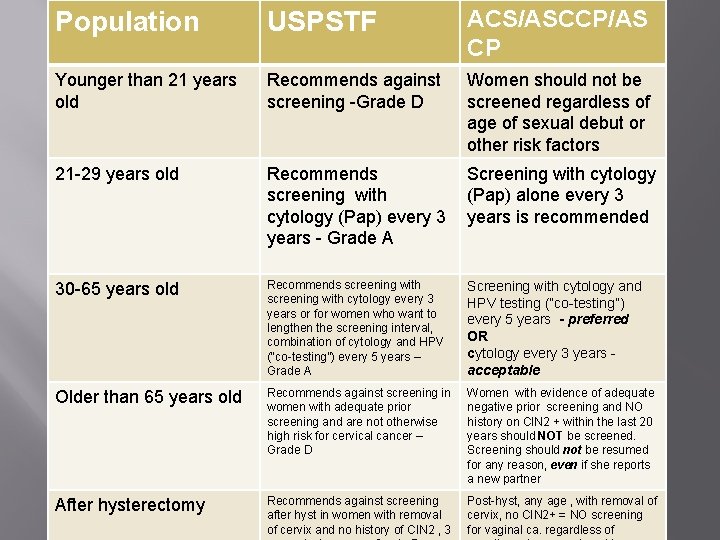
Population USPSTF ACS/ASCCP/AS CP Younger than 21 years old Recommends against screening -Grade D Women should not be screened regardless of age of sexual debut or other risk factors 21 -29 years old Recommends screening with cytology (Pap) every 3 years - Grade A Screening with cytology (Pap) alone every 3 years is recommended 30 -65 years old Recommends screening with cytology every 3 years or for women who want to lengthen the screening interval, combination of cytology and HPV (“co-testing”) every 5 years – Grade A Screening with cytology and HPV testing (“co-testing”) every 5 years - preferred OR cytology every 3 years acceptable Older than 65 years old Recommends against screening in women with adequate prior screening and are not otherwise high risk for cervical cancer – Grade D Women with evidence of adequate negative prior screening and NO history on CIN 2 + within the last 20 years should NOT be screened. Screening should not be resumed for any reason, even if she reports a new partner After hysterectomy Recommends against screening after hyst in women with removal of cervix and no history of CIN 2 , 3 Post-hyst, any age , with removal of cervix, no CIN 2+ = NO screening for vaginal ca. regardless of
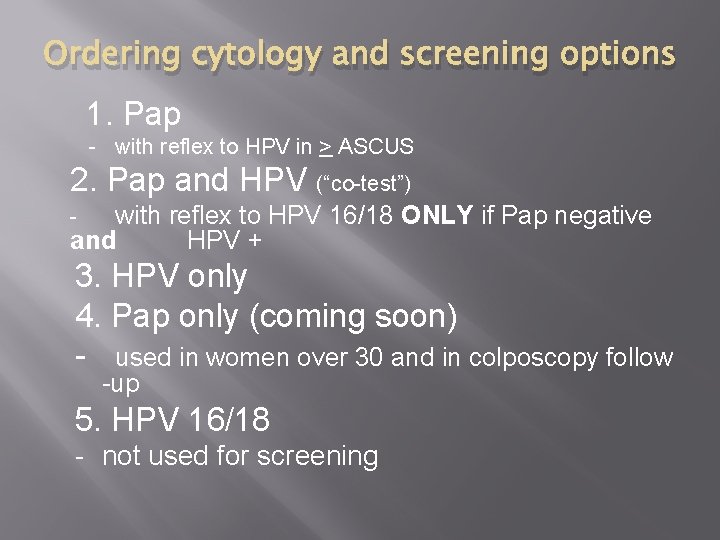
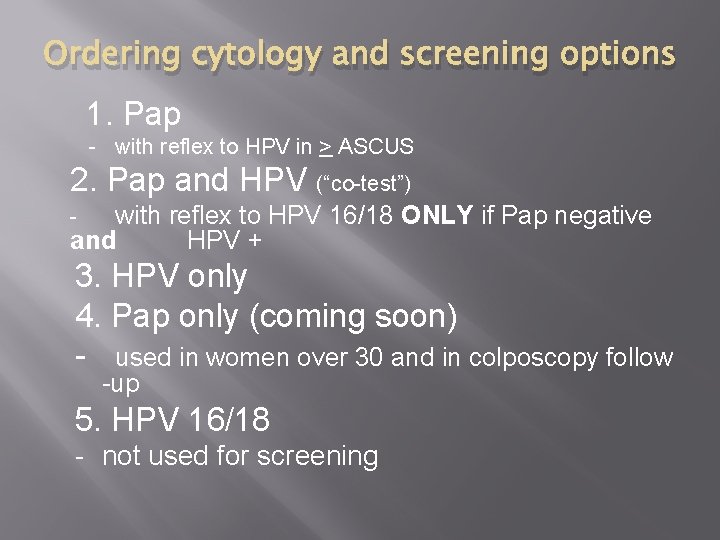
Ordering cytology and screening options 1. Pap - with reflex to HPV in > ASCUS 2. Pap and HPV (“co-test”) with reflex to HPV 16/18 ONLY if Pap negative and HPV + - 3. HPV only 4. Pap only (coming soon) - used in women over 30 and in colposcopy follow -up 5. HPV 16/18 - not used for screening
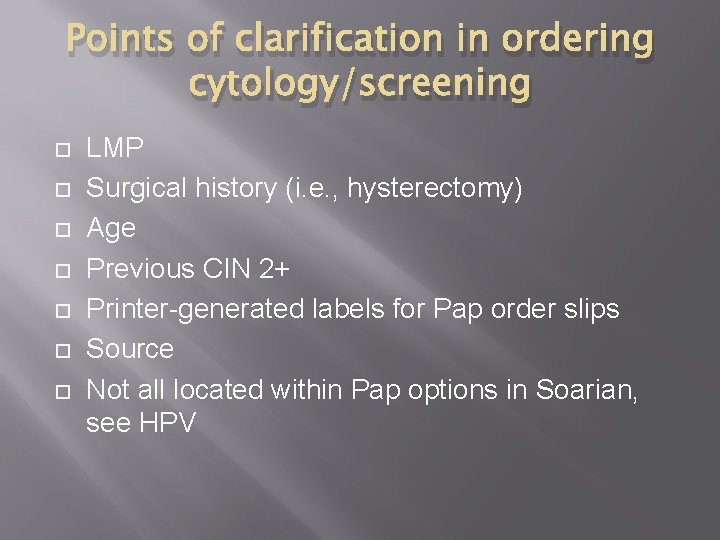
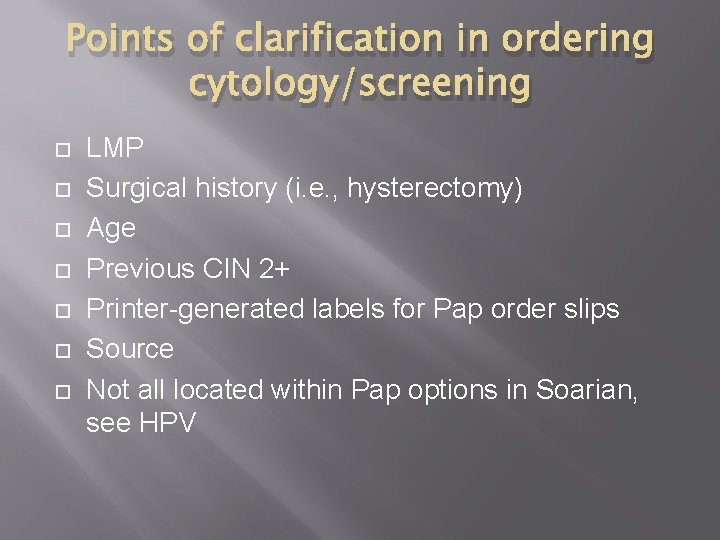
Points of clarification in ordering cytology/screening LMP Surgical history (i. e. , hysterectomy) Age Previous CIN 2+ Printer-generated labels for Pap order slips Source Not all located within Pap options in Soarian, see HPV
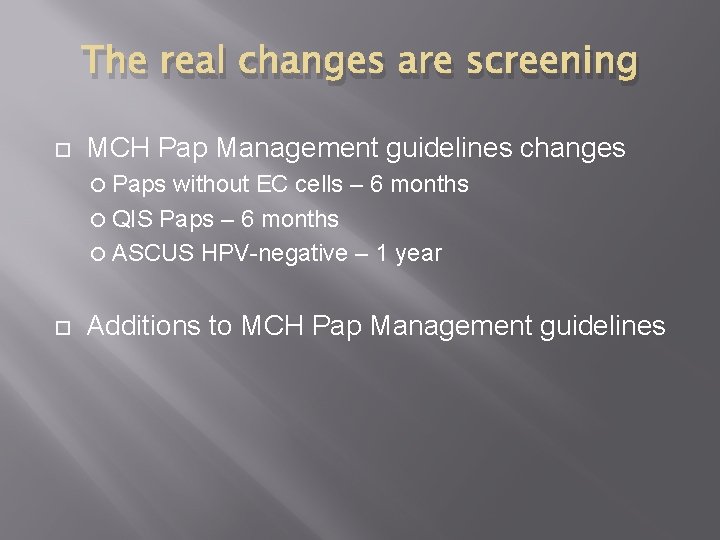
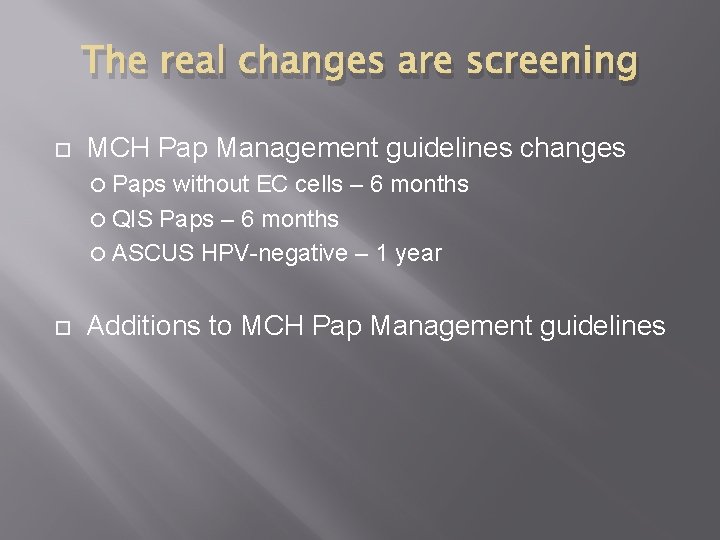
The real changes are screening MCH Pap Management guidelines changes Paps without EC cells – 6 months QIS Paps – 6 months ASCUS HPV-negative – 1 year Additions to MCH Pap Management guidelines
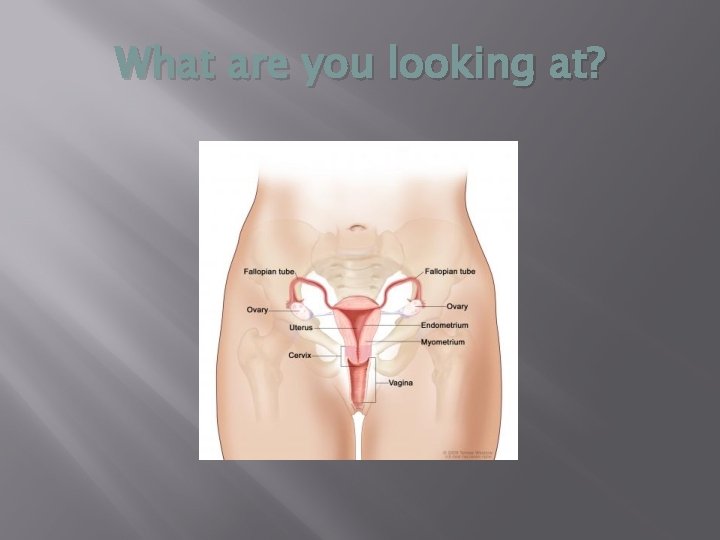
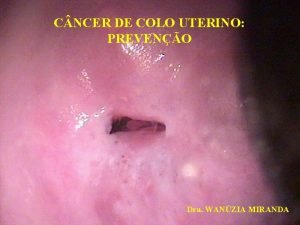
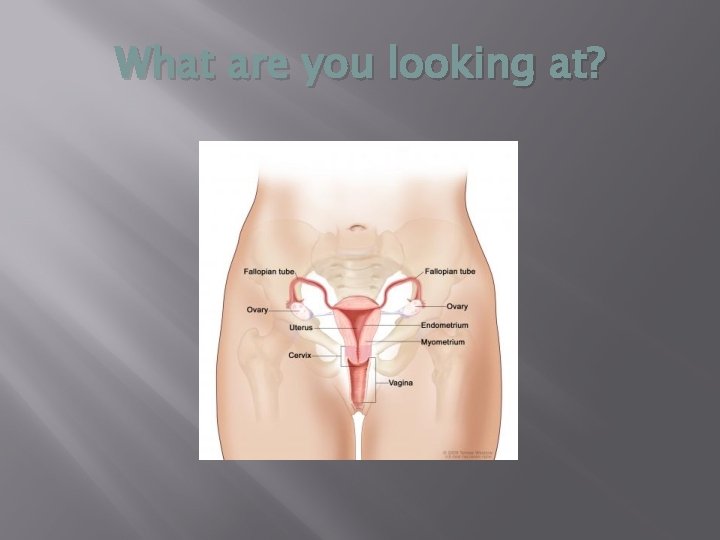
What are you looking at?
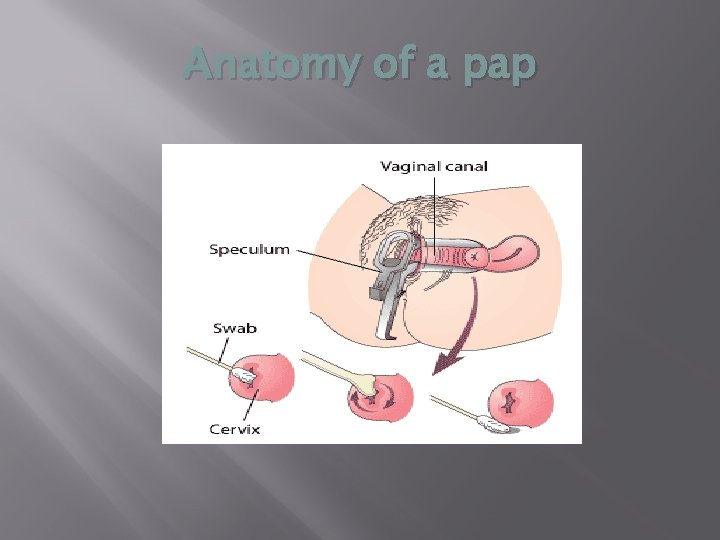
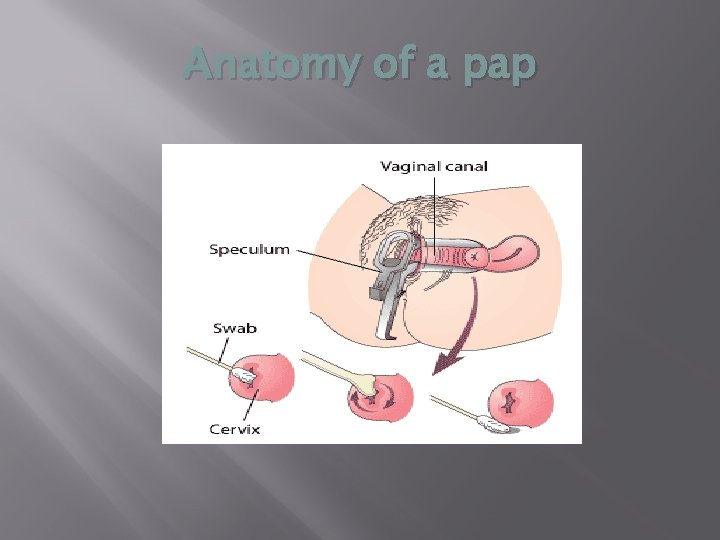
Anatomy of a pap
Types of paps Thin prep Liquid-based Most common Traditional slides Reflex testing HPV in the presence of abnormal cells Routine HPV testing for women > 30 yo Di-gene
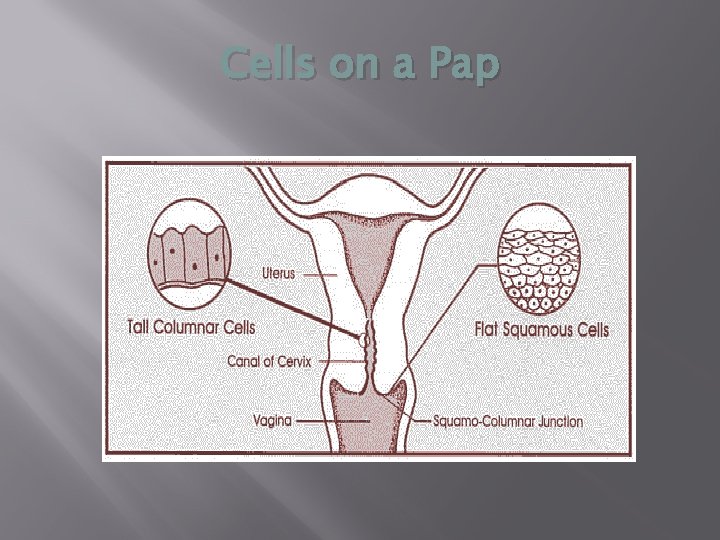
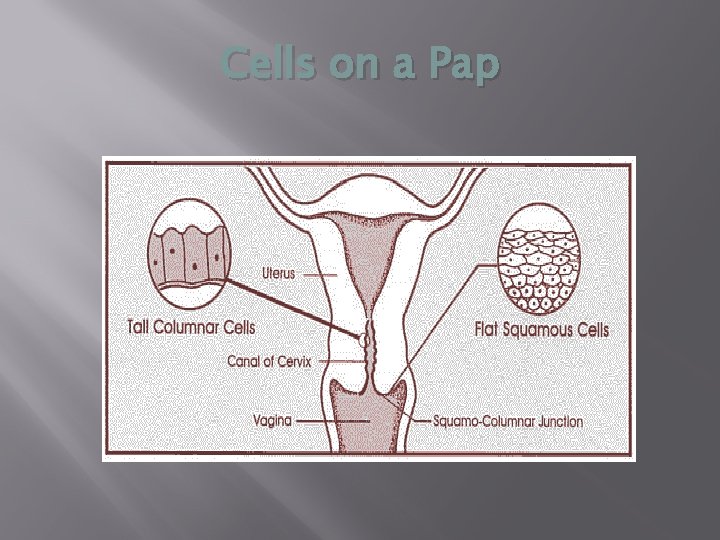
Cells on a Pap
Pap analogy
Dominga 38 years old G 4 P 4 Emigrated to US in 2006 1 child (here) Undocumented 1 st language Mam 2 nd language Spanish No previous Paps Limited access to care Language barriers
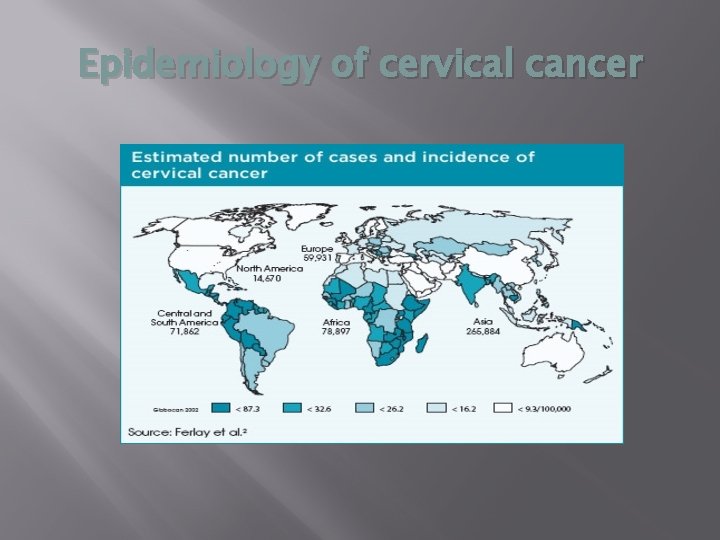
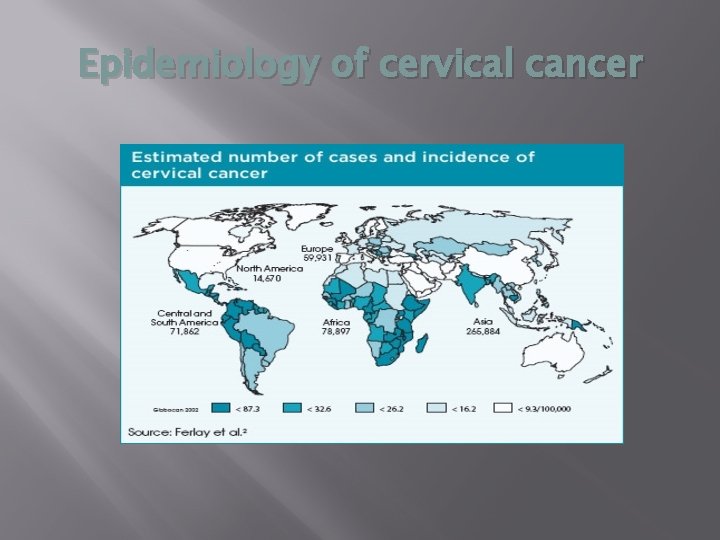
Epidemiology of cervical cancer
Tatiana • • • 28 years old G 4 P 2 Incarcerated Episodic care Low-income Sexually exploited Hx abnormal pap • Care coordination • Health literacy
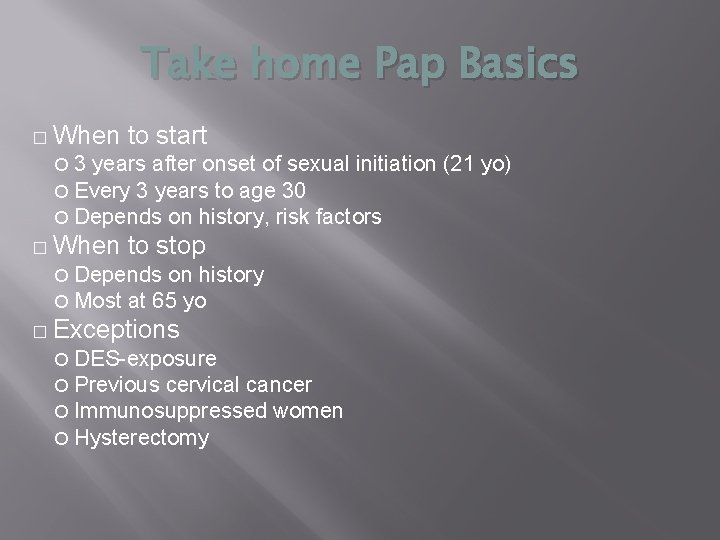
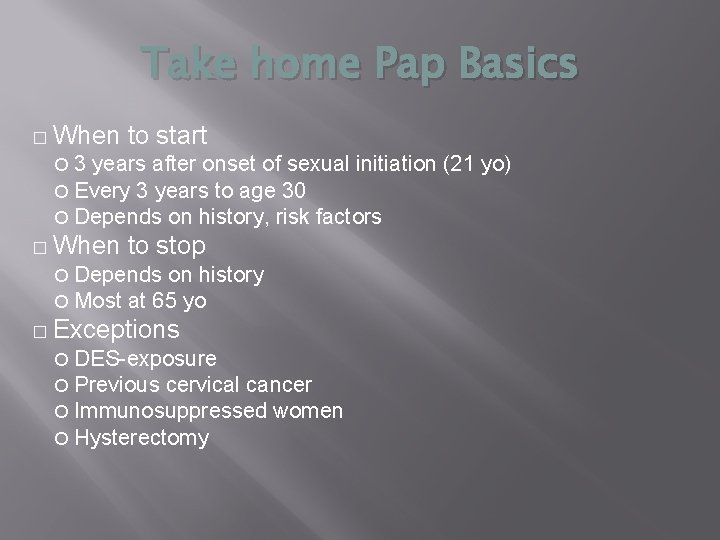
Take home Pap Basics � When 3 years after onset of sexual initiation (21 yo) Every 3 years to age 30 Depends on history, risk factors � When to start to stop Depends on history Most at 65 yo � Exceptions DES-exposure Previous cervical cancer Immunosuppressed women Hysterectomy
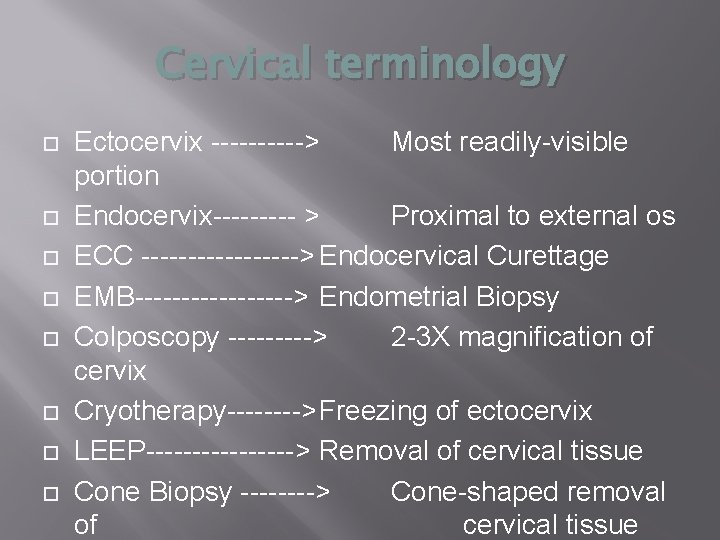
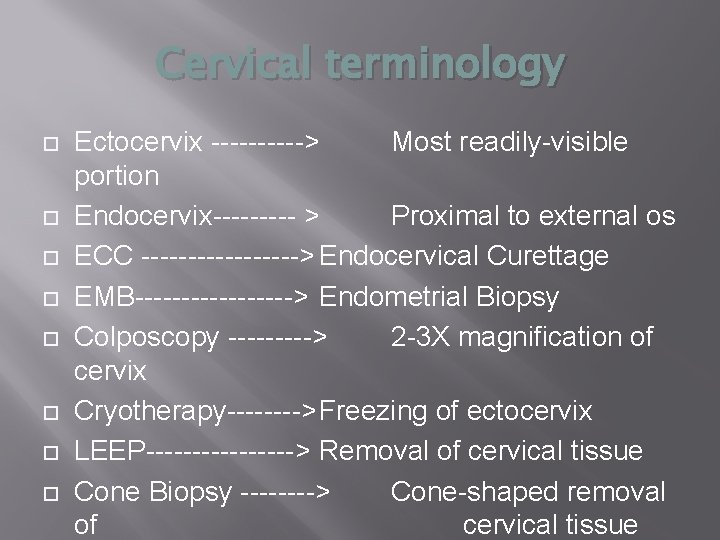
Cervical terminology Ectocervix -----> Most readily-visible portion Endocervix----- > Proximal to external os ECC ---------> Endocervical Curettage EMB---------> Endometrial Biopsy Colposcopy -----> 2 -3 X magnification of cervix Cryotherapy---->Freezing of ectocervix LEEP--------> Removal of cervical tissue Cone Biopsy ----> Cone-shaped removal of cervical tissue
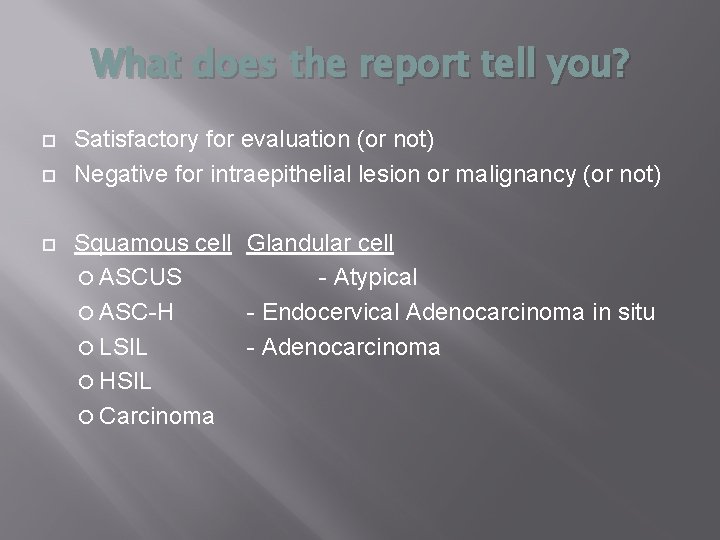
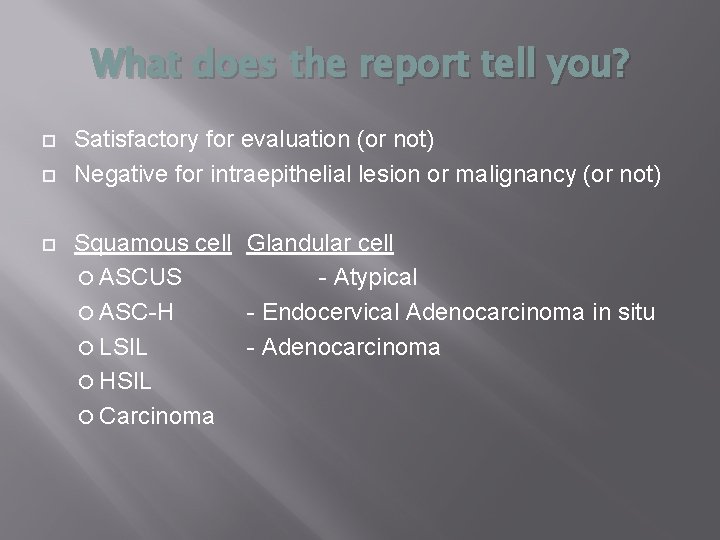
What does the report tell you? Satisfactory for evaluation (or not) Negative for intraepithelial lesion or malignancy (or not) Squamous cell Glandular cell ASCUS - Atypical ASC-H - Endocervical Adenocarcinoma in situ LSIL - Adenocarcinoma HSIL Carcinoma
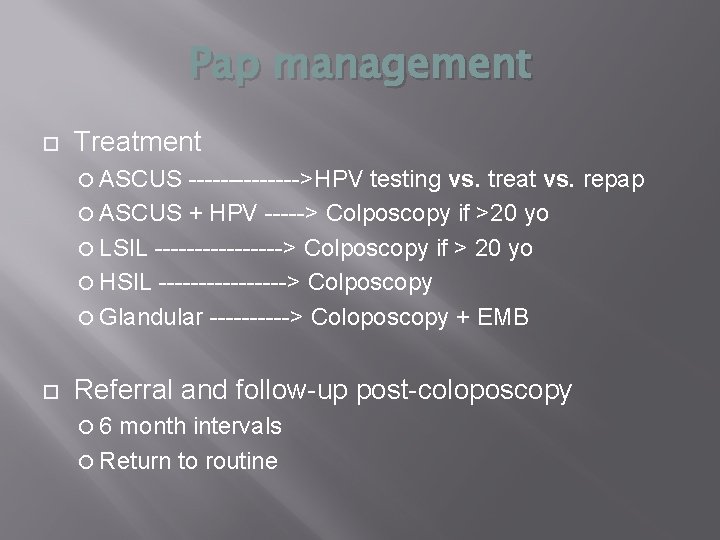
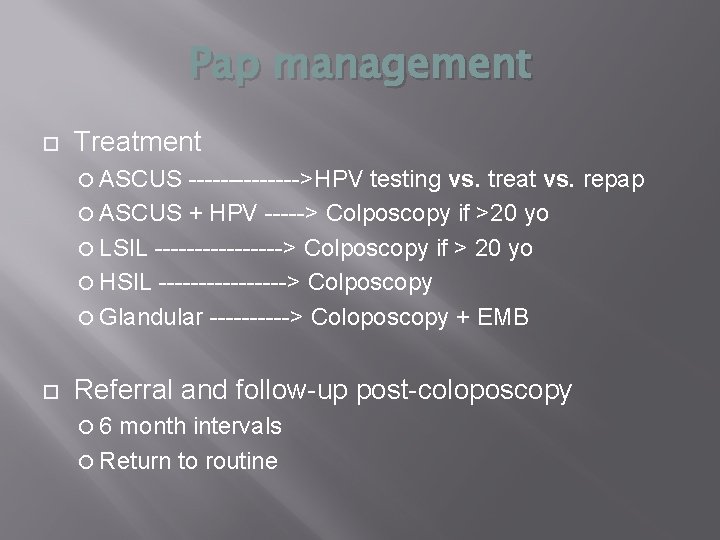
Pap management Treatment ASCUS ------->HPV testing vs. treat vs. repap ASCUS + HPV -----> Colposcopy if >20 yo LSIL --------> Colposcopy if > 20 yo HSIL --------> Colposcopy Glandular -----> Coloposcopy + EMB Referral and follow-up post-coloposcopy 6 month intervals Return to routine
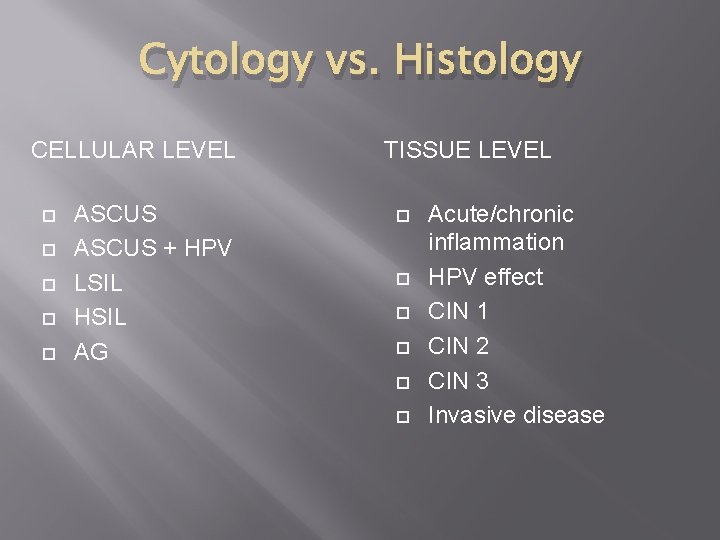
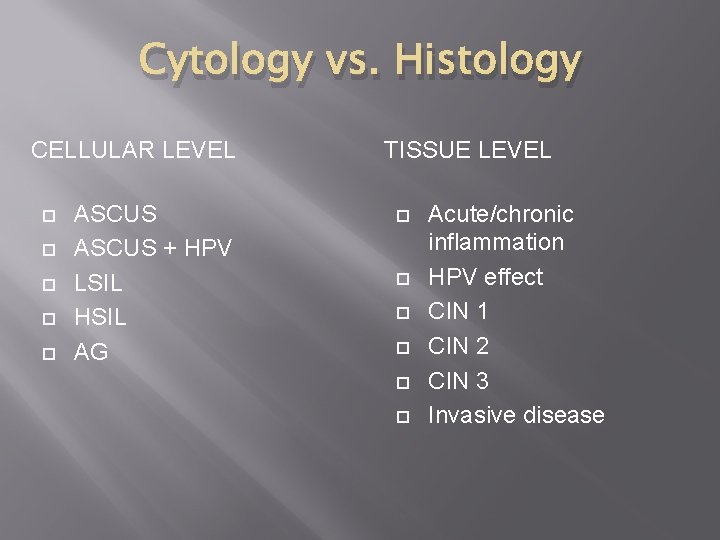
Cytology vs. Histology CELLULAR LEVEL ASCUS + HPV LSIL HSIL AG TISSUE LEVEL Acute/chronic inflammation HPV effect CIN 1 CIN 2 CIN 3 Invasive disease

Basically normal cervix Colposcopic view
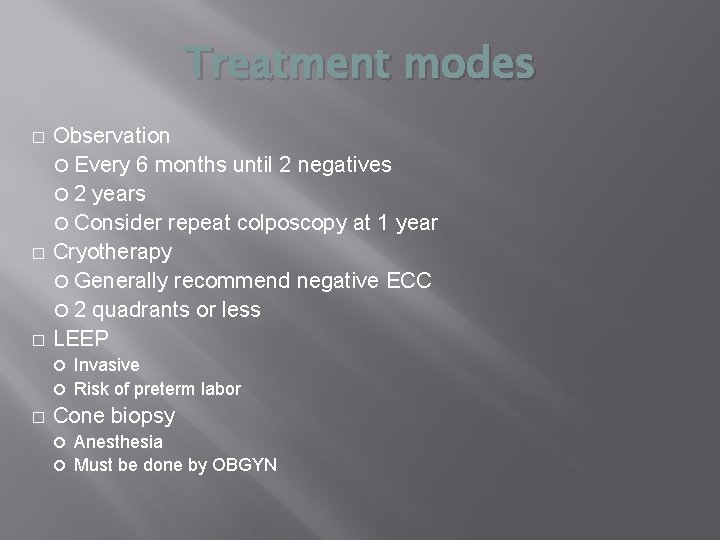
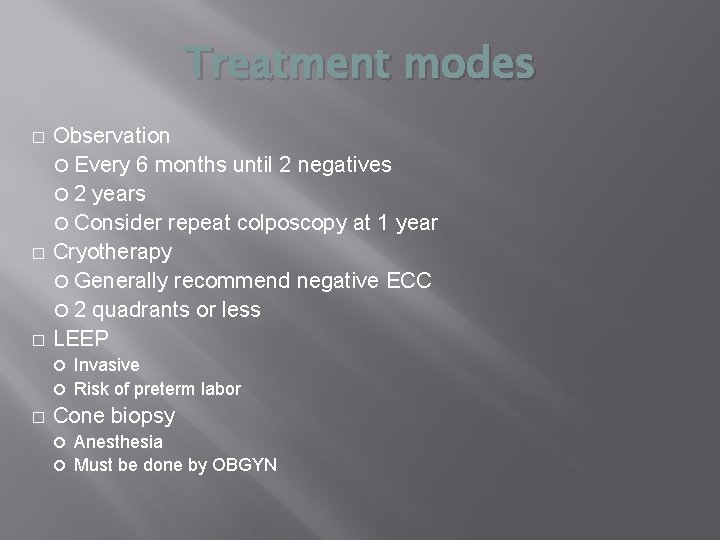
Treatment modes � � � Observation Every 6 months until 2 negatives 2 years Consider repeat colposcopy at 1 year Cryotherapy Generally recommend negative ECC 2 quadrants or less LEEP Invasive Risk of preterm labor � Cone biopsy Anesthesia Must be done by OBGYN
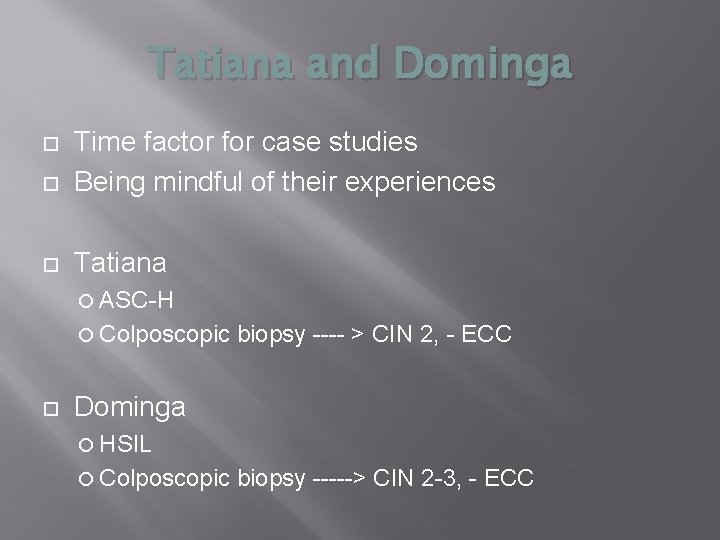
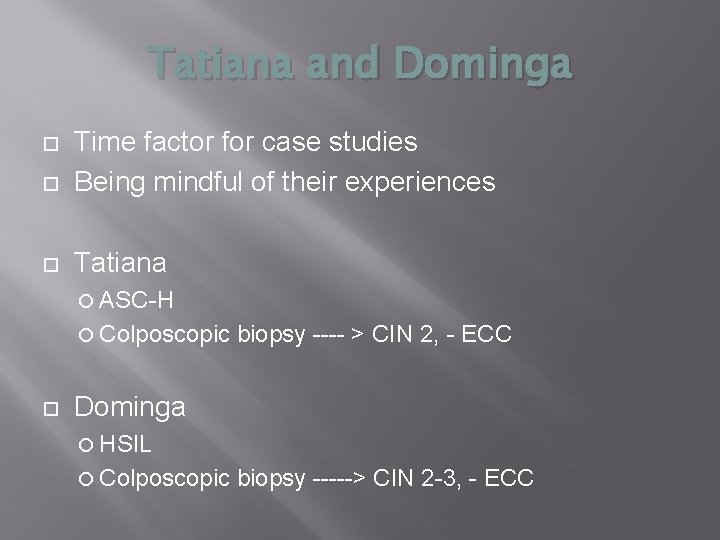
Tatiana and Dominga Time factor for case studies Being mindful of their experiences Tatiana ASC-H Colposcopic biopsy ---- > CIN 2, - ECC Dominga HSIL Colposcopic biopsy -----> CIN 2 -3, - ECC
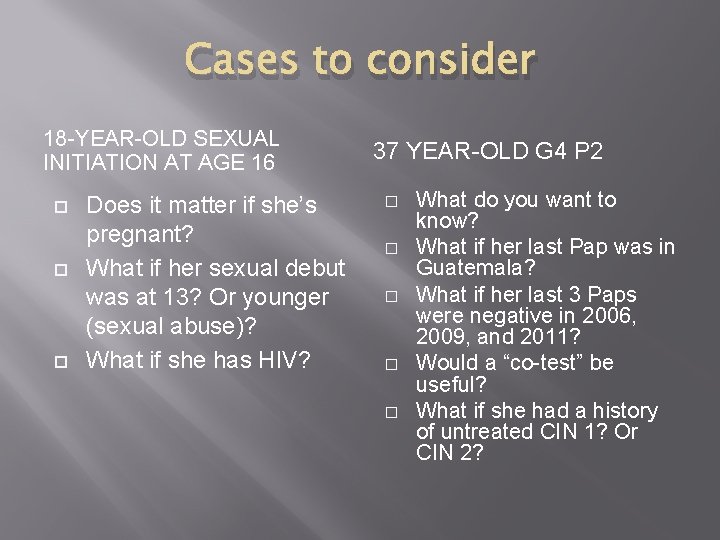
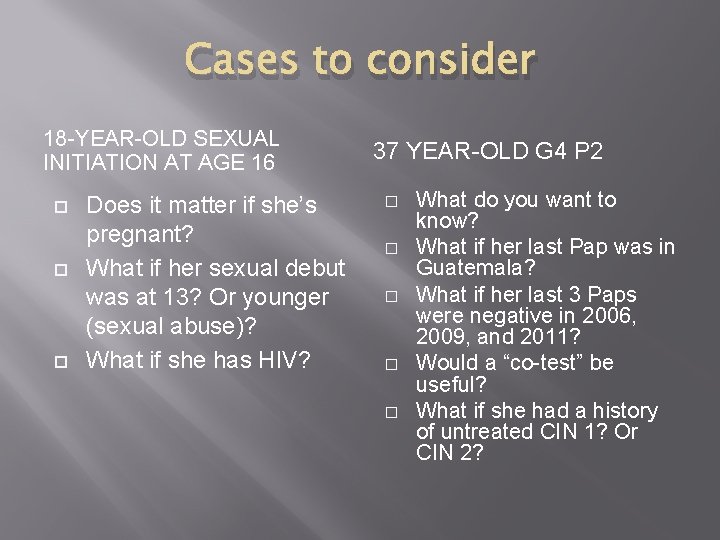
Cases to consider 18 -YEAR-OLD SEXUAL INITIATION AT AGE 16 Does it matter if she’s pregnant? What if her sexual debut was at 13? Or younger (sexual abuse)? What if she has HIV? 37 YEAR-OLD G 4 P 2 � � � What do you want to know? What if her last Pap was in Guatemala? What if her last 3 Paps were negative in 2006, 2009, and 2011? Would a “co-test” be useful? What if she had a history of untreated CIN 1? Or CIN 2?
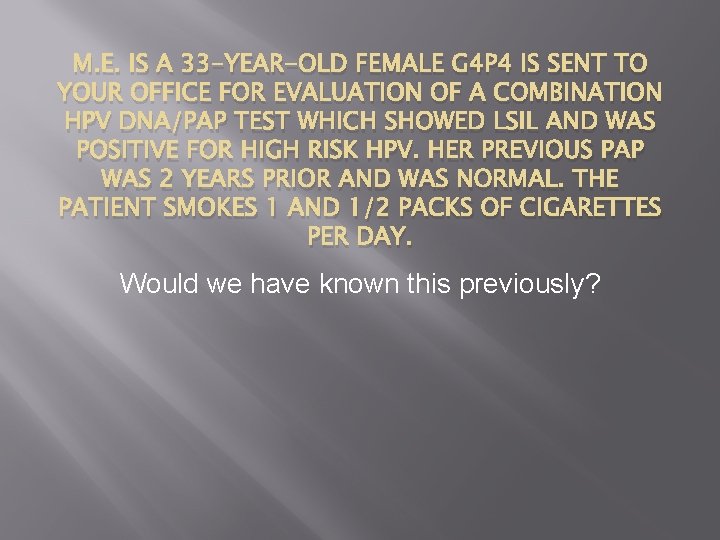
M. E. IS A 33 -YEAR-OLD FEMALE G 4 P 4 IS SENT TO YOUR OFFICE FOR EVALUATION OF A COMBINATION HPV DNA/PAP TEST WHICH SHOWED LSIL AND WAS POSITIVE FOR HIGH RISK HPV. HER PREVIOUS PAP WAS 2 YEARS PRIOR AND WAS NORMAL. THE PATIENT SMOKES 1 AND 1/2 PACKS OF CIGARETTES PER DAY. Would we have known this previously?
LSIL pap questions Identify the common clinical risk factors for cervical dysplasia and cancer. Does M. E. have any of these risk factors? What is the initial management plan of a patient with this abnormal pap smear

CIN level regress Persist at same level progress invasive CIN I 60 30 10 1 CIN II 40 35 20 5 CIN III 30 50 80 12

A 20 -year-old nulligravida presents for her first pelvic examination. She has never been sexually active but has heard that she should be tested for HPV. What do you offer her?
A 35 -year-old woman presents for a Pap test. Although she had a history of cervical intraepithelial neoplasia 2 (CIN 2) in her 20 s, her last 2 Pap tests and HPV tests were negative. She asks you to perform an HPV test. What do you offer her?
An 80 -year-old woman presents for her annual examination. She has never had an abnormal Pap result, nor has she had a hysterectomy. She asks you not to perform a pelvic examination. What do you recommend?
A 35 -year-old woman presents at 15 weeks’ gestation for her first prenatal examination. She has had 2 normal Pap results and wonders why you need to repeat the test, as she is worried about the complications of performing a Pap test during pregnancy. How do you counsel her?
A 40 -year-old woman who is HIV-positive presents for her annual examination. She wonders if she needs more frequent cervical cancer screening. How do you counsel her?

A 60 -year-old woman presents for her annual visit. She had a hysterectomy 30 years ago for “fibroids. ” She recalls a remote history of abnormal Pap test results in her “ 20 s. ” She wonders if she needs a Pap test and an HPV test. How do you counsel her?
A 55 -year-old woman presents for her annual examination. She reports that at age 48 she had a hysterectomy for cervical cancer. She has been without evidence of disease since then and wonders if she needs annual screening and HPV testing. How do you counsel her?
A 20 -year-old presents for her annual examination. She had received the 3 HPV vaccinations 1 year prior to this visit. She asks you whether she needs routine Pap screening with or without the HPV test. What do you tell her?
A 35 -year-old presents for follow-up regarding her recent Pap test. She has no history of abnormal Pap results but most recently had a positive HPV result with a normal Pap. How do you counsel her regarding follow-up?
A 23 -year-old presents for her annual exam with her partner. She has received the HPV vaccination and is wondering whether partner should get vaccinated. What do you tell her?
A 16 -year-old presents for her first annual exam. Her mother asks you about HPV vaccination and which of the 2 vaccines, Gardasil or Cervarix, is best for her daughter. How do you counsel her about the difference between the 2 vaccines?
LSIL in Postmenopausal Women What are acceptable management options HPV testing Repeat cytology at 6 and 12 months Colposcopy ? Estrogen…….
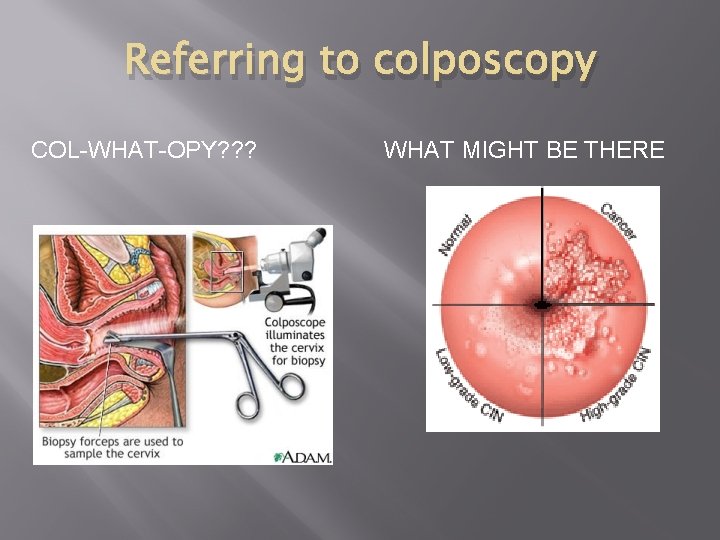
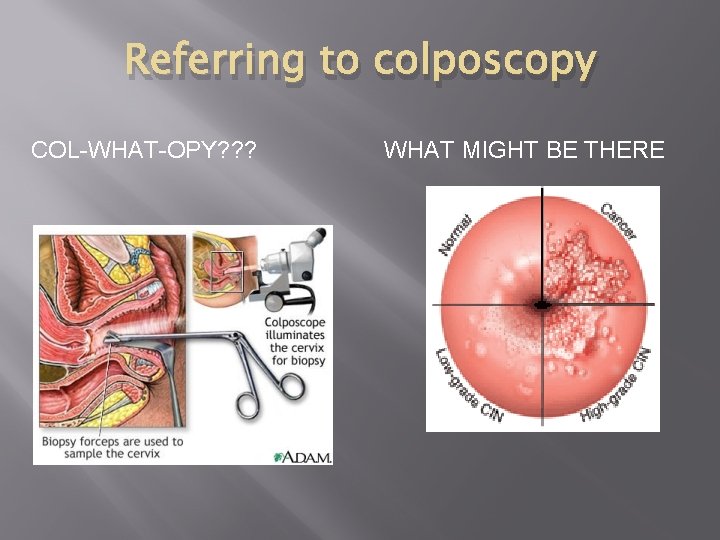
Referring to colposcopy COL-WHAT-OPY? ? ? WHAT MIGHT BE THERE
Becoming a colposcopist Courses vary Basic training Supervision Certification Consider volunteering Observation usually possible PINCC – Oakland organization Other medical missions
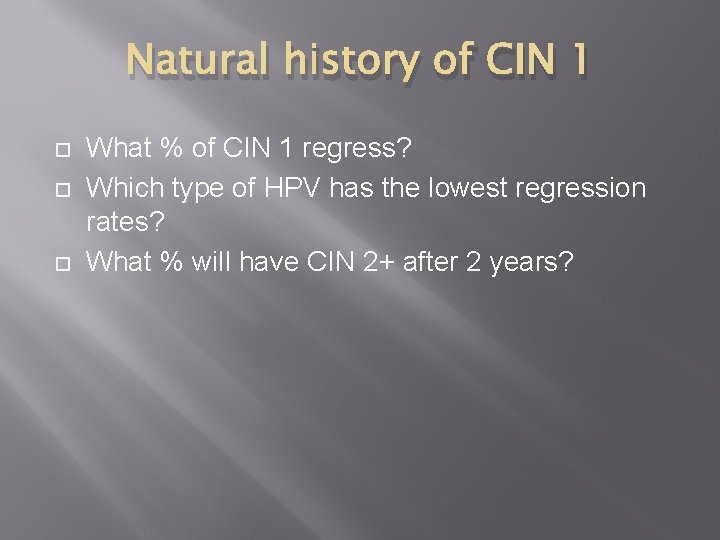
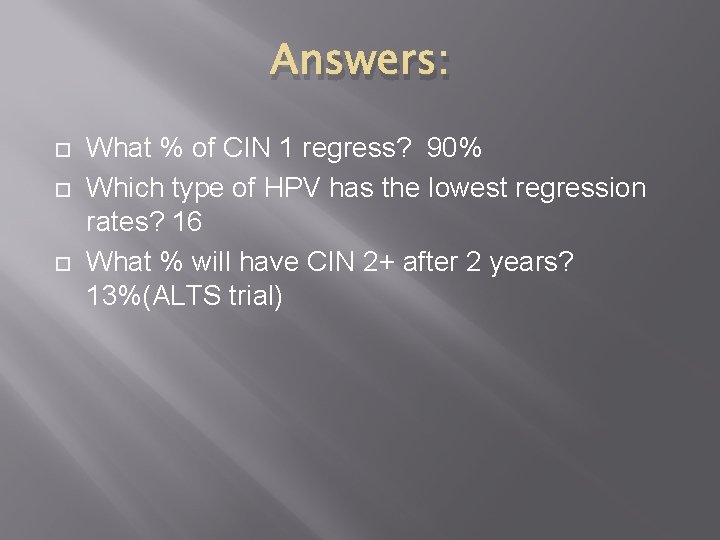
Natural history of CIN 1 What % of CIN 1 regress? Which type of HPV has the lowest regression rates? What % will have CIN 2+ after 2 years?
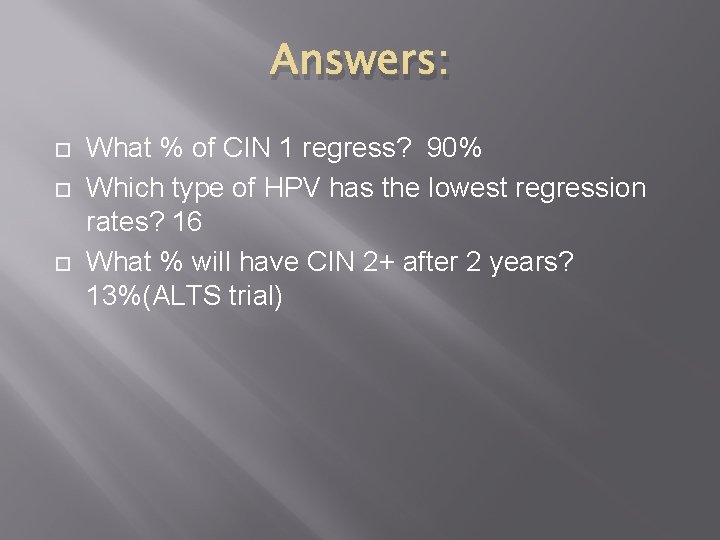
Answers: What % of CIN 1 regress? 90% Which type of HPV has the lowest regression rates? 16 What % will have CIN 2+ after 2 years? 13%(ALTS trial)
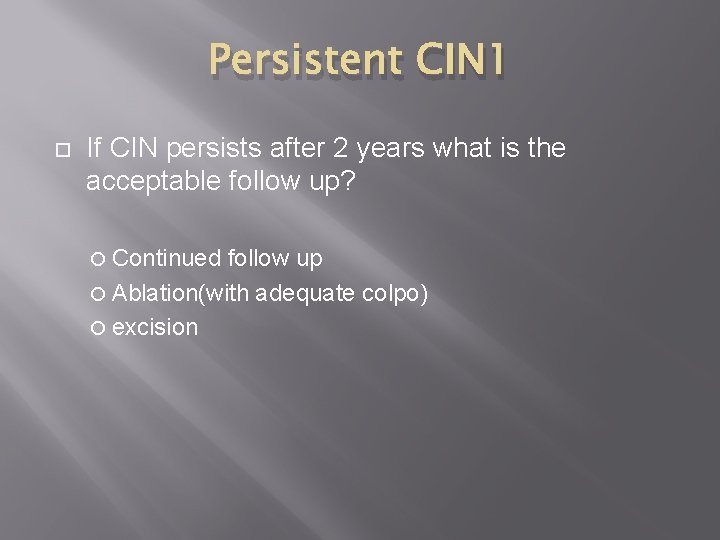
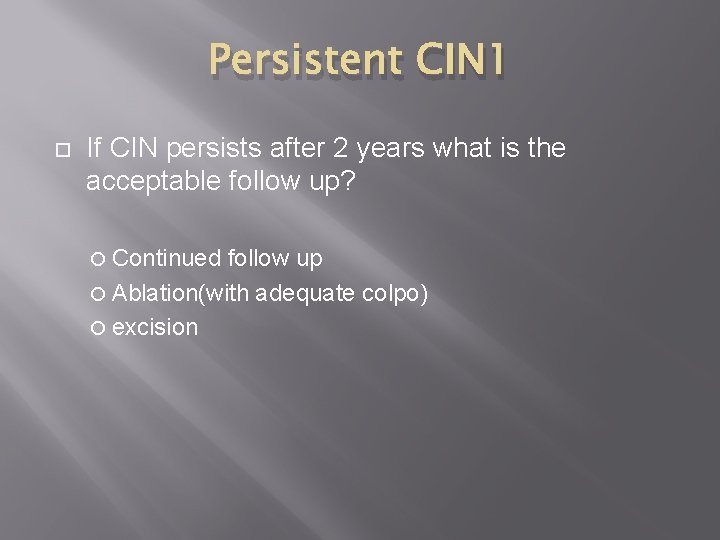
Persistent CIN 1 If CIN persists after 2 years what is the acceptable follow up? Continued follow up Ablation(with adequate colpo) excision
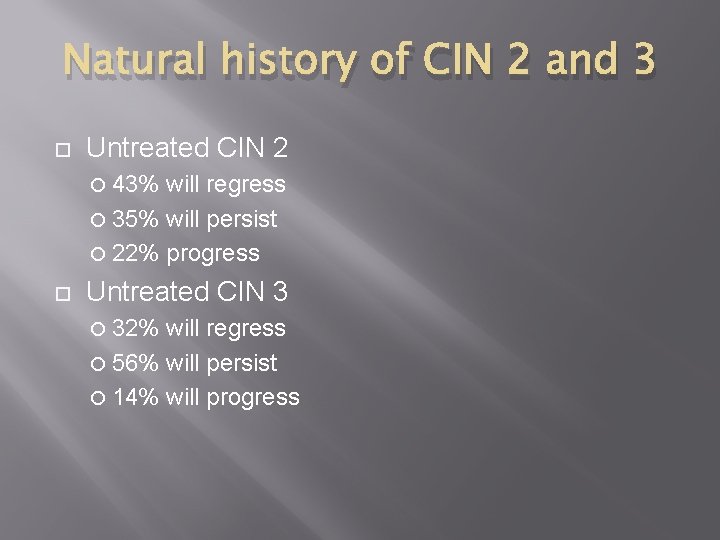
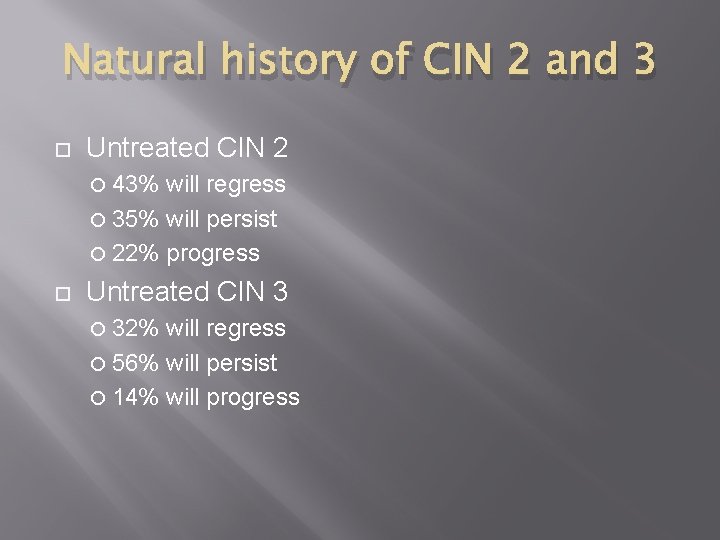
Natural history of CIN 2 and 3 Untreated CIN 2 43% will regress 35% will persist 22% progress Untreated CIN 3 32% will regress 56% will persist 14% will progress
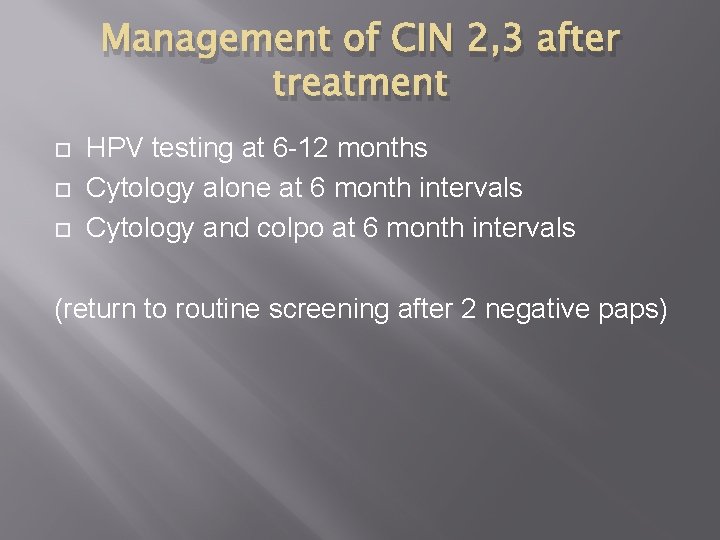
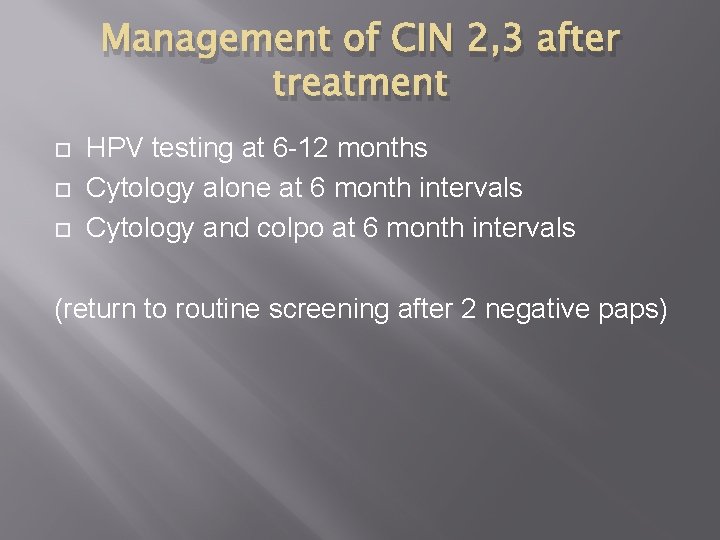
Management of CIN 2, 3 after treatment HPV testing at 6 -12 months Cytology alone at 6 month intervals Cytology and colpo at 6 month intervals (return to routine screening after 2 negative paps)
Management of CIN 2, 3 residual disease i. e. CIN 2, 3 is identified at the margins of a diagnostic excisional procedure or in an ECC obtained immediately after the procedure
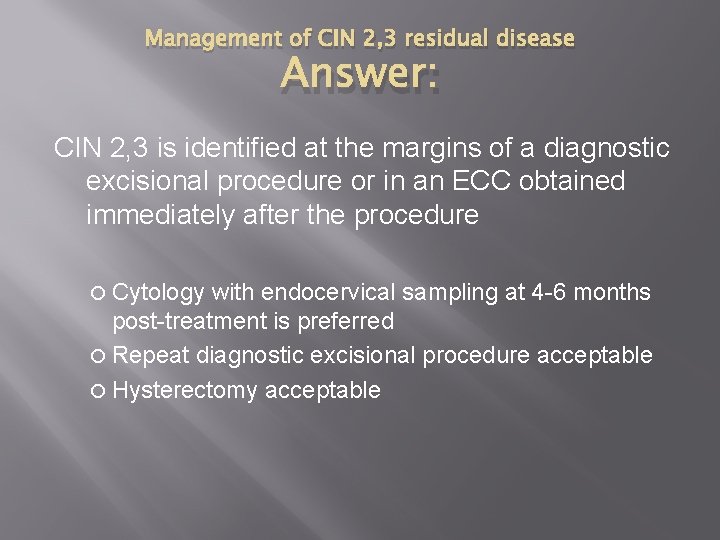
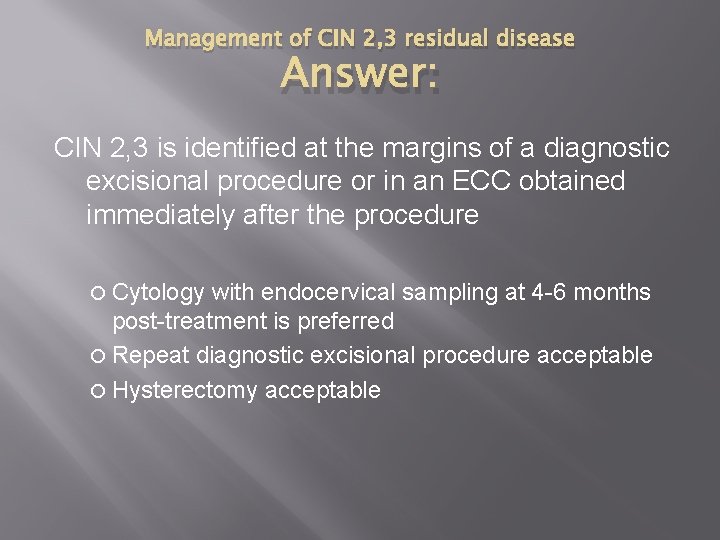
Management of CIN 2, 3 residual disease Answer: CIN 2, 3 is identified at the margins of a diagnostic excisional procedure or in an ECC obtained immediately after the procedure Cytology with endocervical sampling at 4 -6 months post-treatment is preferred Repeat diagnostic excisional procedure acceptable Hysterectomy acceptable
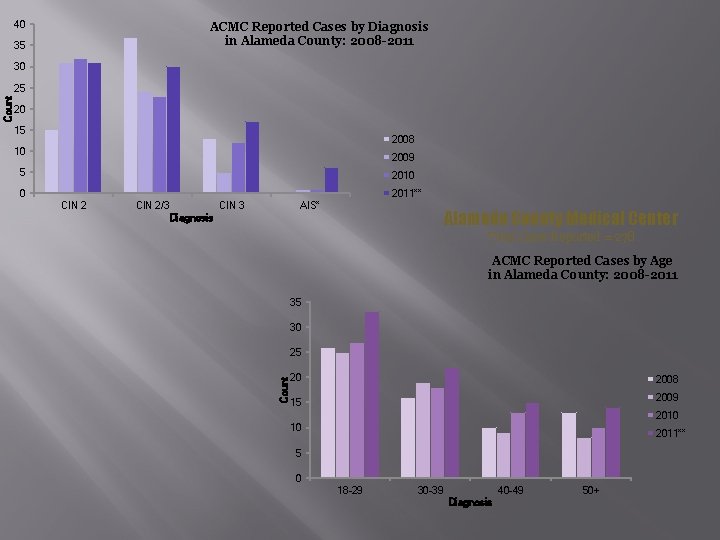
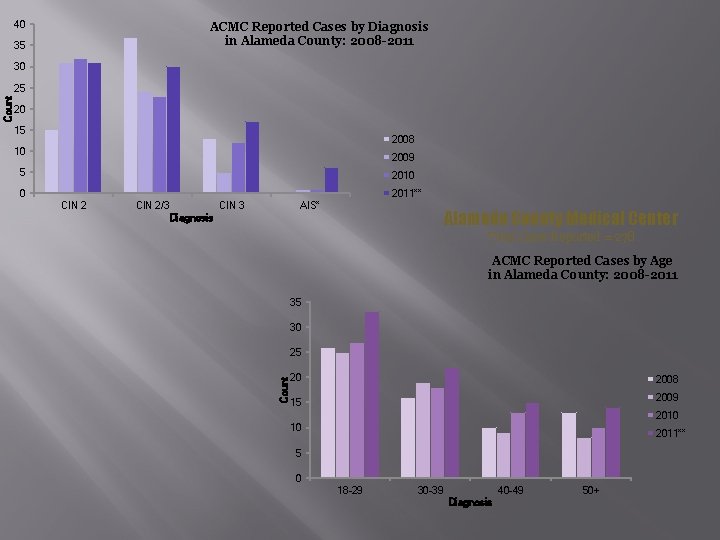
40 ACMC Reported Cases by Diagnosis in Alameda County: 2008 -2011 35 30 20 15 2008 10 2009 5 2010 2011** 0 CIN 2/3 CIN 3 AIS* Alameda County Medical Center Diagnosis Total Cases Reported = 278 ACMC Reported Cases by Age in Alameda County: 2008 -2011 35 30 25 Count 25 20 2008 2009 15 2010 10 2011** 5 0 18 -29 30 -39 40 -49 Diagnosis 50+
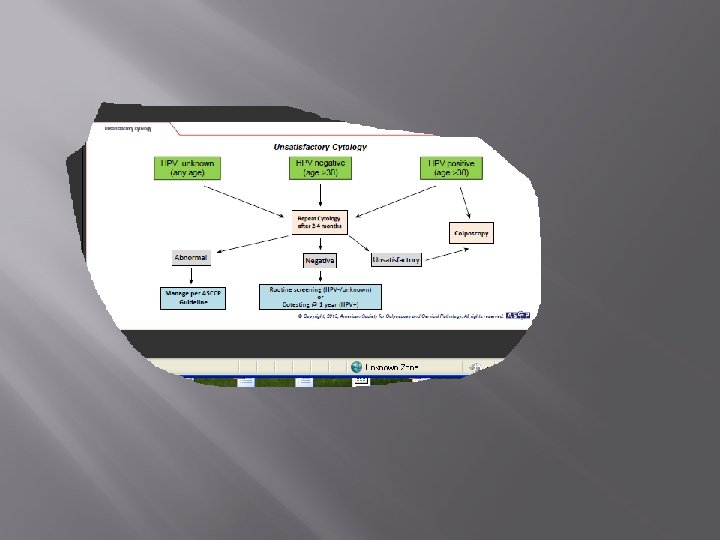
Algorithms http: //www. asccp. org/pdfs/consensus/algorithms _hist_07. pdf http: //www. asccp. org/pdfs/consensus/algorithms _cyto_07. pdf
Resource guides http: //www. familypact. org/Files/CPA_Manageme nt. Of. Abnormal. Cervical. Cytology 6 -27 -2008. pdf www. policarlectures. com
References ACS, American Cancer Society. (2005). Guatemala Proposal: Curbing Cervical Cancer by Building Capacity in Early Education Continuing Education of Cytotechnologists & Visual Inspection with Acetic Acid (VIAA). Atlanta, GA: American Cancer Society, Mid-South Division, International Partnership Program. IARC (2002) Handbook on Cancer Prevention, vol 10, Global Field Experiences JHPIEGO (2001). Cervical Cancer Prevention Guidelines for Low. Resource Settings �DRAFT. Baltimore: Johns Hopkins University. IARC (2002). GLOBOCAN: http: //wwwdep. iarc. fr/globocan/database. htm. Magee, C, et al (2005). Preventive Care for Women in Prison: a Qualitative Community Assessment of the Papanicolaou Test and Follow -up Treatment in California State Women’s Prison, Am J Public Health, 95: 1712 -1717.
References Arguto, I. B. , A. ; Sanchez, G; Betancourt, Z; Robles, S. (2004). Perceived barriers and benefits to cervical cancer screening in Latin America. Preventative Medicine, 39, 91 -98. Blumenthal, G. , L. and Emerson, M. (2003). Implementing Cervical Cancer Screening in Underserved Communities. The Lancet, 10(8), 405 -406. Munoz, N. , From causality to prevention - the example of cervical cancer: my personal contribution to this fascinating history. Public Health Genomics. 2009; 12(5 -6): 368 -71. Epub 2009 Aug 11. Sankaranarayanan, R. , Budukh, A. M. , & Rajkumar, R. (2001). Effective screening programmes for cervical cancer in low- and middle-income developing countries. Bulletin of the World Health Organization, 79(10), 954962. Schiffman M, Clifford G, Buonagro FM. , Classification of weakly carcinogenic human papillomavirus types: addressing the limits of epidemiology at the borderline. Infect Agent Cancer. 2009 Jun 1; 4: 8.
 Alameda county health care for the homeless
Alameda county health care for the homeless Menghitung mcv mch mchc
Menghitung mcv mch mchc Mch indicators
Mch indicators Maternal and child health services
Maternal and child health services Mch indicators full form
Mch indicators full form Mch indicators full form
Mch indicators full form Florida state computer science
Florida state computer science Trombosit histogram
Trombosit histogram Funcion del chipset
Funcion del chipset Mch blood test high
Mch blood test high Cbc with esr
Cbc with esr Anemia mikrositik
Anemia mikrositik Rumus hematokrit
Rumus hematokrit Mch card
Mch card Trofozoiet
Trofozoiet Hpv test for men
Hpv test for men Hpv oral cancer
Hpv oral cancer Hpv vaccine schedule adults
Hpv vaccine schedule adults Hpv cancer prevention
Hpv cancer prevention Hpv testi nasıl yapılır
Hpv testi nasıl yapılır Triage sort
Triage sort Does hpv go away
Does hpv go away Paplloma
Paplloma Hpv type 16 and 18
Hpv type 16 and 18 Hpv type 16 and 18
Hpv type 16 and 18 Dysplasibarnmorska
Dysplasibarnmorska 9 valanlı hpv aşısı
9 valanlı hpv aşısı Hpv
Hpv Hpv
Hpv Hpv cervical cancer
Hpv cervical cancer Wanzia
Wanzia Hpv cervical cancer
Hpv cervical cancer Hpv us
Hpv us Hpv testi nasıl yapılır
Hpv testi nasıl yapılır Hpv infektion
Hpv infektion Hpv
Hpv Genital warts
Genital warts Prevention hpv
Prevention hpv Hpv
Hpv Hpv infection
Hpv infection Epidermal dysplasia verruciformis
Epidermal dysplasia verruciformis Ahcc hpv
Ahcc hpv Hpv discret test
Hpv discret test Hpv
Hpv First 5 alameda
First 5 alameda Corte de alameda
Corte de alameda Off the grid alameda
Off the grid alameda Alameda soccer club
Alameda soccer club Centerpoint alameda county
Centerpoint alameda county Ausd school board meeting
Ausd school board meeting Ies alameda osuna
Ies alameda osuna Alameda county transportation commission
Alameda county transportation commission Diego rivera dream of a sunday afternoon
Diego rivera dream of a sunday afternoon Alameda county hcsa
Alameda county hcsa