HPV Data and Trends Cancer Prevention Promotion Lois























- Slides: 62
HPV Data and Trends: Cancer Prevention Promotion Lois M Ramondetta MD Professor Gynecologic Oncology Department of Gynecologic Oncology and Reproductive Medicine Chief Gynecologic Oncology LBJ Hospital UT MD Anderson Cancer Center & Harris Health System Philip Huang, MD, MPH Health Authority/Medical Director Austin Public Health
Disclaimer & Disclosures • No conflicts of interest.

Objective 1. Discuss recent trends in HPV infection, HPVrelated cancer and HPV vaccination rates 2. Discuss national, state and local activities related to HPV and HPV-related cancer prevention and control
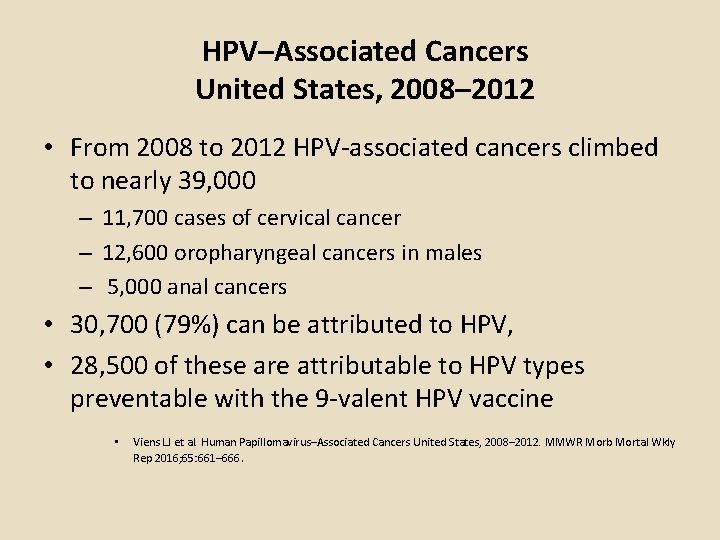
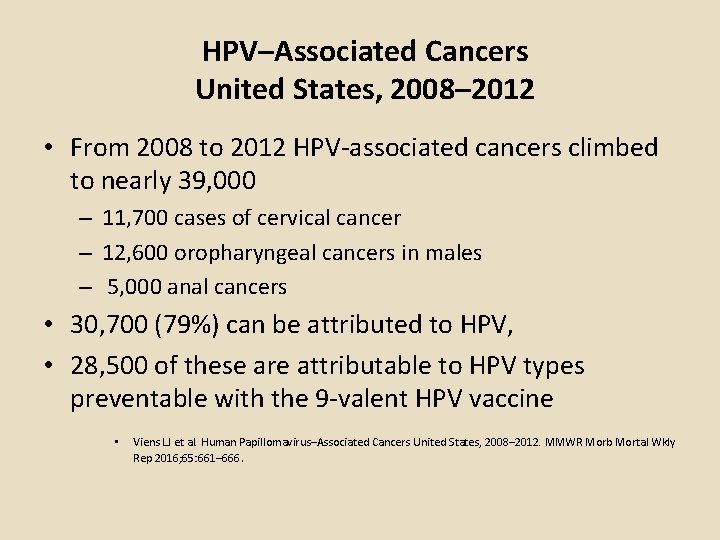
HPV–Associated Cancers United States, 2008– 2012 • From 2008 to 2012 HPV-associated cancers climbed to nearly 39, 000 – 11, 700 cases of cervical cancer – 12, 600 oropharyngeal cancers in males – 5, 000 anal cancers • 30, 700 (79%) can be attributed to HPV, • 28, 500 of these are attributable to HPV types preventable with the 9 -valent HPV vaccine • Viens LJ et al. Human Papillomavirus–Associated Cancers United States, 2008– 2012. MMWR Morb Mortal Wkly Rep 2016; 65: 661– 666.

HPV Infection & Disease: Understanding the Burden • Almost ALL will be infected with at least 1 type HPV at some point • Most will never know they’ve been infected – Can occur with any intimate sexual contact – Intercourse is not necessary for infection • Estimated 79 million Americans currently infected – 14 million new infections/year in the US – Prior to HPV Vax 350, 000 affected by warts every year – HPV infection most common in teens - 20 s Jemal A et al. J Natl Cancer Inst 2013; 105: 175 -201
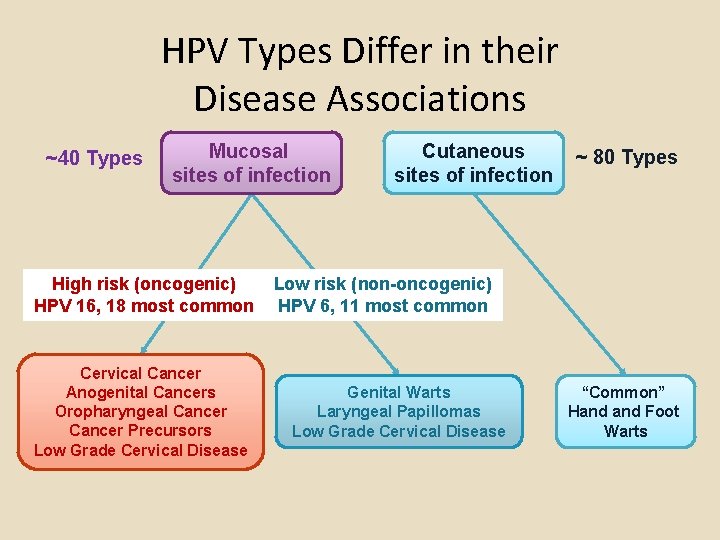
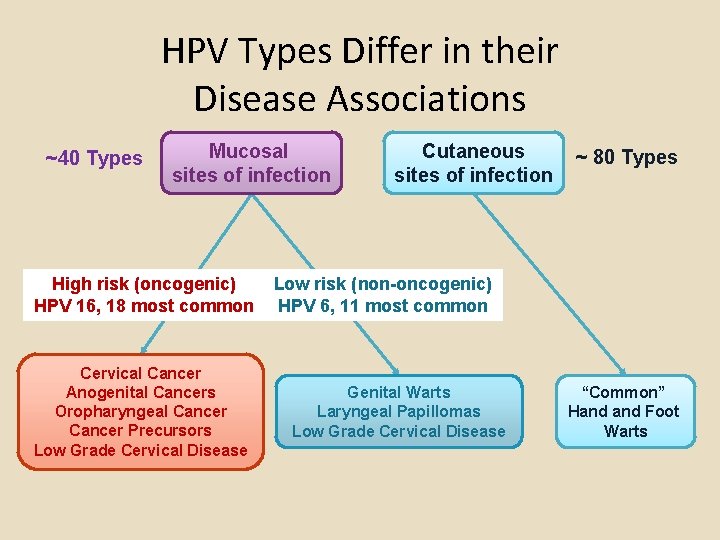
HPV Types Differ in their Disease Associations ~40 Types Mucosal sites of infection High risk (oncogenic) HPV 16, 18 most common Cervical Cancer Anogenital Cancers Oropharyngeal Cancer Precursors Low Grade Cervical Disease Cutaneous sites of infection ~ 80 Types Low risk (non-oncogenic) HPV 6, 11 most common Genital Warts Laryngeal Papillomas Low Grade Cervical Disease “Common” Hand Foot Warts

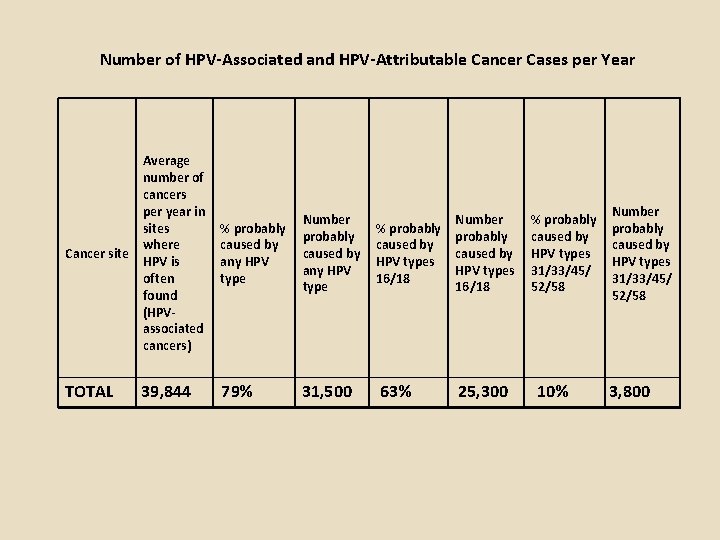
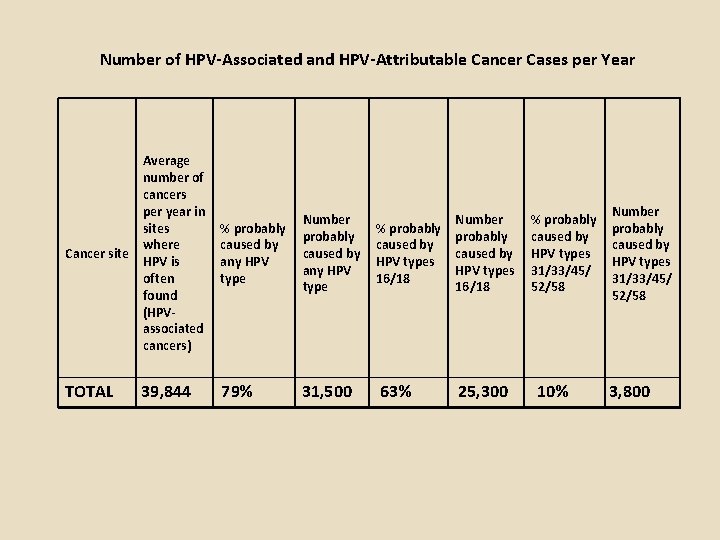
Number of HPV-Associated and HPV-Attributable Cancer Cases per Year Average number of cancers per year in sites where Cancer site HPV is often found (HPVassociated cancers) % probably caused by any HPV type Number probably caused by any HPV type TOTAL 79% 31, 500 39, 844 % probably caused by HPV types 16/18 63% Number probably caused by HPV types 16/18 25, 300 % probably caused by HPV types 31/33/45/ 52/58 10% Number probably caused by HPV types 31/33/45/ 52/58 3, 800

Number of HPV-Associated Cancers by Year and Sex, United States, 2003– 2013

National Health and Nutrition Examination Survey : 2011 - 2014 • 12% of U. S. men are infected with oral HPV – Prevalence among women is 3%. – High-risk oral HPV infection: 7% men & 1%women – In men, oral HPV prevalence highest at ages 50– 54 • Among men and women with same-sex partners – High-risk oral HPV found in 13% and 4%, respectively • Prevalence high-risk oral HPV with >=2 same-sex oral sex partners 22% • Oral HPV infection more common with concurrent genital HPV infection
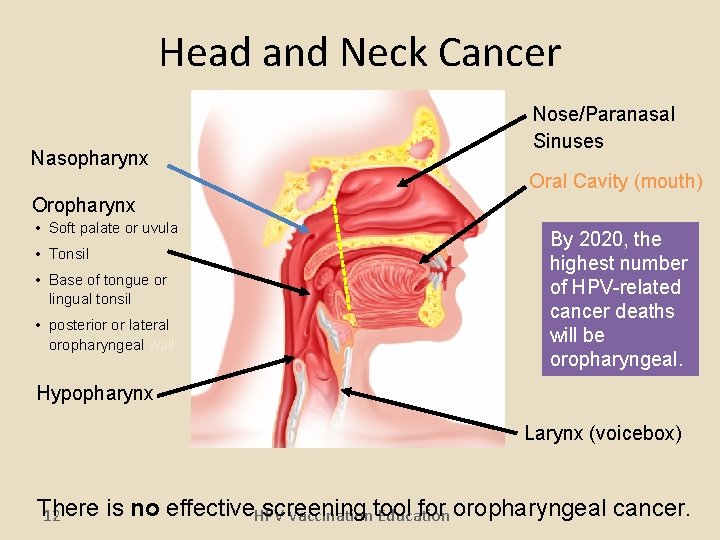
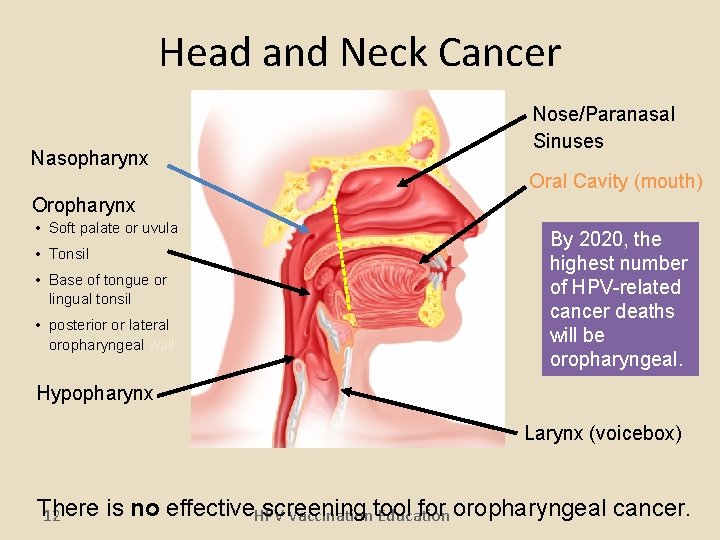
Head and Neck Cancer Nasopharynx Nose/Paranasal Sinuses Oral Cavity (mouth) Oropharynx • Soft palate or uvula • Tonsil • Base of tongue or lingual tonsil • posterior or lateral oropharyngeal wall By 2020, the highest number of HPV-related cancer deaths will be oropharyngeal. Hypopharynx Larynx (voicebox) There is no effective. HPV Vaccination Education screening tool for oropharyngeal cancer. 12
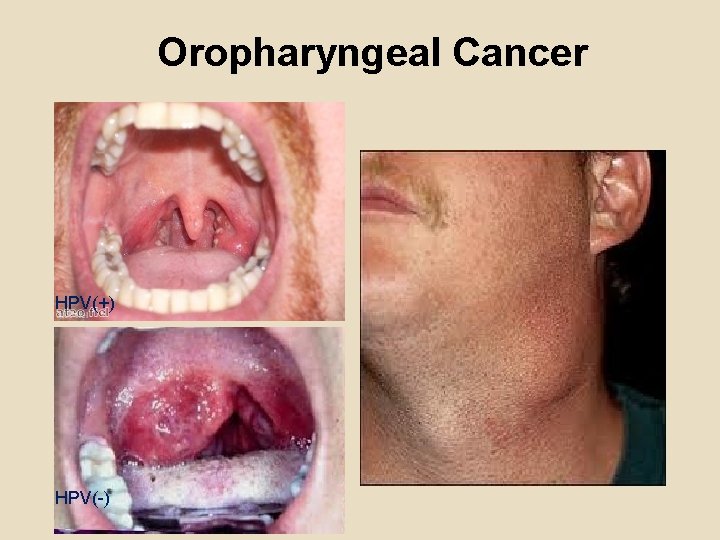
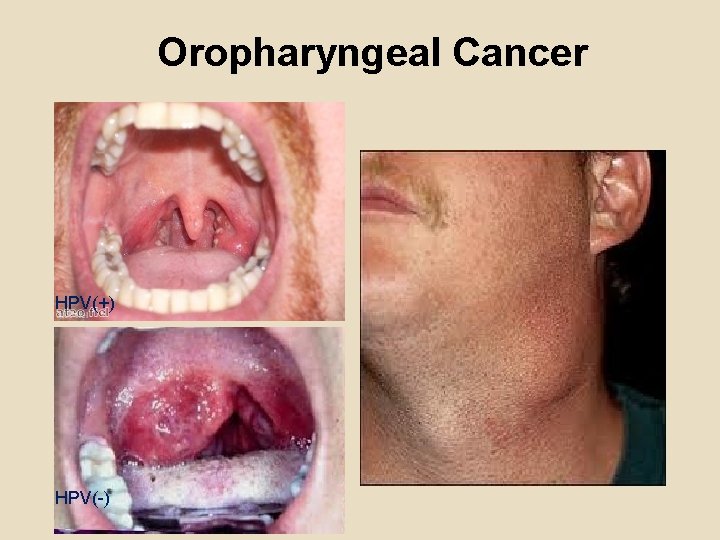
Oropharyngeal Cancer HPV(+) HPV(-)

HPV Prophylactic Vaccines • Recombinant L 1 capsid proteins that form “virus-like” particles (VLP) • Non-infectious and non-oncogenic • Produce higher levels of neutralizing antibody than natural infection HPV Virus-Like Particle
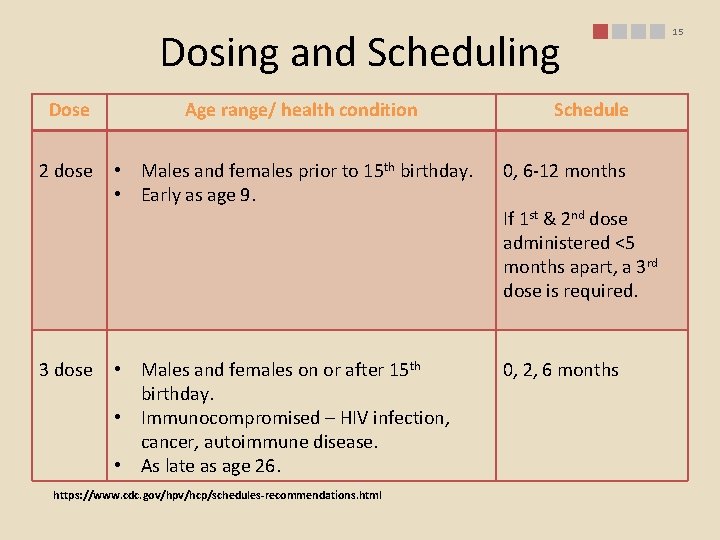
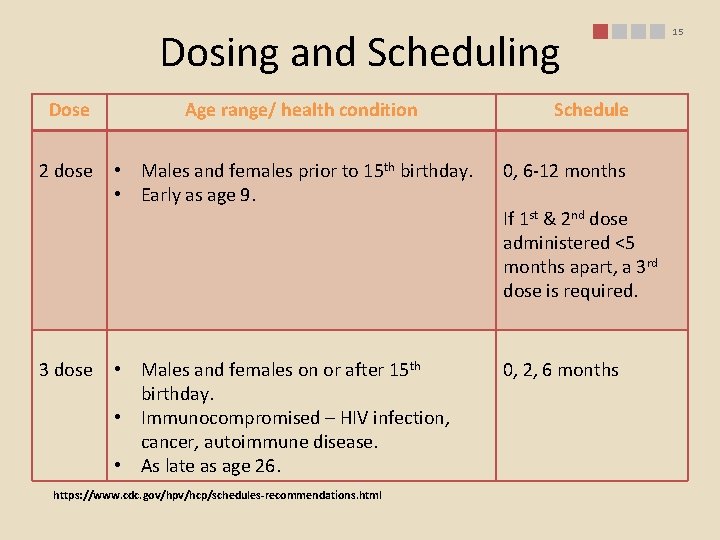
Dosing and Scheduling Dose 2 dose 3 dose Age range/ health condition Schedule • Males and females prior to 15 th birthday. • Early as age 9. 0, 6 -12 months • Males and females on or after 15 th birthday. • Immunocompromised – HIV infection, cancer, autoimmune disease. • As late as age 26. 0, 2, 6 months https: //www. cdc. gov/hpv/hcp/schedules-recommendations. html If 1 st & 2 nd dose administered <5 months apart, a 3 rd dose is required. 15

Monitoring Impact of HPV Vaccine Programs: HPV-associated Outcomes 16
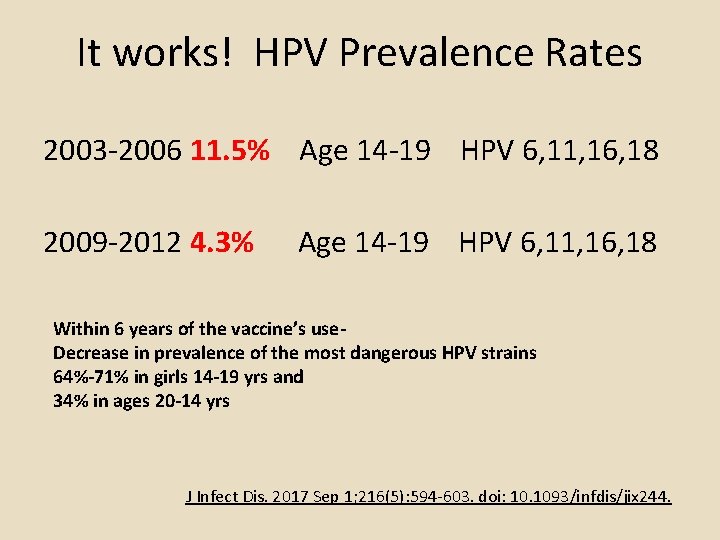
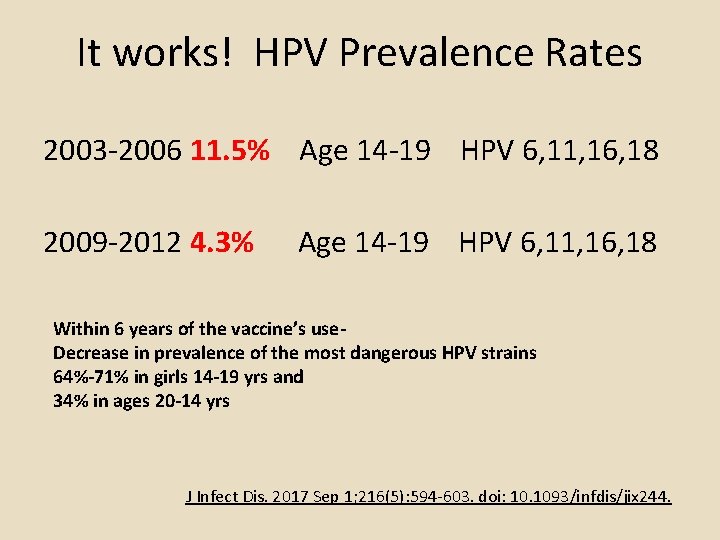
It works! HPV Prevalence Rates 2003 -2006 11. 5% Age 14 -19 HPV 6, 11, 16, 18 2009 -2012 4. 3% Age 14 -19 HPV 6, 11, 16, 18 Within 6 years of the vaccine’s use. Decrease in prevalence of the most dangerous HPV strains 64%-71% in girls 14 -19 yrs and 34% in ages 20 -14 yrs J Infect Dis. 2017 Sep 1; 216(5): 594 -603. doi: 10. 1093/infdis/jix 244.
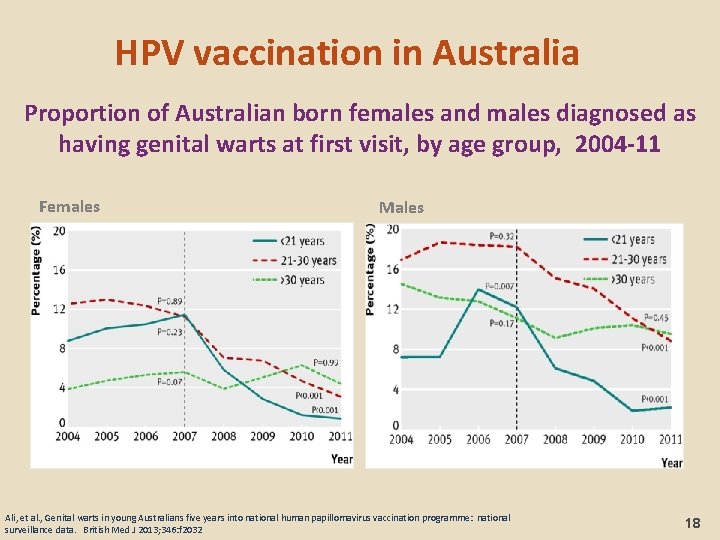
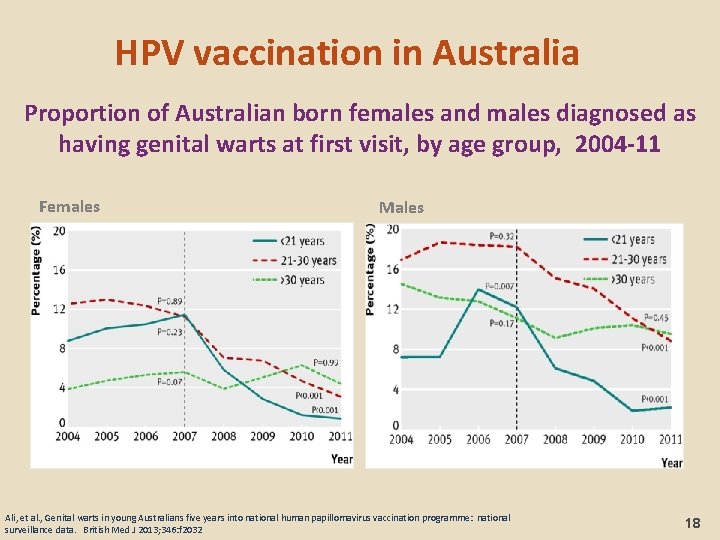
HPV vaccination in Australia Proportion of Australian born females and males diagnosed as having genital warts at first visit, by age group, 2004 -11 Females Males Ali, et al. , Genital warts in young Australians five years into national human papillomavirus vaccination programme: national surveillance data. British Med J 2013; 346: f 2032 18
Recurrent respiratory papillomatosis (RRP) • In United States-800 RRP cases each year – annual medical costs of $123 million • In Australia-new cases of recurrent respiratory papillomatosis in children fell from seven in 2012 to one in 2016. • None of the mothers of the children who were diagnosed with the disease between 2012 and 2016 had been vaccinated against HPV prior to their pregnancy. – Novakovic, D Journal of Infectious Diseases, 2017 https: //doi. org/10. 1093/infdis/jix 498
Reduction in HPV 16/18 -associated high grade cervical lesions (US - 2008 -2012) • Prevalence of HPV 16/18 in CIN 2+ lesions decreased – 53. 6% to 28. 4% among women >= 1 dose (P=<. 001) – Unvaccinated (57. 1% vs 52. 5%; P=. 08) – Unknown vaccination status (55. 0% vs 50. 5%; P=. 71). • Effectiveness for prevention CIN 2+ depends on timing – 21% (95% CI: 1 -37) if initiated vaccination 25 -36 months – 49% (95% CI: 28 -64) ) if initiated vaccination 37 -48 months – 72% (95% CI: 45 -86) if initiated vaccination >48 months prior to the screening test that led to CIN 2+ diagnosis. • Vaccine. 2015 Mar 24; 33(13): 1608 -13.
Impact of Bivalent HPV Vaccine on Oral HPV Infection • Of 7, 466 women 18 -25 yrs randomized to receive HPV vaccine or hepatitis A vaccine – 5, 840 oral specimens at final 4 -year study visit – Oral prevalence of mucosal HPV was low (1. 7%) • 15 HPV 16/18 infections in hepatitis A group vs 1 in HPV vaccine group – estimated vaccine efficacy of 93. 3% Herrero R, et al. Reduced prevalence of oral human papillomavirus (HPV) 4 years after bivalent HPV vaccination in a randomized clinical trial in Costa Rica. PLOS ONE 2013; 8: e 68329 21
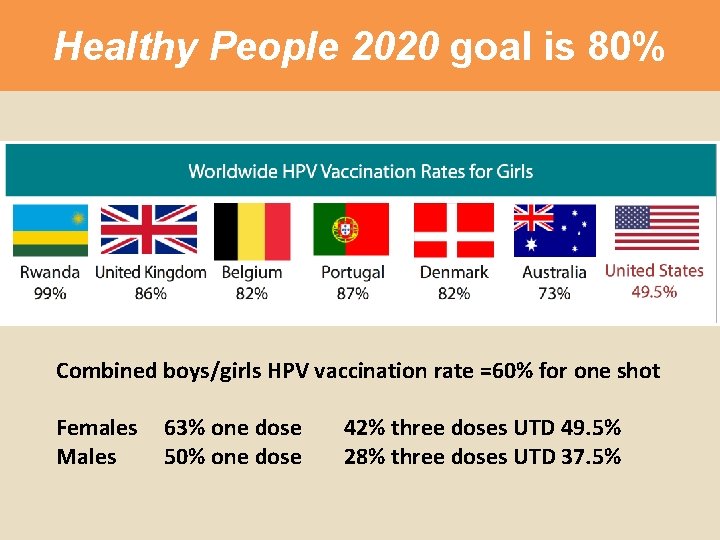
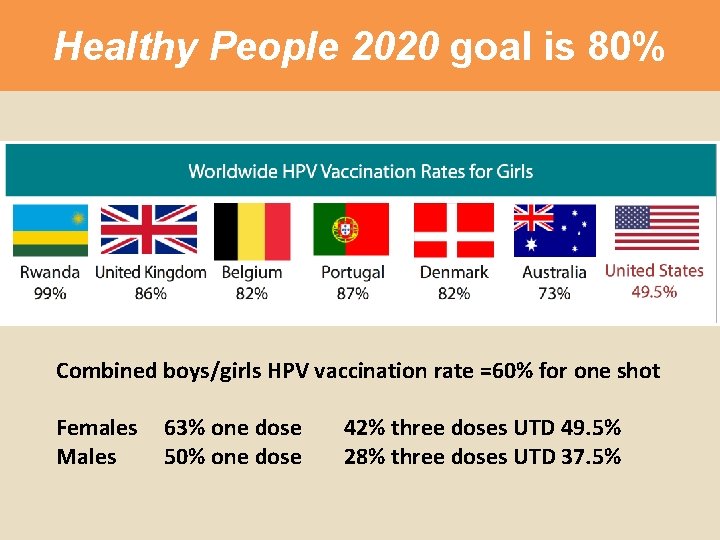
Healthy People 2020 goal is 80% Combined boys/girls HPV vaccination rate =60% for one shot Females Males 63% one dose 50% one dose 42% three doses UTD 49. 5% 28% three doses UTD 37. 5%
NIS-TEEN DATA, 2016 Texas Data

States with the Highest HPV Vaccination Rates All Adolescents (N = 20, 475) UTD 80 70. 8 70 60 55. 7 54 52. 7 51. 2 55. 7 62 56. 9 56. 6 56 50 US Overall Series UTD: 43. 4% 40 30 20 10 an d a bi od e Rh ol ric to f. C Isl um w la Di st De hu as sa c M ar e ts se t ne ai M Yo rk w Ne on t rm Ve i ai w Ha Da No rth Ne w Ha m ps hi re ko ta 0 Walker, T. Y. , Elam-Evans, L. D. , Singleton, J. A. , Yankey, D. , Markowitz, L. E. , Fredua, B. , Williams, C. L. , Meyer, S. A. , Stokley, S. (2017). National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13 -17 Years – United States, 2016. Morbidity and Mortality Weekly Report, 66(33), 874 -882. NIS-Teen Data, 2016

States with the Lowest HPV Vaccination Rates All Adolescents (N = 20, 475) UTD 40 35 30 26. 7 29. 1 30. 5 32. 9 33. 9 34 34. 5 35. 4 35. 6 Arkansas Alabama Kansas US Overall Series UTD: 43. 4% 25 20 15 10 5 0 Wyoming South Mississippi Carolina Utah Texas Indiana Kentucky Walker, T. Y. , Elam-Evans, L. D. , Singleton, J. A. , Yankey, D. , Markowitz, L. E. , Fredua, B. , Williams, C. L. , Meyer, S. A. , Stokley, S. (2017). National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13 -17 Years – United States, 2016. Morbidity and Mortality Weekly Report, 66(33), 874 -882. NIS-Teen Data, 2016
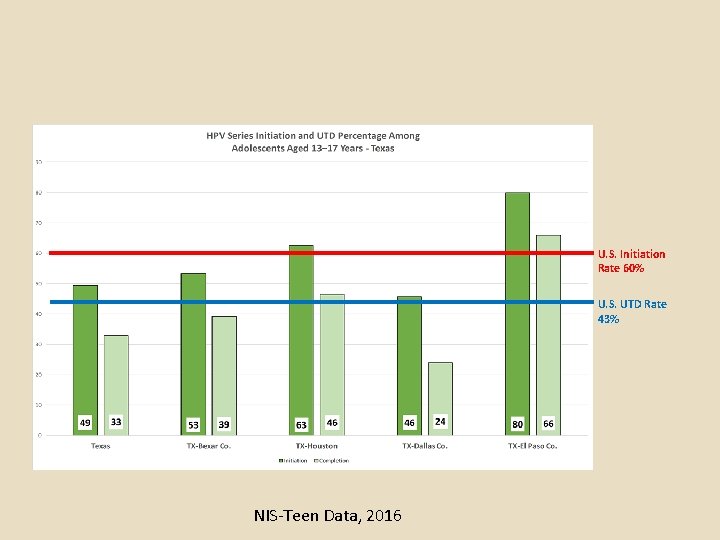
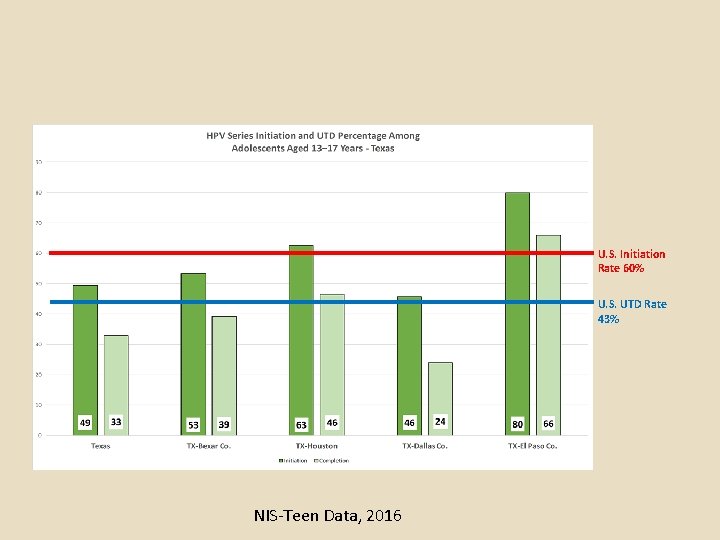
U. S. Initiation Rate 60% U. S. UTD Rate 43% NIS-Teen Data, 2016
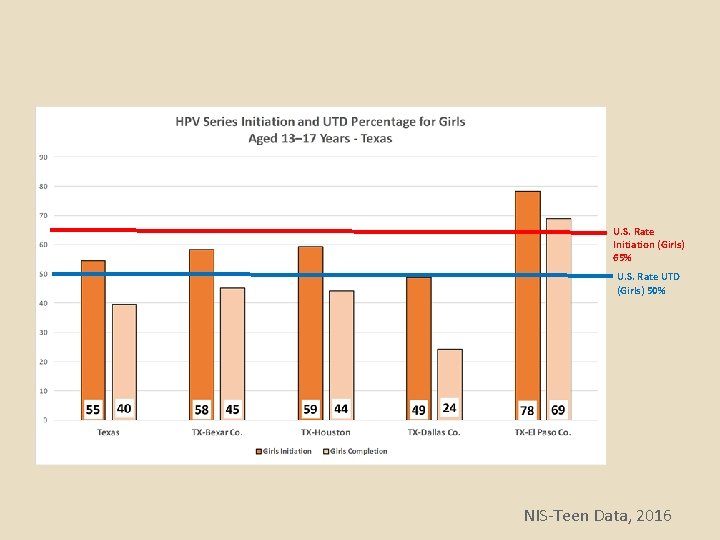
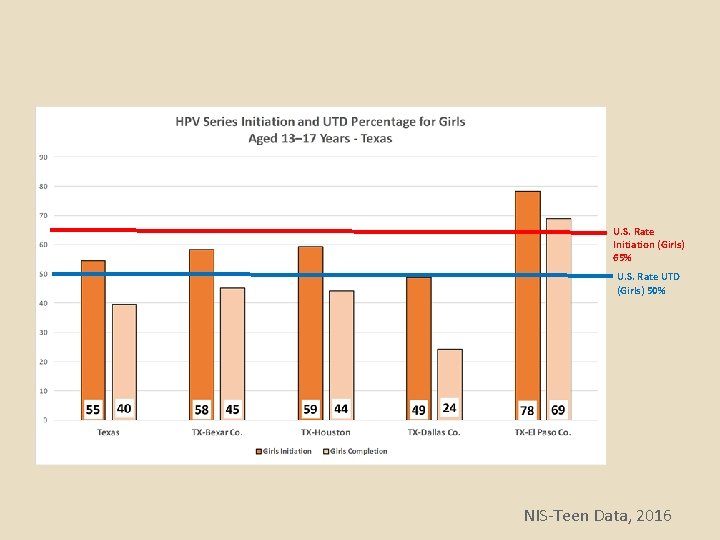
U. S. Rate Initiation (Girls) 65% U. S. Rate UTD (Girls) 50% NIS-Teen Data, 2016
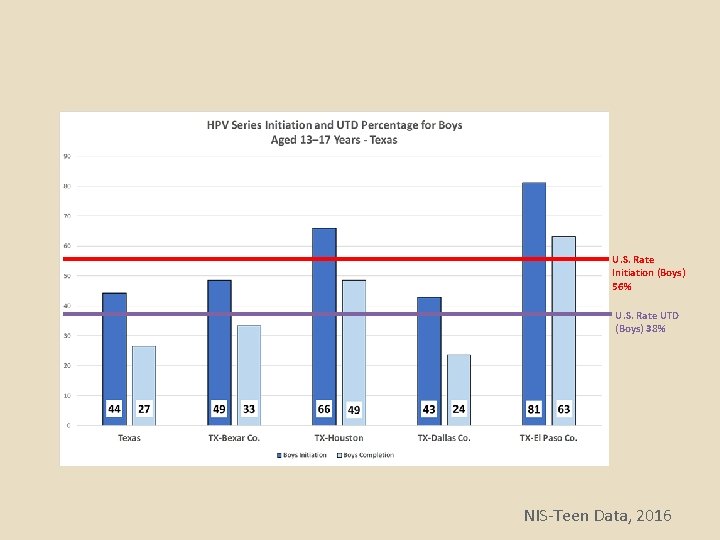
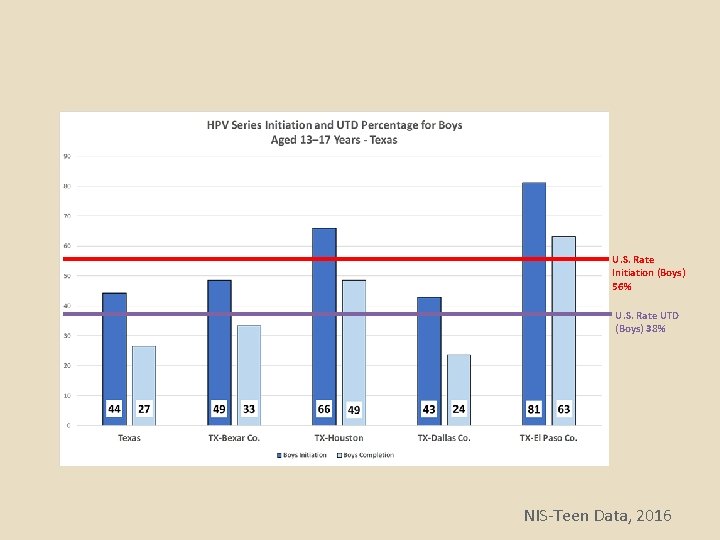
U. S. Rate Initiation (Boys) 56% U. S. Rate UTD (Boys) 38% NIS-Teen Data, 2016

U. S. Rate Initiation (Girls) 65% U. S. Rate Initiation (Boys) 56% NIS-Teen Data, 2016
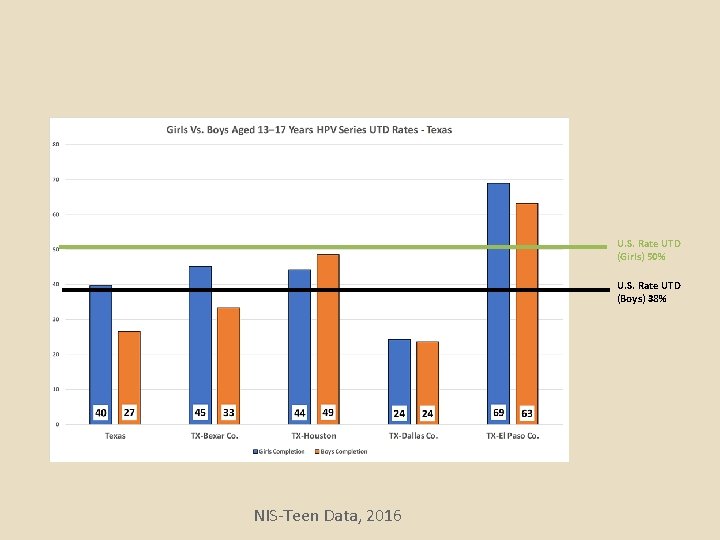
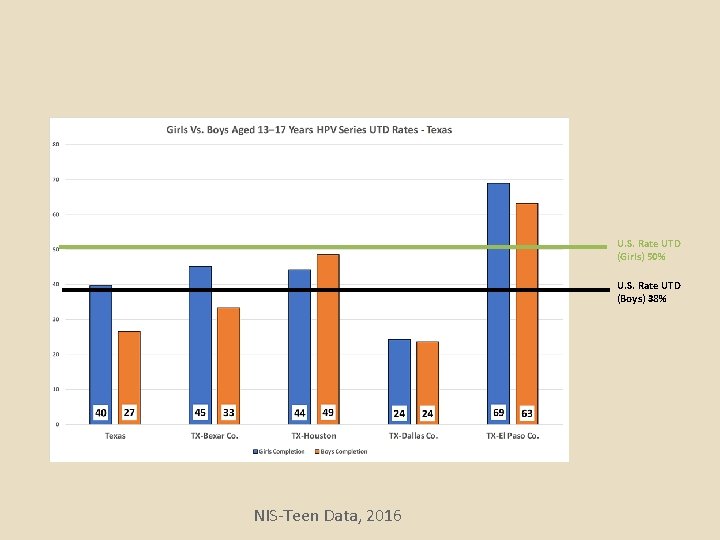
U. S. Rate UTD (Girls) 50% U. S. Rate UTD (Boys) 38% NIS-Teen Data, 2016

Local Reporting of HPV Data
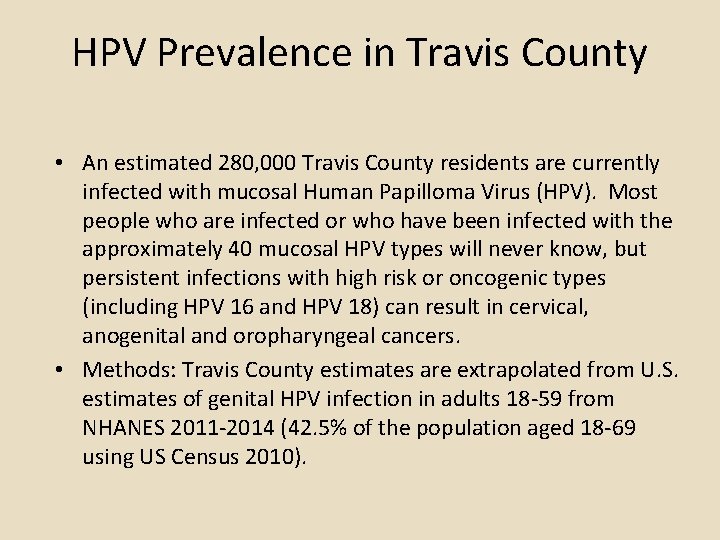
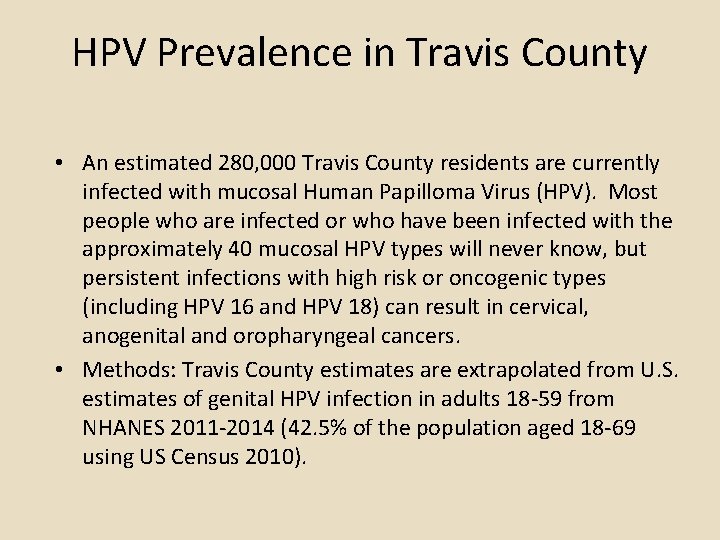
HPV Prevalence in Travis County • An estimated 280, 000 Travis County residents are currently infected with mucosal Human Papilloma Virus (HPV). Most people who are infected or who have been infected with the approximately 40 mucosal HPV types will never know, but persistent infections with high risk or oncogenic types (including HPV 16 and HPV 18) can result in cervical, anogenital and oropharyngeal cancers. • Methods: Travis County estimates are extrapolated from U. S. estimates of genital HPV infection in adults 18 -59 from NHANES 2011 -2014 (42. 5% of the population aged 18 -69 using US Census 2010).
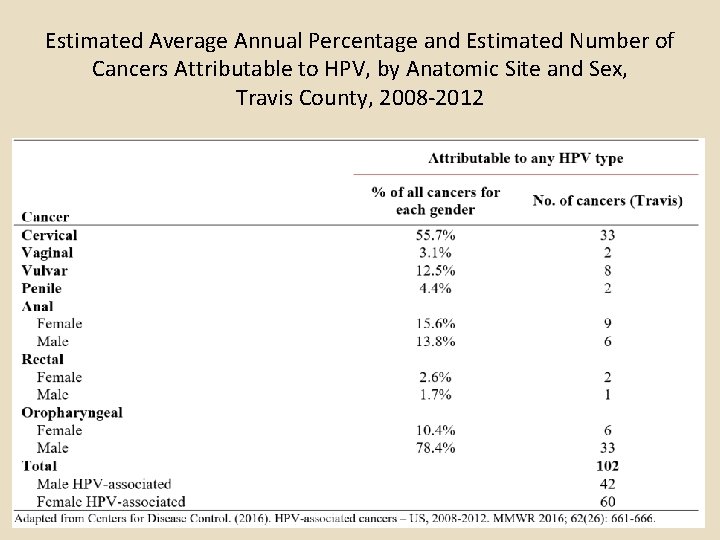
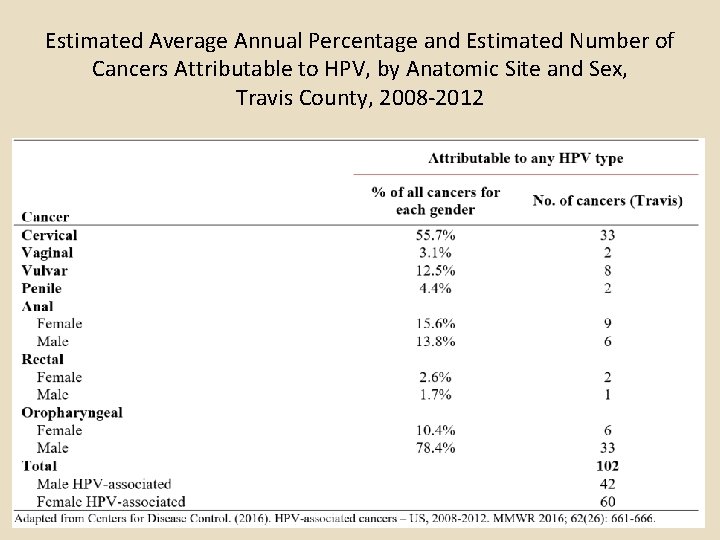
Estimated Average Annual Percentage and Estimated Number of Cancers Attributable to HPV, by Anatomic Site and Sex, Travis County, 2008 -2012

Number of Cases and Incidence Rate of Cervical Cancer, Travis County 2000 -2014
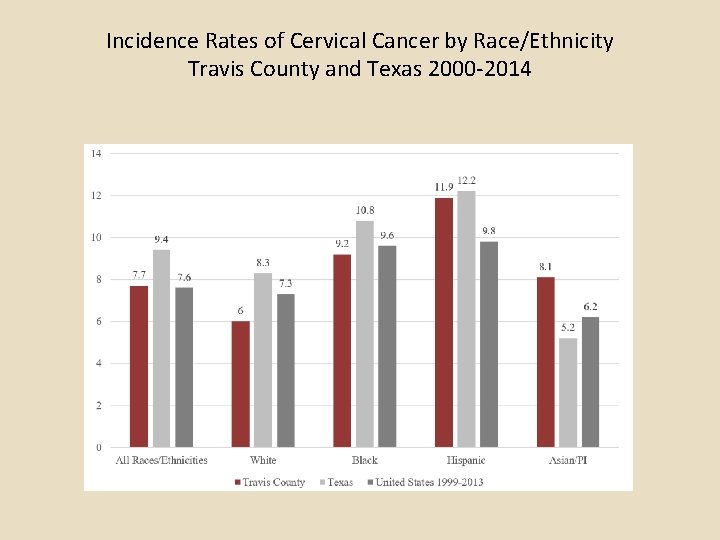
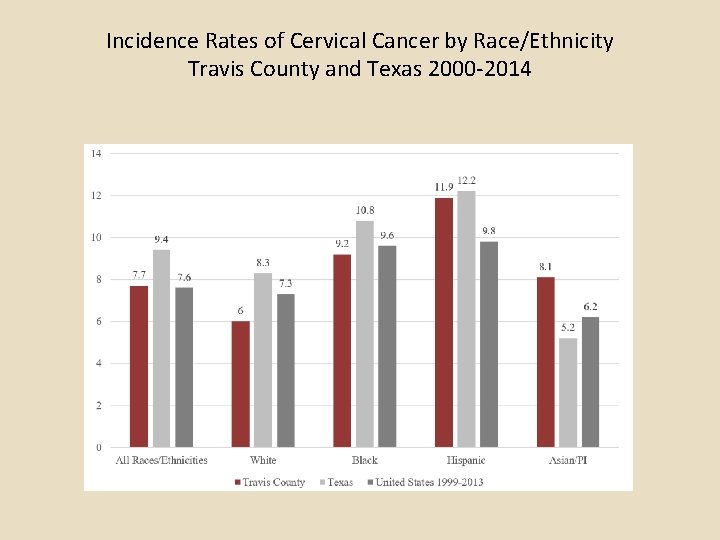
Incidence Rates of Cervical Cancer by Race/Ethnicity Travis County and Texas 2000 -2014
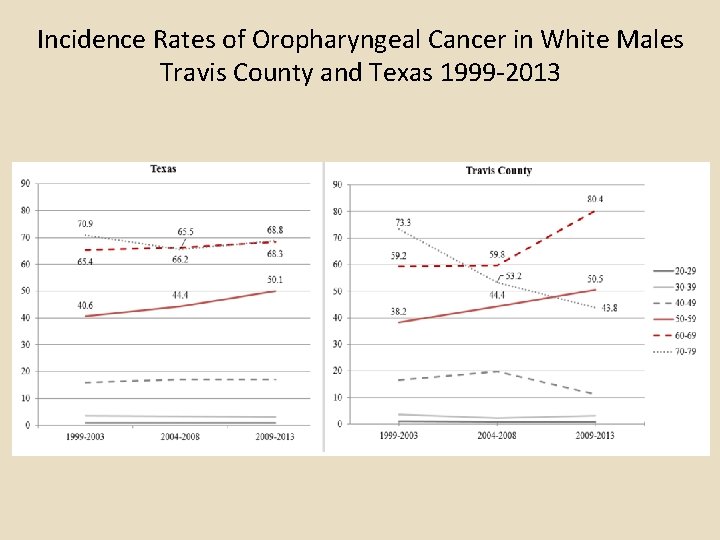
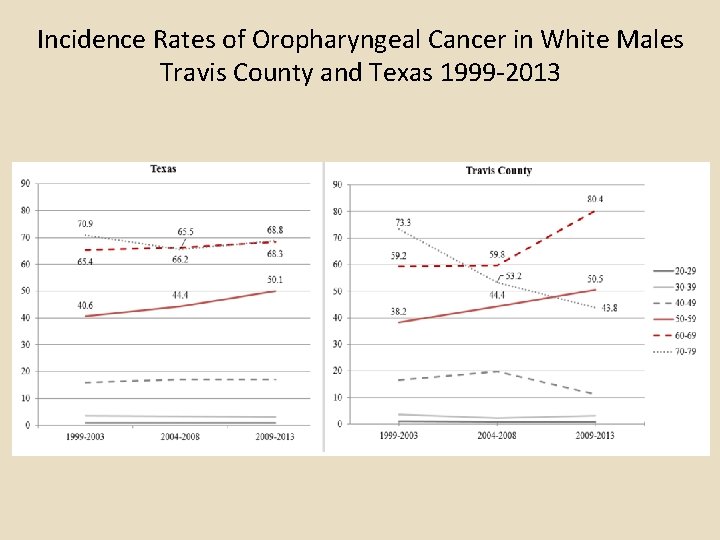
Incidence Rates of Oropharyngeal Cancer in White Males Travis County and Texas 1999 -2013
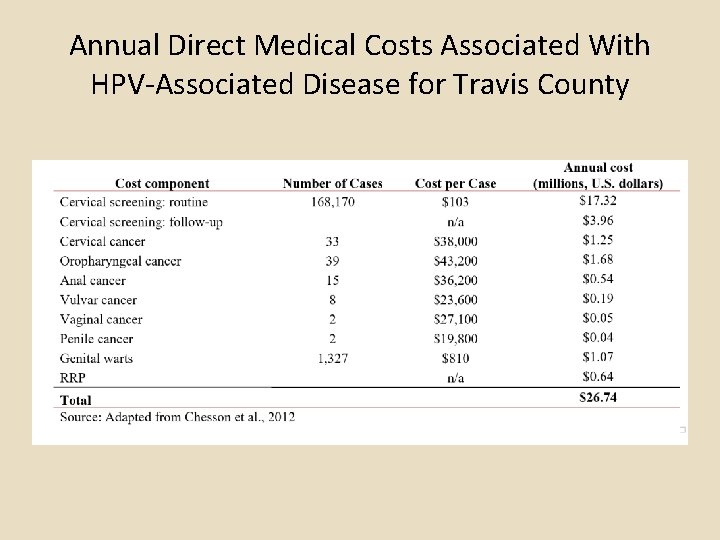
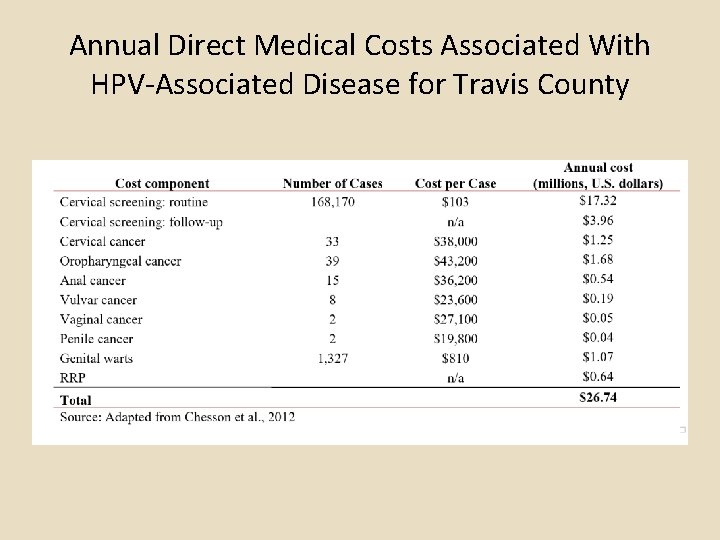
Annual Direct Medical Costs Associated With HPV-Associated Disease for Travis County
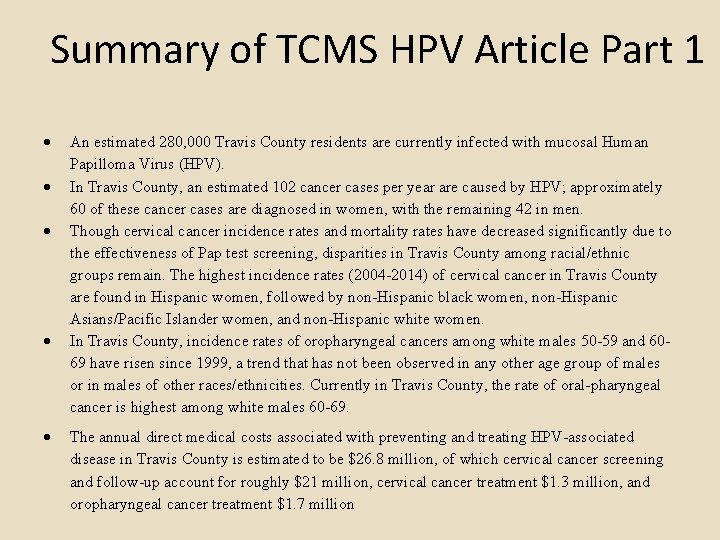
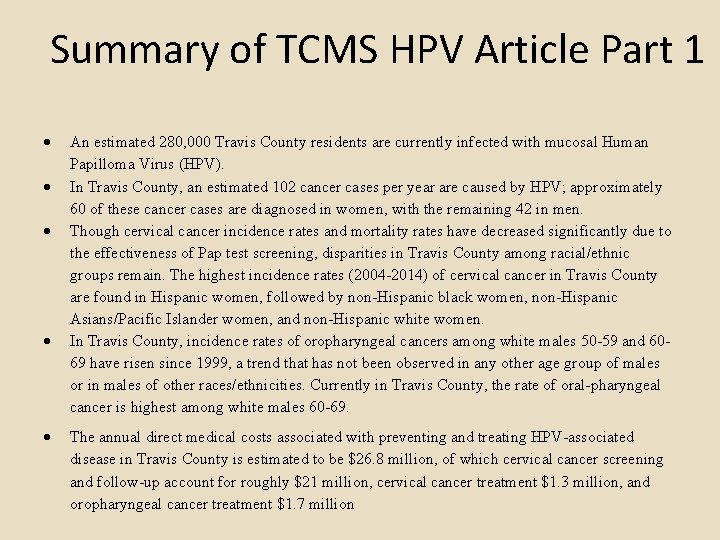
Summary of TCMS HPV Article Part 1 An estimated 280, 000 Travis County residents are currently infected with mucosal Human Papilloma Virus (HPV). In Travis County, an estimated 102 cancer cases per year are caused by HPV; approximately 60 of these cancer cases are diagnosed in women, with the remaining 42 in men. Though cervical cancer incidence rates and mortality rates have decreased significantly due to the effectiveness of Pap test screening, disparities in Travis County among racial/ethnic groups remain. The highest incidence rates (2004 -2014) of cervical cancer in Travis County are found in Hispanic women, followed by non-Hispanic black women, non-Hispanic Asians/Pacific Islander women, and non-Hispanic white women. In Travis County, incidence rates of oropharyngeal cancers among white males 50 -59 and 6069 have risen since 1999, a trend that has not been observed in any other age group of males or in males of other races/ethnicities. Currently in Travis County, the rate of oral-pharyngeal cancer is highest among white males 60 -69. The annual direct medical costs associated with preventing and treating HPV-associated disease in Travis County is estimated to be $26. 8 million, of which cervical cancer screening and follow-up account for roughly $21 million, cervical cancer treatment $1. 3 million, and oropharyngeal cancer treatment $1. 7 million
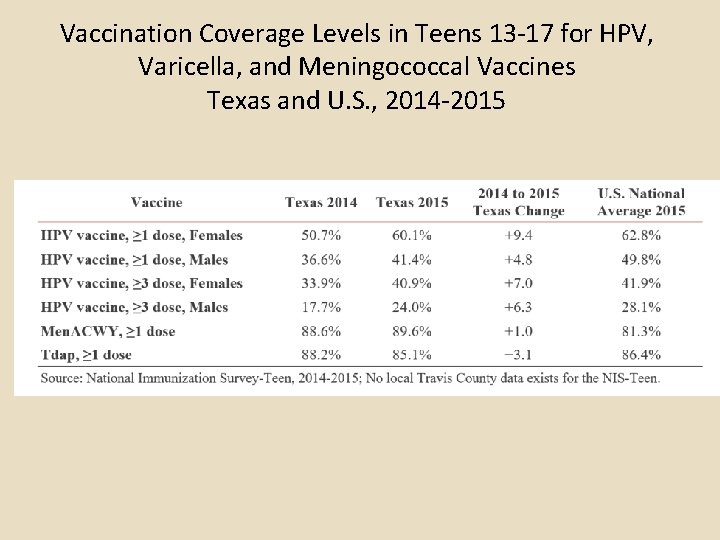
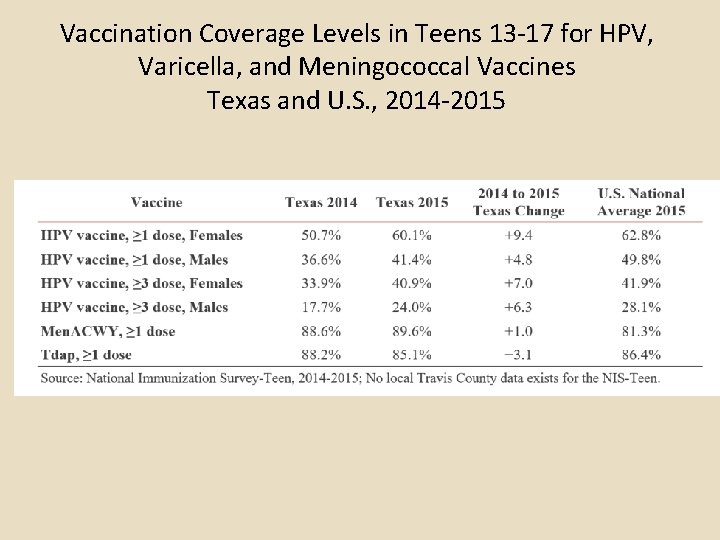
Vaccination Coverage Levels in Teens 13 -17 for HPV, Varicella, and Meningococcal Vaccines Texas and U. S. , 2014 -2015


Factors Regarding HPV Vaccine Uptake • Systematic review of the literature on barriers to HPV vaccination among U. S. adolescents found that a health care professional’s recommendation was one of the most important factors in their decision to obtain HPV vaccination for their children. Additionally, systematic review of interventions to increase HPV vaccine uptake found that providers pose a more significant barrier to vaccine series initiation while patients or families pose a barrier to series completion. Thus, interventions targeting patients and providers have the greatest potential for success.

Talking to Parents About HPV Vaccine
Why are rates so low? Providers • A clear recommendation from YOU-the provider- Is the main reason parents decide to vaccinate
Recommendations Recommend HPV vaccination in the same way and on the same day as all adolescent vaccines. See the fact sheet on “Talking to Parents about HPV Vaccine”. A summary of recommendations for patient and parent education and for medical practices and providers can be found in Table 2. Additional info, including clinician factsheets, FAQ’s and tools and materials for medical practice offices can be found at: www. cdc. gov/HPV

HPV Vaccine Communications During the Healthcare Encounter • Presented as ‘optional’ vs recommended • Mixed or negative opinions about the ‘new vaccine’ and concerns over safety/efficacy • Hesitant to engage in discussion • Ineffective communication skills • Views that teen not at risk and could delay • Lack knowledge about HPV or vaccine • Miss opportunities (few visits for adolescents) Goff S et al. Vaccine 2011; 10: 7343 -9 Hughes C et al. BMC Pediatrics 2011; 11: 74
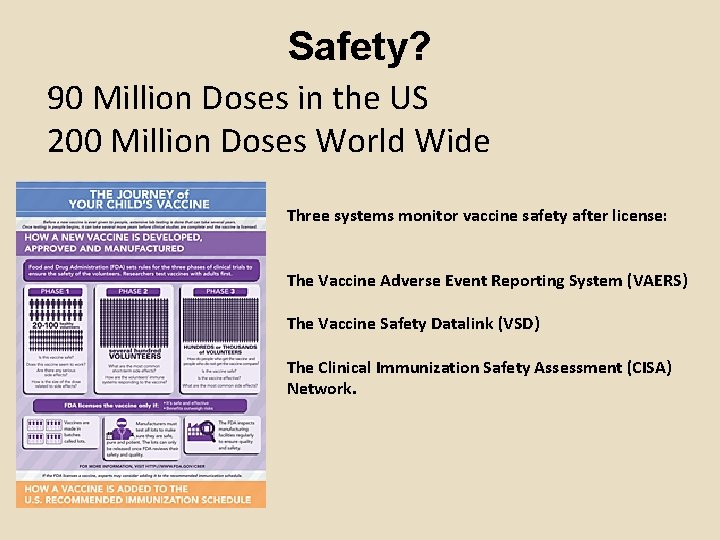
Safety? 90 Million Doses in the US 200 Million Doses World Wide Three systems monitor vaccine safety after license: The Vaccine Adverse Event Reporting System (VAERS) The Vaccine Safety Datalink (VSD) The Clinical Immunization Safety Assessment (CISA) Network.
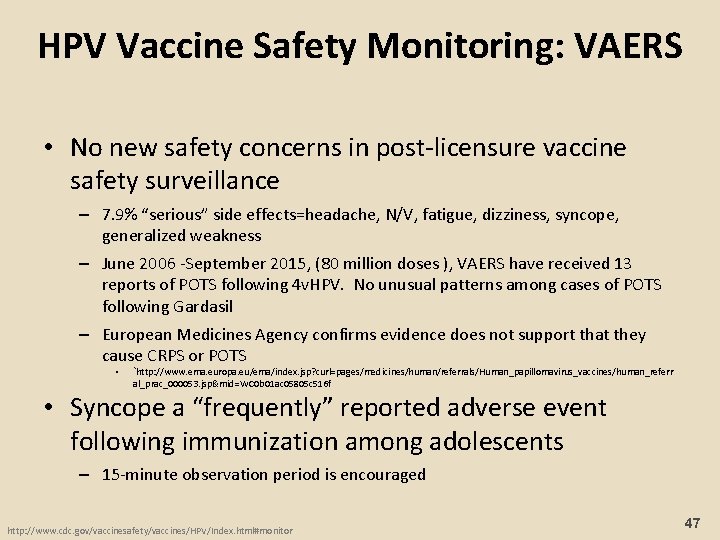
HPV Vaccine Safety Monitoring: VAERS • No new safety concerns in post-licensure vaccine safety surveillance – 7. 9% “serious” side effects=headache, N/V, fatigue, dizziness, syncope, generalized weakness – June 2006 -September 2015, (80 million doses ), VAERS have received 13 reports of POTS following 4 v. HPV. No unusual patterns among cases of POTS following Gardasil – European Medicines Agency confirms evidence does not support that they cause CRPS or POTS • `http: //www. ema. europa. eu/ema/index. jsp? curl=pages/medicines/human/referrals/Human_papillomavirus_vaccines/human_referr al_prac_000053. jsp&mid=WC 0 b 01 ac 05805 c 516 f • Syncope a “frequently” reported adverse event following immunization among adolescents – 15 -minute observation period is encouraged http: //www. cdc. gov/vaccinesafety/vaccines/HPV/Index. html#monitor 47
Evidence Based Interventions
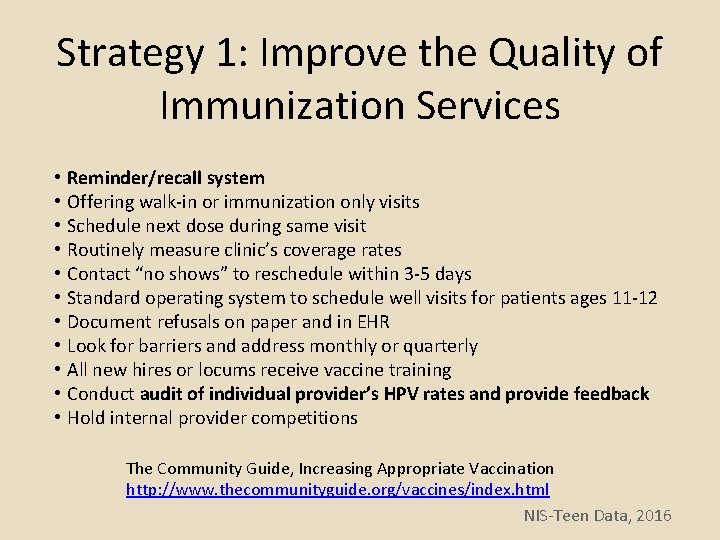
Strategy 1: Improve the Quality of Immunization Services • • • Reminder/recall system Offering walk-in or immunization only visits Schedule next dose during same visit Routinely measure clinic’s coverage rates Contact “no shows” to reschedule within 3 -5 days Standard operating system to schedule well visits for patients ages 11 -12 Document refusals on paper and in EHR Look for barriers and address monthly or quarterly All new hires or locums receive vaccine training Conduct audit of individual provider’s HPV rates and provide feedback Hold internal provider competitions The Community Guide, Increasing Appropriate Vaccination http: //www. thecommunityguide. org/vaccines/index. html NIS-Teen Data, 2016
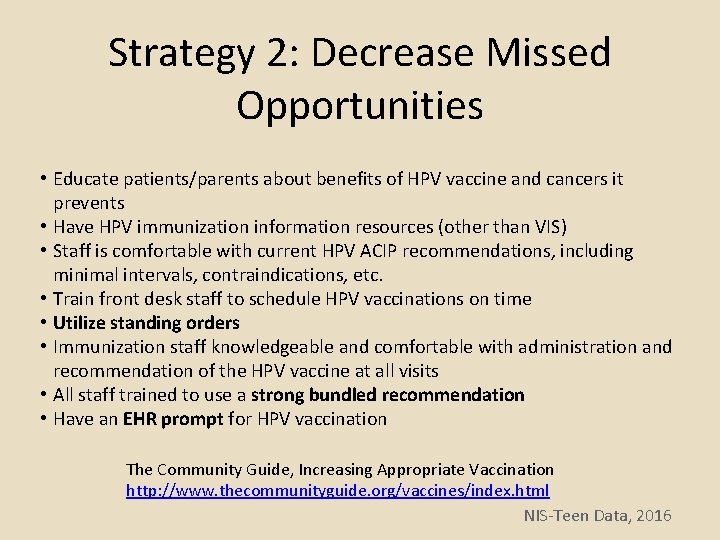
Strategy 2: Decrease Missed Opportunities • Educate patients/parents about benefits of HPV vaccine and cancers it prevents • Have HPV immunization information resources (other than VIS) • Staff is comfortable with current HPV ACIP recommendations, including minimal intervals, contraindications, etc. • Train front desk staff to schedule HPV vaccinations on time • Utilize standing orders • Immunization staff knowledgeable and comfortable with administration and recommendation of the HPV vaccine at all visits • All staff trained to use a strong bundled recommendation • Have an EHR prompt for HPV vaccination The Community Guide, Increasing Appropriate Vaccination http: //www. thecommunityguide. org/vaccines/index. html NIS-Teen Data, 2016
Strategy 3: Improve Completeness and Accuracy of Immunization Data • Have your EHR upload vaccine administration information to your state/city immunization information system (IIS) on a regular basis • Manually input (not scan) information on immunizations previously administered to your patients by other providers into your clinic EHR • Review and utilize the state/city IIS before or during each patient visit to determine which immunizations are due The Community Guide, Increasing Appropriate Vaccination http: //www. thecommunityguide. org/vaccines/index. html NIS-Teen Data, 2016

State and Local Efforts to Promote HPV • Texas HPV Coalition: http: //www. texascancer. info/hpv/ • Texas Medical Association https: //www. texmed. org/HPV/ • Cancer Alliance of Texas http: //cancerallianceoftexas. org q. Texas Department of State Health Services https: //www. dshs. texas. gov/hivstd/info/hpv/

Texas HPV Coalition Tx. HPVCoalition

Provider Training Task Group 2017 PRODUCTS
HPV Vaccination Clearinghouse Resources, information and educational opportunities http: //bit. ly/HPVClearinghouse
Oropharyngeal Video: s u r p u l o e H ease incr s! te a w d e vi 0 to 1, 15 bit. ly/HPV_Oro. Video

Free CME E-Learning for Pediatric & Primary Care Providers CREDIT: https: //www. cmeuniversity. com/course/disclaimer/114605#01 NON-CREDIT: http: //bit. ly/Provider. HPVVideo



Acknowledgements Austin Public Health • Sarah Seidel • Anna Klioueva MD Anderson HPV Moonshot Team • Lori Stevens • Rosalind Bello • Melissa Mims • Bridgette Ma
Questions? HPVMoonshot. Team@mdanderson. org Lois Ramondetta, MD Professor, Department of Gynecologic Oncology and Reproductive Medicine The University of Texas MD Anderson Cancer Center. Co Lead MD Anderson HPV Cancer Moonshot lramonde@mdanderson. org Philip Huang, MD, MPH Health Authority/Medical Director Austin Public Health Philip. Huang@Austin. Texas. gov 512 -972 -5855
Evidence-Based HPV Disease Prevention HPV VACCINE
 Hpv cancer prevention
Hpv cancer prevention Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention High sierra ahec
High sierra ahec Hpv cervical cancer
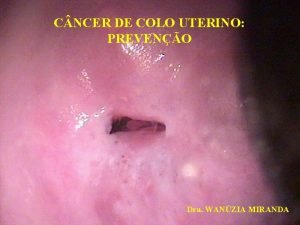
Hpv cervical cancer Hpv cervical cancer
Hpv cervical cancer Prevention hpv
Prevention hpv Health promotion and levels of disease prevention
Health promotion and levels of disease prevention Health promotion and levels of disease prevention
Health promotion and levels of disease prevention Hpv type 16 and 18
Hpv type 16 and 18 Hpv type 16 and 18
Hpv type 16 and 18 Hpv test for men
Hpv test for men Hpv vaccine schedule adults
Hpv vaccine schedule adults Hpv testi nasıl yapılır
Hpv testi nasıl yapılır Triage sort
Triage sort Does hpv go away
Does hpv go away Paplloma
Paplloma Swede score kolposkopi
Swede score kolposkopi Bivalan opa
Bivalan opa Hsil
Hsil Cancerscreening.gov.au
Cancerscreening.gov.au Hpv nic
Hpv nic Hpv us
Hpv us Hpv dna testi
Hpv dna testi Hpv infektion
Hpv infektion Hpv
Hpv How to get hpv
How to get hpv Hpv
Hpv Hpv infection
Hpv infection Epidermal dysplasia verruciformis
Epidermal dysplasia verruciformis Ahcc hpv
Ahcc hpv Hpv discret test
Hpv discret test Cervixdysplasie
Cervixdysplasie Trendlines and regression analysis
Trendlines and regression analysis Lois dohm
Lois dohm The giver chapter 1-5 vocabulary
The giver chapter 1-5 vocabulary What is the theme of the giver
What is the theme of the giver Lois lowery
Lois lowery Loi de nernst
Loi de nernst What does the sled symbolize in the giver
What does the sled symbolize in the giver Lois lowry website
Lois lowry website Loi des rendements décroissants
Loi des rendements décroissants Loi de proust
Loi de proust Loi des circuits
Loi des circuits Lois de newton
Lois de newton 4 lois spirituel
4 lois spirituel John lowry artist
John lowry artist Lois mailou jones facts
Lois mailou jones facts 5 mars 2007
5 mars 2007 Locked in time
Locked in time Lois fried
Lois fried Lois olson sdsu
Lois olson sdsu Lois levitan
Lois levitan Loi des exposants
Loi des exposants Joanna liivak
Joanna liivak Leaf man by lois ehlert
Leaf man by lois ehlert Lois dohm
Lois dohm Lois s hornsby
Lois s hornsby Lois kim
Lois kim Lois des exposants
Lois des exposants Lois ehlert
Lois ehlert La loi dohm
La loi dohm Kentucky real estate license renewal
Kentucky real estate license renewal Lois ramondetta
Lois ramondetta